Abstract
Background
The latest evidence on health literacy in China revealed that only 8% of individuals aged 65–69 years, a segment of the geriatric population, possess adequate health literacy levels, indicating a low level in China. Studies have demonstrated that improving the organizational health literacy of healthcare institutions is a crucial approach to addressing low health literacy among older patients.
Objective
To explore the obstacles hindering the advancement of organizational health literacy in healthcare institutions in meeting the needs of older patients.
Design
A mixed-methods approach was employed to investigate both the status and barriers to the establishment of organizational health literacy within two healthcare institutions.
Participants
Participants included older individuals aged over 60, clinical staff, and managerial personnel from these two health institutions.
Methods
This research utilized the social-ecological model as its theoretical foundation and utilized a mixed-methods approach to examine the current status and challenges in developing organizational health literacy within healthcare institutions. Initially, a survey using a questionnaire (n = 178) was conducted among older patients to evaluate the establishment of organizational health literacy from their perspective. Following this, interviews (n = 22) were carried out with administrators, clinical personnel, and elderly patients to identify the barriers hindering the development of organizational health literacy within healthcare institutions.
Results
Quantitative research indicates that health institutions have been less accommodating to the requirements of older patients, with health information dissemination and communication emerging as the weakest areas. Qualitative investigations revealed three key influencing factors: patient-related factors, including physiological and cognitive decline, as well as low educational attainment among older patients; organizational factors, including inadequate clinical staff numbers, deficient long-term systematic training, and a digital divide resulting from health institutions’ digital advancements; and policy-related factors indicating a lack of regulations governing the establishment of organizational health literacy within healthcare institutions.
Conclusion
The two most vulnerable aspects of OHL in medical institutions regarding the needs of older patients are health information and communication. The factors influencing the construction of OHL in medical institutions are multifaceted, encompassing micro, meso, and macro levels. At the macro level, it is essential for medical institutions to enhance leadership awareness of OHL and to incorporate its development into institutional strategic plans. At the meso-level, medical institutions should be made to optimize the medical environment for elderly patients and to prioritize health literacy training for medical staff. At the micro level, attention must be given to the characteristics and needs of elderly patients. Ultimately, by implementing a comprehensive construction of intervention strategies, the response ability of medical institutions to the needs of elderly patients can be enhanced.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-024-05530-z.
Keywords: A mixed-methods study, Older patients, Health institution, Healthy aging, Organizational health literacy, Social-ecological model
What is already known
Older people in China are generally in a state of low health literacy.
Building the organizational health literacy of health institutions can meet the needs of patients with low health literacy.
What this paper adds
Health institutions are less responsive to the needs of older patients in China, and health information and communication are the two weakest components.
The barriers to organizational health literacy in health institutions included patient-level, organization-level, and political-level barriers.
Introduction
Health literacy refers to individuals’ capacity to access, comprehend, and utilize fundamental health information and services to make informed healthcare choices [1, 2]. The findings from the 2020 national health literacy assessment revealed that only 8% of individuals aged 65–69 possess adequate health literacy, indicating a low level in China. A survey of the health literacy of older people in Sweden found that 49% of older people had inadequate health literacy [3]. The findings of a survey conducted in four American cities indicated that 34% of older adults demonstrated deficiencies in health literacy [4]. A lack of adequate health literacy is a prevalent issue among older individuals. Inadequate health literacy among the older people can result in increased hospitalization rates, increased medical expenses, ineffective communication, diminished healthcare service efficiency, and ultimately, adverse effects on older people health [5–8]. However, previous research has predominantly concentrated on enhancing health literacy among the older people from an individual standpoint [9, 10]. And few studies have explored how to meet the needs of older patients at the health institution level [11].
Organizational health literacy (OHL) is characterized as “the capability of health organizations to furnish services and information that are readily accessible, comprehensible, and usable by patients, aiding them in decision-making, and eliminating existing barriers” [12]. The World Health Organization Health Promotion Glossary of Terms 2021 delineates the role of organizations in promoting health and emphasizes that health literacy is influenced by cultural and situational demands imposed on individuals, organizations, and society. All information providers, including government entities, civil society, and health services, should enable access to reliable information that is both understandable and actionable for all individuals. [13]. Moreover, the Healthy People 2030 Initiative in the United States defines organizational health literacy, recognizes the responsibility of organizations to address health literacy issues, and highlights the critical role of health information and service providers in improving health literacy. It maintains that organizations can simplify health information and healthcare systems to accommodate patients with diverse health literacy levels and encourage patient participation in self-care [14]. OHL within healthcare institutions emphasizes the organizational role in enhancing patient navigation through healthcare systems. It is both consistent and vital for healthcare organizations to address the health literacy requirements of patients and enhance health information and services to render them more comprehensible and accessible [11]. Consequently, the establishment of OHL within healthcare institutions serves as a significant approach to enhance the capacity of health institutions to cater to the needs of patients, particularly older individuals with low health literacy. In recent years, research on OHL in health institutions has been valuable to researchers, but most of the related research has been conducted from the perspective of health institutions [15–22] and only a few studies have been conducted from the perspective of patients [23–25].
The social-ecological systems theory is a comprehensive framework that integrates system theory, sociology, and ecology, offering a theoretical foundation for studying human behavior and its relationship with the external environment. Since its introduction in 1979, the social-ecological systems theory has been extensively utilized across various domains, including child and adolescent development [26–28], social work practice [29, 30], and healthcare [31, 32].
This study examined the status of OHL in health institutions from the perspective of older patients. Additionally, qualitative interviews were conducted with administrators, clinical personnel, and older patients in healthcare institutions to identify the barriers to the development of organizational health literacy. It is anticipated that these findings will offer strategies for enhancing organizational health literacy in healthcare institutions and assist these institutions in addressing the challenges posed by an aging population.
The overall objective of this study was to explore the factors affecting the responsiveness of medical institutions to the needs of older patients. The specific objectives include: (1) to develop an OHL questionnaire grounded in social ecological theory to evaluate the responsiveness of medical institutions to the needs of older patients; and (2) to conduct in-depth interviews with managers of medical institutions, clinical staff, and older patients to identify the barriers to the development of OHL in these institutions.
Methods
Study design
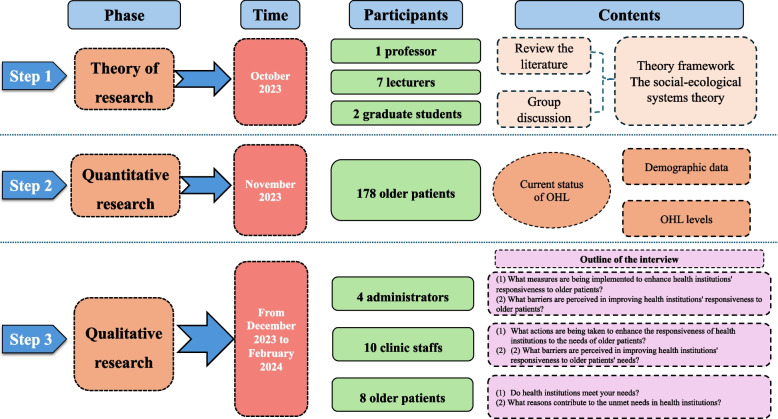
A mixed-method study design involving a combination of a quantitative study and qualitative interviews was used to explore the barriers to the development of OHL in health institutions. In mixed methods research, quantitative approaches are employed to test and validate hypotheses derived from an existing conceptual framework, thereby achieving a broad understanding of the predictors of successful implementation. Conversely, qualitative methods are utilized to delve deeper into understanding the factors contributing to the success or failure of implementing evidence-based practices, or to identify strategies for facilitating implementation [33]. In this study, a questionnaire (n = 178) was administered to older patients to assess the establishment of OHL within healthcare institutions from their perspective. Additionally, interviews were conducted with healthcare institution administrators, clinical staff, and older patients to elucidate the barriers hindering the construction of OHL within healthcare institutions. The flowchart depicting the study’s progression is presented in Fig. 1.
Fig. 1.
Flow chart of the study
Step 1 Theory framework
Charles [34] categorizes the factors influencing human development into three fundamental types: microsystem, mesosystem, and macrosystem. The microsystem pertains to the individual, including the physical, psychological, and social aspects, and places greater emphasis on the individual’s needs, challenges, and strengths. Mesosystems involve any groups, such as family or social groups, primarily assessing the influence of surrounding groups on an individual’s development. Macrosystem refers to the broader social system, comprising society, culture, physical environment, social norms, policies, and economic conditions. Charles Zastro emphasized that human behavior is influenced by interactions with the surrounding environment, where individuals and their environment continuously affect one another [35]. In accordance with the social-ecological model, enhancing the responsiveness of healthcare institutions to the needs of the older people involves not only addressing the needs of older patients but also taking into account the institutional environment. These factors typically impact older individuals’ access to medical resources.
Through literature review and expert discussions, this study identified the five dimensions of OHL within healthcare institutions based on the Ten Attributes of Health Literate Health Care Organizations [36]. The microsystem includes patient empowerment, the mesosystem includes navigation, communication, and health information, and the macrosystem incorporates regulations.
Step 2: Quantitative data collection and analysis
Participants
The participants consisted of older patients hospitalized in two tertiary health institutions located in Yangzhou City, Jiangsu Province, in November 2023, which included a 2,500-bed general health institution and an 1,800-bed teaching health institution. In this study, research participants were selected using a convenient sampling method, and data collection was conducted through the distribution of paper questionnaires. The participants included patients aged 60 years and older, as defined by the World Health Organization (WHO). Additionally, to ensure the inclusion of patients with experience in institutional care, only those with a hospital stay of three days or longer were selected. Furthermore, to enhance the reliability of the study, patients with mental disorders or disorders of consciousness were excluded.
Data collection
Data collection was carried out starting in November 2023, with paper questionnaires administered to older patients in two tertiary health institutions. Initially, trained researchers explained the purpose of the questionnaire to the older patients. After obtaining consent from the older patients for participation in the survey, they completed the questionnaire independently. For those unable to complete the questionnaire on their own, researchers provided assistance through face-to-face questions and answers. Older patients were requested to complete the questionnaire within 20 min. The completed questionnaires were collected on-site, and two members of the research team entered and checked the data to identify any missing items and to discard incorrectly completed questionnaires. The study aimed to analyze 17 influencing factors, considering a potential 20% of invalid responses and the recommendation of, including 5–10 times the number of independent variables in regression analysis. Thus, the targeted sample size ranged from 102 to 204 cases. Out of 190 distributed questionnaires, 178 valid responses were collected, resulting in an effective sample recovery rate of 94%.
Instruments
Demographic data such as age and sex were retrieved from resident medical records by trained researchers.
Currently, there is an absence of a comprehensive assessment tool for the OHL of health institutions from the perspective of older patients, specifically tailored to China's national conditions. To address this gap in the literature, the research team developed a new scale.
The evaluation of OHL within healthcare institutions from the perspective of older patients utilized a 22-item scale developed by the research team. This scale covered five dimensions: patient empowerment (3 items), medical navigation system (6 items), health information (4 items), communication (5 items), and regulation (4 items). The scale employs a 5-point Likert scale, with response options ranging from 1 (strongly disagree) to 5 (strongly agree). The total score for the questionnaire spans from 22 to 110, where higher scores reflect a greater responsiveness of healthcare institutions to the needs of older patients. Two rounds of expert consultation have been conducted, yielding expert authority coefficients of 0.892 and 0.904. Variation coefficients ranged from 0.07 to 0.58 and from 0.07 to 0.25, respectively, while Kendall's concordance coefficients were determined to be 0.165 and 0.215 (all P < 0.001). The reliability and validity of the scale were assessed in two health institutions in China, revealing that the item-level content validity index (I-CVI) ranged between 0.833 and 1.000, whereas the scale-level content validity index (S-CVI/Ave) averaged 0.954. Cronbach's alpha coefficient for the overall scale was found to be 0.937, and the folding coefficient was measured at 0.853. This scale represents a scientifically robust and reliable tool for evaluating organizational health literacy in health institutions, specifically from the perspective of older patients in China. Consequently, this scale was selected for the current study to evaluate the responsiveness of health institutions to the requirements of older patients. In this study, Cronbach’s alpha was calculated as 0.925.
Data analysis
Quantitative data were analyzed using IBM SPSS 26 (IBM Corporation, Somers, NY). Descriptive statistics were used to analyze demographic and questionnaire data. Independent sample t-tests or analysis of variance were utilized to compare the scores of older patients with varying characteristics regarding OHL in health institutions.
Step 3 Qualitative data collection and analysis
Participants
From December 2023 to February 2024, purpose sampling and snowball sampling were used to recruit health institution administrators, clinical staff and older inpatients from the two tertiary health institutions. To gain a deeper understanding of the development of OHL in health institutions, a sample was selected consisting of 4 administrators with over 20 years of management experience, 12 clinical staff possessing clinical experience, and 8 older patients who participated in quantitative research and consented to further participate in qualitative research. The qualitative interviews were conducted by an interview team, which included three members, one of whom was a professor who has been involved in health literacy research for 20 years and has a deep understanding of OHL and extensive experience in qualitative research; the other two were graduate students with a health literacy orientation and experience in qualitative research.
Data collection
Trained researchers conducted comprehensive face-to-face interviews with participants. The sample size for the study was determined based on the principle of data saturation, whereby sampling ceased when no novel topics emerged during data analysis. Individual face-to-face interviews were conducted in a secluded area within the lounge of the healthcare institution’s ward, ensuring a quiet, comfortable, and uninterrupted interview environment.
The interview content was crafted by the research team through deliberations grounded in the Ten Attributes of Health Literate Healthcare Organizations. The interview outline for different research participants was developed by the research group. For older patients, the interview questions included: (1) Do health institutions meet your needs? (2) What reasons contribute to the unmet needs in health institutions? For clinical staff, the interview questions were: (1) What actions are being taken to enhance the responsiveness of health institutions to the needs of older patients? (2) What barriers are perceived in improving health institutions' responsiveness to older patients' needs? The interview outline for healthcare managers comprised: (1) What measures are being implemented to enhance health institutions' responsiveness to older patients? (2) What barriers are perceived in improving health institutions' responsiveness to older patients? Additionally, the questionnaire was designed to evaluate the current responsiveness of medical institutions to older patients' needs, and the content of the interview outline was organized to identify the impediments influencing the responsiveness of health institutions from the viewpoints of health institution administrators, clinical staff, and older patients.
Before the interviews, the purpose of the qualitative study was explained in detail to the participants by the researchers. Following the acquisition of participant consent, key information was recorded, and audio recordings were made. To ensure participant privacy during the study, codes were used instead of using participant names, with "P" denoting older patients, "C" representing clinical staff, and "A" indicating health institution administrators.
Following the interview outline, researchers gathered data via in-depth interviews with participants, adjusting the interview sequence and content as per the specific circumstances encountered during the interviews. To ensure the accuracy and completeness of the interview data, both recordings and notes were utilized to capture non-verbal cues such as expressions, eye contact, and body language of the respondents. Each interview lasted approximately 20–40 min.
The researchers conducted interviews at two tertiary health institutions with the permission of the institutions and the consent of the participants. The interview data were accessible exclusively to the researchers and the participants.
Data analysis
Phenomenological research, a qualitative approach extensively utilized across various disciplines such as medicine, psychology, nursing, education, and other humanities and social sciences [37], serves as a valuable tool in nursing. Particularly in nursing, phenomenological research methods are predominantly employed to investigate subjective cognitive aspects, life experiences, values, and worldviews related to health and illness [38]. Descriptive phenomenology, a subtype of phenomenological research, underscores the direct apprehension of phenomena and the pursuit of understanding devoid of preconceived notions or biases [39]. In this study, descriptive phenomenology was utilized to explore the barriers hindering healthcare institutions’ ability to meet the needs of older patients.
The interviews were promptly transcribed by two researchers within 24 h of completion, with a third researcher reviewing the transcripts for accuracy. Any uncertainties were resolved through discussion among the investigators. To ensure linguistic precision, one researcher proficient in both Chinese and English translated the interviews into English, which were then back-translated into Chinese by another researcher. Using Colizzi’s seven-step method [40], two researchers independently analyzed the transcribed text. The steps followed included: (1) Thoroughly reading the original text multiple times. (2) Identifying and extracting meaningful statements related to healthcare institutions’ ability to address the needs of older patients. (3) Summarizing and coding recurrent barriers hindering healthcare institutions’ ability to meet the needs of older patients. (4) Grouping similar concepts into corresponding thematic rudiments. (5) Describing fundamental themes of hindering barriers to healthcare institutions’ ability to respond to the needs of older patients, linking them to representative interview statements and providing detailed descriptions. (6) Comparing similar theme rudiments, seeking correlations between each, and constructing themes with rich meaning. (7) Presenting the final generated themes to the study participants for verification to ensure the authenticity and accuracy of the results.
Ethics
The study was conducted with ethical approval from the Yangzhou University Medical Ethics Committee and in accordance with relevant guidelines and regulations (YXYLL-2023–038). All participants were aware of the study purpose, risks and benefits and informed consent to participate in this study. The research data were accessible solely to the researchers and the participants.
Results
Quantitative research
Participant characteristics
A total of 178 older inpatients were recruited for the study. The score of older patients' evaluation of OHL in medical institutions was (67.989 ± 17.491). The results from the quantitative analysis indicated that there were statistically significant differences regarding education level, sources of income, monthly household income, types of medical expenses, and place of residence (P < 0.05) (Table 1).
Table 1.
Sociodemographic data of the study population (n = 178)
| Participant characteristics | N = 178 n (%) | OHL (M ± SD) | t/F | p | |
|---|---|---|---|---|---|
| Health institutions | general health institutions | 57 (32%) | 64.877 ± 21.937 | 1.637a | 0.103 |
| teaching health institutions | 121 (68%) | 69.455 ± 14.830 | |||
| Gender | male | 103 (58%) | 67.515 ± 16.281 | 0.423a | 0.673 |
| female | 75 (42%) | 68.640 ± 19.122 | |||
| Age | 60 ~ 74 | 116 (65%) | 69.353 ± 17.167 | 2.691b | 0.071 |
| 75 ~ 89 | 59 (33%) | 66.339 ± 16.895 | |||
| ≥ 90 | 3 (2%) | 47.667 ± 32.332 | |||
| Level of education | Primary school and below | 87 (49%) | 64.862 ± 18.846 | 2.696b | 0.033 |
| Junior high school | 43 (24%) | 68.837 ± 16.059 | |||
| Senior high school | 33 (19%) | 69.697 ± 15.084 | |||
| Junior college | 9 (5%) | 81.556 ± 16.349 | |||
| Bachelor and above | 6 (3%) | 77.500 ± 5.958 | |||
| Occupations | Incumbency | 12 (7%) | 74.333 ± 15.156 | 1.304a | 0.194 |
| Retirement | 166 (93%) | 67.530 ± 17.599 | |||
| Marital status | Unmarried | 1 (1%) | 66.000 ± | 0.301b | 0.825 |
| Married | 162 (91%) | 68.327 ± 17.594 | |||
| Divorced | 2 (1%) | 70.000 ± 4.243 | |||
| Widowed spouse | 13 (7%) | 63.615 ± 18.301 | |||
| Economic source | No regular income | 44 (25%) | 58.750 ± 17.516 | 6.962b | < 0.001 |
| Social insurance | 11 (6%) | 78.909 ± 13.678 | |||
| Child support | 29 (16%) | 68.966 ± 22.669 | |||
| Retirement salary | 94 (53%) | 70.734 ± 14.254 | |||
| Monthly household income | < 3000 CNY | 88 (49%) | 62.364 ± 16.389 | 6.942b | < 0.001 |
| 3000–5000 CNY | 42 (24%) | 74.905 ± 15.783 | |||
| 5000–7000 CNY | 20 (11%) | 70.350 ± 19.701 | |||
| ≥ 7000 CNY | 28 (16%) | 73.607 ± 16.563 | |||
| Types of medical expenses | Employee health insurance | 77 (43%) | 70.390 ± 16.978 | 3.316b | 0.021 |
| Medical insurance for Urban residents | 15 (8%) | 74.800 ± 14.264 | |||
| Self-pay medical treatment | 6 (3%) | 76.000 ± 20.562 | |||
| New Rural Cooperative Medical System | 80 (45%) | 63.800 ± 17.557 | |||
| Place of residence | Rural | 90 (51%) | 63.533 ± 16.523 | 6.298b | 0.002 |
| Town | 23 (13%) | 71.696 ± 19.921 | |||
| Urban | 65 (37%) | 72.846 ± 16.530 | |||
| Caregiver | Care Worker | 17 (10%) | 62.235 ± 18.757 | 1.317b | 0.266 |
| Spouse | 60 (34%) | 69.433 ± 14.507 | |||
| Relatives and friends | 9 (5%) | 59.889 ± 13.896 | |||
| Children | 77 (43%) | 68.182 ± 19.244 | |||
| None | 15 (8%) | 72.600 ± 18.546 | |||
| Length of stay | 3-7d | 118 (66%) | 70.237 ± 16.577 | 3.035b | 0.051 |
| 8-14d | 40 (22%) | 62.950 ± 17.831 | |||
| ≥ 15d | 20 (11%) | 64.800 ± 20.245 |
at test
banalysis of variance
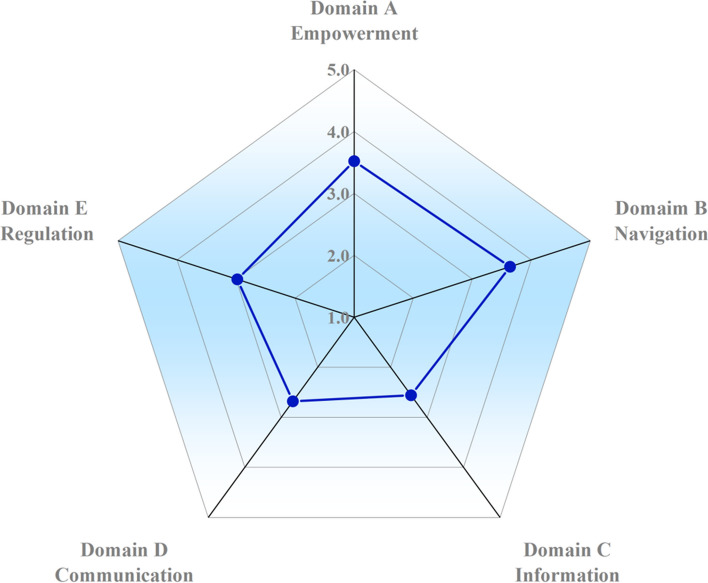
Assessment of scalability
The questionnaire contained five dimensions, among which dimension A (Empowerment) measured the empowerment of medical institutions to patients, reflecting the level of patients; Dimension B (Navigation), dimension C (Information) and dimension D (Communication) measure the physical and humanistic environment of medical institutions, reflecting the level of the organization. Dimension E (Regulation) measures patients' perception of medical policies, reflecting the level of the policy. We used Origin 2021 software to draw the radar plot. The radar plot depicted in Fig. 2 illustrates the findings of the OHL assessment derived from responses received in the questionnaire administered to older patients. Points positioned on the outer part of the radar plot below signify domains that garnered higher scores, indicating they were viewed more favorably, while points closer to the center indicate weaker areas or areas necessitating further attention. The radar plot results reflect the responsiveness of healthcare institutions to the needs of older patients. Health information and communication emerged as the two weakest components based on the assessment.
Fig. 2.
Results of the radar plot
Qualitative research
Following the principles of “adequacy” and “saturation” in qualitative research, a total of 22 interviewees were ultimately included in the study. This comprised 8 older patients, 10 medical staff members, and 4 administrators members. A total of eight older patients participated in the interview. Among these participants, six were aged between 60 and 75 years, while two were between 75 and 90 years. The group comprised four males and four females. Educational backgrounds included two individuals with primary school education, three with junior high school education, and three with senior high school education. All eight patients were married; two reported a monthly household income ranging from 3,000 to 5,000 yuan, four indicated an income between 5,000 and 7,000 yuan, and two reported an income exceeding 7,000 yuan. Regarding health insurance, four had Employee health insurance, one had Medical insurance for Urban residents, and three were part of the New Rural Cooperative Medical System. Four participants lived in urban areas, while four resided in rural regions. Caregiving arrangements included three individuals cared for by their spouses, three by their children, one by friends, and one by a caregiver. Hospitalization duration varied, with three patients hospitalized for less than seven days and five for more than seven days. The interviewed clinical staff consisted of five doctors and five nurses, all of whom had over five years of experience in health institutions, contributing to their substantial clinical expertise. Additionally, four administrative staff members participated in the interview, each with over 20 years of experience, serving as senior administrators in health institutions. Further details regarding the participants can be found in Supplementary Material 1–3.
Interview findings
Patient factors
(1) Physiological function declines in older patients: with increasing age, the vision and hearing of older people gradually decline, which increases the difficulty of accessing medical resources.
P7: My eyesight is not good, especially after COVID-19, and my eyes become tired easily, so I do not want to see the health information that doctors and nurses provide me.
C2: Educating older patients through written materials poses challenges due to age-related visual impairments, making it difficult for many to read clearly.
C6: In communicating with older patients with significant hearing impairment, it is necessary to adjust our pace, elevate our voice, and integrate physical gestures to facilitate effective communication.
(2) Cognitive decline in older patients hampers their capacity to assimilate new information and adapt to emerging technologies.
C1: Older patients may be slower to comprehend and retain instructions, often requiring repeated reminders, particularly when explaining medication administration procedures.
C8: Health education efforts employing WeChat public accounts or videos are hindered for many older patients who do not utilize mobile phones; thus, impeding their access to crucial health information.
(3) Older patients with a low education level encounter difficulties in navigation, communication and access to health information in medical institutions.
P1: I am illiterate. If I need to go out of the ward, my child helps me; I cannot find the place by myself.
C3: Some older patients in Yangzhou can only speak and understand dialects. When our doctors and nurses are not local to Yangzhou, it is difficult to communicate with them.
C7: Some older patients are illiterate. You can only tell them some health knowledge through pictures.
Organizational factors
(1) Inadequate clinical staff: Inadequate clinical staff and their additional non-medical responsibilities result in higher workloads and reduced time for medical staff to interact with older patients.
P1: I rarely see my doctors in the ward. I hope to communicate with them about my health, but they are too busy.
C4: We have so few doctors that it is not easy to perform daily medical work.
A1: There is a shortage of doctors and nurses, leading to a high workload. Aside from clinical duties, they are also required to produce popular science videos.
(2) Systematic training in health literacy for clinical staff is lacking in medical institutions. Greater emphasis is placed on medical and nursing tasks by clinical staff, with insufficient attention given to communication and health education for older patients.
C10: Challenges arise in our workplace. For instance, there was an occasion when communication difficulties with an older patient resulted in conflict. We intend to arrange for nurses to analyze the underlying causes and develop strategies to address such situations. There is a lack of systematic training, and typically, we gather everyone to learn collectively when confronted with challenges.
C5: During pre-employment training for new staff, various sessions will cover topics such as communication and health education. However, once employed, doctors tend to prioritize treatment, resulting in less focus on learning in these areas. Occasionally, health institutions may address these topics in meetings, but there is a lack of systematic training.
P3: It took me a considerable amount of time to wait in line for registration. I was unaware of the existence of a dedicated registration window for the older, as no one informed me about it.
(3) The digitalization of healthcare institutions exacerbates the digital divide. While the initial goal of digitalization is to enhance convenience for patients in accessing medical services, the intricate system and the older people’ difficulties with electronic devices render them a vulnerable group in accessing medical resources.
P5: The registration and payment machines in healthcare institutions are overly complex for us. I am accustomed to queuing in person for doctor appointments.
P8: The development of health institutions is too fast. Now they all make appointments online. Health institutions are developing according to the ideas of young people without considering old people.
C9: Older people are vulnerable to digital development. Many older people are unable to master the functions of OMC only offline, which requires considerable time.
A2: The digital development of health institutions is rapid. To help patients, health institutions have opened many online medical treatment functions, but many older people do not even have smartphones, which makes it inconvenient for them. This is indeed a paradox.
Policy factors
Lack of plans to integrate OHL in health institutions During the interviews, all the interviewees pointed out that there is no policy document to guide the building of OHL in health institutions.
C6: I have not seen regulation in the staff system about building OHL in health institutions.
A2: Health institutions have established regulations, such as communication, navigation within health institutions, and health information, but there are no systematic normative norms for the construction of health literacy in health institutions.
Discussion
This study initially assessed the capability of healthcare institutions to address the requirements of older patients through quantitative analysis. Subsequently, interviews were conducted with managers, clinical staff, and older patients to investigate the obstacles hindering the development of OHL within healthcare institutions. The study revealed a weak response from healthcare institutions to the needs of older patients, with influencing factors spanning patient-level, organization-level, and political-level domains.
Quantitative investigations have indicated the inadequate ability of healthcare institutions to meet the needs of older patients. On one hand, the generally low health literacy levels among the older people in China hinder their access to and utilization of health information, negatively affecting their health outcomes [41, 42]. Additionally, older individuals often experience multiple chronic conditions, increasing their reliance on healthcare institutions [43, 44]. Qualitative inquiries have also identified physiological declines among older patients, such as vision or hearing loss, impairing their ability to access health information and effectively communicate with clinical staff, thereby complicating their access to healthcare resources. Furthermore, cognitive decline in older adults often necessitates repeated education by clinical staff and volunteers due to frequent forgetfulness. Low levels of education contribute significantly to the low health literacy rates among the older people. Those with lower educational attainment tend to be slower in adopting new concepts, possess limited self-awareness, lack awareness of disease prevention strategies, and encounter challenges in acquiring scientific health knowledge and skills, resulting in diminished health literacy [43, 44]. Overall, there is a considerable demand among the older people for healthcare institutions.
On the other hand, the ability of healthcare institutions to address the needs of older patients remains inadequate. Qualitative research indicates that barriers to the establishment of OHL within healthcare institutions also involve organizational and policy-level factors.
From an organizational standpoint, healthcare facilities have not adequately addressed the digital disparity among older patients during the digitalization process. According to the statistical report on China’s internet development status released by the China Internet Information Center in [45], out of 253.88 million individuals aged 60 years and older people in China, only 60.56 million people (24%) had internet access in 2019. Older individuals face challenges in effectively utilizing online health information platforms and telemedicine services, resulting in significant inconvenience in accessing daily health consultations and purchasing medications [46–48]. Consequently, it is imperative for healthcare institutions to simplify electronic systems to facilitate older individuals’ access to health information.
The shortage of medical personnel also significantly influences the development of OHL within healthcare institutions. During interviews, clinical staff expressed difficulties in dedicating time to communicate with older patients and provide health information resources due to the scarcity of medical staff. This finding aligns with previous research indicating that clinical staff often lack sufficient time for health literacy endeavors, especially in communication, owing to staffing shortages [49, 51,50]. Furthermore, the absence of health literacy training for medical personnel in healthcare institutions is recognized as an influencing factor. Several studies on health literacy consistently highlight that healthcare workers generally lack the necessary knowledge and skills to effectively communicate with patients with low health literacy [52]. Hence, healthcare providers should offer training in health literacy, including navigation, health information, and communication, to cater to the needs of older patients.
At the policy level, the researchers examined interview transcripts with administrators and clinical staff in healthcare institutions and discovered a lack of regulations regarding the establishment of OHL within these institutions. This absence of regulation may stem from OHL being a relatively new concept in China, with Chinese scholars only beginning to explore it and not yet conducting empirical research. Consequently, healthcare institutions do not prioritize the development of OHL adequately. A study on barriers to establishing OHL in the German public health sector identified the absence of policy pressure as one of the impediments to OHL establishment in healthcare institutions [17]. The absence of OHL policies and plans in healthcare institutions means that OHL is often excluded from the organization’s mission, vision, and strategic planning; thus, hindering its development. While some health literacy practices may be implemented by frontline staff, most are unfamiliar with the concept of health literacy [53–55]. However, implementing specific regulations outlined in health literacy guides could enhance navigation and patients’ comprehension and utilization of health information in specific settings [56, 57]. Therefore, it is crucial to formulate policies or regulations that integrate OHL into healthcare institution construction planning, enhance healthcare personnel’s awareness of OHL, and foster the establishment of OHL within healthcare institutions.
Thus, medical institutions must take a comprehensive approach when considering various elements involved in the development of OHL. First, it is necessary for medical institutions to elevate the importance of OHL within their leadership, integrate OHL development into their institutional strategic plans, and actively facilitate its construction.
Second, organizational factors should be carefully addressed by medical institutions. Efforts should be made to improve the environment for older patients, including the establishment of designated service windows, simplification of self-service systems, installation of navigational voice systems within hospitals, and the creation of barrier-free access and other convenience facilities. These measures aim to reduce the challenges posed by the digital divide and ensure that older patients' treatment requirements are adequately met. Medical staff allocation should be optimized to provide sufficient time for communication between staff and older patients. In addition, it is essential for medical institutions to focus on enhancing the health literacy training of medical personnel. Systematic training programs and evaluation metrics, such as communication skills development, could be established to improve the ability of medical staff to identify patients with low health literacy and better respond to the needs of older patients.
Medical institutions should also focus on training professionals to support older patients throughout the medical treatment process. This may include developing specialized medical guidance teams to assist older patients with tasks such as pre-examination and triage, registration, payment, and drug collection. Additionally, nursing staff in medical institutions should be trained to provide assistance during hospital examinations for older patients. Furthermore, volunteer teams should be integrated into the management systems of medical institutions to enhance the quality of volunteer services and aid older patients in overcoming challenges encountered during the medical treatment process.
Third, the specific needs of older patients should be carefully considered. Medical institutions can facilitate the acquisition of health information by simplifying the content and increasing the accessibility of health information. For instance, health information can be conveyed using clear and simple language, a combination of images and text to improve comprehension, larger text fonts, and the use of videos to disseminate health knowledge.
Limitations
Firstly, this study solely surveyed older patients in two tertiary health institutions in Yangzhou City, Jiangsu Province, China, potentially limiting the generalizability of the findings due to regional and cultural influences. Future research could broaden the scope by including health institutions from other regions in China to enhance sample representativeness. Secondly, the research team developed the instrument utilized for quantitative research in this study. However, the scale underwent two rounds of expert consultation, enhancing its credibility and reliability. Consequently, the scale can serve as a robust tool for older patients to assess the OHL of healthcare institutions. Thirdly, the quantitative study employs convenience sampling, potentially introducing bias into the research findings because of the significant role of random factors. It is recommended that future research adopt a more stringent sampling technique. Fourthly, the impact of the duration of hospital stays on the research outcomes was not addressed in the quantitative study. Future investigations might explore how varying lengths of hospital stays influence OHL assessments. Lastly, the current study overlooked the association between individual health literacy and OHL among older patients. Subsequent research should consider examining the connection between HL and OHL in medical institutions.
Conclusion
Health information and communication represent two significant weaknesses in medical institutions regarding the fulfillment of the OHL needs of older patients. These aspects should be considered by medical institutions when enhancing the OHL process. The factors influencing the establishment of OHL within medical institutions are multifaceted: patient-related factors, including physiological and cognitive decline, as well as low educational attainment among older patients; organizational factors, including inadequate clinical staff numbers, deficient long-term systematic training, and a digital divide resulting from health institutions’ digital advancements; and policy-related factors indicating a lack of regulations governing the establishment of organizational health literacy within healthcare institutions. At the macro level, OHL development can be integrated into the strategic plan of medical institutions by elevating the leadership's focus on OHL. At the meso level, the medical environment can be optimized for older patients, and emphasis should be placed on the health literacy training of medical personnel. At the micro level, attention should be directed toward the unique characteristics and requirements of older patients. Ultimately, comprehensive intervention strategies can be formulated to enhance the responsiveness of medical institutions to the needs of older patients.
Supplementary Information
Acknowledgements
The authors are grateful to all patients, clinical staff, and administrators who participated in the study.
Author’ contribution
Yongbing Liu and Angela Y. M. Leung design the study and supervise the conduct of the study. Yijing Li, Yanru Kang, Runjie Sun and Xinqi Xu collect the quantitative data. Jie Zhu, Haiyan Fu, Yining Zhang and Jingwen Lin collect the qualitative data. Jie Zhu, Haiyan Fu, Yining Zhang, Jingwen Lin Yijing Li, Yanru Kang, Runjie Sun, Xinqi Xu, Ping Hou, Pei Duan, Jiayuan Tu, Jin Xue, Xine Mao and Jingwen Qin have a group discussion. Jie Zhu wrote the main manuscript text. All authors reviewed the manuscript.
Funding
This work was supported by the Yangzhou Municipal Science and Technology Bureau (Grant Number YZ2023071), the Jiangsu Graduate Research and Innovation Program (Grant Number KYCX23_3631), Opening Project of Suzhong Development Research Institute in 2022 ( Grant Number Szfz202219) and The National Social Science Foundation of China 2024 (Grant Number 24BRK008).
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Declarations
Conflict of interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gustafsdottir SS, Mårtensson L, Sigurdardottir AK, et al. When great responsibility comes with limited options: experiences and needs of older community-dwelling adults regarding accessing, understanding, appraising and using health-related information. BMC Geriatr. 2024;24:640. 10.1186/s12877-024-05236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu C, Wang D, Liu C, et al. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam Med. Community Health. 2020;8:e000351. 10.1136/fmch-2020-000351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wångdahl J, Agerholm J, Liljas A, et al. Health literacy among older adults 77+ in Sweden. Eur J Public Health. 2022;32. 10.1093/eurpub/ckac131.331.
- 4.Gazmararian JA, Baker DW, Williams MV, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545–51. [DOI] [PubMed] [Google Scholar]
- 5.Pien L-C, Cheng W-J, Chang W-P, et al. Relationships between stroke prevalence, health literacy, and oral health-related quality of life in middle-aged and older adults: a national survey study. BMC Geriatr. 2023;23:233. 10.1186/s12877-023-03927-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ong-Artborirak P, Seangpraw K, Boonyathee S, et al. Health literacy, self-efficacy, self-care behaviors, and glycemic control among older adults with type 2 diabetes mellitus: a cross-sectional study in Thai communities. BMC Geriatr. 2023;23:297. 10.1186/s12877-023-04010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu S, Zhao H, Fu J, et al. Current status and influencing factors of digital health literacy among community-dwelling older adults in Southwest China: a cross-sectional study. BMC Public Health. 2022;22:996. 10.1186/s12889-022-13378-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slatyer S, Toye C, Burton E, et al. Measurement properties of self-report instruments to assess health literacy in older adults: a systematic review. Disabil Rehabil. 2022;44:2241–57. 10.1080/09638288.2020.1836044. [DOI] [PubMed] [Google Scholar]
- 9.Xie Y, An W, Zheng C, et al. Multidimensional health literacy profiles and health-related behaviors in the elderly: a cross-sectional survey. Int J Nurs Sci. 2022;9:203–10. 10.1016/j.ijnss.2022.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou X, Yi J, Bai L, et al. Toward a Medication Information Literacy Indicator System for Older Adults: a delphi Study. Health Expect. 2024;27: e14127. 10.1111/hex.14127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bremer D, Klockmann I, Jaß L, et al. Which criteria characterize a health literate health care organization? - a scoping review on organizational health literacy. BMC Health Serv Res. 2021;21:664. 10.1186/s12913-021-06604-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayran O, Özer O. Organizational health literacy as a determinant of patient satisfaction. Public Health. 2018;163:20–6. 10.1016/j.puhe.2018.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Don N and Muscat DM. Health Promotion Glossary 2021. Health Promotion International 2021: 6.
- 14.Pronk NP, Kleinman DV, Richmond TS. Healthy People 2030: Moving toward equitable health and well-being in the United States. EClinicalMedicine. 2021;33: 100777. 10.1016/j.eclinm.2021.100777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang M-C, Wang Y-W, Yu J-H, et al. Evaluating health literacy from an organizational perspective: a cross-sectional study of community health centers. Public Health Nurs. 2024;41:1114–23. 10.1111/phn.13357. [DOI] [PubMed] [Google Scholar]
- 16.Charoghchian Khorasani E, Tavakoly Sany SB, Mahdizadeh M, et al. Attributes of organizational health literacy in health care centers in Iran: A Qualitative Content Analysis Study. Int J Environ Res Public Health. 2022;19:2310. 10.3390/ijerph19042310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehlis A, Locher V, Hornberg C. Barriers to organizational health literacy at public health departments in Germany. Health Lit Res Pract. 2021;5:e264–71. 10.3928/24748307-20210809-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kružliaková N, Porter K, Ray PA, et al. Understanding and advancing organizational health literacy within a public health setting. Health Lit Res Pract. 2021;5:e35–48. 10.3928/24748307-20210114-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenfeld L, Miller A, Garverich S, et al. Performing an organizational health literacy assessment in a shelter serving people with mental illness. Health Lit Res Pract. 2022;6:e167–74. 10.3928/24748307-20220615-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charoghchian Khorasani E, Tavakoly Sany SB, Tehrani H, et al. Review of organizational health literacy practice at health care centers: outcomes, barriers and facilitators. Int J Environ Res Public Health. 2020;17:7544. 10.3390/ijerph17207544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Ballegooie C, Heroux D, Hoang P, et al. Assessing the functional accessibility, actionability, and quality of patient education materials from canadian cancer agencies. Curr Oncol. 2023;30:1439–49. 10.3390/curroncol30020110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baumeister A, Chakraverty D, Aldin A, et al. “The system has to be health literate, too” - perspectives among healthcare professionals on health literacy in transcultural treatment settings. BMC Health Serv Res. 2021;21:716. 10.1186/s12913-021-06614-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dietscher C, Lorenc, J., & Pelikan, J. M. Piloting of the “self-assessment tool to investigate the organizational health literacy of hospitals” following the Vienna Concept of a Health Literate Health Care Organization. 2015.
- 24.Altin SV, Lorrek K, Stock S. Development and validation of a brief screener to measure the Health Literacy Responsiveness of Primary Care Practices (HLPC). BMC Fam Pract. 2015;16:122. 10.1186/s12875-015-0336-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ernstmann N, Halbach S, Kowalski C, et al. Measuring attributes of health literate health care organizations from the patients’ perspective: development and validation of a questionnaire to assess health literacy-sensitive communication (HL-COM). Z Evid Fortbild Qual Gesundhwes. 2017;121:58–63. 10.1016/j.zefq.2016.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Chen X, Allen JL, Hesketh T. The influence of individual, peer, and family factors on the educational aspirations of adolescents in rural China. Soc Psychol Educ. 2023. 10.1007/s11218-023-09765-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Masek E, Gonzalvez A, Rankin L, et al. Qualitative research on the perceptions of factors influencing diet and eating behaviors among primarily latinx seventh-grade students. J Acad Nutr Diet. 2023;123:1011–21. 10.1016/j.jand.2023.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vaezghasemi M, Vogt T, Lindkvist M, et al. Multifaceted determinants of social-emotional problems in preschool children in Sweden: An ecological systems theory approach. SSM Popul Health. 2023;21: 101345. 10.1016/j.ssmph.2023.101345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheerin KM, Brodell R, Huey SJ, et al. Applying ecological systems theory to juvenile legal system interventions outcomes research: a measurement framework. Front Psychol. 2023;14:1177568. 10.3389/fpsyg.2023.1177568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roux DJ, Taplin M, Smit IPJ, et al. Co-Producing narratives and indicators as catalysts for adaptive governance of a common-pool resource within a protected area. Environ Manage. 2023;72:1111–27. 10.1007/s00267-023-01884-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ismail R, Voss JG, Yona S, et al. Classifying stigma experience of women living with HIV in Indonesia through the social ecological model. Health Care Women Int. 2022;43:345–66. 10.1080/07399332.2021.1929989. [DOI] [PubMed] [Google Scholar]
- 32.Liao Y, Cheng X, Li Z, et al. The mediating role of physical activity and health status between a health-supportive environment and well-being: a cross-sectional study. Front Public Health. 2023;11: 1233970. 10.3389/fpubh.2023.1233970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Palinkas LA, Aarons GA, Horwitz S, et al. Mixed method designs in implementation research. Adm Policy Ment Health. 2011;38:44–53. 10.1007/s10488-010-0314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zastro A, Shi Hai-ling. Human Behavior and Social Environment (6th Ed) . 2006.
- 35.Kirst-ashman KK, Zastrow, C.H. Understanding Human Behavior and the Social Environment. 2000.
- 36.Brach C, Keller, D., Hernandez, L. M., Baur, C., Dreyer, B., Schyve, P., & Lemerise, A. J. Ten attributes of health literate health care organizations. In: Academies IoMotN, (ed.). Washington, DC2012.
- 37.Guangfang H. From description to explanation: the shift of phenomenological research path. Social Scientist. 2017;10:52–6. [Google Scholar]
- 38.Shibin L. Education Research from the perspective of phenomenology. J Guizhou Normal University (Social Science Edition). 2010;02:111–4. [Google Scholar]
- 39.Guangfang H. The bloom of Liberation: the soul of phenomenological Philosophy. Soc Sci. 2013;05:9–12. [Google Scholar]
- 40.Wirihana L, Welch A, Williamson M, et al. Using Colaizzi’s method of data analysis to explore the experiences of nurse academics teaching on satellite campuses. Nurse Res. 2018;25:30–4. 10.7748/nr.2018.e1516. [DOI] [PubMed] [Google Scholar]
- 41.Huang Y, Qi F, Wang R, et al. The effect of health literacy on health status among residents in Qingdao, China: a path analysis. Environ Health Prev Med. 2021;26:78. 10.1186/s12199-021-01001-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:155. 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 43.Dang J WL. China Report of the Development on Ageing Industry (2021–2022). Beijing: Social Sciences Academic Press; 2023.
- 44.Tao S, Sun S, Wu S, et al. Current status and influencing factors of health literacy among older adults in combined medical and nursing care institutions: a cross-sectional study. Front Public Health. 2023;11: 1323335. 10.3389/fpubh.2023.1323335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.The 43rd statistical report on internet development in China (in Chinese). Journal of the National Library. 2019;28:1
- 46.von Humboldt S, Low G, Leal I. Health Service Accessibility, Mental Health, and Changes in Behavior during the COVID-19 Pandemic: A Qualitative Study of Older Adults. Int J Environ Res Public Health 2022;19. 10.3390/ijerph19074277 . [DOI] [PMC free article] [PubMed]
- 47.Delgado CE, Silva EA, Castro EABd, et al. COVID-19 infodemic and adult and elderly mental health: a scoping review. Rev Esc Enferm USP. 2021;55:e20210170. 10.1590/1980-220X-REEUSP-2021-0170. [DOI] [PubMed] [Google Scholar]
- 48.Liu S, Lu Y, Wang D, et al. Impact of digital health literacy on health-related quality of life in Chinese community-dwelling older adults: the mediating effect of health-promoting lifestyle. Front Public Health. 2023;11:1200722. 10.3389/fpubh.2023.1200722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Katsaliaki K. Evaluating patient and medical staff satisfaction from doctor-patient communication. Int J Health Care Qual Assur 2022; ahead-of-print. 10.1108/IJHCQA-03-2022-0033. [DOI] [PubMed]
- 50.Zhu W, He J, Guo H. Doctor-patient bilateral matching considering diagnosis and treatment perception in the absence of public health resources. Front Public Health. 2022;10: 1094523. 10.3389/fpubh.2022.1094523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Farmanova E, Bonneville L, Bouchard L. Organizational health literacy: review of theories, frameworks, guides, and implementation Issues. Inquiry. 2018;55: 46958018757848. 10.1177/0046958018757848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Coleman CA, Appy S. Health literacy teaching in US medical schools, 2010. Fam Med. 2012;44:504–7. [PubMed] [Google Scholar]
- 53.Palumbo R, Carmela A. The importance of being health literate: an organizational health literacy approach. Proceedings of the 17th Toulon-Verona Conference ‘Excellence in Services’. England: Liverpool; 2014.
- 54.Zanchetta M, Taher Y, Fredericks S, et al. Undergraduate nursing students integrating health literacy in clinical settings. Nurse Educ Today. 2013;33:1026–33. 10.1016/j.nedt.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 55.Weaver NL, Wray RJ, Zellin S, et al. Advancing organizational health literacy in health care organizations serving high-needs populations: a case study. J Health Commun. 2012;17(Suppl 3):55–66. 10.1080/10810730.2012.714442. [DOI] [PubMed] [Google Scholar]
- 56.Brega AG BJ, Mabachi NM, . AHRQ health literacy universal precautions toolkit, second edition. In: Quality AfHRa, (ed.). 2015.
- 57.Rudd RE AJ. The Health Literacy Environment of Hospitals and Health Centers. In: (NCSALL) NCftSoALaL, (ed.). 2006.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.