Abstract
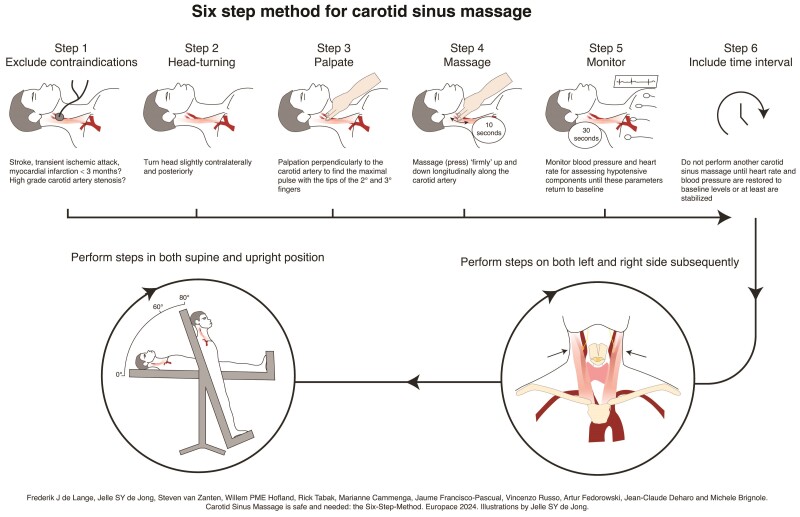
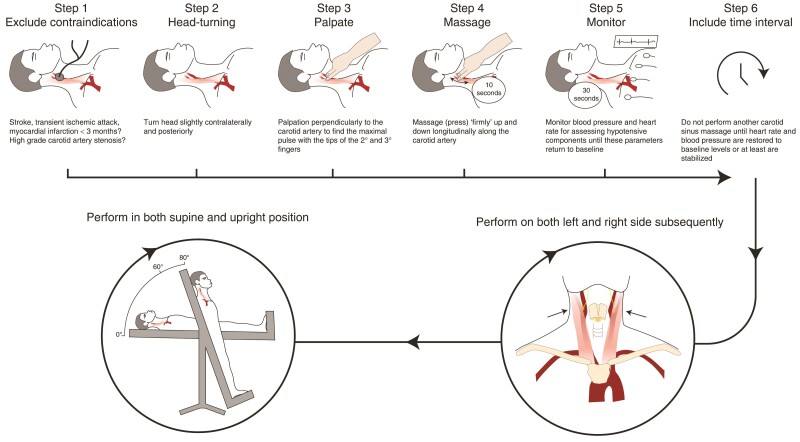
Carotid sinus massage (CSM) as integral part of cardiovascular autonomic testing is indicated in all patients > 40 years with syncope of unknown origin and suspected reflex mechanism. However, large practice variation exists in performing CSM that inevitably affects the positivity rate of the test and may result in an inaccurate diagnosis in patients with unexplained syncope. Even though CSM was introduced into medical practice more than 100 years ago, the method of performing CSM is still largely operator- and centre-dependent, while in many places, the test has been entirely abandoned. Here, we describe a standardized protocol on how to perform CSM, which basic monitoring equipment is necessary and why CSM is a safe procedure to perform. Our aim is to create a uniform approach to perform CSM. The new proposed algorithm, the Six-Step-Method, includes: (i) check history for exclusion CSM; (ii) turn head slightly contralaterally and posterior (see also explanatory video and poster provided as Supplementary material; (iii) palpation to identify carotid sinus location; (iv) massage for 10 s; (v) monitoring of blood pressure and heart rate to assess of the haemodynamic response type; and (vi) include time intervals between subsequent massages. Carotid sinus massage should be performed on both the left and right and in the supine and upright position. The recommended equipment to perform CSM consists of: (i) a tilt table in order to perform CSM in supine and standing position, (ii) a continuous blood pressure monitor or cardiac monitor, and (iii) at least two persons.
Keywords: Carotid sinus massage, Tilt table testing, Syncope, Haemodynamic monitoring, Video recording
Graphical Abstract
Graphical Abstract.
What’s new?
The Six-Step-Method is proposed as standardized protocol to perform carotid sinus massage.
The equipment and personnel to perform carotid sinus massage are reviewed.
Complication rate of carotid sinus massage in historical and current cohorts are reviewed.
Explanatory video and poster of the Six-Step-Method are provided as Supplementary material.
Introduction
Patients presenting after a syncopal episode are often asymptomatic upon evaluation as the event has already passed. To identify the cause of syncope, first, the initial syncope evaluation is performed,1 often yielding a diagnosis. However, when no diagnosis can be made using history taking, an active standing test and an electrocardiogram, further investigation is warranted. One specific cause of syncope, carotid sinus hypersensitivity (CSH), can be triggered manually by the physician. This is done by massaging the carotid sinus. Carotid sinus massage (CSM) is the only diagnostic tool for CSH, an exaggerated response to external stimulation of carotid sinus baroreceptors. Carotid sinus hypersensitivity is defined as a fall in systolic blood pressure of at least 50 mmHg and/or three or more seconds asystole upon applying a firm pressure to the carotid sinus (Figures 1 and 2).1 When asymptomatic, CSH is largely unrelated to syncope and has a low diagnostic value. For this reason, the diagnosis of carotid sinus syndrome (CSS) requires the presence of CSH and reproduction of symptoms (syncope or near-syncope) during massage.1 In the case that the patient does not remember the circumstances before fainting circumstances, then we must rely on symptom recognition during CSM. According to the 2018 European Society of Cardiology (ESC) syncope guidelines,1 CSS is confirmed if CSM causes asystole (>3e seconds) and/or hypotension (>50 mmHg) with reproduction of spontaneous symptoms, and patients have clinical features compatible with a reflex mechanism of syncope.1 With increasing age, CSH becomes more prevalent.2 In patients younger than 40 years old, CSH is very rare.3–5 Therefore, CSM is indicated in all patients > 40 years of age with syncope of unknown origin and compatible with a reflex mechanism.6 However, CSM may also be considered in younger patients who had undergone neck surgery or radiation, especially close to the locus of carotid sinus. A positive response to CSM demands a class I indication for therapy.1
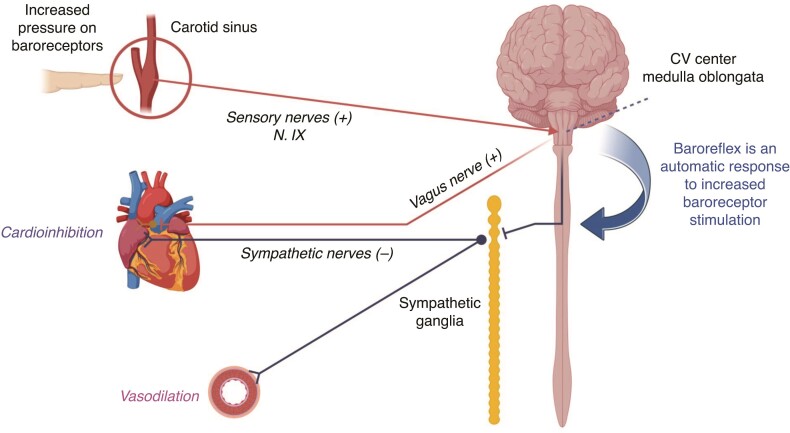
Figure 1.
Schematic drawing of the baroreceptor afferent and autonomic efferent pathways of the baroreflex arc. The afferent signals are transferred to the cardiovascular (CV) centre in medulla oblongata by the glossopharyngeal nerve (IX). When activated, the centre acts through efferents on effector organs via the vagus nerve (X) to the heart, causing bradycardia or asystole, and via sympathetic ganglia, leading to profound vasodilation and hypotension. CSM, carotid sinus massage.
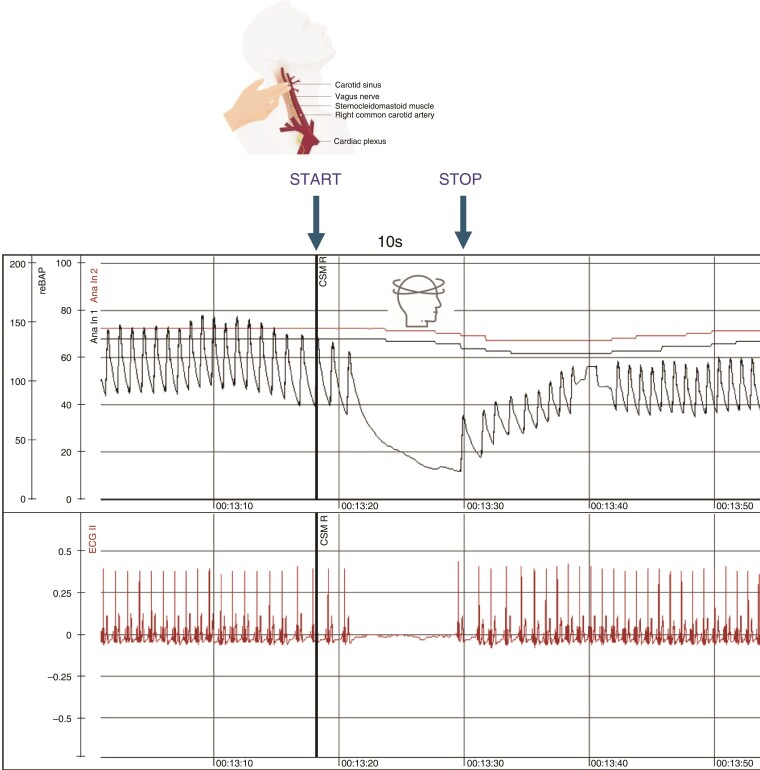
Figure 2.
Carotid sinus massage performed on the right side in supine position in 50-year-old woman with recurrent syncopal attacks occurring in different body positions, including lying in the bed. A profound cardioinhibitory response with sinus arrest of 10 s, syncope, and total reproduction of spontaneous attacks. Please note that the slight deceleration of heart rate in the two beats preceding the marker (‘START’) was due to a gentle pressure to the neck when looking for the maximal pulsation, like we describe in step 3 of the Six-Step-Method. The patient was effectively treated with pacemaker and without recurrences over a period of five years. CSM, carotid sinus massage.
Nevertheless, CSM is largely underutilized in clinical practice and, when performed, its methodology of execution varies as also is the interpretation of its CSM results (see next section). Here, we explore the reasons for the high variability of CSM execution across different countries and diagnostic centres and offer practical instruction on how to perform CSM and how to interpret its results.
Barriers to a proper utilization of carotid sinus massage in the diagnosis of syncope
Inter-operator and inter-centre variability in indications and interpretation of positive responses
The frequency of CSS diagnosed in syncope clinics varies widely in literature, owing to differences in indications, methods of execution of CSM,7 the definition of CSS,8,9 and fear of possible complications caused by the procedure itself.10–12 This results in large practice variation in execution of CSM across different countries and diagnostic centres and makes many physicians sceptical about the real usefulness of the test and reluctant to perform it.2,13
Consequently, CSM is largely underused in clinical practice outside highly specialized syncope facilities, especially in USA, being performed in 0.07–8% among patients investigated for unexplained syncope above 40 years of age.14–19 In a recent survey on syncope units in The Netherlands, CSM is usually not performed at all in 20% of the reporting centres and performed incomplete in 50% of the remaining centres. Among centres that perform CSM, one-fourth of them do this without continuous blood pressure monitoring.20 In Sweden, two out of nine academic centres perform CSM according to the ESC guideline on syncope, and two others perform CSM only in selected cases (national unpublished survey data provided by AF).
Even when CSM is performed in both supine and upright position and on both left and right carotid arteries, the positive diagnostic yield of CSM varies between 4% and 14.6% of examined patients in different settings.21–23 A great inter-operator variability exists. For example, in a recent study,23 the positivity rate varied greatly from 0% to 36% among eight syncope centres with trained staff.
False perception of the risks
It is commonly believed that CSM may in some cases lead to cerebral ischaemic attacks and caution should be taken before performing such procedure.24 This belief comes from the reports of the old literature of the last century. In a pooled analysis of published studies (Table 1), an ischaemic attack had occurred in 30 out of 8319 patients, i.e. 3.6 events per 1000 patients. In most cases, the event was transient with complete rapid recovery. For the above reasons, it is likely that some physicians refrain from performing CSM because of the fear of causing an irreversible damage to the patient and the risk of subsequent liability issues.
Table 1.
Complication rate of carotid sinus massage before the year 2000
| Inclusion period | n (patients) | Age, mean ± SD | Males, % | TIA/stroke (%) | Specification of complication | |
|---|---|---|---|---|---|---|
| Puggioni et al. Am J Cardiol 20023 | 1996–2000 | 1719 | 63 ± 16 | 56% | 3 (0.17%) | TIAs < 24 h in 3 |
| Davies et al. Am J Cardiol 199826 | 1993–1998 | 4000 | 74 ± 14 | na | 11 (0.27%)a | TIAs < 24 h in 9, persistent hemiparesis in 1, visual field loss in 1 |
| Munro et al., JAGS 199427 | na | 1600 | na | na | 7 (0.44%)b | TIAs < 24 h in 4, stroke from 1 to 7 days in 3 |
| Richardson et al. Age ageing 200028 | na | 1000 | 69 ± 10 | 31% | 9 (0.9%)c | TIAs < 24 h in 8, mild weakness of right hand > 24 h |
| Total | 8319 d | 30 (0.36%) | ||||
| 3.6/1000 |
TIAs, transient ischaemic attacks; na, not available; SD, standard deviation.
aDavies: 2 pts had had previous TIA/stroke beyond 6 months. Carotid Doppler normal in 9, stenosis 70% in 2.
b1 pt had 70% carotid artery stenosis.
cDoppler ultrasound normal in 8, carotid stenosis 50% in one.
dTotal patients included in the complication analysis.
Factually, the complication rate has greatly decreased in the last two decades, being two out of 6328 patients, i.e. one case per 10 000 patients in a pooled analysis of three large series of modern syncope units (Table 2), a significant decrease when compared with the old studies of the last century (P < 0.0001). Thus, CSM is a very safe procedure even if we must be aware of reporting bias of outcomes in this pooled analysis of published studies. There, are several possible explanations for this great decrease. Over the past two decades, a shift of epidemiology has occurred that might be responsible for the observed persistently lower complication rate by: (i) better risk assessment in the current practice for older patients with unexplained syncope10; (ii) better preventive and treatment strategies against stroke25; (iii) better selection of patients with unexplained syncope > 40 years of age in whom CSM is indicated and performed; and (iv) the standardization of the method of performing the massage, due to the implementation of the guidelines in current medical practice that recommend the complete initial syncope evaluation in every patient with syncope.1
Table 2.
Complication rate of carotid sinus massage in a modern syncope unit
| Inclusion period | n (patients) | Age, mean ± SD or median (IQR) | Males, % | TIA/stroke (%) | Specification of complication | |
|---|---|---|---|---|---|---|
| Torabi et al. Europace 202321 | 2008–2021 | 1634 | 64 ± 13 | 39% | 0 | 0 |
| Brignole et al. Europace 202022 | 2003–2019 | 3293 | 73 (64–80) | 48% | 2 (0.06%) | TIAs < 24 h in 2 |
| Ungar et al. Age and Ageing 201611 | na | 1401 | 72 ± 16 | 41% | 0 | 0 |
| Total | 6328 a | 2/6328 (0.03%) | 0 | |||
| 3/10 000 |
TIAs, transient ischaemic attacks; SD, standard deviation; na, not available; IQR, interquartile range.
aTotal patients included in the complication analysis.
How to perform carotid sinus massage in supine and upright position: the Six-Step-Method according to the method of symptoms
During CSM instant and rapid changes in blood pressure may occur that makes sphygmomanometer method inadequate. To measure these rapid changes, continuous blood pressure measurements are needed. For the assessment of syncope, this is preferably done using a non-invasive-beat-to-beat blood pressure monitor (e.g. Finapres NOVA® or Task Force®) (Table 3). In this way, instant variations in both blood pressure and heart rate (HR) can be observed during CSM.7,29–31 Continuous blood pressure monitoring is necessary for a precise assessment of the magnitude of the vasodepressor component of the reflex, which can be missed by intermittent measurement traditional blood pressure recording using standard cuff. Nevertheless, we recognize the need to perform CSM also in those settings in which an instrument for continuous non-invasive blood pressure monitoring is not available. In such circumstances, CSM may identify a significant number of patients with cardioinhibitory responses to CSM who may be candidates for pacing or other interventions, however the assessment of an associated hypotensive reflex should be performed by means of other tests, e.g. tilt testing.
Table 3.
Equipment and personnel to perform carotid sinus massage
| Equipment/personnel | Explanation | |
|---|---|---|
| 1 | Tilt table | In order to perform CSM in the upright position after performing CSM in supine position without the risk of injury (see also explanatory video as Supplementary material) |
| 2 | Continuous blood pressure monitor or cardiac monitora | Non-invasive-beat-to-beat monitoring order for detection instant changes in HR and blood pressure |
| 3 | Two persons | One that performs the CSM and one that controls the marker on continuous blood pressure monitor |
CSM, carotid sinus massage; HR, heart rate.
aIn some hospitals, CSM is performed without access to continuous blood pressure monitoring, which is a suboptimal approach as the investigator can miss an important vasodepressive reflex component with negative therapeutic consequences. Thus, the authors encourage applying the most optimal methodology as presented below.
Carotid sinus massage should be performed on both the right side and left side, with the patient in both supine and upright position [in head-up tilt (HUT) between 60 and 80°], resulting in a total of four separate carotid sinus massages per patient (Figure 3, explanatory video and poster provided as Supplementary material in this paper).
Figure 3.
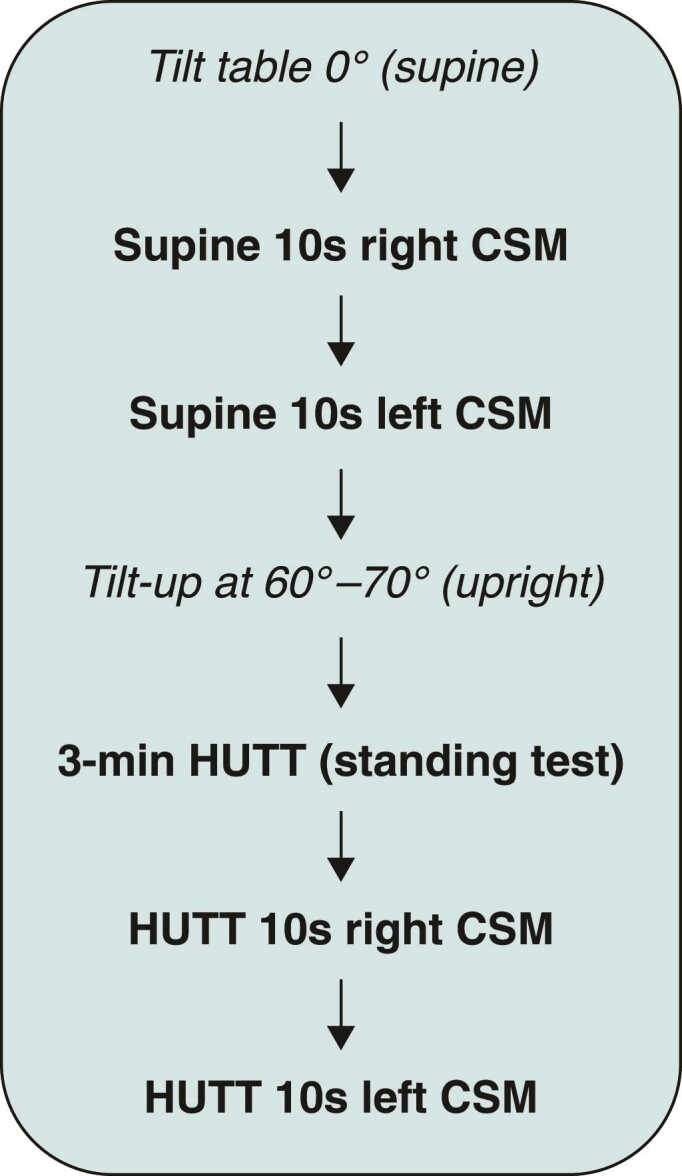
The sequence of carotid sinus massages.
Performing CSM in both supine and upright position is important since CSM can, in some patients, be positive in one position only, and in some cases, the positive response is cardioinhibitory in supine but vasodepressive in standing position.23 To prevent injury of the patient caused by a fall due to syncope during CSM in the upright position, CSM should be performed when patients are fixed by straps as is done during regular head-up tilt testing (HUTT).29,30 In order to perform CSM in the upright position, one must take into account that also in the upright position, both the patient and the haemodynamic parameters should be visible for the operator during and after CSM. Carotid sinus massage can be easily combined with HUTT during short autonomic cardiovascular assessment as recently described and shown in our explanatory video that is included in this paper as Supplementary material32–34 (Table 3, Figure 4). The atropine test is useful to unmask an underlying vasodepressor response in patients with cardioinhibitory response. Since the CSM is performed on a tilt table and it is followed by a tilt testing, atropine test is no longer needed because the vasodepressor response can already be revealed by tilt testing.
Figure 4.
The Six-Step-Method for carotid sinus massage. Carotid sinus massage should be performed in supine position on both left and right sides followed by both the left and right sides in upright position. For this, a tilt table is required to perform CSM in standing position (see also explanatory video as Supplementary file). This figure is also available as a poster provided as Supplementary material.
Here, we describe the Six-Step-Method according to the ‘methods of symptoms’ (Table 4, Figure 3, and Supplementary file).
Table 4.
Six-Step-Method for carotid sinus massage
| Steps | Action | Explanation |
|---|---|---|
| 1 | Check history for exclusion CSM | CSM is contra-indicated in case of TIA/stroke/myocardial infarction in the past 3 months, high-grade carotid stenosis. Auscultation should be performed in unresolved cases or high suspicion of carotid stenosis |
| 2 | Head turning | Turn head slightly contralaterally and posterior |
| 3 | Palpate to orientate | Palpation perpendicularly to the carotid artery to find the maximal pulse with the tips of the 2nd and 3rd fingers |
| 4 | Massage for 10 s | Massage (press) ‘firmly’ up and down longitudinally along the carotid artery |
| 5 | Monitor HR and blood pressure after the CSM | Monitor blood pressure and HR for assessing hypotensive components until these parameters return to baseline |
| 6 | Include time interval to another massage | Do not perform another carotid sinus massage or start CSM in the upright position after achieving CSM in supine position, until heart rate and blood pressure are restored to baseline levels or at least are stabilized (see also explanatory video as Supplementary material). |
TIA, transient ischaemic attack; HR, heart rate; CSM, carotid sinus massage.
The first step is to exclude any contraindication to CSM (Table 4 and Figure 3). It is a common sense to refrain from CSM in patients with a previous transient ischaemic attack/stroke in the last three months and/or confirmed high-grade carotid stenosis.35 To obtain this information, the medical history of patient is sufficient, effective, and easily available in most cases prior to performing CSM. However, in unresolved cases or when the clinical suspicion of carotid stenosis is high, carotid auscultation might be performed followed by optional carotid ultrasound if carotid bruits are present.26,36 Although it should be kept in mind that cerebral complications may occur in absence of a significant carotid stenosis. Indeed, as shown in Table 1, embolic complications occurred in most patients with normal carotid arteries. Probably, the best criterium for the proper selection of patients is an assessment of the risk/benefit ratio. In general, the benefit of performing CSM is greater in those patients who may benefit from a specific effective therapy derived by the diagnosis of CSS, such as pacemaker implantation in cardioinhibitory CSS. For the second step, the patient is asked to turn the head slightly contralaterally posteriorly for a gentle and careful palpation to search for and detect the location of the carotid sinus and where is the exact location of maximal pulsation. When the exact location of the maximal pulsation is confirmed, the CSM may be started (the second person applies the marker available on the monitor for exact labelling of the duration of CSM). We continue with step 3: the massage of the carotid sinus should be applied at the site of the maximum carotid pulse, located between the angle of the jaw and the cricoid cartilage on the anterior margin of the sternocleidomastoid muscle with the neck rotated contralaterally and posterior (step 3) and applied firmly and deeply using two fingers moving up and down along the carotid artery (step 4). Moving up and down during massage is important since the location of the carotid sinus may vary in its location due to anatomic variation.37 According to the ESC guidelines instructions,6 the CSM should be performed for 10 s to allow symptoms to develop and the vasodepressor component to become evident.3,38 Additionally, just before commencing CSM, make sure that the marker is running; this will allow measurement of the RR interval prior to CSM. After the massage is terminated, the HR and blood pressure should be monitored until the haemodynamic parameters have been restored to the baseline level. Usually, this is within 30 s, but the observation may be prolonged in the severe vasodepressor forms (step 5). This longer monitoring period is important to detect the magnitude of the vasodepressor component of the carotid sinus reflex, which occurs later than the cardioinhibitory component and may have important implication for the therapy. Make sure the period of the actual massage is properly marked/indicated. The next CSM should not be performed until heart rate and blood pressure are restored or stabilized at baseline levels (step 6). Record if the patient experiences either a presyncopal or syncopal episode. Ascertain if these symptoms were the same as the spontaneous symptoms (is there recognition?).
Limitations
Carotid sinus massage may be a fatigable reflex such that the order in which is carried out (right-left, supine-upright) may impact outcome. Little is known in the literature at the regard. The merit of this study is that we have standardized the sequence of execution. The impact of the sequence of execution on the results of CSM is outside the scope of this study and should be the aim of another study.
Practical implications
Here, we propose the Six-Step-Method for CSM that can be applied easily and safely in syncope units as part of the short cardiovascular autonomic function assessment.23 When performed during such comprehensive autonomic assessment in appropriate patients in the setting of a specialized syncope unit, the diagnostic yield of CSM is as high as 25% (of which 20% are asystolic forms).23
Conclusions
The Six-Step-Method for CSM is a safe procedure and should be performed, after the initial work-up, in every patient above 40 years, with unexplained syncope that is compatible with a reflex mechanism.
Supplementary Material
Acknowledgements
The authors thank Erik Altena, Jordi Derks, and Max Stokvis for their contribution and help with this manuscript.
Contributor Information
Frederik J de Lange, Department of Clinical and Experimental Cardiology, Amsterdam UMC, University of Amsterdam, Heart Centre, Amsterdam Cardiovascular Sciences, Meibergdreef 9, 1105 AZ, The Netherlands.
Jelle S Y de Jong, Department of Clinical and Experimental Cardiology, Amsterdam UMC, University of Amsterdam, Heart Centre, Amsterdam Cardiovascular Sciences, Meibergdreef 9, 1105 AZ, The Netherlands.
Steven van Zanten, Department of Cardiology, Reinier de Graaf Gasthuis, Delft, The Netherlands.
Willem P M E Hofland, Department of Clinical and Experimental Cardiology, Amsterdam UMC, University of Amsterdam, Heart Centre, Amsterdam Cardiovascular Sciences, Meibergdreef 9, 1105 AZ, The Netherlands.
Rick Tabak, Department of Clinical and Experimental Cardiology, Amsterdam UMC, University of Amsterdam, Heart Centre, Amsterdam Cardiovascular Sciences, Meibergdreef 9, 1105 AZ, The Netherlands.
Marianne Cammenga, Department of Clinical and Experimental Cardiology, Amsterdam UMC, University of Amsterdam, Heart Centre, Amsterdam Cardiovascular Sciences, Meibergdreef 9, 1105 AZ, The Netherlands.
Jaume Francisco-Pascual, Unitat d’Arritmies, Servei de Cardiologia, Hospital Universitari Vall Hebrón i Vall d’Hebron Research Institut, Universitat Autònoma de Barcelona, CIBER-CV, Barcelona, Spain.
Vincenzo Russo, Department of Translational Medical Sciences, Cardiology Unit, University of Campania ‘Luigi Vanvitelli’, Monaldi Hospital, Naples, Italy.
Artur Fedorowski, Department of Cardiology, Karolinska University Hospital, Stockholm, Sweden; Department of Medicine, Karolinska Institute, Stockholm, Sweden.
Jean-Claude Deharo, Assistance Publique—Hôpitaux de Marseille, Centre Hospitalier Universitaire La Timone, Service de Cardiologie, France and Aix Marseille Université, C2VN, 13005 Marseille, France.
Michele Brignole, Department of Cardiology, IRCCS Istituto Auxologico Italiano, Faint & Fall Research Centre, San Luca Hospital, Milan, Italy.
Supplementary material
Supplementary material is available at Europace online.
Funding
No funding declared.
Data availability
The data underlying this article are available in the article and in its online Supplementary material.
References
- 1. Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli Aet al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J 2018;39:1883–948. [DOI] [PubMed] [Google Scholar]
- 2. Kerr SR, Pearce MS, Brayne C, Davis RJ, Kenny RA. Carotid sinus hypersensitivity in asymptomatic older persons: implications for diagnosis of syncope and falls. Arch Intern Med 2006;166:515–20. [DOI] [PubMed] [Google Scholar]
- 3. Puggioni E, Guiducci V, Brignole M, Menozzi C, Oddone D, Donateo Pet al. Results and complications of the carotid sinus massage performed according to the “method of symptoms”. Am J Cardiol 2002;89:599–601. [DOI] [PubMed] [Google Scholar]
- 4. Torabi P, Rivasi G, Hamrefors V, Ungar A, Sutton R, Brignole Met al. Early and late-onset syncope: insight into mechanisms. Eur Heart J 2022;43:2116–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brignole M, Gigli G, Altomonte F, Barra M, Sartore B, Prato Ret al. Il riflesso cardioinibitore provocato dalla stimolazione del seno carotideo nei soggetti normali e con malattie cardiovascolari [Cardioinhibitory reflex provoked by stimulation of carotid sinus in normal subjects and those with cardiovascular disease]. G Ital Cardiol 1985;15:514–9. [PubMed] [Google Scholar]
- 6. Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli Aet al. Practical instructions for the 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J 2018;39:e43–80. [DOI] [PubMed] [Google Scholar]
- 7. van Zanten S, Sutton R, Hamrefors V, Fedorowski A, de Lange FJ. Tilt table testing, methodology and practical insights for the clinic. Clin Physiol Funct Imaging 2024;44:119–30. [DOI] [PubMed] [Google Scholar]
- 8. Krediet CT, Parry SW, Jardine DL, Benditt DG, Brignole M, Wieling W. The history of diagnosing carotid sinus hypersensitivity: why are the current criteria too sensitive? Europace 2011;13:14–22. [DOI] [PubMed] [Google Scholar]
- 9. Wieling W, Krediet CT, Solari D, de Lange FJ, van Dijk N, Thijs RDet al. At the heart of the arterial baroreflex: a physiological basis for a new classification of carotid sinus hypersensitivity. J Intern Med 2013;273:345–58. [DOI] [PubMed] [Google Scholar]
- 10. Hatoum T, Sheldon RS. Syncope and the aging patient: navigating the challenges. Auton Neurosci 2022;237:102919. [DOI] [PubMed] [Google Scholar]
- 11. Ungar A, Rivasi G, Rafanelli M, Toffanello G, Mussi C, Ceccofiglio Aet al. Safety and tolerability of tilt testing and carotid sinus massage in the octogenarians. Age Ageing 2016;45:242–8. [DOI] [PubMed] [Google Scholar]
- 12. Collins NA, Higgins GL 3rd. Reconsidering the effectiveness and safety of carotid sinus massage as a therapeutic intervention in patients with supraventricular tachycardia. Am J Emerg Med 2015;33:807–9. [DOI] [PubMed] [Google Scholar]
- 13. Wu TC, Hachul DT, Darrieux FCDC, Scanavacca MI. Carotid sinus massage in syncope evaluation: a nonspecific and dubious diagnostic method. Arq Bras Cardiol 2018;111:84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brignole M, Disertori M, Menozzi C, Raviele A, Alboni P, Pitzalis MVet al. Management of syncope referred urgently to general hospitals with and without syncope units. Europace 2003;5:293–8. [DOI] [PubMed] [Google Scholar]
- 15. Brignole M, Malasana G, Sherwood RP, Daccarett M, Jetter TL, Hamdan MH. Evaluation of patients with “faint” in an American teaching hospital: a dire need for a standardized approach. Pacing Clin Electrophysiol 2011;34:284–90. [DOI] [PubMed] [Google Scholar]
- 16. Brignole M, Menozzi C, Bartoletti A, Giada F, Lagi A, Ungar Aet al. A new management of syncope: prospective systematic guideline-based evaluation of patients referred urgently to general hospitals. Eur Heart J 2006;27:76–82. [DOI] [PubMed] [Google Scholar]
- 17. Khera S, Kolte D, Iwai S, Palaniswamy C, Harikrishnan P, Gupta Tet al. Permanent pacemaker utilization in older patients with syncope and carotid sinus syndrome. Int J Cardiol 2014;176:1137–8. [DOI] [PubMed] [Google Scholar]
- 18. Fedorowski A, Kulakowski P, Brignole M, de Lange FJ, Kenny RA, Moya Aet al. Twenty-five years of research on syncope. Europace 2023;25:euad163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kulakowski P, Lelonek M, Krynski T, Bacior B, Kowalczyk J, Malkowska Bet al. Prospective evaluation of diagnostic work-up in syncope patients: results of the PL-US registry. Europace 2010;12:230–9. [DOI] [PubMed] [Google Scholar]
- 20. van Zanten S, de Jong JSY, Scheffer MG, Kaal ECA, de Groot JR, de Lange FJ. A cross-sectional nationwide survey of guideline based syncope units in The Netherlands: the SU-19 score—a novel validation for best practices. Europace 2023;26:euae002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Torabi P, Hamrefors V, Sutton R, Brignole M, Fedorowski A. Definitive aetiology of unexplained syncope after cardiovascular autonomic tests in a tertiary syncope unit. Europace 2023;25:euad247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brignole M, Kessisoglu F, Croci F, Solano A, Donateo P, Maggi Ret al. Complementary effectiveness of carotid sinus massage and tilt testing for the diagnosis of reflex syncope in patients older than 40 years: a cohort study. Europace 2020;22:1737–41. [DOI] [PubMed] [Google Scholar]
- 23. Groppelli A, Russo V, Parente E, Comune A, de Lange F, Rivasi G, et al. Detection of the mechanism of autonomic syncope by 24-hour ambulatory blood pressure monitoring and tilt-table short cardiovascular autonomic function assessment (submitted and under review for publication). 2024.
- 24. Pasquier M, Clair M, Pruvot E, Hugli O, Carron PN. Carotid sinus massage. N Engl J Med 2017;377:e21. [DOI] [PubMed] [Google Scholar]
- 25. Banyas P, Jadhav A. Stroke and transient ischemic attack. Prim Care 2024;51:283–97. [DOI] [PubMed] [Google Scholar]
- 26. Davies AJ, Kenny RA. Frequency of neurologic complications following carotid sinus massage. Am J Cardiol 1998;81:1256–7. [DOI] [PubMed] [Google Scholar]
- 27. Munro NC, McIntosh S, Lawson J, Morley CA, Sutton R, Kenny RA. Incidence of complications after carotid sinus massage in older patients with syncope. J Am Geriatr Soc 1994;42:1248–51. [DOI] [PubMed] [Google Scholar]
- 28. Richardson DA, Bexton R, Shaw FE, Steen N, Bond J, Kenny RA. Complications of carotid sinus massage—a prospective series of older patients. Age Ageing 2000;29:413–7. [DOI] [PubMed] [Google Scholar]
- 29. Sutton R, Fedorowski A, Olshansky B, Gert van Dijk J, Abe H, Brignole Met al. Tilt testing remains a valuable asset. Eur Heart J 2021;42:1654–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Thijs RD, Brignole M, Falup-Pecurariu C, Fanciulli A, Freeman R, Guaraldi Pet al. Recommendations for tilt table testing and other provocative cardiovascular autonomic tests in conditions that may cause transient loss of consciousness: consensus statement of the European Federation of Autonomic Societies (EFAS) endorsed by the American Autonomic Society (AAS) and the European Academy of Neurology (EAN). Clin Auton Res 2021;31:369–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. de Lange FJ, Hofland WPME, Ferrara A, Gargaro A, Brignole M, van Dijk JG. A novel and practical method to add video monitoring to tilt table testing. Europace 2023;25:762–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Brignole M, Rivasi G, Fedorowski A. Mechanism-based therapy of non-cardiac syncope: a practical guide. Europace 2024;26:euae073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. de Jong JSY, Blok MRS, Thijs RD, Harms MPM, Hemels MEW, de Groot JRet al. Diagnostic yield and accuracy in a tertiary referral syncope unit validating the ESC guideline on syncope: a prospective cohort study. Europace 2021;23:797–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Russo V, Parente E, Tomaino M, Comune A, Sabatini A, Laezza Net al. Short-duration head-up tilt test potentiated with sublingual nitroglycerin in suspected vasovagal syncope: the fast Italian protocol. Eur Heart J 2023;44:2473–9. [DOI] [PubMed] [Google Scholar]
- 35. O'Shea D, Parry SW, Kenny RA. The Newcastle protocol for carotid sinus massage. J Am Geriatr Soc 2001;49:236–7. [DOI] [PubMed] [Google Scholar]
- 36. Magyar MT, Nam EM, Csiba L, Ritter MA, Ringelstein EB, Droste DW. Carotid artery auscultation—anachronism or useful screening procedure? Neurol Res 2002;24:705–8. [DOI] [PubMed] [Google Scholar]
- 37. Ha SM, Cho YS, Cho GC, Jo CH, Ryu JY. Modified carotid sinus massage using an ultrasonography for maximizing vagal tone: a crossover simulation study. Am J Emerg Med 2015;33:963–5. [DOI] [PubMed] [Google Scholar]
- 38. Almquist A, Gornick C, Benson W Jr, Dunnigan A, Benditt DG. Carotid sinus hypersensitivity: evaluation of the vasodepressor component. Circulation 1985;71:927–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online Supplementary material.