Abstract
Background:
Dural arteriovenous fistula (DAVF) in the anterior cranial fossa (ACF) is known to show a high risk of intracranial hemorrhage. Recently, multi-modal fusion imaging with computed tomography angiography, computed tomography venography, and three-dimensional (3D) rotation angiography have been used preoperatively to ensure anatomical safety. We report on endovascular treatment as a first-line approach for ACFDAVF based on the understanding of vascular anatomy obtained from multi-modal fusion imaging.
Methods:
All patients with ACF-DAVF treated endovascularly as a first-line approach were included in this study. Analyses took into account complications (particularly visual function), immediate angiographic outcomes, and follow-up findings in consecutive patients with ACF-DAVF treated with interventional treatment based on multi-modal fusion imaging.
Results:
Five patients with ACF-DAVF underwent six sessions of transarterial embolization (TAE) in our institution. The five male patients (mean age, 74.5 years; range, 60–84 years) were treated with liquid embolic agents (Onyx, four procedures; n-butyl 2-cyanoacrylate, two procedures). No difference was seen between preoperative image evaluation and image evaluation during the endovascular procedure, and in all cases, a microcatheter was navigated into a target artery assumed from preoperative multi-modal imaging, allowing treatment completion in a single procedure. In all cases, the shunt disappeared completely and visual function after procedure was maintained. At the last follow-up, all patients showed a modified Rankin scale score of 0 or 1 with no recurrences.
Conclusion:
Multi-modal fusion imaging facilitates a 3D understanding of the vascular anatomy, allowing TAE as the first-line treatment for ACF-DAVF.
Keywords: Anterior cranial fossa, Endovascular, Multi-modal 3D imaging, Transarterial embolization
INTRODUCTION
Dural arteriovenous fistula (DAVF) located in the anterior cranial fossa (ACF) is rare, representing 3.7–7% of all DAVFs.[6,15] ACF-DAVF is known to have a high risk of intracranial hemorrhage (45–74%) due to the lack of venous sinuses or cortical venous drainage.[1,3,6,13,15,16] As a result, prompt attention and treatment are important. The anatomical location means that open surgery is still the first-line treatment.[2,11,14] However, interventional treatment for ACFDAVF can now be performed safely and effectively thanks to advances in device technology.[5] Furthermore, the embolic agent Onyx (Medtronic, Minneapolis, Minnesota, USA) became available for use against ACF-DAVF in 2018 in Japan, allowing transarterial embolization (TAE) as a curative therapy for ACF-DAVF. Improvements in the performance of distal access catheters (DACs) and microcatheters have also contributed to the ability of interventional treatment to now safely aim for a radical cure.
One problem with TAE is that feeders for ACF-DAVF include ethmoidal branches of the ophthalmic arteries (OAs), requiring navigation of the microcatheter to a distal position near the shunt to avoid blindness. Multi-fusion imaging comprising computed tomography angiography (CTA), computed tomography venography (CTV), and three-dimensional (3D) rotation angiography had been used preoperatively in all included cases to ensure anatomical safety. The use of multi-modal imaging enables better visualization of the ACF-DAVF pathophysiology both pre- and intraoperatively, improving treatment safety and certainty. We report on cases treated using endovascular treatment as a first-line approach for ACF-DAVF based on an advanced understanding of the vascular anatomy using multi-modal fusion imaging.
MATERIALS AND METHODS
From 2021 to 2023, all patients with ACF-DAVF treated using endovascular techniques as a first-line approach in our institution were included in this study. This retrospective observational study was based on the criteria of the Strengthening the Reporting of Observational Studies in Epidemiology statement. The Institutional Review Board at our hospital approved this study (approval no. 2580). Analyses took into account complications (particularly those involving visual function), immediate angiographic outcomes, and follow-up findings for consecutive patients with ACF-DAVF treated using interventional treatment.
Radiological imaging condition
Multi-modal 3D fusion imaging with 3D digital subtraction angiography (DSA), magnetic resonance (MR) techniques, and CTA were applied for preoperative evaluation of the angioarchitecture in each patient.
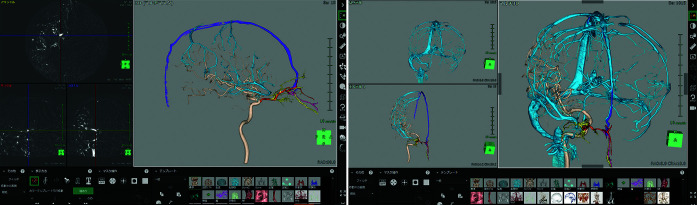
Figure 1 shows multi-modal imaging being created in Synapse Vincent (Fujifilm Co., Tokyo, Japan). Feeder and drainer vessels and the shunt point were confirmed in discussions between the radiologist and neurointerventionist, then maximum intensity projection images were used to follow blood vessels to identify connections (including feeders of small blood vessels) and create images [Figure 1a]. Each feeder was color-coded to facilitate visualization of the run. An intraoperative view for embolization was also created to aid treatment visualization. Figure 1b depicts a representative multi-modal 3D fusion image of ACF-DAVF for preoperative evaluation utilizing Synapse Vincent software (Fujifilm Co.). This diagnostic imaging technique visualizes 3D positional relationships between the skull, dura mater, and brain, allowing the treatment team to discuss more thorough and specific treatment recommendations.
Figure 1:
(a) Maximum intensity projection images are used to follow blood vessels to clarify connections, including feeders for small blood vessels, and to create images. (b) Each feeder should be color-coded to facilitate visualization of the run. Three-dimensional fusion image of anterior cranial fossa-dural arteriovenous fistula for preoperative evaluation utilizing SYNAPSE VINCENT software (Fujifilm Co., Tokyo, Japan).
Endovascular procedures
Neurointerventionists performed all procedures. Unfractionated heparin was administered during the procedure to maintain an activated clotting time of over 300 seconds. The transarterial approach was performed in the standard fashion. An 8-Fr guiding catheter was placed in the appropriate internal carotid artery. A microcatheter was then navigated over the microwire, and selective catheterization of the target artery was performed. A DAC was used to stabilize the microcatheter.
Preoperative multi-fusion imaging was used for catheter navigation to confirm the vascular run and provide a reference for access. These images were also used as a guide to help with wire operation by navigating to the target artery.
Either Onyx or n-butyl 2-cyanoacrylate (NBCA) was used as the embolic agent.
RESULTS
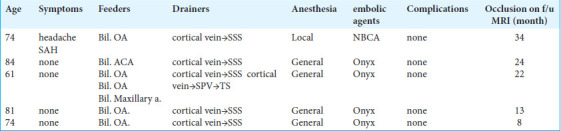
Table 1 summarizes all the cases included in this study. Five patients with ACF-DAVF underwent six sessions of TAE in our institution from 2021 to 2023. One patient presented with subarachnoid hemorrhage, and the remaining four patients were asymptomatic, with the DAVF as an incidental finding. Follow-up ranged from 8 months to 34 months. In this series, arterial supply from bilateral OAs was present in all cases. Associated arterial supply from the anterior cerebral artery (ACA) and internal maxillary artery was present in 1 patient. Cortical venous drainage was seen in all cases. The 6 cases (5 men; mean age, 74.5 years; range, 60–84 years) were treated with a liquid embolic agent (Onyx, n = 4; NBCA, n = 2). TAE was performed under general anesthesia in 4 patients (four cases) and with local anesthesia in 1 patient (two cases). No difference was evident between preoperative image evaluation and image evaluation during interventional radiology (IVR), and in all cases, a microcatheter was navigated into the target artery selected from preoperative multi-modal imaging, allowing treatment completion in a single procedure. In all cases, the shunt disappeared completely, and visual function after the procedure was maintained. At the last follow-up, all patients showed a modified Rankin scale score of 0 or 1 with no recurrences.
Table 1:
Summary of all ACF-DAVF cases.
CASE DESCRIPTIONS
Case 1
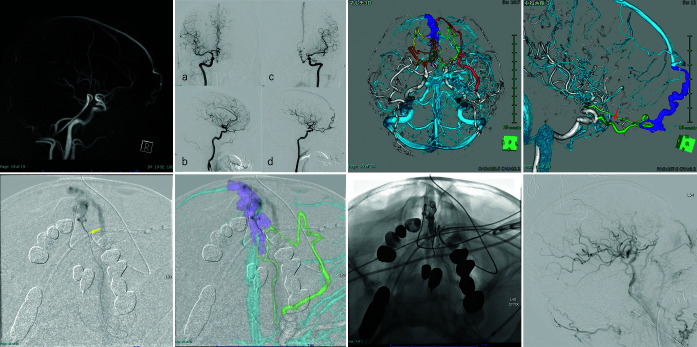
An 84-year-old man presented to the hospital complaining of dizziness. MR imaging of the brain revealed ACF-DAVF [Figure 2a], and the patient was referred to our department. DSA confirmed ACF-DAVF with multiple feeders arising from bilateral OAs, bilateral fronto-orbital arteries, and bilateral maxillary arteries with cortical venous reflux into the superior sagittal sinus (SSS) through the left anterior fronto-orbital vein (Borden type III, Cognard type IV) [Figure 2b].
Figure 2:
(a) Brain magnetic resonance angiography and (b) Digital subtraction angiography reveal anterior cranial fossa-dural arteriovenous fistula. (a and b) Right ICA angiography. (c and d) Left ICA angiography. (c and d) A three-dimensional (3D) reconstructed vascular image visually aids in understanding the 3D angioarchitecture of the shunt. Color coding: Yellow, right anterior ethmoidal artery; orange, right posterior ethmoidal artery (PEA); red, left maxillary artery; green, left PEA; light green, left anterior cerebral artery (ACA). Red arrow: Beginning of the central retinal artery. (e) A front view shows the location of catheters navigated to the shunt through the left ACA. Yellow arrow: the microcatheter close to the shunt. (f) Intraoperative image with superimposed multi-fusion imaging. Image visualization is helped by making the multi-fusion imaging and intraoperative views the same. (g) Onyx penetrates the draining vein beyond the shunt pouch. (h) The shunt point is completely occluded by backflow from the shunt pouch to each feeder, and the shunt disappears.
While reading CTA, CTV, and DSA images, two neurointerventionists and a radiologist collaborated to create multi-modal fusion imaging. The location of the central retinal artery was confirmed based on the resulting images. Multi-modal imaging was reconstructed for preoperative evaluation [Figures 2c and d]. These multi-modal 3D images confirmed the shunt point and bifurcation of the central retinal artery. The images were shared visually to ensure a safe distance for embolic material to flow back through the shunt. Furthermore, these images were used to determine the target artery for TAE. In this case, the left ACA was the target artery for TAE because a microcatheter was predicted to be able to navigate close to the shunt point through the ACA.
The procedure was performed under general anesthesia. Long 8-Fr sheaths were inserted into the right femoral artery. An 8-Fr guiding catheter (RoadMaster; Goodman, Aichi, Japan) was positioned at the origin of the left ICA. First, with the left 8-Fr Roadmaster, a 3.4-Fr Tactics catheter (Technorat Corporation, Aichi, Japan) was navigated with the aid of a DeFrictor bull microcatheter (Medico’s Hirata, Osaka, Japan) and Tenrou1014 guidewire (Kaneka Medix Corp., Osaka, Japan) close to the bifurcation of the left ACA. Moreover, the DeFrictor bull microcatheter (Medico’s Hirata) and CHIKAI ×10 guidewire (Asahi Intecc, Aichi, Japan) were inserted through the left ACA as close to the shunt point as possible [Figure 2e]. Overlaying multi-modal fusion imaging and the intraoperative view simplified the visualization of which feeder should be refluxed and where reflux would be dangerous [Figure 2f]. Onyx was slowly injected with intermittent pauses through the left ACA. Onyx slowly penetrated the draining vein beyond the shunt pouch [Figure 2g]. No glue migrated to the SSS or refluxed to the central retinal artery on either side. The shunt point was completely occluded by backflow from the shunt pouch to each feeder, and the shunt disappeared [Figure 2h]. The patient was discharged without a neurological deficit. Post-embolization MR angiography confirmed complete occlusion, and no recurrence of the fistula was seen during 24 months of follow-up.
Case 2
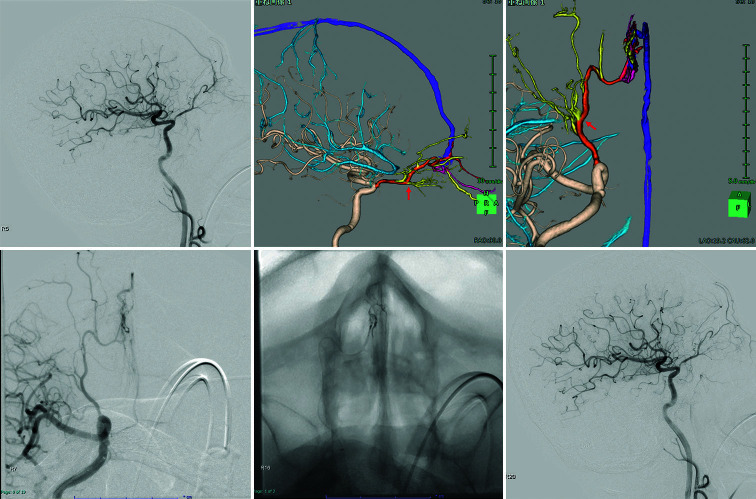
A 74-year-old man presented to the hospital complaining of a headache. MR imaging of the brain revealed ACF-DAVF, and he was referred to our department. DSA confirmed an ACFDAVF with a single feeder, arising from the right OA with cortical venous reflux into the SSS through the right anterior fronto-orbital vein (Borden type III, Cognard type IV) [Figure 3a]. Multi-modal images were reconstructed for preoperative evaluation [Figures 3b and c] and the location of the central retinal artery was clearly confirmed from multi-modal fusion imaging. In this case, the microcatheter was predicted to be able to navigate close to the shunt point through the right posterior ethmoidal artery (PEA). The distance from the central retinal artery was determined to be safe, and TAE was selected.
Figure 3:
(a) Digital subtraction angiography reveals anterior cranial fossa-dural arteriovenous fistula. (b and c) A three-dimensional (3D) reconstructed vascular image visually aids in understanding the 3D angioarchitecture of the shunt. The right posterior ethmoid arteries feed the shunt and drain the superior sagittal sinus through dilated cortical veins. Red arrow (b): Beginning of the central retinal artery. The right posterior ethmoidal artery (c; red arrow) is not tortuous and is close to the shunt point. (d and e) The front view shows the location of catheters navigated to the shunt through the right ophthalmic artery. The microcatheter is close to the shunt. The intermediate distal-access catheter is located in the ophthalmic portion of the right internal carotid artery. (f) The shunt point is completely occluded by backflow from the shunt pouch to each feeder, and the shunt disappears.
The procedure was performed under general anesthesia. A long, 8-Fr sheath was inserted into the right femoral artery. An 8-Fr guiding catheter (FUBUKI; Asahi Intecc) was positioned at the origin of the right ICA. First, using the 8-Fr FUBUKI (Asahi Intecc), a 3.4-Fr Tactics plus catheter (Technorat Corporation, Aichi, Japan) was navigated with the aid of a DeFrictor bull microcatheter (Medico’s Hirata) and Tenrou1014 guidewire (Kaneka Medix Corp.) near to the bifurcation of the right OA. Moreover, a DeFrictor bull microcatheter (Medico’s Hirata) and CHIKAI ×10 guidewire (Asahi Intecc) were inserted through the right PEA as close to the shunt point as possible. Identifying which feeder should be refluxed and where reflux would likely be dangerous was made easy when multi-modal fusion imaging and the intraoperative view were superimposed [Figures 3c and d]. Onyx was slowly injected with intermittent pauses through the right PEA. Onyx slowly penetrated the draining vein beyond the shunt pouch [Figure 3e]. No glue migrated to the SSS or refluxed to the right central retinal artery. The shunt point was completely occluded, and the shunt disappeared in all cases [Figure 3f]. The patient was discharged without a neurological deficit. Post-embolization MR angiography confirmed complete occlusion with no recurrence of the fistula during 13 months of follow-up.
DISCUSSION
No difference was evident between preoperative multi-modal 3D image evaluation and image evaluation during IVR, with all cases involving a microcatheter navigated into a target artery assumed from preoperative multi-modal imaging, allowing treatment to be completed in a single procedure. The preoperative consideration in detail was that using multi-modal 3D imaging, TAE for ACF-DAVF can be performed safely while providing high complete occlusion rates.
Since direct surgery has demonstrated positive clinical outcomes, surgical treatment has been regarded as the major treatment option for ACF-DAVF over the years.[2,10,11,14,17] Anatomically, ACF-DAVF cannot access the shunt pouch via a transvenous approach due to the tortuous cortical veins. Further, ACF-DAVF is usually supplied by branches of the OA, so open surgery is still selected as a first-line treatment due to its superficial location, far from eloquent areas, and easy exposure during craniotomy.[11,14]
On the other hand, the safety and efficacy of endovascular treatment for ACF-DAVF have been extensively reported. [5,9,11] TAE has been described as the primary treatment in cases with non-tortuous transarterial access to the fistula.[1,9] The success rate for surgical treatment of ACFDAVF is between 85% and 95%,[11,15] with a complication rate of 5–9%.[1,15] The success rate for interventional treatment of ACF-DAVF is between 46% and 82.6%, with a complication rate of 3–22.2%.[2,5,7] The transvenous approach for ACFDAVF is safe and effective with a high rate of complete occlusion,[5] but reaching the shunt point would be difficult due to the tortuous drainer vessels.
Device improvement is one factor that has enabled the expansion of the indications for TAE. With the development of highly guided DACs and microcatheters, devices can now be directed close to the shunt location. Another reason IVR is feasible is the availability of Onyx, a non-adhesive embolic agent that may be repeatedly injected and paused to overflow into multiple feeders for embolization. Transarterial treatment of DAVFs using non-adhesive liquid embolic agents as the primary embolic agents is well established. Reports of treatment using Onyx for DAVF have recently increased.[8] Onyx TAE allows easier flow control than NBCA because the injection can be halted, preventing Onyx from flowing into non-target vessels.[4] On the other hand, despite these recent advances in endovascular approaches, treatment of ACF-DAVF continues to pose significant challenges. Complete preoperative comprehension of the distance between the area to which the microcatheter can be guided and the central retinal artery is critical.
The first preoperative consideration is how to avoid the complication of blindness. Confirming the bifurcation of the central retinal artery on multi-modal 3D imaging is crucial. Multi-modal imaging is performed before transarterial treatment to assess which placements are acceptable and thus avoid regurgitation into the central retinal artery. Although the introduction of Onyx and technological advances have made the disease treatable with IVR, multi-modal fusion imaging is now being used to increase safety and efficacy. Multi-modal 3D images provide visual information to the endovascular surgeon and allow all staff involved in the IVR procedure to see the same image, whereas conventional intraoperative imaging alone is insufficient.
Second, target feeders that can be used to navigate close enough to the shunt point are important. TAE can be highly effective and curative if a catheter can be inserted sufficiently close to the fistulous connection.[12] TAE for DAVF may include migration of liquid embolic agent and feeder occlusion if the microcatheter cannot be inserted close enough to the shunt point. Multi-modal imaging provides detailed information on which feeders are most likely to reach the shunt and gives the operator visual information on the target artery to optimize the chance of effective treatment.
Multi-modal imaging is an advantageous tool for keeping not only the surgeon but also the entire treatment team on the same page. Catheter guidance can be predicted using visual confirmation of the vascular architecture. Although quantifying a safe reflux distance is difficult, multi-modal fusion images offer an indicator.
Some issues with 3D fusion images remain. Because the images are created artificially, some degree of error is possible. Fortunately, no image errors that affected the procedures were encountered in this case series, but arterial and venous images in the shunt can be confused in complex, intricate situations. In the future, preoperative multi-modal 3D images could potentially be linked to actual intraoperative images, which would furnish operators with even better indicators to improve the safety and efficacy of treatment further.
CONCLUSION
Advances in DAC and microcatheters and the expansion of indications for Onyx have made ACF-DAVF reliably curable using TAE. Multi-modal fusion imaging facilitates a 3D understanding of the vascular anatomy, helping to make endovascular treatment the first-line treatment for ACFDAVF.
Footnotes
How to cite this article: Kotsugi M, Konishi K, Yokoyama S, Okamoto A, Nakase K, Maeoka R, et al. Transarterial embolization for anterior cranial fossa dural arteriovenous fistula based on multi-modal three-dimensional imaging. Surg Neurol Int. 2024;15:386. doi: 10.25259/SNI_698_2024
Contributor Information
Masashi Kotsugi, Email: igustok@naramed-u.ac.jp.
Kengo Konishi, Email: konishi.nramed@gmail.com.
Shohei Yokoyama, Email: shoheidon1182@gmail.com.
Ai Okamoto, Email: aiokamoto@naramed-u.ac.jp.
Kenta Nakase, Email: ken0619@gmail.com.
Ryosuke Maeoka, Email: r.maeoka@naramed-u.ac.jp.
Ryosuke Matsuda, Email: rmatsuda@naramed-u.ac.jp.
Ichiro Nakagawa, Email: nakagawa@naramed-u.ac.jp.
Ethical approval
The Institutional Review Board approved the research/study at Nara Medical University Hospital, number 2580, dated January 01, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Agid R, Terbrugge K, Rodesch G, Andersson T, Söderman M. Management strategies for anterior cranial fossa (ethmoidal) dural arteriovenous fistulas with an emphasis on endovascular treatment. J Neurosurg. 2009;110:79–84. doi: 10.3171/2008.6.17601. [DOI] [PubMed] [Google Scholar]
- 2.Cannizzaro D, Peschillo S, Cenzato M, Pero G, Resta MC, Guidetti G, et al. Endovascular and surgical approaches of ethmoidal dural fistulas: A multicenter experience and a literature review. Neurosurg Rev. 2018;41:391–8. doi: 10.1007/s10143-016-0764-1. [DOI] [PubMed] [Google Scholar]
- 3.Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: Clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995;194:671–80. doi: 10.1148/radiology.194.3.7862961. [DOI] [PubMed] [Google Scholar]
- 4.Cognard C, Januel AC, Silva NA, Jr, Tall P. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: New management using Onyx. AJNR Am J Neuroradiol. 2008;29:235–41. doi: 10.3174/ajnr.A0817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dabus G, Kan P, Diaz C, Pabon B, Andres-Mejia J, Linfante I, et al. Endovascular treatment of anterior cranial fossa dural arteriovenous fistula: A multicenter series. Neuroradiology. 2021;63:259–66. doi: 10.1007/s00234-020-02536-3. [DOI] [PubMed] [Google Scholar]
- 6.Halbach VV, Higashida RT, Hieshima GB, Wilson CB, Barnwell SL, Dowd CF. Dural arteriovenous fistulas supplied by ethmoidal arteries. Neurosurgery. 1990;26:816–23. doi: 10.1097/00006123-199005000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Hiramatsu M, Sugiu K, Hishikawa T, Nishihiro S, Kidani N, Takahashi Y, et al. Results of 1940 embolizations for dural arteriovenous fistulas: Japanese Registry of Neuroendovascular Therapy (JR-NET3) J Neurosurg. 2019;133:166–73. doi: 10.3171/2019.4.JNS183458. [DOI] [PubMed] [Google Scholar]
- 8.Hou K, Ji T, Guo Y, Xu B, Xu K, Yu J. Current status of endovascular treatment for dural arteriovenous fistulas in the superior sagittal sinus region: A systematic review of the literature. World Neurosurg. 2019;122:133–43. doi: 10.1016/j.wneu.2018.10.145. [DOI] [PubMed] [Google Scholar]
- 9.Inoue A, Tagawa M, Kumon Y, Watanabe H, Shoda D, Sugiu K, et al. Ethmoidal dural arteriovenous fistula with unusual drainage route treated by transarterial embolization. J Neurointerv Surg. 2015;7:e15. doi: 10.1136/neurintsurg-2013-011098.rep. [DOI] [PubMed] [Google Scholar]
- 10.Jee TK, Lee YW, Yeon JY, Kim KH, Jeon P, Kim JS, et al. Surgical strategy for ethmoidal dural arteriovenous fistula. World Neurosurg. 2022;164:e91–8. doi: 10.1016/j.wneu.2022.03.131. [DOI] [PubMed] [Google Scholar]
- 11.Kakarla UK, Deshmukh VR, Zabramski JM, Albuquerque FC, McDougall CG, Spetzler RF. Surgical treatment of high-risk intracranial dural arteriovenous fistulae: Clinical outcomes and avoidance of complications. Neurosurgery. 2007;61:447–57. doi: 10.1227/01.NEU.0000290889.62201.7F. [DOI] [PubMed] [Google Scholar]
- 12.Lin N, Brouillard AM, Mokin M, Natarajan SK, Snyder KV, Levy EI, et al. Direct access to the middle meningeal artery for embolization of complex dural arteriovenous fistula: A hybrid treatment approach. J Neurointerv Surg. 2015;7:e24. doi: 10.1136/neurintsurg-2014-011256.rep. [DOI] [PubMed] [Google Scholar]
- 13.Lv X, Li Y, Liu A, Lv M, Jiang C, Wu Z. Endovascular embolization of dural arteriovenous fistulas of the anterior cranial fossa: Three case reports. Neurol Res. 2008;30:852–9. doi: 10.1179/174313208X310313. [DOI] [PubMed] [Google Scholar]
- 14.Meneghelli P, Pasqualin A, Lanterna LA, Bernucci C, Spinelli R, Dorelli G, et al. Surgical treatment of anterior cranial fossa dural arterio-venous fistulas (DAVFs): A twocentre experience. Acta Neurochir (Wien) 2017;159:823–30. doi: 10.1007/s00701-017-3107-2. [DOI] [PubMed] [Google Scholar]
- 15.Robert T, Blanc R, Smajda S, Ciccio G, Redjem H, Bartolini B, et al. Endovascular treatment of cribriform plate dural arteriovenous fistulas: Technical difficulties and complications avoidance. J Neurointerv Surg. 2016;8:954–8. doi: 10.1136/neurintsurg-2015-011956. [DOI] [PubMed] [Google Scholar]
- 16.Spiotta AM, Hawk H, Kellogg RT, Turner RD, Chaudry MI, Turk AS. Transfemoral venous approach for Onyx embolization of anterior fossa dural arteriovenous fistulae. J Neurointerv Surg. 2014;6:195–9. doi: 10.1136/neurintsurg-2012-010642. [DOI] [PubMed] [Google Scholar]
- 17.Zhang L, Wang H, Pan Y, Mao L, Ding K, Zhu J. Clinical characteristics and microsurgery treatment of anterior cranial fossa dural arteriovenous fistula. J Craniofac Surg. 2019;30:e701–3. doi: 10.1097/SCS.0000000000005661. [DOI] [PubMed] [Google Scholar]