Abstract
Background
The steep increase in knee arthroplasties in lower- and middle-income countries has increased demand for personalised rehabilitation care. Technology-based rehabilitation programs offer potential to replace or augment conventional face-to-face rehabilitation for providing continuum of care. We aimed to systematically develop a theory, evidence-driven, contextualised, and user-centred mobile health platform for people undergoing knee arthroplasty to facilitate monitoring progress during rehabilitation.
Methods
We followed the UK Medical Research Council’s framework and adopted a behaviour design thinking approach, consisting of five steps; (1) conduct multiple literature reviews and cross-sectional surveys to determine the needs and problems experienced during the rehabilitation phase by healthcare professionals and individuals with replaced knees, (2) identify target behaviours along with barriers and facilitators, integrated within the Capability, Opportunity, Motivation-Behaviour (COM-B) framework, (3) identify intervention functions and components, behaviour change techniques, and features for the mobile application, selected after discussions with orthopaedic surgeons, physiotherapists and behavioural experts, (4) develop a prototype application for end-users, and a web-based platform for healthcare professionals, and (5) pilot test the intervention for end-users’ feedback on usability of the application and to identify possible strategies for implementing the intervention package.
Results
Using the COM-B model, education, training, persuasion, enablement, and modelling were chosen as intervention functions for improving adherence to exercise protocol during early-phase of rehabilitation. The application featured five interlinked components; education, training, goal setting and self-management, communication, and a personalized therapy plan utilising 13 behaviour change techniques. An education booklet, exercise videos, text messaging, video consultation, and a digital tool for measuring range of motion were incorporated into the application. Feedback on the interactive prototype and education material was sought from ten patient volunteers and a physiotherapist. Pilot testing in a convenient sample with broad eligibility criteria (n = 30) indicated importance of digital literacy and dedicated time for remote consultation by healthcare provider within the existing clinical work. Overall, the intervention was well received and valued by the end users.
Conclusion
This paper demonstrates the development of a contextualised digital behavioural intervention grounded in behavioural theory and evidence from literature to improve end-user’s engagement with rehabilitation protocols after knee arthroplasty in lower- and middle-income country context.
Trial registration
Study registered prospectively (on 16 February 2023) at Clinical Trials Registry of India (CTRI/2023/02/049792).
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-024-08003-x.
Keywords: Telemedicine, Telerehabilitation, Knee arthroplasty, Mobile application, Telemonitoring
Background
In India, more than 0.2 million knee arthroplasties were performed in 2020, and with the rising burden of osteoarthritis these numbers are only expected to increase [1]. Rehabilitation following knee arthroplasty is essential to aid early and optimal functional recovery [2, 3]. Home-based unsupervised rehabilitation with clinic visits on a need basis is the typical care pathway followed in most healthcare facilities in India [4]. However, adherence to rehabilitation is poor in the area of musculoskeletal health and documented barriers include, lack of supervision [5], self-efficacy [6], and self-management skills [7]. Hence, some level of supervision either in clinic or at home is required to achieve the benefits associated with knee arthroplasty [8]. Our previous research in India has demonstrated considerable gaps in patients’ understanding about the recovery process, lack of mechanism within health systems to support patients after discharge, and a significant out-of-pocket expenditure incurred by patients for availing physiotherapy services at home [9, 10]. Further, crowded tertiary care hospitals, dependency of the elderly on family members, and disabled-unfriendly transport systems make hospital-based supervised programs challenging [11, 12]. This emphasizes the need for developing a remote monitoring strategy for facilitating continuum of care for this patient population.
Widespread use of smartphones and availability of the internet have resulted in an exponential increase in the development of mHealth interventions to improve the reach and effectiveness of healthcare services globally [13], including in older adults [14] and in India [15]. In India, the key challenges in uptake of such interventions were digital literacy, lack of trust, and poor user experience [15]. Recently published systematic reviews have comprehensively landscaped the digital applications reported in scientific journals in India [16] and their impact on health [17]. They highlighted poor methodological quality in the reporting of these interventions, and only few mHealth interventions evaluated the impact using robust study designs [16–18].
In high-income settings, there is considerable variation in the mode, intensity, and delivery of rehabilitation and monitoring progress after knee arthroplasty [19, 20]. Various home-based rehabilitation strategies comprising of home-visits by a physiotherapist or follow-up by telephone calls have been evaluated for effectiveness [21, 22], and were shown to be cost-effective [23]. They are also perceived as acceptable compared to clinic-based supervision, by both healthcare providers (HCPs) [24, 25] and patients [26, 27]. A recent scoping review highlighted the availability of various digital technologies to augment home-based rehabilitation [18]. In this scoping review, we found telephone calls, mobile apps, and wearable sensors were used for remote monitoring while virtual-augmented reality and sensor-based devices (for gamification) facilitated physical rehabilitation. These technologies also enabled therapy planning, communication (one-way or two-way), provision of education, and remote monitoring. Further, use of technology for monitoring and provision of rehabilitation was shown to be feasible among elderly with high end-user satisfaction [18]. However, this evidence is based on research solely conducted in high- and middle-income countries and there is a lack of published research in this domain from lower- and middle-income countries (LMICs). Thus, the technologies used, and the types of interventions evaluated may not be directly applicable to LMICs and their socio-cultural contexts. For example, most of the technologies had copyright licence or were suitable for integration to their local health systems and the educational content and text messaging were geared for those living alone or in nuclear families. Further, several applications required wearables for monitoring physical activity which is not yet commonly used in LMICs and many of the interventions required the users (patients) to have a display monitor or a tablet [18]. Hence, to address the gap in continuum of care following knee arthroplasty while accounting for local sociocultural and economic context, there is a need for evidence and theory-based mHealth and digital intervention that are co-designed with the needs of end-users front and centre [28, 29]. Following these approaches may result in better engagement with mHealth programs [30, 31].
The TeleRehabilitation after knee ArThroplasty (TReAT) project (CTRI/2023/02/049792) aimed to address the gap in post-knee arthroplasty rehabilitation care in India. Consistent with Medical Research Council recommendations for the development of complex interventions ("develop-test-evaluate-implement") [32], the TReAT project comprised of three phases; formative, pilot, and an evaluation, with an aim to implement in large scale, if found effective. The present paper focused on the formative and pilot phase (develop and test stage of MRC) of the intervention wherein we provide a comprehensive description of the development process of a theory and evidence-driven digital behaviour change intervention and discuss how the findings of the pilot testing informed further refinement of the intervention.
Methods
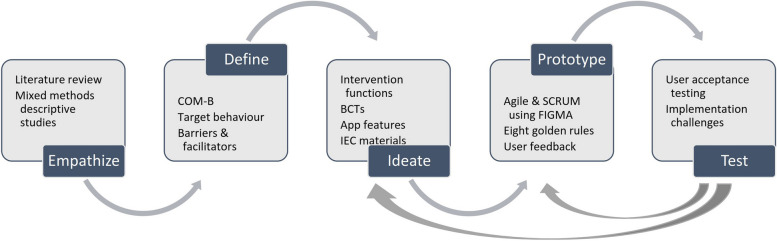
We followed the Behaviour Design Thinking (BDT) model that consists of two interlinked components. ‘Behaviour Design’ refers to diagnosing problems and identifying user needs, and ‘design thinking’ refers to guide the designers for creating user-centric features in the digital application [29]. This was done in several stages using the Behaviour Change Wheel [33], and the IDEAS (Integrate, Design, Assess and Share) framework [34] to ensure engagement with the application leading to behaviour change [35]. The development stages we followed were (1) empathize, (2) define, (3) ideate, (4) prototype, and (5) test. Some of the activities in each stage were iterative to account for user’s need, behaviour, and experiences (Fig. 1). The study protocol was approved by the institutional ethics committee. The study was registered prospectively (on 16 February 2023) at Clinical Trials Registry of India (CTRI/2023/02/049792). Informed consent was obtained from the respondents before data collection.
Fig. 1.
Behaviour Design Thinking approach for the development of the TReAT digital health behavioural intervention
Stages in development of the intervention
Empathize
The objective was to understand HCPs and patients’ needs and identify context specific challenges during the rehabilitation phase. Towards this objective, we concurrently conducted three literature reviews and three cross-sectional surveys at an orthopaedic department within a tertiary care hospital in India. The literature reviews involved, collation of information on post knee arthroplasty rehabilitation challenges as reported by patients and HCPs, identify existing rehabilitation guidelines after knee arthroplasty, and a scoping review of existing mobile and computer-based technologies for delivering and monitoring rehabilitation. A trained research physiotherapist interviewed physiotherapists and orthopaedic surgeons at the hospital. We also approached consecutive patients attending the orthopaedic outpatient department with severe osteoarthritis advised knee arthroplasty or those with recent knee arthroplasty surgery to collect information on experiences and challenges they had after surgery, adherence to rehabilitation physical therapy, health literacy, digital literacy, and home-arrangements they did for facilitating recovery. Further, an e-survey was conducted among practising physiotherapists across India using snowball sampling to understand current physiotherapy practices for post knee arthroplasty rehabilitation.
Each review and survey informed design of the intervention. The literature review of existing physiotherapy practice guidelines and the e-survey of physiotherapists helped guide the development of our post arthroplasty physical rehabilitation protocol. The literature evidence and mixed-methods study on challenges and facilitators to rehabilitation that we have reported elsewhere in detail [10] guided us in defining the target behaviour. The patient survey on home environment modification and health literacy level guided us to develop the education materials. The scoping review of existing mHealth technologies and patient survey on digital literacy guided us to develop the app prototype [18]. Further, our previous experiences in this area also helped to conceptualize the activities of this stage [9, 36–38]. The detailed methods and findings of this formative phase are described in Table 1.
Table 1.
Literature review and primary data collection methodologies for the formative phase
| Objective | Methods | Findings | How did it help? |
|---|---|---|---|
| A literature review to understand challenges faced by patients and healthcare providers during post knee replacement rehabilitation period (1) |
Searched PubMed and Cochrane Library using keywords “knee replacement”, “physical rehabilitation”, “exercises”, “challenges”, “adherence”, “barriers”, “facilitators”, “experiences”, and “challenges” N = 36 relevant articles Articles with participants’ perception = 22 Article with healthcare provider’s perception = 14 |
Participants • Need for psychological & physical support after discharge from hospital, from family members & healthcare providers • Lack of motivation in initiating exercise schedule due to pain Healthcare providers • Delay in returning to routine activities due to lack of periodic monitoring |
Identification of target behaviours along with the barriers & facilitators in following the target behaviour Designing data collection tools for mixed-methods cross-sectional survey |
| A mixed-methods cross-sectional survey to identify challenges in adhering to rehabilitation protocols after knee replacement |
Information captured- • Specific challenges patients and healthcare providers faced during the recovery period and perception about teleconsultation for rehabilitation support (interview of healthcare providers) • A 22-item questionnaire to identify factors related to rehabilitation adherence (knee pain, support from family, focus on recovery, and scheduling of exercises) Quantitative interviews with patients = 79, consecutive sampling Qualitative interviews with patients = 8, convenience sampling Surgeons & physiotherapists = 10 |
• Male: 31 and Female: 48 • Facilitators- intake of pain medications for pain relief and support from family members during recovery phase • Barriers- missing exercises without any reason, unaware of the importance of exercises, and difficulty in commuting to health centre (1) |
Contextual information on the identified target behaviour that can be addressed |
| A systematic literature search on post-acute knee replacement physical therapy |
Searched systematic reviews on Epistemonikos (2) and PubMed on 8th October, 2021 with key words “Knee replacement”, “Knee arthroplasty”, “Rehabilitation”, “Physical therapy”, “Exercise”, and “Physiotherapy” Identified 36 relevant articles |
Clinical practice guidelines (n = 3) (3, 4, 5), Systematic reviews of RCTs reporting evidence for various physiotherapy modalities (n = 28) and Systematic reviews of RCTs reporting evidence for various therapy plans and monitoring mechanisms (n = 30) • Cryotherapy beneficial in post-surgical pain reduction (6) • CPM (7), NMES (8), and TENS (9) little or no effect on pain and function at three months post-surgery • CPM not beneficial in improving ROM of knee joint (7) whereas closed and open kinetic progressive resisted exercises improved ROM as well as muscle strength of knee • Incorporating balance training exercises early recovery phase to improve balance, gait, and function (10) • Monitoring and individualized therapy plan for better patient satisfaction when compared to no monitoring (11) • No significant effect of type of therapy (e.g., aquatic therapy, ergometer cycling) on short- or long-term functional outcomes (12) • Telerehabilitation equally effective in reducing pain and improving function (13) compared to face-to-face • Telerehabilitation: Significant improvement in quality of life, patient satisfaction, and significant decrease in total rehabilitation cost |
Developing post knee replacement physical rehabilitation protocol |
| An e-survey to understand current physiotherapy practices post knee replacement |
Design- Cross-sectional Setting- Online Sample- Practising physiotherapists across India, snowball sampling Information captured- Using study specific questionnaire on therapeutic modalities, type of exercises, most common tools prescribed to patients after knee replacement, clinical parameters opt as progression criteria, perception on importance of prehabilitation and preoperative education for post knee replacement rehabilitation (Supplementary file- Table 1) Total responses- 158 Complete responses- 103 |
• Most used modality for pain relief- Cryotherapy (48%) and use of NEMS (17%) • Ankle, and hip exercises (85.3% and 87.6% respectively) included in the therapy protocol along with knee exercises • Open Kinetic chain, Closed kinetic Chain and combined advised “always” by 42-56% of respondents • Functional exercises “always advised”- walking outdoors (73%), stair climbing (65%) & sit-to-stand exercise (60%) • Most opted clinical parameters to monitor progress- ROM (99%) and muscle strength (98%) • Pre-surgery education advocated by all participants. Proposed topics for education listed in (Supplementary file- Table 2) • 12 to 25 contact sessions between physiotherapists & patients after first month of surgery • Preferred mode- Face-to-face followed by teleconsultation (33%) |
Defining physiotherapy protocols based on current practice patterns |
| A survey to assess level of digital literacy and home environment modifications of patients with knee replacement |
Information captured- Using study specific questionnaire on digital literacy, home environment, and expected support during recovery phase 56 participants, consecutive sampling |
• Fifty-six participants (Male: 17 and Female: 39) • 3/4th owned a personal smart phone • Functions used “daily” with full confidence- Audio calling (86%) and entertainment (48%) • Functions rarely used with no confidence- E-Banking, email and e-shopping functions (Supplementary file-Fig. 1) • Home environment- western style toilet within their homes (100%), railings present inside house (12%) and in bathroom (14%). • Private physiotherapists support either at clinic or home (42%) due to inability to recall exercises and need for physical support during exercises |
Digital literacy – Ensure ease of app interface and choice of patients who can enrol into the program, App manual Home modifications – Developing the contents of education materials |
| A survey to assess health literacy of patients with knee replacement |
Information captured- Using Health literacy questionnaire on nine domains of health literacy The score of each of the nine domains ranged between 1–4 and 1–5 104 participants, consecutive sampling |
• 104 participants (Male: 32 and Female: 72) • Highest score- Ability to actively engage with health care providers [mean 4.0 (SD 0.7)] • Lowest scores- sufficient information to manage their health [mean 2.1(SD 0.7)] and able to appraise available health information [mean 2.5(SD 0.7)(Supplementary file 1: Fig. 1) |
Developing the contents of education materials |
| A scoping review to identify features of existing technologies and to understand the perception of users about the technology for rehabilitation monitoring post-knee replacement (14) |
Searched EMBASE, Medline and PsycINFO via OVID and Cochrane trial for the studies published between 2001–2021, reporting use of mobile application or any other technology for monitoring rehabilitation. Search key terms- “Knee arthroplasty” “Knee replacement”, “mobile”, “web”, “remote sensor”, “computer”, “telerehabilitation”, “m-health” “mobile applications”, “digital technology” and “videoconferencing”. Literature search and screening along with the reference list of eligible articles: Rayyan Protocol of the review: 10.17605/osf.io/srxkc 105 relevant articles |
Use of telerehabilitation methods: 64 studies, Validation studies of sensors for measuring range of motion (ROM) or gait parameters: 28 studies User perception: 38 studies. • Primary functions of remote rehabilitation: education and enablement of performing exercises, goal setting, measuring outcomes such as knee function, pain and ROM, monitoring progress, and communication • End-user involvement during the development stage of the intervention: 4 studies (15, 16, 17, 18) • High levels of satisfaction reported by healthcare providers in use of technology. Reason- reduction in workload, reliability of measurements aided by technology, and ease of reporting and tracking patient data (19, 20, 21) • Patients satisfaction with tele-monitoring- improve access to services, continued support after discharge from hospital without clinic visits, self-management & personalized care by providers (19, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31) • Patients dissatisfaction- lack of in-person examination, and shorter consultation time (19, 27, 31) • Technology use greatly influenced by computer literacy (23, 32) • None of the technologies designed and implemented in lower-middle income countries |
Identification of features and functions of mobile app End-user requirements Lack of evidence from lower-middle income countries context |
1. Pritwani S, Pandey S, Shrivastava P, Kumar A, Malhotra R, Maddison R, et al. Challenges in rehabilitation and continuum of care provision after knee replacement: a mixed-methods study from a low- and middle-income country. Disabil Rehabil. 2023:1–11
2. Epistemonikos: A collaborative, multilingual database of health evidence. https://www.epistemonikos.org/
3. Jette DU, Hunter SJ, Burkett L, Langham B, Logerstedt DS, Piuzzi NS, et al. Physical therapist management of total knee arthroplasty. Physical Therapy. 2020;100 (9):1603-31
4. White NT, Delitto A, Manal TJ, Miller S. The American Physical Therapy Association’s top five choosing wisely recommendations. Phys Ther. 2015;95 (1):9–24
5. Westby MD, Brittain A, Backman CL. Expert consensus on best practices for post-acute rehabilitation after total hip and knee arthroplasty: a Canada and United States Delphi study. Arthritis Care Res (Hoboken). 2014;66 (3):411 − 23
6. Ni SH, Jiang WT, Guo L, Jin YH, Jiang TL, Zhao Y, et al. Cryotherapy on postoperative rehabilitation of joint arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23 (11):3354-61
7. Dávila Castrodad IM, Recai TM, Abraham MM, Etcheson JI, Mohamed NS, Edalatpour A, et al. Rehabilitation protocols following total knee arthroplasty: a review of study designs and outcome measures. Ann Transl Med. 2019;7(Suppl 7):S255
8. Volpato HB, Szego P, Lenza M, Milan SL, Talerman C, Ferretti M. Femoral quadriceps neuromuscular electrical stimulation after total knee arthroplasty: a systematic review. Einstein (Sao Paulo). 2016;14 (1):77–98
9. Zhu Y, Feng Y, Peng L. Effect of transcutaneous electrical nerve stimulation for pain control after total knee arthroplasty: A systematic review and meta-analysis. J Rehabil Med. 2017;49 (9):700-4
10. Zhang W-c, Xiao D. Efficacy of proprioceptive training on the recovery of total joint arthroplasty patients: a meta-analysis. Journal of Orthopaedic Surgery and Research. 2020;15 (1):505
11. Blasco J, Igual-Camacho C, Blasco M, Antón-Antón V, Ortiz-Llueca L, Roig-Casasús S. The efficacy of virtual reality tools for total knee replacement rehabilitation: A systematic review. Physiother Theory Pract. 2021;37 (6):682 − 92
12. Blom AW, Artz N, Beswick AD, Burston A, Dieppe P, Elvers KT, et al. Programme Grants for Applied Research. Improving patients’ experience and outcome of total joint replacement: the RESTORE programme. Southampton (UK): NIHR Journals Library Copyright © Queen’s Printer and Controller of HMSO. ; 2016
13. Seron P, Oliveros M-J, Fuentes-Aspe R, Gutierrez-Arias R, Torres-Castro RC, Merino-Osorio C, et al. Effectiveness of Telerehabilitation in Physical Therapy: A Rapid Overview. Physical therapy. 2021;101 (6)
14. Pritwani S, Shrivastava P, Pandey S, Kumar A, Malhotra R, Maddison R, et al. Mobile and Computer-Based Applications for Rehabilitation Monitoring and Self-Management After Knee Arthroplasty: Scoping Review. JMIR Mhealth Uhealth. 2024;12:e47843
15. Hussain MS, Li J, Brindal E, van Kasteren Y, Varnfield M, Reeson A, et al. Supporting the delivery of total knee replacements care for both patients and their clinicians with a mobile app and web-based tool: Randomized controlled trial protocol. JMIR Research Protocols. 2017;6 (3)
16. Lam AWK, Varona-Marin D, Li Y, Fergenbaum M, Kulic D, Ananthanarayan A, Ayoade, Burns, Burns, Costa, Friedrich, Gockley, Houmanfar, Huang, Kimel, Lam, Lange, Li, Lin, Lin, Lin, Lindeman, Norkin, Piqueras, Rosati, Schmitz, Shin, Singh, Stewart, Sucar, Uzor, Yeh. Automated rehabilitation system: Movement measurement and feedback for patients and physiotherapists in the rehabilitation clinic. Human-Computer Interaction. 2016;31 (3):294–334
17. Argent R, Slevin P, Bevilacqua A, Neligan M, Daly A, Caulfield B. Clinician perceptions of a prototype wearable exercise biofeedback system for orthopaedic rehabilitation: A qualitative exploration. BMJ Open. 2018;8 (10)
18. Stauber A, Schusler N, Schurholz N, Bruns D, Osterbrink J, Nestler N, et al. RECOVER-E - A mobile app for patients undergoing total knee or hip replacement: Study protocol. BMC Musculoskelet Disord. 2020;21 (1):71
19. Parkes RJ, Williams DH, Palmer J, Wingham J. Is virtual clinic follow-up of hip and knee joint replacement acceptable to patients and clinicians? A sequential mixed methods evaluation. BMJ open quality. 2019;8 (1):e000502
20. Neligan M, Daly A, Bevilacqua A, Argent R, Slevin P, Caulfield B. Clinician perceptions of a prototype wearable exercise biofeedback system for orthopaedic rehabilitation: A qualitative exploration. BMJ Open. 2018;8 (10):e026326
21. Onyeukwu C, Smith CN, Oh A, McClincy MP, Bell KM, Devito Dabbs A, et al. A Portable System for Remote Rehabilitation Following a Total Knee Replacement: A Pilot Randomized Controlled Clinical Study. Sensors (Basel, Switzerland). 2020;20 (21)
22. Correia FD, Nogueira A, Magalhães I, Guimarães J, Moreira M, Barradas I, et al. Medium-term outcomes of digital versus conventional home-based rehabilitation after total knee arthroplasty: Prospective, parallel-group feasibility study. JMIR Rehabilitation and Assistive Technologies. 2019;6 (1)
23. Russell TG, Buttrum P, Wootton R, Jull GA. Low-bandwidth telerehabilitation for patients who have undergone total knee replacement: preliminary results. Journal of telemedicine and telecare. 2003;9:S44-7
24. Tousignant M, Boissy P, Moffet H, Corriveau H, Cabana F, Marquis F, et al. Patients’ satisfaction of healthcare services and perception with in-home telerehabilitation and physiotherapists’ satisfaction toward technology for post-knee arthroplasty: an embedded study in a randomized trial. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2011;17 (5):376 − 82
25. van Kasteren Y, Freyne J, Hussain MS. Total Knee Replacement and the Effect of Technology on Cocreation for Improved Outcomes and Delivery: Qualitative Multi-Stakeholder Study. Journal of medical Internet research. 2018;20 (3):e95
26. Kairy D, Tousignant M, Leclerc N, Cote A-M, Levasseur M. The patient’s perspective of in-home telerehabilitation physiotherapy services following total knee arthroplasty. International Journal of Environmental Research and Public Health. 2013;10 (9):3998–4011
27. LeBrun DG, Malfer C, Wilson M, Carroll KM, Wang M, V., Mayman DJ, et al. Telemedicine in an Outpatient Arthroplasty Setting During the COVID-19 Pandemic: Early Lessons from New York City. HSS Journal. 2021;17 (1):25–30
28. Szots K, Konradsen H, Solgaard S, Bogo S, Ostergaard B. Nurse-led telephone follow-up after total knee arthroplasty–content and the patients’ views. Journal of clinical nursing. 2015;24 (19):2890-9
29. Grant S, Judge A, Tonkin EL, Blom AW, Whitehouse MR, Gooberman-Hill R, et al. Using home sensing technology to assess outcome and recovery after hip and knee replacement in the UK: The HEmiSPHERE study protocol. BMJ Open. 2018;8 (7):e021862
30. Massip M, de Batlle J, Barbe F, Torres G, Vargiu E, Miralles F, et al. Implementing Mobile Health-Enabled Integrated Care for Complex Chronic Patients: Patients and Professionals’ Acceptability Study. JMIR mHealth and uHealth. 2020;8 (11):e22136
31. Marsh J, Bryant D, MacDonald SJ, Naudie D, Remtulla A, McCalden R, et al. Are patients satisfied with a web-based followup after total joint arthroplasty? Clinical orthopaedics and related research. 2014;472 (6):1972-81
32. Glinkowski W, Cabaj D, Kostrubała A, Krawczak K, Górecki A, editors. Pre-surgery and post-surgery telerehabilitation for hip and knee replacement - Treatment options review and patient’s attitudes towards telerehabilitation. eChallenges e-2010 Conference; 2010
Define
We identified five target behaviours based on our literature review findings namely, setting up a routine to perform exercise, following pain reduction plan, reducing sedentary behaviour, increasing physical activity, and avoiding activities that harm recovery. We chose the most promising behaviour “adhering to exercises” which was relevant for the immediate post-operative period and could impact long-term behaviour. We considered pain management as a sub-behaviour as post-operative knee pain and adherence to exercises were related to each other. We did not choose decrease in time spent in sedentary behaviour and increase in physical activity as they are relevant in the later stages of recovery. One researcher extracted the finding from the literature related to rehabilitation challenges and grouped the findings using the COM-B framework and two other researchers independently verified the categorisation. Upon iterative discussions the barriers and facilitators were schematically summarised which formed the basis for developing tools and topic guides for conducting the mixed-methods study (Table 1). The quantitative and qualitative findings from patient and HCPs were triangulated to identify behavioural problems and challenges in adhering to rehabilitation protocols (Refer to column A & B of Table 2). Further details of COM-B exercise are reported elsewhere [33].
Table 2.
Mapping of behavioural problems with intervention functions, behaviour change techniques, and mobile app features
| (A) Barriers/facilitators (identified by patient or Physiotherapist)* | (B) COM-B | (C) Intervention function | (D) BCT | (E) App features | (F) Function | (G) App icons |
|---|---|---|---|---|---|---|
|
• Pain interference to perform the exercise (pt and PT) • Lack of information on relationship between pain and exercise (pt) |
Physical capability Reflective motivation |
Education Enablement |
• Adding objects to the environment • Self-monitoring of outcome of the behaviour • Information about health consequences |
Education (knowledge) | An e-booklet consisting of context specific information related to preparing oneself for surgery, knowing about recovery process, and important do and don’ts to safeguard the new knee | Knowledge |
|
• Inadequate skills to perform exercise (PT) • Difficulty to retain information on exercises & advice (pt and PT) |
Physical capability Psychological capability |
Training Enablement |
• Instruction on how to perform the behaviour • Adding objects to the environment |
Training (skill) | Audio visual aids for patients to perform exercises for range of motion, muscle strength, balance, and function | Exercise videos |
|
• Lack of awareness about importance of exercises for recovery (PT) • Lack of motivation in patients for following the exercises (PT) |
Psychological capability Reflective motivation Automatic motivation |
Education Persuasion |
• Self-monitoring of the behaviour • Prompt/cues • Salience of consequences • Framing/reframing |
e-diary and goal setting (self-management and motivation) |
An e-diary to self-monitor pain, range of motion, knee function, activity level, and adherence to exercises. Goal setting of desired activity level at the start of therapy along with rewards on completion of exercise and activity goals. Motivational messages |
My Diary & Range of motion |
|
• Distress due to pain following surgery (pt) • Poor accessibility or high cost to avail physiotherapy services and devices (pt) • Difficulty in commuting to the referral hospital (pt) |
Reflective motivation Environmental opportunity |
Persuasion Enablement |
• Verbal persuasion about capability • Adding objects to the environment |
e-connect (opportunity) | Two-way synchronous and asynchronous consultation via audio, video, and text features | Message & Appointment |
|
• Need for personalized support and comprehensive information (pt and PT) • Need for continued support from health care provider after discharge to home (pt and PT) • Lack of motivation in patients for following the exercises (PT) |
Environmental Opportunity Automatic motivation Reflective motivation |
Enablement Persuasion |
• Social support (practical) • Goal setting (behaviour) • Feedback on outcome of the behaviour |
e-monitor (opportunity) | Facilitating continuum of care between health care provider (surgeon and physiotherapist) and patients by modifying treatment plan based on the progress. |
Progress Therapy plan |
| • Need for physical and psychological support from family (pt) |
Social opportunity Reflective Motivation |
Education Enablement |
• Social support (unspecified) • Social support (emotional) |
e-support (opportunity) | Family members/caregiver will be sensitized to recovery needs via education material, exercise videos. They can also access progress and goals achieved by patient | Family member interface |
Definition of intervention functions: Education- Increasing knowledge or understanding Persuasion- Using communication to induce positive or negative feelings or stimulate action Training- Imparting skills Modelling- Providing an example for people to aspire to or imitate Enablement- Increasing means/reducing barriers to increase capability or opportunity
PT Physiotherapist, pt patient
*Collated from both literature review and primary data collection from individuals undergoing knee replacement, family members and physiotherapist
Ideate
The objective of this stage was to identify intervention functions and ideate innovative solutions for enabling the target behaviour. From a list of nine defined intervention functions [39] (training, education, persuasion, modelling, environmental restructuring, incentivization, restriction, enablement, and coercion), we selected education, training, persuasion, enablement, and modelling using the APEASE (Acceptability, Practicability, Effectiveness, Affordability, Side effects or safety, Equity) criteria [33]. For each of the intervention functions, a set of 14 salient Behaviour Change Techniques (BCTs) from the BCTv1 taxonomy [39] were identified that would act as a mechanism of change to bring about desired behaviour through a digital interface. To validate this process, a workshop was conducted by the research team with a behavioural science expert (Refer to column C & D of Table 2).
The scoping review [18] conducted at the empathize stage, and several mind-mapping sessions conducted by the research team with the clinical team helped in identifying potential features for the app that would deliver the intervention components (Refer column E, and F of Table 2). In summary, the intervention components that emerged were, providing education to patients and family members about recovery following knee arthroplasty, skill building for performing exercises, self-management and goal setting for following rehabilitation protocol, enabling remote communication with HCPs, and enabling HCPs to monitor patient progress remotely and modify personalised exercise plan.
A pictorial education booklet of twelve chapters spanning from pre-operative to late recovery phase was developed in English and Hindi (Supplementary file- Fig. 2). Feedback from researchers and non-researchers was sought using the Suitability Assessment of materials tool [40] and the average suitability assessment score for the booklet was 94.9%. Qualitative interviews conducted with patients and caregivers demonstrated high level of comprehension and relevance of the material to those undergoing knee arthroplasty. Exercise videos for improving range of motion, lower-limb muscle strength, balance, gait, function, and endurance (n = 46 videos) were developed in English and Hindi (Supplementary file- Fig. 3). Qualitative feedback from patients and caregivers visiting the hospital (convenience sampling) indicated the video quality was good and comprehensible. We developed short text messages in English and Hindi that aimed to orient, motivate, notify, and remind either the patients, HCP or family members (Supplementary file- Table 3).
Prototype
The objective of this stage was to develop a minimal viable product with features that could deliver the intervention components. The app (TReAT app) was developed on a platform previously used for delivering a clinical decision support system [41]; compatible for devices running Android 8.0 and above. A multidisciplinary team comprising of HCPs, public health researchers, software developers, UI-UX designer and project manager was established to facilitate a balance between system requirements, such as, designing features for an effective intervention aligned with the existing in-hospital clinical workflow and user requirements such as, addressing the communication gap between the HCPs and patients. The HCPs recommended a mechanism to measure range of motion remotely for monitoring progress. Hence, we utilised the inherent capabilities of gyroscope and accelerometer in a mobile device to develop an app to measure knee range of motion with the aim to incorporate it within the main application.
Various prototyping tools, approaches, and aids were used in the user interface design process of the app. Simple flowcharts were developed in draw.io to outline the app’s structure that served as a foundation for creating low-fidelity wireframes on Figma [42]. These wireframes underwent multiple iterations and feedback with respect to layout, colour, content, navigation, and clickable elements before they were transformed into high fidelity wireframes with content and user flow. The app developmental cycle was structured into 2-week sprints following scrum methodology [43]. The team followed the standard prototype aids such as Nielsen’s 10 usability heuristics [44] and eight golden rules [45].
The app development team along with the members from the research team performed multiple rounds of alpha testing of the app using approaches such as functionality, useability, stress, capacity, and timing. Following the principles of BDT [46], feedback on visual appeal and ease of navigation, comprehensibility of the icon names and menu layout was obtained from ten volunteers (patient = 4 and caregiver = 6; male = 7 and female = 3) aged 33–66 years. They identified a few spelling errors in the app, suggested a zoom-in feature to improve readability in the knowledge material, and suggested a manual as a self-guide for navigating through the app.
Test
The objective of the user acceptance testing was to assess end users’ experiences and expectations and gain insights for implementing the intervention. Consecutive adults (n = 41) advised, scheduled, or who had undergone knee arthroplasty were approached, and 30 consenting participants were enrolled if they or their caregiver had an android smartphone. A member of the research team maintained a diary of all observations made during enrolment and periodic check-in calls made to the enrolled participants. A semi-structured interview guide (Supplementary file-Tables 4, 5 and 6) was developed based on the consolidated framework of implementation research [47]. After at least one month of app usage, 13 willing participants with varying levels of app usage were interviewed via telephone (Supplementary file- Fig. 4). Feedback was obtained from the physiotherapists. Both activities were done by a researcher not involved in patient enrolment. For the analysis of the qualitative interviews, audio transcripts were transcribed verbatim and translated. Two researchers independently coded the transcripts deductively using a priori identified codes and inductively for new emerging codes. Following discussion, codes were grouped into overarching a priori themes. Physiotherapist feedback was grouped into thematic categories.
Results
Description of the app-based intervention
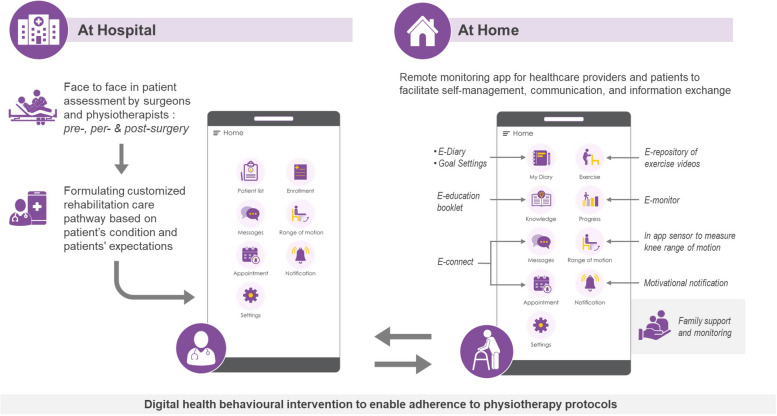
The TReAT intervention developed following BDT principles, aims to facilitate remote monitoring and self-management, promote information and communication exchange between healthcare providers and patients/family members (Fig. 2). It consists of 5 interlinked components-
Fig. 2.
Digital health behavioural intervention to enable adherence to physiotherapy protocols
Education (knowledge): e-education booklet.
Training (exercises): e-repository of exercise videos.
Self-management and goal setting (my diary, my progress, a family member interface): e-diary to self-monitor progress (pain, range of motion, knee function, activity, and exercise adherence), motivational messages on achieving desired goals, and sensitization of family members to recovery needs.
Communication (messages and appointment): e-connect via two-way synchronous and asynchronous consultation via audio, video, and text.
Therapy plan (progress): e-monitoring of progress by HCP to modify treatment plan.
Intervention components are available in the app via patient, family member, and healthcare provider interfaces (Supplementary file- Fig. 5). The app supports both Hindi (local language) and English with the possibility of expanding to other languages. The patients can be enrolled any time before or after the surgery and intervention components such as the education contents and exercises are suitable for both pre- and early stage (3 months) post arthroplasty rehabilitation. The HCP can store basic medical information in the app at the time of enrolment, following which they can prescribe exercises depending upon patient requirement and expectations. The therapy can be updated along with the medical information at any point of time. The app is programmed to send automatic motivational messages at a pre-specified frequency depending on the days since surgery.
The patient and family member can access the education material under the “Knowledge” section. The physiotherapist can assign specific exercises which are grouped under pre-surgical phase and four post-surgical phases. The physiotherapist can also add and edit the number of repetitions, sets, and the time in the day (morning/afternoon/evening) with a provision to add any additional notes for the patient. Only the prescribed exercises can be seen by the patients and family members under the “Exercise” tab. They also receive a notification when the physiotherapist updates the therapy plan.
To facilitate self-monitoring, patients can complete self-reported pain, activity, knee function, and exercise adherence under “My Diary” at specified intervals. Knee pain is captured using Numeric Rating Scale (NRS) [48] (0-No pain, 10-Worst pain imaginable), current activity level using lower extremity activity scale (LEAS) [49], knee function using Knee injury and Osteoarthritis Outcome Score for joint replacement (KOOS, JR) [50]. Pain levels can be entered daily whereas activity and knee function can be entered once in every 15 days for a period of three months. Patients are expected to enter “Yes” or “No” against each of the prescribed exercises daily. They will also receive pop-up messages as reminders to complete the diary. Patients or family member can measure knee range of motion using the “Range of motion” in-app feature. A trend graph of responses to patient reported pain, activity, knee function, and exercise adherence along with flexion and extension of the knee joint can be visualised by the patient, family member and HCP under the “Progress” tab.
One-to-one text and audio messages, still images, and video messages can be exchanged between the HCPs, patients, and family members via the “Messages” section. Patients can request for a video consultation with the HCP via messaging. Under the “Appointment” section, when the HCP schedules an appointment, the patient or family member will be notified. An automatic reminder will also be sent 30 min before the scheduled video consultation. The HCP has an option to cancel the appointment, if required.
End users experience and recommendations
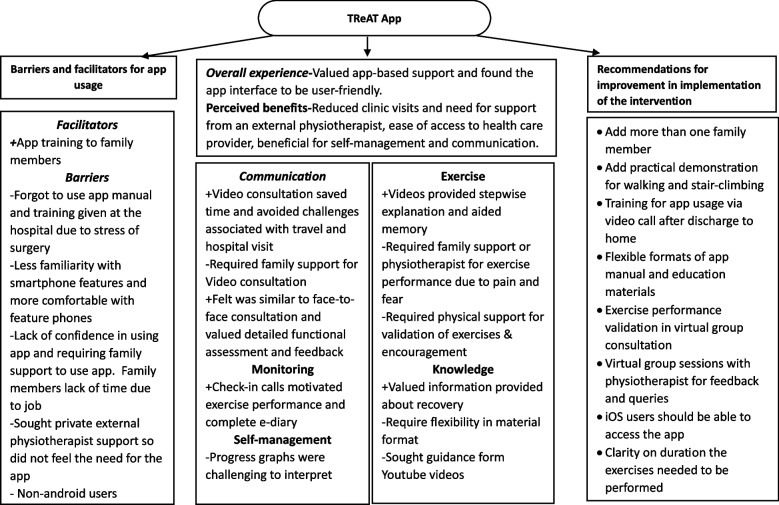
The mean age of the participants (n = 30) was 66.6 years (SD = 7.77) and 80% were women (Supplementary file- Table 7). Most (n = 27) patients had undergone knee arthroplasty, and three were advised or scheduled for surgery for one or both knees. Of the thirteen participants who provided feedback, two had used more than or at least 5 features of the app, seven were partial users (used > 1 but less than 5 features) and four were non-users. Overall, the patients and their family members valued the app-based rehabilitation support. They found it useful as it reduced their clinic visits, need for an in-person physiotherapist, and enabled remote access to an HCP (Fig. 3). Most of them recommended the app for self-management and communication (Supplementary File-Table 8).
“…. The person who visits me after my knee surgery I tell them about this app…. I used to show them the app too that everything is given in this app. How you must do the exercises everything is there. If someone can do the exercises by self, I don’t think they will need help of private PT.” (P130, 54 F, Left Unilateral Knee Replacement).
Fig. 3.
Barriers and facilitators for app usage by patients and family members with recommendations for improvement in intervention
They perceived ‘exercises’, ‘knowledge’, ‘my diary’ and ‘video consultation’ as the most useful features. However, they suggested a briefer app user manual, to have video demonstrations for walking and stair climbing within the app, and possibility of virtual exercise sessions with a physiotherapist.
“Exercises which you have given are really very nice. The steps which you have mentioned are helpful. If someone forgets it, then can have a look again in the video and they will understand it. And secondly, that knowledge section in which you have mentioned how one must take steps, how to climb stairs, how to tie, brace how to tie weights, all these were very useful. I have physiotherapist at home but for those who doesn’t have it is very useful”. (P102, 73 M, Right Total Knee Replacement)
Despite the support provided by the app, the need for physical support by a physiotherapist, especially during the early phases of recovery was often mentioned by patients and family caregivers. This was also evident since 11 people (out of 13 interviewed) had sought physiotherapy consultation at home or at a clinic.
“…because while seeing in the book if we want to bend our knees, we shall do it, but we will not bend it too much. My son is also a physiotherapist but when we hire physiotherapist from outside, they bend knees to the level that is possible, and it allows good movement. They put pressure to straighten your knees. We cannot do it by self without physiotherapist. On seeing we can do normal exercises but when you must bend knees you will not do it to its maximum. They put pressure and made it happen. One more thing when you exercise by yourself you will get tired in half an hour but when physiotherapist comes, they will make you do for an hour. They will do every movement. They will bend it straighten it. (P130, 54F, Left Unilateral Knee Replacement)
Eleven patients out of thirty, did not use the app, even after successful app installation. They needed family support to operate the app since they were not comfortable in using smartphones. Further, those who had appointed an attendant or physiotherapist did not perceive the need for the app.
“… actually, to be honest… had downloaded in my phone, but I couldn’t do it. My kids are outside, if they would have been there, they would have opened and showed it to me.” (P104, 53 F, not yet scheduled surgery).
“I do not use it… I have this person (attendant) who make me to exercise four times a day. I walk now with minimum pain. So, I didn’t feel need to use that app. This app will be helpful to the people who do not have any attendant or someone like this what I feel.” (P113, 76 F, B/L TKR).
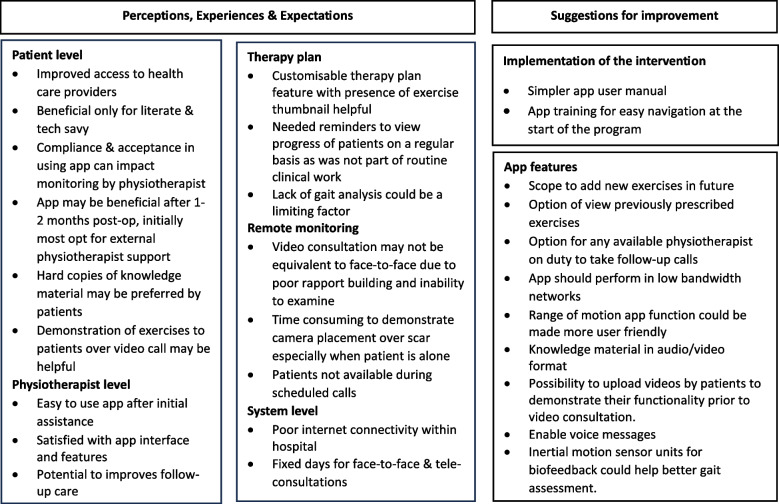
Physiotherapists found the customizable therapy plan with exercise thumbnails to be the most useful features and felt the graphical summary of patient progress would help to monitor and provide care. They strongly believed that end user digital literacy was crucial to make users more compliant in using the app and in completing the diary. They recommended that patients should be trained well in using the app before discharge to home, including positioning of the phone during video consultations. They also recommended an option to add newer exercises or any patient relevant information in the app. Figure 4 provides further details of the experiences and expectations reported during the feedback interviews.
Fig. 4.
Experiences & Expectations of physiotherapists to provide routine care using TReAT mHealth application
The insights we gathered about implementation of the intervention for the trial phase were, imparting training to use the app at the start of the program and during post-surgery teleconsultations in addition to a user manual. Moreover, the participant information materials should be in electronic and paper format.
Discussion
In this manuscript we provide a step-by-step description of the design and development of a technology-based intervention with a user-centric approach wherein we identified the target behaviour and intervention components using the COM-B model and adopted the BDT approach for designing the TReAT app. This app aims to support rehabilitation and facilitate continuum of care for individuals undergoing knee arthroplasty. While smartphones and other wearable technologies are in use especially in high-income countries for health promotion and rehabilitation following knee arthroplasty, few studies reported information on how they were systematically developed [18]. Our effort was to design a context-specific mHealth intervention based on existing evidence, and theory using a systematic approach. However, in the pilot test only just above half the participants used the app with varying levels of engagement.
Findings in context
The context in which this mHealth intervention has been developed and will be implemented differs significantly from those developed for high-income countries. In India, patients first contact, with a physiotherapist typically occurs after hospital admission, usually a day before surgery. There are no routinely followed prehabilitation protocols for knee arthroplasty and postoperative patient-doctor contact time is minimal. This leads to patients and their family members being unaware of the expectations of the recovery process, especially the expected levels of pain. This lack of awareness could negatively impact their outlook to early mobilisation and exercise therapy, which are crucial for better and early functional recovery. Unlike, in western population where returning to independent living is a crucial outcome following arthroplasty, freedom from knee pain and ability to carry on self-care activities within the confines of their home were the key expectations from our patient population. This could be attributed to the considerable support they get from their family and friends. Additionally, due to limited digital literacy among this demography, there is a higher dependence on younger literate relatives. Hence, involving family members was a unique component of our intervention compared to others reported in literature [18]. Further, after suture removal most individuals seek advice from local physiotherapists, who may not follow evidence-based protocols. There have been also instances of unqualified attendants being involved in rehabilitation and it is not uncommon for paid physiotherapists to visit the homes of patients every day for three months. Thus, the intervention intends to provide reliable and correct information for this population and aid in continued communication, and progress monitoring.
Engagement with the TReAT app
For our intervention to successfully achieve its goal, consistent engagement with the app functions by the HCP and the patient or family member will be crucial. These include, reading the education content, communicating through the messaging function, attending the remote consultation at the scheduled time, making use of the exercise videos as an aid for exercise performance and making entries in the diary to objectively view exercise compliance and recovery progress. There are several reasons which could have led to suboptimal engagement in our pilot study. First, we enrolled all patients with smartphones irrespective of their digital literacy which affected their app usage. Hence, it is evident that while evaluating this intervention in a larger comparative trial, at the cost of generalisability, digital literacy will be a key inclusion criterion. Moreover, despite the remote support offered by the app, need for in-person physical support could have undervalued the other functions of the app such as monitoring progress and remote communication. This could be addressed by further explaining the benefits of various components of this intervention rather than focusing only on the exercise component. For HCPs, the need to have another device where the app was installed and poor engagement from the patients’ end could have reduced the HCP’s engagement with the app. In the updated version of the app, the video calling feature will be inbuilt within the app, to reduce using third party sources such as WhatsApp that may divulge the phone numbers of the HCPs. Making the app compatible for iOS will also help in increasing the reach of this intervention among varied smartphone users. Additionally, HCPs found scheduling time for teleconsultations alongside the routine hospital work to be challenging. We believe this is dependent on the motivation levels of the participating physiotherapist and their buy-in for this approach will be required. Ensuring patients and family members are familiar with app navigation before discharge to home, providing a physical copy of education materials alongside the electronic version in the app, motivating patients to engage with the education materials and convincing them of the importance of e-diary will be key requirements during implementation of the trial.
Strengths and limitations
Several frameworks have been proposed to aid design of technology-based interventions [32, 51] that can facilitate replication of successful mHealth behaviour change interventions in varied contexts. However, only few studies have provided adequate description of behavioural theory and frameworks that formed the basis of the intervention components [52, 53]. Adopting a multidisciplinary systematic iterative approach and engaging end users for feedback were the key strengths of our study. However, there were several limitations in the approach we used. One of the limitations, was that patients and family caregivers were engaged only in the later stages of the development (clickable prototype) rather than involving them in co-designing the intervention components. This was due to feasibility issues associated with approaching participants seeking treatment from a publicly funded tertiary care busy hospital. It was challenging to coordinate the place and time availability of various stakeholders that was required for co-designing. We did not explore the feasibility of having an online co-design workshop. Additionally, due to the lack of cross- cultural validated tools for objectively measuring usability and acceptability, we did not use quantitative scores for usability. The self-reported extent of use could have introduced some bias especially for functions that could not be confirmed from the app analytics. For example, viewing the videos and reading the knowledge materials. Further, behaviours such as promoting physical activity and reducing sedentary behaviour were also important long-term outcomes that emerged from the literature review. However, for the current study we focussed on adherence to rehabilitation protocols as the main behaviour which is relevant in the initial months of recovery. Finally, even though the study was performed at a public tertiary care referral hospital with a diverse patient population, testing the application in a private healthcare setup would have provided information from a different sociodemographic profile.
Further initiatives
The pilot testing in real-life setting gave very useful insights for improving the features as well as to identify implementation challenges prior to conducting the randomised controlled trial for evaluating clinical and cost effectiveness of this rehabilitation strategy. While both end-users found the app useful, digital literacy was the single most important factor that determined the extent of use by patients and family members. Integration of remote consultations with routine activities will require change at a higher level in the hospital administration. To get their buy-in we need to first show some clinical benefit and higher patient satisfaction. Hence, when we evaluate the intervention, we will also measure several of the process indicators related to context, reach, fidelity, and acceptability of the intervention that will inform scope for further scalability. The scope for addition of intervention components to promote physical activity and reduce sedentary behaviour in this population and wearable sensors for gait analysis during remote monitoring will require further formative work.
Conclusion
The components of this mHealth intervention have been developed to suit the local needs and feasibly address the current gaps existing in rehabilitation care. Evaluation using a randomised controlled trial will generate crucial evidence on effectiveness, usability, and acceptability of such a strategy which is currently missing in the context of LMICs.
Supplementary Information
Acknowledgements
We would like to thank graphic design specialists, Mr. Jason Dass and Ms. Anshu Manchanda at The George Institute for Global Health, India for designing the graphics in the mobile application. We thank all the study participants, physiotherapists and surgeons who provided feedback on the mobile application and the education materials.
Abbreviations
- mHealth
Mobile health
- COM-B
Capability, Opportunity, Motivation-Behaviour
- BDT
Behaviour Design Thinking
- IDEAS
Integrate, Design, Assess, and Share
- APEASE
Acceptability, Practicability, Effectiveness, Affordability, Side-effects, and Equity
- BCT
Behaviour change thinking
- TReAT
Telerehabilitation after Knee Arthroplasty
- ROM
Range of Motion
- NRS
Numeric Rating scale
- KOOS
Knee injury and osteoarthritis outcome score
- KOOS-JR
Knee injury and osteoarthritis outcome score for joint replacement
- UI-UX
User interface- user experience
Authors' contributions
Conceptualization: ND, RM, RalphM; Funding acquisition: ND; Methodology: ND, RM, SP, PS; Data curation: SP, SG, PS ; Access to patients: RM, AK, AS, SB, NS; Formal analysis: ND, SP, SG, PS, AK ; Project administration: SP, PS, AK; ; Software: DP, SrG, RJ; Writing – Original Draft Preparation- SP, SG, PS; Writing – Review & Editing: ND, RalphM, RM; All authors reviewed the manuscript and ND approved the final manuscript.
Funding
This work was supported by DBT/Wellcome Trust India Alliance under grant number [IA/CPHI/20/1/505224].
Data availability
Study data will be made available upon reasonable request to Niveditha Devasenapathy and after ethical approval.
Declarations
Ethics approval and consent to participate
The project was approved by The George Institute Ethics Committee, The George Institute for Global Health, India (Ref-25/2022) and Institute Ethics Committee, All India Institute of Medical Sciences, Delhi (IEC-856/04.11.2022). Participants were interviewed after obtaining written informed consent.
Consent for publication
Written informed consent for the publication of potentially identifiable images of the professionals was obtained in the study. The study contains no identifiable data of research participants.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sabhya Pritwani and Siaa Girotra are shared first authors.
References
- 1.Vaidya SV, Jogani AD, Pachore JA, Armstrong R, Vaidya CS. India joining the world of hip and knee registries: Present Status-A Leap Forward. Indian J Orthop. 2020;55(Suppl 1):46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Artz N, Elvers KT, Lowe CM, Sackley C, Jepson P, Beswick AD. Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis. BMC Musculoskelet Disord. 2015;16:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang X, Hunter DJ, Vesentini G, Pozzobon D, Ferreira ML. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1):506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aseer PAL, Maiya GA, Kumar MM, Vijayaraghavan PV. Content validation of total knee replacement rehabilitation protocol in Indian population. J Clin Diagn Res. 2017;11(6):YC05-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pua YH, Seah FJ, Seet FJ, Tan JW, Liaw JS, Chong HC. Sex differences and impact of body Mass Index on the Time Course of Knee Range of Motion, knee strength, and Gait Speed after total knee arthroplasty. Arthritis Care Res (Hoboken). 2015;67(10):1397–405. [DOI] [PubMed] [Google Scholar]
- 6.Magklara E, Burton CR, Morrison V. Does self-efficacy influence recovery and well-being in osteoarthritis patients undergoing joint replacement? A systematic review. Clin Rehabil. 2014;28(9):835–46. [DOI] [PubMed] [Google Scholar]
- 7.Buus AAO, Hejlsen OK, Dorisdatter Bjornes C, Laugesen B. Experiences of pre- and postoperative information among patients undergoing knee arthroplasty: a systematic review and narrative synthesis. Disabil Rehabil. 2021;43(2):150–62. [DOI] [PubMed] [Google Scholar]
- 8.Buhagiar MA, Naylor JM, Simpson G, Harris IA, Kohler F. Understanding consumer and clinician preferences and decision making for rehabilitation following arthroplasty in the private sector. BMC Health Serv Res. 2017;17(1):415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malik IV, Devasenapathy N, Kumar A, Dogra H, Ray S, Gautam D, et al. Estimation of expenditure and challenges related to rehabilitation after knee arthroplasty: a hospital-based cross-sectional study. Indian J Orthop. 2021;55(5):1317–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pritwani S, Pandey S, Shrivastava P, Kumar A, Malhotra R, Maddison R et al. Challenges in rehabilitation and continuum of care provision after knee replacement: a mixed-methods study from a low- and middle-income country. Disabil Rehabil. 2023:1–11. [DOI] [PubMed]
- 11.Kumar SG, Roy G, Kar SS. Disability and rehabilitation services in India: issues and challenges. J Family Med Prim are. 2012;1(1):69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Irving G, Neves AL, Dambha-Miller H, Oishi A, Tagashira H, Verho A, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7(10):e017902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organisation. mHealth: new horizons for health through mobile technologies. 2011.
- 14.Parker SJ, Jessel S, Richardson JE, Reid MC. Older adults are mobile too!Identifying the barriers and facilitators to older adults’ use of mHealth for pain management. BMC Geriatr. 2013;13:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.PricewaterhouseCoopers Private Limited CoII. How mHealth can revolutionise the Indian healthcare industry 2017. Available from: https://www.pwc.in/assets/pdfs/publications/2017/how-mhealth-can-revolutionise-the-indian-healthcare-industry.pdf.
- 16.Bassi A, John O, Praveen D, Maulik PK, Panda R, Jha V. Current status and future directions of mHealth interventions for health system strengthening in India: systematic review. JMIR mHealth uHealth. 2018;6(10): e11440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joshi V, Joshi NK, Bhardwaj P, Singh K, Ojha D, Jain YK. The health impact of mHealth interventions in India: systematic review and meta-analysis. Online J Public Health Inf. 2023;15:e50927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pritwani S, Shrivastava P, Pandey S, Kumar A, Malhotra R, Maddison R, et al. Mobile and Computer-based applications for Rehabilitation Monitoring and Self-Management after knee arthroplasty: scoping review. JMIR Mhealth Uhealth. 2024;12: e47843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oatis CA, Li W, DiRusso JM, Hoover MJ, Johnston KK, Butz MK et al. Variations in Delivery and Exercise Content of Physical Therapy Rehabilitation Following Total Knee Replacement Surgery: A Cross-Sectional Observation Study. Int J Phys Med Rehabil. 2014;Suppl 5. [DOI] [PMC free article] [PubMed]
- 20.Naylor JM, Hart A, Harris IA, Lewin AM. Variation in rehabilitation setting after uncomplicated total knee or hip arthroplasty: a call for evidence-based guidelines. BMC Musculoskelet Disord. 2019;20(1):214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jansson MM, Rantala A, Miettunen J, Puhto AP, Pikkarainen M. The effects and safety of telerehabilitation in patients with lower-limb joint replacement: a systematic review and narrative synthesis. J Telemed Telecare. 2022;28(2):96–114. [DOI] [PubMed] [Google Scholar]
- 22.Buhagiar MA, Naylor JM, Harris IA, Xuan W, Adie S, Lewin A. Assessment of outcomes of Inpatient or Clinic-based vs home-based Rehabilitation after total knee arthroplasty: a systematic review and Meta-analysis. JAMA Netw Open. 2019;2(4):e192810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li D, Yang Z, Kang P, Xie X. Home-based compared with Hospital-Based Rehabilitation Program for patients undergoing total knee arthroplasty for Osteoarthritis: a systematic review and Meta-analysis of Randomized controlled trials. Am J Phys Med Rehabil. 2017;96(6):440–7. [DOI] [PubMed] [Google Scholar]
- 24.Massip M, de Batlle J, Barbe F, Torres G, Vargiu E, Miralles F, et al. Implementing Mobile Health-Enabled Integrated Care for Complex Chronic patients: patients and professionals’ acceptability study. JMIR mHealth uHealth. 2020;8(11): e22136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Visperas AT, Greene KA, Krebs VE, Klika AK, Piuzzi NS, Higuera-Rueda CA. A web-based interactive patient-provider Software platform does not increase patient satisfaction or decrease hospital resource utilization in total knee and hip arthroplasty patients in a single large hospital system. J Arthroplasty. 2021;36(7):2290. [DOI] [PubMed] [Google Scholar]
- 26.Correia FD, Nogueira A, Magalhães I, Guimarães J, Moreira M, Barradas I, et al. Medium-term outcomes of digital versus conventional home-based rehabilitation after total knee arthroplasty: prospective, parallel-group feasibility study. JMIR Rehab Assist Technol. 2019;6(1):e13111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang X, Chen X, Kourkoumelis N, Gao R, Li G, Zhu C. A social media–promoted Educational Community of joint replacement patients using the WeChat App: Survey Study. JMIR mHealth uHealth. 2021;9(3): e18763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jennings HM, Morrison J, Akter K, Kuddus A, Ahmed N, Kumer Shaha S, et al. Developing a theory-driven contextually relevant mHealth intervention. Glob Health Action. 2019;12(1): 1550736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Voorheis P, Zhao A, Kuluski K, Pham Q, Scott T, Sztur P, et al. Integrating behavioral Science and Design thinking to develop Mobile Health interventions: systematic scoping review. JMIR Mhealth Uhealth. 2022;10(3): e35799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cole-Lewis H, Ezeanochie N, Turgiss J. Understanding Health Behavior Technology Engagement: pathway to Measuring Digital Behavior Change interventions. JMIR Form Res. 2019;3(4): e14052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to Promote Health Behavior Change: a systematic review and Meta-analysis of the impact of theoretical basis, Use of Behavior Change techniques, and Mode of Delivery on Efficacy. J Med Internet Res. 2010;12(1):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374:n2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1): 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mummah SA, Robinson TN, King AC, Gardner CD, Sutton SIDEAS, Integrate. Design, assess, and share): a Framework and Toolkit of Strategies for the development of more Effective Digital interventions to change Health Behavior. J Med Internet Res. 2016;18(12):e317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yardley L, Spring BJ, Riper H, Morrison LG, Crane DH, Curtis K, et al. Understanding and promoting effective Engagement with Digital Behavior Change interventions. Am J Prev Med. 2016;51(5):833–42. [DOI] [PubMed] [Google Scholar]
- 36.Devasenapathy N, Maddison R, Malhotra R, Zodepy S, Sharma S, Belavy DL. Preoperative quadriceps muscle strength and functional ability predict performance-based outcomes 6 months after total knee arthroplasty: a systematic review. Phys Ther. 2019;99(1):46–61. [DOI] [PubMed] [Google Scholar]
- 37.Devasenapathy N, Malhotra R, Mittal K, Garg B, Kumar V, Zodpey S, et al. Higher disability in Women Than Men Scheduled for Total Knee Arthroplasty for degenerative osteoarthritis: a cross-sectional analysis from India. ACR Open Rheumatol. 2020;2(6):309–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Devasenapathy N, Malhotra R, Garg B, Kumar V, Mittal K, Zodpey S, et al. Trajectories of recovery of disability outcomes after total knee arthroplasty for degenerative osteoarthritis a longitudinal cohort study from India. Osteoarthr Cartil. 2020;28:S380. [Google Scholar]
- 39.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. [DOI] [PubMed] [Google Scholar]
- 40.Doak CCDL, Root GH. Teaching patients with low literacy skills. Philadelphia: J.B. Lippincott Company; 1996. [Google Scholar]
- 41.Raghu A, Praveen D, Peiris D, Tarassenko L, Clifford G. Engineering a mobile health tool for resource-poor settings to assess and manage cardiovascular disease risk: SMARThealth study. BMC Med Inf Decis Mak. 2015;15:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Figma. The collaborative interface design tool. Available from: https://www.figma.com/. Cited 2023 12 July.
- 43.Torrente G, de Souza TQ, Tonaki L, Cardoso AP, Manickchand Junior L, da Silva GO. Scrum Framework and Health Solutions: management and results. Stud Health Technol Inf. 2021;284:290–4. [DOI] [PubMed] [Google Scholar]
- 44.Nielsen J. 10 usability heuristics for user interface design. Nielsen Norman Group. Available from: https://www.nngroup.com/articles/ten-usability-heuristics/.
- 45.Shneiderman B, Plaisant C, Cohen M, Jacobs S, Elmqvist N. Designing the user interface: strategies for effective human-computer interaction. USA: Pearson Education; 2016.
- 46.Stoyanov SR, Hides L, Kavanagh DJ, Wilson H. Development and validation of the user version of the Mobile Application Rating Scale (uMARS). JMIR Mhealth Uhealth. 2016;4(2):e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15(Suppl 1):S17-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saleh KJ, Mulhall KJ, Bershadsky B, Ghomrawi HM, White LE, Buyea CM, et al. Development and validation of a lower-extremity activity scale. Use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am. 2005;87(9):1985–94. [DOI] [PubMed] [Google Scholar]
- 50.Lyman S, Lee YY, Franklin PD, Li W, Cross MB, Padgett DE. Validation of the KOOS, JR: a short-form knee arthroplasty outcomes Survey. Clin Orthop Relat Res. 2016;474(6):1461–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kowatsch T, Otto L, Harperink S, Cotti A, Schlieter H. A design and evaluation framework for digital health interventions. it - Inform Technol. 2019;61(5–6):253–63. [Google Scholar]
- 52.Doiron-Cadrin P, Kairy D, Vendittoli PA, Lowry V, Poitras S, Desmeules F. Feasibility and preliminary effects of a tele-prehabilitation program and an in-person prehablitation program compared to usual care for total hip or knee arthroplasty candidates: a pilot randomized controlled trial. Disabil Rehabil. 2020;42(7):989–98. [DOI] [PubMed] [Google Scholar]
- 53.Gohir SA, Eek F, Kelly A, Abhishek A, Valdes AM. Effectiveness of internet-based exercises aimed at treating knee osteoarthritis: the iBEAT-OA Randomized Clinical Trial. JAMA Netw Open. 2021;4(2):e210012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Study data will be made available upon reasonable request to Niveditha Devasenapathy and after ethical approval.