Abstract
Importance
Previous work demonstrated postoperative hypothyroidism adversely affects wound healing in salvage laryngectomy. Currently, no studies have evaluated the association between wound healing and hypothyroidism in patients undergoing salvage oropharyngectomy.
Objective
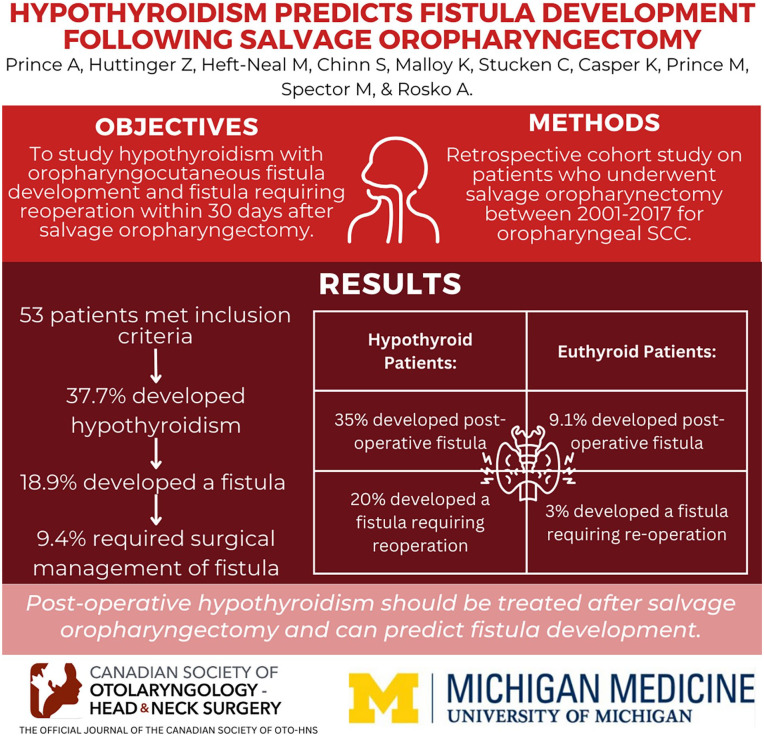
The primary objective was studying hypothyroidism and other factors associated with oropharyngocutaneous fistula development and fistula requiring reoperation within 30 days after salvage oropharyngectomy.
Design
Retrospective cohort study.
Setting
Tertiary academic center.
Participants
All patients who underwent salvage oropharyngectomy for recurrent or second primary oropharyngeal squamous cell carcinoma between 2001 and 2017 after radiation or chemoradiation. Patients with no preoperative thyroid-stimulating hormone (TSH) values were excluded.
Exposures
Salvage oropharyngectomy for recurrent or second primary oropharyngeal squamous cell carcinoma.
Main Outcomes Measures
The principle explanatory variable was postoperative hypothyroidism, defined as TSH greater than 5.5 mIU/L. Univariate, bivariate, and binary logistical regression multivariate analysis was performed.
Results
Fifty-three patients met inclusion criteria, 37.7% of patients developed hypothyroidism, 18.9% developed a fistula, and 9.4% required an operation to manage the fistula. Postoperative fistula rate was 35% among hypothyroid patients, which was significantly greater than among euthyroid patients (9.1%; P = .03). A fistula requiring reoperation occurred in 20% of hypothyroid patients compared with that of euthyroid patients (3%; P = .061). In a multivariate analysis, postoperative hypothyroid patients were at a 9.5-fold increased risk of developing a fistula [95% confidence interval (CI) 1.6-57.0, P = .013]. Additionally, postoperative hypothyroid patients were at 13.6-fold increased risk for development of a fistula requiring reoperation (95% CI 1.2-160.5, P = .038).
Conclusions and Relevance
Postoperative hypothyroidism in patients who underwent salvage oropharyngectomy can predict fistula development and fistula requiring operative management. This study supports the treatment of hypothyroidism after surgery to reduce wound complications.
Keywords: head and neck cancer, salvage surgery, salvage oropharyngectomy, hypothyroidism, wound healing, fistula
Graphical abstract.
Introduction
Squamous cell cancer (SCC) of the oropharynx has a significant disease burden, with an incidence of 18.1 and 6.5 cases per 100,000 men and women, respectively, in the United States. 1 While the incidence of head and neck cancer located at most oral sites is marginally decreasing due to reduced exposure to tobacco and alcohol, the incidence of oropharyngeal carcinomas is increasing.2,3 The increased incidence is being driven by human papilloma virus (HPV) infection, which is currently higher than that of HPV-associated cervical carcinoma.4,5
In patients for whom primary resection is not an option or those who desire functional-organ-preserving therapy, radiation therapy (RT), and chemoradiation therapy (CRT) provide a valid treatment option.6,7 Unfortunately, up to 20% of patients treated for oropharyngeal SCC with RT or CRT experience treatment failure and subsequent recurrence.8,9 In this patient population, salvage surgical management has been demonstrated to provide improved survival compared with nonsurgical management. 10
Fistula development following head and neck surgery is a serious postoperative complication that is associated with increased morbidity, length of hospitalization, and wound-related death.11-14 Oro- and/or pharyngo-cutaneous fistulas have been reported in approximately 10% to 20% of postoperative head and neck cancer patients.15-18 Patients with prior RT or CRT are at increased risk of postoperative wound complications due to the effects of the prior treatment on the local structures and environment. 19 Additionally, patients who have received external beam RT to the head and neck are at increased risk of developing posttreatment hypothyroidism, with incidences of up to 48% in patients who received treatment for oropharyngeal malignancies.20-22
Hypothyroidism has been demonstrated to contribute to poor wound healing and increased risk of fistula development. 23 Spontaneous closure of persistent fistulas after thyroid hormone replacement therapy has been reported, and persistent fistulas have been correlated with ongoing hypothyroidism.24-26 Recent work from our institution demonstrated that postoperative hypothyroidism independently predicted wound-healing complications, including fistula development and fistula formation which required operative management in patients undergoing salvage laryngectomy. 27 To date, however, this association has not been studied in patients undergoing salvage surgical management for SCC within the oropharynx. We hypothesize that patients who develop hypothyroidism in the immediate postoperative period following salvage oropharyngectomy will have an increased risk of fistula formation.
Methods
Study Design/Institutional Review Board
An institutional review board (IRB)–approved (University of Michigan IRB HUM00152046) single-institution retrospective case series was performed using a database of patients treated with primary radiation or chemoradiation, who developed recurrent or second primary SCC of the oropharynx requiring salvage surgery. We defined oropharyngeal tumors as those from the 4 common subsites of base of tongue, palatine tonsils, tonsillar pillars, and pharyngeal wall. Adult patients who underwent salvage surgical treatment for persistent or recurrent oropharyngeal SCC after RT or CRT failure between 2001 and 2017 at the University of Michigan were enrolled in the study (n = 94). As postoperative hypothyroidism was the principal explanatory variable, patients with no preoperative thyroid-stimulating hormone (TSH) values were excluded from this study. All patients who were not biochemically euthyroid preoperatively were also excluded.
Demographics, initial and recurrent clinical T classification and N classification, primary treatment method, neck dissection, pathologic recurrent T and N classification, and preoperative synthroid use were tabulated. Patients were staged in accordance with the seventh edition of the American Joint Committee on Cancer Staging System. Levels of TSH were collected pre- and postoperatively. Patients were classified as hypothyroid if a 7-day postoperative TSH level was greater than 5.5 mIU/L, the lab value cutoff used by our institution to define hypothyroidism. Primary end points of the study were fistula formation within 30 days postoperatively and fistula formation that required operative management during the same period.
Statistical Analysis
Univariate analysis was performed and bivariate associations between clinical variables were tested with nonparametric tests (Fisher’s exact test, χ2 test with Monte Carlo estimates for error terms). The development of hypothyroidism was evaluated using bivariate analysis, and variables with a P-value of less than .1 in the bivariate analysis were included in the multivariate model. The development of fistula and fistula needing reoperation were also evaluated. Bivariate analysis was performed, and variables with a P value lower than .1 in the bivariate analysis were included in the multivariate analysis. Variables that were previously predictive in our cohort and in previous studies were also included in the model. Multivariate analysis was performed using a Backward Wald logistic regression model. Univariate and multivariate analysis was performed using the SPSS version 26 software (IBM, Armonk, NY, USA).
Results
Study Population
Ninety-four patients who underwent salvage oropharyngectomy for recurrent oropharyngeal carcinoma at the University of Michigan Hospital System between September 1998 and March 2017 were identified. Of this original cohort, 41 patients were excluded, due to lack of postoperative TSH values. The final cohort of 53 patients had an average age of 63 years and a mean time to recurrence of 4.7 ± 4.6 years (Table 1). The majority of patients were male (71.7%) and reported either former (62.3%) or current (20.8%) tobacco use. Initial treatment was limited to RT in (35.8%) of patients and the remaining (64.2%) were treated with CRT. At the time of recurrence, most tumors were classified as advanced T-stage (65.3%) or advanced overall stage (69.8%).
Table 1.
Patient Cohort Demographics.
| Patient Demographics | No fistula (n = 43) count (%) | Fistula (n = 10) count (%) | All (n = 53) count (%) | P value |
|---|---|---|---|---|
| Age | ||||
| Mean (years) | 63.7 ± 8.9 | 60.6 ± ± 7.9 | 63.0 ± 8.7 | .313 |
| Sex | ||||
| Male | 30 (69.8%) | 8 (80%) | 38 (71.7%) | .71 |
| Female | 13 (30.2%) | 2 (20%) | 15 (28.3%) | |
| Tobacco | ||||
| Never | 6 (14%) | 2 (20%) | 8 (15.1%) | |
| Former | 28 (65.1%) | 5 (50%) | 33 (62.3%) | .30 |
| Current | 8 (18.6%) | 3 (30%) | 11 (20.8%) | |
| Unavailable | 1 (2.3%) | 0 | 1 (1.9%) | |
| ETOH | ||||
| No | 27 (62.7%) | 8 (80%) | 35 (66%) | |
| Yes | 10 (23.3%) | 1(10%) | 11 (20.8%) | .56 |
| Unavailable | 6 (14%) | 1 (10%) | 7 (13.2%) | |
| HPV | ||||
| Negative | 11 (25.6%) | 1 (10%) | 12 (22.6%) | .119 |
| Positive | 10 (23.2%) | 5 (50%) | 15 (28.3%) | |
| Unavailable | 22 (51.2%) | 4 (40%) | 26 (49.1%) | |
| BMI | ||||
| Mean | 24.4 ± 4.8 | 25.4 ± 7.1 | 24.6 ± 5.24 | .59 |
| Initial radiation | ||||
| Definitive | 34 | 8 | 42 (79.2%) | .91 |
| Adjunctive | 9 | 2 | 11 (20.8%) | |
| Initial chemotherapy | ||||
| No | 15 (34.9%) | 4 (40%) | 19 (35.8%) | 1.0 |
| Yes | 28 (65.1%) | 6 (60%) | 34 (64.2%) | |
| Primary neck dissection | ||||
| No | 27 (62.8%) | 4 (40%) | 31 (58.5%) | .45 |
| Yes | 16 (37.2%) | 6 (60%) | 22 (41.5%) | |
| Primary neck dissection on side of recurrence | ||||
| No | 29 (67.4%) | 6 (60%) | 35 (66.0%) | |
| Yes | 14 (32.6%) | 4 (40%) | 18 (34.0%) | .72 |
| Time to recurrence | ||||
| Mean (years) | 5.0 ± 5 | 3.5 ± 2.7 | 4.7 ± 4.6 | .37 |
| Resection sites | ||||
| Oropharyngectomy alone | 16 (37.2%) | 3 (30%) | 19 (35.8%) | .88 |
| Additional partial/total glossectomy | 13 (30.2%) | 3 (30%) | 16 (30.2%) | |
| Additional laryngectomy | 14 (32.6%) | 4 (40%) | 18 (34%) | |
| Free flap | ||||
| No | 9 (20.9%) | 5 (50%) | 14 (26.4%) | .10 |
| Yes | 34 (79.1%) | 5 (50%) | 39 (73.6%) | |
| Recurrence T classification | ||||
| T1 | 9 (20.9%) | 1 (10%) | 10 (18.9%) | |
| T2 | 4 (9.3%) | 2 (20%) | 6 (11.3%) | .72 |
| T3 | 4 (9.3%) | 1 (10%) | 5 (9.4%) | |
| T4 | 26 (60.55%) | 6 (60%) | 32 (60.4%) | |
| Recurrence N classification | ||||
| N0 | 28 (65.1%) | 6 (60%) | 34 (64.2%) | |
| N1 | 12 (27.9%) | 2 (20%) | 14 (26.4%) | .31 |
| N2 | 3 (7%) | 1 (10%) | 4 (7.6%) | |
| N3 | 0 | 1 (10%) | 1 (1.9%) | |
| Recurrence stage | ||||
| 1 | 10 (23.2%) | 2 (20%) | 12 (22.7%) | |
| 2 | 3 (7%) | 1 (10%) | 4 (7.5%) | .49 |
| 3 | 4 (9.3%) | 1 (10%) | 5 (9.4%) | |
| 4 | 26 (60.5%) | 6 (60%) | 32 (60.4%) | |
Abbreviations: HPV, human papilloma virus; T3, triiodothyronine; T4, thyroxine.
Nineteen patients (35.8%) required oropharyngectomy alone. While the rest of patients required greater resection, including additional subtotal or total glossectomy (30.2%) or laryngectomy (34.0%). Bone resection was required in 8 patients (15.1%). A vascularized free flap was used for reconstruction in 39 patients (73.6%), local or rotational flap in 13 patients (24.5%), and primary closure in the remaining 1 patient (1.9%). When comparing patients that developed a fistula with those that did not, there was no significant difference in demographics, primary treatment, staging, surgical resection, or free-flap reconstruction (Table 1).
Risk Factors for Postoperative Hypothyroidism
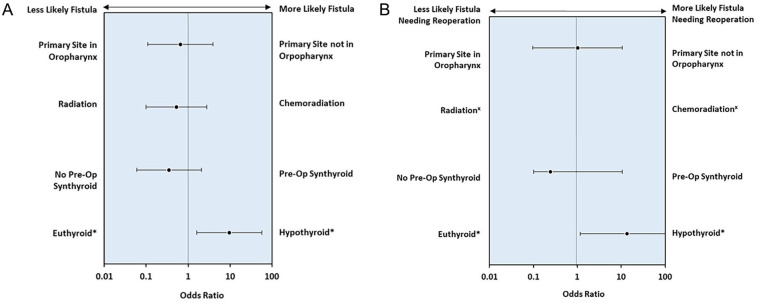
All 53 patients (100%) were biochemically euthyroid preoperatively, although 18 patients (34.0%) were taking thyroid hormone supplementation for a history of hypothyroidism. Postoperatively, 20 patients (37.7%) were hypothyroid, as evidenced by an elevated TSH. Eleven of the 20 postoperative hypothyroid patients were taking preoperative thyroid supplementation. Preoperative thyroid supplementation and primary cancer site were the only predictive factors of postoperative hypothyroidism in bivariate analysis, with a (P = .017) and (P = .004), respectively. Recurrent advanced disease and treatment with CRT were also included in the multivariate logistic model as they have historic predictive value. 27 In the model, preoperative thyroid supplementation [odds ratio (OR) 5.1, 95% confidence interval (CI) 1.2-21.8; P = .026] and primary cancer site (OR 6.5, 95% CI 1.7-25.2; P = .007) were predictive of postoperative hypothyroidism. Recurrent advanced disease (OR 2.6, 95% CI 0.5-13.4; P = .248) and treatment with CRT (OR 2.2, 95% CI 0.5-10.0; P = .3) remained insignificant (Figure 1).
Figure 1.
Factors affecting postoperative hypothyroidism. Multivariate analysis of hypothyroidism development within 30 days postoperatively, with a 95% confidence interval.
*P < .05.
Fistula and Hypothyroidism
The overall oropharyngocutaneous fistula rate in our cohort was 18.9%. In total, 5 patients (9.4%) required a reoperation to manage the fistula. Among the postoperatively-hypothyroid patients, 7 patients (35%) developed a fistula compared with only 3 patients (9.1%) of postoperatively-euthyroid patients (P = .03). Four postoperatively-hypothyroid patients (20%) developed a fistula requiring reoperation, compared with 1 euthyroid patient (3.0%; P = .061) (Figure 2). Importantly, we observed no significant difference in rates of fistula formation in patients undergoing oropharyngectomy compared with those undergoing oropharyngectomy with laryngectomy (35.8% and 34%, respectively, P = .9).
Figure 2.
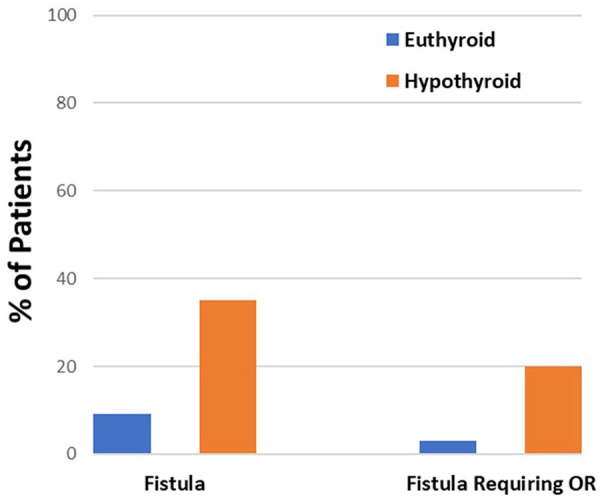
Postoperative hypothyroidism and fistula formation. Bivariate analysis of fistula and reoperation for patients with postoperative hypothyroidism compared with those for euthyroid patients.
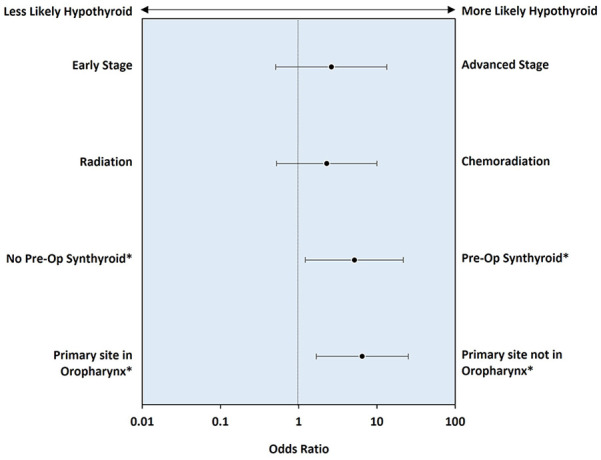
Only postoperative hypothyroidism was predictive for developing postoperative fistula (Table 2). Our multivariate logistic regression model also included primary tumor site, preoperative synthroid treatment, and CRT treatment, as these were significant in prior analysis and potentially help explain the model. In the regression model, patients who experienced postoperative hypothyroidism were at a 9.5-fold increased risk of developing a fistula (95% CI 1.6-57.0, P = .01). All other variables were not significant (Figure 3A).
Table 2.
Multivariate Model of Factors Affecting Fistula Development and Reoperation.
| Factors | Odds Ratio | P Value | 95% CI for Exp(B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| Fistula development | ||||
| Postoperative hypothyroidism | 9.560 | .013* | 1.600 | 57.123 |
| CRT | 0.523 | .445 | 0.099 | 2.755 |
| Primary site in oropharynx | 0.659 | .647 | 0.111 | 3.923 |
| Preoperative synthroid treatment | 0.345 | .247 | 0.057 | 2.096 |
| Fistula needing reoperation | ||||
| Postoperative hypothyroidism | 13.653 | .038* | 1.161 | 160.505 |
| CRT | 219,756,404.000 | .998 | 0.000 | x |
| Primary site in oropharynx | 1.018 | .988 | 0.097 | 10.716 |
| Preoperative synthroid treatment | 0.245 | .327 | 0.015 | 4.062 |
x: This variable did not have any members in one of the comparison groups, and upper CI was unmeasurable.
Abbreviations: B, constant coefficient; CI, confidence interval; CRT, chemoradiation therapy; Exp(B), exponentiation of the B coefficient/odds ratio.
P < .05.
Figure 3.
(A) Factors affecting fistula development. (B) Factors affecting fistula needing reoperation. Multivariate analysis of fistula and fistula needing reoperation with a 95% confidence interval.
x: There were no reoperation events in the chemoradiation subgroup.
*P < .05.
Only postoperative hypothyroidism was predictive for developing a fistula requiring reoperation (Table 2). However, primary tumor site, preoperative thyroid hormone therapy, and prior chemotherapy were included in the multivariate logistical regression model. In the regression model, postoperative hypothyroid patients were at 13.6-fold increased risk of developing a fistula requiring reoperation (95% CI 1.2-160.5, P = .04). All other variables were not significant (Figure 3B).
Discussion
As the incidence of HPV-associated oropharyngeal SCC continues to rise, a greater number of patients are being treated primarily with RT or CRT. These patients are at increased risk of wound complications if salvage surgical therapy is required for recurrence. Here, we report a fistula rate of 18.9% in patients undergoing salvage oropharyngectomy. Do et al reported a similar rate of 21.4% in patients treated with salvage surgery and a fistula rate of 13.3% following primary oropharyngectomy. 15 Notably, the rates of fistula formation following salvage oropharyngectomy are considerably lower than those for salvage laryngectomy, which have been reported at 35% at our institution. 27
Rosko et al identified postoperative hypothyroidism as a modifiable risk factor for fistula development following salvage laryngectomy. 27 Our current work builds upon those data and further supports that hypothyroidism is a modifiable risk factor for postoperative complications, including fistula formation and fistula requiring operative management, following salvage oropharyngeal surgery for head and neck malignancies. In their study, Rosko et al reported postoperative hypothyroidism in approximately 50% of patients following salvage laryngectomy. 27 Here, we report lower rates of hypothyroidism (37.7%) following salvage oropharyngectomy. This discrepancy is often explained by surgical technique, as a total laryngectomy often necessitates transection and/or removal of the thyroid gland. 28 However, this is not supported by our data wherein the rate of hypothyroidism in the postoperative period was not significantly different for patients who underwent a pharyngolaryngectomy (50%) compared with those whose operation did not involve the larynx (31.4%; P = .18). In our study, patients with primary tumors outside of the oropharynx were more at risk of postoperative hypothyroidism (P = .007), likely resulting from greater radiation focused on the neck and thyroid.
In this study, hypothyroidism was the only predictive factor in relation to fistula development and fistula needing reoperation. While vascularized tissue reconstruction has been shown to reduce fistula rates, we were not able to analyze its influence because all but 1 patient received reconstruction. This study helps emphasize the risk of hypothyroidism on fistula development, which is a modifiable risk factor and should be an important consideration for those aiming to improve high rates of pharyngocutaneous fistula or potentially other surgical wounds.
We acknowledge one of the weaknesses of our study is not obtaining triiodothyronine/thyroxine (T3/T4) values. It is possible that some patients were included with elevated TSH and normal T3/T4 indicating subclinical hypothyroidism. There is also some debate about whether TSH is an acute phase reactant and expected to rise in the postoperative period or in a developing fistula. 29 However, prior head and neck studies have demonstrated that TSH is only elevated in select surgical cases, and not consistent with an acute phase reactant.22,30-32 Those studies show how TSH elevation is dependent on specific surgical operations and adjuvant radiation. 30 A recent prospective trial by Heft-Neal et al 33 demonstrates that acute phase reactants such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are relatively stable after salvage laryngectomy and that TSH is increased in patients with wound complications rather than decreased as might be expected in those with an acute illness. Other studies suggest TSH could be the preferred test, as it can detect mild (subclinical) degrees of thyroid hormone excess or deficiency.34,35 In Rosko et al, they demonstrated a linear relationship between increasing TSH and fistula development, potentiating the idea that subclinical hypothyroidism may still increase fistula risk. 27 Additional studies in the field of orthopedics also show evidence that subclinical hypothyroidism can impact wound healing 36 and treatment could be considered. 37 The recent trial by Heft-Neal et al is the first to demonstrate levothyroxine supplementation engendered a significant reduction in fistula and fistula requiring operative intervention after salvage laryngectomy. 33 Our next steps are to evaluate the impact of levothyroxine supplementation on fistula rates after salvage oropharyngectomy.
We suspect physiologically that preoperative euthyroid patients developed hypothyroidism due to surgical disruption of the preradiated and fragile vasculature in the neck. In the nonsalvage setting, paratracheal lymph node dissection has been found to be an independent risk factor for postoperative hypothyroidism, with or without hemi/total thyroidectomy.30,31 Plaat et al have supported that rates of hypothyroidism are even higher in the salvage head and neck surgery setting. 32 This study supports that salvage surgery of the neck likely impacts thyroid function regardless of manipulation of the gland. Our study suggests that thyroid dysfunction after salvage surgery correlates with wound complications. It is likely that T4 or T3 would be more valuable markers of postoperative thyroid function and biochemical hypothyroidism; however, T4/T3 levels and other known acute phase reactants were not routinely monitored in this patient population, nor were comparisons studies completed. In the postoperative period, 5% of patients had a T4 level measured, 2% a T3, and only 2% had either an ESR or CRP level measured. Such is the limitation of a retrospective study. Current prospective studies, which can better evaluate the change in T4/T3 and other acute phase reactions pre- and postoperatively are currently underway at our institution.
Other limitations of this study include its retrospective nature limiting our ability to establish causation. It was also a relatively-small cohort limiting the power of the study, diminishing the utility of logistic regression for variables with small group sizes and creating large CIs. This was exemplified by our inability to evaluate the effect of vascularized tissue reconstruction. There is also the possibility of selection bias, as there was a large cohort of patients without postoperative TSH values not included in this study. The lack of postoperative TSH values was a result of providers either not knowing to order them or because they never order postoperative TSH. The cohort without postoperative TSH values did not have significantly-different demographics, rates of fistula, or fistula needing reoperation (Supplemental Table 1). The treatment of hypothyroidism was also not uniform, and we are not able to evaluate the effect of thyroid replacement. Further research is underway to determine the best acute phase thyroid markers and the most appropriate thyroid replacement protocols.
Conclusion
Postoperative hypothyroidism in patients undergoing salvage oropharyngectomy can predict complications related to wound healing, namely fistula development. Moreover, patients experiencing hypothyroidism are more likely to require operative management after fistula development. These results support previously-published work demonstrating postoperative hypothyroidism was an independent risk factor for fistula development in patients undergoing salvage laryngectomy. This study further supports the role of hypothyroidism management to improve wound healing and reduce postoperative wound complications.
Supplemental Material
Supplemental material, sj-docx-1-ohn-10.1177_19160216241296126 for Hypothyroidism Predicts Fistula Development Following Salvage Oropharyngectomy by Andrew D.P. Prince, Zachary M. Huttinger, Molly E. Heft-Neal, Steven B. Chinn, Kelly M. Malloy, Chaz L. Stucken, Keith A. Casper, Mark E.P. Prince, Matthew E. Spector and Andrew J. Rosko in Journal of Otolaryngology - Head & Neck Surgery
Acknowledgments
None.
Footnotes
Author Contributions: A.D.P.P.: design, conduct, analysis, and presentation. Z.M.H., M.E.H.-N., S.B.C., K.M.M., C.L.S., K.A.C., M.E.P.P., M.E.S., and A.J.R.: design, conduct, and analysis.
Availability of Data and Materials: The datasets generated and/or analyzed during the current study are not publicly available due private information sharing concerns but are available from the corresponding author on reasonable request.
Consent for Publication: Not applicable.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate: An institutional review board (IRB)–approved (University of Michigan IRB HUM00152046) study was performed ethically.
ORCID iD: Andrew D.P. Prince  https://orcid.org/0000-0001-9359-7739
https://orcid.org/0000-0001-9359-7739
Supplemental Material: Additional supporting information is available in the online version of the article.
References
- 1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-249. [DOI] [PubMed] [Google Scholar]
- 2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424. [DOI] [PubMed] [Google Scholar]
- 3. Du M, Nair R, Jamieson L, Liu Z, Bi P. Incidence trends of lip, oral cavity, and pharyngeal cancers: global burden of disease 1990-2017. J Dent Res. 2019;99(2):143-151. [DOI] [PubMed] [Google Scholar]
- 4. D’Souza G, Kreimer AR, Viscidi R, et al. Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356(19):1944-1956. [DOI] [PubMed] [Google Scholar]
- 5. Van Dyne EA, Henley SJ, Saraiya M, Thomas CC, Markowitz LE, Benard VB. Trends in human papillomavirus-associated cancers—United States, 1999-2015. MMWR Morb Mortal Wkly Rep. 2018;67(33):918-924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Feng FY, Kim HM, Lyden TH, et al. Intensity-modulated chemoradiotherapy aiming to reduce dysphagia in patients with oropharyngeal cancer: clinical and functional results. J Clin Oncol. 2010;28(16):2732-2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yeh DH, Tam S, Fung K, et al. Transoral robotic surgery vs. Radiotherapy for management of oropharyngeal squamous cell carcinoma—a systematic review of the literature. Eur J Surg Oncol. 2015;41(12):1603-1614. [DOI] [PubMed] [Google Scholar]
- 8. Lassen P, Eriksen JG, Hamilton-Dutoit S, Tramm T, Alsner J, Overgaard J. Effect of HPV-associated p16INK4A expression on response to radiotherapy and survival in squamous cell carcinoma of the head and neck. J Clin Oncol. 2009;27(12):1992-1998. [DOI] [PubMed] [Google Scholar]
- 9. Taneja C, Allen H, Koness RJ, Radie-Keane K, Wanebo HJ. Changing patterns of failure of head and neck cancer. Arch Otolaryngol Head Neck Surg. 2002;128(3):324-327. [DOI] [PubMed] [Google Scholar]
- 10. Zafereo ME, Hanasono MM, Rosenthal DI, et al. The role of salvage surgery in patients with recurrent squamous cell carcinoma of the oropharynx. Cancer. 2009;115(24):5723-5733. [DOI] [PubMed] [Google Scholar]
- 11. Andrews BT, Smith RB, Hoffman HT, Funk GF. Orocutaneous and pharyngocutaneous fistula closure using a vacuum-assisted closure system. Ann Otol Rhinol Laryngol. 2008;117(4):298-302. [DOI] [PubMed] [Google Scholar]
- 12. Graboyes EM, Yang Z, Kallogjeri D, Diaz JA, Nussenbaum B. Patients undergoing total laryngectomy: an at-risk population for 30-day unplanned readmission. JAMA Otolaryngol Head Neck Surg. 2014;140(12):1157-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hier M, Black MJ, Lafond G. Pharyngo-cutaneous fistulas after total laryngectomy: incidence, etiology and outcome analysis. J Otolaryngol. 1993;22(3):164-166. [PubMed] [Google Scholar]
- 14. Weber RS, Berkey BA, Forastiere A, et al. Outcome of salvage total laryngectomy following organ preservation therapy: the Radiation Therapy Oncology Group trial 91-11. Arch Otolaryngol Head Neck Surg. 2003;129(1):44-49. [DOI] [PubMed] [Google Scholar]
- 15. Do SB, Chung CH, Chang YJ, Kim BJ, Rho YS. Risk factors of and treatments for pharyngocutaneous fistula occurring after oropharynx and hypopharynx reconstruction. Arch Plast Surg. 2017;44(6):530-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Girkar F, Thiagarajan S, Malik A, et al. Factors predisposing to the development of orocutaneous fistula following surgery for oral cancer: experience from a tertiary cancer center. Head Neck. 2019;41(12):4121-4127. [DOI] [PubMed] [Google Scholar]
- 17. Makitie AA, Irish J, Gullane PJ. Pharyngocutaneous fistula. Curr Opin Otolaryngol Head Neck Surg. 2003;11(2):78-84. [DOI] [PubMed] [Google Scholar]
- 18. Nair D, Singhvi H, Mair M, et al. Outcomes of surgically treated oral cancer patients at a tertiary cancer center in India. Indian J Cancer. 2017;54(4):616-620. [DOI] [PubMed] [Google Scholar]
- 19. Marx RE. Osteoradionecrosis: a new concept of its pathophysiology. J Oral Maxillofac Surg. 1983;41(5):283-288. [DOI] [PubMed] [Google Scholar]
- 20. Colevas AD, Read R, Thornhill J, et al. Hypothyroidism incidence after multimodality treatment for stage III and IV squamous cell carcinomas of the head and neck. Int J Radiat Oncol Biol Phys. 2001;51(3):599-604. [DOI] [PubMed] [Google Scholar]
- 21. Mercado G, Adelstein DJ, Saxton JP, Secic M, Larto MA, Lavertu P. Hypothyroidism: a frequent event after radiotherapy and after radiotherapy with chemotherapy for patients with head and neck carcinoma. Cancer. 2001;92(11):2892-2897. [DOI] [PubMed] [Google Scholar]
- 22. Sinard RJ, Tobin EJ, Mazzaferri EL, et al. Hypothyroidism after treatment for nonthyroid head and neck cancer. Arch Otolaryngol Head Neck Surg. 2000;126(5):652-657. [DOI] [PubMed] [Google Scholar]
- 23. Miller MC, Agrawal A. Hypothyroidism in postradiation head and neck cancer patients: incidence, complications, and management. Curr Opin Otolaryngol Head Neck Surg. 2009;17(2):111-115. [DOI] [PubMed] [Google Scholar]
- 24. Alexander MV, Zajtchuk JT, Henderson RL. Hypothyroidism and wound healing: occurrence after head and neck radiation and surgery. Arch Otolaryngol. 1982;108(5):289-291. [DOI] [PubMed] [Google Scholar]
- 25. Talmi YP, Finkelstein Y, Zohar Y. Pharyngeal fistulas in postoperative hypothyroid patients. Ann Otol Rhinol Laryngol. 1989;98(4 Pt 1):267-268. [DOI] [PubMed] [Google Scholar]
- 26. Bohannon IA, Carroll WR, Magnuson JS, Rosenthal EL. Closure of post-laryngectomy pharyngocutaneous fistulae. Head Neck Oncol. 2011;3:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rosko AJ, Birkeland AC, Bellile E, et al. Hypothyroidism and wound healing after salvage laryngectomy. Ann Surg Oncol. 2018;25(5):1288-1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tucker HM. Total laryngectomy: technique. Oper Tech Otolayngol Head Neck Surg. 1990;1(1):42-44. [Google Scholar]
- 29. Economidou F, Douka E, Tzanela M, Nanas S, Kotanidou A. Thyroid function during critical illness. Hormones. 2011;10(2):117-124. [DOI] [PubMed] [Google Scholar]
- 30. Nassar AA, Shoaib AA, Dewidar HM, Azooz KO. Incidence of post total laryngectomy hypothyroidism: effects of thyroid gland surgery and post-operative radiotherapy. Indian J Otolaryngol Head Neck Surg. 2023;75(3):1336-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Turgut OK, Erişen L, Coşkun H, Basut O, Onart S, Hizalan I. Hypothyroidism after primary surgical treatment for laryngeal and hypopharyngeal cancer. Kulak Burun Bogaz Ihtis Derg. 2008;18(3):125-130. [PubMed] [Google Scholar]
- 32. Plaat RE, van Dijk BAC, Muller Kobold AC, et al. Onset of hypothyroidism after total laryngectomy: effects of thyroid gland surgery and preoperative and postoperative radiotherapy. Head Neck. 2020;42(4):636-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Heft-Neal ME, Haring CT, Bellile E, et al. Phase II clinical trial of intravenous levothyroxine to mitigate pharyngocutaneous fistula in euthyroid patients undergoing salvage laryngectomy. Clin Cancer Res. 2024;30(14):2910-2916. [DOI] [PubMed] [Google Scholar]
- 34. Ladenson PW, Singer PA, Ain KB, et al. American Thyroid Association guidelines for detection of thyroid dysfunction. Arch Intern Med. 2000;160(11):1573-1575. [DOI] [PubMed] [Google Scholar]
- 35. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489-499. [DOI] [PubMed] [Google Scholar]
- 36. Jing W, Long G, Yan Z, Ping Y, Mingsheng T. Subclinical hypothyroidism affects postoperative outcome of patients undergoing total knee arthroplasty. Orthop Surg. 2021;13(3):932-941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Calissendorff J, Falhammar H. To treat or not to treat subclinical hypothyroidism, what is the evidence? Medicina. 2020;56(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-ohn-10.1177_19160216241296126 for Hypothyroidism Predicts Fistula Development Following Salvage Oropharyngectomy by Andrew D.P. Prince, Zachary M. Huttinger, Molly E. Heft-Neal, Steven B. Chinn, Kelly M. Malloy, Chaz L. Stucken, Keith A. Casper, Mark E.P. Prince, Matthew E. Spector and Andrew J. Rosko in Journal of Otolaryngology - Head & Neck Surgery