Abstract
Background
Previous studies have reported race-based health disparities in North America. It is unknown if emergency medical service (EMS) treatment of out-of-hospital cardiac arrest (OHCA) varies based on race. We sought to compare markers of resuscitation intensity among different racial groups.
Methods
Using data of adult EMS-treated OHCAs from the Trial of Continuous or Interrupted Chest Compressions During CPR, we analyzed data from participants for whom on-scene return of spontaneous circulation (ROSC) was not achieved. We fit multivariate regression models using a generalized estimating equation, to estimate the association between patient race (White vs. Black vs. “Other”) and the following markers for resuscitation intensity: (1) resuscitation attempt duration; (2) intra-arrest transport; (3) number of epinephrine doses; (4) EMS arrival-to-CPR interval, and (5) 9–1–1 to first shock.
Results
From our study cohort of 5370 cases, the median age was 65 years old (IQR: 53–78), 2077 (39 %) were women, 2121 (39 %) were Black, 596 (11 %) were “Other race”, 2653 (49 %) were White, and 4715 (88 %) occurred in a private location. With reference to White race, Black race was associated with a longer resuscitation attempt duration and a lower number of epinephrine doses; Black and “Other” race were both associated with a lower odds of intra-arrest transport.
Conclusion
We identified race-based differences in EMS resuscitation intensity for OHCA within a North American cohort, although 40% of race data was missing from this dataset. Future research investigating race-based differences in OHCA management may be warranted.
Introduction
With an annual incidence of approximately 350,000 and survival to hospital discharge of 10 %1 in the United States, out-of-hospital cardiac arrest (OHCA) is a major public health issue that requires rapid interventions.2 Previous research has identified factors associated with OHCA outcomes, including bystander cardiopulmonary resuscitation (CPR), emergency medical service (EMS) response time, age, and sex.3, 4 However, it is known that other factors such as race and socioeconomic status are associated with varying incidence, bystander interventions, and survival.5, 6 To illustrate, multiple studies have demonstrated that minoritized groups such as Blacks and Hispanics are less likely to receive bystander CPR.5, 7, 8.
One recent study investigated the difference in CPR quality among racial groups.9 They found that with reference to White, Black patients had higher odds of compression rate compliance and lower odds of intended CPR strategy compliance. To add on to this work, resuscitation intensity by professional rescuers with respect to the race of the patient has not been evaluated. We sought to estimate whether the racial group of the OHCA patient is associated with markers of intense EMS management. For cases that were unable to be resuscitated with on-scene efforts, we compared the length of time EMS committed to attempting resuscitation, after adjusting for geographical region of treatment. We also compared the proportion treated with intra-arrest transport, the number of epinephrine doses provided, the EMS arrival-to-CPR interval, and the 9–1–1 to first shock interval for those with an initial shockable rhythm.
Methods
Study setting & Design
This was a secondary analysis of participants enrolled in the “Trial of Continuous or Interrupted Chest Compressions During CPR” trial (“The CCC Trial”; ClinicalTrials.gov NCT01372748), which has been previously reported.10 Briefly, Resuscitation Outcomes Consortium (ROC)-affiliated EMS agencies across North America between April 1, 2011 to June 30, 2015, enrolled individuals ≥ 18 years of age who were treated with EMS-provided chest compressions (EMS-witnessed arrests and those with do-not-resuscitate [DNR] orders were excluded). The CCC study created 49 similarly sized enrollment clusters by subdividing each ROC site by EMS agency, station, or other unit as appropriate to the site’s EMS structure. Trained ROC data staff abstracted participant characteristics (including race), bystander interventions, time-stamped EMS interventions (including the total number of milligrams [mg] epinephrine administered), in-hospital interventions, and outcomes from clinical records. The three Canadian ROC sites, which accounted for approximately 54 % of cases entered into the ROC Cardiac Arrest Registry11, did not collect data on race.12 We acquired the publicly-available CCC trial dataset from the National Heart, Lung, and Blood Institute Biologic Specimen and Data Repository Information Center (BioLINCC), with approval from the Research Ethics Committee of the University of Fukui (#20180006). BioLINCC provided approval for this analysis (#14582).
Participant selection
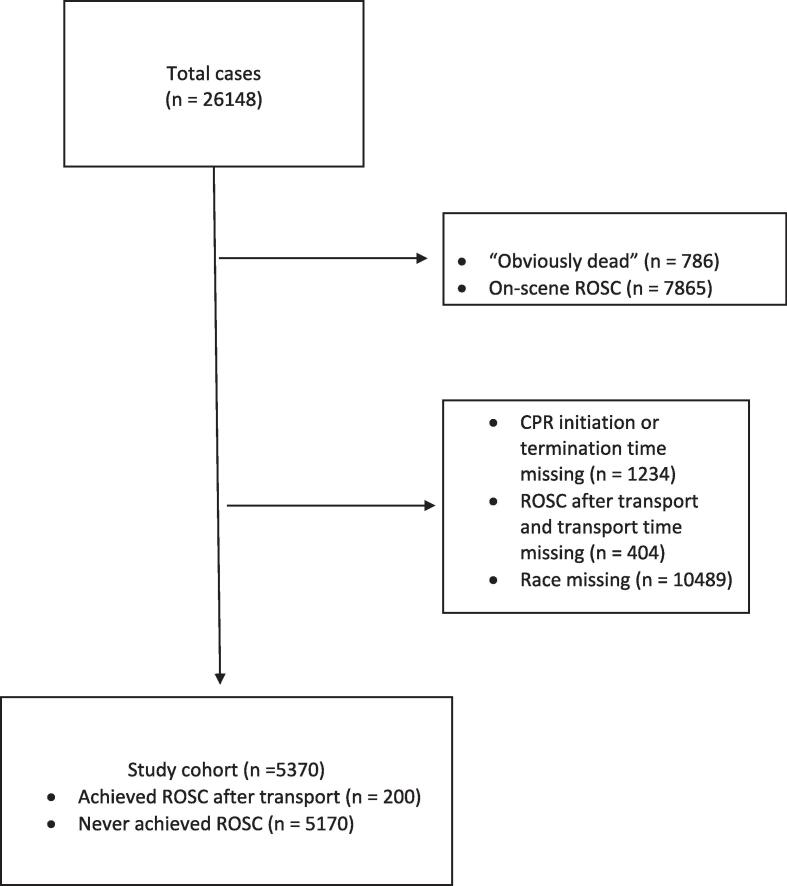
From the CCC trial cases, we excluded those with: (1) on-scene ROSC; (2) “obvious death” (including rigor mortis and dependent lividity) as the reason for resuscitation being aborted; (3) missing data on race and event times required for analysis (including the times of EMS initial CPR, transport, ROSC, and resuscitation cessation).
Outcome measures and variable Definitions
We operationalized several outcomes to serve as surrogate markers for EMS resuscitation intensity. First, we examined the primary outcome of EMS treatment duration for unsuccessful resuscitations, defined as the time interval between the initiation of EMS-performed chest compression and the end of EMS resuscitation, whether due to declaration of death in the prehospital setting or hospital arrival. This represents the duration of time that EMS providers committed to attempting resuscitation. Paramedics’ decision to engage in a prolonged treatment duration reflects a more fervent resuscitation effort. Second, we investigated the outcome of intra-arrest transport, defined as transport to hospital in the absence of any previous episodes of ROSC. This reflects a more intense approach by providers which include the logistical challenges of extrication and transport with ongoing CPR to the nearest hospital. Third, we investigated the outcome of the number of epinephrine doses, also serving as a proxy for a persistent treatment intervention. Epinephrine doses were assumed to have been provided at 1 mg per dose. Fourth, we investigated the time from EMS scene arrival to start of CPR, demonstrating a level of expedience of EMS, traveling from their vehicle to the patient. Fifth, we looked at the 9–1–1 to first shock interval in individuals who had an initial shockable rhythm. This shows the urgency of which EMS arrives on scene, assesses and defibrillates the patient.
The primary exposure variable of interest was race/ethnicity, which was categorized in the CCC Dataset as Black, Hispanic, White, Asian, or Other (defined as “other race” or “multi-racial”). However, given that Hispanic, Asian, and “Other” categories accounted for 11 % of the cases with non-missing data, we classified race/ethnicity into three groups for a more balanced comparison: White, Black, and Other race (including Asian, Hispanic and Other).
Data analysis
We used R (Foundation for Statistical Computing, Vienna, version 4.2.2)13, Microsoft Excel 16.78 (Microsoft Corp, Redmond), and Prism GraphPad Version 10.0.3 for data management and statistical analysis. We described patient and treatment characteristics within racial groups. Categorical variables were described as counts and proportions, whereas continuous variables were detailed with median and interquartile range (IQR).
We performed several analyses with the exposure variable as race and the outcome variables as surrogate measures for EMS treatment intensity. First, we investigated the association of race and the primary outcome of EMS treatment duration. We excluded cases from this model who achieved ROSC at any time, to compare treatment duration attempts among cases with unsuccessful resuscitations. We fit both adjusted and unadjusted multivariable linear regression models to estimate the association between race and treatment duration. Given that EMS practices, including the duration of attempted resuscitation, may be associated with geographical region of treatment we included a generalized estimating equation (GEE) in the model, to adjust for clustering effect. We included adjustment covariates for standard Utstein variables,14 including age, sex, EMS response time (measured from the 9–1–1 call until first EMS vehicle on-scene arrival), initial rhythm, location, bystander CPR, and bystander witnessed status. “White” was used as the reference value. Results were described as estimates and 95 % confidence intervals (CI). In addition, given that the distance from the scene to the hospital may vary (and may not reflect the degree of intensive care provided), we repeated the analysis after excluding cases that were transported to hospital (i.e., restricted to those who were declared dead at the scene).
For our secondary analysis examining the outcome of intra-arrest transport, we included all study cases. We fit both adjusted and unadjusted multivariable logistic regression models, to estimate the association between race and intra-arrest transport. We used the same adjustment strategy as in the primary analysis, and presented estimates as odds ratios with corresponding CI. For our third analysis examining the number of epinephrine doses, we repeated the primary analysis methodology (also excluding cases that had achieved ROSC at any time), however also adjusted for EMS arrival-to-epinephrine interval. Next, we performed our fourth analysis investigating the interval of EMS arrival-to-CPR with the same analytical approach to the primary analysis. This analysis included all cases within our study cohort. Our fifth analysis on the 9–1–1 to first shock interval was performed using the same analytical approach as the primary analysis on patients who had an initial shockable rhythm.
Results
We included 5370 OHCA cases in our analysis (Fig. 1). The median age was 65 years (IQR: 53–78), 2077 (39 %) were female, and 892 (17 %) had initial shockable rhythms (Table 1 and Supplemental Table S1). White patients were the oldest with a median age of 67 years and tended to have more frequent bystander CPR. Black patients tended to have a higher proportion of female cases. Median time intervals for prehospital interventions were similar across racial groups. Surrogate measures for EMS treatment intensity are shown on Table 2. The median treatment duration and epinephrine doses provided was similar across groups, and over half of patients received intra-arrest transport.
Fig. 1.
Study Flow ROSC, return of spontaneous circulation; CPR, cardiopulmonary resuscitation.
Table 1.
Cohort characteristics.
|
Black (n = 2121) |
White (n = 2653) |
Other (n = 596) |
|
|---|---|---|---|
| Time Intervals (minutes), median (IQR) | |||
| 9–1–1 to 1st EMS arrival | 4.3 (3.2, 5.6) | 4.9 (3.7, 6.2) | 4.6 (3.6, 5.7) |
| 9–1–1 to first EMS CPR | 6.7 (5.1, 8.4) | 7.2 (5.7, 9.2) | 6.7 (5.2, 8.2) |
| 9–1–1 to ALS arrival | 5.1 (3.9, 7.1) | 5.8 (4.2, 8.0) | 5.3 (4.0, 7.2) |
| 9–1–1 to first epinephrine | 16 (13, 20) | 15 (12, 19) | 15 (12, 19) |
| 9–1–1 to first successful advanced airway | 18 (14, 22) | 17 (14, 21) | 17 (13, 22) |
| EMS arrival to transport | 20 (16, 26) | 21 (16, 26) | 20 (16, 25) |
| Patient characteristics | |||
| Location type, n (%) | |||
| Public | 225 (11) | 354 (13) | 66 (11) |
| Non-public | 1891 (89) | 2296 (87) | 527 (88) |
| Age (years), median (IQR) | 62 (53, 74) | 67 (54, 81) | 63 (47, 75) |
| Female, n (%) | 940 (44) | 916 (35) | 220 (37) |
| Bystander witnessed, n (%) | 701 (35) | 937 (37) | 197 (33) |
| Bystander CPR, n (%) | 680 (32) | 1292 (49) | 247 (41) |
| Initial rhythm, n (%) | |||
| Shockable | 337 (16) | 465 (18) | 90 (15) |
| Non-shockable | 1775 (84) | 2176 (82) | 505 (85) |
| Declared dead at the scene, n (%) | 797 (38) | 1318 (50) | 246 (41) |
| ROSC after transport, n (%) | 91 (4.3) | 84 (3.2) | 25 (4.2) |
ALS, advanced life support paramedic; advanced airway, supraglottic airway or endotracheal tube; ROSC, return of spontaneous circulation during transport; EMS, emergency medical services; CPR, cardiopulmonary resuscitation; Shockable rhythm, ventricular fibrillation or ventricular tachycardia; Non-shockable rhythm, pulseless electrical activity or asystole; IQR, interquartile range; Other, EMS-assessed race that was not Black or White (e.g Hispanic, Asian, biracial, etc).
Table 2.
Surrogate Measures for Aggressive EMS Treatment.
|
Black (n = 2121) |
White (n = 2653) |
Other (n = 596) |
|
|---|---|---|---|
| Outcomes | |||
| Treatment duration (minutes), median (IQR) | |||
| Full study cohort1 | 25 (20, 31) | 24 (19, 30) | 25 (20, 31) |
| Among those declared dead at the scene2 | 24 (20, 29) | 24 (18, 29) | 24 (19, 30) |
| Intra-arrest transport, n (%) | 1324 (62) | 1335 (50) | 350 (59) |
| Epinephrine doses (number), median (IQR) | 3 (2, 4) | 3 (3, 5) | 3 (2, 4) |
| EMS arrival-to-CPR (minutes), median (IQR) | 2.0 (1.1, 3.4) | 2.2 (1.3, 3.5) | 1.8 (1.1, 2.9) |
| 9–1–1 to first shock (minutes), median (IQR) | 14 (9.1, 22) | 12 (9.0, 21) | 13 (9.6, 21) |
EMS, emergency medical services; CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation during transport; IQR, interquartile range; Other, EMS-assessed race that was not Black or White (e.g Hispanic, Asian, biracial, etc); Intra-arrest transport, patients who were transported to hospital without on-scene ROSC.
Treatment duration calculated as the interval between EMS initiation of resuscitation and termination of resuscitation due to: termination of resuscitation due at the scene, ROSC during transport, or arrival at hospital.
Treatment duration calculated as the interval between EMS initiation of resuscitation and termination of resuscitation due at the scene.
The association of race with outcomes using the adjusted regression analyses with GEE is shown in Table 3. With reference to White race, Black race was associated with a longer duration of treatment attempt in patients without prehospital ROSC (β = 0.662; 95 % CI 0.122, 1.20).
Table 3.
Multivariate regression models with adjusted3 generalized estimating equation (GEE) for the effect of race on EMS treatment bias.
| Exposure | Primary Outcome | Secondary Outcomes | ||||
|---|---|---|---|---|---|---|
| Race | Treatment duration1(mins) | Treatment duration2(mins) | Intra-arrest transport | Epinephrine doses (mg) | EMS arrival-to-CPR (mins) | 911 to first shock (mins) |
| Adjusted3 estimate (95 % CI) |
Adjusted3 estimate (95 % CI) |
Adjusted3 odds ratio (95 % CI) |
Adjusted3 estimate (95 % CI) |
Adjusted3 estimate (95 % CI) |
Adjusted4 estimate (95 % CI) |
|
| White | Reference | Reference | Reference | Reference | Reference | Reference |
| Black | 0.662 (0.122, 1.20) | 0.347 (−0.371, 1.07) | 0.948 (0.932, 0.965) | −0.413 (−0.554, −0.273) | −0.0318 (−0.231, 0.168) | 0.915 (−0.301, 2.130) |
| Other | 0.244 (−0.686, 1.17) | 0.446 (−0.877, 1.77) | 0.969 (0.948, 0.991) | −0.0709 (−0.311, 0.169) | −0.252 (−0.555, 0.0515) | −0.289 (−1.449, 0.872) |
Mins, Minutes; mg, milligrams; EMS, emergency medical services; CPR, cardiopulmonary resuscitation; CI, confidence interval; EMS, emergency medical services; generalized estimating equation, accounts for the cluster effect of 49 regions; Other, EMS-assessed race that was not Black or White (e.g Hispanic, Asian, biracial, etc); ROSC, return of spontaneous circulation.
Treatment duration calculated as the interval between EMS initiation of resuscitation and termination of resuscitation due to: termination of resuscitation due at the scene, or arrival at hospital.
Treatment duration calculated as the interval between EMS initiation of resuscitation and termination of resuscitation due at the scene.
Adjusted for covariates of age, sex, EMS response time, initial rhythm, location, bystander CPR, bystander witnessed, 911 to first epinephrine dose (only for the epinephrine dose analysis).
Adjusted for covariates of age, sex, EMS response time, location, bystander CPR and bystander witnessed (only for cases with an initial shockable rhythm).
With reference to White race, Black (OR 0.948; 95 % CI 0.932, 0.965), and Other race (OR 0.969; 95 % CI 0.948, 0.991) were associated with lower odds of intra-arrest transport. Black race, with reference to White race, was associated with fewer doses of epinephrine (β = -0.413; 95 % CI −0.554, −0.273). We found no association between the EMS-arrival-to-CPR interval or 9–1–1 to first shock interval and racial groups.
Supplemental Tables 1-7 show the association of the outcome measures with each covariate in the adjusted and unadjusted models.
Discussion
From our cohort of over 5000 cases within the CCC trial dataset, we explored the association of race on surrogate markers for EMS treatment intensity. We found that, with reference to White cases, Black race was associated with longer treatment durations and fewer epinephrine doses. Black and Other race were associated with lower odds of intra-arrest transport. No association was observed with EMS arrival-to-CPR interval or 9–1–1 to first shock interval with reference to White. Our findings resemble Schmicker et al., study9 as their results do not demonstrate a systemic under-treatment of any one group or CPR quality metrics being a contributor to racial disparities. Rather, they observed several associations in CPR compression metrics between racial groups. Likewise for our markers of EMS resuscitation intensity, we observed several associations between race and differences in care among OHCA patients that may warrant additional future investigations.
In our study, Other and Black groups were younger and less commonly received bystander CPR, compared to White groups, consistent with previous literature. 5, 7, 8 The reasons for this may be multifactorial. Previous studies suggest less education and resources within communities of ethnic minorities pertaining to cardiac arrest recognition, bystander CPR and AED application.5, 7 Further, a systematic review and meta-analysis suggest that the younger age of minority groups in OHCA could be a demographic factor rather than these groups being more ill.8.
For patients in refractory arrest, our results indicate that Black race was associated with longer treatment duration attempts. To our knowledge, no previous studies have examined differences in the duration of resuscitation attempts for refractory OHCA between racial groups. However, Goldberger and colleagues categorized 435 US hospitals by how long they attempted resuscitation prior to termination among those in refractory arrest.15 Investigators reported that hospitals with the longest attempts at resuscitation had the highest rates of ROSC and survival to hospital discharge, supporting our use of this metric as a marker of resuscitation intensity. In our data, median treatment durations were approximately 25 min, after which there still remains a possibility of achieving ROSC and having favorable eventual outcomes (according to previous large database studies16).
Our investigation of secondary outcomes revealed that Black and Other race had lower odds of intra-arrest transport compared to White. There may be many contributing factors to intra-arrest transport rates. First, recent data indicates that on-scene resuscitation in comparison to intra-arrest transport is associated with a higher probability of survival to discharge,17 and thus the decision not to transport may be, on average, the best treatment decision. However, even among high-performing regions infrequently deploying intra-arrest transport, those chosen for this therapy demonstrate the most favorable characteristics,18 suggesting that there is a grading process by which providers select cases for this therapy, which supports our use of this metric for intensive care. A similar study in Utah looking at the association of race/ethnicity with odds of intra-arrest transport found no significant difference when adjusted for confounders.19 The variation in findings could be due to geographic location, data collection period and confounders such as comorbidities and socioeconomic status compared to our dataset. Intra-arrest transport decisions may also be influenced by community and scene-related factors such as the ability to extricate efficiently and the distance to the hospital. Although the odds ratio show a statistically lower chance of intra-arrest transport in Black and Other race versus White, it’s clinical significance may be minimal in the context of resuscitation intensity.
We evaluated epinephrine doses as a metric of intensive care. The administration of epinephrine is recommended every 3–5 min,20 and thus one would expect to be correlated with treatment duration. Despite similar first-epinephrine times between groups, we saw divergent patterns with regard to treatment durations and epinephrine groups, implying differing practices with regard to intervals between epinephrine doses. Given that longer gaps in epinephrine administration are associated with unfavorable neurological outcomes, these differences may contribute to outcome differences.21, 22.
Although not related to OHCA, there are previous data demonstrating differences in treatment based on race, including differential heart failure treatments of African American patients,23, 24, 25 pain management differences, 26 or the lack of ACE inhibitors prescription for Black individuals from the common conceptions that it is less effective than for White individuals.27 Implicit biases that may affect treatment decisions and outcomes or loss of trust in healthcare professionals.28 One systematic review, using implicit association tests, found that implicit bias exists in most healthcare professionals,29 which may affect clinical decision-making, patient-provider communication and health outcomes.29, 30, 31 As an OHCA requires timely interventions, implicit biases held by EMS providers in this high-stress environment could impact the decision-making of treatment interventions. Although our study cannot measure race-based biases in treatment decisions, this would be an important question for future studies to identify if bias exists in EMS OHCA management.
Limitations
This observational study has limitations. Although paramedic charts were recorded prospectively, our data may include errors. Determining the race of a patient with OHCA, who is rarely able to provide historical details, may have varying accuracy. It is known that OHCA characteristics and outcomes vary across ROC sites in North America32, which may have impacted our results. Further, the timeframe of our dataset (2011–2015) may affect the generalizability of our results to the current time and other regions due to differing patient demographics and EMS protocols. There was a substantial amount of missing data pertaining to race within the CCC dataset, which may have affected our results; however, the main reason was likely non-collection of race-based data at the Canadian ROC sites. Our study cohort only included cases for which resuscitation was attempted, and so the question remains of whether there may be inequities in deciding to forego resuscitation at the scene. Despite accounting for regional differences using the GEE model, we were not able to account for factors such as socioeconomic status, overall healthcare quality and access, or genetic variations among racial groups. Although our results show a statistically significant lower odds of intra-arrest transport in Black and Other race versus White, the results are still relatively close to 1, and thus the clinical significance of these findings may be debatable. Lastly, our analysis utilized clinical trial data, which is susceptible to the Hawthorne effect, where paramedic decision may be altered due to the increased level of observation.
Conclusion
Among EMS-treated OHCAs, we found some differences in surrogate markers for EMS resuscitation intensity: with reference to White race, Black race was associated with longer treatment durations; Black and Other races were associated with lower odds of intra-arrest transport; and, Black race was associated with fewer epinephrine doses. Further research into race-based OHCA treatment may be warranted to provide an increased understanding of potential differences and ensure equitable treatment provisions to those in need.
CRediT authorship contribution statement
Justin Yap: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Data curation, Conceptualization. Jacob Hutton: Writing – review & editing, Methodology, Formal analysis, Data curation, Conceptualization. Marina Del Rios: Writing – review & editing, Conceptualization. Frank Scheuermeyer: Writing – review & editing, Conceptualization. Malini Nair: Writing – review & editing. Laiba Khan: Writing – review & editing. Emad Awad: Writing – review & editing. Takahisa Kawano: Writing – review & editing, Conceptualization. Valerie Mok: Writing – review & editing. Jim Christenson: Writing – review & editing, Supervision, Conceptualization. Brian Grunau: Writing – review & editing, Supervision, Methodology, Conceptualization.
Funding
This project received no specific funding.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We are grateful for the dedication and service of the clinicians and research personnel who contributed to the Resuscitation Outcomes Consortium. The BC Resuscitation Research Collaborative would like to acknowledge funding from the Heart and Stroke Foundation of Canada and the Government of British Columbia, as well as in-kind support from Providence Health Care and BC Emergency Health Services. BG Acknowledges support from Michael Smith Health Research BC.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100806.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Garcia R.A., Girotra S., Jones P.G., McNally B., Spertus J.A., Chan P.S. Variation in Out-of-Hospital Cardiac Arrest Survival Across Emergency Medical Service Agencies. Circ Cardiovasc Qual Outcomes. 2022;15(6):E008755. doi: 10.1161/CIRCOUTCOMES.121.008755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rea T., Kudenchuk P.J., Sayre M.R., Doll A., Eisenberg M. Out of hospital cardiac arrest: Past, present, and future. Resuscitation. 2021;165:101–109. doi: 10.1016/J.RESUSCITATION.2021.06.010. [DOI] [PubMed] [Google Scholar]
- 3.Sasson C., Rogers M.A.M., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 4.Navab E., Esmaeili M., Poorkhorshidi N., Salimi R., Khazaei A., Moghimbeigi A. Predictors of Out of Hospital Cardiac Arrest Outcomes in Pre-Hospital Settings; a Retrospective Cross-sectional Study. Arch Acad Emerg Med. 2019;7(1):e36. [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta N.K., Allam S., Mazimba S., Karim S. Racial, ethnic, and socioeconomic disparities in out-of-hospital cardiac arrest within the United States: Now is the time for change. Hear Rhythm O2. 2022;3(6Part:B):857. doi: 10.1016/J.HROO.2022.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huebinger R., Del Rios M. Disentangling the Complex Web of Out-of-Hospital Cardiac Arrest Socioeconomic Disparities. JAMA Netw Open. 2023;6(5):e2312684–e. doi: 10.1001/JAMANETWORKOPEN.2023.12684. [DOI] [PubMed] [Google Scholar]
- 7.Garcia R.A., Spertus J.A., Girotra S., et al. Racial and Ethnic Differences in Bystander CPR for Witnessed Cardiac Arrest. N Engl J Med. 2022;387(17):1569–1578. doi: 10.1056/NEJMOA2200798/SUPPL_FILE/NEJMOA2200798_DISCLOSURES.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah K.S., Shah A.S., Bhopal R. Systematic review and meta-analysis of out-of-hospital cardiac arrest and race or ethnicity: black US populations fare worse. Eur J Prev Cardiol. 2014;21(5):619–638. doi: 10.1177/2047487312451815. [DOI] [PubMed] [Google Scholar]
- 9.Schmicker R.H., Blewer A., Lupton J.R., et al. The association of race with CPR quality following out-of-hospital cardiac arrest. Resuscitation. 2022;170:194–200. doi: 10.1016/J.RESUSCITATION.2021.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Study Details | Continuous Chest Compressions vs AHA Standard CPR of 30:2 | ClinicalTrials.gov. https://clinicaltrials.gov/study/NCT01372748. Accessed November 27, 2023.
- 11.Nichol G., Thomas E., Callaway C.W., et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/JAMA.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Personal Email Communication with Jim Christenson, Sheldon Cheskes, and Christian Vaillancourt. March 14, 2024.
- 13.R: The R Project for Statistical Computing. https://www.r-project.org/. Accessed October 30, 2023.
- 14.Perkins G.D., Jacobs I.G., Nadkarni V.M., et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest. Circulation. 2015;132(13):1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 15.Goldberger Z.D., Chan P.S., Berg R.A., et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet (london, England). 2012;380(9852):1473–1481. doi: 10.1016/S0140-6736(12)60862-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reynolds J.C., Grunau B.E., Rittenberger J.C., Sawyer K.N., Kurz M.C., Callaway C.W. The Association Between Duration of Resuscitation and Favorable Outcome After Out-of-Hospital Cardiac Arrest: Implications for Prolonging or Terminating Resuscitation. Circulation. 2016;134(25):2084. doi: 10.1161/CIRCULATIONAHA.116.023309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grunau B., Kime N., Leroux B., et al. Association of Intra-arrest Transport vs Continued On-Scene Resuscitation With Survival to Hospital Discharge Among Patients With Out-of-Hospital Cardiac Arrest. JAMA. 2020;324(11):1058–1067. doi: 10.1001/JAMA.2020.14185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grunau B., Kawano T., Rea T.D., et al. Emergency medical services employing intra-arrest transport less frequently for out-of-hospital cardiac arrest have higher survival and favorable neurological outcomes. Resuscitation. 2021;168:27–34. doi: 10.1016/J.RESUSCITATION.2021.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Awad E., Al Kurdi D., Austin Johnson M., Druck J., Hopkins C., Youngquist S.T. Examining the association between ethnicity and out-of-hospital cardiac arrest interventions in Salt Lake City. Utah. Resusc plus. 2024;19 doi: 10.1016/J.RESPLU.2024.100684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Circulation. 2000;102(suppl_1) doi: 10.1161/CIRC.102.SUPPL_1.I-129. [DOI] [Google Scholar]
- 21.Hansen M., Schmicker R.H., Newgard C.D., et al. Time to Epinephrine Administration and Survival From Nonshockable Out-of-Hospital Cardiac Arrest Among Children and Adults. Circulation. 2018;137(19):2032–2040. doi: 10.1161/CIRCULATIONAHA.117.033067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grunau B., Kawano T., Scheuermeyer F.X., et al. The Association of the Average Epinephrine Dosing Interval and Survival With Favorable Neurologic Status at Hospital Discharge in Out-of-Hospital Cardiac Arrest. Ann Emerg Med. 2019;74(6):797–806. doi: 10.1016/J.ANNEMERGMED.2019.04.031. [DOI] [PubMed] [Google Scholar]
- 23.Brody H., Hunt L.M. BiDil: Assessing a Race-Based Pharmaceutical. Ann Fam Med. 2006;4(6):556. doi: 10.1370/AFM.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ellison G.T.H., Kaufman J.S., Head R.F., Martin P.A., Kahn J.D. Flaws in the U.S. Food and Drug Administration’s Rationale for Supporting the Development and Approval of BiDil as a Treatment for Heart Failure Only in Black Patients. J Law Med Ethics. 2008;36(3):449 doi: 10.1111/J.1748-720X.2008.290.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maglo K.N., Rubinstein J., Huang B., Ittenbach R.F. BiDil in the Clinic: An Interdisciplinary Investigation of Physicians’ Prescription Patterns of a Race-Based Therapy. AJOB Empir Bioeth. 2014;5(4):37. doi: 10.1080/23294515.2014.907371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schoenthaler A., Williams N. Looking Beneath the Surface: Racial Bias in the Treatment and Management of Pain. JAMA Netw Open. 2022;5(6):e2216281–e. doi: 10.1001/JAMANETWORKOPEN.2022.16281. [DOI] [PubMed] [Google Scholar]
- 27.Cerdeña J.P., Plaisime M.V., Tsai J. From race-based to race-conscious medicine: how anti-racist uprisings call us to act. Lancet (london, England). 2020;396(10257):1125. doi: 10.1016/S0140-6736(20)32076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vela M.B., Erondu A.I., Smith N.A., Peek M.E., Woodruff J.N., Chin M.H. Eliminating Explicit and Implicit Biases in Health Care: Evidence and Research Needs. Annu Rev Public Health. 2022;43:477. doi: 10.1146/ANNUREV-PUBLHEALTH-052620-103528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall W.J., Chapman M.V., Lee K.M., et al. Implicit Racial/Ethnic Bias Among Health Care Professionals and Its Influence on Health Care Outcomes: A Systematic Review. Am J Public Health. 2015;105(12):e60. doi: 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dehon E., Weiss N., Jones J., Faulconer W., Hinton E., Sterling S. A Systematic Review of the Impact of Physician Implicit Racial Bias on Clinical Decision Making. Acad Emerg Med. 2017;24(8):895–904. doi: 10.1111/ACEM.13214/FULL. [DOI] [PubMed] [Google Scholar]
- 31.Marcelin J.R., Siraj D.S., Victor R., Kotadia S., Maldonado Y.A. The Impact of Unconscious Bias in Healthcare: How to Recognize and Mitigate It. J Infect Dis. 2019;220(Supplement_2):S62–S73 doi: 10.1093/INFDIS/JIZ214. [DOI] [PubMed] [Google Scholar]
- 32.Zive D.M., Schmicker R., Daya M., et al. Survival and variability over time from out of hospital cardiac arrest across large geographically diverse communities participating in the Resuscitation Outcomes Consortium. Resuscitation. 2018;131:74–82. doi: 10.1016/J.RESUSCITATION.2018.07.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.