Abstract
Crohn’s disease (CD) is a transmural inflammatory process that can affect any segment of the gastrointestinal tract. CD has a predilection for the colon and the small bowel, specifically the terminal ileum. Esophageal involvement of CD is exceedingly rare and there is a paucity of data regarding the disease phenotypes, course, complications and treatment. We report a case of an 18-year-old male patient presenting for intermittent dysphagia and epigastric pain. Upper endoscopy revealed esophageal ulcers in the middle esophagus surrounded by normal esophageal mucosa. Biopsies were taken from the ulcerated lesions. Histology revealed granulomatous esophagitis. The stomach and duodenum were unremarkable. An ileo-colonoscopy was performed and showed unremarkable mucosa with normal biopsies. The patient was started on proton pump inhibitors and prednisolone as induction therapy with significant symptomatic improvement within 15 days of therapy. The patient was then started on azathioprine 150 mg once daily as maintenance therapy with complete resolution of symptoms. Esophageal CD is an overlooked entity. This article underscores the need to rule out CD when physicians are confronted by esophageal ulcers on upper endoscopy.
LEARNING POINTS
Dysphagia as the initial presentation of esophageal Crohn’s disease is exceedingly rare.
Esophageal Crohn’s disease be included in the differential diagnosis of esophageal ulcers in the absence of Crohn’s disease of the colon or small bowel.
Treatment of esophageal Crohn’s disease should be tailored to each patient taking into account the patient’s symptoms, disease activity, disease course, phenotype and disease complications.
Keywords: Esophageal ulcers, esophageal Crohn’s disease, prednisolone, azathioprine
INTRODUCTION
Crohn’s disease (CD) is a chronic granulomatous inflammatory disease that can affect any segment of the gastrointestinal tract. Esophageal involvement of CD is exceedingly rare with a prevalence of 1.8% in adults[1]. The diagnosis is usually made in patients known to have CD of the colon or the small bowel in the setting of esophageal symptoms[2]. Esophageal symptoms surfacing as a presenting feature for CD is extremely rare.
CASE PRESENTATION
An 18-year-old male sought medical care for intermittent dysphagia and epigastric pain. The patient denied any weight loss or gastrointestinal symptoms. He denied any fever or aphthous oral ulcers. The patient did not take any medications on regular basis. He had no family history of gastrointestinal inflammatory bowel disease or malignancy. The physical examination was unremarkable. Biochemical workup was normal.
Upper endoscopy revealed multiple ulcers with a punched-out appearance at the level of the middle esophagus (Fig. 1) interspersed with normal surrounding esophageal mucosa. The gastro-esophageal junction, stomach and second portion of the duodenum were normal.
Figure 1.
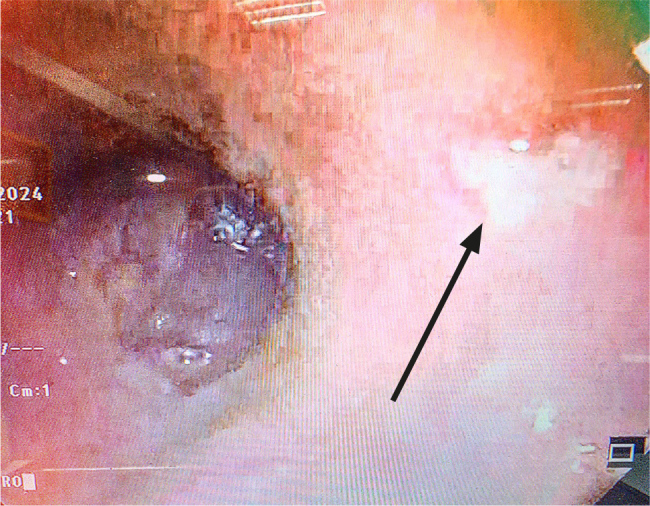
An upper endoscopy revealing a superficial punched out aphthous ulcer (black arrow) with surrounding normal esophageal mucosa.
Ziehl-Nelsen stain and immunohistochemical staining for cytomegalovirus, herpes simplex virus and polymerase chain reaction for Mycobacterium tuberculosis deoxyribonucleic acid were negative. Serology for human immunodeficiency virus was negative. A wide differential diagnosis was considered: gastroesophageal reflux disease, esophageal carcinoma, viral infections, CD, sarcoidosis, tuberculosis, disseminated fungal disease, Bechet’s disease and chronic granulomatous disease. An ileo-colonoscopy was unremarkable with normal biopsies. Magnetic resonance enterography was unremarkable with absence of stenosis or intra-abdominal collections. Histologically, esophageal biopsies revealed erosions with epithelioid granulomas without central necrosis in the lamina propria. A diagnosis of isolated esophageal CD was made. The patient was started on proton pump inhibitors (PPIs) at a dosage of 40 mg once daily along with prednisolone 40 mg once daily as induction therapy. The patient reported symptom improvement within 15 days of treatment. The patient received a course of prednisolone of 40 mg with tapering for 4 weeks concomitantly with azathioprine 150 mg once daily as maintenance therapy. Full resolution of esophageal symptoms was reported 3 weeks following treatment.
One month later, a repeat upper endoscopy was unremarkable with complete resolution of the esophageal ulcers. Histology was normal as well. At present, the patient remains asymptomatic on azathioprine 150 mg once daily.
DISCUSSION
Esophageal involvement of CD is rare and esophageal symptoms as initial presentation of CD is even rarer. Usually, colonic or small bowel CD precedes esophageal CD. Esophageal CD manifests as symptoms of esophageal involvement. Dysphagia and odynophagia are the most common symptoms of esophageal CD[3]. Chest pain and heartburn are other symptoms of esophageal CD. Around 30% of patients with esophageal CD have concomitant oral aphthous ulcerations at the time of diagnosis[4]. Patients with esophageal CD can sometimes exhibit weight loss and extra-intestinal manifestations, such as arthritis, uveitis, and erythema nodosum[5].
Endoscopic findings of esophageal CD are characterized by ulcerations, erosions and cobblestone appearance[6]. Esophageal CD has a predilection for the middle and distal esophagus with the proximal esophagus being less commonly affected by CD[7]. Complications of esophageal CD are fistulas to the stomach and respiratory tract. In severe cases, esophageal strictures can ensue[7]. Histologically, non-caseating granulomas are seldom detected in esophageal CD and they are not necessary for the diagnosis of esophageal CD[8].
The management of esophageal CD is not standardized due to paucity of data, the heterogeneity of cases and lack of clinical trials in the medical literature[9]. PPIs have been shown to provide symptomatic relief and mucosal healing in cases of esophageal CD but their clinical and endoscopic benefits are yet to be proven[9]. Oral systemic steroids are associated with rapid improvement of esophageal symptoms as was exemplified in our case. Antitumor necrosis factors are effective in severe and refractory cases of esophageal CD. Endoscopic dilatation is an option in cases of esophageal strictures[10]. Surgery is opted for in cases of fistulas, refractory strictures and diseases refractory to medical treatment[10]. Induction therapy with prednisolone along with azathioprine maintenance therapy remains the gold standard of treatment in terms of clinical and endoscopic remission and histologic improvement[1,3,7]. Our case highlights the efficacy of PPIs, prednisolone and azathioprine in inducing clinical and endoscopic remission and histologic improvement.
CONCLUSION
Esophageal CD should be incorporated in the differential diagnosis of esophageal ulcers. An upper endoscopy is warranted in patients known to have colonic and small bowel CD with esophageal symptoms. Therefore, an upper endoscopy is crucial to evaluate the extent of the disease. A diagnosis of esophageal CD is confirmed by combined clinical, endoscopic and histologic findings. Treatment should be personalized in terms of varying disease activity, phenotype, disease course and complications.
Footnotes
Conflicts of Interests: The Authors declare that there are no competing interests.
Patient Consent: A signed written informed consent was obtained from the patient prior to writing and submitting the manuscript.
REFERENCES
- 1.Isaacs KL. Crohn’s disease of the esophagus. Curr Treat Options Gastroenterol. 2007;10:61–70. doi: 10.1007/s11938-007-0058-3. [DOI] [PubMed] [Google Scholar]
- 2.Decker GA, Loftus EV, Jr, Pasha TM, Tremaine WJ, Sandborn WJ. Crohn’s disease of the esophagus: clinical features and outcomes. Inflamm Bowel Dis. 2001;7:113–119. doi: 10.1097/00054725-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Kuhlmann JB, Blum HE, Kreisel W, Fischer R. A severe case of odynophagia. BMJ. 2011;343:d3137. doi: 10.1136/bmj.d3137. [DOI] [PubMed] [Google Scholar]
- 4.Zografos GN, Georgiadou D, Thomas D, Kaltsas G, Digalakis M. Drug-induced esophagitis. Dis Esophagus. 2009;22:633–637. doi: 10.1111/j.1442-2050.2009.00972.x. [DOI] [PubMed] [Google Scholar]
- 5.Szaloki T, Toth V, Czako L. Unusual esophageal manifestations of Crohn’s disease. Gastrointest Endosc. 2006;64:121. doi: 10.1016/j.gie.2006.01.036. [DOI] [PubMed] [Google Scholar]
- 6.Naranjo-Rodríguez A, Solórzano-Peck G, López-Rubio F, Calañas-Continente A, Gálvez-Calderón C, González-Galilea A, et al. Isolated oesophageal involvement of Crohn’s disease. Eur J Gastroenterol Hepatol. 2003;15:1123–1126. doi: 10.1097/00042737-200310000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Remes-Troche JM, Argote-Greene M, Rubio-Tapia A, Martínez-Benítez B, Reyes E, Medina-Franco H, et al. Progressive dysphagia caused by isolated esophageal involvement of Crohn’s disease. Inflamm Bowel Dis. 2005;11:515–517. [PubMed] [Google Scholar]
- 8.Lou GC, Yang JM, Huang W, Zhang J, Zhou B. Esophageal Crohn’s disease. Endoscopy. 2009;41:E257. doi: 10.1055/s-0029-1214498. [DOI] [PubMed] [Google Scholar]
- 9.Gheorghe C, Aposteanu G, Popescu C, Gheorghe L, Oproiu A, Popescu I. Long esophageal stricture in Crohn’s disease: a case report. Hepatogastroenterology. 1998;45:738–741. [PubMed] [Google Scholar]
- 10.De Felice KM, Katzka DA, Raffals LE. Crohn’s disease of the esophagus: clinical features and treatment outcomes in the biologic era. Inflamm Bowel Dis. 2015;21:2106–2113. doi: 10.1097/MIB.0000000000000469. [DOI] [PubMed] [Google Scholar]


