Abstract
A man in his 30s with no previous medical history presented to the emergency department with acute dyspnoea. His chest X-ray (CXR) showed a massive left-sided pneumothorax, and a 12Fg post-intercostal drain (ICD) was inserted. Twenty-four hours later there was evidence of blood in the drain, and he had a significant haemoglobin drop of 44 g/l in only one day. His vital signs were stable. A CXR and an urgent computed tomography (CT) scan showed a large haemothorax therefore he was transferred to the tertiary thoracic centre, where he was taken to theatre and had a thoracoscopy and evacuation of a blood clot. Follow-up two weeks later showed complete resolution of the haemopneumothorax.
This case report highlights the rare complication of a massive iatrogenic haemothorax. This was despite all the safety precautions including normal coagulation and platelet count, the patient not being on any anti-coagulant drugs and an ICD approach via the triangle of safety for insertion of the small-bore tube. In the case of iatrogenic haemothorax, urgent resuscitation and surgical treatment are needed as this is a life-threatening situation.
LEARNING POINTS
Iatrogenic haemothorax post-intercostal drain (ICD) insertion has not been reported in recent literature since the new British Thoracic Society (BTS) guidelines advised ultrasound-assisted procedure for pleural effusions, and a ‘triangle of safety’ for pneumothorax patients. Nevertheless, it should be included in the differential diagnoses as it still could happen.
If it is a massive haemothorax, cardiothoracic surgeons must be notified immediately.
Point-of-care ultrasound can be used to diagnose pleural fluid while awaiting a chest X-ray. However, point-of-care ultrasound will not be able to differentiate between blood and normal pleural fluid, whereby a formal chest CT can.
Keywords: Intercostal chest drain, haemothorax, haemopneumothorax
INTRODUCTION
Haemothorax is a collection of blood in the pleural cavity as a sequela of chest trauma, a ruptured aortic aneurysm and perforation of intrathoracic vessels during central venous catheterisation or an intercostal chest drain. Diagnosis is made by upright chest X-ray (CXR) or point-of-care ultrasound, and a computed tomography (CT) scan of the chest. Intervention depends on the size and severity of the symptoms. A minimal haemothorax is up to 400 ml of blood in the pleural space, while a medium haemothorax is from 400 to 1000 ml. If the collection is more than 1000 ml, it is considered a massive haemothorax. Tube thoracostomy is the treatment of choice; however, if there is retained haemothorax, fibrinolysis and consequently video-assisted thoracoscopy surgery will be indicated[1]. If all prior procedures fail, open thoracotomy will be performed.
According to the British Thoracic Society (BTS) national audit, only 1% of iatrogenic haemothorax post-intercostal drain (ICD) can result in iatrogenic haemothorax[2]. To reduce the risk of haemothorax during an ICD procedure anticoagulation agents must be stopped in time, and blood clotting factors and platelet count must be checked and corrected if necessary. It must be ultrasound guided (for pleural effusion) and a fine-bore needle ≤ 14Fg must be used[3]. For pneumothorax, insertion should be done in the ‘triangle of safety’. In non-urgent ICDs, insertion of the tube must be avoided if patient is anticoagulated, has liver disease or bleeding diathesis, until the international normalised ratio is less than 1.5.
CASE DESCRIPTION
A man in his 30s with ten pack-year smoking history was admitted to the emergency department (ED) of a district general hospital with 24-hour history of left-side pleuritic chest pain, dyspnoea and a productive cough. He was a fit man and had no previous medical history and was not on any regular medications. There was no significant family history. On clinical examination he was tall thin, and dyspnoeic at rest. A chest examination revealed a hyper resonant left-side chest with reduced air entry at the same side. He required 3 l/min of oxygen to maintain saturation above 94%. His pulse rate was 61 bpm, blood pressure was 120/84 mmHg; cardiac examination was normal.
At the time of the presentation to ED, initial investigations showed negative COVID-19 and influenza results, and haemoglobin was 138 g/l with normal renal function. CXR showed a left-side pneumothorax (Fig. 1), and the diagnosis of massive primary pneumothorax was made. The initial treatment for massive spontaneous pneumothorax was a Rocket® 12Fg Seldinger chest drain (Fig. 2). His initial coagulation and platelets were normal, and a chest drain was inserted in the triangle of safety. The next day, the patient developed a large haemothorax (Fig. 3) and was transferred to the tertiary cardiothoracic centre for thoracoscopy, evacuation of blood clots and apical blebectomy. Two weeks after the thoracoscopy, a CXR showed resolution of haemopneumothorax (Fig. 4). Two months later, the patient had remained healthy and asymptomatic, with a clear CXR.
Figure 1.

Chest radiograph demonstrating a massive left pneumothorax with no tracheal deviation.
Figure 2.

Chest radiograph after insertion of 12Fg Rocket Seldinger ICD in the emergency department.
Figure 3.
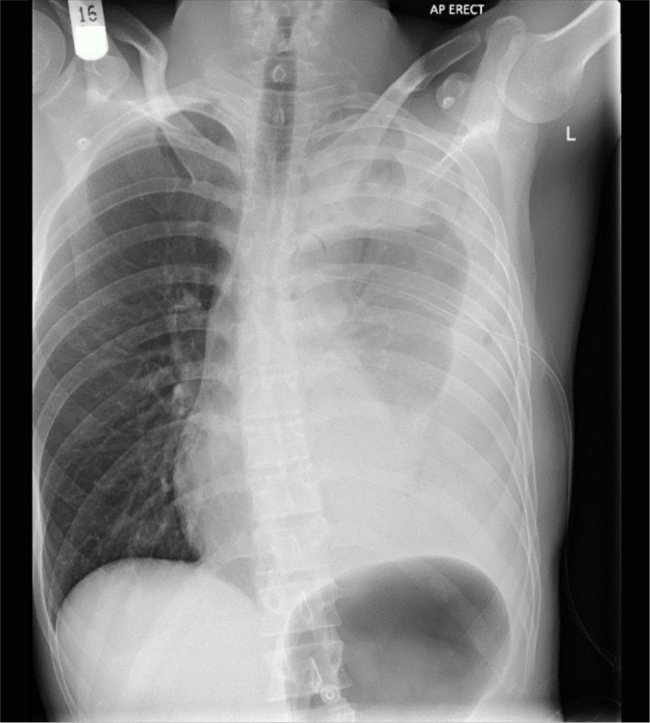
Haemopneumothorax post-ICD insertion.
Figure 4.

Chest X-ray two weeks following left thoracoscopy and evacuation of clots showing a virtually complete resolution of haemopneumothorax.
DISCUSSION
A major haemothorax was produced after the insertion of a 12Fg Rocket Seldinger ICD tube in a young healthy man, despite all safety precautions of checking for normal bloods (platelets and coagulation) and inserting the drain in the triangle of safety. The most common mechanism of injury is damage to the intercostal vessels, lung parenchyma or the surrounding tissues, resulting in bleeding into the pleural space by using sharp instruments, or by the chest tube itself[1]. Hence, the insertion of ICD must follow the guidelines recommended by the BTS. As far as we know, there are not many reported cases of iatrogenic haemothorax following an insertion of a small-size ICD tube, especially when all the safety precautions have been undertaken as outlined above. There is a report of a male patient who was on aspirin and ticagrelor who had a pleural aspiration performed, which resulted in a massive haemothorax. His condition improved after withholding double anti-platelet therapy, performing a blood transfusion and inserting a Rocket 12Fg Seldinger chest drain[4]. It is paramount for doctors to recognise these risks and follow the guidelines by the BTS while inserting a chest drain to minimise the likelihood of causing haemothorax. There have been no new cases of iatrogenic haemothorax after insertion of ICD reported since ultrasound has been part of the BTS guideline in patients with pleural effusion[5]. We are reporting this case to raise a warning that even using all the safety mechanisms as per the guidance, there is still possibility of iatrogenic haemothorax post-ICD insertion. As per the BTS guidelines for pleural disease, primary spontaneous pneumothorax should be treated conservatively if the patient is minimally symptomatic. If patient has good support and the centre has follow-up facilities, the patient can have ambulatory management. However, needle aspiration or ICD insertion should be considered if neither conservative nor ambulatory treatment is feasible[5]. Despite all the safety precautions taken, serious complications can occur, and the operator needs to be aware and be vigilant to look out for them.
Footnotes
Conflicts of Interests: The Authors declare that there are no competing interests.
Patient Consent: We confirm the acquisition of the signed patient consent.
REFERENCES
- 1.Zeiler J, Idell S, Norwood S, Cook A. Hemothorax: a review of the literature. Clin Pulm Med. 2020;27:1–12. doi: 10.1097/CPM.0000000000000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hooper C, Maskell N team BTS audit team. British Thoracic Society national pleural procedures audit 2010. Thorax. 2011;66:636–637. doi: 10.1136/thoraxjnl-2011-200077. [DOI] [PubMed] [Google Scholar]
- 3.Havelock T, Teoh R, Laws D, Gleeson F Group BTS Pleural Disease Guideline Group. Pleural procedures and thoracic ultrasound: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65:ii61–76. doi: 10.1136/thx.2010.137026. [DOI] [PubMed] [Google Scholar]
- 4.Chattopadhyay GK, Pardeshi P, Malapanjudi J, Varney V, Quadery R. Iatrogenic haemothorax – does extra benefit go hand-in-hand with extra risk? A case report and review of literature. Clin Med (Lond) 2020;20:s14. doi: 10.7861/clinmed.20-2-s14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts ME, Rahman NM, Maskell NA, Bibby AC, Blyth KG, Corcoran JP, et al. British Thoracic Society Guideline Development Group. British Thoracic Society Guideline for pleural disease. Thorax. 2023;78:s1–s42. doi: 10.1136/thorax-2022-219784. [DOI] [PubMed] [Google Scholar]


