Abstract
The level of dynamic mechanical instability between the bony parts of the ankle joint provides important information on biomechanical function. However, the dynamics of the distance between the talus and lateral malleolus during gait remain unclear. This study aimed to compare the distance between the talus and lateral malleolus and the ankle joint angles during the stance phase of gait between individuals with chronic ankle instability (CAI) and healthy adults. The comparison was conducted using a synchronized ultrasound (US) imaging with a three-dimensional motion analysis (MA) system. This cross-sectional study included 12 participants (5 males, 7 females; age, 20.5 ± 1.8 years; height, 166.6 ± 9.4 cm; body weight, 60.2 ± 5.3 kg; body mass index, 21.7 ± 2.0 kg/m2; 16 feet) with CAI and 10 healthy controls (4 males, 6 females; age, 21.2 ± 1.6 years; height, 164.6 ± 10.5 cm; body weight, 56.8 ± 11.3 kg; body mass index, 20.8 ± 2.6 kg/m2; 20 feet). The distance between the talus and lateral malleolus during gait was significantly increased in the CAI group compared with that in the control group throughout the stance phase. The ankle dorsiflexion angle was smaller in the CAI group during the middle and terminal stance phases. Additionally, the ankle inversion angle was greater in the CAI group than in the control group. Our findings show the application of the synchronized US and MA system in the assessment of mechanical instability in CAI group, which may be used to determine treatment efficacy.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-78682-y.
Keywords: Ultrasonography, Motion capture, Joint instability, Biomechanics, Ankle joint
Subject terms: Ligaments, Musculoskeletal system
Introduction
Lateral ankle sprain (LAS) is the most common musculoskeletal sports injury1. Recurrent LAS is present in approximately 18.0%–47.0% of cases, making it one of the most serious complications2. This high recurrence rate leads to a risk of progression to chronic ankle instability (CAI), which is observed in approximately 40–70% of patients following LAS3,4. CAI is a condition characterized by repetitive episodes or perceptions of the ankle giving way; ongoing symptoms such as pain, weakness, or reduced ankle range of motion; diminished self-reported function; and recurrent ankle sprains that persist for more than 1 year after the initial injury5. Compared to healthy individuals, patients with CAI display changes in ankle movement under dynamic conditions such as walking and sports activities6–8. Notably, a comparative analysis of ankle joint movements during gait between patients with CAI and healthy individuals revealed that patients with CAI had an increased ankle inversion angle during the early stance phase, a decreased ankle dorsiflexion angle during the middle stance phase, and an increased ankle plantarflexion angle during the terminal stance phase9. These differences in ankle kinematics from healthy individuals are thought to contribute to increased inversion stress on the lateral ankle, which may play a role in LAS recurrence10.
Altered ankle kinematics in CAI cases may also be affected by lack of stability in the lateral ankle ligament complex. A cross-sectional study evaluating the extent of lateral ankle ligament damage in 938 CAI cases using ultrasound (US) imaging revealed significant findings and reported that 92% of patients exhibited morphological abnormalities in the ligaments constituting the lateral ankle, particularly the anterior talofibular ligament (ATFL)11. The function of the ATFL is crucial not only for restraining the forward movement of the talus but also for inhibiting excessive ankle inversion. Therefore, patients with CAI have increased range of anterior movement of the talus and instability during ankle inversion. Recently, US has been adopted to assess biomechanical ankle instability12,13. A study correlating the anterior displacement of the talus relative to the tibia using US and radiography demonstrated a strong correlation, indicating the utility of US methods in evaluating bone displacement14. Additionally, the distance between the talus and lateral malleolus, which can be measured by placing the US probe on the lateral side of the ankle, showed a high correlation with the anterior talar displacement measured using stress radiographs15. A comparative study using US to assess the distance between the talus and lateral malleolus in individuals with CAI and healthy individuals indicated no significant difference in neutral ankle position. However, the CAI group showed a larger distance by approximately 2.8 mm in the ankle inversion position than did the healthy group16. Overall, these findings suggest that the stress on the ATFL potentially increases owing to the increase in the distance between the talus and lateral malleolus in specific ankle positions and that the stress on the ATFL may increase in certain ankle positions due to the increase in the distance between the talus and lateral malleolus. Nevertheless, these studies were conducted only under non-weight-bearing and static conditions.
Caputo et al. reported that increasing the weight load led to greater anterior talar displacement in ATFL injury cases compared with healthy cases17, implying that there may be different trends under loading conditions compared with those under static conditions. Additionally, compared with healthy individuals, patients with CAI demonstrate different joint movements during gait. However, identifying the distance between the talus and lateral malleolus on the basis of joint movements alone is difficult.
Therefore, the current study aimed to compare the distance between the talus and lateral malleolus as well as the ankle joint angles during the stance phase of gait between patients with CAI and healthy individuals using a synchronized US with a three-dimensional motion analysis (MA) system. We hypothesized that the distance between the talus and lateral malleolus would be increased during the stance phase of gait in patients with CAI compared with that in healthy individuals.
Material and methods
Participants
Twenty-two young adults voluntarily participated in this cross-sectional, observational study. The participants in the CAI group were screened using the following inclusion criteria, which were based on previous research: history of severe LAS leading to unloading, immobilization, or abnormal gait; two or more previous LAS incidents; Cumberland Ankle Instability Tool (CAIT) score ≤ 2418; and no history of substantial musculoskeletal surgical disorders in the lower limb, excluding ankle sprains19,20. The inclusion criteria for the control group were the following: no history of ankle sprains; CAIT score ≥ 25; no history of significant musculoskeletal surgical disorders in the lower limb19,20. The Foot Posture Index (FPI) was evaluated to confirm the foot and ankle alignments in both groups21. Participants with a FPI score of − 6 to + 10 (highly pronated foot) or − 5 to − 12 (highly supinated foot) were excluded23. The participants were subsequently divided into two groups—namely, the CAI group, which comprised 12 participants (5 males and 7 females; 16 feet), and the control group, which included 10 participants (4 males and 6 females; 20 feet). In the CAI group, 8 participants experienced only unilateral injuries, whereas 4 (2 males and 2 females) sustained bilateral injuries. Table 1 presents basic information about the participants.
Table 1.
General characteristics of participants in the CAI and control groups. Date are shown as mean ± SD. CAI, chronic ankle instability; BMI, body mass index; CAIT, Cumberland ankle instability tool; FPI, Foot Posture Index; SD, standard deviation.
| CAI group (n = 12, 16feet) |
Control group (n = 10, 20feet) |
p- value | |
|---|---|---|---|
| Sex (male/female) | 5/7 | 4/6 | |
| Age (years) | 20.5 ± 1.8 | 21.2 ± 1.6 | 0.189 |
| Height (cm) | 166.6 ± 9.4 | 164.6 ± 10.5 | 0.197 |
| Body weight (kg) | 60.2 ± 5.3 | 56.8 ± 11.3 | 0.409 |
| BMI (kg/m2) | 21.7 ± 2.0 | 20.8 ± 2.6 | 0.194 |
| The number ankle sprain (times) | 3.6 ± 2.0 | 0 ± 0 | < 0.001 |
| CAIT (score) | 15.3 ± 5.4 | 29.3 ± 0.6 | < 0.001 |
| FPI (score) | 2.1 ± 0.6 | 2.2 ± 1.0 | 0.964 |
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Hiroshima University Epidemiological Research Ethics Committee (approval number: E-2187). Informed consent was obtained from all participants.
Experimental procedure
Assessment of the distance between the talus and the lateral malleolus using B-mode US during gait
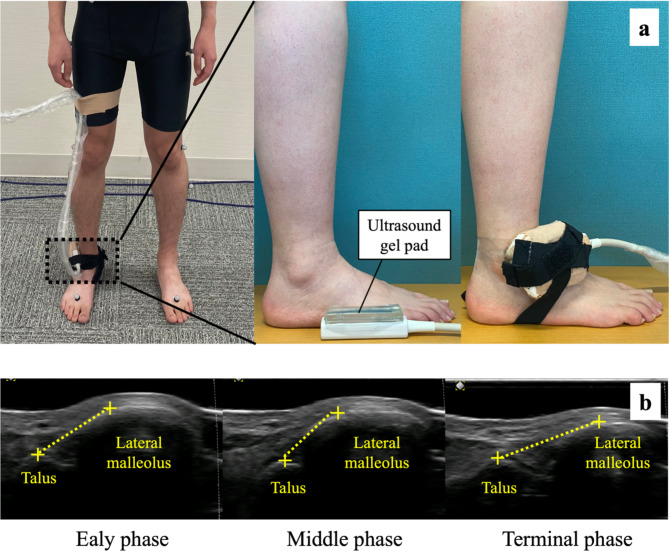
The distance between the talus and lateral malleolus was measured using a US system (Art Us EXT-1H; Telemed, Vilnius, Lithuania) with a US probe (5–11 MHz, 60–mm field of view; Echoblaster; Telemed) in B mode. First, a US gel pad (Yasojima Proceed Co., Ltd., Kobe, Japan) was placed between the US probe and the skin to enhance image quality and avoid pressure on the skin surface. Figure 1 shows the position of the US probe on the lateral side of the ankle. The placement of the US probe was adjusted to visualize the anterolateral aspect of the lateral neck of the talus and lateral malleolus along the ATFL on the US image22. Once the US probe position was optimized, it was rigidly secured using bands. To standardize the positioning of the US probe, the skin of each participant was marked to ensure no deviations.
Fig. 1.
The placement of the US probe on the lateral side of the ankle (a). The dynamics of the distance between the talus and lateral malleolus during gait (b).
Gait analysis
The participants walked 6 m over eight force plates (OR-6, 1,000 Hz; AMTI, Watertown, MA, USA). Gait analysis was conducted using a three-dimensional MA system (Vicon Motion Systems Ltd., Oxford, UK) equipped with 16 infrared cameras operating at 100 Hz23. The US system in this study was synchronized with a three-dimensional MA, triggering the simultaneous capture of a B-mode US video at 80 frames/s and an image depth of 60 mm24. Additionally, a software-based cine loop input function with a trigger switch (Telemed Echowave II, Vilnius, LT) was implemented to synchronize the US system with three-dimensional MA25. To ensure uniform marker placement, the same examiner placed 16 reflective markers on the lower body of each participant according to the Conventional Gait Model (Plug-in-Gait)24. After acquiring data in a static standing position, the participants performed two preliminary trials before walking across the force plates at their self-selected pace. The participants were instructed to take two initial steps before stepping onto the force plates. Finally, three gait trials were performed on each side.
Data analysis
The initial force plate data were processed along with the foot contact time points, and the gait phases were identified using a threshold of 10N for the vertical ground reaction force. The measurement of the distance between the talus and lateral malleolus was measured using Tracker version 5.1.5 (Open Source Physics; https://www.compadre.org) on B-mode US video, measuring the shortest distance between the anterolateral aspect of the lateral neck of the talus and lateral malleolus22. The stance phase from heel-strike to toe-off was normalized to 100 frames using normalization software. The one-stance phase was further divided into three stance subphases: early stance (0–33 frames), middle stance (34–66 frames), and terminal stance (67–100 frames)26.
Statistical analyses
Statistical analyses were performed using the Statistical Package for the Social Sciences version 28.0 for Mac (IBM Corp., Armonk, NY, USA). The normality of all results was confirmed using the Shapiro–Wilk test. The ICC1,3 was evaluated for the distance between the talus and lateral malleolus measured with the US system. The ICC1,3 was regarded as excellent if > 0.74, good if 0.60–0.74, fair if 0.40–0.59, and poor if < 0.40. Additionally, the standard error of the measurement was calculated for the US data at each stance phase for the CAI and control groups to demonstrate the accuracy of the measurements.
Two-way split-plot analysis of variance (ANOVA) was conducted, considering the presence or absence of CAI as an intersubject factor and the three phases of the gait cycle (early stance, middle stance, and terminal stance) as intrasubject factors. This analysis aimed to confirm the presence of an interaction effect between levels and main effects within levels. For items showing significant interaction or main effect, post hoc comparisons were conducted using unpaired t-tests between groups with Bonferroni correction. The ηp2 values were used to measure the effect size. The required sample size was calculated using priori power analysis (F-test) with G*Power 3.1 (Heinrich Heine University, Düsseldorf, Germany). The analysis, which assumed an effect size of f = 0.87 and an alpha level of p < 0.05, resulted in a total sample size of 17. Therefore, this study had sufficient power and an adequate sample size. The post-hoc observed power analysis, based on ηp2, used sample sizes of 16 feet for the CAI group and 20 feet for the control group. The post-hoc analysis resulted in an alpha level of P < 0.05 and a statistical power of 0.801, indicating adequate power. Statistical significance was set at P < 0.05.
Results
The results of the intraclass correlation coefficient (ICC1,3) for the distance between the talus and lateral malleolus between the CAI and control groups during the stance phase of gait are presented in Table 2. All ICC1,3 values for the measured variables demonstrated good results, exceeding 0.6.
Table 2.
Reproducibility of the distance between the talus and lateral malleolus during the stance phase of gait in the CAI and control groups. ICC, intraclass correlations coefficient; SEM, standard error of the measurements; CAI, chronic ankle instability. The SEM was calculated using the formula s√1-ICC. Values in parentheses are 95% confidence intervals for the ICC and lower and upper limits for the SEM.
| Stance phase | CAI group | Control group | |||||
|---|---|---|---|---|---|---|---|
| ICC 1,3 | 95% CI | SEM | ICC 1,3 | 95% CI | SEM | ||
| Distance between the talus and lateral malleolus | Early stance | 0.754 | 0.439–0.906 | 0.209 | 0.736 | 0.448–0.887 | 0.172 |
| Middle stance | 0.799 | 0.544–0.924 | 0.216 | 0.681 | 0.334–0.863 | 0.201 | |
| Terminal stance | 0.776 | 0.489–0.915 | 0.185 | 0.807 | 0.596–0.917 | 0.241 | |
The analysis of variance for the presence of CAI, distance between the talus and lateral malleolus, and ankle joint angles during the stance phase
The results of the two-way split-plot ANOVA, with the presence or absence of CAI as the intersubject factor and the t distance between the talus and lateral malleolus and ankle angles during the three phases of the gait cycle as the intrasubject factors, are presented in Table 3. Items showing significant interaction effects were the distance between the talus and lateral malleolus (F = 10.684, P = 0.002, partial η2 [ηp2] = 0.239) and the ankle dorsiflexion/plantarflexion angle (F = 12.056, P = 0.001, ηp2 = 0.248). No significant interaction effect was observed for the ankle eversion/inversion angle (F = 0.765, P = 0.925, ηp2 = 0.022).
Table 3.
Two-way split-plot ANOVA results of the distance between the talus and lateral malleolus, ankle dorsiflexion/plantar flexion angle and ankle eversion/inversion angle.
| Stance phase | Interaction (CAI*phase) | Main effect (CAI) | Main effect (phase) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Early phase | Middle phase | Terminal phase | ||||||||||||||||
| CAI group | Control group | CAI group | Control group | CAI group | Control group | F | p | ηp2 | Observed power | F | p | ηp2 | Observed power | F | p | ηp2 | Observed power | |
| Distance between the talus and lateral malleolus, mm | 18.96 ± 1.96 * | 16.06 ± 1.04 | 17.45 ± 1.67 * | 14.45 ± 1.28 † | 20.01 ± 1.64 *, § | 15.47 ± 1.50 ‡ | 10.684 | 0.002 | 0.239 | 0.888 | 42.410 | < 0.001 | 0.555 | 1.000 | 70.453 | < 0.001 | 0.674 | 1.000 |
|
Ankle dorsiflexion/plantarflexion, ° +, dorsiflexion; −, plantarflexion |
2.02 ± 2.10 | 2.37 ± 1.88 | 9.43 ± 2.14 † | 12.22 ± 1.91 *, † | 9.89 ± 3.56 | 14.23 ± 2.80 *, ‡ | 12.056 | 0.001 | 0.248 | 0.931 | 14.252 | < 0.001 | 0.295 | 0.956 | 94.344 | < 0.001 | 0.896 | 1.000 |
|
Ankle eversion/inversion, ° +, eversion ; −, inversion |
0.68 ± 0.57 | 1.34 ± 1.41 | -0.44 ± 0.48 | 0.42 ± 1.28 | -1.28 ± 0.87 | -0.65 ± 1.27 | 0.765 | 0.925 | 0.022 | 0.070 | 4.390 | < 0.044 | 0.114 | 0.530 | 165.632 | < 0.001 | 0.830 | 1.000 |
Data are shown as mean ± standard deviation. D Cohen’s d, ηp2 partial eta-squared; p, p-value. The distance between the talus and lateral malleolus and the ankle dorsiflexion/plantarflexion angle showed significant differences based on the basis of the presence of CAI. Significant main effects are observed for the distance between the talus and lateral malleolus, ankle dorsiflexion/plantarflexion angle, and ankle eversion/inversion angle. CAI, chronic ankle instability. * post-hoc test (P < 0.001) between the CAI and control groups, † post-hoc test (P < 0.001) between the early stance and middle stance, ‡ post-hoc test (P < 0.05), § post-hoc test (P < 0.001) between the middle stance and terminal stance. The ankle dorsiflexion/plantarflexion angles were d = 1.376 in middle stance, and d = 1.371 in terminal stance.
The main effects for the group were observed for the ankle eversion/inversion angles. Additionally, the main effects of the stance phase were observed on the ankle eversion/inversion angles.
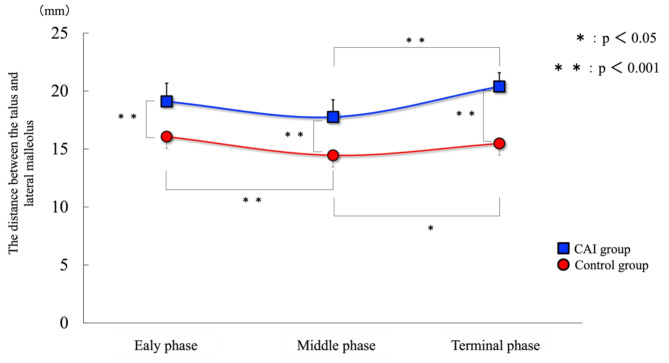
Comparison of the distance between the talus and lateral malleolus between the CAI and control groups during each stance phase
The results comparing the distance between the talus and lateral malleolus between the CAI and control groups during the different phases of the stance period are presented in Fig. 2. In the early stance, the CAI group exhibited a significantly larger distance between the talus and lateral malleolus than the control group (18.96 ± 1.96 vs. 16.06 ± 1.04 mm, P < 0.001). In the middle stance, the corresponding values were 17.45 ± 1.67 mm for the CAI group and 14.45 ± 1.28 mm for the control group, showing a significant difference (P < 0.001). During the terminal stance phase, the CAI group continued to have a significantly larger distance between the talus and lateral malleolus than the control group (20.01 ± 1.64 vs. 15.47 ± 1.50 mm, P < 0.001).
Fig. 2.
Comparison of the distance between the talus and lateral malleolus between the CAI and control groups during stance phases. Compared to the control group, the CAI group shows a significant increase in the distance between the talus and lateral malleolus during the early, middle, and terminal stance phases.
Intragroup comparisons between the stance phase revealed that the distance between the talus and lateral malleolus in the CAI group showed minimal differences between the early stance and the middle stance (P = 0.065) but significant increases from the middle stance to the terminal stance (P < 0.001). Conversely, in the control group, the distance between the talus and lateral malleolus significantly increased from the early stance to the middle stance (P < 0.001) and further increased from the middle stance to the terminal stance (P < 0.05).
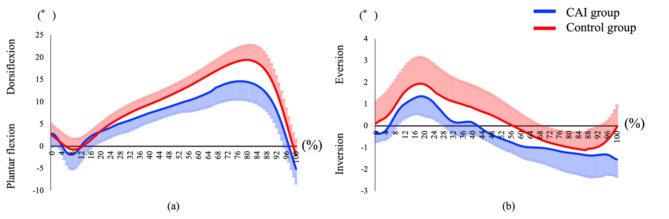
Comparison of the ankle dorsiflexion/plantarflexion angles between the CAI and control groups during the stance phase
Table 3 and Fig. 3a present the results of the comparison of ankle dorsiflexion/plantarflexion angles between the CAI and control groups during the stance phase. During the middle and terminal stance phases, the ankle dorsiflexion angle was significantly smaller in the CAI group than in the control group (P < 0.001).
Fig. 3.
Comparison of ankle dorsiflexion/planter flexion angle by stance phases between the CAI and control groups (a). Comparison of ankle eversion/inversion angle by stance phases between the CAI and control groups (b).
Intragroup comparisons between the stance phase revealed that the CAI group showed a significant increase in ankle dorsiflexion/plantarflexion angles from early stance to middle stance (P < 0.001), but there was no significant difference from middle stance to terminal stance (P = 1.000). The control group also showed a significant increase in ankle dorsiflexion/plantarflexion angles from early stance to middle stance (P < 0.001), followed by a significant decrease from middled stance to terminal stance (P < 0.05). The differences in ankle dorsiflexion/plantar flexion angles during the stance phase, with and without the probe, were not statistically significant (Supplemental Fig. 1).
Comparison of the ankle eversion/inversion angles between the CAI and control groups during the stance phase
Table 3 and Fig. 3b illustrate the ankle eversion/inversion angles between the CAI and control groups during the stance phase. During the stance phase of gait, the inversion angles in the CAI group were significantly larger than those in the control group (P < 0.001).
Discussion
This is the first study to clarify the dynamics of the distance between the talus and lateral malleolus during the stance phase of gait using a synchronized US with MA approach, showing good measurement reproducibility. The most notable result was that the distance between the talus and lateral malleolus in the CAI group was significantly increased compared with that in the control group during all phases of stance: 2.9 mm (16%) in the early stance, 3.0 mm (18%) in the middle stance, and 4.6 mm (23%) in the terminal stance. CAI cases exhibit anterior displacement of the talus relative to the tibia, possibly due to morphological abnormalities, such as complete or partial rupture and elongation of the ATFL27,28.
In this study, the distance between the talus and lateral malleolus during the early stance phase in the CAI group was 2.9 mm greater than that in the control group. Additionally, during the early stance phase, the ankle inversion angle increased in the CAI group. However, the two groups did not differ in terms of ankle plantarflexion and dorsiflexion angles. A previous study measuring the distance between the talus and lateral malleolus under static conditions in the neutral position reported a difference of only 0.2 mm between the CAI and control groups, suggesting no significant variation under static conditions16. Of note, we were able to capture changes in the distance between the talus and lateral malleolus during the early stance of gait under dynamic conditions, which may not be comparable to static conditions. This likely resulted in different outcomes under dynamic conditions compared with those under static conditions because the distance between the talus and lateral malleolus changes with variations in ankle position16 and anterior talar displacement increases with weight-bearing, as previously reported17. The increased distance between the talus and lateral malleolus in the early stance phase of gait observed in this study, coupled with the increased ankle inversion angles during the stance phase of gait in patients with CAI, may be indicative of a higher risk of recurrent LAS. Additionally, characteristics of the peroneal muscle group with CAI include a delayed muscle reaction time and reduced muscle activity29,30. The peroneal muscles are crucial for counteracting ankle inversion. An increase in ankle inversion angle can widen the distance between the talus and lateral malleolus16, and the increase in inversion angle during the early stance phase may have contributed to this effect.
During the middle stance, the distance between the talus and lateral malleolus in the CAI group increased by 3.0 mm, and the ankle dorsiflexion angle was 2.9° smaller in the CAI group than in the control group. A study using a three-dimensional bone model to investigate the contact area between the tibia and the talus revealed that in patients with CAI during the middle stance, the contact pressure between the tibia and talus was displaced anteriorly compared with that in control individuals31. This confirmed our study result, which indicated that the distance between the talus and lateral malleolus increased during the middle stance of gait in the CAI group. Moreover, anterior displacement of the talus may lead to insufficient posterior sliding motion, as indicated by the distance between the talus and lateral malleolus during the middle stance in CAI cases. This could have contributed to the reduction in the range of ankle dorsiflexion observed in the CAI group during the middle and terminal stance phases of gait32. Anterior displacement of the talus relative to the tibia during dorsiflexion in CAI cases may result in impingement between the anterior inferior aspect of the tibia and the anterior talus, contributing to the occurrence of anterior ankle impingement syndrome, which is commonly observed in CAI cases33.
The CAI group exhibited no difference in the distance between the talus and lateral malleolus from early to middle stances but showed an increase from middle to terminal stances. In contrast, the control group exhibited an increase in this distance from early to middle stances and again from middle to terminal stances. With respect to the ankle dorsiflexion/plantarflexion angles, the CAI group displayed an increase from early to middle stances with no further change, whereas the control group exhibited an increase from early to middle stances and subsequently a decrease from middle to terminal stances. These findings may indicate that normal ankle motion occurs during gait because the talus moves posteriorly when the ankle dorsiflexes, shortening the distance between the talus and lateral malleolus. Conversely, when the ankle plantarflexes, the talus moves anteriorly, increasing the distance between the talus and lateral malleolus. These observations are based on findings in cadaver studies34.
Our data revealed the dynamics of the talus, which could not be identified using MA systems alone. A study that used dual fluoroscopy reported an increased anterior displacement of the talus relative to the tibia during gait, despite revealing no significant differences in ankle joint motion35. However, these studies have limitations, including the risk of radiation exposure, need to place the foot in a predetermined position, and deviations from normal gait patterns35. Synchronization of the US and MA system in this study allowed for measurements that were closely similar to normal gait without the risk of radiation exposure. Additionally, this method provided objective data on talus dynamics, which previously could only be inferred from joint movements. This might have considerable clinical value for establishing treatment and preventive interventions for LAS. Future research should investigate the relationship between joint movements and the distance between the talus and lateral malleolus to determine which specific joint movements should be targeted during gait interventions.
This study has some limitations that warrant discussion. First, we did not consider the severity of LAS, which might affect the structures around the ankle joint, including the ligaments. The frequency of LAS may also influence the outcomes. Second, individual differences in the shape of the talus and lateral malleolus have been reported15. Therefore, factors such as sex differences should be considered to improve the accuracy of measurements. Third, the selection criteria for the CAI group requires further consideration. CAI involves complex factors related to joint structure, muscle strength, and balance around the ankle joint, all of which should be evaluated in future studies, while examining changes in the distance between the talus and lateral malleolus and in ankle joint motion during gait. Lastly, we cannot rule out the possibility that the US probe may have influenced ankle kinematics during gait.
In conclusion, the application of the synchronized US and MA system revealed differences in tibiotalar kinematics between patients with CAI and healthy controls, revealed that the distance between the talus and lateral malleolus during the stance phase of gait was significantly increased in the CAI group. The CAI group exhibited a decrease in dorsiflexion angle and an increase in ankle inversion angle. These results suggest that the CAI group experiences increased tensile stress on the ATFL during the stance phase of gait, even if no differences of the talofibular distance were identified under static conditions. Application of a synchronized US and MA system may serve as a novel evaluation tool to assess physical therapy and orthopedic treatment on tibiotalar kinematics in patients with CAI during the stance phase of gait.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank the participants in this study, as well as Editage for English language editing.
Author contributions
S.O., N.M. and Y.I.: Investigation, Resources, Writing–original draft, and Writing–review & editing; T.T., S.A. and H.I.: Software, Visualization, and Formal analysis; A.I. and A.B.: Data curation; S.T. and M.K.: Formal analysis; T.N. and N.A.: Investigation, Resources, Writing–original draft, Writing–review & editing, and Methodology; Y.U.: Formal analysis and Data curation.
Data availability
The datasets for the present study are available upon request from the corresponding author.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tsubasa Tashiro, Email: tsubasatashiro716@hiroshima-u.ac.jp.
Yukio Urabe, Email: yurabe@hiroshima-u.ac.jp.
References
- 1.Roos, K. G., Kerr, Z. Y., Mauntel, T. C., Djoko, A. & Dompier, T. P. The epidemiology of lateral ligament complex ankle sprains in national collegiate athletic association sports. Am. J. Sports Med.45, 201–209 (2017). [DOI] [PubMed] [Google Scholar]
- 2.Herzog, M., Kerr, Y., Marshall, W. & Wikstrom, A. Epidemiology of ankle sprains and chronic ankle instability. J. Athl. Train.54, 603–610 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doherty, C. et al. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: a prospective cohort analysis. Am. J. Sports Med.44, 995–1003 (2016). [DOI] [PubMed] [Google Scholar]
- 4.Phillip, A. et al. Evidence review for the 2016 international ankle consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med.50, 1496–1505 (2016). [DOI] [PubMed] [Google Scholar]
- 5.Hertel, J. & Corbett, R. O. An updated model of chronic ankle instability. J. Athl. Train.54, 572–588 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown, C. N., Bowser, N. & Orellana, A. Dynamic postural stability in females with chronic ankle instability. Med. Sci. Sports Exerc.42, 2258–2263 (2010). [DOI] [PubMed] [Google Scholar]
- 7.Yu, P., Mei, Q., Xiang, L., Fernandez, J. & Gu, Y. Differences in the locomotion biomechanics and dynamic postural control between individuals with chronic ankle instability and copers: A systematic review. Sports Biomechanics21, 531–549 (2022). [DOI] [PubMed] [Google Scholar]
- 8.Kwon, Y. U., Harrison, K., Kweon, S. J. & Williams, D. S. B. Ankle coordination in chronic ankle instability, coper, and control groups in running. Med. Sci. Sports Exerc.52, 663–672 (2020). [DOI] [PubMed] [Google Scholar]
- 9.Lee, L., Ha, S., Chae, S., Jeong, H. S. & Lee, S. Y. Altered biomechanics in individuals with chronic ankle instability compared with copers and controls during gait. J. Athl. Train.57, 760–770 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koldenhoven, R. M., Hart, J., Saliba, S., Abel, M. F. & Hertel, J. Gait kinematics & kinetics at three walking speeds in individuals with chronic ankle instability and ankle sprain copers. Gait Posture10, 169–175 (2019). [DOI] [PubMed] [Google Scholar]
- 11.Li, Q., Li, Y. & Hua, Y. Prevalence and injury patterns of CFL injury in chronic lateral ankle instability: an observational cross-sectional study using ultrasound. J. Foot Ankle Surg.18, S106725162300193X (2023). [DOI] [PubMed] [Google Scholar]
- 12.Abdeen, R., Comfort, P., Starbuck, C. & Nester, C. Ultrasound characteristics of foot and ankle structures in healthy, coper, and chronically unstable ankles. Ultrasound Med.38, 917–926 (2019). [DOI] [PubMed] [Google Scholar]
- 13.Cao, S. et al. Imaging diagnosis for chronic lateral ankle ligament injury: A systemic review with meta-analysis. J. Orthop. Surg. Res.13, 122 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saengsin, J., Bhimani, R., Sato, G., Hagemeijer, N. C. & Mirochnik, K. Use of portable ultrasonography for the diagnosis of lateral ankle instability. J. Orthop. Res.40, 2421–2429 (2022). [DOI] [PubMed] [Google Scholar]
- 15.Lee, K. T. et al. New method of diagnosis for chronic ankle instability: Comparison of manual anterior drawer test, stress radiography and stress ultrasound. Knee Surg Sports Traumatol Arthrosc.22, 1701–1707 (2014). [DOI] [PubMed] [Google Scholar]
- 16.Croy, T., Saliba, S. A., Saliba, E., Anderson, M. W. & Hertel, J. Differences in lateral ankle laxity measured via stress ultrasonography in individuals with chronic ankle instability, ankle sprain copers, and healthy individuals. J. Orthop. Sports Phys. Ther.42, 593–600 (2012). [DOI] [PubMed] [Google Scholar]
- 17.Caputo, A. M. et al. In Vivo Kinematics of the Tibiotalar Joint After Lateral Ankle Instability. Am J Sports Med.37, 2241–2248 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gribble, P. A. et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the international ankle consortium. J Athl Train.49, 121–127 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delahunt, E. et al. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med. Sci. Sports Exerc.42, 2106–2121 (2010). [DOI] [PubMed] [Google Scholar]
- 20.Hiller, C. E., Refshauge, K. M., Bundy, A. C., Herbert, R. D. & Kilbreath, S. L. The Cumberland ankle instability tool: A report of validity and reliability testing. Arch. Phys. Med. Rehabil.87, 1235–1241 (2006). [DOI] [PubMed] [Google Scholar]
- 21.Redmond, A. C., Crosbie, J. & Ouvrier, R. A. Development and validation of a novel rating system for scoring standing foot posture: the Foot Posture Index. Clin. Biomech.21, 89–98 (2006). [DOI] [PubMed] [Google Scholar]
- 22.Özgül, B., Starbuck, C., Polat, M. G., Abdeen, R. & Nester, C. Inter and intra-examiner reliability of musculoskeletal ultrasound scanning of anterior talofibular ligament and ankle muscles. J. Ultrasound26, 137–146 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maeda, N. et al. Quantitative evaluation of the vertical mobility of the first tarsometatarsal joint during stance phase of gait. Sci. Rep.12, 9246 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tashiro, T., Ikuta, Y., Maeda, N., Arima, S. & Morikawa, M. First tarsometatarsal joint mobility in hallux valgus during gait: a synchronized ultrasound and three-dimensional motion capture analysis. J. Med. Ultrasonics28, 331–339 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brand, A. et al. Recovery of the medial gastrocnemius muscle after calcaneus fracture differs between contractile and elastic components. Clin. Biomech.96, 105664 (2022). [DOI] [PubMed] [Google Scholar]
- 26.Kim, E. J. et al. Inter-segmental foot kinematics during gait in elderly females according to the severity of hallux valgus. J. Orthop. Res.38, 2409–2418 (2020). [DOI] [PubMed] [Google Scholar]
- 27.Hertel, J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J. Athl. Train.37, 364–375 (2002). [PMC free article] [PubMed] [Google Scholar]
- 28.Liu, K. et al. Increased ligament thickness in previously sprained ankles as measured by musculoskeletal ultrasound. J. Athl. Train.50, 193–198 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tashiro, T. et al. Tensiomyographic neuromuscular response of the peroneus longus and tibialis anterior with chronic ankle instability. Healthcare.9, 707 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arima, S. et al. Morphological and functional characteristics of the peroneus muscles in patients with lateral ankle sprain: An ultrasound-based study. Medicina58, 70 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bae, J. Y., Park, K. S., Seon, J. K. & Jeon, I. Analysis of the effects of normal walking on ankle joint contact characteristics after acute inversion ankle sprain. Ann. Biomed. Eng.43, 3015–3024 (2015). [DOI] [PubMed] [Google Scholar]
- 32.Kobayashi, T. et al. Characteristics of the statics muscle stiffness of ankle planter flexors in individuals with chronic ankle instability. J. Med. Ultrason.50, 561–570 (2023). [DOI] [PubMed] [Google Scholar]
- 33.Lavery, K. P., McHale, K. J., Rossy, W. H. & Theodore, G. Ankle impingement. J. Orthop. Surg. Res.11, 97 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khawaji, B. & Soames, R. The anterior talofibular ligament: A detailed morphological study. Foot.25, 141–147 (2015). [DOI] [PubMed] [Google Scholar]
- 35.Cao, S. et al. In vivo kinematics of functional instability patients during the stance phase of walking. Gait Posture.73, 262–268 (2019). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets for the present study are available upon request from the corresponding author.