Abstract
Mucormycosis is a life-threatening fungal infection caused by Mucorales fungi, characterized by angioinvasion and tissue necrosis. While it predominantly affects immunocompromised individuals, it can also occur in immunocompetent patients through traumatic inoculations, such as contaminated surgical dressings or injections.
We report two cases of cutaneous mucormycosis following the shared use of contaminated intramuscular corticosteroid injections (dexamethasone). Case 1 involved a 54-year-old male farmer with rapidly progressing necrotic lesions and multi-organ failure, resulting in death despite aggressive treatment. Case 2 involved a 48-year-old female nursing technician who developed similar necrotizing lesions and also succumbed to multi-organ failure after extensive debridement and antifungal therapy.
These cases underscore the rapid deterioration associated with mucormycosis, an infection with a high mortality rate even in immunocompetent individuals. The hallmark of the disease is rapidly progressing necrosis due to vascular invasion and thrombosis. Mucormycosis following contaminated injections, though rare, is devastating. Early recognition and aggressive treatment, including surgical debridement and antifungal therapy, are critical but may not always prevent fatal outcomes. Strict infection prevention precautions and epidemiological surveillance are needed to prevent iatrogenic infections.
LEARNING POINTS
Direct inoculation of Mucorales species through contaminated injections is a rare but serious route of infection, highlighting the importance of proper handling of medical equipment.
Mucormycosis can occur in immunocompetent individuals following traumatic events or contaminated procedures, and it often leads to rapid tissue necrosis and high mortality if not promptly treated.
Early surgical debridement and antifungal therapy are critical for managing mucormycosis, though survival remains poor even with aggressive intervention.
Keywords: Mucormycosis, necrotizing fasciitis, contaminated injection
INTRODUCTION
Mucormycosis is a severe, life-threatening fungal infection caused by filamentous fungi of the subphylum Mucormycotina[1]. Characterized by its angioinvasive nature, the infection often leads to tissue necrosis due to vascular invasion and subsequent thrombosis. The primary modes of transmission include inhalation of spores, traumatic inoculation, or ingestion of contaminated substances. While mucormycosis predominantly affects immunocompromised individuals, primary cutaneous forms can also manifest in immunocompetent patients following traumatic events such as contaminated surgical dressings, burns, or injections[2]. In rare cases, mucormycosis is associated with iatrogenic injections, typically in diabetic patients receiving insulin. When infection involves the deeper layers of tissue, necrotizing fasciitis may develop, characterized by rapid progression and poor prognosis. In the cases presented, both patients experienced necrotizing fasciitis with rapid clinical deterioration, leading to death within days of symptom onset.
We present two cases of cutaneous mucormycosis following the shared use of an intramuscular corticosteroid injection (dexamethasone), emphasizing the aggressive nature of the infection and its rare transmission route.
CASE DESCRIPTIONS
Case 1
A 54-year-old male farmer from Potiretama (Ceará, Brazil) presented in a rural hospital on April 18, 2023, with dry cough, odynophagia, and fever without receiving any treatment. Although his respiratory symptoms resolved after 2 days, his fever persisted, and painful erythematous-violaceous lesions appeared on his left thigh, trunk, and upper left limb. Laboratory tests revealed leukocytosis (leukocytes: 31,300/μl, segmented neutrophils: 25,040/μl) and acute renal failure (creatinine: 1.6 mg/dl). He was then admitted at the Hospital Geral Dr. César Cals on April 28 in critical condition, with necrotic skin lesions (Fig. 1) and severe metabolic acidosis (creatine phosphokinase: 35,866 U/l, bicarbonate: 9 mEq/l). Despite treatment with broad-spectrum antibiotics, bicarbonate replacement, and renal replacement therapy, the patient’s condition deteriorated rapidly, leading to septic shock, requiring endotracheal intubation and vasopressor support. An emergency bedside debridement was performed, but the patient died on April 30, 2023, due to irreversible hemodynamic instability. The patient’s family disclosed that he had received an intramuscular injection of dexamethasone, with the syringe shared with another patient who had a similar clinical presentation.
Figure 1.

Cutaneous mucormycosis presenting with extensive necrotic tissue, black eschar formation, and ulceration on the patient’s chest, indicating aggressive fungal invasion and tissue ischemia.
Case 2
A 48-year-old female nursing technician, also from Potiretama (Ceará, Brazil) developed localized hyperemia and vesicles at the site of an intramuscular injection of dexamethasone and diclofenac in her right thigh on April 21, 2023. Erythematous-violaceous lesions with central necrosis subsequently developed on her abdominal wall, right thigh, and axilla. This patient was a nursing technician at a hospital in the rural area of the interior of Brazil and diverted a vial of dexamethasone from the hospital, administering the injection first in the initial case and then to herself to relieve arthralgia, without aseptic precautions, at home, 7 days before the onset of the illness in the first case. It was reported that the needle used for her injection had been contaminated after contact with the patient from Case 1. She was admitted to the hospital on April 30 with worsening cutaneous lesions and persistent fever. Despite antibiotic therapy and multiple surgical debridements (Fig. 2), her condition worsened. By May 2, she developed acute kidney injury requiring hemodialysis. Biopsy revealed thrombosed vessels with adjacent ischemia and the presence of pauciseptate hyphae (Fig. 3 and 4). Polymerase chain reaction (PCR) analysis of the tissue confirmed the presence of Mucorales species. Despite aggressive treatment with liposomal amphotericin B and voriconazole, the patient ultimately succumbed to multi-organ failure on May 23, 2023.The health authorities of the state of Ceará were notified for epidemiological surveillance and local investigation.
Figure 2.

Extensive necrotic ulcer with exposed underlying tissue located on the patient’s trunk, demonstrating advanced tissue destruction and signs of severe infection.
Figure 3.
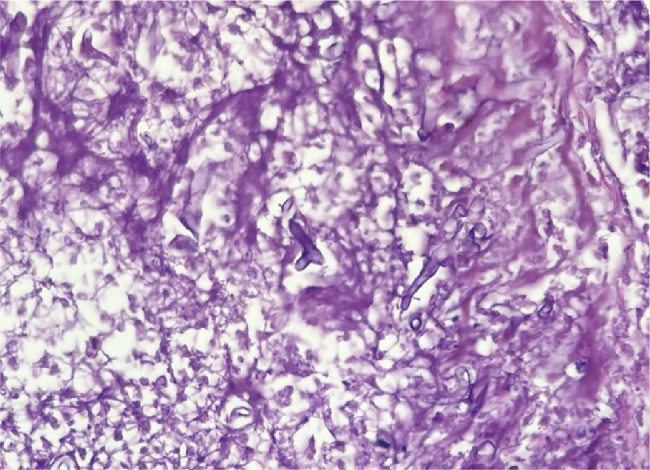
Vessel wall and lumen demonstrating thrombosis with intact pauciseptate hyphae, indicative of mucormycosis, seen under hematoxylin and eosin (HE) staining at 20x magnification.
Figure 4.
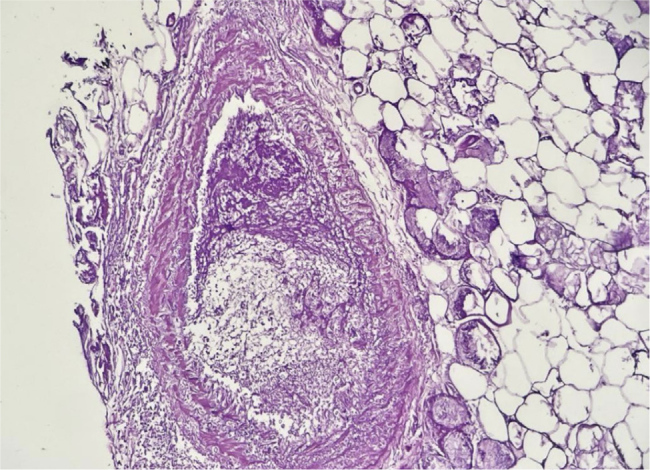
Presence of a deeply thrombosed, muscular-walled vessel with surrounding tissue ischemia, characteristic of angioinvasive mucormycosis.
DISCUSSION
Mucormycosis, caused by fungi of the order Mucorales, is an aggressive, angioinvasive infection that carries a high mortality rate, even in immunocompetent individuals. The most common causative pathogens include Rhizopus, Mucor, Rhizomucor, Apophysomyces, and Cunninghamella[3]. The clinical manifestations of mucormycosis are diverse and depend on the route of infection, the site involved, and the host’s immune status. Hallmark features of the infection include rapidly progressing necrosis, resulting from vascular invasion, thrombosis, and tissue ischemia[4].
Cutaneous mucormycosis is the third most common form of the disease, following the rhino-orbito-cerebral and pulmonary forms. Cutaneous manifestations typically begin with painful erythematous or violaceous lesions, which progress to necrotic ulcers and eschars. In advanced cases, the infection extends into deeper tissues, involving muscle, fascia, and even bone, as seen in necrotizing fasciitis[5]. Other clinical signs include induration, vesicle formation, and rapidly spreading soft tissue destruction. Fever and systemic symptoms are often present, especially when deeper structures are involved, or dissemination occurs. A recent review of 291 cases of cutaneous mucormycosis revealed that 42.5% of infections remained localized, while 44.5% extended into deep tissues, and 13% were disseminated[6]. The disseminated form progresses rapidly, often leading to gangrene and systemic involvement. Mucormycosis frequently occurs in immunocompromised patients, but nearly 50% of cutaneous cases are seen in immunocompetent individuals, typically following trauma or injury. Major risk factors include surgical wounds, burns, or contaminated medical equipment, as seen in the cases reported here. There are several reported cases of mucormycosis following the injection of medications, especially insulin, typically in patients with underlying risk factors such as leukemia and decompensated diabetes[7–9]. In these instances, the contaminated intramuscular injections likely served as a direct route for inoculation with Mucorales, leading to rapid onset necrotizing fasciitis, a severe form of soft tissue infection. Necrotizing fasciitis is known for its aggressive nature, rapidly destroying soft tissues, spreading along fascial planes, and leading to systemic complications and death despite early intervention. Diagnosing cutaneous mucormycosis can be challenging, as the early lesions may resemble other conditions, such as aspergillosis, bacterial synergistic gangrene, or pyoderma gangrenosum[5]. Targetoid lesions may raise suspicion for autoimmune diseases, drug reactions, or neoplastic disorders. Hence, it is crucial to maintain a high index of suspicion for mucormycosis, particularly in patients with a history of trauma or injections with contaminated medical equipment.
In Brazil, mucormycosis is relatively rare, with an estimated incidence of 0.2 per 100,000 inhabitants[2,10]. A review of 25 cases of cutaneous mucormycosis in the country identified various local risk factors, including surgery (17%), burns (16%), motor vehicle accidents (12%), and contaminated injection needles (13%). In some instances, contamination of needles with soil has been implicated as a source of transmission, underscoring the importance of investigating environmental factors, such as soil contamination with Mucorales, which are ubiquitous in decaying organic matter, soil, compost, and contaminated food. Early and aggressive surgical debridement remains a cornerstone of treatment for mucormycosis, as it facilitates the removal of necrotic tissue and reduces the fungal burden. Antifungal therapy, particularly with liposomal amphotericin B at doses of 5–10 mg/kg per day, is the first-line pharmacologic treatment. Isavuconazole and posaconazole are recommended as alternative agents. While combination antifungal regimens have shown promise in experimental models, there is insufficient clinical data to recommend their routine use in human cases.
CONCLUSION
These two cases highlight the aggressive nature and poor prognosis of mucormycosis, even in immunocompetent patients. Early recognition, aggressive debridement, and prompt antifungal therapy are crucial to improving survival. Continued surveillance and awareness are essential, particularly in cases involving contaminated medical equipment or traumatic events. Further research into the environmental sources of Mucorales in specific regions is necessary to help prevent future outbreaks.
Footnotes
Conflicts of Interests: The Authors declare that there are no competing interests.
Patient Consent: The patients’ families provided consent for the publication of this case report.
REFERENCES
- 1.Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19(12):e405–e421. doi: 10.1016/S1473-3099(19)30312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prakash H, Chakrabarti A. Global Epidemiology of Mucormycosis. J Fungi (Basel) 2019;5:26. doi: 10.3390/jof5010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steinbrink JM, Miceli MH. Mucormycosis. Infect Dis Clin North Am. 2021;35:435–452. doi: 10.1016/j.idc.2021.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta I, Baranwal P, Singh G, Gupta V. Mucormycosis, past and present: a comprehensive review. Future Microbiol. 2023;18:217–234. doi: 10.2217/fmb-2022-0141. [DOI] [PubMed] [Google Scholar]
- 5.Castrejón-Pérez AD, Welsh EC, Miranda I, Ocampo-Candiani J, Welsh O. Cutaneous mucormycosis. An Bras Dermatol. 2017;92:304–311. doi: 10.1590/abd1806-4841.20176614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Skiada A, Drogari-Apiranthitou M, Pavleas I, Daikou E, Petrikkos G. Global Cutaneous Mucormycosis: A Systematic Review. J Fungi (Basel) 2022;8:194. doi: 10.3390/jof8020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HS, Kim WS, Kim HK, Kang SH, Lee TJ, Hong SA, et al. Primary Mucormycosis Infection in the Submandibular Area After Esthetic Lipolytic Injection in An Immunocompetent Patient: A Case Report. Indian J Dermatol. 2022;67:58–61. doi: 10.4103/ijd.ijd_469_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Delie A, Vlummens P, Creytens D, Steel E. Cutaneous mucormycosis as result of insulin administration in an AML patient: Case report and review of the literature. Acta Clin Belg. 2017;72:352–356. doi: 10.1080/17843286.2016.1266802. [DOI] [PubMed] [Google Scholar]
- 9.Chambers CJ, Reyes Merin M, Fung MA, Huntley A, Sharon VR. Primary cutaneous mucormycosis at sites of insulin injection. J Am Acad Dermatol. 2011;64:e79–81. doi: 10.1016/j.jaad.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 10.Giacomazzi J, Baethgen L, Carneiro LC, Millington MA, Denning DW, Colombo AL, et al. The burden of serious human fungal infections in Brazil. Mycoses. 2016;59:145–150. doi: 10.1111/myc.12427. [DOI] [PubMed] [Google Scholar]


