Abstract
Background
Face‐to‐face interventions for promoting physical activity (PA) are continuing to be popular but their ability to achieve long term changes are unknown.
Objectives
To compare the effectiveness of face‐to‐face interventions for PA promotion in community dwelling adults (aged 16 years and above) with a control exposed to placebo or no or minimal intervention.
Search methods
We searched CENTRAL, MEDLINE, EMBASE, CINAHL, and some other databases (from earliest dates available to October 2012). Reference lists of relevant articles were checked. No language restrictions were applied.
Selection criteria
Randomised controlled trials (RCTs) that compared face‐to‐face PA interventions for community dwelling adults with a placebo or no or minimal intervention control group. We included studies if the principal component of the intervention was delivered using face‐to‐face methods. To assess behavioural change over time the included studies had a minimum of 12 months follow‐up from the start of the intervention to the final results. We excluded studies that had more than a 20% loss to follow‐up if they did not apply an intention‐to‐treat analysis.
Data collection and analysis
At least two authors independently assessed the quality of each study and extracted data. Non‐English language papers were reviewed with the assistance of an interpreter who was an epidemiologist. Study authors were contacted for additional information where necessary. Standardised mean differences (SMDs) and 95% confidence intervals (CIs) were calculated for continuous measures of self‐reported PA and cardio‐respiratory fitness. For studies with dichotomous outcomes, odds ratios (ORs) and 95% CIs were calculated.
Main results
A total of 10 studies recruiting 6292 apparently healthy adults met the inclusion criteria. All of the studies took place in high‐income countries. The effect of interventions on self‐reported PA at one year (eight studies; 6725 participants) was positive and moderate with significant heterogeneity (I² = 74%) (SMD 0.19; 95% CI 0.06 to 0.31; moderate quality evidence) but not sustained in three studies at 24 months (4235 participants) (SMD 0.18; 95% CI ‐0.10 to 0.46). The effect of interventions on cardiovascular fitness at one year (two studies; 349 participants) was positive and moderate with no significant heterogeneity in the observed effects (SMD 0.50; 95% CI 0.28 to 0.71; moderate quality evidence). Three studies (3277 participants) reported a positive effect on increasing PA levels when assessed as a dichotomous measure at 12 months, but this was not statistically significant (OR 1.52; 95% CI 0.88 to 2.61; high quality evidence). Although there were limited data, there was no evidence of an increased risk of adverse events (one study; 149 participants). Risk of bias was assessed as low (four studies; 4822 participants) or moderate (six studies; 1543 participants). Any conclusions drawn from this review require some caution given the significant heterogeneity in the observed effects. Despite this, there was some indication that the most effective interventions were those that offered both individual and group support for changing PA levels using a tailored approach. The long term impact, cost effectiveness and rates of adverse events for these interventions was not established because the majority of studies stopped after 12 months.
Authors' conclusions
Although we found evidence to support the effectiveness of face‐to‐face interventions for promoting PA, at least at 12 months, the effectiveness of these interventions was not supported by high quality studies. Due to the clinical and statistical heterogeneity of the studies, only limited conclusions can be drawn about the effectiveness of individual components of the interventions. Future studies should provide greater detail of the components of interventions, and assess impact on quality of life, adverse events and economic data.
Keywords: Adult, Aged, Female, Humans, Male, Middle Aged, Young Adult, Exercise, Motor Activity, Counseling, Counseling/methods, Health Promotion, Health Promotion/methods, Randomized Controlled Trials as Topic
Plain language summary
Face‐to‐face interventions for promoting physical activity
Participating in insufficient amounts of physical activity leads to an increased risk of a number of chronic diseases, and physical and mental health problems. Regular physical activity should be a goal for all adults and can provide social, emotional and physical health benefits. The majority of adults are not active at recommended levels. We included a total of 10 studies recruiting 6292 apparently healthy adults in this review. The findings of the review indicate that interventions can successfully support adults' attempts to become active and fitter, for example with personal counselling and advice, feedback and offering choices of exercise, and supervision. Outcomes are improved if the intervention comprises a specified type of physical activity and is supervised by a non‐health professional using a combination of group and individual approaches. New physical activity can be maintained for up to at least one year and does not increase the risk of falls or exercise related injuries. More research is needed to establish which methods of exercise promotion work best in the long term to encourage specific groups of people to be more physically active.
Summary of findings
Summary of findings for the main comparison. Face‐to‐face interventions versus control for promoting physical activity.
| Face‐to‐face interventions versus control for promoting physical activity | ||||||
| Patient or population: patients with promoting physical activity Settings: Intervention: face‐to‐face interventions versus control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Face‐to‐face interventions versus control | |||||
| Cardio‐respiratory fitness: 12 months Sub maximal assessment of cardio‐respiratory fitness Follow‐up: mean 12 months | The mean cardio‐respiratory fitness: 12 months in the intervention groups was 7.23 standard deviations higher (5.82 lower to 20.28 higher) | 426 (2 studies) | ⊕⊕⊕⊝ moderate1 | SMD 7.23 (‐5.82 to 20.28) | ||
| Dichotomous outcomes: 12 months Self‐reported PA questionnaire Follow‐up: mean 12 months | Study population | OR 1.58 (0.91 to 2.75) | 3261 (3 studies) | ⊕⊕⊕⊕ high | ||
| 284 per 1000 | 385 per 1000 (265 to 521) | |||||
| Moderate | ||||||
| 300 per 1000 | 404 per 1000 (281 to 541) | |||||
| Dichotomous outcomes: 24 months Self‐reported PA questionnaire Follow‐up: mean 24 months | Study population | OR 1.19 (1.02 to 1.39) | 2701 (1 study) | ⊕⊕⊕⊕ high | ||
| 346 per 1000 | 387 per 1000 (351 to 424) | |||||
| Moderate | ||||||
| 346 per 1000 | 386 per 1000 (350 to 424) | |||||
| Self‐reported physical activity: 24 months Self‐reported PA questionnaire Follow‐up: median 24 months | The mean self‐reported PA: 24 months in the intervention groups was 0.18 standard deviations higher (0.1 lower to 0.46 higher) | 4235 (3 studies) | ⊕⊕⊕⊕ high | SMD 0.18 (‐0.10 to 0.46) | ||
| Self‐reported physical activity: 12 months Self‐reported PA questionnaire Follow‐up: mean 12 months | The mean self‐reported PA: 12 months in the intervention groups was 0.18 standard deviations higher (0.06 to 0.31 higher) | 23825 (8 studies) | ⊕⊕⊕⊝ moderate1 | SMD 0.19 (0.06 to 0.31) | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Background
This review focuses on face‐to‐face interventions that promote physical activity (PA). It is part of a suite of three complementary reviews that provide both an update and a progression for the previously completed Cochrane review assessing 'Interventions for promoting physical activity' (Foster 2005a). The titles of the other reviews in this suite are:
'Face‐to‐face versus remote and web 2.0 interventions for promoting physical activity';
'Remote and web 2.0 interventions for promoting physical activity'.
The evidence base for both face‐to‐face PA promotion and remote and web 2.0 interventions is rapidly growing and diverging. Consequently, we divided this Cochrane update into two separate reviews that focus on of each of these delivery methods compared to true control groups. The third review enabled a head‐to‐head comparison between these intervention approaches for promoting PA. In all of the reviews we also considered how the effectiveness of PA interventions is influenced by implementing the intervention to a group or individually. The paradigm through which we approached these different methods of PA intervention delivery in this suite of reviews is summarised below (Figure 1).
1.

Delivery of PA interventions described according to interaction with implementer and other participants.
Description of the condition
The health benefits of adequate levels of PA have been well documented (WHO 2010a). Previous systematic reviews and meta‐analyses of observational studies have demonstrated the role of PA in the prevention and treatment of coronary heart disease, hypertension, stroke, type II diabetes, obesity, metabolic syndrome, breast cancer, colon cancer, osteoporosis, falls, depression, anxiety and negative self‐concept (Haskell 2007; Janssen 2010; Kesaniemi 2001; Nelson 2007; Strong 2005; Warburton 2006; Williams 2001). It is estimated that in 2008 physical inactivity caused 9% of premature mortality and 5.3 million deaths worldwide (Lee 2012). This included between 6% to 10% of all deaths from major non‐communicable diseases globally. The burden of such diseases is also increasing rapidly in low‐ and middle‐income countries (Lee 2012; WHO 2010b).
The World Health Organization (WHO) recommends that adults should accumulate at least 150 minutes of moderate intensity or 75 minutes of vigorous intensity PA, or an equivalent combination of aerobic PA, throughout the week (WHO 2010a). This should be achieved in bouts of at least 10 minutes duration (WHO 2010a). Muscle strengthening activities involving the major muscle groups are also recommended on at least two days per week (WHO 2010a). Investigations into the dose‐response relationship indicate that PA at levels higher than the minimum recommendations confer greater health benefit (Kesaniemi 2001; WHO 2010a).
The available data suggest that 31.1% of the world's adult population are not meeting the minimum recommendations for PA (Hallal 2012). The direct economic burden of physical inactivity is 1.5% to 3.0% of healthcare system costs and it is an emerging expense in low‐and middle‐income countries (Oldridge 2008). It has been estimated that increasing the number of people that achieve the WHO PA recommendations by 10% or 25% would prevent more than 553,000 and 1.3 million deaths, respectively, globally each year (Lee 2012).
Description of the intervention
It has long been accepted that various interventions can promote PA participation and improve health (Dishman 1996). This has prompted growing global interest and investment in PA interventions by different stakeholders using a variety of methods (Heath 2012). It is evident that there are opportunities to influence personal, social and environmental determinants of PA in different contexts and populations (Bauman 2012). A previous Cochrane review found that PA interventions had a moderate effect on participation levels (Foster 2005a). However, conclusions could not be drawn about the effectiveness of isolated components for achieving and maintaining recommended levels of PA in the population.
For the purposes of this review an intervention is any deliberate attempt to increase the PA levels of the participants. It may be delivered using various methods and implemented through a broad range of professions (for example health professional, exercise specialist, PA researchers). This is consistent with the principles of the previous versions of this review (Foster 2005a). The critical additional component of face‐to‐face interventions is that the interaction with the implementer occurs in person. These interventions can be delivered to groups or individually and several examples are presented below (Table 2).
1. Examples of strategies used in typical face‐to‐face physical activity interventions.
| Face‐to‐face intervention | |
| Individual | 1) Counselling session to assess self‐efficacy and skills training to enhance options to be physically active |
| 2) Personal training to improve fitness delivered directly by instructor in the gym | |
| 3) Health professionals distributing booklets to patients that describe the benefits of physical activity | |
| Group | 1) Exercise class to improve strength delivered directly by instructor in a community park |
| 2) Education sessions for physical activity opportunities at a community health centre | |
| 3) Group bush walking session co‐ordinated by a hike leader |
How the intervention might work
One of the earliest reviews of determinants of PA stated that few interventions or adherence studies were based on any theoretical or psychological models (Dishman 1990). However, when the review was repeated four years later the authors noted a marked increase in the use of theories in studies and interventions (Dishman 1994). It is now accepted that well designed PA interventions are based upon behavioural theories (Bartholomew 2001), but understanding how these are translated into practical strategies needs further evaluation (Foster 2005a). Behavioural theories provide a foundation for an intervention that can explain the drivers of PA behaviour and potential pathways for change (Foster 2005b). They also inform the planning, development and implementation of PA interventions, and the majority of studies have adopted social psychology theories (Biddle 2011).
Most of the theory previously applied to PA interventions has stemmed from face‐to‐face approaches. Epidemiological studies have tried to explain the variation of PA behaviour by examining the impact of different factors or correlates. These have been described as operating at two levels, the intrinsic and extrinsic levels (Sallis 1997). Correlates like social class, personality, cognition, attitudes and beliefs operate at an intrinsic level. Extrinsic factors are divided into incentive structures like sports facilities or access to green spaces, and legal restrictions like prohibitive laws (Sallis 1999). Intrinsic factors have received greater attention than the external factors in attempts to explain behavioural choices influenced by face‐to‐face interventions.
Four common theories were cited in the reviews conducted by Dishman (Dishman 1990; Dishman 1994). These were the Health Belief Model (HBM) (Becker 1974); the Theory of Reasoned Action/Planned Behaviour (TRA) (Fishbein 1975); Social Cognitive Theory (SCT) (Bandura 1986); and the Transtheoretical Model of behaviour change (TTM) (Prochaska 1982). These models have 'conceptual convergence' (Biddle 2001) and share two common constructs (Rodgers 1991):
outcome expectancy, the belief that the behaviour will lead to a specific outcome;
social norms, the influence of expected behaviours within a social group.
More recently other theories have emerged that include the Health Action Process Model (Schwarzer 2008); the Common Sense Model of Illness Perceptions (Hagger 2003); and the Behavioural Choice Theory (Epstein 2001). These models tend to encompass the connection between intrinsic and extrinsic drivers of behaviour.
There are several common strategies used in face‐to‐face interventions for changing PA behaviour that can be grounded in each of these theoretical models, and some examples of applying these were described previously (Table 2). Firstly, stimulus control is the manipulation of factors that prompt and improve accessibility to PA opportunities while reducing the desirability and appeal of sedentary behaviour (Foster 2005b). The provision of exercise classes and walking groups in local communities are examples that are typically delivered face‐to‐face. Secondly, drawing the attention of the participant to the immediate benefits of PA reinforces the behaviour and may increase the likelihood that it will be repeated (Hillsdon 2002). This may include the face‐to‐face provision of rewards, progress reviews, and praise from practitioners or peers. Each of these strategies can contribute to building social support and developing self‐efficacy for engaging in PA (McAuley 1994). However, the key component of these face‐to‐face approaches may be the elicitation of empathy as the implementer (Miller 2012; Rogers 1969):
understands the participants' feelings;
responds to what has been said in a way that reflects the participants' mood;
conveys the ability to share the participants' feelings.
Why it is important to do this review
Although it is known that the behaviour of individuals can be influenced by PA interventions, the most effective delivery method is not clear (Foster 2005a). In recent times there has been an emergence of remotely delivered interventions that has accelerated with the advent of web 2.0 technology (van den Berg 2007). This impetus has displaced several more traditional face‐to‐face methods of implementing PA interventions (van den Berg 2007).
It is intended that this review will provide an up‐to‐date indication of the effectiveness of face‐to‐face PA interventions. Understanding the effectiveness of these more traditional approaches to implementation should influence PA policy makers and professionals. Completing this update ensures that the most effective implementation methods are identified and is integral for optimising health‐related outcomes related to the promotion of PA participation.
Objectives
Primary
To compare the effectiveness of face‐to‐face interventions for physical activity (PA) promotion in community dwelling adults (aged 16 years and above) with a control exposed to placebo or no or minimal intervention.
Secondary
If sufficient data exist, the following secondary objectives will be assessed.
Does delivering the intervention to a group versus individually versus mixed (a combination of group and individually) influence the effectiveness in changing PA?
Does the professional delivering the intervention (for example health professional, exercise specialist) influence the effectiveness in changing PA?
Does specifying PA type (for example walking, jogging, aerobics) influence the effectiveness in changing PA?
Does supervising the prescribed PA influence the effectiveness in changing PA?
Does including theory based counselling as part of the intervention influence the effectiveness in changing PA?
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) that compared face‐to‐face PA interventions for community dwelling adults with a placebo or no or minimal intervention control group. We included studies if the principal component of the intervention was delivered using face‐to‐face methods. To assess behavioural change over time the included studies had a minimum of 12 months follow‐up from the start of the intervention to the final results. We excluded studies that had more than a 20% loss to follow‐up if they did not apply an intention‐to‐treat analysis.
Types of participants
Community dwelling adults, aged 16 years to any age, who were free from pre‐existing medical conditions or with no more than 10% of participants with pre‐existing medical conditions that may have limited participation in PA.
We excluded interventions for trained athletes or sports students.
We only included studies that measured PA at an individual level.
Types of interventions
Face‐to‐face PA interventions could be delivered using supervised methods (for example exercise class) or an unsupervised approach (for example home exercise programme), or both. The interventions could be delivered to groups or individuals. They could involve one‐off or ongoing interactions between the implementer and the participants that included:
counselling or advice, or both;
self‐directed or prescribed exercise, or both;
home based or facility based exercise, or both;
written education or motivational support material, or both.
We excluded mass media and multiple risk factor interventions.
The comparison was with a control group exposed to placebo or no or minimal intervention.
Types of outcome measures
Primary outcomes
The primary outcomes of this review included data that assessed change between baseline and follow‐up for:
cardio‐respiratory fitness (CF), which is often used as a marker for PA and demonstrates similar associations with health related outcomes (Blair 2001). It was either estimated from a submaximal fitness test or recorded directly from a maximal fitness test. CF was typically expressed as a VO2 max score, which is an abbreviation for maximal oxygen uptake (ml/kg/min or ml/min).
PA levels expressed as an estimate of total energy expenditure (kcal/kg/week or kcal/week), total minutes completed at a moderate or vigorous intensity, proportion that reached a predetermined threshold level (for example meeting current public health recommendations), or frequency of participation. PA could be assessed using objective methods (for example accelerometers, pedometers) or more subjective tools (for example PA diary, survey), or both.
Both 12 and 24 month outcomes were included in the analysis.
Secondary outcomes
The secondary outcomes of this review included data relevant to:
quality of life (for example quality‐adjusted life years (QALYs));
cost (for example cost‐benefit, cost‐utility);
adverse events (for example musculoskeletal injury, cardiovascular event).
Search methods for identification of studies
Electronic searches
We searched the following databases between the 9 October 2012 and 11 October 2012:
CENTRAL (Issue 9 of 12, September 2012) in The Cochrane Library;
MEDLINE (Ovid) (1946 to week 4 September 2012);
EMBASE Classic and EMBASE (Ovid) (1947 to Week 40 2012);
CINAHL Plus with Full Text (EBSCO);
PsycINFO (Ovid) (1806 to week 1 October 2012);
Web of Science.
We based the search on the previous methods used for the 'Interventions for promoting physical activity' Cochrane review (Foster 2005a) (Appendix 1) and updated the methods with some amendments (Appendix 2).
The Cochrane RCT filter (sensitivity maximising) was applied to MEDLINE (Ovid) and search terms as suggested in the Cochrane Handbook for Systematic Reviews of Interventions were used to limit the studies to RCTs in EMBASE (Ovid) (Lefebvre 2011). Adaptations of these filters were used in the other databases except for CENTRAL.
We did not apply any language restriction to the searches.
Searching other resources
We conducted handsearching for the International Journal of Behavioural Nutrition and Physical Activity (February 2004 to October 2012). The reference lists of all relevant articles identified during the search were checked by the authors. We also used published systematic reviews of PA interventions as a source for identifying RCTs.
We communicated directly with authors to identify and request unpublished studies and data. A comprehensive list of relevant articles along with the inclusion criteria for the review were sent to the first author of each paper that met the inclusion criteria to ask if they knew of any additional published or unpublished studies which were relevant.
Data collection and analysis
Selection of studies
Two authors (CF, JR) independently manually screened the titles identified in the initial search to exclude those that were obviously outside the scope of the review. The authors were conservative at this stage and where disagreement occurred the citation was included for abstract review. Two authors (CF, JR) independently reviewed the abstracts of all citations that passed the initial title screening. They applied the following inclusion criteria to determine if the full paper was needed for further scrutiny.
Did the study:
aim to examine the effectiveness of a PA or CF promotion strategy to increase PA or CF levels;
use principally face‐to‐face methods to promote PA to the intervention group;
allocate participants to the intervention or control group using a method of randomisation;
have a control group that was exposed to placebo or no or minimal intervention;
include adults aged 16 years and older;
recruit community dwelling adults that were free of chronic disease or with no more than 10% of participants with pre‐existing medical conditions that may limit participation in PA;
have a follow‐up period of at least 12 months between commencing the intervention and measuring the outcomes;
analyse the results by intention to treat or, failing that, was there less than a 20% loss to follow‐up.
The authors were conservative at this stage and where disagreement occurred the citation was included for full text review. Two authors (CF, JR) reviewed the full texts of all studies that passed the abstract screening, using the inclusion criteria described above, to identify a final set of eligible studies. The studies included in the previous 'Interventions for promoting physical activity' Cochrane review were also allocated within the new suite of reviews by two authors (CF, JR) (Foster 2005a). When there was persisting disagreement it was resolved by consensus after a third author (MH or MT) reviewed the study in question. Publications and reports that utilised the same data were linked to avoid replication in the analysis.
Data extraction and management
The data extraction form was independently piloted by two authors (CF, JR) and subsequently adjusted to ensure that it captured the relevant data. One author (CF or JR) and a Research Fellow from the Warwick Medical School (NF) independently extracted the data from all of the selected studies using the standard form. When there was disagreement a third author reviewed the study and consensus was reached (CF or JR, the author out of these two that did not do the initial data extraction). We separately extracted the data from multiple publications of the same study and then combined them to avoid replication. Any missing or ambiguous data were clarified with the study first author via e‐mail.
Assessment of risk of bias in included studies
The risk of bias was only assessed and reported for studies that met the inclusion criteria (Higgins 2011).
Two authors (CF, JR) assessed the risk of bias. Where there was disagreement between the review authors in risk of bias assessment, a third author (MH or MT) was asked to independently appraise the study and discrepancies were resolved by consensus between all three authors.
We assessed the studies for the five general domains of bias: selection, performance, attrition, detection, and reporting. Quality scores were allocated for:
allocation sequence generation;
allocation concealment;
incomplete outcome data;
selective outcome reporting;
comparable groups at baseline;
contamination between groups;
validated outcome measures;
outcome measure applied appropriately;
final analysis adjusted for baseline PA levels;
outcome assessment that was independent and blinded;
intention‐to‐treat analysis.
When sufficient information was available, we classified each study as a 'high' or 'low' risk of bias for each item. When there was a lack of information or uncertainty over the potential for bias, we described the domain as 'unclear'. We judged the quality of the evidence as 'low', 'medium', or 'high' given consideration of the study design and size, and the potential impact of the identified weaknesses noted in the risk of bias table for each study.
Measures of treatment effect
For each study with dichotomous outcomes, we expressed the effect size using an odds ratio (OR). For each study with continuous outcomes, we expressed the effect size using the standardised mean difference (SMD) between the post‐intervention values of the randomised groups. We completed a narrative summary of the study results and when there were sufficient data we completed a formal meta‐analysis of the included studies.
Unit of analysis issues
When possible, we analysed the studies using the mean and standard deviation (SD) and visualised the results using forest plots. Alternatively we reported only the point estimates with confidence intervals (CIs) and P values.
When a study had more than one study arm relevant to this review, we examined the overall effects of the intervention versus control by combining the data from the related study arms. We calculated the mean and SD according to the overall numbers within each arm using established approaches (Higgins 2011).
For each study with dichotomous outcomes we calculated an OR and 95% CI. We used the number of participants in each arm that were reported as an event (for example active at a predetermined level) or no event (for example not active). Where appropriate, we calculated individual study effects and then the pooled effect sizes as ORs with 95% CIs using a random‐effects model. We calculated any missing 95% CIs using established approaches (Higgins 2008).
Dealing with missing data
We excluded studies that had a high degree of incomplete data (that is less than 40% of data) during the risk of bias assessment or when it appeared that missing data were likely to be associated with the reported intervention effect. We contacted the authors of potentially included studies if missing data were unclear or the data had not been fully reported. Missing data were captured in the data extraction form and reported in the risk of bias table.
Assessment of heterogeneity
We quantified and evaluated the amount of heterogeneity to determine whether the observed variation in the study results was compatible with the variation expected by chance alone (Deeks 2011). Heterogeneity was assessed through examination of the forest plots and quantified using the I2 statistic.
Assessment of reporting biases
We plotted trial effect against standard error and presented it as a funnel plot (Sterne 2011). Asymmetry could be caused by a relationship between effect size and sample size or by publication bias, and we also examined any observed effect for clinical heterogeneity (Sterne 2011).
Data synthesis
When possible we reported all continuous outcomes on the original scale. If the outcomes were combined from different scales we standardised them as required for the analysis. We only completed a meta‐analysis when the data were clinically homogeneous, and we followed established Cochrane methods (Deeks 2011). If data were available, sufficiently similar, and of adequate quality, we used the Cochrane Collaboration's statistical software, Review Manager 2012, to perform the statistical analyses. We used a random‐effects model as the default to incorporate heterogeneity between studies. We did not combine evidence from differing study designs and outcome types in the same forest plot (Christinsen 2009).
Subgroup analysis and investigation of heterogeneity
We performed subgroup analyses to compare interventions that were delivered:
to a group versus individually versus mixed (combined group and individually);
by a health professional versus a non‐health professional;
with a PA type specified versus not specified;
with direct supervision versus unsupervised;
with theory based counselling versus without theory based counselling.
Sensitivity analysis
We conducted a sensitivity analysis for studies that definitively definitively met at least 50% of the applicable criteria reported in the 'Risk of bias' tables.
Results
Description of studies
See 'Characteristics of included studies'; 'Characteristics of excluded studies'; 'Characteristics of studies awaiting classification'; 'Characteristics of ongoing studies'
Results of the search
From 27,299 de‐duplicated hits, the full texts of 193 papers were retrieved for examination against the inclusion criteria (Figure 2). There were 12 papers describing 10 studies that met the inclusion criteria (Aittasalo 2004; Calfas 2000; Cunningham 1987; Grandes 2011; Harland 1999; Hillsdon 2002; Katz 2008; King 1991; Kriska 1986; Stewart 2001).
2.
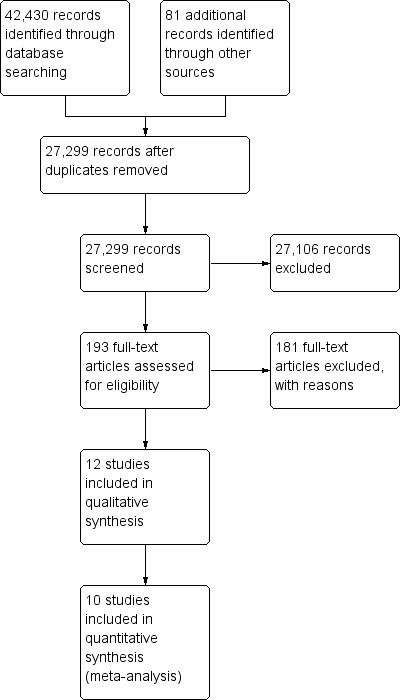
Study flow diagram.
All searches were completed in October to November 2012. The results of the searches of the electronic databases are found in Table 3.
2. Search results for electronic databases.
| Database searched | Number of hits |
| CINAHL | 4454 |
| The Cochrane Library | 6703 |
| EMBASE | 8930 |
| MEDLINE Ovid | 11431 |
| PsycINFO Ovid | 4156 |
| Science Citation Index Expanded | 6756 |
| Total | 42430 |
| After de‐duplication | 27299 |
Included studies
There were 7265 apparently healthy adults who participated in the 10 included studies. The majority of studies recruited both genders, with one study recruiting women only (Kriska 1986) and one study recruiting men only (Cunningham 1987). The stated age range of participants was from 18 to 90 years, and five of the studies specifically targeted adults aged between 40 and 65 years (Cunningham 1987; Harland 1999; Hillsdon 2002; King 1991; Kriska 1986). Details on the ethnic groups of participants were reported in four studies (Cunningham 1987; Hillsdon 2002; Katz 2008; King 1991), with proportions of participants in ethnic minorities ranging from 0% to 68%. Participants were recruited from primary healthcare setiings in five studies (Calfas 2000; Grandes 2011; Harland 1999; Hillsdon 2002; Katz 2008) and the workplace in one study (Aittasalo 2004). All of the studies took place in high‐income countries.
The intervention was delivered individually in five studies (Aittasalo 2004; Grandes 2011; Harland 1999; Hillsdon 2002; Katz 2008) and as a mix between individual and group delivery in the other five studies (Calfas 2000; Cunningham 1987; King 1991; Kriska 1986; Stewart 2001). In four of the studies the intervention was delivered by health professionals (Aittasalo 2004; Grandes 2011; Harland 1999; Katz 2008), and was primarily supervised in three studies (Cunningham 1987; King 1991; Kriska 1986). The PA type was specified in three studies (Cunningham 1987; Kriska 1986; Stewart 2001), and theory based counselling formed part of the intervention in five studies (Aittasalo 2004; Harland 1999; Hillsdon 2002; Katz 2008; Stewart 2001).
Eight studies included PA self‐report at 12 months as an outcome measure (Aittasalo 2004; Calfas 2000; Cunningham 1987; Grandes 2011; Hillsdon 2002; Katz 2008; Kriska 1986; Stewart 2001) and this was sustained for 24 months in three of these studies (Calfas 2000; Grandes 2011; Kriska 1986). Three studies reported a dichotomous outcome variable for PA at 12 months (Aittasalo 2004; Grandes 2011; Harland 1999) and one of these presented follow‐up data at 24 months (Grandes 2011). There were two studies that reported cardiovascular fitness at 12 months (Cunningham 1987; King 1991).
Eight of the included studies were from the Foster 2005a review (Aittasalo 2004; Calfas 2000; Cunningham 1987; Harland 1999; Hillsdon 2002; King 1991; Kriska 1986; Stewart 2001) and two studies were identified by the updated search (Grandes 2011; Katz 2008).
Excluded studies
The reasons for excluding papers that underwent full text review are outlined in the 'Characteristics of excluded studies' table. Three main reasons contributed to more than 80% of the exclusions. The most prevalent was less than 12 months follow‐up (n = 78), followed by no appropriate control or intervention group (n = 37) or a remote and web 2.0 intervention only (n = 31). There were also two ongoing studies that met the inclusion criteria but had insufficient data at the time of this review (Iliffe 2010; Wilson 2010).
Risk of bias in included studies
We assessed the risk of bias of the included studies as low in four studies (Grandes 2011; Hillsdon 2002; King 1991; Stewart 2001) and there was a moderate risk of bias in the remaining six studies (Aittasalo 2004; Calfas 2000; Cunningham 1987; Harland 1999; Katz 2008; Kriska 1986) (Figure 3; Figure 4).
3.
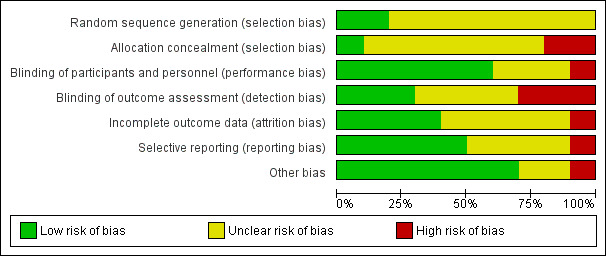
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
4.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All of the included studies used randomised controlled designs. One study was assessed to have low risk of bias for both allocation sequence generation and concealment (Hillsdon 2002). Grandes 2011 was assessed to have a low risk of bias only for allocation sequence generation, and all other studies were unclear in their approach to allocation generation or concealment. Five studies were assessed as having a low risk of selection bias as they reported comparable groups at baseline (Harland 1999; Hillsdon 2002; King 1991; Kriska 1986; Stewart 2001).
Blinding
We did not rate studies on whether participants were blinded to their group allocation. This would not be appropriate for studies of this type as it would be impossible to blind participants to a PA intervention. We did assess studies on their performance bias, which included an evaluation of whether the outcome assessments were performed independently and by an assessor who was blinded to participant allocation status. Only three studies were assessed to have a low risk of performance bias on these criteria (Grandes 2011; Harland 1999; King 1991). Five studies were assessed to have a high risk of bias for blinding and independence of outcome assessment (Calfas 2000; Cunningham 1987; Hillsdon 2002; Kriska 1986; Stewart 2001), with two studies rated as unclear (Aittasalo 2004; Katz 2008).
Nine studies were judged to have a low risk of detection bias (Aittasalo 2004; Calfas 2000; Cunningham 1987; Grandes 2011; Hillsdon 2002; Katz 2008; King 1991; Kriska 1986; Stewart 2001). This was an assessment of the validity and quality of outcome measures plus their appropriateness of application with the participants. The outcome measure used by Harland 1999 did not report any measurement metrics and was adapted from a national survey tool.
Incomplete outcome data
Two studies were assessed as being at low risk of attrition bias as they had reported complete outcome data and presented reasons for any participant dropouts (Cunningham 1987; Hillsdon 2002). Three studies were assessed as being at high risk of bias for not reporting any attrition data (Aittasalo 2004; Calfas 2000; King 1991), with five studies assessed as unclear (Grandes 2011; Harland 1999; Katz 2008; Kriska 1986; Stewart 2001).
Selective reporting
Six studies were assessed as at low risk of reporting bias (Aittasalo 2004; Calfas 2000; Cunningham 1987; Harland 1999; Hillsdon 2002; King 1991), with the remaining four studies assessed as unclear (Hillsdon 2002; Katz 2008; Kriska 1986; Stewart 2001).
Other potential sources of bias
Other potential sources of bias included two criteria assessed in the earlier version of this review (Foster 2005a). These were: adjusting the final results for baseline values of PA, and adopting an intention‐to‐treat analysis approach.
Adjusting for baseline values of PA is particularly important in behaviour change studies as there is a likelihood of overestimating effects if baseline adjustment is not performed when using dichotomous outcome measures (for example per cent of adults achieving recommended level of PA). Only six studies had a low risk of bias for this criterion (Aittasalo 2004; Calfas 2000; Grandes 2011; Hillsdon 2002; King 1991; Stewart 2001). Three studies did not adjust their final results for baseline PA levels (Cunningham 1987; Harland 1999; Kriska 1986) with Katz 2008 assessed as unclear.
Intention‐to‐treat analysis underpins the principles of an RCT design to minimise bias. Therefore, we considered failure to include all randomised participants in the final outcome analysis within their allocated group as a critical risk of bias. Five studies were assessed to have conducted an intention‐to‐treat anlaysis (Grandes 2011; Harland 1999; Hillsdon 2002; Kriska 1986; Stewart 2001), with the other five studies not meeting this criterion (Aittasalo 2004; Calfas 2000; Cunningham 1987; Katz 2008; King 1991). The proportion of participants in studies that did not perform an intention‐to‐treat analysis and who were lost to follow‐up ranged from 3.9% to 15.9%.
Effects of interventions
See: Table 1
Cardio‐respiratory fitness
Two studies (349 participants) reported the effect of their intervention on cardio‐respiratory fitness (Cunningham 1987; King 1991). The pooled effect was positive and moderate with no significant heterogeneity in the observed effects (SMD 0.50; 95% CI 0.28 to 0.71), see Analysis 1.1.
1.1. Analysis.
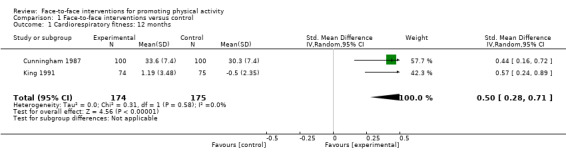
Comparison 1 Face‐to‐face interventions versus control, Outcome 1 Cardiorespiratory fitness: 12 months.
King 1991 reported a significant difference in VO2 max between the intervention and control groups at 12 months follow‐up (SMD 0.57; 95% CI 0.24 to 0.89). Participants received baseline physiological assessments and then were prescribed group based training at high intensity plus written information, PA logs, and phone calls. They attended local exercise classes at least three times per week for 12 months. Telephone calls were made once a week for the first four weeks, twice a week for the next four weeks, and then once a month for 12 months.
Cunningham 1987 reported a significant difference in VO2 max between the intervention and control groups at 12 months follow‐up (SMD 0.44; 95% CI 0.16 to 0.72). Participants received three group exercise sessions per week and were encouraged to do one additional home based session.
Self‐reported physical activity ‐ reported as a dichotomous measure
Three studies (3277 participants) reported the effect of their intervention on PA as a dichotomous measure at 12 months (Aittasalo 2004; Grandes 2011; Harland 1999). The pooled effect was positive but not statistically significant (OR 1.52; 95% CI 0.88 to 2.61), see Analysis 1.2.
1.2. Analysis.

Comparison 1 Face‐to‐face interventions versus control, Outcome 2 Dichotomous outcomes: 12 months.
Aittasalo 2004 found significant differences in the proportion of participants reporting increases in leisure time PA levels at 12 months (OR 3.65; 95% CI 1.53 to 8.68). The participant’s current leisure time PA was assessed by a trained nurse and an individual goal was set. All participants were given a supplementary leaflet about PA, developed for the contemplation and preparation stages, plus a written weekly PA plan and a self‐monitoring PA diary for the next follow‐up visit. At the follow‐up visits (after eight weeks, six and 12 months) progress was reviewed and, if necessary, the plan modified. During all the visits emphasis was put on strengthening the participant’s positive impressions of his or her capability to follow the plan (self‐efficacy). Three fitness tests were also administered at baseline, six and 12 months.
Harland 1999 reported a similar result but it was not statistically significant (OR 1.29; 95% CI 0.73 to 2.28). All participants completed a baseline assessment of self‐reported PA, physical measures, and a cycle ergometer fitness test. They received feedback of their results, brief advice about their present level of PA in comparison to recommended levels, written health information, and 19 leaflets about local PA facilities and activities. In addition, each participant was allocated to one of four intervention groups: (i) one motivational interview; (ii) one motivational interview plus vouchers for free use of local facilities; (iii) six motivational interviews over 12 weeks; and (iv) six motivational interviews over 12 weeks plus vouchers.
Grandes 2011 found no significant difference after 12 months in the proportion of participants reporting that they achieved the recommended level of 150 minutes of at least moderate intensity PA per week (OR 1.13; 95% CI 0.96 to 1.33). However, after 24 months there was a significant difference between the intervention and control groups (OR 1.19; 95% CI 1.02 to 1.39), see Analysis 1.3. Participants received brief advice from physicians and educational materials within a 15 minute intervention plus an individualised PA plan. The intervention was supported by web based software to prompt and guide the physician and patient session.
1.3. Analysis.

Comparison 1 Face‐to‐face interventions versus control, Outcome 3 Dichotomous outcomes: 24 months.
Self‐reported physical activity ‐ reported as a continuous measure
Eight studies (6725 participants) reported their main outcome as one of several continuous measures of PA (Aittasalo 2004; Calfas 2000; Cunningham 1987; Grandes 2011; Hillsdon 2002; Katz 2008; Kriska 1986; Stewart 2001). Measures included estimated energy expenditure (kcals/day, kcals/week of moderate or vigorous PA (MVPA)), total time of PA (mean mins/week of MVPA), and mean number of occasions of PA in past four weeks. The pooled effect at 12 months was positive and moderate with significant heterogeneity (I² = 74%) (SMD 0.19; 95% CI 0.06 to 0.31), see Analysis 1.4.
1.4. Analysis.
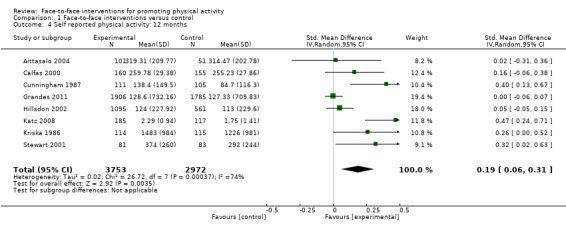
Comparison 1 Face‐to‐face interventions versus control, Outcome 4 Self reported physical activity: 12 months.
Three of these studies (4235 participants) reported follow‐up measures at 24 months (Calfas 2000; Grandes 2011; Kriska 1986). Kriska 1986 found a significant difference in weekly total energy (kcal/week) at 12 months (SMD 0.26; 95% CI 0.00 to 0.52) and 24 months (SMD 0.54; 95% CI 0.27 to 0.80). The participants received a baseline physical assessment, eight week walking training programme with organised walks, and then a choice of group or independent walking. Participants monitored their walking with monthly logs and were also offered social meetings. Participants received follow‐up phone calls, cards, and incentives to maintain compliance. Calfas 2000 found no significant difference in total energy expenditure (kcal/kg/wk) at 12 months (SMD 0.16; 95% CI ‐0.06 to 0.38) and 24 months (SMD 0.06; 95% CI ‐0.16 to 0.29). The participants received a 15 week cognitive behavioural education course, which comprised 15 x 50 minute lectures followed by 15 x 110 minute laboratory experiences that were led by peer health facilitators and included the practice of behavioural management strategies as homework. Participants received two course credits and could attend two supervised exercise sessions per week. All participants received monthly follow‐up phone calls and monthly written materials for 15 months. The pooled effect at 24 months was not statistically significant (SMD 0.18; 95% CI ‐0.10 to 0.46), see Analysis 1.5.
1.5. Analysis.

Comparison 1 Face‐to‐face interventions versus control, Outcome 5 Self reported physical activity: 24 months.
The interventions for Aittasalo 2004, Cunningham 1987 and Grandes 2011 were described previously. Aittasalo 2004 found no significant difference at 12 months in the number of minutes of leisure time PA each week (SMD 0.02; 95% CI ‐0.31 to 0.36). Cunningham 1987 found a significant difference at 12 months in the number of minutes of high intensity PA (SMD 0.40; 95% CI 0.13 to 0.67). Grandes 2011 found no significant difference in PA volume (unit used to estimate the metabolic cost of physical activity ‐ MET/h/week) at both 12 months (SMD 0.00; 95% CI ‐0.06 to 0.07) and 24 months (SMD 0.01; 95% CI ‐0.05 to 0.08). Hillsdon 2002 reported no significant difference between the participants receiving either advice or counselling to exercise and control participants (SMD 0.05; 95% CI ‐0.05 to 0.15).
Katz 2008 tested the effectiveness of the Pressure Systems Model for PA promotion and reported positive effects at 12 months for outcomes, assessed by the Yale Physical Activity Survey (SMD 0.47; 95% CI 0.24 to 0.71). Intervention patients were categorised into groups and received tailored counselling based on motivational interviewing plus handout materials. Categorisation was based on answers to two questions that determined the approach undertaken by the counselling physician, and these included prompts on how to overcome specific patient barriers to exercise.
Stewart 2001 reported a significant net difference of 82 kcal per day between the intervention and control arms (95% CI 73.9 to 90.1), with a positive effect (SMD 0.32; 95% CI 0.02 to 0.63). The intervention group received face‐to‐face counselling based on social cognitive theory (Bandura 1986). In addition, they were offered further individual follow‐up appointments, educational materials, phone calls and monthly workshops about PA.
We found no evidence of publication bias (Figure 5).
5.

Funnel plot of comparison: 1 Face‐to‐face interventions versus control, outcome: 1.4 Self‐reported physical activity: 12 months.
Sensitivity analysis by study quality
We examined the pooled effects for the three types of outcome data (self‐reported PA, dichotomous and cardio‐respiratory fitness outcomes) by an assessment of study risk of bias. We stratified studies based on their risk of bias assessments (ROB), see Table 4 and Table 5, by only pooling estimates of effects for studies that had a lower risk of bias (≥ 50% of the ROB criteria). Pooled estimates were presented for each outcome type, see Analysis 2.1, Analysis 2.2, Analysis 2.3, Analysis 2.4, Analysis 2.5. Four studies were included (5636 participants) after the sensitivity analysis (King 1991; Grandes 2011; Hillsdon 2002; Stewart 2001). A positive but non‐significant pooled estimate was found for the three studies reporting self‐reported PA effects at 12 months (SMD 0.05; 95% CI ‐0.05 to 0.15), see Analysis 2.4. Grandes 2011 found a positive effect on PA levels at 24 months when reported as a dichotomous variable (OR 1.19; 95% CI 1.02 to 1.39) but found no interim effect at 12 months.
3. Risk of bias and quality scores for included studies.
| Study | Allocation sequence generation | Allocation concealment | Incomplete outcome data | Selective outcome reporting | Comparable groups at baseline | Contamination between groups |
| Aittasalo 2004 | U | U | N | Y | U | U |
| Calfas 2000 | U | U | N | Y | U | NA |
| Cunningham 1987 | U | U | Y | Y | U | NA |
| Grandes 2011 | Y | N | U | Y | U | NA |
| Harland 1999 | U | U | U | Y | Y | NA |
| Hillsdon 2002 | Y | Y | Y | U | Y | NA |
| Katz 2008 | U | U | U | U | U | NA |
| King 1991 | U | U | N | Y | Y | NA |
| Kriska 1986 | U | U | U | U | Y | NA |
| Stewart 2001 | U | U | U | U | Y | NA |
4. Risk of bias and quality scores for included studies.
| Study | Validated outcome measures | Applied appropriately | Final analysis adjusted for baseline physical activity levels | Outcome assessment independent and blinded | Intention‐to‐treat analysis |
| Aittasalo 2004 | Y | Y | Y | U | N |
| Calfas 2000 | Y | U | Y | N | N |
| Cunningham 1987 | Y | Y | N | N | N |
| Grandes 2011 | Y | Y | Y | Y | Y |
| Harland 1999 | U | U | N | Y | Y |
| Hillsdon 2002 | Y | Y | Y | N | Y |
| Katz 2008 | Y | Y | U | U | N |
| King 1991 | Y | Y | Y | Y | N |
| Kriska 1986 | Y | Y | N | N | Y |
| Stewart 2001 | Y | Y | Y | N | Y |
2.1. Analysis.

Comparison 2 Face‐to‐face interventions versus control (risk of bias score ≥ 50%), Outcome 1 Cardiorespiratory fitness: 12 months.
2.2. Analysis.

Comparison 2 Face‐to‐face interventions versus control (risk of bias score ≥ 50%), Outcome 2 Dichotomous outcomes: 12 months.
2.3. Analysis.
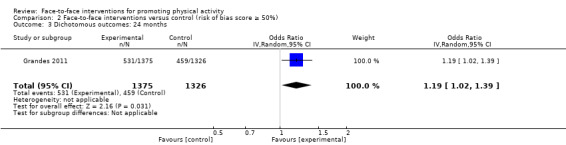
Comparison 2 Face‐to‐face interventions versus control (risk of bias score ≥ 50%), Outcome 3 Dichotomous outcomes: 24 months.
2.4. Analysis.

Comparison 2 Face‐to‐face interventions versus control (risk of bias score ≥ 50%), Outcome 4 Self reported physical activity: 12 months.
2.5. Analysis.

Comparison 2 Face‐to‐face interventions versus control (risk of bias score ≥ 50%), Outcome 5 Self reported physical activity: 24 months.
Secondary outcomes
Quality of life
Only one study reported quality of life outcomes, using the Short Form (SF)‐36 measure, see Table 6 (Grandes 2011). The authors reported no differences between the intervention and control groups for Physical And Mental Component scores for the SF‐36 (assessed at 12 and 24 months). No other study reported any quality of life outcomes.
5. Quality of life outcomes.
| Study | Quality of life outcomes |
| Aittasalo 2004 | Not reported |
| Calfas 2000 | Not reported |
| Cunningham 1987 | Not reported |
| Grandes 2011 | Physical And Mental Component scores for SF‐36 were assessed at 12 and 24 months but no differences were reported between intervention and control groups for these variables |
| Harland 1999 | Not reported |
| Hillsdon 2002 | Not reported |
| Katz 2008 | Not reported |
| King 1991 | Not reported |
| Kriska 1986 | Not reported |
| Stewart 2001 | Not reported |
Cost effectiveness
No studies reported report data on cost effectiveness, see Table 7.
6. Cost effectiveness.
| Study | Cost effectiveness |
| Aittasalo 2004 | Not reported |
| Calfas 2000 | Not reported |
| Cunningham 1987 | Not reported |
| Grandes 2011 | Not reported |
| Harland 1999 | Not reported |
| Hillsdon 2002 | Not reported |
| Katz 2008 | Not reported |
| King 1991 | Not reported |
| Kriska 1986 | Not reported |
| Stewart 2001 | Not reported |
Adverse events
Only King 1991 reported data on adverse events, see Table 8. PA related non‐cardiac injuries were few and were similar in number across the study arms. These included mild muscular fatigue, strain, or soreness during the initial three to four months of intervention across both PA arms.
7. Adverse events.
| Study | Adverse events |
| Aittasalo 2004 | Not reported |
| Calfas 2000 | Not reported |
| Cunningham 1987 | Not reported |
| Grandes 2011 | Not reported |
| Harland 1999 | Not reported |
| Hillsdon 2002 | Not reported |
| Katz 2008 | Not reported |
| King 1991 | There were several sprains and fractures reported, but there was no difference between the groups and none of the injuries caused any of the participants to withdraw from the study. No cardiac events were reported |
| Kriska 1986 | Not reported |
| Stewart 2001 | Not reported |
Secondary objectives
8. Who delivers intervention and follow‐up, and individual or group approach.
| Study | Who delivered the primary dose of intervention? | Intervention individual or group based primary dose | Who delivered the follow‐up dose of intervention? | Intervention individual or group based follow‐up |
| Aittasalo 2004 | Occupational nurse | Individual | Occupational nurse | Individual |
| Calfas 2000 | Behavioural and exercise science lecturers | Group | Peer health educators | Group and individual |
| Cunningham 1987 | Exercise leaders | Group | Exercise leaders | Group and individual |
| Grandes 2011 | Physicians | Individual | Physicians | Individual |
| Harland 1999 | Health visitor | Individual | Health visitor | Individual |
| Hillsdon 2002 | Exercise specialist | Individual | Exercise specialist | Individual |
| Katz 2008 | Physicians | Individual | Physicians | Individual |
| King 1991 | Project staff member | Individual | Group based training provided by community exercise instructors with physical education degrees. Project staff member made follow‐up phone calls | Individual and group |
| Kriska 1986 | Exercise leaders | Individual and group | Exercise leaders | Individual and group |
| Stewart 2001 | Trained staff | Individual and group | Counsellor | Individual and group |
9. Intensity of primary intervention and follow‐up, and physical activity choice and supervision.
| Study | Primary dose intensity | Physical activity choice | Physical activity supervision | Follow‐up frequency and dose |
| Aittasalo 2004 | Counselling session focusing on assessment of PA and construction of PA plan | Participants choose own activities | Unsupervised | Follow up meetings at 8, 24 and 12 months. Fitness group received additional fitness tests at baseline and 6 months |
| Calfas 2000 | 50 minute faculty led lecture | Participants choose own activities | Unsupervised | Additional weekly lectures and peer led laboratories plus phone calls and written materials |
| Cunningham 1987 | Participants were instructed to participate in 3 group exercise sessions per week and were encouraged to do one additional home based session | Three group based exercise classes plus one additional occasion per week | Supervised | Three group based exercise classes per week |
| Grandes 2011 | GPs provided brief advice about the benefits of PA, or brief advice plus a 3 month PA prescription | Participants choose own activities | Unsupervised | An additional 15 minute appointment was offered to the brief advice group to prescribe a 3 month PA plan. Review of progress was conducted opportunistically |
| Harland 1999 | 40 minute motivational interview counselling plus a PA plan. Additional group received vouchers to use local PA facilities | Participants choose own activities | Unsupervised | Up to five additional interviews offered over the first 12 weeks of the intervention, plus vouchers |
| Hillsdon 2002 | 30 minute motivational interview counselling using decisional balance, assessment of current PA etc., or advice to exercise, plus printed materials | Participants choose own activities | Unsupervised | All participants received follow up phone calls at 2, 6, 10, 18, 26, 34 weeks. Calls were supposed to last no more than 3 minutes |
| Katz 2008 | Motivational interview counselling using decisional balance, assessment of current PA, plus printed materials | Participants choose own activities | Unsupervised | Follow‐up arranged by consent between physicians and patients if needed. Identified local opportunities to exercise plus additional written materials |
| King 1991 | Participants received a baseline physiological assessment and then were prescribed group based training at high intensity plus written information for 12 months 30‐40 minutes duration |
Group based attended local classes (3 x week) | Supervised | Four phone calls in first four weeks, then two calls in next four weeks, followed by once a month for 12 months. Phone calls were used to monitor progress, answer questions and provide feedback from activity logs |
| Kriska 1986 | Participants received eight weeks of walking training in groups, plus encouraged to walk once a week independently | Prescribed group walking plus independent walking | Supervised | After the walking training the participants could choose group or independent walking up to 3 miles per walk. Monthly walking self‐monitoring sheets were collected at end of each month, plus frequent social gatherings, phone calls, mail‐outs, and birthday cards. Rewards and incentives were given for distances achieved, plus newsletters. Unspecified frequency of follow‐up activities |
| Stewart 2001 | Participants received a client centred interview using motivational, cognitive, behavioural techniques. Plus access to 10 workshops with emphasis on attending the first two workshops | Participants choose own activities but emphasis on walking | Unsupervised | Access to 10 follow‐up workshops plus phone calls and written information |
Does delivering the intervention to a group versus individually versus mixed (combined group and individually) influence the effectiveness in changing PA?
Only four studies adopted an individual approach as part of their intervention (5801 participants), with a non‐significant pooled estimated effect (SMD 0.11; 95% CI ‐0.04 to 0.27) (Aittasalo 2004; Grandes 2011; Hillsdon 2002; Katz 2008), see Analysis 3.1. No studies adopted a consistent group based approach as part of their intervention. Four studies used both individual and group approaches (924 participants) with a positive pooled estimate effect (SMD 0.27; 95% CI 0.14 to 0.40) with no significant heterogeneity (Calfas 2000; Cunningham 1987; Kriska 1986; Stewart 2001), see Analysis 3.2.
3.1. Analysis.
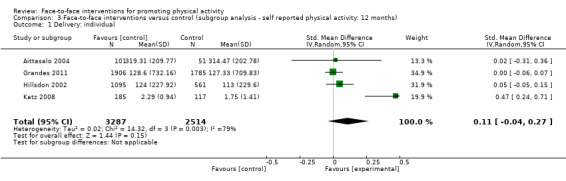
Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 1 Delivery: individual.
3.2. Analysis.

Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 2 Delivery: mixed (individual and group).
Does the professional delivering the intervention (for example health professional, exercise specialist) influence the effectiveness in changing PA?
Three studies (4145 participants) delivered their interventions via a health professional, with a positive but non‐significant pooled effect estimate (SMD 0.16; 95% CI ‐0.15 to 0.48) (Aittasalo 2004; Grandes 2011; Katz 2008), see Analysis 3.3. Five studies (2580 participants) delivered their interventions via a non‐health professional with a positive and significant pooled effect estimate (SMD 0.20; 95% CI 0.06 to 0.35) (Calfas 2000; Cunningham 1987; Hillsdon 2002; Kriska 1986; Stewart 2001), see Analysis 3.4. Although it appears that there is a differential effect between non‐ versus heath professional intervention delivery, only two of the five studies in the non‐health professional group had low risk of bias and their combined effect estimate was positive but not significant (SMD 0.15; 95% CI ‐0.11 to 0.40) (Hillsdon 2002; Stewart 2001).
3.3. Analysis.

Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 3 Implementer: health professional.
3.4. Analysis.
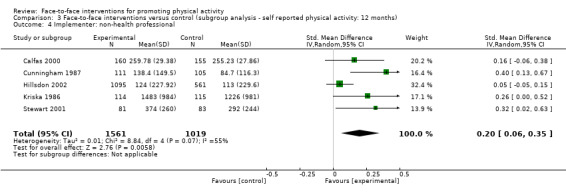
Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 4 Implementer: non‐health professional.
Does specifying physical activity type (for example walking, jogging, aerobics) influence the effectiveness in changing PA?
Three studies (609 participants) specified the type of PA for their participants (Cunningham 1987; Kriska 1986; Stewart 2001) with a positive pooled effect estimate (SMD 0.33; 95% CI 0.17 to 0.49), see Analysis 3.5. Five studies (6116 participants) offered a choice of PA to their participants (Aittasalo 2004; Calfas 2000; Grandes 2011; Hillsdon 2002; Katz 2008) and their combined effect estimate was positive but not significant (SMD 0.12; 95% CI ‐0.01 to 0.25), see Analysis 3.6.
3.5. Analysis.

Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 5 Physical activity type: specified.
3.6. Analysis.
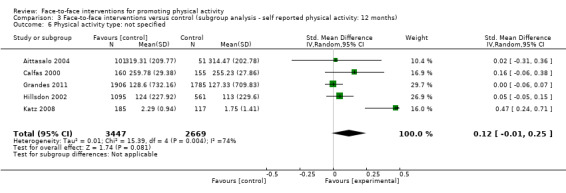
Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 6 Physical activity type: not specified.
Does supervising the prescribed physical activity influence the effectiveness in changing PA?
Two studies (445 participants) supervised their participants performing their PA prescription (Cunningham 1987; Kriska 1986) while six studies (6280 participants) did not supervise the participants (Aittasalo 2004; Calfas 2000; Grandes 2011; Hillsdon 2002; Katz 2008; Stewart 2001). The pooled effect estimate for supervised studies was positive (SMD 0.33; 95% CI 0.14 to 0.51), see Analysis 3.7. However, these two studies had a high risk of bias. The three low risk of bias studies in the unsupervised group did not have a significant positive pooled effect estimate (SMD 0.05; 95% CI ‐0.05 to 0.15).
3.7. Analysis.

Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 7 Prescribed physical activity: supervised.
Does including theory based counselling as part of the intervention influence the effectiveness in changing PA?
Four studies based their interventions and strategies on an expressed theory or model of behaviour change (Aittasalo 2004; Hillsdon 2002; Katz 2008; Stewart 2001). Aittasalo 2004 adapted strategies based upon the Transtheoretical Model of behaviour change (Prochaska 1982). Hillsdon 2002 and Katz 2008 used similar motivational based counselling strategies to support change, for example exploring patient ambivalence to change. Stewart 2001 delivered face‐to‐face counselling based on social cognitive theory (Bandura 1986). These studies produced a positive but non‐significant pooled effect estimate (SMD 0.21; 95% CI ‐0.02, 0.44), see Analysis 3.9. The four studies that did not base their interventions on an expressed theory also produced a positive but non‐significant pooled effect estimate (SMD 0.18; 95% CI ‐0.01, 0.37) (Calfas 2000; Cunningham 1987; Grandes 2011; Kriska 1986), see Analysis 3.10.
3.9. Analysis.
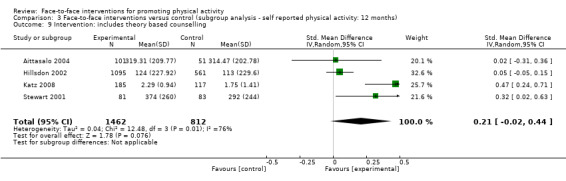
Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 9 Intervention: includes theory based counselling.
3.10. Analysis.

Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 10 Intervention: does not include theory based counselling.
Discussion
Summary of main results
We found consistent evidence to support the effectiveness of face‐to‐face interventions for promoting PA. These interventions have a positive moderate sized effect on increasing self‐reported PA and measured cardio‐respiratory fitness, at least at 12 months. However, the effectiveness of these interventions was not significant when considering only the higher quality studies, particularly for self‐reported PA at 12 months. We were not able to more rigorously assess the longer term effectiveness of face‐to‐face interventions to promote PA, beyond 12 months.
Including some group work in the intervention appeared to improve the effectiveness of the intervention. However, we were unable to assess the effectiveness of face‐to‐face interventions delivered in a group setting only. Instead, several studies included multiple intervention methods, which made it difficult to tease apart which intervention components were the active ingredients. The complexity of PA interventions appears to have increased over time. Indeed, it may actually be the interaction of multiple intervention components that is critical in facilitating PA behaviour change and this requires further investigation. Despite this, it appears that supervising participants' PA and specifying its type may improve the effectiveness of an intervention. Conversely, non‐health professionals appeared to deliver more effective interventions than health professionals.
There was a paucity of data reporting cost effectiveness, quality of life and adverse events. Given the apparent evolution towards more complex and multi‐faceted PA interventions, we believe that these are important considerations when assessing the public health value of an intervention. This should be a priority for future research.
Overall completeness and applicability of evidence
Our review demonstrates that there is moderate quality evidence to support the effectiveness of face‐to‐face interventions for promoting PA, but we note that the majority of studies targeted adults aged 40 to 65 years. Our conclusions are however limited because of the homogeneity of the target populations in the included studies. The participants in the studies that were reviewed were generally white, well educated and middle aged, and it is possible that the observed effects may be different in the wider population. There were no studies in this review that examined the effectiveness of interventions in minority groups of any kind or low‐ and middle‐income countries. Although studies in these settings were identified in the initial literature search, there continues to be a dearth of quality research in marginalised and poorer populations.
Furthermore, there were only a small number of new long term studies of face‐to‐face intervention for PA promotion. There was also a paucity of studies reporting data on quality of life, cost effectiveness and adverse events.
The completion of studies and applicability of this evidence may be limited by the relative cost of face‐to‐face interventions. Although the success of interventions delivered partly in groups and by non‐health professionals may improve intervention accessibility and cost effectiveness, this is offset by the apparent importance of intervention supervision. Further research is indicated exclusively into group based interventions and cost effectiveness.
Quality of the evidence
Since eight of the 10 included papers were from the previous review of interventions to promote PA to adults (Foster 2005a), the overall quality of the included studies did not remarkably improve in this update. However, it is promising to see that the most recent included study (Grandes 2011) scored the best of all the studies on the risk of bias assessment. We can only speculate that this is in response to our call for improved study quality to assess PA intervention effectiveness (Foster 2005a).
An overall strength of the studies was the consistent application of appropriate and validated outcome measures. This is particularly important given the small differences in changing levels of PA between the intervention and control groups, as intervention effects wane. We recognise that most studies used self‐report measures of PA, which are subject to recall bias and may lack precision but any misclassification is non‐differential (as both intervention and control groups complete the measure) and attenuate the effect of the intervention. This problem did not apply to measures of cardio‐respiratory fitness.
However, there were mixed responses to the other risk of bias criteria and several factors were widely unreported. This accounted for the few studies that were retained in the sensitivity analysis by study quality. It is important to recognise that none of the studies blinded participants to their group allocation, and we felt that this criterion was not appropriate to our studies because it is very difficult to do this for PA interventions.
It is also worth noting the large number of papers that were excluded from this review because they had an inadequate follow‐up period or did not have an appropriate control group. There is clearly an indication for future PA intervention studies to address these basic quality criteria.
Potential biases in the review process
One limitation of this review is potential publication bias. Other types of interventions may exist but have not been submitted or accepted for publication, or only those with positive results have been published. However, we identified little evidence of publication bias from our funnel plots.
Agreements and disagreements with other studies or reviews
Our results are consistent with recent systematic reviews of face‐to‐face interventions focusing on middle aged or older adults. We undertook a more stringent set of inclusion criteria than our previous review and only two new studies were added to our previous set (Foster 2005a). Our review is based on an increase in length of follow‐up from six to 12 months and a tighter focus on face‐to‐face interventions. Although our findings show a positive and moderate pooled effect on self‐reported PA at 12 months (SMD 0.19; 95% CI 0.06 to 0.31), the eight studies in the analysis had significant heterogeneity and suffered from a high risk of bias. Only one of the two new studies (Grandes 2011) was assessed to have a low risk of bias. These findings are mirrored in other systematic reviews of PA interventions for older adults. Hobbs 2013 reported an identical pooled effects size for PA interventions for older adults using counselling and lifestyle advice for self‐reported PA outcomes (SMD 0.19; 95% CI 0.10 to 0.28). Conn 2011 reported on randomised and non‐randomised PA interventions (n = 99,011 participants) and calculated a mean effect size for the comparison of intervention groups versus control groups that was positive but not significant (SMD 0.19; 95% CI –0.14 to 0.53). Both reviews were also unable to tease out what the active ingredients of a face‐to‐face intervention were and they were limited by the poor quality of the included studies. There was also significant heterogeneity among the included studies as reflected by the l2 statistic.
Our review highlighted the narrow type of participants who are recruited to participate in PA studies, for example five of the studies specifically targeted adults aged between 40 and 65 years. As such, any successful intervention may be at risk of increasing existing health inequalities because of differential responses in recruitment (Foster 2011). This concern is also shared by Humphrey and Ogilvie's innovative systematic review of reviews (Humphreys 2013) looking at the differential effects of population level PA interventions on social inequalities. They also observed that interventions compared effectiveness by gender followed by age, ethnicity, and socioeconomic status.
Authors' conclusions
Implications for practice.
There is some evidence to support the impact of face‐to‐face interventions to promote PA to older adults but this is limited by the heterogeneity of the studies. Therefore, only limited conclusions can be drawn about the effectiveness of individual components of the interventions as we are unable to demonstrate what the most effective strategies were within the interventions. However, there was some indication that the most effective interventions were those that offered both individual and group support for changing PA levels using a tailored approach. There was limited evidence that such interventions improved quality of life, cost effectiveness or incidence of adverse events. High quality studies investigating the long term effectiveness of face‐to‐face interventions on promoting PA remain a pressing need.
Implications for research.
There is a clear need for future RCTs to build and improve this evidence base by assessing the impact of face‐to‐face PA interventions for at least 12 months and ideally up to 24 months. It is imperative to assess the effect of interventions on participants from varying socioeconomic or ethnic groups, and to gather quality of life, cost effectiveness and adverse event data. In this review we have only been able to describe what was done within the interventions but were unable to unpick what elements worked (were most effective) within the interventions.
What's new
| Date | Event | Description |
|---|---|---|
| 30 August 2013 | Amended | Although we were able to find evidence to support the effectiveness of face‐to‐face interventions for promoting physical activity, at least at 12 months, the effectiveness of these interventions were not supported by high quality studies. |
Acknowledgements
The authors wish to acknowledge Karen Rees, Nadine Flowers and the Cochrane Heart Group for their contributions and support during the planning of this suite of reviews.
Appendices
Appendix 1. Search strategies 2005
MEDLINE (Ovid)
1 exp Exertion/ 2 Physical fitness/ 3 exp "Physical education and training"/ 4 exp Sports/ 5 exp Dancing/ 6 exp Exercise therapy/ 7 (physical$ adj5 (fit$ or train$ or activ$ or endur$)).tw. 8 (exercis$ adj5 (train$ or physical$ or activ$)).tw. 9 sport$.tw. 10 walk$.tw. 11 bicycle$.tw. 12 (exercise$ adj aerobic$).tw. 13 (("lifestyle" or life‐style) adj5 activ$).tw. 14 (("lifestyle" or life‐style) adj5 physical$).tw. 15 or/1‐14 16 Health education/ 17 Patient education/ 18 Primary prevention/ 19 Health promotion/ 20 Behaviour therapy 21 Cognitive therapy 22 Primary health care 23 Workplace/ 24 promot$.tw. 25 educat$.tw. 26 program$.tw. 27 or/16‐26 28 15 and 27
RCT filter (Dickersin 1995)
EMBASE
1.((((health‐education) or (health‐education‐research)) or ((patient‐education) or (patient‐education‐and‐counseling)) or ((health‐promotion) or (health‐promotion‐international)) or (primary‐health‐care) or ((workplace) or (workplace‐)) or (promot*) or ((promot*) or ((educat*) or ((program*) and ((((exertion) or (fitness) or (fitness‐) or ((fitness) or (fitness‐)) or (exercise) or ((exercise) or (sport) or (walk*))) 2.((research) or (((((random‐controlled) or (random‐sample) or (randomisation) or (randomised) or (randomised‐controlled) or (randomization) or (randomization‐) or (randomizd) or (randomize) or (randomized) or (randomized‐block) or (randomized‐controlled) or (randomized‐controlled‐trial) or (randomized‐control)) or ((double‐blind) or (double‐blind‐procedure)) or ((single‐blind) or (single‐blind‐procedure))) and (ec=human)) or (clinical) or (clin*) or (trial*) or (((clin* near trial*) in ti) and (ec=human)) or (clin*) or (trial*) or (((clin* near trial*) in ab) and (ec=human)) or (sing*) or (doubl*) or (trebl*) or (tripl*) or (blind*) or (mask*) or (((sing* or doubl* or trebl* or tripl*) near (blind* or mask*)) and (ec=human)) or ((placebos) or (placebo‐controlled)) or ((placebo* in ti) and (ec=human)) or ((placebo* in ab) and (ec=human)) or ((random* in ti) and (ec=human)) or ((random in ab) and (ec=human)) or (research)) ec=human) 3.((((studies) or (prospective‐study) or (follow‐up) or (comparative) or (evaluation)) and (ec=human))
CINAHL
1.exact{controlled} 2.exact{randomized} 3.exact{random‐assignment} 4.exact{double‐blind} 5.exact{single‐blind} 6.#1 or #2 or #3 or #4 or #5 7.exact{animal} 8.exact{human} 9.#6 not #7 10.exact{clinical} 11.(clin* near trial*) in ti 12.(clin* near trial*) in ab 13.(singl* or doubl* or trebl* or tripl*) near (blind* or mask*) 14.(#13 in ti) or (#13 in ab) 15.placebos 16.placebo* in ti 17.placebo* in ab 18.random* in ti 19.random* in ab 20.exact{research‐methodology} 21.#10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 22.#18 or #19 or #20 23.#21 or #22 24.animal 25.human 26.#23 not #24 27.#26 or #9 or #8 or #25 28.exact{comparative} 29.study 30.#28 and #29 31.exact{evaluation} 32.studies 33.#31 and #32 34.exact{follow‐up} 35.exact{propsective} 36.#35 and #32 37.control* or prosepctiv* or volunteer* 38.(#37 in ti) or (#37 in ab) 39.#38 or #36 or #33 or #30 40.#39 not #24 41.#39 or #27 or #9 42.explode "exertion/"/ all subheadings 43."physical fitness" 44.explode "physical education and training"/ all subheadings 45.explode "sports"/ all subheadings 46.explode "dancing"/ all subheadings 47.explode "exercise therapy"/ all subheadings 48.(physical$ adj5 (fit$ or train$ or activ$ or endur$)).tw. 49.(exercis$ adj5 (train$ or physical$ or activ$)).tw. 50.sport$.tw. 51.walk$.tw. 52.bicycle$.tw 53.(exercise$ adj aerobic$).tw. 54.(("lifestyle" or life‐style) adj5 activ$).tw. 55.(("lifestyle" or life‐style) adj5 physical$).tw. 56.#42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or (exercise$) or (aerobic$) or ("lifestyle") or (activ$) or ("lifestyle") or (life‐style) or (physical$) 57.health education 58.patient education 59.primary prevention 60.health promotion 61.behaviour therapy 62.cognitive therapy 63.primary health care 64.workplace 65.promot$.tw. 66.educat$.tw. 67.program$.tw. 68.#57 or #58 or #59 or #60 or #61 or #62 or #63 or #64 or #65 or #66 or #67 69.#68 and #56 70.#69 and #41
PsycLIT
1.exertion 2.physical‐fitness 3.exercise 4.explode exercise 5.sport 6.walk* 7.cycle 8.#1 or #2 or #3 or #4 or #5 or #6 or #7 9.health education 10.patient education 11.primary prevention 12.health promotion 13.behaviour therapy 14.cognitive therapy 15.primary health care 16.workplace 17.promot$.tw. 18.educat$.tw. 19.program$.tw. 20.#9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 21.#8 and #20 22.controlle 23.randomized 24.random‐assignment 25.double‐blind 26.single‐blind 27.#22 or #23 or #24 or #25 or #26 28.animal 29.human 30.#27 not #28 31.clinical 32.(clin* near trial*) in ti 33.clin* near trial*) in ab 34.(singl* or doubl* or trebl* or tripl*) near (blind* or mask*) 35.(#34 in ti) or (#34 in ab) 36.placebos 37.placebo* in ti 38.placebo* in ab 39.random* in ti 40.random* in ab 41.research‐methodology} 42.#31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 43.#39 or #40 or #41 44.#42 or #43 45.animal 46.human 47.#44 not #45 48.#47 or #30 or #29 or #46 49.comparative 50.study 51.#49 and #50 52.evaluation 53.studies 54.#52 and #53 55.follow‐up 56.propsective 57.#56 and #53 58.control* or prosepctiv* or volunteer* 59.(#58 in ti) or (#58 in ab) 60.#59 or #57 or #54 or #51 61.#60 not #45 62.#60 or #48 or #30 63.#62 and #21
SPORTDISCUS
1.'physical activity' 2.exercise 3.fitness 4.sedentary 5.housebound 6.aerobics or circuits or swimming or aqua or jogging or running or cycling or fitness or yoga or walking or sport 7.patient education 8.primary prevention 9.health promotion 10.behaviour therapy 11.cognitive therapy 12.primary health care 13.workplace 14.controlled 15.randomized 16.random‐assignment 17.double‐blind 18.single‐blind 19.clinical 20.placebos 21.comparative 22.evaluation 23.study
SIGLE
1.explode "Exertion/"/ all subheadings 2."Physical fitness" 3.explode "Physical education and training"/ all subheadings 4.explode "Sports"/ all subheadings 5.explode "Dancing"/ all subheadings 6.explode "Exercise therapy"/ all subheadings 7.(physical$ adj5 (fit$ or train$ or activ$ or endur$)).tw. 8.(exercis$ adj5 (train$ or physical$ or activ$)).tw. 9.sport$.tw. 10.walk$.tw. 11.bicycle$.tw 12.(exercise$ adj aerobic$).tw. 13.(("lifestyle" or life‐style) adj5 activ$).tw. 14.(("lifestyle" or life‐style) adj5 physical$).tw. 15.#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or (exercise$) or (aerobic$) or ("lifestyle") or (activ$) or ("lifestyle") or (life‐style) or (physical$) 16.Health Education 17.Patient education 18.Primary prevention 19.Health promotion 20.Behaviour therapy 21.Cognitive therapy 22.Primary health care 23.Workplace 24.promot$.tw. 25.educat$.tw. 26.program$.tw. 27.#16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 28.#15 and #27
SCISEARCH
1.((promot$ or uptake or encourag$ or increas$ or start) near (physical adj activity)) 2.(promot$ or uptake or encourag$ or increas$ or start) near exercise 3.(promot$ or uptake or encourag$ or increas$ or start) near (aerobics or circuits or swimming or aqua$) 4.(promot$ or uptake or encourag$ or increas$ or start) near (jogging or running or cycling) 5.(promot$ or uptake or encourag$ or increas$ or start) near ((keep adj fit) or (fitness adj class$) or yoga) 6.(promot$ or uptake or encourag$ or increas$ or start) near walking 7.(promot$ or uptake or encourag$ or increas$ or start) near sport$
Appendix 2. Search strategies 2012
CENTRAL
#1MeSH descriptor: [Physical Fitness] this term only #2MeSH descriptor: [Physical Exertion] this term only #3MeSH descriptor: [Physical Education and Training] explode all trees #4MeSH descriptor: [Sports] explode all trees #5MeSH descriptor: [Dancing] this term only #6MeSH descriptor: [Exercise Therapy] explode all trees #7physical* near activ* #8physical* near train* #9physical* near fit* #10exercise* near train* #11exercise* near activ* #12exercise* near physical* #13sport* #14walk* #15bicycle* #16exercise* near aerobic* #17((life next style*) near activ*) #18life‐style* near activ* #19lifestyle* near activ* #20((life next style*) near physical*) #21life‐style* near physical* #22lifestyle* near physical* #23#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 #24#12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 #25#23 or #24 #26MeSH descriptor: [Health Education] this term only #27MeSH descriptor: [Patient Education as Topic] this term only #28MeSH descriptor: [Primary Prevention] this term only #29MeSH descriptor: [Health Promotion] explode all trees #30MeSH descriptor: [Behavior Therapy] this term only #31MeSH descriptor: [Cognitive Therapy] this term only #32MeSH descriptor: [Primary Health Care] this term only #33MeSH descriptor: [Workplace] this term only #34promot* #35educat* #36program* #37#26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 #38#25 and #37
MEDLINE Ovid
1. Physical Exertion/ 2. Physical Fitness/ 3. exp "Physical Education and Training"/ 4. exp Sports/ 5. Dancing/ 6. exp Exercise Therapy/ 7. exp Exercise/ 8. (physical$ adj5 (fit$ or train$ or activ$ or endur$ or exertion$)).tw. 9. (exercis$ adj5 (train$ or physical$ or activ$)).tw. 10. sport$.tw. 11. walk$.tw. 12. bicycle$.tw. 13. ((exercise$ adj3 aerobic$) or aerobics).tw. 14. ((lifestyle or life‐style) adj5 activ$).tw. 15. ((lifestyle or life‐style) adj5 physical$).tw. 16. or/1‐15 17. Health Education/ 18. Patient Education as Topic/ 19. Primary Prevention/ 20. exp Health Promotion/ 21. Behavior Therapy/ 22. Cognitive Therapy/ 23. Primary Health Care/ 24. Workplace/ 25. promot$.tw. 26. educat$.tw. 27. program$.tw. 28. or/17‐27 29. 16 and 28 30. randomized controlled trial.pt. 31. controlled clinical trial.pt. 32. randomized.ab. 33. placebo.ab. 34. drug therapy.fs. 35. randomly.ab. 36. trial.ab. 37. groups.ab. 38. 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 39. exp animals/ not humans.sh. 40. 38 not 39 41. 29 and 40 42. (200412$ or 2005$ or 2006$ or 2007$ or 2008$ or 2009$ or 2010$ or 2011$ or 2012$).ed. 43. 41 and 42
EMBASE Ovid
1. exp exercise/ 2. fitness/ 3. physical education/ 4. exp sport/ 5. dancing/ 6. exp kinesiotherapy/ 7. (physical* adj5 (fit* or train* or activ* or endur* or exert*)).tw. 8. (exercis* adj5 (train* or physical* or activ*)).tw. 9. sport*.tw. 10. walk*.tw. 11. ((exercise* adj aerobic*) or aerobic*).tw. 12. ((lifestyle or life‐style) adj5 activ*).tw. 13. bicycle*.tw. 14. ((lifestyle or life‐style) adj5 physical*).tw. 15. or/1‐14 16. health education/ 17. patient education/ 18. primary prevention/ 19. health promotion/ 20. behavior therapy/ 21. cognitive therapy/ 22. primary health care/ 23. workplace/ 24. promot*.tw. 25. educat*.tw. 26. program*.tw. 27. or/16‐26 28. 15 and 27 29. random$.tw. 30. factorial$.tw. 31. crossover$.tw. 32. cross over$.tw. 33. cross‐over$.tw. 34. placebo$.tw. 35. (doubl$ adj blind$).tw. 36. (singl$ adj blind$).tw. 37. assign$.tw. 38. allocat$.tw. 39. volunteer$.tw. 40. crossover procedure/ 41. double blind procedure/ 42. randomized controlled trial/ 43. single blind procedure/ 44. 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 45. (animal/ or nonhuman/) not human/ 46. 44 not 45 47. 28 and 46 48. (200412* or 2005* or 2006* or 2007* or 2008* or 2009* or 2010* or 2011* or 2012*).dd. 49. 47 and 48 50. limit 49 to embase
CINAHL Plus with Full Text EBSCO
S34 S33 Limiters ‐ Exclude MEDLINE records S33 S31 and S32 S32 EM 20041201‐20121010 S31 S20 and S30 S30 S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 S29 TX allocat* S28 TX control* S27 TX assign* S26 TX placebo* S25 (MH "Placebos") S24 TX random* S23 TX (clinic* N1 trial?) S22 PT clinical trial S21 (MH "Clinical Trials+") S20 S10 and S19 S19 S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 S18 (TI promot* or educat* or program*) or (AB promot* or educat* or program*) S17 (MH "Work Environment") S16 (MH "Primary Health Care") S15 (MH "Behavior Therapy+") S14 (MH "Health Promotion") S13 (MH "Preventive Health Care") S12 (MH "Patient Education") S11 (MH "Health Education") S10 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 S9 (TI sport* or walk* or bicycle* or exercis* or aerobic*) or (AB sport* or walk* or bicycle* or exercis* or aerobic*) S8 (TI physical N5 (fit* or train* or activ* or endur* or exert*)) or (AB physcial* N5 (fit* or train* or activ* or endur* or exert*)) S7 (TI exercis* N5 (train* or physical* or activ*)) or (AB exercis* N5 (train* or physical* or activ*)) S6 (MH "Exercise+") or (MH "Therapeutic Exercise+") S5 (TI (lifestyle* or life‐style*) N5 (activ* or physical*)) or (AB (lifestyle* or life‐style*) N5 (activ* or physical*)) S4 (MH "Sports+") or (MH "Dancing+") S3 (MH "Physical Education and Training") S2 (MH "Physical Fitness") S1 (MH "Exertion")
PsycINFO
1. exp exercise/ 2. physical fitness/ 3. physical activity/ 4. exp sports/ 5. physical education/ 6. (physical$ adj5 (fit$ or train$ or activ$ or endur$ or exertion$)).tw. 7. (exercis$ adj5 (train$ or physical$ or activ$)).tw. 8. sport$.tw. 9. walk$.tw. 10. bicycle$.tw. 11. ((exercise$ adj3 aerobic$) or aerobics).tw. 12. ((lifestyle or life‐style) adj5 activ$).tw. 13. ((lifestyle or life‐style) adj5 physical$).tw. 14. or/1‐13 15. health education/ 16. client education/ 17. health promotion/ 18. prevention/ 19. primary health care/ 20. behavior therapy/ 21. cognitive therapy/ 22. cognitive behavior therapy/ 23. workplace*.tw. 24. promot$.tw. 25. educat$.tw. 26. program$.tw. 27. or/15‐26 28. 14 and 27 29. random*.tw. 30. trial.ab. 31. groups.ab. 32. factorial$.tw. 33. crossover$.tw. 34. cross over$.tw. 35. cross‐over$.tw. 36. placebo$.tw. 37. assign$.tw. 38. allocat$.tw. 39. volunteer$.tw. 40. clinical trials/ 41. (doubl$ adj blind$).tw. 42. (singl$ adj blind$).tw. 43. or/29‐42 44. 28 and 43 45. (200412* or 2005* or 2006* or 2007* or 2008* or 2009* or 2010* or 2011* or 2012*).up. 46. 44 and 45
Web of Science
# 20 #19 AND #18 # 19 TS=(random* or blind* or allocat* or assign* or trial* or placebo* or crossover* or cross‐over*) # 18 #17 AND #8 # 17 #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 # 16 TI=(promot* or educat* or program*) # 15 TS=(workplace) # 14 TS=(primary health care) # 13 TS=(cognitive therap*) # 12 TS=((behaviour or behavior) NEAR/2 therap*) # 11 TS=(health NEAR/2 promot*) # 10 TS=(primary prevent*) # 9 TS=((health educat*) or (patient* educat*)) # 8 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 # 7 TS=((lifestyle* or life‐style*) NEAR/5 (activ* or physcial*)) # 6 TS=((exercis* NEAR/2 aerobic*) or aerobic*) # 5 TS=(sport* or danc* or walk* or bicycle*) # 4 TS=(physical* educat*) # 3 TS=(exercis* NEAR/5 (train* or physical* or activ*)) # 2 TS=(physical NEAR/5 (fit* or train* or activ* or endur* or exert*)) # 1 TS=(exercis* therap*)
Data and analyses
Comparison 1. Face‐to‐face interventions versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cardiorespiratory fitness: 12 months | 2 | 349 | Std. Mean Difference (IV, Random, 95% CI) | 0.50 [0.28, 0.71] |
| 2 Dichotomous outcomes: 12 months | 3 | 3277 | Odds Ratio (IV, Random, 95% CI) | 1.52 [0.88, 2.61] |
| 3 Dichotomous outcomes: 24 months | 1 | 2701 | Odds Ratio (IV, Random, 95% CI) | 1.19 [1.02, 1.39] |
| 4 Self reported physical activity: 12 months | 8 | 6725 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [0.06, 0.31] |
| 5 Self reported physical activity: 24 months | 3 | 4235 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.10, 0.46] |
Comparison 2. Face‐to‐face interventions versus control (risk of bias score ≥ 50%).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cardiorespiratory fitness: 12 months | 1 | 149 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [0.24, 0.89] |
| 2 Dichotomous outcomes: 12 months | 1 | 2853 | Odds Ratio (IV, Random, 95% CI) | 1.13 [0.96, 1.33] |
| 3 Dichotomous outcomes: 24 months | 1 | 2701 | Odds Ratio (IV, Random, 95% CI) | 1.19 [1.02, 1.39] |
| 4 Self reported physical activity: 12 months | 3 | 5511 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.05, 0.15] |
| 5 Self reported physical activity: 24 months | 1 | 3691 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.05, 0.08] |
Comparison 3. Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Delivery: individual | 4 | 5801 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.04, 0.27] |
| 2 Delivery: mixed (individual and group) | 4 | 924 | Std. Mean Difference (IV, Random, 95% CI) | 0.27 [0.14, 0.40] |
| 3 Implementer: health professional | 3 | 4145 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.15, 0.48] |
| 4 Implementer: non‐health professional | 5 | 2580 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [0.06, 0.35] |
| 5 Physical activity type: specified | 3 | 609 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [0.17, 0.49] |
| 6 Physical activity type: not specified | 5 | 6116 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.01, 0.25] |
| 7 Prescribed physical activity: supervised | 2 | 445 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [0.14, 0.51] |
| 8 Prescribed physical activity: unsupervised | 6 | 6280 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [0.01, 0.27] |
| 9 Intervention: includes theory based counselling | 4 | 2274 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.02, 0.44] |
| 10 Intervention: does not include theory based counselling | 4 | 4451 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.01, 0.37] |
3.8. Analysis.

Comparison 3 Face‐to‐face interventions versus control (subgroup analysis ‐ self reported physical activity: 12 months), Outcome 8 Prescribed physical activity: unsupervised.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aittasalo 2004.
| Methods | ||
| Participants | Workplace employees from nine different sites | |
| Interventions | The participant’s current LTPA was assessed by a trained nurse and an individual goal for PA was set. All participants were given a supplementary leaflet about PA, developed for the contemplation and preparation stages, plus a written weekly PA plan and a self monitoring PA diary for the next follow‐up visit. At the follow‐up visits (after 8 weeks, 6 and 12 months) progress was reviewed and, if necessary, modified. During all the visits, emphasis was put on strengthening the participant’s positive impressions of their capability to follow the plan (self‐efficacy). Three fitness test were also administered at baseline, 6 and 12 months. | |
| Outcomes | Self‐reported PA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Clear presentation of participant numbers at each stage of trial |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcomes reported |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were analysed |
| Other bias | Low risk | Validated outcome measures |
Calfas 2000.
| Methods | ||
| Participants | Primary care patients | |
| Interventions | Participants received a 15 week cognitive behavioural education course, which comprised 15 x 50 minute lectures followed by 15 x 110 minute laboratory experiences that were led by peer health facilitators and included practice of behavioural management strategies as homework. Participants received two course credits and could attend two supervised exercise sessions per week. All participants received monthly follow‐up phone calls and monthly written materials for 15 months. | |
| Outcomes | Self‐reported PA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Clear presentation of participant numbers at each stage of trial |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcomes reported |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were analysed |
| Other bias | Unclear risk | Validated outcome measures |
Cunningham 1987.
| Methods | ||
| Participants | Retirees from community centre | |
| Interventions | Participants received 3 group exercise sessions per week and were encouraged to do one additional home based session | |
| Outcomes | Self‐reported PA Cardio‐respiratory fitness |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participant numbers were not clearly reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All outcomes reported |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were analysed |
| Other bias | Unclear risk | Fitness assessment reliability reported |
Grandes 2011.
| Methods | ||
| Participants | Primary care patients | |
| Interventions | Physician delivered brief advice and educational materials within a 15 minute intervention, plus an individualised PA plan. The intervention was supported by web based software to prompt and guide the physician and patient session | |
| Outcomes | Self‐reported PA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Authors reported a total of 70 family physicians as allocation units from 13 health centres that were randomised before patient recruitment, in a 1:1 ratio using computer generated random numbers provided by a central site. Baseline characteristics of these participants were balanced between both comparison groups with regard to the primary and secondary outcomes, as well as to the majority of sociodemographic and risk factors |
| Allocation concealment (selection bias) | High risk | Randomisation of physicians before patient recruitment prevented concealment of the patient enrolment process |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Clear presentation of participant numbers at each stage of trial |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Trained nurses working in exercise laboratories who performed baseline and follow‐up measurements at 6, 12 and 24 months were blinded to the allocation group of the participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcomes reported |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were analysed |
| Other bias | Low risk | Validated outcome measures |
Harland 1999.
| Methods | ||
| Participants | Primary care patients | |
| Interventions | All participants completed a baseline assessment of self‐reported PA, physical measures and cycle ergometer fitness test. They received feedback on their results, brief advice about their present level of PA and comparison to recommended levels, plus written health information, 19 leaflets about local PA facilities and activities. In addition, each participant was allocated to one of four intervention groups: (i) one motivational interview; (ii) one motivational interview plus vouchers for free use of local facilities; (iii) 6 motivational interviews over 12 weeks; and (iv) 6 motivational interviews over 12 weeks plus vouchers. | |
| Outcomes | Self‐reported PA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | After their baseline assessment, participants were randomised in blocks of 10. They chose blind from a set of 10 randomly ordered cards corresponding to intervention or control groups and were allocated to the group drawn. Baseline characteristics were evenly distributed in control and intervention groups |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participant numbers were clearly reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blinded to the allocation group of the participants |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All outcomes reported |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were analysed |
| Other bias | Low risk | ITT but the outcome measure used by Harland 1999 did not report any measurement metrics and was adapted from a national survey tool |
Hillsdon 2002.
| Methods | ||
| Participants | Primary care patients | |
| Interventions | Participants received brief negotiation plus follow‐up phone calls, or direct advice plus phone calls | |
| Outcomes | Self‐reported PA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation performed by independently in monthly batches which produced balanced groups at baseline |
| Allocation concealment (selection bias) | Low risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participant numbers were clearly reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Assessor knew allocation status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcomes reported |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were analysed |
| Other bias | Low risk | Validated outcome measures, ITT |
Katz 2008.
| Methods | ||
| Participants | Primary care patients | |
| Interventions | Participants received five sessions of the Pressure Systems Model. This comprised tailored counselling based on motivational interviewing plus handout materials addressing barriers to PA | |
| Outcomes | Self‐reported PA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated but no significant (P > 0.05) differences were observed in gender, illness/injury/disability and PA between the intervention and control sites at baseline. However, marital status, race and education level differed significantly (P < 0.05) between the intervention and control sites at baseline |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All outcomes reported |
| Selective reporting (reporting bias) | High risk | All outcomes stated were analysed |
| Other bias | High risk | Validated outcome measures |
King 1991.
| Methods | ||
| Participants | Inactive community older volunteers aged 50‐65 years | |
| Interventions | Participants received baseline physiological assessments and then were prescribed group based training at high intensity plus written information, PA logs and phone calls. They attedned local exercise classes at least three times per week for 12 months. Telephone calls were made once a week for the first four weeks, twice a week for the next four weeks and then once a month for 12 months. | |
| Outcomes | Cardio‐respiratory fitness | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned to one of the four exercise training conditions using a computerised version of the Efron procedure |
| Allocation concealment (selection bias) | High risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Clear presentation of participant numbers at each stage of trial |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessment staff were blind to the results of the subjects' previous visits |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All outcomes reported |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were analysed |
| Other bias | Low risk | Validated outcome measures |
Kriska 1986.
| Methods | ||
| Participants | Older women | |
| Interventions | Participants received a baseline physical assessment, eight week walking training programme with organised walks and then a choice of group or independent walking. Participants monitored their walking with monthly logs and were also offered social meetings. Participants also received follow‐up phone calls, cards, and incentives to maintain compliance. | |
| Outcomes | Self‐reported PA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Does not describe dropout numbers |
| Selective reporting (reporting bias) | Unclear risk | Some outcomes were analysed |
| Other bias | Low risk | Validated outcome measures |
Stewart 2001.
| Methods | ||
| Participants | Health maintenance organisation members | |
| Interventions | Participants received social cognitive theory based counselling to develop and maintain their own PA routine using locally available resources. They also attended informational meetings, individual planning sessions, monthly group workshops that were augmented by PA diaries, telephone calls, newsletters, and functional fitness assessments. Participants were strongly encouraged to attend the first two of 10 workshops where a walking clinic was offered. | |
| Outcomes | Self‐reported PA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated but none of the measures differed significantly at baseline |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Clear presentation of participant numbers at each stage of trial |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All outcomes reported but as graphs |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated were analysed |
| Other bias | Low risk | Validated outcome measures |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aggarwal 2010 | Multiple risk factor intervention |
| Aittasalo 2006 | Less than 12 months follow‐up |
| Akiyama 2007 | Less than 12 months follow‐up |
| Albright 2005 | No appropriate control or intervention group |
| Albright 2012 | No appropriate control or intervention group |
| Andersen 2012 | Less than 12 months follow‐up |
| Anderson 2005 | No appropriate control or intervention group |
| Armit 2005 | Less than 12 months follow‐up |
| Armit 2009 | Less than 12 months follow‐up |
| Baker 2008 | No appropriate control or intervention group |
| Baker 2008a | No appropriate control or intervention group |
| Baker 2011 | Less than 12 months follow‐up |
| Baruth 2010 | More than 20% loss to follow‐up |
| Baruth 2010a | No appropriate control or intervention group |
| Bennett 2008 | Less than 12 months follow‐up |
| Berlant 2004 | No appropriate control or intervention group |
| Bowen 2006 | No appropriate control or intervention group |
| Buman 2011 | No appropriate control or intervention group |
| Caperchione 2006 | No appropriate control or intervention group |
| Carr 2012 | Less than 12 months intervention |
| Carroll 2010 | Less than 12 months intervention |
| Castro 2011 | Remote and web 2.0 intervention |
| Cheung 2008 | Less than 12 months intervention |
| Connell 2009 | Insufficient data |
| Cox 2006 | Study aim irrelevant |
| Cox 2008 | Study aim irrelevant |
| Cox 2011 | Study aim irrelevant |
| Cox 2011a | Study aim irrelevant |
| Crain 2010 | Remote and web 2.0 intervention |
| de Vreede 2007 | Less than 12 months follow‐up |
| Dorgo 2009 | Less than 12 months follow‐up |
| Dorgo 2011 | Less than 12 months follow‐up |
| Dubbert 2002 | Less than 12 months follow‐up |
| Duncan 2005 | No appropriate control or intervention group |
| Duru 2010 | Less than 12 months follow‐up |
| Elley 2003 | Remote and web 2.0 intervention |
| Elley 2004 | Remote and web 2.0 intervention |
| Elley 2011 | Remote and web 2.0 intervention |
| Estabrooks 2011 | Less than 12 months follow‐up |
| Evers 2012 | Less than 12 months follow‐up |
| Farmandbar 2012 | Insufficient data |
| Ferney 2009 | Less than 12 months follow‐up |
| Findorff 2007 | Inappropriate primary outcome |
| Finni 2011 | No appropriate control or intervention group |
| Fitzsimons 2008 | No appropriate control or intervention group |
| Fitzsimons 2012 | No appropriate control or intervention group |
| Fortier 2007 | Less than 12 months follow‐up |
| Fortier 2007a | Less than 12 months follow‐up |
| Fortier 2011 | Less than 12 months follow‐up |
| Fortier 2011a | Less than 12 months follow‐up |
| Freene 2011 | No appropriate control or intervention group |
| French 2011 | Less than 12 months follow‐up |
| Froehlich‐Grobe 2012 | More than 10% of participants with a pre‐existing medical condition |
| Fujita 2003 | Less than 12 months follow‐up |
| Fukuoka 2011 | No appropriate control or intervention group |
| Gine‐Garriga 2009 | More than 10% of participants with a pre‐existing medical condition |
| Godin 2010 | Less than 12 months follow‐up |
| Goldstein 1999 | Less than 12 months follow‐up |
| Greaney 2008 | Multiple risk factor intervention |
| Green 2002 | Less than 12 months follow‐up |
| Hardcastle 2012 | Non‐randomised study |
| Hardeman 2011 | Remote and web 2.0 intervention |
| Harrison 2005 | More than 10% of participants with a pre‐existing medical condition |
| Havenar 2007 | More than 20% loss to follow‐up |
| Heesch 2004 | Face‐to‐face versus remote and web 2.0 interventions |
| Herrera‐Sanchez 2006 | Multiple risk factor intervention |
| Hind 2010 | Less than 12 months follow‐up |
| Hosper 2008 | Non‐randomised study |
| Hovell 2008 | Multiple risk factor intervention |
| Hughes 2009 | Less than 12 months follow‐up |
| Inoue 2003 | Less than 12 months follow‐up |
| Isaacs 2007 | Less than 12 months follow‐up |
| Jimmy 2005 | Non‐randomised study |
| Jolly 2009 | Less than 12 months follow‐up |
| Juneau 1987 | Less than 12 months follow‐up |
| Kerse 2005 | Remote and web 2.0 intervention |
| King 1988 | Less than 12 months follow‐up |
| King 2006 | No appropriate control or intervention group |
| King 2007 | Remote and web 2.0 intervention |
| Kinmonth 2008 | Remote and web 2.0 intervention |
| Kolt 2007 | Remote and web 2.0 intervention |
| Kolt 2009 | No appropriate control or intervention group |
| Kolt 2012 | No appropriate control or intervention group |
| Kriska 2012 | Study aim irrelevant |
| Lamb 2002 | No appropriate control or intervention group |
| Lawton 2008 | Remote and web 2.0 intervention |
| Lawton 2009 | Remote and web 2.0 intervention |
| LeCheminant 2011 | Less than 12 months follow‐up |
| Leung 2012 | No appropriate control or intervention group |
| Lombard 1995 | Less than 12 months follow‐up |
| Macmillan 2011 | Less than 12 months follow‐up |
| Marcus 2007 | No appropriate control or intervention group |
| Marcus 2007a | No appropriate control or intervention group |
| Marcus 2007b | Remote and web 2.0 intervention |
| Marcus 2007c | Remote and web 2.0 intervention |
| Marshall 2003 | Less than 12 months follow‐up |
| Marshall 2004 | Less than 12 months follow‐up |
| Martinson 2008 | Remote and web 2.0 intervention |
| Martinson 2010 | Remote and web 2.0 intervention |
| McAuley 2007 | No appropriate control or intervention group |
| McAuley 2012 | Remote and web 2.0 intervention |
| McEachan 2011 | No appropriate control or intervention group |
| McGowan 2009 | Less than 12 months follow‐up |
| McGowan 2009a | Less than 12 months follow‐up |
| McMurdo 2010 | Less than 12 months follow‐up |
| Merom 2007 | Less than 12 months follow‐up |
| Muda 2006 | Less than 12 months follow‐up |
| Murphy 2010 | More than 10% of participants with a pre‐existing medical condition |
| Napolitano 2006 | Remote and web 2.0 intervention |
| Napolitano 2010 | Remote and web 2.0 intervention |
| Newton 2004 | Less than 12 months follow‐up |
| Nichols 2000 | Less than 12 months follow‐up |
| Nies 2006 | No appropriate control or intervention group |
| Norris 2000 | Less than 12 months follow‐up |
| Norton 2011 | Non‐randomised study |
| Opdenacker 2008 | More than 20% loss to follow‐up |
| Opdenacker 2011 | More than 20% loss to follow‐up |
| Oppert 2007 | Less than 12 months follow‐up |
| Paasche‐Orlow 2012 | No appropriate control or intervention group |
| Papandonatos 2012 | Remote and web 2.0 intervention |
| Peels 2012 | Remote and web 2.0 intervention |
| Pekmezi 2009 | Less than 12 months follow‐up |
| Pekmezi 2010 | No appropriate control or intervention group |
| Petrella 2003 | No appropriate control or intervention group |
| Petrella 2006 | More than 20% loss to follow‐up |
| Petrella 2010 | No appropriate control or intervention group |
| Pinto 2002 | Less than 12 months follow‐up |
| Pinto 2005 | Less than 12 months follow‐up |
| Plotnikoff 2007 | More than 20% loss to follow‐up |
| Plotnikoff 2010 | More than 20% loss to follow‐up |
| Poulsen 2007 | More than 20% loss to follow‐up |
| Prestwich 2012 | Less than 12 months follow‐up |
| Ransdell 2004 | Less than 12 months follow‐up |
| Reed 2008 | Less than 12 months follow‐up |
| Reid 1979 | Less than 12 months follow‐up |
| Resnick 2002 | Less than 12 months follow‐up |
| Rose 2007 | Remote and web 2.0 intervention |
| Sarkisian 2010 | No appropriate control or intervention group |
| Schneider 2011 | No appropriate control or intervention group |
| Sevick 2007 | Remote and web 2.0 intervention |
| Sheeran 2012 | Less than 12 months follow‐up |
| Sherwood 2008 | Remote and web 2.0 intervention |
| Simons‐Morton 2001 | No appropriate control or intervention group |
| Skar 2011 | Less than 12 months follow‐up |
| Slootmaker 2005 | Less than 12 months follow‐up |
| Smith 2000 | Less than 12 months follow‐up |
| Sorensen 2007 | Less than 12 months follow‐up |
| Sorensen 2008 | Less than 12 months follow‐up |
| Spittaels 2007 | Less than 12 months follow‐up |
| Spittaels 2007a | Less than 12 months follow‐up |
| Steele 2007 | Less than 12 months follow‐up |
| Steele 2009 | Less than 12 months follow‐up |
| Stevens 1998 | Less than 12 months follow‐up |
| Talbot 2010 | Less than 12 months follow‐up |
| Talbot 2011 | Less than 12 months follow‐up |
| Tan 2006 | Less than 12 months follow‐up |
| Taylor 2005 | Less than 12 months follow‐up |
| Thogersen‐Ntoumani 2010 | Less than 12 months follow‐up |
| Thomas 2012 | No appropriate control or intervention group |
| Vainionpää 2007 | Study aim irrelevant |
| van Sluijs 2006 | Less than 12 months follow‐up |
| van Stralen 2008 | Remote and web 2.0 intervention |
| van Stralen 2009 | Remote and web 2.0 intervention |
| van Stralen 2009a | Remote and web 2.0 intervention |
| van Stralen 2010 | Remote and web 2.0 intervention |
| van Stralen 2011 | Remote and web 2.0 intervention |
| Visek 2011 | Less than 12 months follow‐up |
| von Thiele 2008 | Study aim irrelevant |
| Wadsworth 2010 | Less than 12 months follow‐up |
| Wanner 2009 | No appropriate control or intervention group |
| Wanner 2010 | No appropriate control or intervention group |
| Watkinson 2010 | Less than 12 months follow‐up |
| Whitehead 2007 | Less than 12 months follow‐up |
| Wilcox 2007 | More than 20% loss to follow‐up |
| Williams 2004 | Remote and web 2.0 intervention |
| Williams 2006 | Remote and web 2.0 intervention |
| Williams 2011 | No appropriate control or intervention group |
| Wilson 2009 | Less than 12 months follow‐up |
Characteristics of ongoing studies [ordered by study ID]
Iliffe 2010.
| Trial name or title | ProAct 65+ trial |
| Methods | Pragmatic 3 arm parallel design cluster controlled trial |
| Participants | Older adults aged 65 years and over |
| Interventions | Class based exercise (FAME), home based exercise (OEP) and usual care |
| Outcomes | Achievement of recommended PA targets |
| Starting date | 2010 |
| Contact information | Professor S Iliffe, Department of Primary Care & Population Health, University College London, Rowland Hill St, London NW3 2PF, UK. s.iliffe@pcps.ucl.ac.uk |
| Notes |
Wilson 2010.
| Trial name or title | "Positive Action for Today's Health" (PATH) trial |
| Methods | Cluster randomised controlled trial (three communities matched on census tract information ‐ crime, PA, ethnic minorities, and income) |
| Participants | Adults aged 18 year or older who are residents of three communities |
| Interventions | The three communities have been randomised to receive one of the three interventions: an intervention that combines a police‐patrolled‐walking program with a social marketing intervention, a police‐patrolled walking program only, or no‐walking related intervention (general health education only) |
| Outcomes | Objective assessment of PA using Actical min MVPA/day, assessed at 12, 18 and 24 months |
| Starting date | 2010 |
| Contact information | Professor D Wilson, Department of Psychology, University of South Carolina, Columbia, SC 29208, United States. wilsondk@mailbox.sc.edu |
| Notes |
Differences between protocol and review
Study selection
The six month follow‐up period was extended to 12 months in response to the recommendations from the previous versions of this review, which called for better study quality with longer follow‐up periods (Foster 2005a).
Data extraction
The identified authors undertaking this task were modified.
Assessing the risk of bias
The identified authors undertaking this task were modified and the criteria for completing this task were explicitly identified.
Unit of analysis
The method for dealing with multiple intervention arms in a study was changed and these arms were not compared to a split control group. Instead, the relevant intervention arms were combined for comparison against the existing control group using established approaches (Higgins 2011).
Subgroup analysis
The following refinements were made to the subgroup analysis based on the data that were available in the identified studies.
The inclusion of a comparison of group versus individual versus mixed (group and individual) was removed from the primary outcome measures section and more appropriately included as a subgroup analysis. This comparison also became a secondary rather than a primary objective.
The prescription of the intervention was changed to focus on whether the type of PA was specified, and if theory based counselling was included.
The intensity of the intervention delivery was changed to focus on whether the PA participation was directly supervised.
Sensitivity analysis
The threshold for 'low' risk was specified as meeting at least 50% of the applicable risk of bias criteria.
Contributions of authors
All named authors contributed to the conceptual planning of this suite of reviews to update the previously completed Cochrane review assessing 'Interventions for promoting physical activity' (Foster 2005a). This manuscript was initially drafted by Justin Richards and Charlie Foster. Editorial contributions were received from Margaret Thorogood and Melvyn Hillsdon.
Sources of support
Internal sources
British Heart Foundation Core Grant (021/P&C/Core/2010/HPRG), UK.
External sources
NIHR Cochrane Incentive Scheme 2012, UK.
Declarations of interest
Melvyn Hillsdon has received a research council grant to investigate the feasibility of a primary care PA intervention. This was not a study of outcomes and therefore had no bearing on this review. He has been a member of a NICE programme development group on walking and cycling and was paid for travel expenses.
New
References
References to studies included in this review
Aittasalo 2004 {published data only}
- Aittasalo M, Miilunpalo S, Suni J. The effectiveness of physical activity counseling in a work‐site setting. A randomized, controlled trial. Patient Education and Counseling 2004;55(2):193‐202. [DOI] [PubMed] [Google Scholar]
Calfas 2000 {published data only}
- Calfas KJ, Sallis JF, Nichols JF, Sarkin JA, Johnson MF, Caparosa S, et al. Project GRAD: two‐year outcomes of a randomized controlled physical activity intervention among young adults. Graduate Ready for Activity Daily. American Journal of Preventive Medicine 2000;18(1):28‐37. [DOI] [PubMed] [Google Scholar]
Cunningham 1987 {published data only}
- Cunningham DA, Rechnitzer PA, Howard JH, Donner AP. Exercise training of men at retirement: a clinical trial. Journal of Gerontology 1987;42(1):17‐23. [DOI] [PubMed] [Google Scholar]
Grandes 2011 {published data only}
- Grandes G, Sanchez A, Montoya I, Ortega Sanchez‐Pinilla R, Torcal J. Two‐year longitudinal analysis of a cluster randomized trial of physical activity promotion by general practitioners. PLoS ONE 2011; Vol. 6, issue 3:e18363. [DOI] [PMC free article] [PubMed]
- Grandes G, Sanchez A, Sanchez‐Pinilla RO, Torcal J, Montoya I, Lizarraga K, et al. Effectiveness of physical activity advice and prescription by physicians in routine primary care: a cluster randomized trial. Archives of Internal Medicine 2009;169(7):694‐701. [DOI] [PubMed] [Google Scholar]
- Grandes G, Sanchez A, Torcal J, Sanchez‐Pinilla RO, Lizarraga K, Serra J, et al. Targeting physical activity promotion in general practice: Characteristics of inactive patients and willingness to change. BMC Public Health 2008;8:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harland 1999 {published data only}
- Harland J, White M, Drinkwater C, Chinn D, Farr L, Howel D. The Newcastle exercise project: a randomised controlled trial of methods to promote physical activity in primary care. BMJ 1999;319(7213):828‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hillsdon 2002 {published data only}
- Hillsdon M, Thorogood M, White I, Foster C. Advising people to take more exercise is ineffective: a randomized controlled trial of physical activity promotion in primary care. International Journal of Epidemiology 2002;31(4):808‐15. [DOI] [PubMed] [Google Scholar]
Katz 2008 {published data only}
- Katz DL, Shuval K, Comerford BP, Faridi Z, Njike VY. Impact of an educational intervention on internal medicine residents' physical activity counselling: the Pressure System Model. Journal of Evaluation in Clinical Practice 2008;14(2):294‐9. [DOI] [PubMed] [Google Scholar]
King 1991 {published data only}
- King AC, Haskell WL, Taylor CB, Kraemer HC, DeBusk RF. Group‐ vs home‐based exercise training in healthy older men and women. A community‐based clinical trial. JAMA 1991;266(11):1535‐42. [PubMed] [Google Scholar]
Kriska 1986 {published data only}
- Kriska AM, Bayles C, Cauley JA, LaPorte RE, Sandler RB, Pambianco G. A randomized exercise trial in older women: increased activity over two years and the factors associated with compliance. Medicine and Science in Sports and Exercise 1986;18(5):557‐62. [PubMed] [Google Scholar]
Stewart 2001 {published data only}
- Stewart AL, Verboncoeur CJ, McLellan BY, Gillis DE, Rush S, Mills KM, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2001;56(8):M465‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Aggarwal 2010 {published data only}
- Aggarwal B, Liao M, Mosca L. Predictors of physical activity at 1 year in a randomized controlled trial of family members of patients with cardiovascular disease. Journal of Cardiovascular Nursing 2010;25(6):444‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aittasalo 2006 {published data only}
- Aittasalo M, Miilunpalo S, Kukkonen‐Harjula K, Pasanen M. A randomized intervention of physical activity promotion and patient self‐monitoring in primary health care. Preventive Medicine 2006;42(1):40‐6. [DOI] [PubMed] [Google Scholar]
Akiyama 2007 {published data only}
- Akiyama Y, Furuichi M, Miyachi M, Takeda N, Sakai K, Oka K, et al. Effect of individual feedback information in a correspondece course type walking program based on behavioral science. Japanese Journal of Physical Fitness and Sports Medicine 2007;56(1):157‐65. [Google Scholar]
Albright 2005 {published data only}
- Albright C L, Pruitt L, Castro C, Gonzalez A, Woo S, King AC. Modifying physical activity in a multiethnic sample of low‐income women: one‐year results from the IMPACT (Increasing Motivation for Physical ACTivity) project. Annals of Behavioral Medicine 2005;30(3):191‐200. [DOI] [PubMed] [Google Scholar]
Albright 2012 {published data only}
- Albright CL, Steffen AD, Novotny R, Nigg CR, Wilkens LR, Saiki K, et al. Baseline results from Hawaii's Na Mikimiki Project: a physical activity intervention tailored to multiethnic postpartum women. Women & Health 2012;52:265‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andersen 2012 {published data only}
- Andersen E, Burton NW, Anderssen S A. Physical activity levels six months after a randomised controlled physical activity intervention for Pakistani immigrant men living in Norway. International Journal of Behavioral Nutrition and Physical Activity 2012;9:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anderson 2005 {published data only}
- Anderson RT, King A, Stewart AL, Camacho F, Rejeski WJ. Physical activity counseling in primary care and patient well‐being: Do patients benefit?. Annals of Behavioral Medicine 2005;30(2):146‐54. [DOI] [PubMed] [Google Scholar]
Armit 2005 {published data only}
- Armit CM, Brown WJ, Ritchie CB, Trost SG. Promoting physical activity to older adults: a preliminary evaluation of three general practice‐based strategies. Journal of Science & Medicine in Sport 2005;8(4):446‐50. [DOI] [PubMed] [Google Scholar]
Armit 2009 {published data only}
- Armit CM, Brown WJ, Marshall AL, Ritchie CB, Trost SG, Green A, et al. Randomized trial of three strategies to promote physical activity in general practice. Preventive Medicine 2009;48(2):156‐63. [DOI] [PubMed] [Google Scholar]
Baker 2008 {published data only}
- Baker G, Gray SR, Wright A, Fitzsimons C, Nimmo M, Lowry R, et al. The effect of a pedometer‐based community walking intervention "Walking for Wellbeing in the West" on physical activity levels and health outcomes: a 12‐week randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2008; Vol. 5, issue 1:44. [DOI] [PMC free article] [PubMed]
Baker 2008a {published data only}
- Baker G, Mutrie N, Lowry R. Using pedometers as motivational tools: Are goals set in steps more effective than goals set in minutes for increasing walking?. International Journal of Health Promotion and Education 2008;46(1):21‐6. [Google Scholar]
Baker 2011 {published data only}
- Baker G, Mutrie N, Lowry R. A comparison of goals set in steps using a pedometer and goals set in minutes: A randomized controlled trial. International Journal of Health Promotion and Education 2011;49(2):60‐8. [Google Scholar]
Baruth 2010 {published data only}
- Baruth M, Wilcox S, Blair S, Hooker S, Hussey J, Saunders R. Psychosocial mediators of a faith‐based physical activity intervention: implications and lessons learned from null findings. Health Education Research 2010;25(4):645‐55. [DOI] [PubMed] [Google Scholar]
Baruth 2010a {published data only}
- Baruth M, Wilcox S, Dunn AL, King AC, Marcus BH, Rejeski WJ, et al. Psychosocial mediators of physical activity and fitness changes in the activity counseling trial. Annals of Behavioral Medicine 2010;39(3):274‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bennett 2008 {published data only}
- Bennett JA, Young HM, Nail LM, Winters‐Stone K, Hanson G. A telephone‐only motivational intervention to increase physical activity in rural adults: a randomized controlled trial. Nursing Research 2008;57(1):24‐32. [DOI] [PubMed] [Google Scholar]
Berlant 2004 {published data only}
- Berlant NE. Increasing adherence to an exercise intervention. Dissertation Abstracts International: Section B: The Sciences and Engineering 2004;65(5‐B):2612. [Google Scholar]
Bowen 2006 {published data only}
- Bowen DJ, Fesinmeyer MD, Yasui Y, Tworoger S, Ulrich CM, Irwin M L, et al. Randomized trial of exercise in sedentary middle aged women: Effects on quality of life. International Journal of Behavioral Nutrition and Physical Activity 2006; Vol. 3:34. [DOI] [PMC free article] [PubMed]
Buman 2011 {published data only}
- Buman MP, Giacobbi PR Jr, Dzierzewski JM, Aiken Morgan A, McCrae CS, Roberts BL, et al. Peer volunteers improve long‐term maintenance of physical activity with older adults: a randomized controlled trial. Journal of Physical Activity & Health 2011;8 Suppl 2:S257‐66. [PMC free article] [PubMed] [Google Scholar]
Caperchione 2006 {published data only}
- Caperchione C, Mummery K. The utilisation of group process strategies as an intervention tool for the promotion of health‐related physical activity in older adults. Activities, Adaptation & Aging 2006;30(4):29‐45. [Google Scholar]
Carr 2012 {published data only}
- Carr LJ, Dunsiger SI, Lewis B, Ciccolo JT, Hartman S, Bock B, et al. Randomized Controlled Trial Testing an Internet Physical Activity Intervention for Sedentary Adults. Health Psychology 2012;32:328‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carroll 2010 {published data only}
- Carroll JK, Lewis BA, Marcus BH, Lehman EB, Shaffer ML, Sciamanna CN. Computerized tailored physical activity reports. A randomized controlled trial. American Journal of Preventive Medicine 2010;39(2):148‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Castro 2011 {published data only}
- Castro CM, Pruitt LA, Buman MP, King AC. Physical activity program delivery by professionals versus volunteers: the TEAM randomized trial. Health Psychology 2011;30(3):285‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cheung 2008 {published data only}
- Cheung PPY, Chow BC, Parfitt G. Using environmental stimuli in physical activity intervention for school teachers: a pilot study. International Electronic Journal of Health Education 2008;11:1‐10. [Google Scholar]
Connell 2009 {published data only}
- Connell CM, Janevic MR. Effects of a telephone‐based exercise intervention for dementia caregiving wives: a randomized controlled trial. Journal of Applied Gerontology 2009; Vol. 28, issue 2:171‐94. [DOI] [PMC free article] [PubMed]
Cox 2006 {published data only}
- Cox KL, Burke V, Beilin LJ, Grove JR, Blanksby BA, Puddey IB. Blood pressure rise with swimming versus walking in older women: the Sedentary Women Exercise Adherence Trial 2 (SWEAT 2). Journal of Hypertension 2006;24:307‐14. [DOI] [PubMed] [Google Scholar]
Cox 2008 {published data only}
- Cox KL, Burke V, Beilin LJ, Derbyshire AJ, Grove JR, Blanksby BA, et al. Short and long‐term adherence to swimming and walking programs in older women ‐ The Sedentary Women Exercise Adherence Trial (SWEAT 2). Preventive Medicine 2008;46(6):511‐7. [DOI] [PubMed] [Google Scholar]
Cox 2011 {published data only}
- Cox K, Kane E, Burke V, Beilin L. Effects of education and motivational interviewing on short and long‐term participation in a home‐based physical activity program. Journal of Science and Medicine in Sport 2011;14:e13. [Google Scholar]
Cox 2011a {published data only}
- Cox K, Kane E, Burke V, Phillips M, Beilin L. Long‐term effects of 6‐months of home‐based physical activity and counselling on the mental health of older adults: The MOVES study. Journal of Science and Medicine in Sport 2011;14:e14‐5. [Google Scholar]
Crain 2010 {published data only}
- Crain AL, Martinson BC, Sherwood NE, O'Connor PJ. The long and winding road to physical activity maintenance. American Journal of Health Behavior 2010;34:764‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
de Vreede 2007 {published data only}
- Vreede PL, Meeteren NL, Samson MM, Wittink HM, Duursma SA, Verhaar HJ. The effect of functional tasks exercise and resistance exercise on health‐related quality of life and physical activity. A randomised controlled trial. Gerontology 2007;53(1):12‐20. [DOI] [PubMed] [Google Scholar]
Dorgo 2009 {published data only}
- Dorgo S, King GA, Brickey GD. The application of peer mentoring to improve fitness in older adults. Journal of Aging & Physical Activity 2009;17:344‐61. [DOI] [PubMed] [Google Scholar]
Dorgo 2011 {published data only}
- Dorgo S, King GA, Bader JO, Limon JS. Comparing the effectiveness of peer mentoring and student mentoring in a 35‐week fitness program for older adults. Archives of Gerontology & Geriatrics 2011;52(3):344‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dubbert 2002 {published data only}
- Dubbert PM, Cooper KM, Kirchner KA, Meydrech EF, Bilbrew D. Effects of nurse counseling on walking for exercise in elderly primary care patients. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2002;57(11):M733‐40. [DOI] [PubMed] [Google Scholar]
Duncan 2005 {published data only}
- Duncan GE, Anton SD, Sydeman SJ, Newton RL Jr, Corsica JA, Durning PE, et al. Prescribing exercise at varied levels of intensity and frequency: a randomized trial. Archives of Internal Medicine 2005;165(20):2362‐9. [DOI] [PubMed] [Google Scholar]
Duru 2010 {published data only}
- Duru OK, Sarkisian CA, Leng M, Mangione CM. Sisters in motion: a randomized controlled trial of a faith‐based physical activity intervention. Journal of the American Geriatrics Society 2010;58(10):1863‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elley 2003 {published data only}
- Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ 2003;326(7393):793. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elley 2004 {published data only}
- Elley CR, Kerse N, Arroll B, Swinburn B, Ashton T, Robinson E. Cost‐effectiveness of physical activity counselling in general practice. New Zealand Medical Journal 2004;117(1207):U1216. [PubMed] [Google Scholar]
Elley 2011 {published data only}
- Elley CR, Garrett S, Rose SB, O'Dea D, Lawton BA, Moyes SA, et al. Cost‐effectiveness of exercise on prescription with telephone support among women in general practice over 2 years. British Journal of Sports Medicine 2011;45(15):1223‐9. [DOI] [PubMed] [Google Scholar]
Estabrooks 2011 {published data only}
- Estabrooks PA, Smith‐Ray RL, Almeida FA, Hill J, Gonzales M, Schreiner P, et al. Move More: Translating an efficacious group dynamics physical activity intervention into effective clinical practice. International Journal of Sport & Exercise Psychology 2011;9:4‐18. [Google Scholar]
Evers 2012 {published data only}
- Evers A, Klusmann V, Ziegelmann J P, Schwarzer R, Heuser I. Long‐term adherence to a physical activity intervention: the role of telephone‐assisted vs. self‐administered coping plans and strategy use. Psychology & Health 2012;27:784‐97. [DOI] [PubMed] [Google Scholar]
Farmandbar 2012 {published data only}
- Farmandbar RA, Niknami SH, Heydarnia AR. Effect of an integrated transtheoretical model and self‐determination theory on the promotion and maintenance of exercise behavior. Journal of Guilan University of Medical Sciences 2012;20(82):1. [Google Scholar]
Ferney 2009 {published data only}
- Ferney SL, Marshall AL, Eakin EG, Owen N. Randomized trial of a neighborhood environment‐focused physical activity website intervention. Preventive Medicine 2009;48(2):144‐50. [DOI] [PubMed] [Google Scholar]
Findorff 2007 {published data only}
- Findorff MJ, Stock HH, Gross CR, Wyman JF. Does the Transtheoretical Model (TTM) explain exercise behavior in a community‐based sample of older women?. Journal of Aging & Health 2007;19(6):985‐1003. [DOI] [PubMed] [Google Scholar]
Finni 2011 {published data only}
- Finni T, Saakslahti A, Laukkanen A, Pesola A, Sipila S. A family based tailored counselling to increase non‐exercise physical activity in adults with a sedentary job and physical activity in their young children: design and methods of a year‐long randomized controlled trial. BMC Public Health 2011;11:944. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fitzsimons 2008 {published data only}
- Fitzsimons CF, Baker G, Wright A, Nimmo MA, Ward Thompson C, Lowry R, et al. The 'Walking for Wellbeing in the West' randomised controlled trial of a pedometer‐based walking programme in combination with physical activity consultation with 12 month follow‐up: rationale and study design. BMC Public Health 2008;8:259. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fitzsimons 2012 {published data only}
- Fitzsimons CF, Baker G, Gray SR, Nimmo MA, Mutrie N, Scottish Physical Activity Research. Does physical activity counselling enhance the effects of a pedometer‐based intervention over the long‐term: 12‐month findings from the Walking for Wellbeing in the West study. BMC Public Health 2012;12:206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fortier 2007 {published data only}
- Fortier MS, Hogg W, O'Sullivan TL, Blanchard C, Reid RD, Sigal RJ, et al. The physical activity counselling (PAC) randomized controlled trial: rationale, methods, and interventions. Applied Physiology, Nutrition, & Metabolism = Physiologie Appliquee, Nutrition et Metabolisme 2007;32:1170‐85. [DOI] [PubMed] [Google Scholar]
Fortier 2007a {published data only}
- Fortier MS, Sweet SN, O'Sullivan TL, Williams GC. A self‐determination process model of physical activity adoption in the context of a randomized controlled trial. Psychology of Sport and Exercise 2007;8:741‐57. [Google Scholar]
Fortier 2011 {published data only}
- Fortier MS, Hogg W, O'Sullivan TL, Blanchard C, Sigal RJ, Reid RD, et al. Impact of integrating a physical activity counsellor into the primary health care team: physical activity and health outcomes of the Physical Activity Counselling randomized controlled trial. Applied Physiology, Nutrition, & Metabolism = Physiologie Appliquee, Nutrition et Metabolisme 2011;36(4):503‐14. [DOI] [PubMed] [Google Scholar]
Fortier 2011a {published data only}
- Fortier MS, Wiseman E, Sweet SN, O'Sullivan TL, Blanchard CM, Sigal RJ, et al. A moderated mediation of motivation on physical activity in the context of the Physical Activity Counseling randomized control trial. Psychology of Sport and Exercise 2011;12:71‐8. [Google Scholar]
Freene 2011 {published data only}
- Freene N, Waddington G, Chesworth W, Davey R, Goss J. 'Physical activity at home (PAAH)', evaluation of a group versus home based physical activity program in community dwelling middle aged adults: rationale and study design. BMC Public Health 2011;11:883. [DOI] [PMC free article] [PubMed] [Google Scholar]
French 2011 {published data only}
- French DP, Williams SL, Michie S, Taylor C, Szczepura A, Stallard N, et al. A cluster randomised controlled trial of the efficacy of a brief walking intervention delivered in primary care: study protocol. BMC Family Practice 2011;12:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Froehlich‐Grobe 2012 {published data only}
- Froehlich‐Grobe K, Aaronson LS, Washburn RA, Little T D, Lee J, Nary DE, et al. An exercise trial for wheelchair users: project workout on wheels. Contemporary Clinical Trials 2012;33:351‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fujita 2003 {published data only}
- Fujita K, Nagatomi R, Hozawa A, Ohkubo T, Sato K, Anzai Y, et al. Effects of exercise training on physical activity in older people: a randomized controlled trial. Journal of Epidemiology 2003;13(2):120‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fukuoka 2011 {published data only}
- Fukuoka Y, Komatsu J, Suarez L, Vittinghoff E, Haskell W, Noorishad T, et al. The mPED randomized controlled clinical trial: applying mobile persuasive technologies to increase physical activity in sedentary women protocol. BMC Public Health 2011;11:933. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gine‐Garriga 2009 {published data only}
- Gine‐Garriga M, Martin C, Puig‐Ribera A, Anton JJ, Guiu A, Cascos A, et al. Referral from primary care to a physical activity programme: establishing long‐term adherence? A randomized controlled trial. Rationale and study design. BMC Public Health 2009;9:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Godin 2010 {published data only}
- Godin G, Belanger‐Gravel A, Amireault S, Gallani MC, Vohl MC, Perusse L. Effect of implementation intentions to change behaviour: moderation by intention stability. Psychological Reports 2010;106(1):147‐59. [DOI] [PubMed] [Google Scholar]
Goldstein 1999 {published data only}
- Goldstein MG, Pinto BM, Marcus BH, Lynn H, Jette AM, Rakowski W, et al. Physician‐based physical activity counseling for middle‐aged and older adults: a randomized trial. Annals of Behavioral Medicine 1999;21(1):40‐7. [DOI] [PubMed] [Google Scholar]
Greaney 2008 {published data only}
- Greaney ML, Riebe D, Ewing Garber C, Rossi JS, Lees FD, Burbank PA, et al. Long‐term effects of a stage‐based intervention for changing exercise intentions and behavior in older adults. Gerontologist 2008;48(3):358‐67. [DOI] [PubMed] [Google Scholar]
Green 2002 {published data only}
- Green BB, McAfee T, Hindmarsh M, Madsen L, Caplow M, Buist D. Effectiveness of telephone support in increasing physical activity levels in primary care patients. American Journal of Preventive Medicine 2002;22(3):177‐83. [DOI] [PubMed] [Google Scholar]
Hardcastle 2012 {published data only}
- Hardcastle S, Blake N, Hagger MS. The effectiveness of a motivational interviewing primary‐care based intervention on physical activity and predictors of change in a disadvantaged community. Journal of Behavioral Medicine 2012;35:318‐33. [DOI] [PubMed] [Google Scholar]
Hardeman 2011 {published data only}
- Hardeman W, Kinmonth AL, Michie S, Sutton S. Theory of planned behaviour cognitions do not predict self‐reported or objective physical activity levels or change in the ProActive trial. British Journal of Health Psychology 2011;16(Pt 1):135‐50. [DOI] [PubMed] [Google Scholar]
Harrison 2005 {published data only}
- Harrison RA, Roberts C, Elton PJ. Does primary care referral to an exercise programme increase physical activity one year later? A randomized controlled trial. Journal of Public Health 2005;27(1):25‐32. [DOI] [PubMed] [Google Scholar]
Havenar 2007 {published data only}
- Havenar J. Adapted motivational interviewing for increasing physical activity: A 12 month clinical trial. Dissertation Abstracts International: Section B: The Sciences and Engineering 2007;68(4‐B):2291. [Google Scholar]
Heesch 2004 {published data only}
- Heesch K, Masse LC, Frankowski RF, Dunn AI. Adherence Within and Between Lifestyle Physical Activity Groups in Project PRIME. Journal of Physical Activity & Health 2004;1:29‐44. [Google Scholar]
Herrera‐Sanchez 2006 {published data only}
- Herrera‐Sanchez B, Mansilla‐Dominguez JM, Perdigon‐Florencio P, Bermejo‐Caja C. Efectiveness of clinical counseling after increasing physical activity. A prospective randomized study. Medicina Clinica 2006;126(10):361‐3. [DOI] [PubMed] [Google Scholar]
Hind 2010 {published data only}
- Hind D, Scott EJ, Copeland R, Breckon JD, Crank H, Walters SJ, et al. A randomised controlled trial and cost‐effectiveness evaluation of "booster" interventions to sustain increases in physical activity in middle‐aged adults in deprived urban neighbourhoods. BMC Public Health 2010;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hosper 2008 {published data only}
- Hosper K, Deutekom M, Stronks PK. The effectiveness of "Exercise on Prescription" in stimulating physical activity among women in ethnic minority groups in the Netherlands: protocol for a randomized controlled trial. BMC Public Health 2008;8:406. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hovell 2008 {published data only}
- Hovell MF, Mulvihill MM, Buono MJ, Liles S, Schade DH, Washington TA, et al. Culturally tailored aerobic exercise intervention for low‐income Latinas. American Journal of Health Promotion 2008;22(3):155‐63. [DOI] [PubMed] [Google Scholar]
Hughes 2009 {published data only}
- Hughes SL, Seymour RB, Campbell RT, Whitelaw N, Bazzarre T. Best‐practice physical activity programs for older adults: findings from the national impact study. American Journal of Public Health 2009;99(2):362‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Inoue 2003 {published data only}
- Inoue S, Odagiri Y, Wakui S, Katoh R, Moriguchi T, Ohya Y. Randomized controlled trial to evaluate the effect of a physical activity intervention program based on behavioural medicine. Journal of Tokyo Medical University 2003; Vol. 61:154‐65.
Isaacs 2007 {published data only}
- Isaacs AJ, Critchley JA, Tai SS, Buckingham K, Westley D, Harridge SDR, et al. Exercise evaluation randomised trial (EXERT): A randomised trial comparing GP referral for leisure centre‐based exercise, community‐based walking and advice only. Health Technology Assessment 2007;11(10):iii‐104. [DOI] [PubMed] [Google Scholar]
Jimmy 2005 {published data only}
- Jimmy G, Martin BW. Implementation and effectiveness of a primary care based physical activity counselling scheme. Patient Education & Counseling 2005;56(3):323‐31. [DOI] [PubMed] [Google Scholar]
Jolly 2009 {published data only}
- Jolly K, Duda JL, Daley A, Eves FF, Mutrie N, Ntoumanis N, et al. Evaluation of a standard provision versus an autonomy promotive exercise referral programme: rationale and study design. BMC Public Health 2009;9:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Juneau 1987 {published data only}
- Juneau M, Rogers F, Santos V, Yee M, Evans A, Bohn A, et al. Effectiveness of self‐monitored, home‐based, moderate‐intensity exercise training in middle‐aged men and women. American Journal of Cardiology 1987;60(1):66‐70. [DOI] [PubMed] [Google Scholar]
Kerse 2005 {published data only}
- Kerse N, Elley CR, Robinson E, Arroll B. Is physical activity counseling effective for older people? A cluster randomized, controlled trial in primary care. Journal of the American Geriatrics Society 2005;53(11):1951‐6. [DOI] [PubMed] [Google Scholar]
King 1988 {published data only}
- King AC, Taylor CB, Haskell WL, Debusk RF. Strategies for increasing early adherence to and long‐term maintenance of home‐based exercise training in healthy middle‐aged men and women. American Journal of Cardiology 1988;61(8):628‐32. [DOI] [PubMed] [Google Scholar]
King 2006 {published data only}
King 2007 {published data only}
- King AC, Friedman R, Marcus B, Castro C, Napolitano M, Ahn D, et al. Ongoing physical activity advice by humans versus computers: the Community Health Advice by Telephone (CHAT) trial. Health Psychology 2007;26(6):718‐27. [DOI] [PubMed] [Google Scholar]
Kinmonth 2008 {published data only}
- Kinmonth AL, Wareham NJ, Hardeman W, Sutton S, Prevost AT, Fanshawe T, et al. Efficacy of a theory‐based behavioural intervention to increase physical activity in an at‐risk group in primary care (ProActive UK): a randomised trial. Lancet 2008;371(9606):41‐8. [DOI] [PubMed] [Google Scholar]
Kolt 2007 {published data only}
- Kolt GS, Schofield GM, Kerse N, Garrett N, Oliver M. Effect of telephone counseling on physical activity for low‐active older people in primary care: a randomized, controlled trial. Journal of the American Geriatrics Society 2007;55(7):986‐92. [DOI] [PubMed] [Google Scholar]
Kolt 2009 {published data only}
- Kolt GS, Schofield GM, Kerse N, Garrett N, Schluter PJ, Ashton T, et al. The healthy steps study: a randomized controlled trial of a pedometer‐based green prescription for older adults. Trial protocol. BMC Public Health 2009;9:404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kolt 2012 {published data only}
- Kolt GS, Schofield GM, Kerse N, Garrett N, Ashton T, Patel A. Healthy Steps trial: pedometer‐based advice and physical activity for low‐active older adults. Annals of Family Medicine 2012;10(3):206‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kriska 2012 {published data only}
- Kriska A, Rockette‐Wagner B, Bray GA, Florez H, Edelstein S, Reddy D, et al. Impact of lifestyle intervention on sedentary time in subjects at high‐risk for diabetes. Diabetes 2012;61:A48‐9. [Google Scholar]
Lamb 2002 {published data only}
- Lamb SE, Bartlett HP, Ashley A, Bird W. Can lay‐led walking programmes increase physical activity in middle aged adults? A randomised controlled trial. Journal of Epidemiology and Community Health 2002;56(4):246‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lawton 2008 {published data only}
- Lawton BA, Rose SB, Elley CR, Dowell AC, Fenton A, Moyes SA. Exercise on prescription for women aged 40‐74 recruited through primary care: two year randomised controlled trial. BMJ 2008;337:a2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lawton 2009 {published data only}
- Lawton BA, Rose SB, Elley CR, Dowell AC, Fenton A, Moyes SA. Exercise on prescription for women aged 40 to 74 recruited through primary care: two year randomised controlled trial [with consumer summary]. British Journal of Sports Medicine 2009; Vol. 43, issue 2:120‐3. [PubMed]
LeCheminant 2011 {published data only}
- LeCheminant JD, Smith JD, Covington NK, Hardin‐Renschen T, Heden T. Pedometer use in university freshmen: a randomized controlled pilot study. American Journal of Health Behavior 2011;35(6):777‐84. [DOI] [PubMed] [Google Scholar]
Leung 2012 {published data only}
- Leung W, Ashton T, Kolt GS, Schofield GM, Garrett N, Kerse N, et al. Cost‐effectiveness of pedometer‐based versus time‐based Green Prescriptions: The Healthy Steps Study. Australian Journal of Primary Health 2012;18(3):204‐11. [DOI] [PubMed] [Google Scholar]
Lombard 1995 {published data only}
- Lombard DN, Lombard TN, Winett RA. Walking to meet health guidelines: the effect of prompting frequency and prompt structure. Health Psychology 1995;14(2):164‐70. [DOI] [PubMed] [Google Scholar]
Macmillan 2011 {published data only}
- Macmillan F, Fitzsimons C, Black K, Granat MH, Grant MP, Grealy M, et al. West End Walkers 65+: a randomised controlled trial of a primary care‐based walking intervention for older adults: study rationale and design. BMC Public Health 2011;11:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marcus 2007 {published data only}
- Marcus BH, Lewis BA, Williams DM, Dunsiger S, Jakicic JM, Whiteley JA, et al. A comparison of Internet and print‐based physical activity interventions. Archives of Internal Medicine 2007;167(9):944‐9. [DOI] [PubMed] [Google Scholar]
Marcus 2007a {published data only}
- Marcus BH, Lewis BA, Williams DM, Whiteley JA, Albrecht AE, Jakicic JM, et al. Step into Motion: a randomized trial examining the relative efficacy of Internet vs. print‐based physical activity interventions. Contemporary Clinical Trials 2007;28(6):737‐47. [DOI] [PubMed] [Google Scholar]
Marcus 2007b {published data only}
- Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht A, et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychology 2007;26(4):401‐9. [DOI] [PubMed] [Google Scholar]
Marcus 2007c {published data only}
- Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht AE, et al. Examination of print and telephone channels for physical activity promotion: Rationale, design, and baseline data from Project STRIDE. Contemporary Clinical Trials 2007;28(1):90‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marshall 2003 {published data only}
- Marshall AL, Bauman AE, Owen N, Booth ML, Crawford D, Marcus BH. Population‐based randomized controlled trial of a stage‐targeted physical activity intervention. Annals of Behavioral Medicine 2003;25(3):194‐202. [DOI] [PubMed] [Google Scholar]
Marshall 2004 {published data only}
- Marshall AL, Bauman AE, Owen N, Booth ML, Crawford D, Marcus BH. Reaching out to promote physical activity in Australia: a statewide randomized controlled trial of a stage‐targeted intervention. American Journal of Health Promotion 2004;18(4):283‐7. [DOI] [PubMed] [Google Scholar]
Martinson 2008 {published data only}
- Martinson BC, Crain AL, Sherwood NE, Hayes M, Pronk NP, O'Connor PJ. Maintaining physical activity among older adults: six‐month outcomes of the Keep Active Minnesota randomized controlled trial. Preventive Medicine 2008;46(2):111‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martinson 2010 {published data only}
- Martinson BC, Sherwood NE, Crain AL, Hayes MG, King AC, Pronk NP, et al. Maintaining physical activity among older adults: 24‐month outcomes of the Keep Active Minnesota randomized controlled trial. Preventive Medicine 2010;51(1):37‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
McAuley 2007 {published data only}
- McAuley E, Morris KS, Motl RW, Hu L, Konopack JF, Elavsky S. Long‐term follow‐up of physical activity behavior in older adults. Health Psychology 2007;26(3):375‐80. [DOI] [PubMed] [Google Scholar]
McAuley 2012 {published data only}
- McAuley E, Wojcicki TR, White SM, Mailey EL, Szabo AN, Gothe N, et al. Physical activity, function, and quality of life: design and methods of the FlexToBa trial. Contemporary Clinical Trials 2012;33:228‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
McEachan 2011 {published data only}
- McEachan RR, Lawton RJ, Jackson C, Conner M, Meads DM, West RM. Testing a workplace physical activity intervention: a cluster randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2011;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
McGowan 2009 {published data only}
- McGowan E, Prapavessis H, Podolinsky N, Gray C, Elkayam J. The effect of a self‐efficacy intervention on objective measures of physical activity in first and second‐degree relatives of colon cancer patients. Psycho‐Oncology 2009;18:S255‐6. [Google Scholar]
McGowan 2009a {published data only}
- McGowan E, Prapavessis H, Podolinsky N, Gray C, Elkayam J. Examining the relationships between self‐efficacy and objective measures of physical activity behavior in first‐ and second‐degree relatives of colon cancer patients. Psycho‐Oncology 2009;18:S73‐4. [Google Scholar]
McMurdo 2010 {published data only}
- McMurdo MET, Sugden J, Argo I, Boyle P, Johnston DW, Sniehotta FF, et al. Do pedometers increase physical activity in sedentary older women? A randomized controlled trial. Journal of the American Geriatrics Society 2010;58(11):2099‐106. [DOI] [PubMed] [Google Scholar]
Merom 2007 {published data only}
- Merom D, Rissel C, Phongsavan P, Smith BJ, Kemenade C, Brown WJ, et al. Promoting walking with pedometers in the community ‐ The step‐by‐step trial. American Journal of Preventive Medicine 2007;32:290‐7. [DOI] [PubMed] [Google Scholar]
Muda 2006 {published data only}
- Muda S H, Kadir AAbd. The effectiveness of physical activity counseling in Primary Care Clinic. University Science Malaysia Hospital 2006; Vol. 13, issue 4:249‐53.
Murphy 2010 {published data only}
- Murphy S, Raisanen L, Moore G, Edwards RT, Linck P, Williams N, et al. A pragmatic randomised controlled trial of the Welsh National Exercise Referral Scheme: protocol for trial and integrated economic and process evaluation. BMC Public Health 2010; Vol. 10:352. [DOI] [PMC free article] [PubMed]
Napolitano 2006 {published data only}
- Napolitano MA, Whiteley JA, Papandonatos G, Dutton G, Farrell NC, Albrecht A, et al. Outcomes from the women's wellness project: a community‐focused physical activity trial for women. Preventive Medicine 2006;43(6):447‐53. [DOI] [PubMed] [Google Scholar]
Napolitano 2010 {published data only}
- Napolitano MA, Borradaile KE, Lewis BA, Whiteley JA, Longval JL, Parisi AF, et al. Accelerometer use in a physical activity intervention trial. Contemporary Clinical Trials 2010; Vol. 31, issue 6:514‐23. [DOI] [PMC free article] [PubMed]
Newton 2004 {published data only}
- Newton RL Jr, Perri MG. A randomized pilot trial of exercise promotion in sedentary African‐American adults. Ethnicity & Disease 2004;14(4):548‐57. [PubMed] [Google Scholar]
Nichols 2000 {published data only}
- Nichols JF, Wellman E, Caparosa S, Sallis JF, Calfas KJ, Rowe R. Impact of a worksite behavioral skills intervention. American Journal of Health Promotion 2000;14(4):218‐21, ii. [DOI] [PubMed] [Google Scholar]
Nies 2006 {published data only}
- Nies M A, Partridge T. Comparison of 3 interventions to increase walking in sedentary women. American Journal of Health Behavior 2006;30:339‐52. [DOI] [PubMed] [Google Scholar]
Norris 2000 {published data only}
- Norris SL, Grothaus LC, Buchner DM, Pratt M. Effectiveness of physician‐based assessment and counseling for exercise in a staff model HMO. Preventive Medicine 2000;30(6):513‐23. [DOI] [PubMed] [Google Scholar]
Norton 2011 {published data only}
- Norton LH, Norton KI, Lewis N, Dollman J. A comparison of two short‐term intensive physical activity interventions: methodological considerations. International Journal of Behavioral Nutrition and Physical Activity 2011;8:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Opdenacker 2008 {published data only}
- Opdenacker J, Boen F, Coorevits N, Delecluse C. Effectiveness of a lifestyle intervention and a structured exercise intervention in older adults. Preventive Medicine 2008;46(6):518‐24. [DOI] [PubMed] [Google Scholar]
Opdenacker 2011 {published data only}
- Opdenacker J, Delecluse C, Boen F. A 2‐year follow‐up of a lifestyle physical activity versus a structured exercise intervention in older adults. Journal of the American Geriatrics Society 2011;59(9):1602‐11. [DOI] [PubMed] [Google Scholar]
Oppert 2007 {published data only}
- Oppert JM, Tafflet M, Fourchaud L, Lommez A, Bailleul C, Borys JM, et al. Physical activity promotion in insufficiently active adults: a randomised trial based on telephone counseling. International Journal of Obesity 2007;31:S214. [Google Scholar]
Paasche‐Orlow 2012 {published data only}
- Paasche‐Orlow M, Silliman R, Winter M, Cheng D, Henault L, Bickmore T. Efficacy of a computer‐based intervention to promote walking in older adults. Journal of the American Geriatrics Society 2012;60:S4. [DOI] [PubMed] [Google Scholar]
Papandonatos 2012 {published data only}
- Papandonatos GD, Williams DM, Jennings EG, Napolitano MA, Bock BC, Dunsiger S, et al. Mediators of physical activity behavior change: Findings from a 12‐month randomized controlled trial. Health Psychology 2012;31(4):512‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peels 2012 {published data only}
- Peels DA, Stralen MM, Bolman C, Golsteijn RH, Vries H, Mudde AN, et al. Development of web‐based computer‐tailored advice to promote physical activity among people older than 50 years. Journal of Medical Internet Research 2012;14:e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pekmezi 2009 {published data only}
- Pekmezi DW, Neighbors CJ, Lee CS, Gans KM, Bock BC, Morrow KM, et al. A culturally adapted physical activity intervention for Latinas: a randomized controlled trial. American Journal of Preventive Medicine 2009;37(6):495‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pekmezi 2010 {published data only}
- Pekmezi DW, Williams DM, Dunsiger S, Jennings EG, Lewis BA, Jakicic JM, et al. Feasibility of using computer‐tailored and internet‐based interventions to promote physical activity in underserved populations. Telemedicine Journal & E‐Health 2010;16(4):498‐503. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petrella 2003 {published data only}
- Petrella RJ, Koval JJ, Cunningham DA, Paterson DH. Can primary care doctors prescribe exercise to improve fitness? The Step Test Exercise Prescription (STEP) project. American Journal of Preventive Medicine 2003;24(4):316‐22. [DOI] [PubMed] [Google Scholar]
Petrella 2006 {published data only}
- Petrella R. Cost effectiveness of a community‐based exercise program for older adults. Clinical Journal of Sport Medicine 2006;16:191‐3. [PubMed] [Google Scholar]
Petrella 2010 {published data only}
- Petrella RJ, Lattanzio CN, Shapiro S, Overend T. Improving aerobic fitness in older adults: effects of a physician‐based exercise counseling and prescription program. Canadian Family Physician 2010;56(5):e191‐200. [PMC free article] [PubMed] [Google Scholar]
Pinto 2002 {published data only}
- Pinto BM, Friedman R, Marcus BH, Kelley H, Tennstedt S, Gillman MW. Effects of a computer‐based, telephone‐counseling system on physical activity. American Journal of Preventive Medicine 2002;23(2):113‐20. [DOI] [PubMed] [Google Scholar]
Pinto 2005 {published data only}
- Pinto BM, Goldstein MG, Ashba J, Sciamanna CN, Jette A. Randomized controlled trial of physical activity counseling for older primary care patients. American Journal of Preventive Medicine 2005;29(4):247‐55. [DOI] [PubMed] [Google Scholar]
Plotnikoff 2007 {published data only}
- Plotnikoff RC, Brunet S, Courneya KS, Spence JC, Birkett NJ, Marcus B, et al. The efficacy of stage‐matched and standard public health materials for promoting physical activity in the workplace: the Physical Activity Workplace Study (PAWS). American Journal of Health Promotion 2007;21(6):501‐9. [DOI] [PubMed] [Google Scholar]
Plotnikoff 2010 {published data only}
- Plotnikoff RC, Pickering MA, Rhodes RE, Courneya KS, Spence JC. A test of cognitive mediation in a 12‐month physical activity workplace intervention: Does it explain behaviour change in women?. International Journal of Behavioral Nutrition and Physical Activity 2010;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Poulsen 2007 {published data only}
- Poulsen T, Elkjaer E, Vass M, Hendriksen C, Avlund K. Promoting physical activity in older adults by education of home visitors. European Journal of Ageing 2007;4(3):115‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prestwich 2012 {published data only}
- Prestwich A, Conner MT, Lawton RJ, Ward JK, Ayres K, McEachan RR. Randomized controlled trial of collaborative implementation intentions targeting working adults' physical activity. Health Psychology 2012;31(4):486‐95. [DOI] [PubMed] [Google Scholar]
Ransdell 2004 {published data only}
- Ransdell LB, Robertson LA, Ornes L, Moyer‐Mileur L. Generations exercising together to improve fitness (GET FIT): A pilot study designed to increase physical activity and improve health‐related fitness in three generations of women. Women and Health 2004;40(3):77‐94. [DOI] [PubMed] [Google Scholar]
Reed 2008 {published data only}
- Reed J, Malvern L, Muthukrishnan S, Hardy R, King L. An ecological approach with primary‐care counseling to promote physical activity. Journal of Physical Activity & Health 2008;5(1):169‐83. [DOI] [PubMed] [Google Scholar]
Reid 1979 {published data only}
- Reid EL, Morgan RW. Exercise prescription: a clinical trial. American Journal of Public Health 1979;69(6):591‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Resnick 2002 {published data only}
- Resnick B. Testing the effect of the WALC intervention on exercise adherence in older adults. Journal of Gerontological Nursing 2002;28(6):40‐9. [DOI] [PubMed] [Google Scholar]
Rose 2007 {published data only}
- Rose SB, Lawton BA, Elley CR, Dowell AC, Fenton AJ. The 'Women's Lifestyle Study', 2‐year randomized controlled trial of physical activity counselling in primary health care: rationale and study design. BMC Public Health 2007;7:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sarkisian 2010 {published data only}
- Sarkisian C, Trejo L, Mangione C, Wang PC, Frank J, Prohaska T. A randomized controlled trial of a behavioral intervention to increase walking among older latinos. Journal of General Internal Medicine 2010;25:S212‐3. [Google Scholar]
Schneider 2011 {published data only}
- Schneider JK, Cook JH, Luke DA. Unexpected effects of cognitive‐behavioural therapy on self‐reported exercise behaviour and functional outcomes in older adults. Age & Ageing 2011;40(2):163‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sevick 2007 {published data only}
- Sevick MA, Napolitano MA, Papandonatos GD, Gordon AJ, Reiser LM, Marcus BH. Cost‐effectiveness of alternative approaches for motivating activity in sedentary adults: results of Project STRIDE. Preventive Medicine 2007;45(1):54‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sheeran 2012 {published data only}
- Sheeran P, Harris P, Vaughan J, Oettingen G, Gollwitzer PM. Gone exercising: Mental contrasting promotes physical activity among overweight, middle‐aged, low‐SES fishermen. Health Psychology Aug 2012;32:802‐9. [DOI] [PubMed] [Google Scholar]
Sherwood 2008 {published data only}
- Sherwood NE, Martinson BC, Crain AL, Hayes MG, Pronk NP, O'Connor PJ. A new approach to physical activity maintenance: rationale, design, and baseline data from the Keep Active Minnesota Trial. BMC Geriatrics 2008;8:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simons‐Morton 2001 {published data only}
- Simons‐Morton DG, Blair SN, King AC, TM Morgan, WB Applegate, O'Toole M, et al. Effects of physical activity counseling in primary care: the Activity Counseling Trial: a randomized controlled trial. JAMA 2001;286(6):677‐87. [DOI] [PubMed] [Google Scholar]
Skar 2011 {published data only}
- Skar S, Sniehotta FF, Molloy GJ, Prestwich A, Araujo‐Soares V. Do brief online planning interventions increase physical activity amongst university students? A randomised controlled trial. Psychology & Health 2011;26:399‐417. [DOI] [PubMed] [Google Scholar]
Slootmaker 2005 {published data only}
- Slootmaker SM, Chin A, Paw MJ, Schuit AJ, Seidell JC, Mechelen W. Promoting physical activity using an activity monitor and a tailored web‐based advice: design of a randomized controlled trial [ISRCTN93896459]. BMC Public Health 2005;5:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2000 {published data only}
- Smith BJ, Bauman AE, Bull FC, Booth ML, Harris MF. Promoting physical activity in general practice: a controlled trial of written advice and information materials. British Journal of Sports Medicine 2000;34(4):262‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sorensen 2007 {published data only}
- Sorensen JB, Kragstrup J, Kjaer K, Puggaard L. Exercise on prescription: trial protocol and evaluation of outcomes. BMC Health Services Research 2007;7:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sorensen 2008 {published data only}
- Sorensen JB, Kragstrup J, Skovgaard T, Puggaard L. Exercise on prescription: a randomized study on the effect of counseling vs counseling and supervised exercise. Scandinavian Journal of Medicine & Science in Sports 2008;18(3):288‐97. [DOI] [PubMed] [Google Scholar]
Spittaels 2007 {published data only}
- Spittaels H, Bourdeaudhuij I, Brug J, Vandelanotte C. Effectiveness of an online computer‐tailored physical activity intervention in a real‐life setting. Health Education Research 2007;22(3):385‐96. [DOI] [PubMed] [Google Scholar]
Spittaels 2007a {published data only}
- Spittaels H, Bourdeaudhuij I, Vandelanotte C. Evaluation of a website‐delivered computer‐tailored intervention for increasing physical activity in the general population. Preventive Medicine 2007;44(3):209‐17. [DOI] [PubMed] [Google Scholar]
Steele 2007 {published data only}
- Steele R, Mummery WK, Dwyer T. Using the Internet to promote physical activity: a randomized trial of intervention delivery modes. Journal of Physical Activity & Health 2007;4(3):245‐60. [DOI] [PubMed] [Google Scholar]
Steele 2009 {published data only}
- Steele RM, Mummery WK, Dwyer T. A comparison of face‐to‐face or internet‐delivered physical activity intervention on targeted determinants. Health Education & Behavior 2009;36:1051‐64. [DOI] [PubMed] [Google Scholar]
Stevens 1998 {published data only}
- Stevens W, Hillsdon M, Thorogood M, McArdle D. Cost‐effectiveness of a primary care based physical activity intervention in 45‐74 year old men and women: a randomised controlled trial. British Journal of Sports Medicine 1998;32(3):236‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Talbot 2010 {published data only}
- Talbot LA. Lifestyle activity to improve fitness among National Guard personnel. TriService Nursing Research Program (TSNRP). TriService Nursing Research Program (TSNRP), 2010.
Talbot 2011 {published data only}
- Talbot LA, Metter EJ, Morrell CH, Frick KD, Weinstein AA, Fleg JL. A pedometer‐based intervention to improve physical activity, fitness, and coronary heart disease risk in National Guard personnel. Military Medicine 2011;176(5):592‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tan 2006 {published data only}
- Tan EJ, Xue QL, Li T, Carlson MC, Fried LP. Volunteering: A physical activity intervention for older adults ‐ The Experience Corps (R) Program in Baltimore. Journal of Urban Health: Bulletin of the New York Academy of Medicine 2006;83(5):954‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2005 {published data only}
- Taylor AH, Fox KR. Effectiveness of a primary care exercise referral intervention for changing physical self‐perceptions over 9 months. Health Psychology 2005;24(1):11‐21. [DOI] [PubMed] [Google Scholar]
Thogersen‐Ntoumani 2010 {published data only}
- Thogersen‐Ntoumani C, Loughren EA, Duda JL, Fox KR, Kinnafick FE. "Step by Step". A feasibility study of a lunchtime walking intervention designed to increase walking, improve mental well‐being and work performance in sedentary employees: Rationale and study design. BMC Public Health 2010;10:578. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2012 {published data only}
- Thomas GN, Macfarlane DJ, Guo B, Cheung BM, McGhee SM, Chou KL, et al. Health promotion in older Chinese: a 12‐month cluster randomized controlled trial of pedometry and "peer support". Medicine & Science in Sports & Exercise 2012;44(6):1157‐66. [DOI] [PubMed] [Google Scholar]
Vainionpää 2007 {published data only}
van Sluijs 2006 {published data only}
- Sluijs EM, Poppel MN, Twisk JW, Mechelen W. Physical activity measurements affected participants' behavior in a randomized controlled trial. Journal of Clinical Epidemiology 2006;59(4):404‐11. [DOI] [PubMed] [Google Scholar]
van Stralen 2008 {published data only}
- Stralen MM, Kok G, Vries H, Mudde AN, Bolman C, Lechner L. The Active plus protocol: systematic development of two theory‐ and evidence‐based tailored physical activity interventions for the over‐fifties. BMC Public Health 2008;8:399. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Stralen 2009 {published data only}
- Stralen MM, Vries H, Mudde AN, Bolman C, Lechner L. The working mechanisms of an environmentally tailored physical activity intervention for older adults: A randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2009;6:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Stralen 2009a {published data only}
- Stralen MM, Vries H, Mudde AN, Bolman C, Lechner L. Efficacy of two tailored interventions promoting physical activity in older adults. American Journal of Preventive Medicine 2009;37(5):405‐17. [DOI] [PubMed] [Google Scholar]
van Stralen 2010 {published data only}
- Stralen MM, Vries H, Bolman C, Mudde AN, Lechner L. Exploring the efficacy and moderators of two computer‐tailored physical activity interventions for older adults: a randomized controlled trial. Annals of Behavioral Medicine 2010;39(2):139‐50. [DOI] [PubMed] [Google Scholar]
van Stralen 2011 {published data only}
Visek 2011 {published data only}
- Visek AJ, Olson EA, DiPietro L. Factors predicting adherence to 9 months of supervised exercise in healthy older women. Journal of Physical Activity & Health 2011;8(1):104‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
von Thiele 2008 {published data only}
- Thiele Schwarz U, Lindfors P, Lundberg U. Health‐related effects of worksite interventions involving physical exercise and reduced workhours. Scandinavian Journal of Work, Environment & Health 2008;34(3):179‐88. [DOI] [PubMed] [Google Scholar]
Wadsworth 2010 {published data only}
- Wadsworth DD, Hallam JS. Effect of a web site intervention on physical activity of college females. American Journal of Health Behavior 2010;34:60‐9. [DOI] [PubMed] [Google Scholar]
Wanner 2009 {published data only}
- Wanner M, Martin‐Diener E, Braun‐Fahrlander C, Bauer G, Martin BW. Effectiveness of active‐online, an individually tailored physical activity intervention, in a real‐life setting: randomized controlled trial. Journal of Medical Internet Research 2009;11(3):e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wanner 2010 {published data only}
- Wanner M, Martin‐Diener E, Bauer G, Braun‐Fahrlander C, Martin BW. Comparison of trial participants and open access users of a web‐based physical activity intervention regarding adherence, attrition, and repeated participation. Journal of Medical Internet Research 2010;12:e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watkinson 2010 {published data only}
- Watkinson C, Sluijs EM, Sutton S, Marteau T, Griffin SJ. Randomised controlled trial of the effects of physical activity feedback on awareness and behaviour in UK adults: the FAB study protocol [ISRCTN92551397]. BMC Public Health 2010;10:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whitehead 2007 {published data only}
- Whitehead D, Bodenlos JS, Cowles ML, Jones GN, Brantley PJ. A stage‐targeted physical activity intervention among a predominantly African‐American low‐income primary care population. American Journal of Health Promotion 2007;21(3):160‐3. [DOI] [PubMed] [Google Scholar]
Wilcox 2007 {published data only}
- Wilcox S, Laken M, Bopp M, Gethers O, Huang P, McClorin L, et al. Increasing physical activity among church members: community‐based participatory research. American Journal of Preventive Medicine 2007;32(2):131‐8. [DOI] [PubMed] [Google Scholar]
Williams 2004 {published data only}
- Williams K, Prevost AT, Griffin S, Hardeman W, Hollingworth W, Spiegelhalter D, et al. The ProActive trial protocol ‐ a randomised controlled trial of the efficacy of a family‐based, domiciliary intervention programme to increase physical activity among individuals at high risk of diabetes [ISRCTN61323766]. BMC Public Health 2004;4:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2006 {published data only}
- Williams DM, Papandonatos GD, Napolitano MA, Lewis BA, Whiteley JA, Marcus BH. Perceived enjoyment moderates the efficacy of an individually tailored physical activity intervention. Journal of Sport & Exercise Psychology 2006;28:300‐9. [Google Scholar]
Williams 2011 {published data only}
- Williams DM, Papandonatos GD, Jennings EG, Napolitano MA, Lewis BA, Whiteley JA, et al. Does tailoring on additional theoretical constructs enhance the efficacy of a print‐based physical activity promotion intervention?. Health Psychology 2011;30(4):432‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2009 {published data only}
- Wilson K, Brookfield D. Effect of goal setting on motivation and adherence in a six‐week exercise program. International Journal of Sport and Exercise Psychology 2009;7(1):89‐100. [Google Scholar]
References to ongoing studies
Iliffe 2010 {published data only}
- Iliffe S, Kendrick D, Morris R, Skelton D, Gage H, Dinan S, et al. Multi‐centre cluster randomised trial comparing a community group exercise programme with home based exercise with usual care for people aged 65 and over in primary care: protocol of the ProAct 65+ trial. Trials [Electronic Resource] 2010;11(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2010 {published data only}
- Wilson DK, Trumpeter NN, George SM, Coulon SM, Griffin S, Lee Van Horn M, et al. An overview of the "Positive Action for Today's Health" (PATH) trial for increasing walking in low income, ethnic minority communities. Contemporary Clinical Trials 2010;31(6):624‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Bandura 1986
- Bandura A. Social foundations of thought and action: social cognitive theory. Englewood Cliffs: Prentice Hall, 1986. [Google Scholar]
Bartholomew 2001
- Bartholomew LK, Parcel GS, Kok G, Gottlieb NH. Intervention mapping: designing theory‐ and evidence‐based health promotion programs. Mountain View: Mayfield, 2001. [Google Scholar]
Bauman 2012
- Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW. Correlates of physical activity: why are some people physically active and others not?. Lancet 2012;380(9838):258‐71. [DOI] [PubMed] [Google Scholar]
Becker 1974
- Becker M. The health belief model and sick role behaviour. Health Education Monographs 1974;2:409‐19. [Google Scholar]
Biddle 2001
- Biddle S, Mutrie N. Psychology of physical activity: determinants, well‐being and interventions. London: Routledge, 2001. [Google Scholar]
Biddle 2011
- Biddle S, Foster C. Health behaviour change through physical activity & sport. In: Houlihan B editor(s). Handbook of Sport Development. Abingdon: Routledge, 2011. [Google Scholar]
Blair 2001
- Blair SN, Cheng Y, Holder JS. Is physical activity or physical fitness more important in defining health benefits?. Medicine and Science in Sports and Exercise 2001;33(6 Suppl):S379‐99; discussion S419‐20. [DOI] [PubMed] [Google Scholar]
Christinsen 2009
- Christinsen R, Nair S. Statistical method guidelines for Cochrane Public Health reviews. Melbourne: Cochrane Public Health Group Report, 2009.
Conn 2011
- Conn V, Hafdahl A, Mehr D. Interventions to increase physical activity among healthy adults: Meta‐analysis of outcomes. American Journal of Public Health 2011;101(4):751–8. [DOI: 10.2105/AJPH.2010.194381] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Dickersin 1995
- Dickersin K, Scherer, Lefebvre C. Identifying relevant studies from systematic reviews. In: Chalmers I, Altman DG editor(s). Systematic Reviews. London: BMJ Publishing Group, 1995:64‐74. [Google Scholar]
Dishman 1990
- Dishman RK. Determinants of participation in physical activity. In: Bouchard C, Shephard RJ, Stephens T, Sutton JR, McPherson BD editor(s). Exercise, fitness and health: a consensus of current knowledge. Champaign: Human Kinetics, 1990. [Google Scholar]
Dishman 1994
- Dishman RK, Sallis JF. Determinants and interventions for physical activity and exercise. In: Bouchard C, Shephard RJ, Stephens T editor(s). Physical activity, fitness and health: international proceedings and consensus statement 1992. Champaign: Human Kinetics, 1994. [Google Scholar]
Dishman 1996
- Dishman RK, Buckworth J. Increasing physical activity: a quantitative synthesis. Medicine and Science in Sports and Exercise 1996;28(6):706‐19. [DOI] [PubMed] [Google Scholar]
Epstein 2001
- Epstein LH, Roemmich JN. Reducing sedentary behavior: role in modifying physical activity. Exercise and Sport Sciences Reviews 2001;29(3):103‐8. [DOI] [PubMed] [Google Scholar]
Fishbein 1975
- Fishbein M, Azjen I. Belief, attitude, intention and behaviour. New York: Whiley, 1975. [Google Scholar]
Foster 2005a
- Foster C, Hillsdon M, Thorogood M, Kaur A, Wedatilake T. Interventions for promoting physical activity. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI: 10.1002/14651858.CD003180.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Foster 2005b
Foster 2011
- Foster C, Brennan G, Matthews A, McAdam C, Fitzsimons C, Mutrie N. Recruiting participants to walking intervention studies: a systematic review. International Journal of Behavioral Nutrition and Physical Activity 2011;8:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hagger 2003
- Hagger MS, Orbell S. A met‐analytical review of the common‐sense model of illness representations. Psychology and Health 2003;18(2):141‐84. [Google Scholar]
Hallal 2012
- Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380(9838):247‐57. [DOI] [PubMed] [Google Scholar]
Haskell 2007
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116(9):1081‐93. [DOI] [PubMed] [Google Scholar]
Heath 2012
- Heath GW, Parra DC, Sarmiento OL, Andersen LB, Owen N, Goenka S, et al. Evidence‐based intervention in physical activity: lessons from around the world. Lancet 2012;380(9838):272‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JP, White IR, Wood AM. Imputation methods for missing outcome data in meta‐analysis of clinical trials. Clinical trials 2008;5(3):225‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hobbs 2013
- Hobbs N, Godfrey A, Lara L, Errington L, Meyer T, Rochester L, et al. Are behavioral interventions effective in increasing physical activity at 12 to 36 months in adults aged 55 to 70 years? A systematic review and meta‐analysis. BMC Medicine 2013;11:75. [DOI: 10.1186/1741-7015-11-75] [DOI] [PMC free article] [PubMed] [Google Scholar]
Humphreys 2013
- Humphreys D, Ogilvie D. Synthesising evidence for equity impacts of population‐based physical activity interventions: a pilot study. International Journal of Behaviour Nutrition and Physical Activity 2013;10:76. [DOI: 10.1186/1479-5868-10-76] [DOI] [PMC free article] [PubMed] [Google Scholar]
Janssen 2010
- Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school‐aged children and youth. International Journal of Behavioral Nutrition and Physical Activity 2010;7:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kesaniemi 2001
- Kesaniemi YK, Danforth E Jr, Jensen MD, Kopelman PG, Lefebvre P, Reeder BA. Dose‐response issues concerning physical activity and health: an evidence‐based symposium. Medicine and Science in Sports and Exercise 2001;33(6 Suppl):S351‐8. [DOI] [PubMed] [Google Scholar]
Lee 2012
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non‐communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380(9838):219‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
McAuley 1994
- McAuley E, Courneya KS, Rudolph DL, Lox CL. Enhancing exercise adherence in middle‐aged males and females. Preventive Medicine 1994;23(4):498‐506. [DOI] [PubMed] [Google Scholar]
Miller 2012
- Miller WM, Rollnick S. Motivational Interviewing: Helping People Change. New York: The Guildford Press, 2012. [Google Scholar]
Nelson 2007
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116(9):1094‐105. [DOI] [PubMed] [Google Scholar]
Oldridge 2008
- Oldridge NB. Economic burden of physical inactivity: healthcare costs associated with cardiovascular disease. European Journal of Cardiovascular Prevention and Rehabilitation 2008;15(2):130‐9. [DOI] [PubMed] [Google Scholar]
Prochaska 1982
- Prochaska JM, DiClemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy: Theory, Research & Practice 1982;19(3):276‐88. [Google Scholar]
Review Manager 2012 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Rodgers 1991
- Rodgers W, Brawley LR. The role of outcome expectancies in participation motivation. Journal of Sport & Exercise Psychology 1991;13(4):411‐27. [Google Scholar]
Rogers 1969
- Rogers CR. Freedom to learn: a view of what education might become. 2nd Edition. Columbus: Charles Merill Publishing Company, 1969. [Google Scholar]
Sallis 1997
- Sallis JF, Owen N. Ecological models. In: Glanz K, Lewis FM, Rimmer BK editor(s). Health behaviour and health education: theory, research, and practice. San Francisco: Jossey‐Bass, 1997. [Google Scholar]
Sallis 1999
- Sallis JF, Owen N. Physical activity & behavioural medicine. Thousand Oaks: Sage, 1999. [Google Scholar]
Schwarzer 2008
- Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Applied Psychology: An International Review 2008;57:1‐29. [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D. Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Intervention Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Strong 2005
- Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, et al. Evidence based physical activity for school‐age youth. Journal of Pediatrics 2005;146(6):732‐7. [DOI] [PubMed] [Google Scholar]
van den Berg 2007
- Berg MH, Schoones JW, Vliet Vlieland TP. Internet‐based physical activity interventions: a systematic review of the literature. Journal of Medical Internet Research 2007;9(3):e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Warburton 2006
- Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. Canadian Medical Association Journal 2006;174(6):801‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2010a
- World Health Organization (WHO). Global recommendations on physical activity for health. Geneva: WHO, 2010. [PubMed]
WHO 2010b
- World Health Organization (WHO). Global status report on noncommunicable diseases. Geneva: WHO, 2010.
Williams 2001
- Williams PT. Physical fitness and activity as separate heart disease risk factors: a meta‐analysis. Medicine and Science in Sports and Exercise 2001;33(5):754‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]


