Abstract
Purpose
We determined whether racial/ethnic differences in patient experiences with care influence timeliness and type of initial surgical breast cancer treatment for a sample of female Medicare cancer patients.
Methods
We conducted a retrospective cohort study using the linked Epidemiology and End Results-Consumer Assessment of Healthcare Providers and Systems (SEER-CAHPS) dataset. The outcomes were: (1) time-to-initial surgical treatment, and (2) type of treatment [breast conserving surgery (BCS) vs. mastectomy]. The indicators were reports of four types of patient experiences with care including doctor communication, getting care quickly, getting needed care, and getting needed Rx. Interaction terms in each multivariable logistic model examined if the associations varied by race/ethnicity.
Results
Of the 2069 patients, 84.6% were White, 7.6% Black and 7.8% Hispanic. After adjusting for potential confounders, non-Hispanic Black patients who provided excellent reports of their ability to get needed prescriptions had lower odds of receiving surgery within 2-months of diagnosis, compared to NH-Whites who provided less than excellent reports (aOR: 0.29, 95% CI 0.09–0.98). There were no differences based on 1-month or 3-month thresholds. We found no other statistically significant effect of race/ethnicity. As to type of surgery, among NH Blacks, excellent reports of getting care quickly were associated with higher odds of receiving BCS versus mastectomy (aOR: 2.82, 95% CI 1.16–6.85) compared to NH Whites with less than excellent reports. We found no other statistically significant differences by race/ethnicity.
Conclusion
Experiences with care are measurable and modifiable factors that can be used to assess and improve aspects of patient-centered care. Improvements in patient care experiences of older adults with cancer, particularly among minorities, may help to eliminate racial/ethnic disparities in timeliness and type of surgical treatment.
Keywords: Neoplasm, Cancer treatment, Surgery, Inequities, Quality care, Survivorship
Background
Breast cancer is the second leading cause of cancer death in the United States (US) [1]. Although breast cancer incidence is higher among non-Hispanic Whites compared to other race/ethnicities, mortality rates are higher for non-Hispanic Blacks [2]. The recommended initial treatment for most patients with early-stage breast cancer is surgical treatment [3]. Timeliness of initiation of treatment is considered a measure of high quality care [4], and minimizing time-to-surgery can positively impact cancer outcomes [5, 6]. Although optimal times from breast cancer diagnosis to initial treatment are not well established, many researchers examine one-month intervals to treatment [6–8], and have found that mortality increases with delays longer than two months [6, 9]. Initial surgical treatment options for early-stage breast cancer patients include breast conserving surgery (BCS) and mastectomy. Both options have comparable survival rates [10], and decisions to select initial surgical treatment often depend on providers’ recommendations and patients’ preferences [11–13]. Researchers have found that patient-based decisions about type of initial surgical treatment take into account concerns about cancer recurrence, risks and side effects related to radiation, and body image issues [11]. According to these findings, incorporating patients’ values and preferences are important for initial surgical treatment, but to date, no study has examined whether patient experiences with care impact timeliness and type of surgical treatment.
Racial/ethnic disparities in timeliness and receipt of type of surgery exist. Compared to non-Hispanic Whites, Black patients are less likely to receive initial surgical treatment within three months of their diagnosis [14, 15]. Minority patients receive BCS at lower rates than their White counterparts [16, 17]. In fact, Blacks are 42% less likely than Whites to receive BCS versus mastectomy [16], and Hispanics receive BCS at a lower frequency than Whites (37.1% vs 42.7%) [17]. Researchers have also found that the association between patient preferences and surgical treatment decisions vary by race/ethnicity [11]. However, the extent of the effect of race/ethnicity on the association between patient experiences and surgical treatment choices is yet to be explored. Patient experiences with care can indicate access, timeliness, communication with providers, and overall perceptions of encounters with physicians or specialists [18]. Racial/ethnic minorities tend to report poorer experiences compared to non-Hispanic White patients [19]. Positive reports of patient experiences with care are associated with high-quality cancer care and treatment [19–21]. Thus, it is also likely that the association between patient experiences and initial surgical care varies by race/ethnicity and might drive high-quality surgical care.
This study examined racial/ethnic disparities between four patient care experiences and (1) time to initial surgery and (2) type of initial surgery among women diagnosed with early-stage breast cancer. We hypothesized that the relation between patient care experiences on time to and type of initial breast cancer surgery varied by race/ethnicity.
Methods
Data source
We conducted a retrospective cohort study using data from SEER-CAHPS (surveillance, epidemiology, and end results—consumer assessment of healthcare providers and systems [22]). This linked dataset is a collaborative effort between the National Cancer Institute’s (NCI) Surveillance, Epidemiology, and End Results (SEER) cancer registry data and the Centers for Medicare and Medicaid Services’ (CMS) Medicare Consumer Assessment of Healthcare Providers and Systems (CAHPS). The SEER component of this dataset provides information on cancer statistics (1973–2013), the CMS component provides information on medical enrollment data and administrative and billing claims from Medicare beneficiaries enrolled in Fee for Service (FFS) plans (2002–2016), and the CAHPS survey component provides information from patients’ responses to surveys assessing experiences with care across different domains (1997–2015). The study was reviewed and granted exempt status by the UTHealth Committee for Protection of Human Subjects (HSC-SPH-20–0812).
Study population
The study population consisted of females with a primary and only diagnosis of early stage breast cancer, 65 or older (age at survey completion), who completed a CAHPS survey within 24 months prior to their cancer diagnosis, and who were continuously enrolled in Medicare for at least 11 of the 12 months prior to survey completion. We considered continuous enrollment as enrollment on the fifteenth day of the month for 12 consecutive months, with no more than one-month interruption. If beneficiaries completed multiple surveys, we used the survey collected closest to the cancer diagnosis date.
Exclusion criteria
We excluded patients diagnosed with multiple malignant cancer types, breast carcinoma in situ, or metastatic cancer, and those without a record of receiving breast cancer surgery as initial treatment because we were interested in examining type and time to initial cancer-directed surgery. We also excluded records with missing information on race/ethnicity and variable categories with insufficient variation of responses (Fig. 1).
Fig. 1.
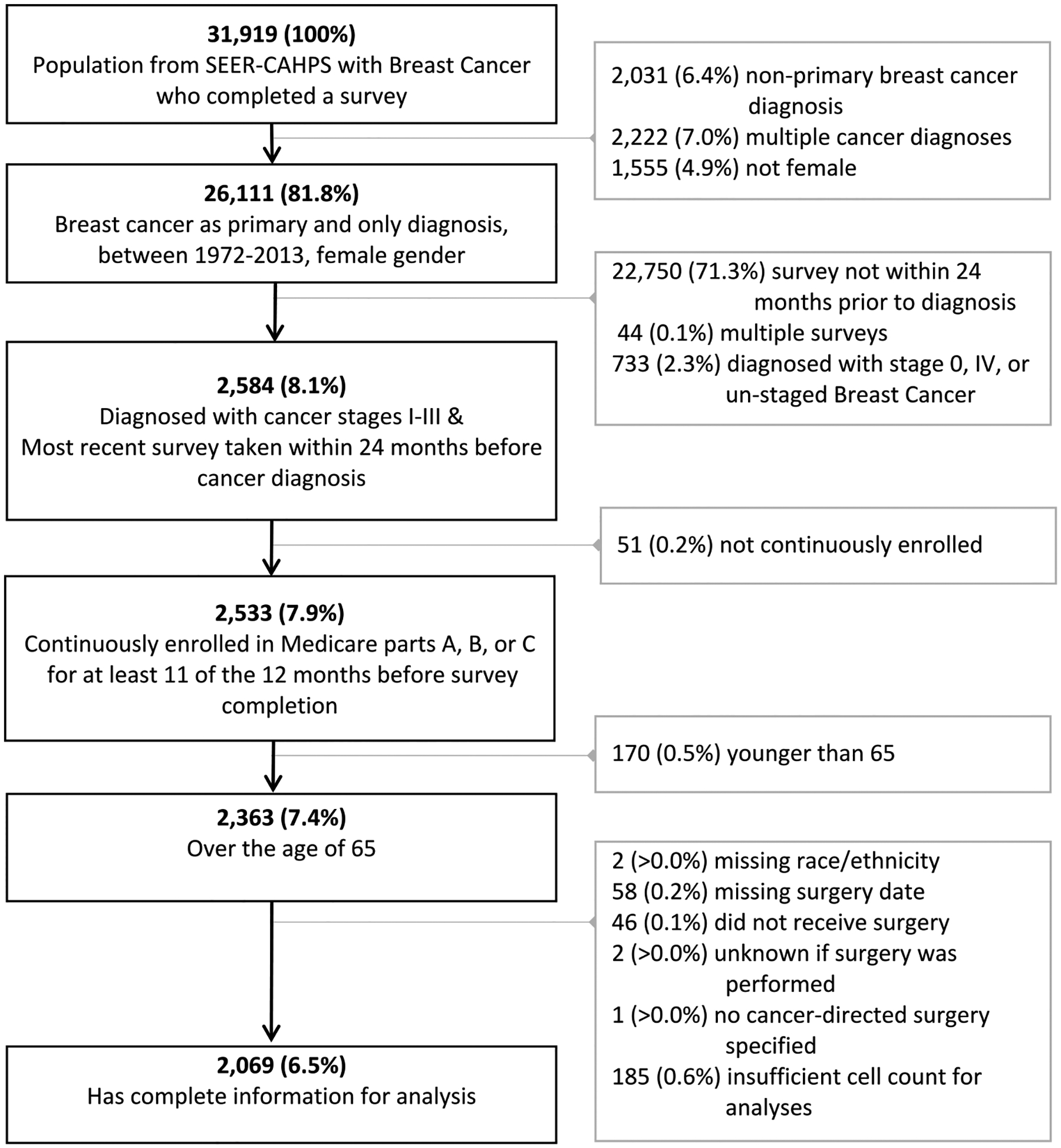
CONSORT diagram for study population
Outcomes
Time to initial surgical treatment was defined as months between diagnosis date and initial surgical treatment date. We used the SEER clinical diagnosis date (comprised of month and year) and assigned a midpoint for the day of diagnosis (15th of each month) to create each diagnosis date. Initial surgical treatment was created using the SEER initial course of treatment variable (consisting of month and year) and we assigned a midpoint for the day, as described above. Then, we created three outcome variables reflecting the time from diagnosis to initial surgical treatment, categorized as: less than or equal to 1 month, vs. otherwise; less than or equal to 2 months, vs. otherwise, less than or equal to 3 months, vs. otherwise. These categorizations were selected for comparability with other researchers who have used 1-month increments to assess timeliness of initial breast cancer treatment [6, 8].
Type of surgery was defined as receipt of BCS or mastectomy. We identified treatment information using a SEER variable which describes the surgical procedure performed as first course of cancer-directed therapy. Then we used SEER breast cancer surgical codes to dichotomize surgery type into: BCS (codes ≥ 20 and ≤ 39) or mastectomy (codes ≥ 40 and ≤ 80) [23].
Predictor variables
Patient experiences with care were assessed as multi-item composite scores of doctor communication, getting needed care, getting care quickly, and getting needed prescriptions. Survey respondents were asked about these domains thinking about their health care encounters in the last 6 months. A sample item is (getting care quickly): How often did you get care as soon as you thought you needed it? Each item was rated as 1 = never, 2 = sometimes, 3 = usually, and 4 = always. Composite items were scored using linear scoring [24], where higher scores indicated more positive assessments of reports of care. For ease of interpretation composite measures were transformed to a 0–100 scale. Because the CAHPS score distributions were negatively skewed, we dichotomized reports of patient experiences into less than excellent (0 to < 90 scores) and excellent reports of care (≥ 90–100 scores) [21, 25].
Covariates
The following covariates were included because they have been associated with time to surgical treatment and type of treatment received [26, 27]: disease stage, number of self-reported comorbidities, race/ethnicity, age at the time of survey completion, educational attainment, marital status, SEER geographic region, Medicare plan, survey administration mode, and year of survey completion. Analyses were adjusted for time since survey completion to account for changes over time.
Statistical analyses
Descriptive statistics were calculated to characterize the sample population. We used chi-square tests to examine sample characteristics across time-to-surgery categories of less than 1 month, between 1 and 2 months, and more than 2 months of diagnosis. We also used one-way ANOVA analyses to assess the mean scores of our selected patient care experiences across time-to-surgery categories. Next, we conducted multivariable logistic regression models adjusting for clinical and demographic characteristics to examine the relation between receiving timely initial surgical treatment and patient care experiences. To examine the effect of racial/ethnic background on the relation between care experiences on time-to-surgery, we included an interaction term (race/ethnicity by reports of patient care experiences) to each model. For type of surgery received, our second outcome, we conducted multivariable logistic regression analyses to examine the association between patient care experiences and type of surgical treatment received, while adjusting for clinical and demographic characteristics. Interaction terms were added to assess the effects of race/ethnicity on the relation between reports of care and surgery type.
We assessed the association between racial/ethnic background on timely receipt of surgical treatment and type of initial surgery received. First, we adjusted for demographics, then for demographic and clinical characteristics. Significance tests and confidence intervals for the estimates were 2-sided. All analyses were conducted in Stata statistical software version 16 [28].
Results
The analytic sample consisted of 2069 individuals (Fig. 1). The proportion of patients receiving surgery treatment within 1 month of diagnosis was 55%, between 1 and 2 months was 29%, and more than 2 months was 16%. The proportion of patients who received BCS was 58.6% vs. 41.4% who received mastectomy. Mean scores for getting needed care and getting prescription drugs were significantly different across racial/ethnic categories, but we found no mean differences by time-to-surgery categories or type of surgery (Table 1).
Table 1.
Demographic and clinical characteristics by time-to-surgery category, racial/ethnic background, and surgery type (N = 2069)
| Characteristic | Total sample, n (%) | Time from cancer diagnosis to initial surgical therapy | Racial/ethnic background | Surgical treatment type | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Less than 1 month, n = 1130 (55%) | Between 1 and 2 months, n = 604 (29%) | More than 2 months, n = 335 (16%) | P-value | Non-hispanic White (n = 1750) | Non-hispanic Black (n = 158) | Hispanic (n = 161) | P-value | Mastectomy (n = 856) 41.4% | BCS (n = 1213) 58.6% | P-value | ||
| Age at survey | ||||||||||||
| Median | 75.0 | 74.7 | 75.6 | 74.6 | 0.592 | 75.2 | 73.0 | 73.8 | <0.001 | 75.9 | 74.3 | 0.004 |
| Mean (SD) | 75.6 (6.4) | 75.5 (6.5) | 75.8 (6.0) | 75.7 (6.6) | 75.8 (6.4) | 73.9 (6.0) | 74.9 (5.9) | 76.1 (6.4) | 75.3 (6.3) | |||
| 66–69 | 471 (22.8) | 276 (24.4) | 118 (19.5) | 77 (23.0) | 0.172 | 379 (21.7) | 49 (31.0) | 43 (26.7) | 0.027 | 180 (21.0) | 291 (24.0) | 0.019 |
| 70–74 | 577 (27.9) | 311 (27.5) | 169 (28.0) | 97 (29.0) | 483 (27.6) | 49 (31.0) | 45 (27.9) | 218 (25.5) | 359 (29.6) | |||
| 75–79 | 501 (24.2) | 256 (22.7) | 171 (28.3) | 74 (22.1) | 424 (24.2) | 36 (22.8) | 41 (25.5) | 231 (27.0) | 270 (22.3) | |||
| 80–84 | 338 (16.3) | 187 (16.6) | 98 (16.2) | 53 (15.8) | 303 (17.3) | < 11% | < 12% | 142 (16.6) | 196 (16.2) | |||
| 85 + | 182 (8.8) | 100 (8.8) | 48 (8.0) | 34 (10.1) | 161 (9.2) | < 7% | < 7% | 85 (9.9) | 97 (8.0) | |||
| Race/ethnicity | 0.037 | – | 0.797 | |||||||||
| Non-hispanic White | 1,750 (84.6) | 973 (86.1) | 505 (83.6) | 272 (81.2) | – | – | – | 719 (84.0) | 1,031 (85.0) | |||
| Non-hispanic Black | 158 (7.6) | 83 (7.4) | 51 (8.4) | 24 (7.2) | – | – | – | 69 (8.1) | 89 (7.3) | |||
| Hispanic | 161 (7.8) | 74 (6.5) | 48 (8.0) | 39 (11.6) | – | – | – | 68 (7.9) | 93 (7.7) | |||
| Marital status | 0.971 | 0.006 | 0.714 | |||||||||
| Not married | 1,120 (54.1) | 610 (54.0) | 325 (53.8) | 185 (55.2) | 927 (53.0) | 108 (68.3) | 85 (52.8) | 462 (54.0) | 658 (54.3) | |||
| Married | 871 (42.1) | 475 (42.0) | <43% | <42% | 755 (43.1) | < 29% | < 42% | 365 (42.6) | 506 (41.7) | |||
| Unknown | 78 (3.8) | 45 (4.0) | <4% | <4% | 68 (3.9) | < 7% | < 7% | 29 (3.4) | 49 (4.0) | |||
| Education level | 0.165 | <0.001 | 0.024 | |||||||||
| High school or less | 1,165 (56.3) | 654 (57.9) | 321 (53.2) | 190 (56.7) | 945 (54.0) | 107 (67.7) | 113 (70.2) | 507 (59.2) | 658 (54.3) | |||
| Some college + | 904 (43.7) | 476 (42.1) | 283 (46.8) | 145 (43.3) | 805 (46.0) | 51 (32.3) | 48 (29.8) | 349 (40.8) | 555 (45.7) | |||
| Self-reported comorbidities | 0.194 | 0.014 | 0.149 | |||||||||
| 0 | 1,624 (78.5) | 899 (79.6) | 476 (78.8) | 249 (74.3) | 1397 (79.8) | 114 (72.2) | 113 (70.2) | 662 (77.3) | 962 (79.3) | |||
| 1 | 318 (15.4) | 166 (14.7) | 95 (15.7) | 57 (17.0) | 254 (14.5) | 31 (19.6) | 33 (20.5) | 131 (15.3) | 187 (15.4) | |||
| 2 + | 127 (6.1) | 65 (5.6) | 33 (5.5) | 29 (8.7) | 99 (5.7) | 13 (8.2) | 15 (9.3) | 63 (7.4) | 64 (5.3) | |||
| Tumor stage | 0.906 | 0.178 | <0.001 | |||||||||
| I | 1212 (58.6) | 662 (58.6) | 357 (59.1) | 193 (57.6) | 1,040 (59.4) | 84 (53.2) | 88 (54.6) | 352 (41.1) | 860 (70.9) | |||
| II–III | 857 (41.4) | 468 (41.4) | 247 (40.9) | 142 (42.4) | 710 (40.6) | 74 (46.8) | 73 (45.4) | 504 (58.9) | 353 (29.1) | |||
| Type of surgery | 0.438 | 0.797 | – | |||||||||
| Breast conserving | 1213 (58.6) | 655 (57.9) | 351 (58.2) | 207 (61.8) | 1,031 (58.9) | 89 (56.3) | 93 (57.8) | – | – | |||
| Mastectomy | 856 (41.4) | 475 (42.1) | 253 (41.8) | 128 (38.2) | 719 (41.1) | 69 (43.7) | 68 (42.2) | – | – | |||
| Medicare plan | <0.001 | <0.001 | 0.783 | |||||||||
| MA PDP | 430 (20.8) | 193 (17.1) | 148 (24.5) | 89 (26.6) | 327 (18.7) | 57 (36.1) | 46 (28.6) | 182 (21.3) | 248 (20.5) | |||
| MA only | 865 (41.8) | 504 (44.6) | 235 (38.9) | 126 (37.6) | 737 (42.1) | 53 (33.5) | 75 (46.6) | 354 (41.4) | 511 (42.1) | |||
| FFS PDP | 314 (15.2) | 162 (14.3) | 96 (15.9) | 56 (16.7) | 275 (15.7) | 22 (13.9) | 17 (10.6) | 136 (15.9) | 178 (14.7) | |||
| FFS only | 460 (22.2) | 271 (24.0) | 125 (20.7) | 64 (19.1) | 411 (23.5) | 26 (16.5) | 23 (14.2) | 184 (21.5) | 276 (22.7) | |||
| Geographic region | <0.001 | <0.001 | <0.001 | |||||||||
| West | 1159 (56.0) | 588 (52.0) | 356 (59.0) | 215 (64.2) | 992 (56.7) | 40 (25.3) | 127 (78.9) | 482 (56.3) | 677 (55.8) | |||
| Midwest | 181 (8.7) | 96 (8.5) | 60 (9.9) | 25 (7.5) | 158 (9.0) | <11% | <7% | 81 (9.5) | 100 (8.2) | |||
| North East | 322 (15.6) | 191 (16.9) | 79 (13.1) | 52 (15.5) | 278 (15.9) | 26 (16.5) | 18 (11.2) | 98 (11.4) | 224 (18.5) | |||
| South | 407 (19.7) | 255 (22.6) | 109 (18.5) | 43 (12.8) | 322 (18.4) | <48% | <7% | 195 (22.8) | 212 (17.5) | |||
| Survey administration mode | 0.639 | <0.001 | 0.388 | |||||||||
| 357 (17.3) | 197 (17.4) | 108 (17.9) | 52 (15.5) | 277 (15.8) | 37 (23.4) | 43 (26.7) | 155 (18.1) | 202 (16.7) | ||||
| Phone | 1712 (82.7) | 933 (82.6) | 496 (82.1) | 283 (84.5) | 1,473 (84.2) | 121 (76.6) | 118 (73.3) | 701 (81.9) | 1,011 (83.3) | |||
| Survey year | <0.001 | <0.001 | 0.099 | |||||||||
| 1997–2000 | 360 (17.4) | 234 (20.7) | 90 (14.9) | 36 (10.8) | 308 (17.6) | 23 (14.6) | 29 (18.0) | 167 (19.5) | 193 (15.9) | |||
| 2001–2005 | 787 (38.0) | 450 (39.8) | 217 (35.9) | 120 (35.8) | 689 (39.4) | 43 (27.2) | 55 (34.2) | 314 (36.7) | 473 (39.0) | |||
| 2007–2011 | 922 (44.6) | 446 (39.5) | 297 (49.2) | 179 (53.4) | 753 (44.0) | 92 (58.2) | 77 (47.8) | 375 (43.8) | 547 (45.1) | |||
| Time from survey to cancer diagnosis | 0.619 | 0.581 | 0.619 | |||||||||
| ≤ 6 months | 547 (26.4) | 291 (25.8) | 165 (27.3) | 91 (27.2) | 473 (27.0) | 35 (22.2) | 39 (24.2) | 221 (25.8) | 326 (26.9) | |||
| 6 to < 12 mo | 550 (26.6) | 299 (26.5) | 164 (27.2) | 87 (25.9) | 454 (26.0) | 46 (29.1) | 50 (31.1) | 230 (26.9) | 320 (26.4) | |||
| 12 to< 18 mo | 476 (23.0) | 254 (22.5) | 135 (22.4) | 87 (25.9) | 408 (23.3) | 34 (21.5) | 34 (21.1) | 188 (22.0) | 288 (23.7) | |||
| 18 to 24 mo | 496 (24.0) | 286 (25.3) | 140 (23.1) | 70 (21.0) | 415 (23.7) | 43 (27.2) | 38 (23.6) | 217 (25.3) | 279 (23.0) | |||
| Doctor communication (n = 1578) | 88.5 (16.8) | 88.2 (16.6) | 89.3 (16.4) | 87.8 (18.3) | 0.421 | 88.3 (17.0) | 88.4 (15.6) | 90.2 (16.4) | 0.515 | 89.1 (15.9) | 88.0 (17.4) | 0.186 |
| Getting care quickly (n = 1546) | 83.9 (23.2) | 84.3 (22.6) | 84.2 (23.1) | 82.1 (25.3) | 0.383 | 84.1 (22.7) | 80.0 (28.2) | 85.1 (24.3) | 0.182 | 84.9 (22.4) | 83.3 (23.7) | 0.194 |
| Getting needed care (n = 1701) | 88.3 (21.2) | 88.5 (21.5) | 88.7 (20.5) | 86.7 (21.3) | 0.422 | 89.0 (20.4) | 83.5 (26.2) | 84.4 (24.2) | 0.002 | 89.4 (20.4) | 87.5 (21.7) | 0.072 |
| Getting needed Rx (n = 1763) | 91.0 (20.5) | 90.8 (21.5) | 91.2 (20.0) | 91.6 (18.0) | 0.808 | 91.9 (19.4) | 83.9 (22.8) | 89.0 (22.8) | <0.001 | 90.2 (22.1) | 91.6 (19.3) | 0.134 |
P-value represents a two-sided t-test, chi-square test, or one-way ANOVA
mo months
CAHPS means are unadjusted
Association between racial/ethnic background and time to initial surgical treatment
We found that compared to non-Hispanic Whites, Hispanics had lower odds of receiving initial surgery within 2 months of diagnosis (aOR: 0.67, 95% CI 0.45–0.99), adjusting for demographic and clinical characteristics. There were no differences based on 1 month or 3 months thresholds. We did not find any significant differences in treatment initiation within 1, 2, or 3 months of diagnosis between non-Hispanic Black and non-Hispanic White patients (Table 2).
Table 2.
Results of multivariable models assessing the association between race/ethnicity and (a) time to surgical treatment (less than 1 month, less than 2 months, or less than 3 months from diagnosis), (b) type of surgery (BCS vs mastectomy)
| Time to surgerya | Treatment typeb | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤ 1 month | ≤ 2 months | ≤ 3 months | BCS vs mastectomy | |||||||||||
| Model° | N | OR | 95% | CI | OR | 95% | CI | OR | 95% | CI | N | OR | 95% | CI |
| Model 1: Unadjusted | 2069 | 2069 | 2069 | |||||||||||
| Non-hispanic Black | 0.88 | 0.64 | 1.22 | 1.03 | 0.65 | 1.62 | 0.90 | 0.65 | 0.90 | 0.65 | 1.25 | |||
| Hispanic | 0.68 * | 0.49 | 0.94 | 0.58 ** | 0.39 | 0.84 | 0.95 | 0.69 | 0.95 | 0.69 | 1.32 | |||
| Model 2: Adjusted for demographics | 2069 | 2069 | 2069 | |||||||||||
| Non-hispanic Black | 0.79 | 0.56 | 1.11 | 0.92 | 0.57 | 1.48 | 0.93 | 0.66 | 0.93 | 0.66 | 1.31 | |||
| Hispanic | 0.75 | 0.53 | 1.04 | 0.66* | 0.44 | 0.99 | 0.95 | 0.68 | 0.95 | 0.68 | 1.33 | |||
| Model 3: Adjusted for demographics and clinical characteristics | 2069 | 2069 | 2069 | |||||||||||
| Non-hispanic Black | 0.78 | 0.56 | 1.10 | 0.93 | 0.58 | 1.50 | 1.02 | 0.71 | 1.02 | 0.71 | 1.48 | |||
| Hispanic | 0.74 | 0.53 | 1.04 | 0.67 * | 0.45 | 0.99 | 1.01 | 0.72 | 1.01 | 0.72 | 1.45 | |||
Reference category is non-hispanic Whites
Models were adjusted for: age, marital status, SEER geographic region, self-reported comorbidities, tumor stage, type of surgery, medicare plan, survey administration mode, survey year, and time since survey
Modeling odds of breast conserving surgery(BCS) vs mastectomy adjusted for: age, marital status, SEER geographic region, self-reported comorbidities, tumor stage, medicare plan, survey administration mode, survey year, and time since survey Bold represents significant at
p < 0.05,
p < 0.01, ***p < 0.001
Effect of race/ethnicity on the association between patient care experiences and time to initial surgical treatment
Among Blacks, excellent reports of getting needed prescriptions were associated with lower odds of getting surgery within 2 months of diagnosis (aOR 0.29, 95% CI 0.09–0.98; Table 3), compared to Whites with less than excellent reports. We found no other statistically significant effect of race/ethnicity on the association between experiences with care and time to surgery.
Table 3.
Results of models assessing the effect of race/ethnicity on the relation between composite measures of patient experiences and time to initial surgical treatment
| Time to surgery | ≤ 1 month | ≤ 2 months | ≤ 3 months | ≤ 1 month | ≤ 2 months | ≤3 months | ≤ 1 month | ≤ 2 months | ≤3 months | ≤ 1 month | ≤ 2 months | ≤ 3 months | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N analyzed | 1578 | 1578 | 1578 | 1546 | 1546 | 1546 | 1701 | 1701 | 1701 | 1763 | 1763 | 1731† | ||||||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| CAHPS measure | Doctor communication | Getting care quickly | Getting needed care | Getting needed Rx | ||||||||||||||||||||
| Less than excellent | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | ||||||||||||
| Excellent reports | 0.88 | [0.69–1.12] | 1.19 | [0.86–1.64] | 1.75 | [0.84–3.64] | 0.96 | [0.76–1.20] | 1.08 | [0.80–1.47] | 0.87 | [0.42–1.80] | 1.01 | [0.80–1.27] | 1.15 | [0.85–1.57] | 0.83 | [0.39–1.78] | 1.12 | [0.87–1.45] | 1.33 | [0.95–1.86] | 1.95 | [0.98–3.88] |
| Race/ethnicity | ||||||||||||||||||||||||
| NH White | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | ||||||||||||
| NH Black | 0.98 | [0.49–1.93] | 2.37 | [0.70–8.05] | 1.05 | [0.13–8.56] | 0.79 | [0.42–1.49] | 0.82 | [0.36–1.88] | 0.21 * | [0.06–0.75] | 0.70 | [0.37–1.31] | 0.94 | [0.41–2.15] | 0.24 * | [0.07–0.86] | 0.89 | [0.47–1.69] | 2.30 | [0.78–6.78] | 0.75 | [0.16–3.56] |
| Hispanic | 0.74 | [0.36–1.52] | 1.11 | [0.43–2.84] | 1.55 | [0.19–12.6] | 0.50 * | [0.25–0.99] | 0.79 | [0.35–1.74] | 0.98 | [0.12–7.90] | 0.53 * | [0.28–0.99] | 0.61 | [0.30–1.23] | 0.25 * | [0.07–0.86] | 0.83 | [0.39–1.74] | 1.14 | [0.44–2.95] | 0.35 * | [0.14–0.87] |
| Interactions | ||||||||||||||||||||||||
| White *less than excellent | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | ||||||||||||
| Black *excellent reports | 0.62 | [0.27–1.43] | 0.30 | [0.08–1.17] | 0.31 | [0.03–3.35] | 1.00 | [0.44–2.28] | 1.51 | [0.49–4.67] | 7.67 | [0.71–82.78] | 1.29 | [0.58–2.86] | 1.17 | [0.39–3.50] | 1.86 | [0.32–10.82] | 0.95 | [0.44–2.06] | 0.29 * | [0.09–0.98] | 0.53 | [0.08–3.52] |
| Hispanic * excellent reports | 1.02 | [0.43–2.39] | 0.56 | [0.19–1.64] | 0.49 | [0.04–5.59] | 1.81 | [0.78–4.19] | 0.62 | [0.24–1.64] | 0.48 | [0.05–4.88] | 1.28 | [0.58–2.82] | 1.02 | [0.41–2.54] | 8.91 | [0.84–94.65] | 0.93 | [0.39–2.18] | 0.40 | [0.14–1.15] | 1.00 | |
Separate logistic regression models for each CAHPS measure were conducted; all models were adjusted for: age, marital status, SEER geographic region, self-reported comorbidities, tumor stage, type of surgery, medicare plan, survey administration mode, survey year, and time since survey
NH non-hispanic, Rx prescriptions
n = 1731 because of low variability of distribution of reports of getting needed drugs by outcome (surgery < 3 months) among Hispanic; Bold represents significant at
p < 0.05, **p < 0.01, ***p < 0.001
Association between racial/ethnic background and type of surgical treatment
We did not find any statistically significant differences of type of surgery across racial and ethnic groups. Before adjusting for demographic and clinical characteristics, minority patients had lower odds of receiving BCS versus mastectomy compared to non-Hispanic Whites; though, this relation was not statistically significant. After also adjusting for clinical characteristics, the odds ratio showed no association between type of initial surgery and race/ethnic background (Table 2).
Effect of race/ethnicity on the association between patient care experiences and type of surgical treatment
Among Blacks, excellent reports of their ability to get care quickly were associated with increased odds of getting BCS versus mastectomy (aOR 2.82, 95% CI 1.16–6.85; Table 4), compared to Whites with less than excellent reports. We found no other statistically significant differences by race/ethnicity on the association between care experiences and type of initial surgery received.
Table 4.
Results of models assessing the effect of race/ethnicity on the relation between patient experiences and type of initial surgical treatment (BCS vs mastectomy)
| Surgical type | BCS | BCS | BCS | BCS | ||||
|---|---|---|---|---|---|---|---|---|
| OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | OR | [95% CI] | |
| N analyzed | 1578 | 1546 | 1701 | 1763 | ||||
| CAHPS measure | Doctor communication | Getting care quickly | Getting needed care | Getting needed Rx | ||||
| Less than excellent reports | Ref | Ref | Ref | Ref | ||||
| Excellent reports | 0.85 | [0.66–1.10] | 0.86 | [0.68–1.10] | 0.83 | [0.65–1.06] | 1.07 | [0.82–1.40] |
| Race/ethnicity | ||||||||
| Non-hispanic White | Ref | Ref | Ref | Ref | ||||
| Non-hispanic Black | 1.13 | [0.56–2.30] | 0.65 | [0.33–1.27] | 0.71 | [0.37–1.37] | 1.02 | [0.52–2.00] |
| Hispanic | 0.95 | [0.44–2.02] | 1.23 | [0.59–2.55] | 1.37 | [0.70–2.68] | 1.04 | [0.48–2.27] |
| Race by reports of care interactions | ||||||||
| White * less than excellent reports | Ref | Ref | Ref | Ref | ||||
| Black * excellent reports | 0.96 | [0.40–2.27] | 2.82 * | [1.16–6.85] | 1.97 | [0.85–4.57] | 1.07 | [0.48–2.42] |
| Hispanic * excellent report | 1.26 | [0.51–3.11] | 0.99 | [0.40–2.42] | 0.61 | [0.26–1.39] | 1.05 | [0.43–2.56] |
Modeling odds of BCS (breast conserving surgery vs mastectomy)
Excellent reports consist of scores 90–100, and less than excellent reports consist of scores ≤ 89.99.
Separate logistic regression models were conducted for each patient experience measure
Models were adjusted for: age, race/ethnicity, marital status, SEER geographic region, self-reported comorbidities, tumor stage, medicare plan, survey administration mode, survey year, and time since survey.
Bold represents significant at
p < 0.05, **p < 0.01, ***p < 0.001
Discussion
We found that the association of patient care experiences with time to and type of initial breast cancer surgery varies for patients of diverse racial/ethnic backgrounds. Previous studies have found racial/ethnic differences in reports of patient care experiences [19], but to our knowledge this is the first study to determine differential effects of race/ethnicity on time to and type of initial breast cancer surgical treatment. Our study is in line with national imperatives for impacting health disparities as outlined by the Agency for Healthcare Research and Quality urging the assessment of relevant patient-centered care factors for at-risk populations [29].
Our findings also showed that Hispanics had lower odds of receiving initial breast cancer surgery within 2 months of diagnosis, compared to non-Hispanic Whites. This is consistent with other studies which have found that Hispanics experience longer-than-6-weeks delays in receipt of initial breast cancer surgical treatment more frequently than non-Hispanic Whites (15.3% vs 8.1%, respectively) [30]. Other studies have found that socio-demographic and clinical factors are associated with delays in surgical treatment [7]. Our study went further by adjusting for potential confounders and still found that race/ethnic background contributes to delays in receipt of timely initial breast cancer treatment.
Other researchers have found that Black patients are less likely to report excellent experiences with care [19] and more likely to experience delays in receiving initial breast cancer treatment [4, 31, 32]. We found that Black patients who provided excellent reports of care had lower odds of receiving surgical treatment within 2 months of their diagnosis. This was contrary to our expectations, yet these findings could reflect that care experiences among Black patients, although reported as excellent, can still be associated with deficits in health care delivery impacting cancer care. Findings from qualitative research conducted with Black patients highlight the discordance between high reports of care experiences and accounts of their actual experiences of sub-optimal care, including experiencing racial discrimination [33]. Perceived discrimination interferes with receipt of quality care for Blacks [34]. Thus, examining the gradient of reports in patient care experiences among racial/ethnic minorities can help understand the substantive meanings of their reports and aid in efforts to achieve culturally-sensitive delivery of care.
Our findings also showed that among Blacks, excellent reports of their ability to get care quickly were associated with higher odds of BCS versus mastectomy. These findings may be related to access barriers. It has been previously reported that racial/ethnic minorities have limited access to radiation oncology specialists that may be needed for adjuvant radiation following BCS [35]. In this study, patients’ excellent reports of their ability to get care quickly could be an indication that they had access to radiation oncologist services, and elected BCS because they would have been able to receive adjuvant radiation following their surgery. The pathway concerning the relation between patient experiences with care and receipt of BCS requires further study. Future research should explore other factors that may play a role in that pathway, such as confidence in obtaining needed care. The relation between patient experiences with care and breast cancer surgical care has been understudied. In fact, most investigators have focused on examining patients’ beliefs, values and preferences related to surgery type [36], but have not assessed patient experiences with care. Due to space limitations, our findings on the relation between patient experiences with care and surgical outcomes can be found as supplementary material (Appendices A and B).
The clinical and research implications of our study are centered around the differential effects of race/ethnicity on patient care experiences and surgical treatment. First, perceptions of minority patients about their care are not static experiences and should be assessed through the care continuum. Second, reports of experiences with care are measurable and modifiable factors that could be addressed by future interventions to improve the delivery of high-quality care. Lastly, routine assessment of experiences with care among racial/ethnic minorities is needed to achieve an equitable and patient-centered healthcare system in the U.S.
Strengths and limitations
Our findings should be considered in the context of several strengths and limitations. Previous published studies indicated that patient care experiences are associated with improved outcomes; however, only recently, have investigators examined the association between patient care experiences and cancer-related outcomes [37]. Thus, our findings advance the body of knowledge about the role of patient care experiences on cancer-related care and highlight the need to include the assessment of these experiences in frameworks of cancer care. We capitalized on the opportunity to use the SEER-CAHPS linked data resource to investigate racial/ethnic disparities in the association between patient care experiences and the type and timeliness of surgical breast cancer treatment. Our findings support the importance of improving the delivery of care among minorities experiencing inequities in cancer care. One of our study limitations concerns the focus on BCS versus mastectomy to the exclusion of receipt of radiation therapy following BCS. Second, this study did not separate mastectomy into unilateral, bilateral or surgery with reconstruction types. Although we believe that these treatment types are important to examine, we wanted to assess receipt of initial treatment. We hope to explore other outcomes in subsequent studies. Third, while we adjusted our multivariable models for demographic and clinical characteristics, we did not adjust for clinical factors such as tumor size, nodal status, genetic mutations that are associated with receipt of mastectomy, facility type where cancer care was obtained, or the type of physician on whom patients based their reports. Fourth, our findings are presented with the caveat that racial/ethnic minorities are less likely to respond to patient care experience surveys [38] and have greater rates of missing responses than Whites [39], which might result in under-representation of responses from minority groups. Lastly, our study findings may not be relevant to younger women or generalizable to all Medicare populations.
Conclusions
Our study contributes findings related to racial/ethnic disparities in receipt of initial breast cancer surgery among older Medicare beneficiaries. Examining patient care experiences with care can help assess aspects of patient-centered care that could be enhanced or improved (e.g., communication with providers, promptness of care, accessibility of needed care, and overall evaluations of care). Our findings can help inform policies to improve access and availability of care and can identify patient-centered practices that may ultimately lead to improved delivery of care.
Supplementary Material
Acknowledgements
This study used the linked SEER-CAHPS data resource. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; the Centers for Medicare & Medicaid Services; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-CAHPS data resource.
Funding
Efforts by Mariana Arevalo, PhD, MSPH were supported by a pre-doctoral fellowship at the University of Texas Health Science Center at Houston, School of Public Health, Susan G. Komen Traineeship in Breast Cancer Disparities (GTDR14300827). SEER-CAHPS data were procured by Albert J. Farias, PhD with support from a University of Texas Health Science Center at Houston School of Public Health Cancer Education and Career Development Program grant from the National Cancer Institute (R25-CA57712). Efforts by Trevor A. Pickering, PhD, MS were supported by grants UL1TR001855 and UL1TR000130 from the National Center for Advancing Translational Science (NCATS) of the U.S. National Institutes of Health. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the funding bodies.
Abbreviations
- US
United States
- BCS
Breast conserving surgery
- SEER-CAHPS
Surveillance, epidemiology, and end results—consumer assessment of healthcare providers and systems
- NCI
National Cancer Institute
- SEER
Surveillance, epidemiology, and end results
- CMS
Centers for medicare and medicaid services
- CAHPS
Medicare consumer assessment of healthcare providers and systems
- FFS
Fee for service
- ANOVA
Analysis of variance
Footnotes
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s10549-023-07148-y.
Conflict of interest Authors have no relevant financial or non-financial interests to disclose.
Ethical approval The study was reviewed and granted exempt status by the UTHealth Committee for Protection of Human Subjects (HSC-SPH-20–0812).
Patient consent to participate This study used a large population-based dataset with unidentifiable patient information.
Data availability
Codes are available from the corresponding author upon reasonable request. SEER-CAHPS linked dataset used for this manuscript is publicly available through the National Cancer Institute, Division of Cancer Control and Population Sciences.
References
- 1.United States Cancer Statistics Working Group (2020) “U.S. Cancer Statistics Data Visualizations Tool, based on 2019 submission data (1999–2017).” United States Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. www.cdc.gov/cancer/dataviz. Released in June 2020. Accessed June, 2020 [Google Scholar]
- 2.American Cancer Society (2019) “Breast Cancer Facts and Figures 2019–2020, ” American Cancer Society, Atlanta, 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf [Google Scholar]
- 3.Moo TA, Sanford R, Dang C, Morrow M (2018) Overview of breast cancer therapy. PET Clin 13(3):339–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halpern M, Holden D (2012) Disparities in timeliness of care for US Medicare patients diagnosed with cancer. Curr Oncol 19(6):e404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright GP, Wong JH, Morgan JW, Roy-Chowdhury S, Kazanjian K, Lum SS (2010) Time from diagnosis to surgical treatment of breast cancer: factors influencing delays in initiating treatment. Am Surg 76(10):1119–1122 [PubMed] [Google Scholar]
- 6.Bleicher RJ et al. (2016) “Time to surgery and breast cancer survival in the United States,” (in eng). JAMA Oncol 2(3):330–339. 10.1001/jamaoncol.2015.4508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Padilla-Ruiz M et al. (2020) Factors that influence treatment delay for patients with breast cancer. Ann Surg Oncol 28:1–8 [DOI] [PubMed] [Google Scholar]
- 8.Ho PJ, Cook AR, Binte NK, Ri M, Liu J, Li J, Hartman M (2020) Impact of delayed treatment in women diagnosed with breast cancer: a population-based study. Cancer Med 9(7):2435–2444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richards M, Westcombe A, Love S, Littlejohns P, Ramirez A (1999) Influence of delay on survival in patients with breast cancer: a systematic review. The Lancet 353(9159):1119–1126 [DOI] [PubMed] [Google Scholar]
- 10.Fisher B et al. (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347(16):1233–1241 [DOI] [PubMed] [Google Scholar]
- 11.Hawley ST et al. (2009) Decision involvement and receipt of mastectomy among racially and ethnically diverse breast cancer patients. J Natl Cancer Inst 101(19):1337–1347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morrow M et al. (2009) Surgeon recommendations and receipt of mastectomy for treatment of breast cancer. JAMA 302(14):1551–1556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katz SJ et al. (2005) Patient involvement in surgery treatment decisions for breast cancer. J Clin Oncol 23(24):5526–5533 [DOI] [PubMed] [Google Scholar]
- 14.Silber JH et al. (2013) Characteristics associated with differences in survival among black and white women with breast cancer. JAMA 310(4):389–397 [DOI] [PubMed] [Google Scholar]
- 15.Sheppard VB et al. (2015) Disparities in breast cancer surgery delay: the lingering effect of race. Ann Surg Oncol 22(9):2902–2911 [DOI] [PubMed] [Google Scholar]
- 16.Mandelblatt J et al. (2005) “Breast cancer prevention in community clinics: will low-income Latina patients participate in clinical trials?” (in eng). Prev Med 40(6):611–618. 10.1016/j.ypmed.2004.09.004 [DOI] [PubMed] [Google Scholar]
- 17.Morris CR, Cohen R, Schlag R, Wright WE (2000) Increasing trends in the use of breast-conserving surgery in California. Am J Public Health 90(2):281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anhang Price R et al. (2014) “Examining the role of patient experience surveys in measuring health care quality” (in eng). Med Care Res Rev 71(5):522–554. 10.1177/1077558714541480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Farias AJ, Ochoa CY, Toledo G, Bang SI, Hamilton AS, Du XL (2020) “Racial/ethnic differences in patient experiences with health care in association with earlier stage at breast cancer diagnosis: findings from the SEER-CAHPS data” (in eng). Cancer Causes Control 31(1):13–23. 10.1007/s10552-019-01254-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farias AJ, Toledo G, Ochoa CY, Hamilton AS (2021) Racial/ethnic disparities in patient experiences with health care in association with earlier stage at colorectal cancer diagnosis: findings from the SEER-CAHPS data. Med Care 59(4):295–303 [DOI] [PubMed] [Google Scholar]
- 21.Mollica MA et al. (2017) “Examining colorectal cancer survivors’ surveillance patterns and experiences of care: a SEER-CAHPS study” (in eng). Cancer Causes Control 28(10):1133–1141. 10.1007/s10552-017-0947-2 [DOI] [PubMed] [Google Scholar]
- 22.Chawla N et al. (2015) “Unveiling SEER-CAHPS®: a new data resource for quality of care research” (in eng). J Gen Intern Med 30(5):641–650. 10.1007/s11606-014-3162-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Cancer Institute. “Surgery Codes Breast” https://seer.cancer.gov/archive/manuals/2011/Surgery_Codes_Breast_09272011.pdf. Accessed Oct 2020
- 24.National Cancer Institute. “Guidance on analytic approaches when modeling items and composites in analyses using SEER-CAHPS data”. https://healthcaredelivery.cancer.gov/seer-cahps/researchers/approaches_guidance.html. Accessed 19 Oct 2019
- 25.Lines LM, Cohen J, Halpern MT, Smith AW, Kent EE (2019) “Care experiences among dually enrolled older adults with cancer: SEER-CAHPS, 2005–2013” (in eng). Cancer Causes Control 30(10):1137–1144. 10.1007/s10552-019-01218-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Halpern MT, Urato MP, Kent EE (2017) “The health care experience of patients with cancer during the last year of life: analysis of the SEER-CAHPS data set” (in eng). Cancer 123(2):336–344. 10.1002/cncr.30319 [DOI] [PubMed] [Google Scholar]
- 27.Wilson RT et al. (2007) Disparities in breast cancer treatment among American Indian, Hispanic and non-Hispanic white women enrolled in Medicare. J Health Care Poor Underserved 18(3):648–664 [DOI] [PubMed] [Google Scholar]
- 28.Stata Statistical Software (2019) StataCorp LP, College Station, TX [Google Scholar]
- 29.Agency for Healthcare Research and Quality. “Six Domains of Health Care Quality.” https://www.ahrq.gov/talkingquality/measures/six-domains.html
- 30.Smith EC, Ziogas A, Anton-Culver H (2013) Delay in surgical treatment and survival after breast cancer diagnosis in young women by race/ethnicity. JAMA Surg 148(6):516–523 [DOI] [PubMed] [Google Scholar]
- 31.Selove R et al. (2016) Time from screening mammography to biopsy and from biopsy to breast cancer treatment among Black and White, women Medicare beneficiaries not participating in a health maintenance organization. Womens Health Issues 26(6):642–647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gorin SS, Heck JE, Cheng B, Smith SJ (2006) “Delays in breast cancer diagnosis and treatment by racial/ethnic group” (in eng). Arch Intern Med 166(20):2244–2252. 10.1001/archinte.166.20.2244 [DOI] [PubMed] [Google Scholar]
- 33.Ochoa CY, Toledo G, Iyawe-Parsons A, Navarro S, Farias AJ (2021) Multilevel influences on black cancer patient experiences with care: a qualitative analysis. JCO Oncol Pract 17(5):e645–e653 [DOI] [PubMed] [Google Scholar]
- 34.Cuevas AG, O’Brien K, Saha S (2016) African American experiences in healthcare: “I always feel like I’m getting skipped over.” Health Psychol 35(9):987. [DOI] [PubMed] [Google Scholar]
- 35.Bellavance EC, Kesmodel SB (2016) Decision-making in the surgical treatment of breast cancer: factors influencing women’s choices for mastectomy and breast conserving surgery. Front Oncol 6:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gu J, Groot G, Boden C, Busch A, Holtslander L, Lim H (2018) Review of factors influencing women’s choice of mastectomy versus breast conserving therapy in early stage breast cancer: a systematic review. Clin Breast Cancer 18(4):e539–e554 [DOI] [PubMed] [Google Scholar]
- 37.Mohan CS et al. (2020) The association between patient experience and healthcare outcomes using SEER-CAHPS patient experience and outcomes among cancer survivors. J Geriatr Oncol 12:623–631 [DOI] [PubMed] [Google Scholar]
- 38.Anhang Price R et al. (2022) A systematic review of strategies to enhance response rates and representativeness of patient experience surveys. Med Care 60(12):910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klein DJ et al. (2011) Understanding nonresponse to the 2007 medicare CAHPS survey. Gerontologist 51(6):843–855. 10.1093/geront/gnr046 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Codes are available from the corresponding author upon reasonable request. SEER-CAHPS linked dataset used for this manuscript is publicly available through the National Cancer Institute, Division of Cancer Control and Population Sciences.


