Abstract
Background
Risk factors for alcohol withdrawal delirium include heavy drinking, prior alcohol withdrawal delirium or convulsions, nondrug sedative use, and a history of tachycardia, withdrawal, and infections.
Case Presentation
A 76‐year‐old man with a history of heavy drinking and type 2 diabetes was hospitalized for hypothermia, rhabdomyolysis, and acute renal failure after a typhoon. He developed alcohol withdrawal symptoms 24 h after his last drink, leading to severe withdrawal delirium characterized by restlessness, delusions, and altered consciousness. Treatment included lorazepam, in addition to comprehensive care for his physical condition. His condition fluctuated, especially at night, with his psychiatric symptoms exacerbated by his physical illnesses, suggesting delirium due to the coexistence of severe and multiple physical illnesses. After 44 days, following substantial improvements in both mental and physical health with perospirone, the patient was discharged.
Conclusion
This case emphasizes the need for multidisciplinary collaboration in the treatment of such patients, especially during disasters, and the importance of long‐term monitoring for elderly patients with alcohol dependence syndrome after a disaster.
Keywords: alcohol withdrawal delirium, delirium due to physical illnesses, disaster
A 76‐year‐old heavy drinker with type 2 diabetes developed severe alcohol withdrawal delirium after being hospitalized for conditions caused by a typhoon, necessitating treatment with lorazepam and comprehensive care. This case highlights the importance of multidisciplinary treatment and long‐term monitoring for elderly patients with alcohol dependence, particularly after disasters.
1. INTRODUCTION
Alcohol withdrawal delirium consists of a variety of symptoms and signs that occur in alcohol‐dependent individuals within 24–48 h after their last drink. According to Western data, the incidence of alcohol withdrawal delirium is 15%, and the incidence of withdrawal convulsions is 3%–15%. 1 Alcohol withdrawal delirium is characterized by a decreased level of consciousness, disorientation, recent memory impairment, disruption of the sleep–wake cycle, transient perceptual disturbances (visual, auditory, tactile, and olfactory disturbances), worsening of symptoms in the evening, varying agitation, and coarse tremors of the limbs and body. Suggested risk factors for alcohol withdrawal delirium include recent heavy drinking, a history of past alcohol withdrawal delirium or withdrawal convulsions, the use of nondrug sedatives/hypnotics, a history of tachycardia (heart rate > 120 beats/min), frequent withdrawal episodes or medical problems, and current infection. 2 , 3
Moreover, there are no reports of alcohol withdrawal delirium due to forced sobriety following a disaster. Therefore, we report a case in which alcohol withdrawal delirium and delirium due to physical illness occurred consecutively in a patient brought to the emergency department after a disaster. Written consent for this case report was obtained from the patient's family.
2. CASE
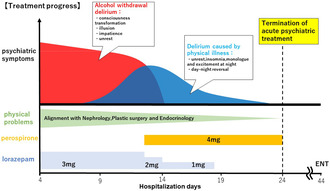
A 76‐year‐old man with hypothermia, rhabdomyolysis, acute renal failure, and acne on the back of his left leg was admitted to the emergency room. He had worked as a metal worker since he graduated from junior high school and had his first drink at 18 years old. When he was 25 years old, he married and had two children; after his wife passed away when he was in his 50s, he consumed more than one bottle of sake (200 g pure alcohol) per day (for the past 10 years). He constantly argued with his siblings and children due to problems caused by drinking while working, driving under the influence of alcohol, and drinking in general, and their relationships had become strained. He had no history of alcohol withdrawal delirium, but he had experienced withdrawal symptoms such as hand tremors and sweating on several occasions when he was unable to drink. He had type 2 diabetes mellitus. The day before a large typhoon damaged his house, he had been drinking in the morning and was intoxicated in his living room at night. When the river near his home overflowed and flooded his house before dawn the next day, he awoke and attempted to evacuate, but the tatami fell out, and his left leg was stuck in the water. He became unable to move and lost consciousness. He was found by a neighbor later that morning and was transported to our hospital by a medical helicopter. At the time of transport, his vital signs were as follows: blood pressure (BP): 168/112 mmHg, pulse (P): 94 beats/min, body temperature (BT): 26.9°C, and Japan Coma Scale (JCS) score: I‐3. Blood tests revealed an aspartate transaminase (AST) level of 1083 U/I, an alanine transaminase (ALT) level of 219 U/L, a gamma‐glutamyl transpeptidase (γ‐GTP) level of 1151 U/L, a creatinine (Cre) level of 1.06 mg/dL, a blood urea nitrogen (BUN) level of 25 mg/dL, a C‐reactive protein (CRP) level of 0.98 mg/dL, a creatine kinase (CK) level of >40 000 mg/dL, a myocardial band (Mb) of >20 000 ng/dL, a white blood cell (WBC) count of 14 400/μL, a blood glucose level of 153 mg/dL, and a glycated hemoglobin (HbA1c) level of 8.6%. On the second day after admission (approximately 24 h after his last drink), the patient developed early alcohol withdrawal symptoms including hand tremors, sweating, and insomnia, and on the third day after admission (approximately 60 h after his last drink), he began to experience restlessness and delusions of consciousness. He also became agitated and had altered consciousness, resulting in withdrawal delirium. At the onset of withdrawal delirium, the patient received a score of 15 points on the Clinical Institute Withdrawal Assessment for Alcohol Scale‐Revised (CIWA‐Ar). The next day, the psychiatric liaison team was consulted, and on the fourth day after admission, we started treatment for withdrawal delirium in collaboration with other departments. Lorazepam (3 mg/day) was started, and the patient showed some improvement; however, his symptoms of restlessness, confusion, and altered consciousness persisted, so he was transferred to the psychiatric ward on the eighth day after admission (see Figure 1 for the subsequent course of treatment in the psychiatric ward). Immediately after transfer, the patient continued to experience active delusions, disorientation, and restlessness and required observation due to the high risk of falling and self‐extraction of intravenous drips. However, the patient continued to experience restlessness, monolog, and unintelligible speech, mainly at night. The psychiatric symptoms characteristic of withdrawal delirium disappeared, and the patient's consciousness was clear during most of the day; however, at night, the situation changed drastically, and his speech and behavior became uncoordinated. Additionally, he had many direct causes of delirium due to the coexistence of severe and multiple physical illnesses. On Day 13, lorazepam was tapered off, and 4 mg of perospirone was added. The patient's delirium improved, and all psychotropic drugs were eventually discontinued. The patient needed time to recover from acute renal failure and acne on the dorsum of the left leg, as well as from rhabdomyolysis and disuse syndrome, and to continue treatment for his physical diseases in close cooperation with physicians in the respective departments. The patient was transferred to the hospital on the 44th day after admission to continue his rehabilitation despite the improvement of his physical disease.
FIGURE 1.
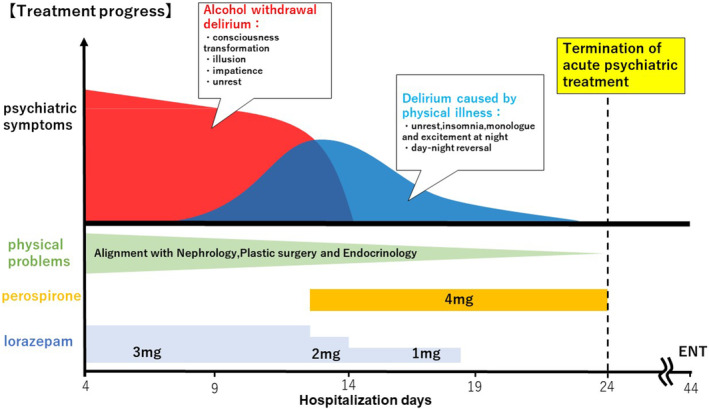
Clinical course of the patient.
3. DISCUSSION
This patient had many risk factors for withdrawal delirium, 4 , 5 , 6 , 7 including a morning alcohol consumption habit, the frequent consumption of more than 80 g of pure alcohol, an AST level of 80 U/I or higher, hallucinations, disorientation, a CIWA‐Ar score of 15 points or higher, advanced age, and the presence of medical complications. The incidence of delirium in the ICU among individuals who drank 25 g/day or more of alcohol was 39% in one study. 8 These patients were at high risk for developing delirium. Withdrawal delirium usually resolves within a few days or a week at most, and in rare cases, mild disturbance of consciousness may persist for a month or longer. 9 In this case, the delirium lasted for a long time, but we believe that delirium due to alcohol withdrawal and delirium due to physical illness occurred consecutively. This is because the psychiatric symptoms characteristic of withdrawal delirium, such as delusions and visions of small animals, disappeared on the 12th day after admission, and thereafter, the patient showed restlessness and impaired consciousness only at night, indicating a clear change in his condition. In this patient, the number and severity of medical complications were high, and delirium due to physical illness was thought to have coexisted at the time of admission due to multiple delirium risk factors.
Problems caused by alcohol abuse negatively affect family members and lead to high levels of interpersonal conflict, domestic violence, parental inappropriateness, child abuse and negligence, separation and divorce, and financial and legal problems as well as clinical problems related to alcohol abuse. 10 Furthermore, compared to being married, living alone is associated with heavy drinking (age‐adjusted odds ratio (OR); 95% confidence interval (CI): 2.15; 1.55–3.00 for men) and alcohol dependence (OR: 3.66; 2.39–5.59 for men). 7 , 8 , 9 , 10 , 11 The patient was hospitalized urgently for the treatment of his physical condition and was forced to abstain from alcohol. However, because of his original alcohol consumption problem, he had become estranged from his family, and because he was elderly, cognitively impaired and lived alone, he could not provide clear information, making it difficult to accurately assess his alcohol consumption habit and delaying treatment and early intervention for his alcohol‐related diseases.
In summary, this case emphasizes the need for multidisciplinary collaboration in the treatment of such patients, especially during disasters, and the importance of long‐term monitoring for elderly patients with alcohol dependence syndrome after a disaster.
AUTHOR CONTRIBUTIONS
KK, HC, and ST were involved in the clinical investigations. KK and NYF wrote the manuscript. SY, OT, SY, KY, SN, and NYF were involved in the literature review. All the authors have read and approved the final manuscript.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests to report. Norio Yasui‐Furukori is an editorial board member of Neuropsychopharmacology Reports and a coauthor of this article. To minimize bias, they were excluded from all editorial decision‐making related to the acceptance of this article for publication.
ETHICS STATEMENT
Approval of the Research Protocol by an Institutional Review Board: The ethics committee of the School of Medicine at Dokkyo Medical University determined that there was no need to review this case.
Informed Consent: Written informed consent was obtained from the patient's family for the publication of this case report.
Registry and the Registration No. of the Study/Trial: N/A.
Animal Studies: N/A.
Kikuchi K, Hasegawa C, Sasaki T, Sato Y, Owada T, Shindo Y, et al. Continuous alcohol withdrawal delirium and physical illness‐associated delirium in a man brought to the emergency department after a disaster: A case report. Neuropsychopharmacol Rep. 2024;44:486–489. 10.1002/npr2.12446
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
REFERENCES
- 1. Saitz R, O'Malley S. Pharmacotherapies for alcohol abuse: withdrawal and treatment. Med Clin N Am. 1997;81:881–902. [DOI] [PubMed] [Google Scholar]
- 2. Bayard M, Mcintyre J, Hill KR, Max B, Jonah M, Keith RH., Jack WJ. Alcohol withdrawal syndrome. Am Fam Physician. 2004;69:1443–1450. [PubMed] [Google Scholar]
- 3. Khan A, Levy P, Dehorn S, et al. Predictors of mortality in patients with delirium tremens. Acad Emerg Med. 2008;14:788–790. [DOI] [PubMed] [Google Scholar]
- 4. Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Diagnosis and management of acute alcohol withdrawal. CMAJ. 1999;160(5):675–680. [PMC free article] [PubMed] [Google Scholar]
- 5. Kosten TR, O'Connor PG. Management of drug and alcohol withdrawal. N Engl J Med. 2003;348(18):1786–1795. [DOI] [PubMed] [Google Scholar]
- 6. Kraemer KL, Mayo‐Smith MF, Calkins DR. Independent clinical correlates of severe alcohol withdrawal. Subst Abus. 2003;24(4):197–209. [DOI] [PubMed] [Google Scholar]
- 7. Schuckit MA. Recognition and management of withdrawal delirium (delirium tremens). N Engl J Med. 2014;371(22):2109–2113. [DOI] [PubMed] [Google Scholar]
- 8. Kudo A, Takase H, Katagai H. Are heavy alcohol drinkers prone to delirium in the ICU? J Intensive Care Med J. 2011;18:355–362. (In Japanese). [Google Scholar]
- 9. Kimura M. Alcohol withdrawal delirium. Psychiatry. 2018;60(3):243–252. (In Japanese). [Google Scholar]
- 10. Pickens RW, Preston KL, Miles DR, Gupman AE, Johnson EO, Newlin DB, et al. Family history influence on drug abuse severity and treatment outcome. Drug Alcohol Depend. 2001;61(1):261–270. [DOI] [PubMed] [Google Scholar]
- 11. Joutsenniemi K, Martelin T, Kestilä L, Martikainen P, Pirkola S, Koskinen S. Living arrangements, heavy drinking and alcohol dependence. Alcohol. 2007;42(5):480–491. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.


