Abstract
Background:
Filum terminale lipomas (FTLs) are congenital lumbosacral anomalies that can cause tethered cord syndrome (TCS). Most patients with TCS caused by FTL are children, and these are only rarely present in adults.
Case Description:
A 64-year-old male presented with long-standing bilateral lower-limb weakness and bladder dysfunction. The lumbar magnetic resonance imaging revealed an FTL of the conus, which was not displaced. Following sectioning, the patient’s bilateral lower limb weakness resolved, and his bladder function improved.
Conclusion:
TCS caused by an FTL in late middle-aged patients is rare. After undergoing untethering with resection of the lipoma, the patient sustained resolution of his motor deficit and improvement in his bladder function.
Keywords: Adult, Filum terminale, Lipoma, Spinal dysraphism, Tethered cord syndrome

INTRODUCTION
Filum terminale lipoma (FTL) can cause tethered cord syndrome (TCS). Magnetic resonance imaging (MRI) studies have shown that FTLs involve the conus in 0.24–5% of cases.[2,7] These lesions are rarely encountered in adults. Here, a 64-year-old male presented with chronic bilateral lower extremity deficits accompanied by bladder dysfunction that improved following resection of the FTL tethering his conus.
CASE DESCRIPTION
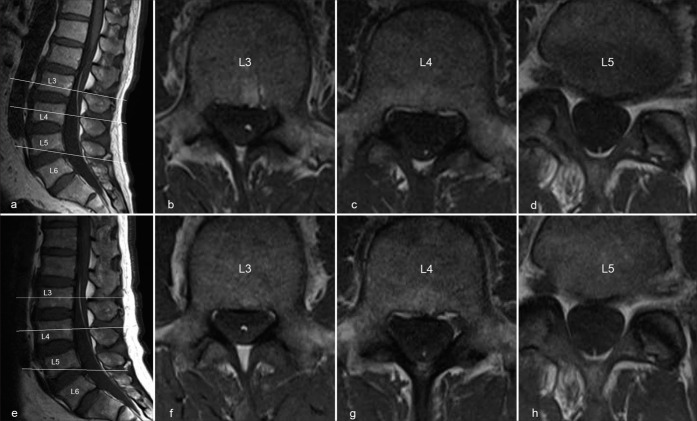
A 64-year-old male presented with chronic lower-limb weakness that was greater on the left side than on the right side, along with numbness, hyperactive patellar responses, and bladder dysfunction. His visual analog scale (VAS) scores were 30 mm for lower back pain, 20 mm for buttock and leg pain, and 50 mm for numbness of the buttock and leg. The Oswestry Disability Index (ODI) score was 84%. Cerebrospinal fluid studies were normal. Lumbar T1-weighted imaging showed hyperintensity of the thickened filum terminale dorsal to the spinal canal, suggesting an FTL [Figure 1]. The conus medullaris terminated at the superior edge of the L2 vertebral body (i.e., normal location), and there was no conus migration in the supine versus prone position on MRI [Figure 1].
Figure 1:
(a-d) Lumbosacral magnetic resonance imaging (MRI) in the supine position. (a) Sagittal T1-weighted image showing hyperintensity of the thickened filum terminale. (b-d) Axial T1-weighted images at the levels of the white lines in panel a. (e-h) Lumbosacral MRI in the prone position. MRI scan in the prone position showed no deviation in the filum terminale run, compared with MRI scan in the supine position. (f-h) Axial T1-weighted images at the levels of the white lines in panel e.
Surgery
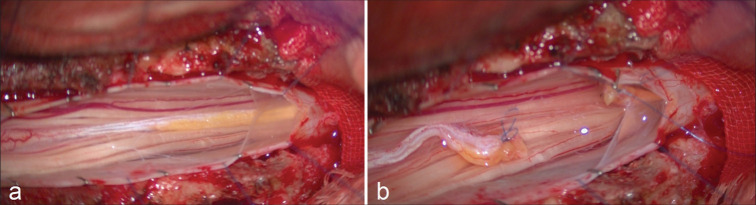
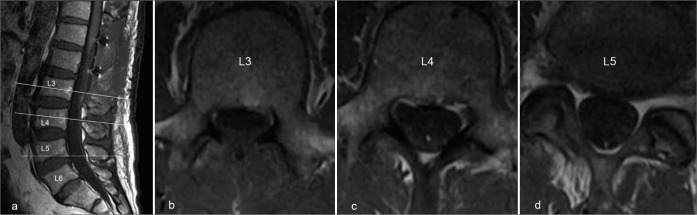
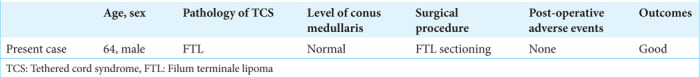
The patient underwent FTL sectioning. Thickening of the fatty tissue at the level of the filum terminale was observed during surgery [Figure 2]. Biopsy confirmed a benign lipoma (i.e., homogeneous proliferation of mature adipose tissue). Post-operative MRI confirmed complete resection of the lipoma [Figure 3]. Postoperatively, the patient’s lower extremity symptoms/signs resolved, while the VAS scores improved (20 mm for lower back pain, 0 mm for buttock and leg pain, and 0 mm for numbness of the buttock and leg), along with the ODI (i.e., a score of 14% 3 months postoperatively). A summary of the present case is given in Table 1.
Figure 2:
(a) Intraoperative findings showing a thickening fatty tissue localized in the filum terminale. (b) The thickened filum terminale is transected, and the tethered cord is released.
Figure 3:
(a-d) Post-operative lumbosacral magnetic resonance imaging in the supine position. (a and b) Sagittal and axial T1-weighted image showing removal of the filum terminale lipoma. (b-d) Axial T1-weighted images at the levels of the white lines in panel a.
Table 1:
Summary of the present case.
DISCUSSION
Rare FTL in adults
The prevalence of FTL and thickened fatty filum terminale ranges from 0.24% to 5%.[2,7]
TCS is conventionally defined as having a low-lying conus medullaris that terminates below the vertebral body of L2.[3] Typically, FTLs are present in children, with rare symptomatic cases being found in adults (mean: 24.09 years and range: 18–34).[1]
MR diagnosis of FTL with TCS
MRI is the best imaging tool to diagnose FTL with TCS. Stamates et al. reported that an MRI performed in the prone position is a sensitive and specific tool for the diagnosis of TCS.[6] Karraslan et al. reported sagittal spinopelvic differences in TCS owing to fatty filum terminale.[4] Age-related changes in the sagittal balance between thoracic kyphosis and lumbar lordosis may increase the tension in the spinal cord, resulting in the development of TCS.
Indications for surgery for FTL
Surgical release of the tethered filum terminale is necessary to relieve TCS. Klekamp reported 85 patients with a tethered cord that was not diagnosed in childhood.[5] Of them, 43 patients (51 ± 15 years) developed a TCS; they concluded that surgery in adult patients with TCS should be reserved for those with symptoms.
CONCLUSION
FTLs in adults with TCS are rare. Older patients should be considered surgical candidates for detethering if they are sufficiently symptomatic.
Footnotes
How to cite this article: Hashimoto J, Kawasaki T, Kobayashi T, Ioroi Y, Takayama M. Tethered cord syndrome in an adult with filum terminale lipoma: A case report. Surg Neurol Int. 2024;15:375. doi: 10.25259/SNI_708_2024
Contributor Information
Jun Hashimoto, Email: hashi10n999@gmail.com.
Toshinari Kawasaki, Email: tkawasaki821@gmail.com.
Tamaki Kobayashi, Email: kobayashitamak@gmail.com.
Yoshihiko Ioroi, Email: yioroi@kuhp.kyoto-u.ac.jp.
Motohiro Takayama, Email: m.takayama.md@katsura.com.
Ethical approval
The research/study approved by the Institutional Review Board at Kyoto Katsura Hospital, number 2024-43, dated July 29, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Akay KM, Erşahin Y, Cakir Y. Tethered cord syndrome in adults. Acta Neurochir (Wien) 2000;142:1111–5. doi: 10.1007/s007010070038. [DOI] [PubMed] [Google Scholar]
- 2.Brown E, Matthes JC, Bazan C, 3rd, Jinkins JR. Prevalence of incidental intraspinal lipoma of the lumbosacral spine as determined by MRI. Spine (Phila Pa 1976) 1994;19:833–6. doi: 10.1097/00007632-199404000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Hoffman HJ, Hendrick EB, Humphreys RP. The tethered spinal cord: Its protean manifestations, diagnosis and surgical correction. Childs Brain. 1976;2:145–55. doi: 10.1159/000119610. [DOI] [PubMed] [Google Scholar]
- 4.Karraslan B, Gulsuna B, Toktas O, Borcek AO. Saggital spinoplevic alignment in tethered cord syndrome and split cord malformation. Br J Neurosurg. 2024;38:1114–9. doi: 10.1080/02688697.2022.2034741. [DOI] [PubMed] [Google Scholar]
- 5.Klekamp J. Tethered cord syndrome in adults. J Neurosurg Spine. 2011;15:258–70. doi: 10.3171/2011.4.SPINE10504. [DOI] [PubMed] [Google Scholar]
- 6.Stamates MM, Frim DM, Yang CW, Katzman GL, Ali S. Magnetic resonance imaging in the prone position and the diagnosis of tethered spinal cord. J Neurosurg Pediatr. 2018;21:4–10. doi: 10.3171/2017.3.PEDS16596. [DOI] [PubMed] [Google Scholar]
- 7.Uchino A, Mori T, Ohno M. Thickened fatty filum terminale: MR imaging. Neuroradiology. 1991;33:331–9. doi: 10.1007/BF00587817. [DOI] [PubMed] [Google Scholar]