Abstract
Background
Adverse events occur frequently at emergency departments (ED) because of several risk factors related to varying conditions. It is still unclear, which factors lead to patient safety incident reports.
The aim of this study was to explore the root causes behind ED-associated patient safety incidents reported by personnel, and based on the findings, to suggest learning objectives for improving patient safety.
Methods
The study material included incident reports (n = 340) which concerned the ED of a teaching hospital over one year. We used a mixed method combining quantitative descriptive statistics and qualitative research by inductive content analysis and deductive Ishikawa root cause analysis.
Results
Most (76.5%) incidents were reported after patient transfer from the ED. Nurses reported 70% of incidents and physicians 7.4%. Of the reports, 40% were related to information flow or management. Incidents were evaluated as no harm (29.4%), mild (46%), moderate (19.7%), and severe (1.2%) harm to the patient. The main consequences for the organization were reputation loss (44.1%) and extra work (38.9%).
In the qualitative analysis, nine specific problem groups were found: insufficient introduction, adherence to guidelines and protocols, insufficient human resources, deficient professional skills, medication management deficiencies, incomplete information transfer from the ED, language proficiency, unprofessional behaviour, identification error, and patient-dependent problems.
Six organizational themes were identified: medical staff orientation, onboarding and competence requirements; human resources; electronic medical records and information transfer; medication documentation system; interprofessional collaboration; resources for specific patient groups such as geriatric, mental health, and patients with substance abuse disorder. Entirely human factor-related themes could not be defined because their associations with system factors were complex and multifaceted.
Individual and organizational learning objectives were addressed, such as adherence to the proper use of instructions and adequate onboarding.
Conclusions
System factors caused most of the patient safety incidents reported concerning ED. The introduction and training of ED -processes is elementary, as is multiprofessional collaboration. More research is needed about teamwork skills, patients with special needs and non-critical patients, and the reporting of severe incidents.
Keywords: Emergency department, Incident report, Information flow, Communication, Introduction, Teamwork, Medication record, Workload, Patient safety
Introduction
In the last 25 years, patient safety in health care began to be noted more widely by increased research. Human and system factors in healthcare and their role in patient safety were recognized [1, 2]. Preventing death and injury from medical errors requires systemwide changes and human factors must be observed when building a healthcare organization [3].
Data from Sweden during 2013–2019 shows that about 12% of patients admitted to hospital suffered from adverse events and over half of these events were estimated to be preventable [4]. Preventable mortality in hospitalized patients seems to be the 15th leading cause of death in the USA and still requires the attention of policymakers, hospital management and professionals [5]. The emergency department is a special operating environment with many features that cause problems for patient safety: fast pace and constant interruptions [6], working conditions—particularly the stressful working conditions experienced by professionals [7], insufficient medical history and an inadequate examination [8]. The number of actual diagnostic errors in EDs was quite similar to those in the rest of healthcare [8]. However, diagnostic errors occur more frequently in emergency departments than in other hospital units, with certain contributory factors leading to these errors [9]. Nevertheless, there is still a lack of knowledge about the actual root causes behind the problems [10, 11].
The World Health Organization (WHO) defines an incident as any deviation from usual medical care that either causes an injury to the patient (harmful incident) or poses a risk of harm (no harm incidents and near misses) [12]. An incident is any temporary or permanent unwanted effect caused to the patient by the treatment. The effects can be physical, psychological, emotional, social, or financial. An adverse event is a harmful incident that results in preventable harm to a patient. A near miss is an incident in which the patient is not affected. A no harm incident is one in which an event affected a patient but resulted in no discernible harm.
In 2015 in Finland, urgent care in primary health care and the emergency departments of specialized health care were integrated to form larger units called joint EDs, significantly reforming acute health care throughout the country [13]. Most health organizations in Finland use a web-based incident reporting system [14]. Reporting is voluntary and can be done anonymously both by patients and professionals when an event endangering patients’ safety is detected. Evidence on the root causes of adverse events is insufficient and more research is needed to develop methods to improve patient safety worldwide [15]. In this paper the term teamwork includes communication, coordination and cooperation with willingness and ability to communicate and coordinate with each other (comparable to non-technical skills like leadership, teamwork, decision making and situation awareness) [16]. The root causes behind patient safety incidents in EDs have not been studied in Finland. The purpose of our study was to recognize the root causes of patient safety incidents and map how to influence the underlying risks of adverse events in the current form of EDs in Finland.
Aims
The aim of the study was to analyze patient safety incident reports concerning ED, to classify human and system factors, and the root causes that can be identified from the reports. Then, based on these findings, to suggest Individual and organizational learning objectives.
The research questions were:
What kind of conclusions can be made from the existing quantitative information about incident reporters, report types, event conditions and other factors involved.
What are the typical root causes behind patient safety incidents in EDs as identified by the incident reporter?
What kind of problems and system-related themes can be recognized from incident reports, and how are they related to the Ishikawa root cause categories?
What kind of measures and safety management processes should be recommended by the organization and trainers to ensure the employees have sufficient competence and thus improve patient safety in EDs?
Methods
Study design
The study is an observational cross-sectional register-based study using quantitative and qualitative methods. The methodological framework was a combination of inductive and deductive analyzes. The reviewed data consisted of voluntary patient safety incident reports from personnel in a teaching hospital. The incident reporting system consisted of structured and free-text fields.
Study setting
Vaasa Central Hospital is a secondary teaching hospital in Western Finland with a catchment area of about 170 000 inhabitants. All walk-in patients are assessed before admission, and emergency medical services (paramedics) also bring patients to the ED. All incident reports over a one-year period were collected for analysis. The study was approved by the medical director of the hospital district. As it was a register study, approval or consent by the ethics committee was not required by the Finnish law of medical research [17]. Good scientific practice criteria were applied according to the national advisory board on research ethics [18].
Data collection
The study material consisted of the patient incident reports (n = 2558) from Vaasa Central Hospital District during the year 2017. All the 429 incident reports concerned the ED. Reports made by patients were removed, and the remaining 340 reports served as the research sample for the quantitative analysis and 270 reports remained for the qualitative analysis after saturation of the data. In principle, the incident reporting system is anonymous, but occasionally patient identification information was included in the report and thus was removed before reading and classifying the reports.
Data analysis
Descriptive statistics
Statistical analysis of the data was performed with IBM SPSS program version 28 in the hospital's data protection environment. From the structured fields of the incident reports, relevant main categories and subcategories were selected as variables for the analysis. Incomplete reports were also included in the analysis, and they were named as other or unspecified in the results.
Some subgroups were irrelevant for this study, and they were united under the same main category. One example is information flow, which included subcategories for information flow about diagnosis, laboratory examinations, follow up and environment. Categorical variables were presented with frequencies and percentages. Only descriptive statistics were performed.
Qualitative analysis
The systematic reading of 340 incident reports was carried out (M.H.) until the material started to become saturated (n = 270) and new problems or themes were not found. The sample for qualitative analysis consisted of 270 incident reports with free text descriptions. The technical process started by first separating and printing the descriptive textual data onto paper. The problems found were color coded and then sorted into groups and collected in order of frequency. Findings concerning the reporter´s perceptions of the root causes were also noted, and themes identified.
In the first inductive reasoning process, the content analysis [19] of free texts in the reports aimed to find different and repetitive problem groups among the incidents. The problems typically referred to skills, behavior or acts of the personnel, e.g. human factors. However, simultaneously, the role of the system emerged in almost all the reports. The problem groups were named regarding the incident reporter´s perception of the root cause behind the incident or by what was considered as the probable cause by the researcher. If more than one problem was found, the more significant one was chosen. After initial analysis, 13 problem groups were found. After iterative analysis with another researcher (S.K.), it was possible to combine some of the groups, thus, leaving ten groups.
Analysis of case descriptions within the problem groups, led to the discovery of the organizational factors (themes) to which the problems were related. Identification of these themes was processed by analogical reasoning of probable contributing system factors behind the problem. Initially, fifteen themes were identified. After iteration of the theme analysis with another researcher (S.K.), the number of themes was reduced to six. These themes were linked with problem groups, and it was found that several themes could be linked with each problem group.
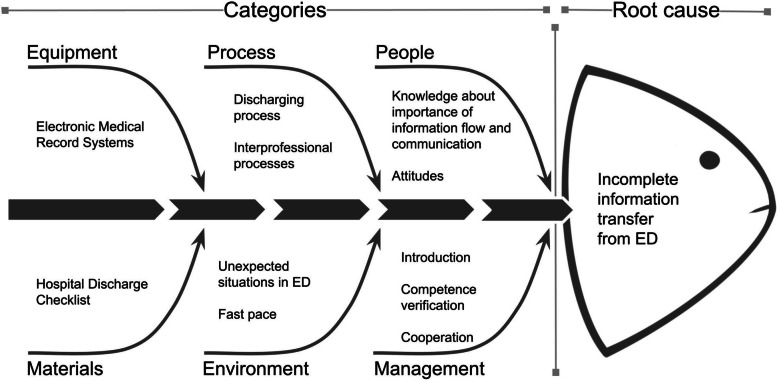
As a deductive reasoning process was applied, each problem group 1–10 was categorized into subgroups using an Ishikawa fish bone diagram [20]. An Ishikawa fishbone diagram is a visual method for root cause analysis that organizes cause-and-effect relationships into categories. Ishikawa main categories are equipment, process, people, materials, environment, and management. This management tool is used for quality control in health care organizations worldwide. It provides comparability, which allows an evaluation of the meaning of the findings in this study. The classification structure of the incident reports analyzed in this research is based on Ishikawa's root cause analysis. The researcher (M.H.) inserted each problem separately into the Ishikawa diagram. The reporters’ perceptions of the root causes were inserted into main Ishikawa categories.
Finally, the researcher (M.H.) created learning objectives for 1) Individual competence requirements and 2) safety management processes proposals in the organization to prevent future incidents. The proposed learning objectives were considered by the research group from the point of view of professional experience in an ED, patient safety management, learning objectives, risk management and incident prevention.
Results
Descriptive statistics
Incidents regarding the ED (n = 340) formed the second-largest percentage (18%) of all incidents reported in the hospital district during the study period. Only the combined reports on all the wards formed a greater percentage (46%). The incident reports concerning the ED were evenly distributed during the 24/7 working hours in proportion to the number of patients. No time frames for patient safety incident reports or any variation by weekdays were observed (data not shown).
Most reports concerning the ED were made by another departments (76.5%), typically after the patient was transferred. These incidents were reported by emergency medical services (paramedics), ward personnel, special outpatient departments, operative units, healthcare centers, home nursing personnel, nursing homes and pharmacies (Table 1). Most of the incidents (70%) were reported by nurses. Physicians made 7.4% of the reports while other healthcare workers were responsible for the remainder. Near-misses comprised 25% and harmful incidents 74% of the reports. One percent of the reports were observational findings or proposals. The largest category (39.7%) was related to information flow or information management. The second- largest category was related to drug and fluid therapy or blood transfusions (23.8%). Incidents concerning diagnosis accounted for 4.9% and invasive procedures for 1.3% of the reports. Proposals on how to avoid similar harm in the future were recorded as follows: no action required 12.8%, providing information and having conversations with personnel 58%, planning development projects 19.4%, apprising the management team 9.7%. Information about what kind of actualized harm occurred were not available within the scope of this analysis. Table 1 provides descriptive statistics from the incident reports.
Table 1.
provides descriptive statistics from the incident reports
| Variable | n | % | Variable | n | % |
|---|---|---|---|---|---|
| Professional group of the reporter | Estimated consequence to the organisation* | ||||
| Emergency medical services (paramedics) | 1 | 0.3 | No harm | 35 | 5.7 |
| Physician | 25 | 7.4 | Reputation loss | 271 | 44.1 |
| Nurse, radiographer, laboratory technician | 238 | 70.0 | Personnell damage | 1 | 0.2 |
| Practical nurse or other care giver | 14 | 4.1 | Material damage | 3 | 0.5 |
| Research staff | 9 | 2.6 | Extra work | 239 | 38.9 |
| Other | 26 | 7.6 | Prolonged treatment | 40 | 6.5 |
| Missing | 27 | 7.9 | Extra costs | 13 | 2.1 |
| Total | 340 | 100 | Missing | 12 | 2.0 |
| Report type | Total | 614 | 100 | ||
| No harm or near miss incident | 85 | 25.0 | Incident report involved with* | ||
| Observational finding or proposal | 4 | 1.2 | Aseptics | 12 | 2.7 |
| Harmful incident | 251 | 73.8 | Diagnosis | 22 | 4.9 |
| Total | 340 | 100 | Emergency medical services (paramedics) | 5 | 1.1 |
| Action proposal to avoid similar harm in the future* | Invasive treatment | 6 | 1.3 | ||
| No action | 46 | 12.8 | Laboratory or radiographing | 22 | 4.9 |
| Information of and conversation with personnel | 209 | 58.1 | Device or use of device | 1 | 0.2 |
| Planning of development project | 70 | 19.4 | Drug or fluid therapy or blood transfusion | 106 | 23.8 |
| Informing management team | 35 | 9.7 | Information flow or information management | 177 | 39.7 |
| Total | 360 | 100 | Violence | 13 | 2.9 |
| Event condition and factors involved* | Accident | 2 | 0.4 | ||
| Nonindetifiable or normal situation | 2 | 0.4 | Other action | 80 | 17.9 |
| Communication and information flow | 155 | 30.1 | Total | 446 | 100 |
| Training and introduction | 55 | 10.7 | Unit of reporter | ||
| Devices and equipment | 2 | 0.4 | ED itself | 80 | 23.5 |
| Medication | 4 | 0.8 | Emergency medical services (paramedics) | 7 | 2.1 |
| Management or organisation | 12 | 2.3 | Hospital bed ward | 143 | 42.1 |
| Patient and family | 18 | 3.5 | Operative unit | 6 | 1.8 |
| Teamwork | 30 | 5.8 | Special outpatient departments | 15 | 4.4 |
| Operating methods | 143 | 27.8 | General practice bedward | 28 | 8.2 |
| Resources | 42 | 8.2 | Healthcare center (GP) | 16 | 4.7 |
| Missing | 52 | 10.1 | Home nursing | 8 | 2.4 |
| Total | 515 | 100 | Nursing home | 7 | 2.1 |
| Estimated consequence to the patient | Pharmacy | 8 | 2.4 | ||
| No harm | 100 | 29.4 | Other | 22 | 6.5 |
| Mild harm | 157 | 46.2 | Total | 340 | 100 |
| Moderate harm | 67 | 19.7 | Free text answer was given with the report** | 293 | 86.2 |
| Severere harm | 4 | 1.2 | No free text answer | 47 | 13.8 |
| Not estimated | 8 | 2.4 | Total | 340 | 100 |
| Missing | 4 | 1.2 | *Multiple answer choices allowed | ||
| Total | 340 | 100 | ** Answers used in qualitative analysis |
Qualitative analysis
In the content analysis, a total of ten problem groups were found by an inductive reasoning process. Analogical reasoning led to the identification of six themes that were all connected to system factors or the organizational level. We tried to identify themes related purely to human factors, but it was not possible to separate them from system factors in the incident reports. For example, in some incident reports, it was unclear whether the problem was related to human factors or the performance of operating tools like the electronic medical record system (EMR). Information from the physician´s point of view was not usually available because the reporter was most often a nurse. In most of the cases where the performer (the professional whose act was concern) was a physician, the incident was evaluated as concerning organizational problems or processes. In some reports, the mandatory fields of the form were completed in contradiction to the written text. In a few of the reports, the case was not an incident but due to the progress of the illness. The main conclusion was that the root causes behind the incidents were usually more related to system factors rather than to the performance of difficult treatment tasks by the staff. Multifaceted connection between themes, problem groups and Ishikawa categories with the number of reports is shown in Table 2. An example of the deductive reasoning process of the Ishikawa diagram is shown in Fig. 1. The problems and reporters’ perception, or if missing, researchers’ evaluation of the root cause behind the problem that caused the event described in the incident report in Table 3.
Table 2.
Shows connection between themes, problem groups and Ishikawa categories. Includes number of reports analyzed
| Problem groups | Themes | Ishikawa | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| The problem that causes the event described | Number of reports concerned | A. Medical staff orientation, onboarding and competence requirements | B.Human resources on duty | C. Electronic medical records and information transfer | D. Medication documentation system | E. Interprofessional collaboration and teamwork | F. Professional resources for specific patient groups* | Equipment | Process | People | Materials | Environment | Management |
| 1. Insufficient introduction/lack of guidelines and protocols or adherence to following them | 28 | X | X | X | X | X | X | X | X | ||||
| 2. Insufficient human resources available | 18 | X | X | X | X | X | X | X | X | X | |||
| 3. Deficient professional skills | 62 | X | X | X | X | X | X | X | X | X | |||
| 4. Medication Management Deficiencies | 70 | X | X | X | X | X | X | X | X | X | X | X | X |
| 5. Incomplete information transfer from ED | 44 | X | X | X | X | X | X | X | X | X | X | X | |
| 6. Language proficiency | 6 | X | X | X | X | X | X | X | X | ||||
| 7. Unprofessional behavior | 4 | X | X | X | X | X | X | X | X | X | |||
| 8. Identification error | 12 | X | X | X | X | X | X | X | |||||
| 9. Patient-dependent problem | 13 | X | X | X | X | X | X | X | X | ||||
| 10.Other | 13 | X | X | X | X | X | X | X | |||||
| TOTAL | 270 | ||||||||||||
Fig. 1.
Example of deductive reasoning process by Ishikawa diagram
Table 3.
Shows results of inductive and analogical reasoning
| Event description | Reporters’ perception, or if missing, researchers’ evaluation of the root cause | Theme, the concern involves with | The problem that causes the event described |
|---|---|---|---|
| Orders given by physician were contradictory to organizational guidelines | Physician on call is unfamiliar with hospital wards and departments and guidelines how to report and arrange follow up treatment and document instructions. |
A. Medical staff orientation, onboarding and competence requirements E. Interprofessional collaboration and teamwork F. Professional resources for specific patient groupsa |
1. Insufficient introduction and either lack of guidelines and protocols or adherence to following them |
| Physician was not familiar with basic documentation and follow-up instructions | |||
| Physician did not know what instructions to follow when discharging a patient to a ward or home | |||
| Physician was unfamiliar with hospital wards and departments and how to arrange follow-up treatment and provide instructions | |||
| Physician directed the patient’s follow-up to wrong department | |||
| The patient was sent to ask the health center for a follow-up examination that cannot be obtained from the health center. | |||
| The patient with need for intense follow-up was transferred to ward which has no possibility to take any laboratory tests during the weekend | |||
| Physician on-call did not know what telephone to use or did not use any | The physician is unfamiliar with mandatory tools like telephones, checklists and contact information | ||
| Employee did not know where to find the contact information for the consultant | |||
| Instructions for using preoperational checklist were not clear or known and the checklist was not used | |||
| The patient from the ED going to the operating room did not have the appropriate surgical preparation checklist like marking the operative side, urinary catheter, and blood order. | |||
| The patient did not receive medicines and blood tests because the orders were not carried out correctly | The new electronic system had been implemented in the ED, but there was no introduction or training of using it | ||
| Referral did not reach the correct follow-up treatment department | |||
| When treating a critical patient, roles and responsibilities were not clear between different medical specialities | Multiprofessional cooperation principles are not familiar to all physicians | ||
| Physicians of different medical specialities did not know their responsibilities | |||
| Consultant ordered the patient to have an operation but did not inform the nurse in charge | |||
| Discharged dementia patients’ report did not reach follow-up care (see prob 5) | Insufficient knowledge in the ED about reporting principles and processes for patients with special needs | ||
| Treatment of threatening alcohol delirium was referred to a psychiatric nurse and medication was not implemented properly in time | |||
| Too many tasks for nurses caused delay of treating elderly patient. |
Shortage of nurses/ nursing personnel: No basic nursing staff for taking care of basic hygiene like diaper change and medication delays when nurses doing it |
A. Medical staff orientation, onboarding and competence requirements B. Human resources on duty D. Medication documentation system E. Interprofessional collaboration and teamwork |
2. Insufficient human resources available |
| The patient was lying in his feces and urine for five hours, which damaged the skin. | |||
| Because of treatment delay, the patient became delirious and was medicated with a sedative. | |||
| No diaper change for an elderly patient visiting the ED for a day | |||
| Shortage of nursing staff caused delay in starting important intravenous antibiotics. | |||
| The patient did not have a cannula and antibiotics were given a few hours later in the ward after discharge from the ED | |||
| The ED physician had no possibility to leave the ED and help on the ward, or the treatment of the patients in the ED would have delayed. | Shortage of physicians | ||
| Need for an on-call physician to come to the ward because there was a patient in a severe condition, but it was impossible to leave the ED | |||
| Acute need to look for contact information of a discharged patient, but there was no time to do it |
Shortage of helping personnel: No staff to update and organize important instructions and the list of telephone numbers |
||
| The physician tried to call these numbers, but they said they were not in use. Contact information was not updated. | |||
| Physician could not open the ECG in the ED, because of the machine was broken, Insufficient equipment like a broken ECG device and no staff to take care of it. | |||
| There was no time to find out if the elderly person needed help at home | |||
| Could not find important information about the patient easily and there was no time for nurse to keep searching | |||
| Many inexperienced physicians at the same time who were slow and who needed to consult very much and could not help on the ward | Inexperienced physician and no consult | ||
| Very inexperienced physician gave inadequate treatment and instructions | |||
| No time for young physician to familiarize with the instructions. Orders were inadequate. | |||
| The medication list was incorrect or old, and it had not been checked in the ED | Lack of medication information managing personnel and poor medication documentation system | ||
| Challenge to find adequate medication from differing medication documentation systems and lack of time to do it. No personnel to do it. | |||
| Nurse could not recognize the critical patients during triage | A discrepancy between the level of requirements of triage nurse and competence of doing it. |
A. Medical staff orientation, onboarding and competence requirements B. Human resources on duty E. Interprofessional collaboration and teamwork F. Professional resources for specific patient groupsa |
3. Deficient professional skills |
| The patient with a wound that needed stitches was sent home without seeing a physician | |||
| Triage took the patient in the ED even if there was no need for treatment in the ED | |||
| Young patient with symptoms of sepsis triaged to GP | |||
| COPD patient´s dyspnea and CO2 retention were treated improperly in the ED and the patient did not get proper treatment until on the ward | A discrepancy between the level of requirements of the ED physician and competence of doing it. | ||
| Physician could not recognize a critical immunosuppressed patient | |||
| The physician did not recognize the signs of serious operative condition and transferred the patient to the ward too early. | |||
| The physician did not recognize psychiatric emergency and discharged the patient without psychiatric consultation | |||
| The physician did not read documentation of paramedics and missed critical information. | Poor skills of multiprofessional collaboration | ||
| Critical information about the psychiatric patient was not given when reporting the patient | |||
| The physician did not ensure that follow-up instructions were clear to the patient. | Poor skills of communication | ||
| Dementia patients were discharged from the ED without confirmation that they could manage alone. | Lack of knowledge about the special needs of the geriatric patient and the discharge process of dementia patients | ||
| Dementia patient´s discharged from the ED without informing home nurse or family | |||
| A dementia patient who had fever and who was totally dependent on other people´s care was sent home from the ED by taxi without shoes or informing family or home care. It was wintertime. | |||
| Nurse made a cast and forgot the ECG electrode inside | Lack of training special skills of plastering. | ||
| Medication list was incorrect when the patient discharged from the ED to the ward or home. | Lack of knowledge about importance about current medication documentation and no protocol for it |
A. Medical staff orientation, onboarding and competence requirements B. Human resources on duty C. Electronic medical records and information transfer D. Medication documentation system. E. Interprofessional collaboration and teamwork F. Professional resources for specific patient groupsa |
4. Medication Management Deficiencies |
| Incomplete prescription or medication order | |||
| The patient started taking wrong medication after discharge from the ED because of outdated medication list. | |||
| Medication was not up-to-date when treating a current illness and the patient was at risk of obtaining harmful drugs | |||
| The patient was not able to remember new mediation because of dementia, and no documentation of medication changes was given from the ED. | |||
| Nurse or physician could not reconcile medication because of different medical documentation systems | Different medical documentation systems between treating facilities | ||
| Medication prescribed from GP was not given to the patient in the ED, because of separate documentation systems | |||
| Not possible to find out the current medication, because of different electronic medical records and medical documentation systems between treatment facilities and lack of time | |||
| No time to do proper Medication Reconciliation for nurse or physician | Lack of time | ||
| Not possible to find out the current medication fast enough | |||
| No Hospital Discharge Checklist or not using it | Process problems in discharging | ||
| The receiving care facility did not get proper instructions about the patient’s treatment | Lack of knowledge about the importance of information transfer to follow-up care or the process for doing it |
A. Medical staff orientation, onboarding and competence requirements C. Electronic medical records and information transfer D. Medication documentation system. E. Interprofessional collaboration and teamwork F. Professional resources for specific patient groupsa |
5. Incomplete information transfer from ED |
| Patient’s vital signs were poor already while transferring, but information on the situation was not given in the report | |||
| No written or oral reporting to the follow-up treatment facilities | |||
| The patient is transferred from the ED to ward with symptoms of gastroenteritis without informing ward and without isolation | |||
| The patient had infectious disease, but the information did not reach the ward when transferring | |||
| The physician did not ensure that dementia patient understands the instructions and did not document them | Lack of time and personnel to ensure that information about a discharging dementia patient and follow-up treatment instructions are given to caretakers | ||
| Information about dementia patient´s discharging, and follow-up treatment instructions did not reach the home nursing service | |||
| Dementia patient was sent back to nursing home without any document about visit in the ED or telephone report | |||
| Referral for further examinations was missing | Inappropriate tools for data transfer between organizations | ||
| The patient documents and laboratory results taken in the ED were not seen in GP | |||
| We did not see central hospital records anywhere. No paper came with the patient. | |||
| Relevant information did not receive psychiatric patient, because of separate documentation systems | |||
| The physician did not give the instructions to patient and did not document them in the system | Lack of knowledge about the importance of patient information | ||
| Unclear follow-up instructions to the patient after discharging the ED | |||
| Physician in the evening shift examined only Swedish-speaking patients | No language requirement for professionals |
A. Medical staff orientation, onboarding and competence requirements B. Human resources on duty |
6. Language proficiency |
| Information available only in one language and professional did not understand it | |||
| Treatment delayed because only patients with same language as the physician were treated during the night | |||
| There was no time for proper use of interpreting service | Lack of time or problems using interpreting tools | ||
| Time shortage when treating patients in need of interpreting services | |||
| Professional did not know how to use interpreting telephone | |||
| Senior consultant refused to come to the ward when asked | Lack of physician resources for help on wards during on-call shifts. |
A. Medical staff orientation, onboarding and competence requirements B. Human resources on duty E. Interprofessional collaboration and teamwork F. Professional resources for specific patient groupsa |
7. Unprofessional behavior |
| Disrespectful speech towards mental health patients | Prejudgment of psychiatric patients | ||
| The ED personnel talked unprofessionally about the skills of the psychiatry staff when patient was present | Poor skills of multiprofessional collaboration and respect for other professionals | ||
| Behavior problems or disrespect towards nurses on the ward | |||
| Patient urgently transferred to operation unit and wrong patient information was attached | Urgent situation |
A. Medical staff orientation, onboarding and competence requirements E. Interprofessional collaboration and teamwork |
8. Identification error |
| The patient had an invalid social security number on the ID wristband. | No protocol for identification in Triage or not employing it properly | ||
| Patient did not have ID wristband at all | |||
| Patient´s contact information had not been asked in triage | |||
| Medication order to the wrong patient | |||
| Aggressive patient or threat of violence | Lack of knowledge about treating special patient groupsa |
A. Medical staff orientation, onboarding and competence requirements B. Human resources on duty F. Professional resources for specific patient groupsa |
9. Patient-dependent problem |
| Treatment of a patient with challenging behavior like delirium | Shortage of staff and time to react to unexpected situations. | ||
| Aggressive psychiatric patient needed two nurses and other patients’ treatment delays | |||
| Suicidal action | |||
| Aggressive suicidal patient and no permission to sign referral to compulsory treatment | Deficiencies as regards physician´s legal rights |
A. Medical staff orientation, onboarding and competence requirements B. Human resources on duty |
10. Other |
| Treatment delayed because of a change of shift | Deficiencies in shift scheduling | ||
| Interruption of information flow caused by shift change |
aGeriatric, mental health and substance abuse disorder patients
Themes
Theme A. medical staff orientation, onboarding and competence requirements
Insufficient introduction to physicians before on-call shift was thought to be one reason for their lack of knowledge and familiarization with guidelines and processes, and poor documentation of medication and instructions. This theme was connected to all the problem groups.
Theme B. human resources on duty
Necessary resources were mentioned, e.g. specialized coordinating discharge personnel for the elderly, assistance staff for medical recording, technical support, and secretarial help for physicians and nurses, caregivers or practical nurses to perform basic patient care like changing diapers, and finally experienced medical staff to help inexperienced physicians and triage nurses.
Theme C. electronic medical records and information transfer
This theme was about information flow onwards from the ED when discharging patient to wards or nursing homes, and the information flow within the team or to the patient from the physician. Challenges related to communication tools are mentioned repeatedly in the reports.
Theme D. medication documentation system
Medication consistency problems were reported before coming to the ED and after discharge. Medication was not updated properly. There were also challenges with medication management tools, e.g. different EMR between the hospital and primary care. This problem emerged especially among elderly people with dementia.
Theme E. interprofessional collaboration and teamwork
Deficiencies in multiprofessional collaboration, especially in patients with less serious conditions or low complexity conditions (defined as ambulatory arrival, low-acuity triage level, and discharged) treated in the ED, without critical circumstances: not reading the documentation provided by other professionals, lack of oral communication or not making telephone contacts to consultants/nurses/ the ward when necessary.
Theme F. professional resources for special patient groups such as geriatric, mental health, and substance abuse disorder
Identifying the special needs of geriatric patients did not occur as expected. Identification of this theme was based on reports outside the ED, by professionals who worked with the elderly, and who noticed a lack of competence in the ED on this topic. Reports that concerned the special needs of psychiatric patients and patients with substance abuse disorder also belong to this theme due to similar finding.
Analysis of problem groups
Group 1
Insufficient introduction and either lack of guidelines and protocols or adherence to following them (Linked to themes A, E and F and Ishikawa main root causes: process, people, materials, environment, and management.)
The organization's operating processes were unclear to the professionals. Most frequently this was reported by a physician. Guidelines were not familiar, the physician on call did not know which mobile phone they should carry, or they did not carry a mobile phone at all. The basics of patient onward reporting was not performed. Physicians on call were not familiar with patients' follow-up treatment protocols. There was ambiguity about who should take responsibility for patients with the need for critical treatment, and to which ward certain kinds of patient should be transferred.
“Physicians were not aware of what is happening and who is operating, and there was no clear protocol for process. Nurses did not get enough information about decisions made by physicians and were confused.”
“Different instructions from different physicians for treating bone fracture and confusion about follow-up instructions…”
Group 2
Insufficient human resources available (Linked to themes A, B, D and E, and Ishikawa main root causes: equipment, process, people, environment, and management.)
Some basic functions seemed to fail due to the need for haste and the excessive number of patients in relation to the amount of time needed for personnel to perform tasks. Shortage of nurses, experienced physicians and assisting staff, such as secretaries or pharmacists, were the three most significant causes mentioned in reports. Small but critical technical issues emerged in several reports.
“Patient with wound to be stitched needed to wait too long because of shortage of nurses”.
“The phone numbers of the ED surgery's phone have been missing for 2 months already…”
Group 3
Deficient professional skills (Linked to themes A, B, E and F, and Ishikawa main root causes: process, people, materials, environment, and management).
Several reports were about mistriage considered to be caused by inexperienced nurses or nurses without proper onboarding for this specific task performing triage. In most of these reports, the severity of the patient’s condition was not recognized, and the patient was triaged to a general practitioner (GP) while there was need for specialized emergency services. Some patients did not need to be treated in the ED at all and were thought to be exacerbating the number of patients.
“A 24-year-old patient with active cancer and fever triaged to GP and waited for 6 hours…” and “Paracetamol intoxication was not recognised in triage…” and “The patient was triaged to ED for a cortisone injection due to long-term wrist pain...”
In several reports, the physician did not recognize a severe illness and treated an ED- patient alone while there was no senior physician consultant available. Incompetence in teamwork was reported when important information was available in the referral or documentation of the paramedics, but the physician did not notice that information.
“The patient was transferred to ward from ED with several nonserious diagnosis, which turned out as urgent serious operative condition, which could be seen in tests performed by ED.”
“Physician did not notice the primary care physician´s referral and critical medication was delayed.”
Reports concerning geriatric patients were usually made by professionals who worked with the elderly and dementia patients in other locations than the ED. This problem was repeated in many reports, and most of these reports underlined the insufficient understanding about the special needs of this group in EDs. Patient abandonment was mentioned.
“96-year-old patient fainted again in the morning in ED when going to the toilet but was discharged from the hospital alone during the same morning without informing family”.
Group 4
Medication Management Deficiencies (Linked to themes A – F, and Ishikawa main root causes: equipment, process, people, materials, environment, and management.)
Reports were made in wards, by GPs, or home nursing care after discharge from the ED, or in the ED when a patient was arriving needing emergency care. Reporters stated there was a lack of a reliable system for confirming that medical records were up-to-date. The problem was even worse if the patient had dementia and could not correct the information themselves. Recurrence of the problem gave the impression of desperation by the professionals involved. Usually there was no harm for the patient, and eventually it was reported as “no harm”. It was evaluated that if a medication error had occurred, the risk of a serious adverse event would have been significant.
In patient transfers from "ED to ward, there was discrepancy between physician´s text and electronic medication record.” and “…we cannot see the medical record of the healthcare centre.” “Patient almost received wrong medication but was corrected in time. It took a significant amount of effort and time from nurses. “
Group 5
Incomplete information transfer from ED (Linked to themes A, C – F, and Ishikawa main root causes: equipment, process, people, materials, environment, and management).
Insufficiencies of written or oral reports from the ED to wards or other follow-up treatment facilities. Repeatedly, an elderly patient was discharged from the ED to a primary health care ward in a severe condition. Instructions for treatment, such as pain medicine or treatment limitations, were missing even if the patient´s survival prognosis was poor. There was a lack of information flow to home nursing and nursing home personnel who have no possibility to see report in electronical systems from the ED. Paper reports were also missing.
“Patient transferred to ward without informing about a contagious infection. Should have been in isolation.”
Group 6
Language proficiency (Linked to themes A, B – E, and Ishikawa main root causes: equipment, process, people, materials, environment, and management).
The circumstances described were related to bilingualism in the region. Patient safety was evaluated to be endangered if the physician was not able to communicate in the same language as the patient (Finnish or Swedish). A proper interpreting service was not available or used and was the reason there was a treatment delay.
“There are only physicians, who speak one language, working in the ED. The treatment of patients requiring a different language was delayed for hours.”
Group 7
Unprofessional behavior (Linked to themes A, B, E, F, and Ishikawa main root causes: process, people, materials, environment, and management).
Some co-workers acted unethically or spoke disrespectfully about other professionals behind their back. Disrespectful talk about psychiatric patients or patients with substance abuse disorder were also mentioned in a few reports.
Group 8
Identification error (Linked to themes A and E, and Ishikawa main root causes: process, people, materials, environment, and management).
An urgent patient taken to the operating room straight from the ED was confused with a patient with the same name, and the social security number was not checked. There were a few reports about not updating patients’ contact information in triage. A few reports were about physicians confusing patients.
“The nurse noticed that the physician accidentally wrote an ultrasound referral for the wrong patient.”
Group 9
Patient-dependent problem (Linked to themes A, B and F, and Ishikawa main root causes: process, people, materials, environment, and management).
Usually in these reports the patient was under the influence of drugs or alcohol, or the patient was suffering from a mental illness or dementia.
“Aggressive and inappropriate behavior of patient caused extra work for personnel.”
Group 10
Other (Linked to themes A and B, and Ishikawa main root causes: process, people, materials, environment, and management).
According to some reports, unexpected situations emerged in ED such as exceptional backlogs, several critical patients at the same time or delays during shift changes. This group was chosen if the case under review did not belong to any other group or information in the report was incomplete. One report included details about legal rights.
“Aggressive suicidal patient and physician has no legal right to place patient on involuntary psychiatric hold”
These findings have led to learning objectives for individual competence requirements and safety management process proposals in the organization from the point of view of professional experience and teaching, patient safety and risk management, and incident prevention. It is mandatory for the organisation to ensure professionals suitability for a specific job. Commitment to an introduction process before working in the ED and proper use of patient identification protocols were examples of individual competence requirements. Proposals for safety management processes in the organization included competence requirements for professionals before working in EDs and resourcing more staff e.g. discharge personnel, secretary, caretakers, pharmacists, technical assistance, and physician resources for ward consultations. All learning objectives are shown in Table 4.
Table 4.
Shows learning objectives to improve patient safety in Emergency Department
| Individual competence requirements | Safety management process proposals in the organization |
|---|---|
| Obligation to attend introduction before working in the ED | Requirement for adequate introduction to the working environment, instructions, and tools before working in the ED |
| Teamwork skills training | Organized teamwork training also concerning non-urgent tasks |
| Technical skills training before working in the ED, e.g. simulation training | Competence requirements for professionals before working in the ED. Including language skills |
| Knowledge about patients with special needs, such as geriatric, psychiatric and substance use patients | Appropriate staffing for patients with special needs, e.g./such as psychiatric and dementia patients |
| Medication safety and documentation requirements | Proper and practical medication documentation system |
| Risk management | Risk management |
| Proper use of patient identification protocol | Requirement to use the protocol for identification. |
| Adherence to a patient safety culture and the relevant tools | Recorded follow -up about patient safety improvements |
| Adherence to the proper use of instructions, learning communication skills, and effective interaction with other treatment facilities | Cooperation with other organizations |
| Awareness, respect, and cooperation with other professional groups | Management meetings and organized training and cooperation in multi-professional teams |
| Commitment to complying with instructions | Clear instructions and guidelines for professionals specifying the implementation processes |
| Consideration of the role of patients and understanding the importance of communication and interaction with patients and families | Consideration of the patient's role and special needs in the planning of patient processes and instructions. |
| Commitment to using interpretation tools | Proper interpreting services and tools and adequate use of their implementation |
| Commitment to incident reporting and a patient safety culture | Organized processes for teaching incident reporting and handling reports with multi professional team |
| Commitment to using the Hospital Discharge checklist | Requirements to use the Hospital Discharge Checklist |
| Commitment to the respect of all professional groups | Resourcing of staff, such as, discharge personnel, secretary, caretakers, pharmacists, technical assistance and more physician resources to ward consulting |
Discussion
Our findings constitute the first research conducted on this subject to the best of our knowledge. Issues other than severe incidents, medical care, or technical skills seem to be the greatest cause of reported patient safety incidents in the ED. The reported incidents were frequently related to teamwork skills such as communication and information flow, and to professional skills. However, medication management deficiencies also emerged. Another notable finding was that three quarters of the reports were from another location after discharge from the ED. Furthermore, most reports were by nursing staff.
Our findings raise a significant concern whether the most serious incidents go unreported when using a voluntary and anonymized incident reporting system. In addition, the question arose as to how reports made elsewhere than the ED are handled to improve patient safety in the ED. A mandatory and easily used incident reporting system might be a better option to obtain an overall picture of ED incidents, especially those with serious consequences.
Mild harm was assessed as the most common consequences for patients, causing loss of reputation and extra work for the organization. According to our findings, extra work is not only irritating but also causes significant concern about patient safety by the reporters. The results also demonstrated that reputation issues are important in health care organizations [21].
Only about one percent of reports estimated the consequences for the patient as severe. Analysis of textual data gave the impression that the consequences of reported incidents may be more serious than the original report handler had estimated. Therefore, it would be important to analyze incident reports in multiprofessional and, in some cases interorganizational teams, so the opinion of different professionals can be taken into account. As a result, proposals could be seen by the correct professionals and lead to the appropriate continuous improvements. Consequences evaluated as mild harm for the patient need more specific research from the point of view of the patient before the consequence assessment can be considered valid [22].
In most reports concerning the acts of professionals, deficiencies were found at the organizational level in six themes. Such issues as medical staff orientation, onboarding and competence requirement had connections to all the problem groups found. Based on these findings, more resources should be allocated to process development, training, and onboarding at EDs before commencing work especially for physicians [23] and triage nurses [24]. Moreover, increase in support staff, e.g. secretarial assistance, pharmacists, and caretakers for hygienic needs in EDs would probably free up physicians and nurses to focus on medical treatment of patients [25].
In a previous study on Finnish health care, two percent of reports were made by physicians [26] but this result is not fully comparable because it also considered social work in which physicians rarely work. Nevertheless, in our study more than two -thirds of all reports were made by nurses. It is known that nurses are more aware of the existence of the incident reporting system and physicians seem to be too busy or uncomfortable to use it [27]. However, it is important to explore ways to develop the system to improve reporting activity – especially by physicians.
It is known that human factors must be carefully considered when designing electronic medication management systems (EMMS) or computerized physician order entry (CPOE) systems, and there is potential to develop these systems to improve patient safety [28]. The results of our study indicate that the electronic medication management system does not perform optimally. In several reports, the problem of data transfer was described between different organizations and challenges with the EMMS.
Not using the checklist seems to endanger patient safety, especially when discharging patients forward from ED. This is in line with the previous study that checklists are effective tools for improving patient safety [29]. Increasing concerns about patient safety and the need for interprofessional teamwork, especially in EDs, were already noted in a review on measuring non-technical skills [30]. Although there were situations that lead to incident reports about problems in teamwork in this study, they were usually about non-urgent patients or patients with special needs like geriatric patients or patients with mental illness or substance abuse disorder. The treatment in ED’s of these patient groups has been studied previously with similar findings [31–33].
Communication problems are known to cause a significant portion of adverse events in EDs. Correct information may be available, but its flow and processing may not work as intended [34, 35]. A safe patient experience requires not only the expertise of professionals but also adequate communication and professional behavior [36].
Triage in EDs plays a considerable role in patient safety [37]. A critical start for the treatment process is the triage in the ED, which is why triage nurses need sufficient previous work experience [24]. As also shown in this study, the professional skills and experience of physicians and triage nurses play an important role in identifying critically ill patients and prioritizing limited resources to those who need them most urgently [38].
The findings of this study also support previous research that the actions taken after problems emerge are still insufficient [39]. There are efforts to develop the processes in EDs but the desired improvements and implementation are not being achieved as expected, and planned patient safety improvement actions should be more visible in organizations [40]. Visible actions by organizations that improve patient safety also strengthen staff commitment [40].
Simulations are known to be an effective way to promote patient safety in acute patient care. Simulation training is constantly increasing; safe and effective training methods for health care professionals and teamwork are central to it [41]. However, such training usually focuses on treating critical emergency patients. Interprofessional familiarity increases patient safety in medical teams in many ways [42]. Deficiencies in physicians´ actions, like incomplete orders and lack of information flow with the patient, raise concern whether the teamwork and multiprofessional collaboration still play too small a role in the training of physicians. Medical schools still focus primarily on technical skills and medical science among their own professional groups, even if the perceived benefit of multiprofessional collaboration has been demonstrated [43]. This problem opens discussion about the educational structure of medical schools and provides a new perspective.
According to these findings, different issues need to be reconsidered in management and resourcing emergency departments. More consideration needs to be given to organizational safety management processes and individual competence requirements for medical staff. It is important to recognize organizational deficiencies behind events that appear to be errors of an individual.
More research is needed on the reporting activity of severe incidents connected to patient records. This study also provides a new insight for teamwork when treating those patients who do not need urgent emergency care but rather normal acute care in the ED. In this study, insufficient instructions and lack of information flow in reports processed for these patients was especially considered. It would be important to clarify, through further research, whether patient safety improvement measures are sufficient in relation to the need for change. More research could also be carried out on what kind of consequence incidents reported as mild actually had for patients. Further research also needs to be done on the role of patient safety and multiprofessional training in medical education, and its effects on patient safety implementation in the ED.
Strengths
In this research, the sample was larger than usual in qualitative studies and the number of reports gives some additional meaning to the qualitative results. While this sample was from only one ED unit, the key results can be generalized, at least to the whole of Finland, because all EDs follows the same regulations and guidelines [13]. The bilingualism of the catchment area of the hospital under review affects the results regarding linguistic communication, which is noteworthy regarding increasing transnational diversity in societies.
The criteria for ensuring the quality of qualitative research include elements such as credibility, transferability, dependability, and confirmability [44]. In our research, credibility was achieved by the large sample size of authentic reports from the national incident reporting system. Transferability of the results was realized by using comprehensive and detailed narratives in context. The qualitative main results were iterated with two other researchers: one from the same area of working experience (S.K.) and one researcher from a different area of working experience (H.T.), ensuring dependability of the research. Confirmability was achieved with complete agreement by peer debriefing of two researchers (M.H. and S.K.) concerning their observations based on years of working experience in the ED and patient safety education. Data were also analyzed with both inductive and deductive reasoning.
Limitations
It must be noted that incident reporting is not mandatory and therefore, some events may go unreported. Also, the professionals' individual differences, experience and the patient safety culture of the unit probably affect reporting activity and the content of reports. In this sample as elsewhere, the content of events may be unevenly distributed because nurses are probably more knowledgeable about incident reporting. In addition, they report more incidents than physicians, who have more concerns about consequences but lack the time to report [27]. In the deductive part of the analysis, the Ishikawa classes were easily found, and most of the problem groups fitted into several classes, which indicates the complex and multifaceted nature of this subject.
An incident reporting tool (Haipro) used in the study hospitals was introduced in Finland in 2007 [14]. Since then, several commercial providers have produced electronic incident reporting systems for healthcare organizations and studies of the results have been published [45]. However, the usability of this framework has not been researched, especially in EDs.
Conclusions
The underlying causes of reported patient safety incidents in EDs can be complex and multifaceted. However, it is unclear whether the most serious incidents are underrepresented. Due to these findings, patient safety can be improved in EDs by concentrating on basic working conditions such as proper introductions, multiprofessional interactions and resources. According to the Client and Patient Safety Strategy and Implementation Plan 2022–2026 [46] published by Finnish government everyone must be committed to action to promote safety, and multi-sectoral cooperation enhances an atmosphere of respect and appreciation between professionals. This is in line with the findings of this research and reinforces the need to implement this plan in the ED environment. More research is also needed about teamwork skills, patients with special needs and non-critical patients, and the reporting of severe incidents. There is need to do more research in this area and develop patient safety in EDs.
Acknowledgements
Thank language examiner Elizabeth Nyman of Turku University for language revision, Morag Tolvi for language revision and layout finishing and artist Nea Luurila for the realization of the fishbone illustration.
Abbreviations
- ED
Emergency Department
- MSAH
The Finnish Ministry of Social Affairs and Health
- EMR
Electronic medical record system
- EMMS
Electronic medication management systems
- CPOE
Computerized physician order entry
Authors’ contributions
All authors (MH, HT, AR, SK, and TI) participated in the concept and design of the study. MH and AR performed the data collection. MH and AR prepared the first draft of the quantitative parts. MH, HT and SK prepared the first draft of the qualitative parts and MH and TI prepared the first draft of the whole manuscript. All authors critically revised and the proposal, the analysis and interpretation of the data and design of the article. All authors read and approved the final manuscript. All the authors participated the revision process.
Funding
Funding from the University of Turku and the Finnish Medical Association was received by the corresponding author (M.H.).
Data availability
The study material is available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
As this was a registry study, ethics approval or consent to participate by the ethics committee was not required by the Finnish law of medical research.( Finnish Law of medical research 9.4.1999 https://www.finlex.fi/fi/laki/ajantasa/1999/19990488).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Reason J. Human error: models and management. BMJ. 2000;320(7237):768–70 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1117770/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ. 1998;316(7138):1154–115 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1112945/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kohn L, Corrigan J. Donaldson M. To Err is Human: Building a Safer Health System. Institute of medicine (US). National Academies Press; 2000. 10.17226/9728 [PubMed]
- 4.Socialsyrensen, Sweden 2021. En indikatorbaserad uppföljning. Utifrån den nationella handlingsplanen för ökad patientsäkerhet i hälso- och sjukvården – Agera för säker vård för säker vård. (An indicator-based follow-up for safe care. Based on the national action plan for increased patient safety in health care – Act for safe care.) https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2021-9-7552.pdf
- 5.Rodwin B, Bilan V, Merchant N, et al. Rate of Preventable Mortality in Hospitalized Patients: A Systematic Review and Meta-analysis. J Gen Intern Med. 2020;35(7):2099–106 https://pubmed.ncbi.nlm.nih.gov/31965525/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berg LM, Källberg A, Göransson KE, et al. Interruptions in emergency department work: an observational and interview study. BMJ Qual Saf. 2013;22:656–63. 10.1136/BMJQS-2013-001967. [DOI] [PubMed] [Google Scholar]
- 7.Schneider A, Wehler M, Weigl M. Effects of work conditions on provider mental well-being and quality of care: a mixed-methods intervention study in the emergency department. BMC Emerg Med. 2019;19:1. 10.1186/s12873-018-0218-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2006;49(2):125–256. 10.1016/J.ANNEMERGMED.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 9.Hussain F, Cooper A, Carson-Stevens A, et al. Diagnostic error in the emergency department: learning from national patient safety incident report analysis. BMC Emerg Med. 2019;19:77. 10.1186/s12873-019-0289-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hirsch, K., Peth, H., Williams, M. Root-cause analysis is useful for ED problems. Relias Media (2004) - Continuing Medical Education Publishing 2004–06–01. https://www.reliasmedia.com/articles/2840-root-cause-analysis-is-useful-for-ed-problems
- 11.White AA, Wright SW, Blanco R, et al. Cause-and-effect analysis of risk management files to assess patient care in the emergency Department. Acad Emerg Med. 2004;11(10). https://onlinelibrary.wiley.com/doi/pdf/10.1197/j.aem.2004.04.012 [DOI] [PubMed]
- 12.World Health Organization. Patient Safety Incident Reporting and Learning Systems. Technical Report and Guidance; 2020. https://www.who.int/publications/i/item/9789240010338
- 13.The Finnish Ministry of Social Affairs and Health order. Finnlex. STM. 2014. https://www.finlex.fi/fi/laki/alkup/2014/20140782
- 14.Awanic Oy. Reporting System for Safety Incidents in Health Care Organizations https://awanic.fi/haipro/eng/
- 15.Amaniyan S, Faldaas BO, Logan PA, Vaismoradi M. Learning from patient safety incidents in the emergency department: a systematic review. J Emerg Med. 2019;58(2):P234–244. 10.1016/J.JEMERMED.2019.11.015. [DOI] [PubMed] [Google Scholar]
- 16.Bearman C, Hayes P, Thomason M. Facilitating teamwork in emergency management: The team process checklist. Int J Disaster Risk Reduction. 2023;94. https://www.sciencedirect.com/science/article/pii/S2212420923002558#bib22
- 17.The Finnish Parliament. Finnish Law of medical research 9.4.1999/488 https://www.finlex.fi/fi/laki/ajantasa/1999/19990488
- 18.The Finnish Research Ethics Advisory Board. Good scientific practice and procedures for handling misconduct and fraud in science. NATIONAL ADVISORY BOARD ON RESEARCH ETHICS 2002. www.tenk.fi
- 19.Vears, D.F., Gillam, L. Inductive content analysis: A guide for beginning qualitative researchers. Health Professional Education: A Multi-Professional Journal. 2022;23(1). https://fohpe.org/FoHPE/article/view/544
- 20.Kaoru Ishikawa. What Is Total Quality Control? The Japanese way. 1985. [Google Scholar]
- 21.Bevan G, Evans A, Nuti S. Reputations count: why benchmarking performance is improving health care across the world. Health Econ Policy Law. 2019;14(2):141–61 https://pubmed.ncbi.nlm.nih.gov/29547363/. [DOI] [PubMed] [Google Scholar]
- 22.Sahlström M, Partanen P, Turunen H. Patient-reported experiences of patient safety incidents need to be utilized more systematically in promoting safe care. Int J Qual Health Care. 2018;30(10):778–85 https://www.researchgate.net/publication/324604899_Patient-reported_experiences_of_patient_safety_incidents_need_to_be_utilized_more_systematically_in_promoting_safe_care. Advance Access Publication Date: 16 April 2018. [DOI] [PubMed] [Google Scholar]
- 23.Stassen P, Westerman D, et al. Novice Doctors in the Emergency Department: A Scoping Review. Cureus. 2022;14(6):e26245 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9308466/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bahlibi TT, Tesfamariam EH, Andemeskel YM, Weldegiorgis GG. Effect of triage training on the knowledge application and practice improvement among the practicing nurses of the emergency departments of the National Referral Hospitals, 2018; a pre-post study in Asmara. Eritrea BMC Emerg Med. 2022;22:190. 10.1186/s12873-022-00755-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lavander P, Meriläinen M, Turkki L. Working time use and division of labour among nurses and health-care workers in hospitals – a systematic review. J Nurs Manag. 2016 Nov. 24(8):1027–1040. Original Article. https://onlinelibrary.wiley.com/doi/abs/10.1111/jonm.12423 [DOI] [PubMed]
- 26.Rauhala A, Kinnunen M, Kuosmanen A, et al. What does voluntary reporting system of patient safety incidents tell? SLL 16.11.2018 46/2018 vsk 73 s. 2716 – 2720 https://www.researchgate.net/publication/331589860_Mita_vapaaehtoiset_vaaratapahtumailmoitukset_kertovat
- 27.Kaya S, Karaman S, Demir IB, et al. Attitudes and Barriers to Incident Reporting for Doctors and Nurses in a University Hospital’s Surgery Departments. J Basic Clin Health Sci. 2020;4:108–13 https://dergipark.org.tr/tr/download/article-file/1460525. [Google Scholar]
- 28.Awad S, Amon K, Baillie A, et al. Human factors and safety analysis methods used in the design and redesign of electronic medication management systems: a systematic review (2023). Int J Med Informatics. 2023;172:105017. 10.1016/J.IJMEDINF.2023.105017. [DOI] [PubMed] [Google Scholar]
- 29.Thomassen O, Storesund A, Softeland E, Brattebo G. The effects of safety checklists in medicine: a systematic review. Wiley Online Library; 2013. https://onlinelibrary.wiley.com/doi/pdfdirect/10.1111/aas.12207 [DOI] [PubMed]
- 30.Cooper S, Endacott R, Cant R. Measuring non-technical skills in medical emergency care: a review of assessment measures. Open Access Emerge Med. 2010;2:7–16 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4806821/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schick B, Mayer B, Jäger M, et al. Emergency medical care of patients with psychiatric disorders - challenges and opportunities: Results of a multicenter survey. BMC Emerge Med. 2022;22:173 https://bmcemergmed.biomedcentral.com/articles/10.1186/s12873-022-00722-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lucke JA, Mooijaart SP, Heeren P, et al. Providing care for older adults in the Emergency Department: expert clinical recommendations from the European Task Force on Geriatric. Eur Geriatr Med. 2021;13:309–17. 10.1007/s41999-021-00578-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang X, Wang N, Hou F. Emergency Department Visits by Patients with Substance Use Disorder in the United States. West J Emerg Med. 2021;22(5):1076–85 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8463055/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bijani M, Abedi S, Karimi S, et al. Major challenges and barriers in clinical decision-making as perceived by emergency medical services personnel: a qualitative content analysis. BMC Emerg Med. 2021;21:11. 10.1186/s12873-021-00408-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schnapp, B.H., Sun, J.E., Kim, J.L. et al. Cognitive error in an academic emergency department (2018). Diagnosis (Berl). 2018;25;5(3):135–142. 10.1515/dx-2018-0011. https://pubmed.ncbi.nlm.nih.gov/30016277/ [DOI] [PubMed]
- 36.Venesoja A, Castrén M, Tella S, Lindström V. Patients’ perceptions of safety in emergency medical services: an interview study. BMJ Open. 2020;10:e037488. 10.1136/BMJOPEN-2020-037488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fekonja Z, Kmetec S, Fekonja U, et al. Factors contributing to patient safety during triage process in the emergency department: a systematic review. J Clin Nurs. 2023;32(17–18):5461–77. 10.1111/JOCN.16622. [DOI] [PubMed] [Google Scholar]
- 38.Sax DR, Warton EM, Mark DG, et al. Evaluation of the Emergency Severity Index in US Emergency Departments for the Rate of Mistriage. JAMA Netw Open. 2023;6(3):e233404 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2802556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liukka M, Hupli N, Turunen H. Problems with incident reporting: Reports lead rarely to recommendations. J Clin Nurs. 2018;28(6). https://www.researchgate.net/publication/329952186_Problems_with_incident_reporting_Reports_lead_rarely_to_recommendations [DOI] [PubMed]
- 40.Uibu E, Põlluste K, Lember M, Toompere K, Kangasniemi M. Planned improvement actions based on patient safety incident reports in Estonian hospitals: a document analysis. BMJ Open Quality. 2023;12:e002058. 10.1136/bmjoq-2022-002058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bienstock J, Heuer A. A review on the evolution of simulation-based training to help build a safer future. Medicine (Baltimore). 2022;101(25):e29503 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9276079/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iyasere CA, Wing J, Martel JN, et al. Effect of Increased Interprofessional Familiarity on Team Performance, Communication, and Psychological Safety on Inpatient Medical Teams: A Randomized Clinical Trial. JAMA Intern Med. 2022;182(11):1190–8 https://pubmed.ncbi.nlm.nih.gov/36215043/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ainsworth J. Exploring medical students’ early experiences of interacting with the multi-disciplinary team (MDT): A qualitative study. MedEdPublish. 2016;2021(10):30 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10361541/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahmed SK. The pillars of trustworthiness in qualitative research. Journal of Medicine, Surgery and Public Health April 2024. https://www.sciencedirect.com/science/article/pii/S2949916X24000045?via%3Dihub
- 45.Sahlström, M. Patient participation in promoting patient safety – Finnish patients´ and patient safety experts´ views. Dissertation 2019. https://erepo.uef.fi/bitstream/handle/123456789/20435/urn_isbn_978-952-61-2961-7.pdf?sequence=1&isAllowed=y
- 46.Finnish ministry of social affairs and health. The Client and Patient Safety Strategy and Implementation Plan 2022–2026 https://julkaisut.valtioneuvosto.fi/bitstream/handle/10024/164212/STM_2022_12.pdf?sequence=1&isAllowed=y
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The study material is available from the corresponding author on reasonable request.