Abstract
Key Clinical Message
Chin augmentation by hyaluronic acid filler injection rarely causes abnormal bone resorption in the mentum. Thus, when taking the history of a patient with jaw deformity, it is imperative to check the history of treatment of the mentum.
Abstract
Hyaluronic acid (HA) filler injection is a common procedure in nonsurgical cosmetic chin augmentation. Due to its high biocompatibility and simple injection technique, HA filler injection is a popular procedure. However, adverse events such as allergic reactions and foreign body reactions have been reported in some cases. In this study, we report a case of skeletal Class II jaw deformity in which bone resorption was observed in the mentum after HA filler injection. The purpose of this study is to discuss the indications for HA filler injection in skeletal Class II cases that require orthognathic surgery. The patient was a 30‐year‐old woman. To improve retrusion of the mentum, she has been receiving HA filler injections in the mentum three times every 6 months in the cosmetic surgery clinic since 2015. However, the retrusion of the mentum did not improve, which prompted here to visit the orthodontic clinic. Radiographs and CT revealed bowl‐shaped bone resorption surrounding the foreign bodies in the mentum. She was diagnosed with maxillary protrusion, vertical maxillary excess, mandibular retrusion, and bilateral condylar resorption. Bimaxillary orthognathic surgery (BOGS) and removal of residual HA fillers were planned after completion of the preoperative orthodontic treatment. After BOGS, the foreign bodies were completely removed, and the resorption cavities were filled with excess bone segments from the surgical sites. X‐ray photoelectron spectroscopy analysis of the foreign bodies suggested the presence of HA. One year after the BOGS, no progression of condylar resorption occurred, and bone healing at the mentum had a good prognosis. Therefore, the patient underwent reduction and advancement genioplasty. She was satisfied with her facial profile and occlusal function. Unexpected bone resorption in the mentum caused by HA filler injection is often discovered incidentally. Although, patients may feel hesitant to confess their history of treatment of the mentum, it is important to ensure that they are carefully interviewed.
Keywords: bone resorption, chin augmentation, hyaluronic acid (HA), orthognathic surgery
1. INTRODUCTION
Hyaluronic acid (HA) filler injection has been widely used in plastic and cosmetic surgeries for soft tissue augmentation and facial wrinkle reduction. 1 , 2 HA filler injection is a popular procedure compared with genioplasty owing to its convenience, immediate effect, and safety. 3 , 4 , 5 HA is a natural acidic mucopolysaccharide and is an important component of the skin, subcutaneous tissue, vitreous humor, synovial membrane, and synovial fluid, 6 , 7 and widely used in orthopedics to relieve joint pain from osteoarthritis or rheumatoid arthritis. Owing to its excellent biocompatibility, HA is resistant to infections, allergic reactions, and foreign body reactions. It is degraded and resorbed in vivo within 3–6 months. 8 , 9 Contrarily, chemically modified HA is stabilized for long‐term retention via chemical cross‐linking. 10 , 11 In 2003, the use of synthetic HA derivatives was approved by the Food and Drug Administration in the United States for soft tissue augmentation. At present, they are widely used for nonsurgical chin augmentation.
In some cases, retrusion of the mentum is accompanied by skeletal problems such as mandibular retrusion, condylar resorption, and vertical maxillary excess. In these cases, appropriate orthodontic skeletal assessment and subsequent orthognathic surgery are essential for skeletal improvement. However, there is a trend toward an increase in the volume and frequency of HA filler injections in patients seeking nonsurgical treatment for skeletal problems. Unexpected bone resorption of the mentum has been reported as a rare adverse event; although, the potential adverse effects of HA filler injection are minimal, as aforementioned. 12 , 13 In a retrospective study, Guo et al. 13 analyzed the clinical factors causing bone resorption with HA filler injection and found that bone resorption was associated with the volume of HA injected each time, the frequency of injection, and the interval between injections. Herein, we report a case of jaw deformity with bone resorption in the mentum after HA filler injection. We conducted X‐ray photoelectron spectroscopy (XPS) analysis to identify the foreign body substance. Our results suggested that the foreign body was HA.
2. CASE PRESANTATION
2.1. Case history
A 30‐year‐old woman visited a cosmetic surgery clinic with a chief complaint of esthetic disorder due to retrusion of the mentum. Since 2015, she has been receiving HA filler injections three times every 6 months to 1 year. However, the retrusion of the mentum did not improve. Thus, she visited an orthodontic clinic in August 2021, where she was diagnosed with skeletal maxillary protrusion with vertical maxillary excess and skeletal mandibular retrusion with condylar resorption. After 6 months of follow‐up, the condylar resorption did not improve, so preoperative orthodontic treatment was initiated. In July 2022, after completion of preoperative orthodontic treatment, the patient visited our department for orthognathic surgery. The patient had no medical history, family history, hereditary diseases, or diseases currently under treatment. The course of the treatment over time is summarized and illustrated in a flow chart in Figure 1.
FIGURE 1.
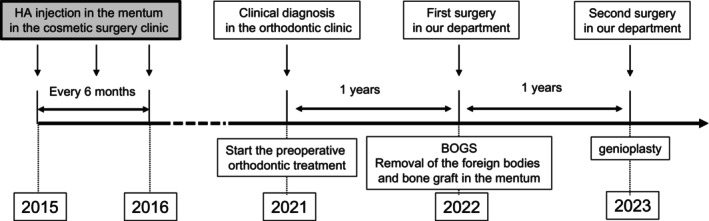
Flow‐chart of the course of treatment.
2.2. Diagnosis and treatment
At the initial visit, her facial appearance was asymmetric and dolichofacial, and her lateral appearance was convex (Figure 2A). She had difficulty with lip closure and had a gummy smile that exposure of the maxillary alveolar gingiva was about 7 mm at smiling. Intra‐oral examination indicated a bilateral Class II molar relationship. The upper and lower dental midline was aligned to the facial midline. The patient had proclined upper incisors with an overjet of 3 mm (Figure 2B). The radiographic findings were reduced bilateral mandibular ramus with bilateral mandibular head resorption and mandibular retrusion (Figure 2C, D). The patient had no temporomandibular joint symptoms; however, imaging examination showed erosion and osteosclerosis of the bilateral condylar heads (Figure 2E, F). Two bilateral concavities and radiopaque foreign bodies were detected in the mentum (Figure 3). Based on the diagnosis of skeletal Class II, maxillary protrusion with vertical maxillary excess, skeletal mandibular retrusion with condylar resorption, and bone resorption in the mentum induced by foreign bodies, bimaxillary orthognathic surgery (BOGS) (Le Fort I osteotomy, inverted L‐shaped ramus osteotomy (ILRO)), and extraction of foreign bodies in the mentum were performed in July 2022. The planned movement of each landmark was U1; 7 mm up, PNS; 4 mm up, U6; 5.5 mm up, LL6; 3.2 mm advance, LR6; 3.8 mm advance, Pog; 8.0 mm advance, and the bone gap was approximately 4 mm at the margin of mandible body. After placing the patient in the planned position based on preoperative virtual planning, the maxilla and mandible were fixed with absorbable plates and a T‐shaped titanium plates, respectively (Figure 4A). As presented in Figure 4B, clear, elastic, and soft foreign bodies were detected under the periosteum in the mentum. Although there was no evidence of infection, the foreign bodies were carefully dissected because of their adhesion to the periosteum and scar tissue. Residual bone from the osteotomy was grafted onto the dish‐shaped bone defects after the foreign body removal. Decortication was not performed because there was blood supply from the perforator vessels from the bottom of bone defects.
FIGURE 2.
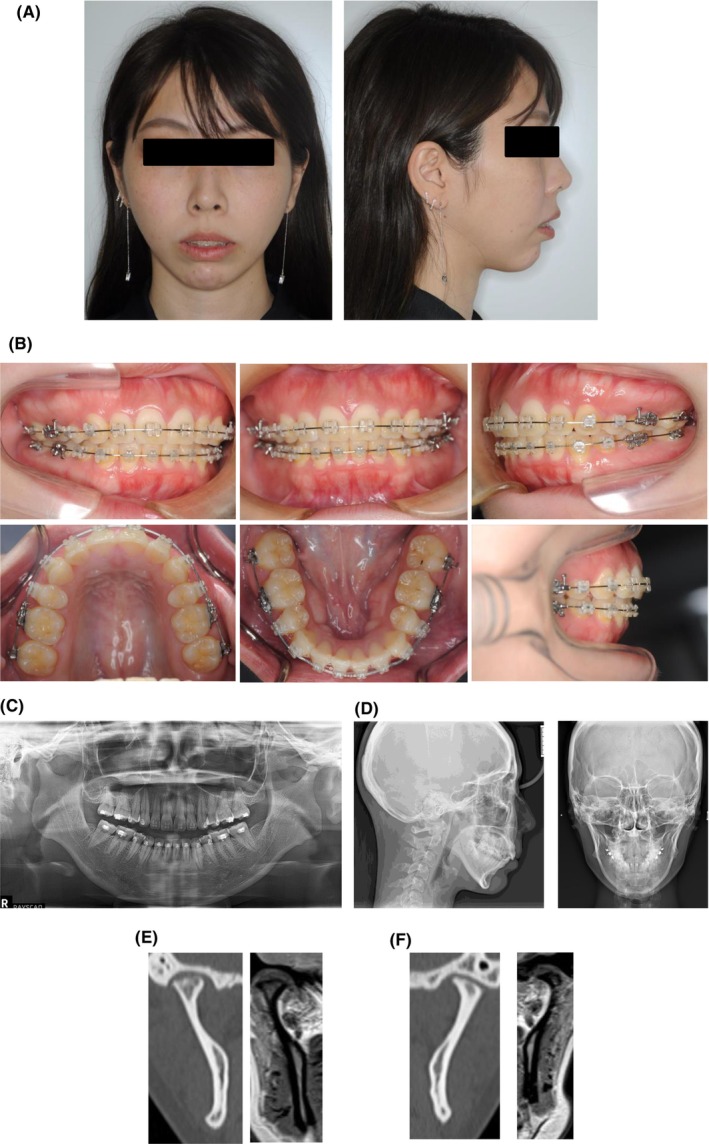
Preoperative findings. (A) Facial photographs. (B) Intraoral photographs. (C) Panoramic radiographs. (D) Cephalometric radiographs. Coronal view of the right condyle (E) and left condyle (F) in CT (the left panel) and MRI (the right panel).
FIGURE 3.
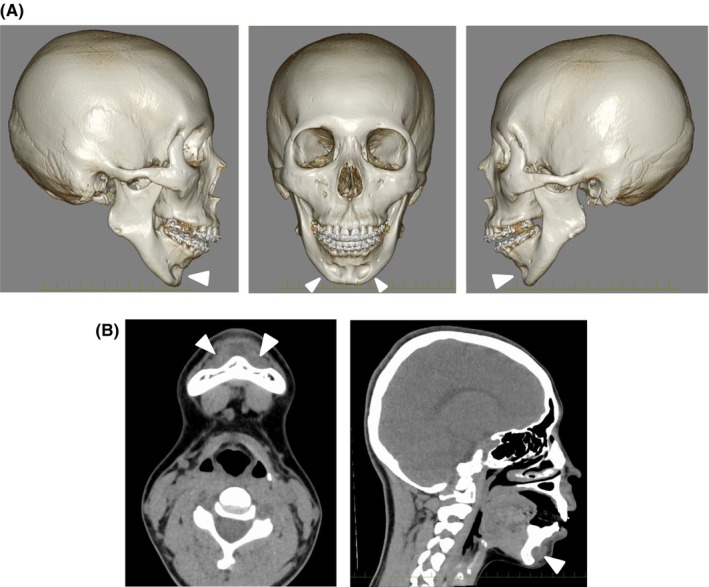
Foreign body appearance in CT. (A) Three‐dimensional CT view of the bone defect (allow head) in the mentum. (B) Soft tissue mode of CT. Arrow heads indicate foreign bodies.
FIGURE 4.
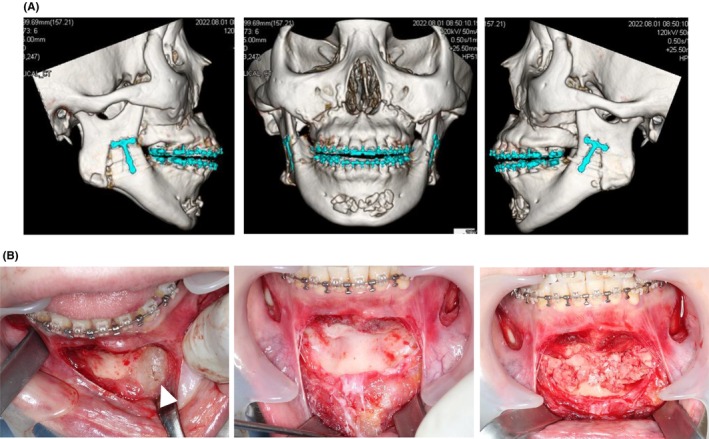
Operative findings. (A) Postoperative view of 3D‐CT. (B) Intraoperative photographs. (Left panel) arrow heads indicate foreign bodies. (Midpanel) bone defects after foreign body removal. (Right panel) bone graft to the defects.
2.3. Examination of the foreign bodies
The two foreign bodies measured about 30 × 7 mm and 15 × 7 mm, respectively, and were elastic and soft (Figure 5A). Histopathological examination revealed a hematoxylin‐positive foreign body on HE staining (Figure 5B, C), and mild inflammatory cell infiltration and multinucleated giant cells were found in the peripheral fibrous connective tissue and muscle tissue of the foreign bodies (Figure 5D,E). To identify the foreign bodies, XPS was performed (Figure 6). A wide‐scan XPS spectrum (Figure 6A) had two strong peaks assigned to C1s (open arrow head) and O1s (closed arrow head) orbitals. No photoelectron emissions were detected for S2p and N1s. This observation was confirmed by narrow‐scan analysis (Figure 6B–E). Shoulder peaks are seen in spectra for C1s (Figure 6B) and O1s (Figure 6C), indicating the presence of C–OH and C–O–C moieties. These results suggest that the major elements contained in the foreign bodies are carbon, oxygen, and hydrogen. According to this result as well as the clinical background, it is likely that the foreign bodies are made of HA. Although glycosaminoglycan HA should contain nitrogen, we could not detect this element by the XPS analysis (Figure 6D, E), probably because nitrogen is a trace component of HA and thus photoelectron emissions from the N1s orbital was not noticeable.
FIGURE 5.
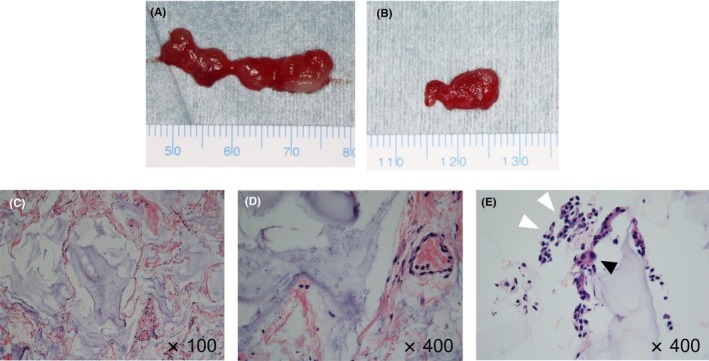
Histopathological study. (A) Photograph of the foreign bodies on the right side defect (A) and the left side defect (B). (C–E) Histopathological photographs. (C) ×100, (D, E) ×400. The white arrowheads in (E) indicate inflammatory cell infiltration, and the black arrowheads indicate multinucleated giant cells.
FIGURE 6.
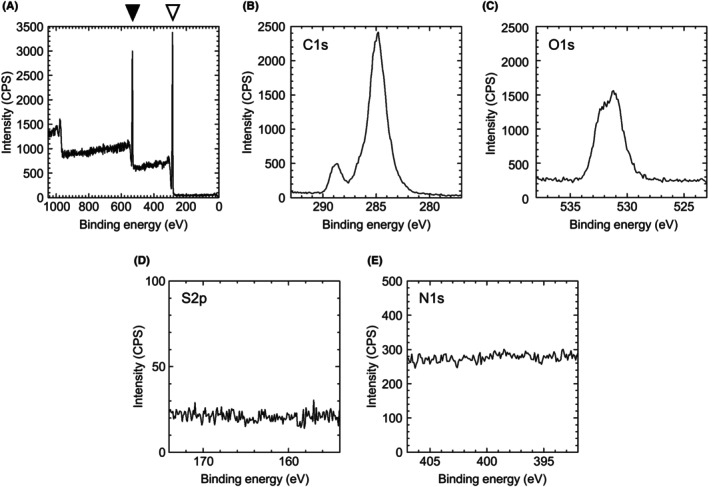
XPS analysis of the foreign body. (A) Wide‐scan spectrum of the foreign body. Peaks assigned to C1s (black arrowhead) and O1s orbitals (white arrowhead) were observed. (B–E) Narrow‐scan spectra for (B) C1s, (C) O1s, (D) S2p, and (E) N1s orbitals. Note that shoulder peaks seen in spectra (B) and (C) suggest the presence of C–OH and C–O–C moieties. No clear peaks were observed for S2p in spectrum d and N1s orbitals in spectrum (E). In spectra (A–E), binding energy was calibrated with C1s (248.8 eV).
2.4. Outcome and follow‐up
One year after the BOGS, the condylar resorption was not advance. In addition, radiographs revealed that the concavities at the mentum were obscured (Figure 7). To improve the patient's facial proportion, genioplasty was performed in August 2023. Consequently, bone defects disappeared by bone grafting, and the ideal position and shape of the mentum could be obtained (Figure 8A). At present, 1.5 years after the BOGS, relapse and condylar resorption did not occur, and the patient achieved good facial proportion and occlusal function (Figure 8B, C).
FIGURE 7.
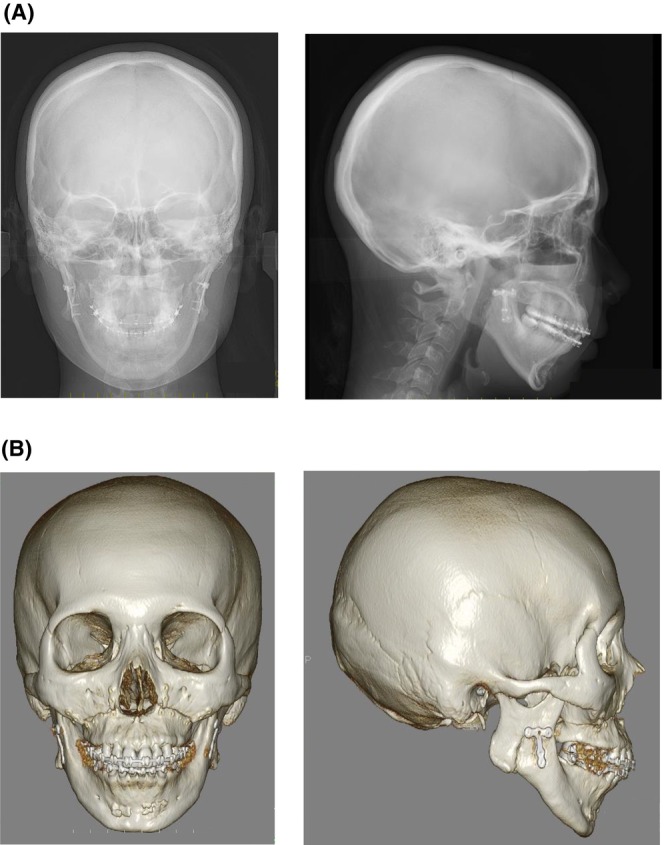
Radiographic findings 1 year after the BOGS. Cephalometric radiographs (A) and CT (B) at 1 year after the BOGS.
FIGURE 8.

Operative findings at genioplasty, final occlusion, and facial appearance. (A) Photograph of the mentum at genioplasty. (B) Facial photographs 1.5 years after the BOGS. (C) Intraoral photographs 1.5 years after the BOGS.
3. DISCUSSION
In the present case, BOGS and bone grafting were performed to improve the jaw deformity and morphology of abnormal bone resorption in the mentum caused by HA filler injection. Furthermore, the foreign body was identified as HA via XPS analysis, and it was found that the unexpected bone resorption was caused by HA filler injection.
A clinically ideal filler needs to be safe and effective. It must also have the properties of long‐term chemical stability, safe absorption in vivo, biocompatibility, nontoxicity, nonantigenicity, noninflammatory, low cost, and easy storage. 14 As filler injection therapy is usually performed on an outpatient basis, it should ideally be easy to perform, maintain the bulging state for a long time without any foreign body reaction at the injection site, and be easily removed or resorbed back to the pretreated state if necessary. 15 However, the absence of tissue reaction indicates the absence of degradation or resorption. Therefore, at present, no filler that meets all the requirements exists. Among the fillers used in soft tissue augmentation is HA, which is derived from living organisms and has no organ or species specificity. Therefore, HA induces no allergic reaction and has high biocompatibility. 16 HA filler injection is the most popular nonsurgical procedure for chin augmentation.
Bone resorption in the mentum is a known complication of chin augmentation. 12 , 13 It is often caused by the materials of chin implants, such as silicone, polyethylene, and polyamide. Yeung et al. 17 conducted a systematic review of bone resorption using different implants and fillers after chin augmentation. They reported that the prevalence of bone resorption caused by HA filler injection is considerably low compared with that caused by other chin implants. However, Guo et al. 13 conducted a retrospective study of bone resorption in the mentum with HA filler injection and analyzed the clinical factors causing this condition. They reported that bone resorption was associated with the volume of HA injected each time, frequency of injection, and interval between injections. In this case, HA filler injection was performed three times every 6 months to 1 year; however, the volume of HA filler injected each time was unknown.
Robinson et al. reported bone resorption with chin implants 18 and advocated the classification of bone resorption patterns in 1972. 19 Robinson's classification assessed the amount of bone resorption by comparing the installed implant volume with the depth of bone resorption. In the present case, although the exact volume of the HA filler was unknown, the bone defect volume was approximately half that of the filler, and the maximum depth of the defects was more than 5 mm. Based on the results, the present case was classified as grade III, which is the most severe category. The patient in this case visited the orthodontic clinic because of complaints of lack of esthetic improvement, which led to the incidental detection of bone resorption of the mentum. However, in the absence of infection, allergic reaction, or cosmetic disturbance, the chances of being aware of the bone resorption in the mentum may be low, and it is possible that there are potential patients with bone resorption of the mentum. Therefore, Polo emphasized the importance of regular follow‐up with cephalography to detect bone resorption at an early stage and reported a flow chart of the follow‐up algorithm after chin augmentation. 20
The mechanism of bone resorption with chin augmentation is generally recognized due to continuous compressive force exerted on the cortical bone of the mentum by the mentalis muscle. Matarasso et al. reported that progressive bone resorption following silastic chin augmentation was associated with labial incompetence. 21 , 22 They hypothesized that lip closure with labial competence induced a hypertonic state in the mentalis muscle. In general, many patients undergoing chin augmentation were diagnosed with skeletal Class II mandibular retrusion. Chin augmentation with implants or fillers is unable to improve the position of the mentalis muscle. Thus, after chin augmentation, mentalis muscle tension is induced by lip closure, the cortical bone of the mentalis is exposed to continuous compressive force, and bone resorption is induced. In the present case, the skeletal diagnosis was also Class II, and difficulty in lip closure was observed at the initial visit. Based on these results, accurate skeletal diagnosis before chin augmentation is critical to prevent unexpected bone resorption.
Sagittal split ramus osteotomy (SSRO) is the most performed procedure of orthognathic surgery in the mandible. 23 However, the counterclockwise rotation of the distal segment with an increase in the height of the mandibular branch is problematic in terms of postoperative stability and adverse effects on the temporomandibular joint. Reduction of blood supply to the proximal segment may induce progressive condylar resorption. On the other hand, ILRO may reduce the risk of condylar head resorption because the position of the gonion does not change before and after surgery and blood supply from the temporalis muscle to the proximal segment can be maintained. 24 In this case, because of the deformity due to significant condylar head resorption, ILRO was chosen instead of SSRO to maximize blood supply to the proximal segments and postoperative stability.
Patients who have received HA injections are considered to have a high demand for cosmetic improvement because of their desire for improvement of their facial proportions. For this reason, it is important to inform them that in order to improve the proportion of the mentum, they must first undergo bone grafting in the area of resorption of the mentum. After the osteogenesis is confirmed, genioplasty will be necessary. It is important to explain that since the mentum has been damaged by HA injections, there is a scar tissue and poor blood supply. Clinicians should consider the prevention of infection and autogenous bone grafting is the most desirable procedure.
XPS is a method of elemental analysis of an object's surface through measurement of the kinetic energy of photoelectrons emitted when a sample is irradiated with X‐rays. 25 In XPS analysis, the sample is irradiated with soft X‐rays, and the binding energy is determined by measuring the velocity of the photoelectrons (electrons excited by light) emitted when the material is ionized. Using the spectrum obtained from the binding energy analysis, it is possible to determine the elements contained in the sample. The shape of the spectrum also gives an approximate idea of the existing chemical bonds. Figure 6A presents two sharp peaks in the wide scan results. The right peak (open arrow head) is based on carbon and the left peak (closed arrow head) is based on oxygen. Figure 6B, C presents the results of the carbon and oxygen narrow scans, respectively. A shoulder is observed on the carbon and oxygen peaks, suggesting that they contain C–OH and C–O–C. These results suggest that the sample is probably HA; although, nitrogen was not detected most likely because it is relatively a trace element in HA. The presence of proteins is excluded because we did not detect sulfur and thus the sample seemed not to be of biological origin. As a whole, it is assumed that the foreign bodies are made of a relatively pure, externally injected polysaccharide, most likely identified as HA based on its clinical course. It was therefore concluded that the bone resorption in the mentum was caused by the HA filler injection.
A limitation of this study is that it is a single case report and cannot consider how the amount and frequency of HA injections affected bone resorption in the mentum as in clinical studies such as Guo et al. 13 On the other hand, in this study, XPS showed that the foreign bodies were HA. This suggests that long‐term exposure to artificial synthetic HA in the mentum directly causes abnormal bone resorption.
AUTHOR CONTRIBUTIONS
Takayuki Nakagawa: Conceptualization; writing – original draft. Shigehiro Ono: Conceptualization; supervision; writing – original draft. Miyuki Sakuma: Resources; visualization. Yoko Ishida: Resources; visualization. Kuniko Mizuta: Conceptualization; supervision; writing – original draft. Ryo Uetsuki: Resources; visualization. Keijyuro Odan: Resources; visualization. Yuko Shintaku: Writing – review and editing. Masataka Higuchi: Writing – review and editing. Yutaka Matsushita: Writing – review and editing. Shunichi Kojima: Writing – review and editing. Isao Hirata: Writing – review and editing. Koichi Kato: Conceptualization; writing – review and editing. Tomonao Aikawa: Conceptualization; supervision; writing – review and editing.
FUNDING INFORMATION
No financial support was received for this study.
CONFLICT OF INTEREST STATEMENT
The authors of this article claim that they do not have any conflict of interest.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
The authors would like to thank Enago (www.enago.jp) for the English language review. The authors would also like to thank Yoshiaki Ninomiya, Yasuki Ishioka, Takako Naruse, Nao Yamakado, Misaki Akagi, Chieko Niwata, Daitoku Murakami, Ayumi Fujii, Yoshiteru Yamashita, and Jun Ashida (Hiroshima University Graduate School) for their critical support of this study.
Nakagawa T, Ono S, Sakuma M, et al. A case of bone resorption in the mentum caused by hyaluronic acid filler in a patient with skeletal Class II jaw deformity. Clin Case Rep. 2024;12:e9150. doi: 10.1002/ccr3.9150
DATA AVAILABILITY STATEMENT
All data are available upon request from the corresponding author.
REFERENCES
- 1. Matarasso SL, Carruthers JD, Jewell ML, Restylane CG. Consensus recommendations for soft‐tissue augmentation with nonanimal stabilized hyaluronic acid (Restylane). Plast Reconstr Surg. 2006;117:3S‐34S. [DOI] [PubMed] [Google Scholar]
- 2. Rohrich RJ, Ghavami A, Crosby MA. The role of hyaluronic acid fillers (Restylane) in facial cosmetic surgery: review and technical considerations. Plast Reconstr Surg. 2007;120:41S‐54S. [DOI] [PubMed] [Google Scholar]
- 3. Ou Y, Wu M, Liu D, et al. Nonsurgical chin augmentation using hyaluronic acid: a systematic review of technique, satisfaction, and complications. Aesth Plast Surg. 2023;47(4):1560‐1567. [DOI] [PubMed] [Google Scholar]
- 4. Holt S, Fronek L, Witfill K. Nonsurgical augmentation of the chin using a lateral to medial approach with hyaluronic acid based filler: a case series. J Clin Aesthet Dermatol. 2023;16(10):40‐42. [PMC free article] [PubMed] [Google Scholar]
- 5. DeLorenzi C, Weinberg M, Solish N, Swift A. The long‐term efficacy and safety of a subcutaneously injected large‐particle stabilized hyaluronic acid‐based gel of nonanimal origin in esthetic facial contouring. Dermatologic Surg. 2009;35:313‐321. [DOI] [PubMed] [Google Scholar]
- 6. Fakhari A, Berkland C. Applications and emerging trends of hyaluronic acid in tissue engineering, as a dermal filler and in osteoarthritis treatment. Acta Biomater. 2013;9(7):7081‐7092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goa KL, Benfield P. Hyaluronic acid. A review of its pharmacology and use as a surgical aid in ophthalmology, and its therapeutic potential in joint disease and wound healing. Drugs. 1994;47(3):536‐566. [DOI] [PubMed] [Google Scholar]
- 8. Bergeret‐Galley C. Comparison of resorbable soft tissue fillers. Aesthet Surg J. 2004;24(1):33‐46. [DOI] [PubMed] [Google Scholar]
- 9. Matti BA, Nicolle FV. Clinical use of Zyplast in correction of age‐ and disease‐related contour deficiencies of the face. Aesth Plast Surg. 1990;14(3):227‐234. [DOI] [PubMed] [Google Scholar]
- 10. Burdick JA, Prestwich GD. Hyaluronic acid hydrogels for biomedical applications. Adv Mater. 2011;23(12):H41‐H56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zheng Shu X, Liu Y, Palumbo FS, Luo Y, Prestwich GD. In situ crosslinkable hyaluronan hydrogels for tissue engineering. Biomaterials. 2004;25(7–8):1339‐1348. [DOI] [PubMed] [Google Scholar]
- 12. Guo X, Song G, Zong X, Jin X. Bone resorption in mentum induced by unexpected soft‐tissue filler. Aesthet Surg J. 2018;38(10):NP147‐NP149. [DOI] [PubMed] [Google Scholar]
- 13. Guo X, Zhao J, Song G, et al. Unexpected bone resorption in mentum induced by the soft‐tissue filler hyaluronic acid: a preliminary retrospective cohort study of Asian patients. Plast Reconstr Surg. 2020;146(2):147e‐155e. [DOI] [PubMed] [Google Scholar]
- 14. Alster TS, West TB. Human‐derived and new synthetic injectable materials for soft‐tissue augmentation: current status and role in cosmetic surgery. Plast Reconstr Surg. 2000;105(7):2515‐2525. [DOI] [PubMed] [Google Scholar]
- 15. Maas CS, Papel ID, Greene D, Stoker DA. Complications of injectable synthetic polymers in facial augmentation. Dermatologic Surg. 1997;23(10):871‐877. [PubMed] [Google Scholar]
- 16. Requena L, Requena C, Christensen L, Zimmermann US, Kutzner H, Cerroni L. Adverse reactions to injectable soft tissue fillers. J Am Acad Dermatol. 2011;64(1):1‐34. [DOI] [PubMed] [Google Scholar]
- 17. Yeung AWK, Wong NSM. Mandibular bone resorption following chin augmentation: a systematic review. Front Surg. 2022;9:815106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Robinson M, Shuken R. Bone resorption under plastic chin implants. J Oral Surg. 1969;27(2):116‐118. [PubMed] [Google Scholar]
- 19. Robinson M. Bone resorption under plastic chin implants. Follow‐up of a preliminary report. Arch Otolaryngol. 1972;95(1):30‐32. [DOI] [PubMed] [Google Scholar]
- 20. Polo M. Bone resorption under chin implants: the orthodontist's role in its diagnosis and management. Am J Orthod Dentofacial Orthop. 2017;151(1):201‐208. [DOI] [PubMed] [Google Scholar]
- 21. Matarasso A, Elias AC, Elias RL. Labial incompetence: a marker for progressive bone resorption in silastic chin augmentation. Plast Reconstr Surg. 1996;98(6):1007‐1014. [DOI] [PubMed] [Google Scholar]
- 22. Matarasso A, Elias AC, Elias RL. Labial incompetence: a marker for progressive bone resorption in silastic chin augmentation: an update. Plast Reconstr Surg. 2003;112(2):676‐678. [DOI] [PubMed] [Google Scholar]
- 23. Wolford LM, Bennett MA, Rafferty CG. Modification of the mandibular ramus sagittal split osteotomy. Oral Surg Oral Med Oral Pathol. 1987;64(2):146‐155. [DOI] [PubMed] [Google Scholar]
- 24. Aymach Z, Nei H, Kawamura H, van Sickels J. Evaluation of skeletal stability after surgical‐orthodontic correction of skeletal open bite with mandibular counterclockwise rotation using modified inverted L osteotomy. J Oral Maxillofac Surg. 2011;69(3):853‐860. [DOI] [PubMed] [Google Scholar]
- 25. Briggs D, Seah MP. Practical Surface Analysis. 2nd ed. Wiley; 1990. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available upon request from the corresponding author.


