Introduction
Vagally-mediated atrio-ventricular block (VAVB) is defined as paroxysmal or persistent functional second- or third-degree AVB induced by a marked activation of the parasympathetic tone of a vagal nerve, regulating its function (extrinsic) [1–5].
VAVB is one of three types of paroxysmal AVBs recognized by current literature, and it should be differentiated based on atropine challenge test and EPS from intrinsic paroxysmal AVB (due to intrinsic disease of the AV conduction system) and extrinsic idiopathic paroxysmal AVB (associated with low levels of endogenous adenosine) [1–4]. Proper diagnosis of VAVB may often be overlooked or missed owing to its unfamiliarity, unpredictability, and in some cases, a lack of clear evidence of atrioventricular conduction disease during normal 1:1 conduction [5]. Moreover, complex etiologies may coexist in a single patient; therefore, the other two forms of AVB and other substrates of vagal incompetence should always be investigated in the diagnostic process.
VAVB characterized by a sudden increase in parasympathetic tone causes transient, unpredictable, usually non-specific symptoms (palpitations, fatigue, lassitude, inability to concentrate, forgetfulness, irritability, dizziness, presyncope, syncope) impairing quality of life and/or permanent AVB with severe debilitating refractory symptoms requiring permanent cardiac pacing.
Implantation of a pacemaker (PM) constitutes an ultimate treatment of AVB according to 2021 ESC guidelines on cardiac pacing [6]; however, cardioneuroablation (CNA), a technique introduced by JC Pachon two decades ago, has emerged as an alternative treatment for management of patients with excessive vagal activation and VAVB [7, 8]. The detailed management strategies for VAVB have not yet been established, implemented, and validated in randomized clinical trials (RCT); however, prior case series, one single-center cohort study, and a recently published large multicenter retrospective international registry demonstrated the potential therapeutic role of CNA in the treatment of VAVB [9–16].
CNA based on endocardial radiofrequency catheter ablation of parasympathetic ganglionated plexi (GPs) located in the atria and septum induces neuromodulation of sino-atrial node (SAN) and/or atrio-ventricular node (AVN), correcting hypervagotonia, offering etiologic treatment of vagally mediated bradyarrhythmias [7–12]. Although CNA is already described in the literature as a promising alternative treatment for permanent pacing in extrinsic VAVB, it is still considered an experimental method without ESC recommendations, mainly due to the lack of randomized clinical trials (RCT) [1, 6–13, 16–18].
The purpose of this study is a head-to-head assessment of two methods of VAVB treatment: elective pacemaker implantation and CNA guided by electrophysiological study (EPS) and extracardiac vagal nerve stimulation (ECVS). This is the first attempt in the literature to evaluate the feasibility, efficacy, and safety of CNA in VAVB in a controlled trial, which may contribute to the future evaluation of this method in the guidelines and implementation of management strategies for patients with presumed VAVB.
Methods
Study design
The TELE-SPACER Trial and Registry is a randomized, controlled, prospective, multicenter, noncommercial, proof-of-concept, unblinded clinical trial and registry, designed to compare head-to-head two methods of treatment of VAVB: standard, guideline-recommended cardiac pacing and a novel method — CNA, guided by electrophysiological study (EPS) and extracardiac vagal nerve stimulation (ECVS).
The study is registered at clinicaltrials.gov [https://www.clinicaltrials.gov/], identifier NCT05774262, and is independently managed by Scientia Research Institute, Bydgoszcz, Poland and the Steering and Scientific Committee. The trial is currently recruiting. Enrollment began on January 1, 2024.
The TELE-SPACER study will enroll a minimum of 100 participants in the trial and up to 200 participants in the registry with indications for elective PM implantation due to AVB according to 2021 ESC guidelines on cardiac pacing and positive atropine tests in sinus rhythm as confirmation of increased vagal tone.
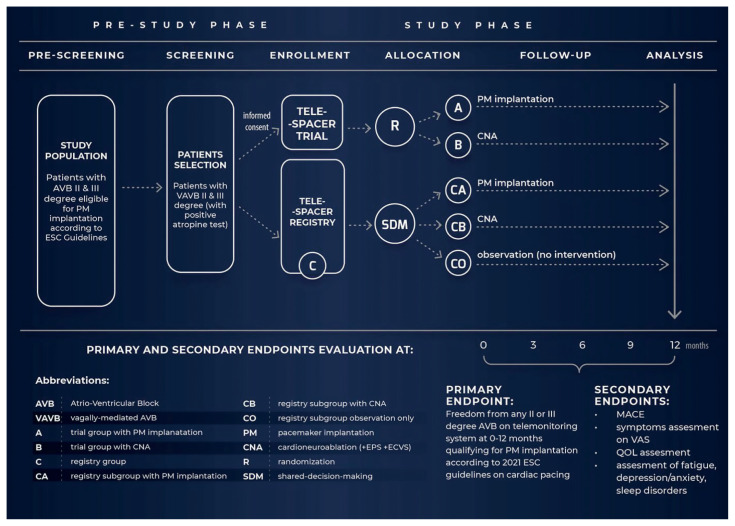
Participants in the trial will be randomized into 2 groups: either PM therapy (group A, n = 50) or CNA (group B, n = 50). Participants who choose to opt out of randomization will be included in the registry (group C) and will be offered patient-tailored intervention through shared decision-making (SDM), either PM implantation (CA) or CNA (CB) or observation only (CO). The study design is presented in Figure 1.
Figure 1.
Study design of the TELE-SPACER trial and registry, MACE — major adverse cardiac events; QOL — quality of life; VAS — visual analog scale
Recruitment will take place in two distinct phases (pre-screening and screening). In pre-screening the local investigator will analyze medical records for eligibility to identify potential participants with AVB and positive atropine test. In the screening phase eligible participants will be invited for consultation to discuss, explore, and compare possible treatment options and participation in the study. The investigator will depict the study protocol, including potential risks and benefits. The patient will be offered a copy of the consent form to take home to consider participation. Participants will have a choice to sign the informed consent to participate in the trial or to opt out of randomization to take part in the registry (group C). Only participants who truly understand the protocol of the study and voluntarily sign written informed consent will be included. Participants will be able to withdraw from the study at any time without compromising their medical care.
Randomization will be performed centrally and assigned to each patient via an automated system using allocation concealment technique 1:1 to either intervention group A or B, until the moment of assignment. The randomization list will be blocked per center with randomly varying block sizes of 2 and 4. The treatment allocation will not be blinded to the patient or follow-up physician. Participants in either arm of the study will be followed-up on a regular basis for 12 months. During the 12-month study duration, the use of effective contraception will be recommended for women of child-bearing age.
Parameter analysis baseline, including ECG telemonitoring, QOL, and symptoms, will take place at 0, 3, 6, and 12 months. All measured parameters, as well as demographic and clinical data, will be recorded in the study database.
Study population
The TELE-SPACER study will enroll approximately 300 participants (a minimum of 100 participants in the trial and up to 200 in the registry) 18–75 years old, males and females, with second- or third-degree AVB with positive atropine test, meeting the criteria for PM implantation according to 2021 ESC guidelines on cardiac pacing. Inclusion and exclusion criteria are summarized in Table 1. The recruitment will take place at 9 sites in Poland by medical referral. Patient enrollment is anticipated to last 2–3 years. The population of elderly patients > 75 years old, frequently with concomitant heart disease, is excluded because the demonstration of a clear cause–effect relationship between symptoms and AV block will be difficult to achieve.
Table 1.
Inclusion and exclusion criteria in the TELE-SPACER trial and registry
| Inclusion criteria |
| Written informed consent to participate in the study Age 18–75 years At least one indication of the European Society of Cardiology (ESC) for elective pacemaker implantation due to isolated (without SND and BBB) paroxysmal, persistent or reflex AVB:
|
| Exclusion criteria |
| SND with indication for PM implantation Severe, prolonged bradycardia in advanced AVB requiring temporary cardiac pacing Persistent RBBB or LBBB Advanced ventricular arrhythmia with indication for ICD implantation in primary or secondary prevention of SCD Recent catheter ablation of cardiac arrhythmias < 3 months Planned ablation of the AV junction Implanted PM/ICD/CRT Uncontrolled hypertension ESC 3 (BP ≥ 180/110 mmHg) Diabetes mellitus type 1 or 2 CKD — moderate to severe (eGFR < 60 mL/min/1.73 m2) Familial hypercholesterolemia (cholesterol > 8 mmol/L (> 310 mg/dL) High 10-year cardiovascular risk on SCORE2 for patients 40–69 years of age and on SCORE2-OP for patients 70–89 years of age Documented ASCV:
Cardiomyopathies with indication for ICD implantation for primary or secondary prevention of SCD Previous cardiac surgery or percutaneous valve intervention Decompensated chronic diseases (endocrine, metabolic, electrolyte disorders, etc.) Musculoskeletal disorders with indication for PM implantation Acute infection or any other concomitant disease that is considered a contraindication for percutaneous procedures and/or PM implantation Pregnancy, breastfeeding, or planned pregnancy within 12 months The presence of a mental illness or limitation of cognitive functions that prevent independent participation in the study, including the use of telemedicine services Contraindications to the procedures used in the study Any identified abnormality that is considered by the investigator a contraindication to participation in the study due to data interpretation or safety issues |
Interventions
After enrollment, all participants in the trial and registry (group A, B, and C) will receive a dedicated telemonitoring kit consisting of a portable ECG device (Kardia 6L, AliveCor, USA) and a tablet with network connection enabling regular self-testing and symptom monitoring to document AVB and clinically important arrhythmias. Participants will be monitored 24/7 by a telemonitoring center specialized in cardiac arrhythmias and implantable device monitoring. In case of severe AVB or life-threatening arrhythmias, the emergency system will be called.
Participants in group A (PM, n = 50) will be implanted with a PM (DDD pacemaker or its modification as HBP/LBBAP - His-Purkinje or left bundle branch area pacing).
Participants in group B (CNA, n = 50) will be referred for EPS and simultaneous CNA after exclusion of advanced distal AV blocks. This group will be additionally implanted after randomization with an ICM (Insertable Cardiac Monitor) device (Confirm Rx™ Model DM3500, Abbott) paired with a MerlinNet remote monitoring system (Abbott), capable of rapid remote review of electrocardiograms by the medical team of a 24/7 telemonitoring center. Data will be transmitted per schedule, patient-triggered, and automatically in case of alert events set by the clinic, with the same thresholds for automatic episode recording.
CNA will be performed under general anesthesia by experienced operators (at least 50 CNA procedures performed). After EPS biatrial, binodal, anatomically guided CNA will be performed under ECVS guidance (vagal hyperactivity demonstration at the onset of the CNA with asystole or AVB on atrial pacing and its complete disappearance after a successful CNA). Additional ablation substrates will also be allowed and performed.
If the effectiveness of the CNA is not immediately confirmed during the procedure by ECVS, the patient will be further monitored with ICM and a Kardia 6L system, and the second CNA will be scheduled within 2 months. If the second CNA is not successful and/or its immediate effectiveness is not confirmed (meeting the ESC criteria for PM implantation after CNA), the patient will be referred for PM implantation crossing over into group A.
All participants (group A, B, and C) will be assessed with innovative remote cardiovascular autonomic testing (CAT) at 0, 3, and 12 months with video-conference tools, ECG monitoring devices (Pocket ECG, Medicalgorythmics, Poland), and the supervision of medical staff to document variability of the autonomic nervous system subjected to standard stress stimuli in patient home environment.
All participants (group A, B, and C) will be asked to complete questionnaires on health-related quality of life (QOL) (EQ-5D-5L), AVB symptoms based on VAS (Visual Analog Scale), Fatigue Assessment Scale (FAS), Modified Hospital Anxiety and Depression Scale (HADS-M), and Sleep Quality Scale (SQS) at 0, 6, and 12 months.
Participants included in the registry (group C) will undergo an individually tailored intervention through SDM with the option of implantation of PM (subgroup CA), CNA (subgroup CB), or observation only (subgroup CO).
The safety of the interventions will be assessed immediately after the procedure and monthly with monitoring of major adverse cardiovascular events (MACE) by the Central Investigation Safety Committee. All outcome events will be adjudicated by the Central Adjudication Committee, which does not include members of the Scientific and Steering Committee.
Endpoints
Primary endpoint
Freedom from any second- or third-degree AVB on a telemonitoring system at 0–12 months qualifying for PM implantation according to 2021 ESC guidelines on cardiac pacing.
Secondary endpoints
Occurrence of MACE, defined as: death, non-fatal stroke, non-fatal myocardial infarction, or thromboembolic events at 0, 3, 6, 12 months. Occurrence of other peri-procedural and long-term complications such as: hemopericardium/tamponade, damage to SAN or AVN, pericarditis, esophageal damage, or major vascular complications requiring surgical intervention (large vein stenosis, hemorrhage, hematoma, fistula, pseudoaneurysm) at 0, 3, 6, and 12 months.
Assessment of time-to-event of the first recurrence of any second- or third-degree AVB on a telemonitoring system at 0–12 months.
Assessment of the effect of CNA and PM implantation on AVB symptoms using a VAS (visual analog scale), which indicates the general health status, with 100 indicating the best health and 0 indicating the worst health status (time frame: 0, 6, 12 months).
Assessment of the effect of CNA and PM implantation on health-related quality of life (QOL) using the EQ-5D-5L questionnaire, which comprises 5 dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is scored on a scale of 1–5 points, which describes the patient’s health state. The maximum score of 1 indicates the best health state, while higher scores indicate more severe or frequent problems (time frame: 0, 6, 12 months).
Assessment of the effect of CNA and PM implantation on fatigue using the Fatigue Assessment Scale (FAS). The FAS is a 10-item scale evaluating chronic fatigue. Each item of the FAS is answered using a five-point Likert-type scale ranging from 1 (“never”) to 5 (“always”). Total scores can range from 10, indicating the lowest level of fatigue, to 50, denoting the highest (time frame: 0, 6, 12 months).
Assessment of the effect of CNA and PM implantation on depression/anxiety using the Modified Hospital Anxiety and Depression Scale (HADS-M), a validated, standardized 16-item questionnaire to evaluate the association between anxiety and depression and the degree of illness acceptance in patients. Total scores range from 0 to 64. Higher scores indicate a greater degree of anxiety or depression (time frame: 0, 6, 12 months).
Assessment of the effect of CNA and PM implantation on sleep disorders using the Sleep Quality Scale (SQS) questionnaire, consisting of 28 items. The SQS evaluates 6 domains of sleep quality (daytime symptoms, restoration after sleep, problems initiating and maintaining sleep, difficulty waking, and sleep satisfaction). Using a four-point, Likert-type scale, respondents indicate how frequently they exhibit certain sleep behaviors (0 = “few,” 1 = “sometimes,” 2 = “often,” and 3 = “almost always”). Total scores can range from 0 to 84, with higher scores demonstrating more acute sleep problems (time frame: 0, 6, 12 months).
Statistical analysis
Statistical analysis will be performed by an independent statistician blinded to the allocation of patients. A per-protocol approach will be used. Statistical analysis will include objective and subjective parameters of the primary and secondary endpoints. For both types of endpoints descriptive (parametric and non-parametric) statistics will be used, tests of significant differences between groups at established time points (0, 6, and 12 months), and differences between parameters within a single group (A or B), measured by non-parametric tests. The difference between results will be considered statistically significant at p-value ≤ 0.05 with Bonferroni correction for multiple comparisons.
We expect a statistically significant difference between groups A and B in both objective and subjective endpoints, meaning the following:
— reduction in the number of patients requiring PM implantation in group B compared to group A (all patients with implanted PM);
— significant improvement of the symptoms and quality of life in group B measured by questionnaires.
The objective endpoint examining the onset of second- or third-degree AVB episodes after PM/CNA will be assessed at 0–12 months. It will specify the number of the episodes for group B. Occurrence of ≥ 1 episode of second- or third-degree AVB or the need for earlier (0–12 months) PM implantation will be an indicator of CNA failure in group B, assuming the presence of PM stimulation in group A at the level of 93–100%.
The effectiveness of CNA vs. PM will be considered statistically significant at the level of p < 0.01 in the absence of second- or third-degree AVB within 12 months after the CNA procedure in 33% of patients (12/30) - assuming 90% statistical power, with simultaneous assumption of 100% effectiveness of PM stimulation in group A. This result will mean a reduction in the need for PM implantation in 33% of responders.
Assuming the incidence of PM implantation at 0–12 months as 28/30 (93%) in group A and 18/30 (60%) in group B, and statistical power of 90%, the group size should be 29 patients per group to obtain a statistical level of 0.01. However, the number of patients in each group was increased to validate other endpoints. This translates into at least 33% reduction of the need for PM implantation.
Discussion
Although cardiac pacing is considered the pillar of cardiology practice to treat AVB, no studies to date have proven a benefit of prophylactic pacemaker implantation in patients with VAVB, defined as paroxysmal or permanent AVB with positive response to atropine test and exclusion of other intrinsic and extrinsic causes [1–6].
Furthermore, permanent cardiac pacing does not prevent recurrence of syncopal events in 12–25% of cases at two-year follow up [21–23]. The reason for this finding is most likely not a homogeneous population with a minority with extrinsic VAVB included in the studies on cardiac pacing or other causes of syncope, never diagnosed before.
On the other hand, we already have evidence based on case reports, small observational studies, and the large registry PIRECNA, discussed in the EHRA/HRS scientific statement on cardioneuroablation, demonstrating that CNA inducing neuromodulation of SAN and/or AVN offers an etiologic, selective treatment of VAVB and seems a very promising therapeutic modality [8–13, 16, 18, 19–20]. However, the studies, especially the multicenter registry PIRECNA, cause interpretative difficulties due to the heterogeneity of the groups with AVB overlapping with VVS and SND and the selection of age groups (usually younger and middle-aged population), discrepancies between the inclusion criteria, and qualitative follow-up, causing the risk of widespread use of this method in patients with undefined AVB etiology and non-specific symptoms [17].
These observations have led to the design of RCT that compares head-to-head CNA to PM implantation in VAVB in a homogeneous population with well-defined etiology and symptoms to verify the feasibility, efficacy, and safety of CNA.
TELE-SPACER is the first study that uses continuous telemedical ECG-monitoring and innovative remote CAT to assure qualitative follow-up for 12 months. To evaluate the quality of life, the study design includes indicators of subjective symptoms and QOL in VAVB patients before and after PM/CNA, as essential metrics measuring the patient’s clinical status and outcome to prove clear cause-effect correlation between symptoms and treatment effectiveness.
In summary, the TELE-SPACER control trial represents much awaited research, first RCT in patients with VAVB, in whom CNA may become a viable alternative to PM implantation, shifting paradigms in electrocardiology, provided that the study will demonstrate at least non-inferiority of CNA in these individuals.
Limitation of the study
Due to the limited budget, the researchers were unable to extend the study up to 3 years, although we take under consideration the possibility of late recurrence of AVB due to vagal reinnervation.
Due to the limited budget of the study, only the patients in group B (CNA) will be monitored with ICM. However, we offer 24/7 tele-monitoring for all patients.
Owing to differences in techniques and methodology of PM implantation and CNA we are unable to blind the study.
The researchers would like to have more answers from genetic testing and micro-biopsies, but owing to limited resources it was not possible to implement them in this study, nor precise mapping and imaging of the interventricular septum in MRI.
Acknowledgements
The authors thank Przemysław Magielski, MD (Scientia Research Institute) for extraordinary efforts of CRO; Sara Goj (American Heart of Poland S.A.) for administrative management; and Marzena Krawiec and Mikołaj Basza, MD (Telemedycyna Polska S.A.) for the support in the development of the project.
Footnotes
Ethics statement: The TELE-SPACER study protocol was approved by the independent Ethics Committee of Institutional Board Review of Medical Chamber in Bielsko-Biała, Poland, KBE 2022/9/29/1. The study conforms with the principles outlined in the 1964 Declaration of Helsinki and its later amendments. All participants, after explicit information from the investigator, will voluntarily sign the informed written consent. All participants will be able to withdraw from the study at any time without compromising their medical care.
Author’s contribution: The study concept and protocol were developed by Sebastian Stec, MD, PhD (Primary Investigator) and Edyta Stodółkiewicz-Nowarska, MD, PhD (Primary Co-Investigator). The article was drafted by ESN. All authors, exclusively members of the Steering and Scientific Committee, critically reviewed and approved the final manuscript.
Conflict of interests: S.S. is the author of several patents and a shareholder of Medicine S.A. No specific product of any company will be used in this trial.
Clinical trial registration: URL: https://www.clinicaltrials.gov; NCT05774262.
Funding: The study is funded by grant 2022/ABM/03/00035 awarded to American Heart of Poland S.A. by ABM (Agencja Badań Medycznych, Poland).
Data availability
The data that support the findings of this study will be available upon reasonable request from the corresponding author with permission of the Steering Committee and American Heart of Poland S.A.
References
- 1.Brignole M, Moya A, de Lange FJ, et al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J. 2018;39(21):1883–1948. doi: 10.1093/eurheartj/ehy037. [DOI] [PubMed] [Google Scholar]
- 2.Alboni P, Holz A, Brignole M. Vagally mediated atrioventricular block: pathophysiology and diagnosis. Heart. 2013;99(13):904–908. doi: 10.1136/heartjnl-2012-303220. [DOI] [PubMed] [Google Scholar]
- 3.Aste M, Brignole M. Syncope and paroxysmal atrioventricular block. Journal of Arrhythmia. 2017;33(6):562–567. doi: 10.1016/j.joa.2017.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brignole M, Deharo JC, Guieu R. Syncope and idiopathic (Paroxysmal) AV block. Cardiol Clin. 2015;33(3):441–447. doi: 10.1016/j.ccl.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Lee S, Wellens HJJ, Josephson ME. Paroxysmal atrioventricular block. Heart Rhythm. 2009;6(8):1229–1234. doi: 10.1016/j.hrthm.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Glikson M, Nielsen JC, Kronborg MB, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. EP. 2022;24:71–164. doi: 10.1093/europace/euab232. [DOI] [PubMed] [Google Scholar]
- 7.Pachon JC, Pachon EI, Pachon JC, et al. “Cardioneuroablation”--new treatment for neurocardiogenic syncope, functional AV block and sinus dysfunction using catheter RF-ablation. Europace. 2005;7(1):1–13. doi: 10.1016/j.eupc.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Pachon-M JC, Ortencio FA, Pachon-M EI, et al. Treatment of symptomatic functional atrioventricular block by cardioneuroablation as an alternative to Pacemaker implantation. JACC Case Rep. 2022;4(15):990–995. doi: 10.1016/j.jaccas.2022.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aksu T, Golcuk E, Yalin K, et al. Simplified cardioneuroablation in the treatment of reflex syncope, Functional AV Block, and sinus node dysfunction. Pacing Clin Electrophysiol. 2016;39(1):42–53. doi: 10.1111/pace.12756. [DOI] [PubMed] [Google Scholar]
- 10.Aksu T, Gopinathannair R, Bozyel S, et al. Cardioneuroablation for treatment of atrioventricular block. Circulation: Arrhythmia and electrophysiology. 2021;14(9):e010018. doi: 10.1161/circep.121.010018. [DOI] [PubMed] [Google Scholar]
- 11.Wileczek A, Polewczyk A, Kluk M, et al. Ultrasound-guided imaging for vagus nerve stimulation to facilitate cardioneuroablation for the treatment of functional advanced atrioventricular block. Indian Pacing Electrophysiol J. 2021;21(6):403–406. doi: 10.1016/j.ipej.2021.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoneda F, Shizuta S, Makiyama T, et al. Selective cardioneuroablation of the posteromedial left ganglionated plexus for drug-resistant swallow syncope with functional atrioventricular block. HeartRhythm Case Rep. 2023;9(8):513–517. doi: 10.1016/j.hrcr.2023.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi NH, Hong J, Moak JP. Cardioneuroablation for pediatric patients with functional sinus node dysfunction and paroxysmal atrioventricular block. J Cardiovasc Electrophysiol. 2024;35(2):221–229. doi: 10.1111/jce.16145. [DOI] [PubMed] [Google Scholar]
- 14.Donateo P. A standardized conventional evaluation of the mechanism of syncope in patients with bundle branch block. Europace. 2002;4(4):357–360. doi: 10.1053/eupc.2002.0265. [DOI] [PubMed] [Google Scholar]
- 15.Baysal E, Guler T, Gopinathannair R, et al. Catheter ablation of atrioventricular block. JACC: Case Reports. 2020;2(11):1793–1801. doi: 10.1016/j.jaccas.2020.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aksu T, Piotrowski R, Tung R, et al. Procedural and Intermediate-term results of the electroanatomical-guided cardioneuroablation for the treatment of supra-hisian Second- or Advanced-degree Atrioventricular Block: the PIRECNA multicentre registry. Europace. 2024;26(7) doi: 10.1093/europace/euae164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deharo JC, Fedorowski A, Brignole M. Cardioneuroablation for treatment of atrioventricular block: to cure the patient or the electrocardiogram? Europace. 2024;26(7) doi: 10.1093/europace/euae156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aksu T, Brignole M, Calo L, et al. Cardioneuroablation for the treatment of reflex syncope and functional bradyarrhythmias: A scientific statement of the European Heart Rhythm Association (EHRA) of the ESC, the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Society (APHRS) and the Latin American Heart Rhythm Society (LAHRS) Europace. 2024;26(8) doi: 10.1093/europace/euae206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stec S, Wileczek A, Reichert A, et al. Shared decision making and cardioneuroablation allow discontinuation of permanent pacing in patients with vagally mediated bradycardia. J Cardiovasc Dev Dis. 2023;10(9) doi: 10.3390/jcdd10090392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stec S, Jankowska-Polańska B, Jagielski D, et al. Rationale and design of SAN.OK randomized clinical trial and registry: Comparison of the effects of evidence-based pacemaker therapy and cardioneuroablation in sinus node dysfunction. Cardiol J. 2022;29(6):1031–1036. doi: 10.5603/CJ.a2022.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brignole M, Ammirati F, Arabia F, et al. Syncope Unit Project (SUP) Two Investigators. Assessment of a standardized algorithm for cardiac pacing in older patients affected by severe unpredictable reflex syncopes. Eur Heart J. 2015;36(24):1529–1535. doi: 10.1093/eurheartj/ehv069. [DOI] [PubMed] [Google Scholar]
- 22.Brignole M, Donateo P, Tomaino M, et al. International Study on Syncope of Uncertain Etiology 3 (ISSUE-3) Investigators. Benefit of pacemaker therapy in patients with presumed neurally mediated syncope and documented asystole is greater when tilt test is negative: an analysis from the third International Study on Syncope of Uncertain Etiology (ISSUE-3) Circ Arrhythm Electrophysiol. 2014;7(1):10–16. doi: 10.1161/CIRCEP.113.001103. [DOI] [PubMed] [Google Scholar]
- 23.Yasa E, Ricci F, Holm H, et al. Pacing therapy in the management of unexplained syncope: a tertiary care centre prospective study. Open Heart. 2019;6(1):e001015. doi: 10.1136/openhrt-2019-001015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kulakowski P, Baran J, Sikorska A, et al. Cardioneuroablation for reflex asystolic syncope: Mid-term safety, efficacy, and patient’s acceptance. Heart Rhythm. 2024;21(3):282–291. doi: 10.1016/j.hrthm.2023.11.022. [DOI] [PubMed] [Google Scholar]
- 25.Piotrowski R, Baran J, Sikorska A, et al. Cardioneuroablation for Reflex Syncope. JACC: Clinical Electrophysiology. 2023;9(1):85–95. doi: 10.1016/j.jacep.2022.08.011. [DOI] [PubMed] [Google Scholar]
- 26.Wichterle D, Jansova H, Stiavnicky P, et al. Cardioneuroablation focused on the atrioventricular node: a comparison of right and left atrial approach. European Heart Journal. 2022;43(Supplement_2) doi: 10.1093/eurheartj/ehac544.656. [DOI] [Google Scholar]
- 27.Kulakowski P, Baran J, Sikorska A, et al. Cardioneuroablation for reflex asystolic syncope: Mid-term safety, efficacy, and patient’s acceptance. Heart Rhythm. 2024;21(3):282–291. doi: 10.1016/j.hrthm.2023.11.022. [DOI] [PubMed] [Google Scholar]
- 28.Sutton R, Fedorowski A, Olshansky B, et al. Tilt testing remains a valuable asset. Eur Heart J. 2021;42(17):1654–1660. doi: 10.1093/eurheartj/ehab084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aksu T, Guler TE, Bozyel S, et al. Usefulness of post-procedural heart rate response to predict syncope recurrence or positive head up tilt table testing after cardioneuroablation. Europace. 2020;22(9):1320–1327. doi: 10.1093/europace/euaa230. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study will be available upon reasonable request from the corresponding author with permission of the Steering Committee and American Heart of Poland S.A.