Abstract
Purpose:
To report a case of Light Adjustable Lens™ (LAL, RxSight, Aliso Viejo, CA) implantation in a patient with bilateral 50-cut radial keratotomy (RK) and discuss related preoperative, intraoperative, and postoperative considerations.
Methods:
A 78-year-old patient with history of bilateral 50-cut RK underwent phacoemulsification with implantation of LALs in both eyes one month apart. Although LAL technology was not approved specifically for addressing limitations in intraocular lens calculation post-RK due to corneal topography irregularity, the patient opted for this lens due to its ability to make post-operative adjustments to its refractive power. At postoperative month one following the second eye surgery, YAG capsulotomy was performed in both eyes. At postoperative month two following the second eye surgery, the patient began LAL adjustments spaced 1–2 weeks apart for a total of 2 LAL adjustments and 2 lock-in sessions.
Results:
Our patient achieved a final refraction of −0.25 +0.25 × 110 with an UDVA of 20/20–2 in the right eye and −0.25 +0.50 × 135 with an UDVA 20/25–1 in the left eye.
Conclusions:
The LAL may be a promising option for patients undergoing cataract surgery after RK, although further studies are needed to understand long-term changes in eyes with RK and the inability of LAL to address all aspects of corneal aberration.
Keywords: light adjustable lens, radial keratotomy, post-refractive cataract surgery
Introduction
Intraocular lens (IOL) calculations in cataract surgery after prior radial keratotomy (RK) are a well-known challenge given refractive instability of the cornea throughout the day and risk for postoperative hyperopic surprise and progressive shift.1 Even with modern formulas such as the Barrett TK True-K, studies show only 50% of eyes achieve ±0.5 D of their refractive target due to inaccuracies in determining the true corneal power and the effective lens position in post-RK eyes.2,3,4 The Light Adjustable Lens (LAL; RxSight, Inc., Aliso Viejo, CA, USA) is an IOL implant that uses ultraviolet light (UV) treatments postoperatively to adjust the shape of the lens and therefore its refractive power. Because the LAL can be adjusted postoperatively to reduce residual refractive error following cataract surgery, it is a promising option for patients with less predictable refractive outcomes such as eyes with a history of corneal refractive surgery, although its effectiveness in enhancing refractive outcome predictability in patients with prior corneal refractive surgery remains to be evaluated in larger studies. Postoperatively, multiple refractions and adjustments can be repeated until the patient’s final refractive target is achieved. In this report, we present a case of bilateral LAL implantation after phacoemulsification in a patient with a history of 50-cut RK that achieved the desired target refraction without complication.
Case Presentation
A 78-year-old male was referred to an academic university cornea clinic for cataract surgery evaluation. The patient reported blurry vision and glare at night preventing him from driving. He did not complain of subjective changes in vision based on time of day. The patient had a past ocular history of myopia and underwent radial keratotomy (RK) in both eyes 35 years ago.
On ophthalmologic examination, his uncorrected distance visual acuity (UDVA) in the right eye was 20/50+2 and left eye was 20/60+1. His preoperative manifest refraction in the right eye was −1.50 +2.25 × 145 with a best-corrected distance VA of 20/30–2 and left eye was +0.25 +1.25 × 040 with a best-corrected distance VA of 20/50. Preoperative potential acuity pinhole was 20/20 in both eyes. Dilated exam showed myopic peripapillary atrophy but was otherwise unremarkable. Central corneal pachymetry was 495 microns in the right eye and 491 microns in the left eye. Corneal topography showed typical post-RK pattern with central flattening in both eyes (Figure 1A). The average keratometry values obtained from corneal topography, tomography, and optical biometry showed good agreement (35.78 – 36.23 D for the right eye and 35.11 – 36.1 D for the left eye). He had moderate dilation of 5 mm that improved to 6 mm after 3 rounds of 1% tropicamide and 10% phenylephrine. His corneal exam showed 50-cut RK with cuts extending to the limbus with a central iron line in both eyes (Figure 1B). He had 2+ nuclear sclerotic cataracts in both eyes.
Figure 1:
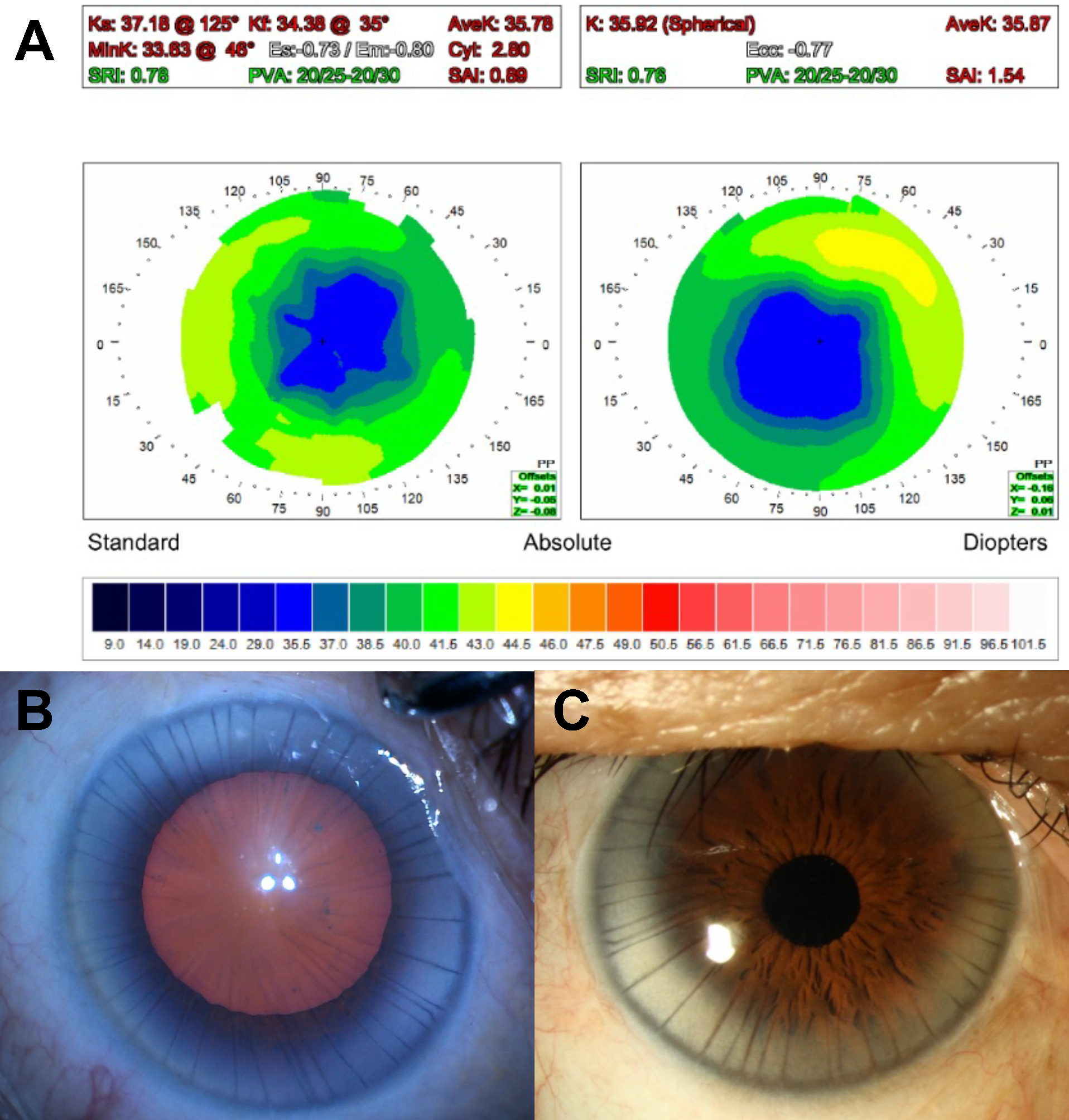
A) Preoperative corneal topography shows central flattening consistent with post-RK in both eyes. Right eye shows average keratometry of 35.78 D and cylinder of 2.8 D x 125 degrees. Left eye shows average keratometry of 35.87 D and spherical (0 D of cylinder). B) Intraoperative view of the right eye prior to starting cataract surgery shows 50-cut RK on the cornea, 6 mm of pupillary dilation, and 2+ nuclear sclerotic cataract. C) Postoperative exam of the right eye shows a clear and compact cornea with a round miotic pupil.
A detailed discussion of the potential lens options and the risk for residual postoperative ametropia were performed with the patient, including that irregularities on corneal topography may not be fully correctable with LAL. However due to the ability to make adjustments post-operatively, the patient opted for LAL placement in both eyes. Barrett TK True-K formula for RK was used, and the power of the LAL was selected for a target refraction of plano in both eyes (−0.09 D in the right eye and −0.14 D in the left eye). He underwent uncomplicated phacoemulsification of the right eye followed by the left eye one month later. Surgical technique was as follows: the paracentesis was created at the limbus between RK incisions, and a small scleral tunnel was fashioned temporally for the main incision to avoid overlapping an RK incision; trypan blue was used to enhance visualization of the capsule due to corneal distortions from the RK incisions; at the end of the case, the scleral tunnel was sutured, conjunctival peritomy was closed, and a fluorescein strip was used to confirm the entire cornea was Seidel negative (Supplementary Video 1).
Postoperatively, the patient remained Seidel negative with clear and compact corneas in both eyes (Figure 1C), however the patient was noted to have mild visually significant central posterior capsular opacification (PCO) in both eyes. At the postoperative month (POM) one visit following the second eye, the patient underwent uncomplicated YAG capsulotomy in both eyes. One month later (POM3 in the right eye and POM2 in the left eye), the patient began LAL adjustments. His postoperative refraction prior to LAL adjustments was −1.50 +2.25 × 150 for an UDVA of 20/25 in the right eye and −2.25 +1.50 × 180 for an UDVA of 20/30–2 in the left eye. Two rounds of LAL adjustments and two lock-in sessions were performed 1–2 weeks apart to improve short-term refractive stability, and his final refraction was −0.25 +0.25 × 110 with an UDVA of 20/20–2 in the right eye at POM4 and −0.25 +0.50 × 135 for an UDVA 20/25–1 in the left eye at POM3.
Discussion
In the 1980s, RK was one of the most commonly performed refractive surgery procedures for myopia with the number of cuts usually ranging from 4 to 24. Our patient underwent 50-cut RK, which to our knowledge is the highest number of RK incisions reported in the literature. The Prospective Evaluation of Radial Keratotomy (PERK) study demonstrated a diurnal fluctuation of refractive error as well as progressive hyperopic shift over time.5 RK changes the curvature of the central cornea leading to inaccuracies in biometric measurements and poor predictability in IOL calculations despite advancements in modern formulas. To combat this, counseling the patient about less predictable outcomes as well as targeting some residual myopia, even for distance correction, is preferred to avoid a hyperopic surprise and account for hyperopic drift over time. Prior to LAL, there was also a relative absence of procedures available to address post-operative ametropia; PRK is much less predictable in these patients and LASIK is not advisable in many settings.
The introduction of the LAL provides an opportunity to noninvasively adjust refractive power of the IOL postoperatively. In patients with a history of corneal refractive surgery, it is important to set realistic patient expectations that LAL may not fully correct irregularities from corneal topography. Therefore, post-RK patients with fewer irregularities on corneal topography may predict higher rate of success with LAL. In general, post-refractive eyes, including post-RK eyes, are more prone to refractive surprise and therefore may be good candidates for the LAL to allow for correction of residual refractive error. General indications for LAL in RK patients include adequate pupillary dilation (at least 6 mm but ideally ≥7 mm) and ability to tolerate 3–5 UV light treatments and to wear UV-blocking glasses until one day after the LAL has been locked-in. We prefer to target plano for post-RK LAL implantation since the LAL adjustments can correct ±2.0 D of residual spherical error and 2.75 D of residual cylinder.6 Moshirfar et al were the first to describe the use of LAL in a patient with prior 8-cut RK who achieved UDVA of 20/25 in both eyes.7 Our case provides another example in which LAL was used to mitigate refractive surprise after cataract surgery in post-RK eyes.
While a clear corneal incision may be used in certain cases where there is sufficient clearing between RK incisions (typically 8-cuts or fewer), our patient had previously undergone 50-cut RK necessitating a scleral tunnel to avoid transecting RK incisions. Prior studies have reported that the most common complication during cataract surgery in post-RK eyes was RK incision dehiscence.8,9 Care must be taken intraoperatively to avoid excess strain on the already weakened cornea and may require lower infusion pressure and minimizing number of times entering and exiting the anterior chamber. At the end of our patient’s surgery, Seidel testing was performed on all RK and surgical incisions to ensure watertight closure.
In our patient, PCO was noted at the POM1 visit of the left eye (POM2 visit of the right eye). While some studies have concluded that refractive changes after YAG capsulotomy are insignificant, other studies have shown hyperopic, myopic, or cylindric refractive changes.10 Due to RK incisional swelling, the refractive outcome following cataract surgery in post-RK eyes is often initially hyperopic and it may take 6–12 weeks for the edema to improve and refraction to stabilize.11 Given this, LAL adjustments should be performed no earlier than six weeks postoperatively to ensure a stable refraction. In our patient’s case, the history of high myopia also increased the of risk of retinal detachment, however, after a detailed risk/benefit discussion, the decision was made to proceed with YAG capsulotomy prior to LAL adjustments to provide better refractive measurements while waiting for the cornea to stabilize postoperatively. Patients should also be counseled regarding the prolonged recovery time in which they must continue to wear UV-blocking glasses.
In conclusion, this case demonstrates the use of LALs in a patient with 50-cut RK undergoing cataract surgery that achieved an excellent short-term UDVA in both eyes. Careful cataract surgery preoperative, intraoperative, and postoperative management are keys to a successful post-RK patient outcome. Further studies are needed to evaluate long-term results and stability in post-RK patients receiving LALs.
Supplementary Material
Supplementary Video 1: Microsurgical Video for 50-Cut Radial Keratotomy (RK) Cataract Surgery with the Light Adjustable Lens (LAL). The paracentesis was created at the limbus between RK incisions, and a small scleral tunnel was fashioned temporally for the main incision to avoid overlapping an RK incision. Trypan blue was used to enhance visualization of the capsule due to corneal distortions from the RK incisions. Intraocular infusion pressure was lowered to 40 mmHg to prevent strain on RK incisions. At the end of the case, the scleral tunnel was sutured, conjunctival peritomy was closed, and a fluorescein strip was used to confirm the entire cornea was Seidel negative.
Funding:
This study was supported by K08 EY033859 from the National Eye Institute, Career Development Award from the Research to Prevent Blindness, and grant from the All May See Foundation to Dr. Pasricha. This work was made possible in part by the UCSF Vision Core Grant (P30 EY002162) and Research to Prevent Blindness Unrestricted Grant to the University of California San Francisco, Department of Ophthalmology.
Footnotes
Conflicts of Interest: J.M.S. and N.D.P. report consulting fees from Zeiss. The other authors have no conflicts of interest.
References
- 1.Koch DD, Liu JF, Hyde LL, Rock RL, Emery JM. Refractive complications of cataract surgery after radial keratotomy. Am J Ophthalmol. 1989;108:676–82 [DOI] [PubMed] [Google Scholar]
- 2.Shetty N, Sathe P, Aishwarya Francis M, Shetty R. Comparison of intraocular lens power prediction accuracy of formulas in American Society of Cataract and Refractive Surgery post-refractive surgery calculator in eyes with prior radial keratotomy. Indian J Ophthalmol. 2023. Sep;71(9):3224–3228. doi: 10.4103/IJO.IJO_3417_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leite de Pinho Tavares R, de Almeida Ferreira G, Ghanem VC, Ghanem RC. IOL Power Calculation After Radial Keratotomy Using the Haigis and Barrett True-K Formulas. J Refract Surg. 2020. Dec 1;36(12):832–837. doi: 10.3928/1081597X-20200930-02. [DOI] [PubMed] [Google Scholar]
- 4.Gouvea L, Sioufi K, Brown CE, Waring Iv G, Chamon W, Rocha KM. Refractive Accuracy of Barrett True-K vs Intraoperative Aberrometry for IOL Power Calculation in Post-Corneal Refractive Surgery Eyes. Clin Ophthalmol. 2021. Oct 27;15:4305–4315. doi: 10.2147/OPTH.S334489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waring GO 3rd, Lynn MJ, McDonnell PJ. Results of the prospective evaluation of radial keratotomy (PERK) study 10 years after surgery. Arch Ophthalmol. 1994. Oct;112(10):1298–308. doi: 10.1001/archopht.1994.01090220048022. [DOI] [PubMed] [Google Scholar]
- 6.FDA Summary of Safety and Effectiveness Data P160055. 2017. Nov 22, https://www.accessdata.fda.gov/cdrh_docs/pdf16/P160055B.pdf
- 7.Moshirfar M, Duong AA, Shmunes KM, Castillo-Ronquillo YS, Hoopes PC. Light Adjustable Intraocular Lens for Cataract Surgery After Radial Keratotomy. J Refract Surg. 2020. Dec 1;36(12):852–854. doi: 10.3928/1081597X-20201002-01. [DOI] [PubMed] [Google Scholar]
- 8.Soare C, Patel DS, Ionides A. Cataract surgery outcomes in eyes with previous radial keratotomy. Eye (Lond). 2022. Sep;36(9):1804–1809. doi: 10.1038/s41433-021-01716-6. Epub 2021 Aug 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meduri A, Urso M, Signorino GA, Rechichi M, Mazzotta C, Kaufman S. Cataract surgery on post radial keratotomy patients. Int J Ophthalmol. 2017. Jul 18;10(7):1168–1170. doi: 10.18240/ijo.2017.07.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moshirfar M, Basharat NF, Seitz TS, Peterson CM, Stapley SR, Ziari M, Bundogji N, Ronquillo YC, Hoopes PC. Refractive Changes After Nd:YAG Capsulotomy in Pseudophakic Eyes. Clin Ophthalmol. 2023. Jan 7;17:135–143. doi: 10.2147/OPTH.S395605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alio JL, Abdelghany AA, Abdou AA, Maldonado MJ. Cataract surgery on the previous corneal refractive surgery patient. Surv Ophthalmol. 2016. Nov-Dec;61(6):769–777. doi: 10.1016/j.survophthal.2016.07.001. Epub 2016 Jul 15. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Video 1: Microsurgical Video for 50-Cut Radial Keratotomy (RK) Cataract Surgery with the Light Adjustable Lens (LAL). The paracentesis was created at the limbus between RK incisions, and a small scleral tunnel was fashioned temporally for the main incision to avoid overlapping an RK incision. Trypan blue was used to enhance visualization of the capsule due to corneal distortions from the RK incisions. Intraocular infusion pressure was lowered to 40 mmHg to prevent strain on RK incisions. At the end of the case, the scleral tunnel was sutured, conjunctival peritomy was closed, and a fluorescein strip was used to confirm the entire cornea was Seidel negative.


