Abstract
Purpose: A routine preoperative assessment is considered both ineffective and inefficient. Despite the widespread application of lean thinking in healthcare, there is little evidence of successful experiences in preoperative admissions in order to reduce “No value added” activities. A conceptual framework reporting the drivers (clinic, tools, innovation, organization, and governance) and impacts (patient, efficiency, sustainability, time, learning and growth) was developed. Methodology: Drawing on the experience of an Italian high complexity hospital, this paper analyzes the case study by reporting evidence on how to implement lean in preoperative assessment and how to evaluate the positive results obtained. Results: Applying lean principles, the identification of value improved the appropriateness of care by creating 40 personalized pathways; the value stream resulted in a reduction of “No Value Added Time” from 37% to 28%, chest X-rays from 41% to 14% and cardiac visits from 49% to 37%; the pursuit of continuous flow through innovation contributed to increase the use of digitalization; the new pull organization helped to reduce the average time spent per year by 1.5 h; the continuous improvement was ensured through the governance of results. Conclusion: The proposed framework should be used to improve the quality of care in preoperative admissions by adopting the lean drivers for successful implementation and reporting the impacts.
Keywords: Lean healthcare, preoperative assessment, quality improvement, value time
Introduction
The necessity of undergoing a preoperative assessment (PA), i.e., “the clinical investigation that precedes anaesthesia for surgical or non-surgical procedures” 1 (p. 1749) is a crucial step of the entire peri-operative pathway. The preoperative evaluation consists in a complex hospital activity that involves a huge number of patients.
Garcìa-Miguel and colleagues, claiming the relevance of PA stated “thorough clinical PA of the patient is more important than routine preoperative tests, which should be requested only when justified by clinical indications” 1 (p.1749). There is a large debate on routine tests in PAs with the evidence that claims multiple negative effects, when routines are not clinically required, on both patients' comfort and healthcare providers’ efficiency. 2
Removing unnecessary activities in order to improve the value for patients and optimize flows and processes is in line with the principles of lean management. Lean is an improvement approach widely used by healthcare organizations 3 worldwide to deliver high quality services, create value from a patient-centered point of view and try to remove “No Value Added” (NVA) activities, i.e., those services/tests for which people are not willing to pay. 4
According to the literature, there is a wide research on lean management adoption in the operating room. 5 However, although the relevance of the PA within the entire peri-operative pathway for improving both patients’ health outcomes and the organization’s efficiency, very few studies addressed the implementation of the lean methodology to specifically improve this complex service.6–8 There is a lack of evidence framing guidelines on how to “lean” PA according to lean thinking, defining the drivers for an improvement re-organization. 9
According to the evidence on preoperative routine assessment and moving from these research gaps, a high complex research and academic hospital located in the North of Italy, dealing with a preoperative organization characterized by routines tests for all patients, queues, delays, discomfort both for patients and healthcare personnel and, thus, inefficiencies, and activities without value for patients, decided to implement and carry on an improvement project aimed at increasing the quality of care and reducing waste in this hospital activity.
The hospital setting analyzed within the scope of this study represents an excellence both at national and international level for its competence in lean management. It counts more than 10 years of experience with lean principles adoption, reaching a hospital-wide implementation (more than 250 projects implemented), with a disseminated culture of quality improvement and an overall engagement of personnel (1031 people trained until 2021) on lean techniques and methodology (i.e., administrative staff, physicians, nurses, and other health professionals such as physiotherapists, technics of radiotherapy). It was one of the first hospitals to have re-organized the entire PA according to lean management, representing a best practice for healthcare organizations worldwide.
Thus, the aim of this work is to give evidence on how to implement lean management in the PA and how to assess the results obtained, by providing a conceptual framework that follows lean principles. The organizational transformation reported through a case study provides insights for applications of the framework in other hospital settings.
Theoretical background
Lean management emerged from manufacturing industries, 10 in the Toyota Production System. The five principles of lean are: (i) the identification of value from the customers’ perspective; (ii) the understanding of the value stream; (iii) the identification and improvement of the process flow; (iv) the adoption of a “pull” logic; (v) continuous improvement to achieve perfection. It was adopted in the healthcare sector to reduce waste (Muda), thus improving processes, reaching a widespread diffusion within hospitals operations worldwide. 11 Although the potential of lean management in healthcare, evidence still highlights a lack of systematic adoption, fully developing the methodology, and of frameworks able to capture the systemic nature of lean implementation at hospital level and report the related impacts. 12
Recent studies have tried to provide general frameworks to support both the implementation of lean management and the evaluation of the impacts. For example, Barberato Henrique and colleagues identified a lean healthcare assessment framework based on three levels – tools, methods and people – in order to ensure the sustainability of lean initiatives’ impacts. 13 Analyzing multiple case studies, Centauri and colleagues derived a conceptual framework composed by both social (i.e., structure and people) and technical (i.e., technology and production processes) components and including also the influence of the external context. 14
Recently, Marsilio and Pisarra 15 provided a theoretical framework through a meta-review that embraces the socio-technical drivers that support both quality improvement practices at organizational level and the lean implementation process. Some studies tried to focus on specific applications. Sales-Coll presented a consolidated model that allowed to improve both the overall efficiency in operation rooms and the patients’ perceived value. 16 However, to the extent of our knowledge there is no evidence of lean implementation frameworks in the PA. Shah and Ward defined lean production as “an integrated socio-technical system whose main objective is to eliminate waste”. 17 Moving from the evidence of previous works, the present paper aims at analyzing how to implement lean management in the PA (i.e., which are the main areas of intervention - “driving pillars”), and how to assess the impacts, by providing a conceptual socio-technical framework.
The theoretical framework
The frame proposed took inspiration from previous works, particularly, from the study of Marsilio and Pisarra (2021) (Table 1). Nevertheless, it was adapted to the specificities of the case study presented and, particularly to PA’s characteristics.
Table 1.
PA Socio-technical Dimensions and impacts.
| PA lean socio-technical drivers and impacts | Marsilio and Pisarra (2021) lean socio-technical dimensions and impacts | |
|---|---|---|
| Social dimension | Culture of quality | Organizational culture |
| Social dimension | Clinical pillar | Organizational structure |
| Impact | Patient | Patient |
| Technical dimension | Lean tools | Techniques and tools |
| Impact | Efficiency | Financial/Internal process |
| Technical dimension | Innovation | Layout |
| Impact | Sustainability | Learning and growth |
| Technical dimension | Organization | Techniques and tools |
| Impact | Times | Internal process |
| Social dimension | Governance | Strategic management/Organizational culture |
| Impact | Learning & growth | Learning and growth |
All the socio-technical dimensions were included. The external context was not considered since the framework includes only in-hospital components for lean implementation.
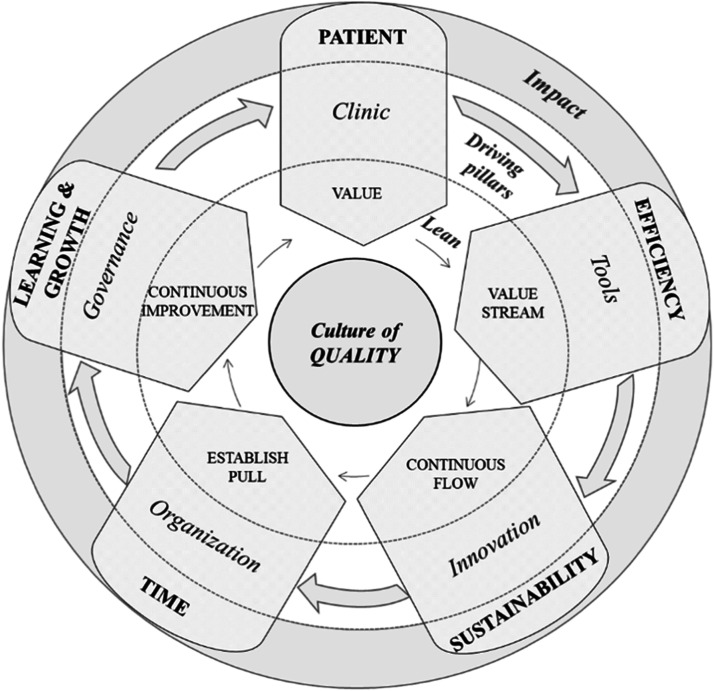
The implementation framework is reported in Figure 1 by aligning the success factors and impacts to the five lean principles.
Figure 1.
The conceptual PA framework for lean implementation and impacts control.
The central aspect is the organizational culture of quality. Lean implementation requires the creation of a continuous improvement culture. The simple application of lean tools to processes does not exploit the potential of lean principles in a holistic perspective. 18 Moreover, the organizational lean culture should be oriented towards the education and training, motivation, and engagement of employees. 19
The pillars and the related impacts are summarized as follows:
⁃ VALUE IDENTIFICATION. The clinic pillar involves both identifying value and stratifying risks. Within this phase, the engagement of clinicians is fundamental to eliminate routine PAs. 1 Frontline staff should be empowered and trained to identify and address problems: the people doing the work are the best suited to create solutions. 20 Impacts are attributed to patients: i.e., health outcomes, improved appropriateness, and patient value.
⁃ VALUE STREAM. Lean tools, such as the Value Stream Map, enable the creation of the value stream and identification of both “Value” activities and non-value-added activities, i.e., those that do not contribute to an efficient care. From the hospital's perspective, the impacts of using lean tools are related to the waste reduction and improvement of the efficiency. 21
⁃ CREATE FLOW. In order to achieve the continuous flow of processes, innovation can be used to introduce new technologies and procedures. Digital technologies combined with lean can improve flows. 22 The introduction of technologies and innovation allows the sustainability of the organization and the engagement of personnel. 23
⁃ ESTABLISH PULL. At an organizational level, lean management re-organizes processes to implement a pull logic. The application of tools to redesign pathways is fundamental and has positive results on both quality of care and efficiency and, thus, on the reduction of waiting times. 24
⁃ CONTINUOUS IMPROVEMENT. Governance should drive a functional system of performance management. Gonçalves Pinheiro and Misaghi proposed a pyramidal multiple level lean governance framework (for IT enterprise) related to lean principles. 25 The impacts encompass the growth and education of the staff and the organization. 19
Methods
Most of the studies reported in literature provide lean implementation evidence in hospital settings based on real case studies. 26 This work adopts a qualitative approach, based on the case study methodology. 27 Particularly, it is a longitudinal-explanatory single-case study. This methodology was adopted to fully consider the complexity of the context in which the lean initiative occurred. It is also able to “illuminate a decision or a set of decisions: why they were taken, how they were implemented, and with what results” 27 (p.12)
Study setting
The transformation initiative involved a research, hospitalization and healthcare scientific institute organization located in the North of Italy. Preoperative admissions average 110 patients per day.
The hospital investigated provides insights thanks to its expertise and diffused lean culture within the overall organization. The requirements suggested in this work are also those to which healthcare organizations worldwide are going through in the wake of the COVID-19 pandemic (e.g., digitalization). The problem related to routine preoperative assessments is investigated within the international literature 1 and the presented lean model might be scaled-up in the preoperative admissions of other national and international hospital settings. Accordingly, NICE guidelines firstly suggested the model. 28
Data collection
Data collection used multiple sources, i.e., archival data (internal clinical database, organizational records with flow chart and protocols), documents (minutes of meetings, written reports of events, administrative documents), and direct observations by attending the 15 multidisciplinary groups’ meetings (i.e., 5 h per group for a total of 75 h) that allowed for the construction of the personalized preoperative pathways, with the aim of improving data validity through triangulation.
The study observed a sample of patients over a period of 3 years, with 14,466 patients in 2019, 9,419 patients in 2020, and 14,091 patients in 2021.
Results
Case study design
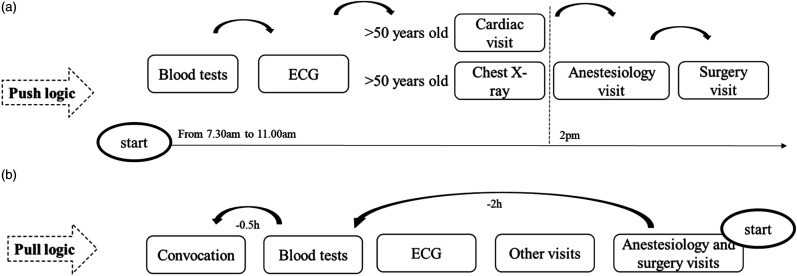
Before the re-organization through lean methods, the PA consisted in routines, decided by each clinical unit. All patients in had blood tests, with appointments from 7.30 a.m. to 11.00 a.m. and ECG tests. The other visits were organized with age routines i.e., cardiac visits and chest X-rays for all the patients over 50 years old. Starting from 2 p.m. till 7 p.m., preoperative was completed by the anesthesiology and surgery visits. The project, studied in 2019, was implemented in January 2020.
How to implement lean management in the preoperative assessment
Enabling factor
Culture of quality
Lean thinking principles were diffused by the hospital’s leadership that has been always focused on ensuring a culture of continuous improvement. Education and training have been also promoted. A multidisciplinary core team, composed by the Quality Manager, the anesthesiologists’ Department Director and the Operations Manager, met 15 clinical groups to discuss how to review preoperative pathways to add quality, include innovation and grant sustainability. 15 multidisciplinary groups (representing the different units) were created.
Driving pillars
Value
Clinic
Evidence-based medicine (EBM) drove the beginning of the project particularly from the need to reduce complications and adversities 29 and improve patients’ outcomes.
A multidisciplinary team followed NICE guidelines 28 to identify the patients’ risk and procedures’ severity. A “patient-centered” perspective was adopted for the stratification of the PA's pathways, by analyzing which tests and visits could be considered with value for patients.
Value stream
Lean tool
The team introduced the concept of “Value Time” as the time spent for activities, medical visits, and tests during the PA without waiting and waste of time.
Focusing on value, the multidisciplinary groups:
⁃ eliminated the “No Value Added” activities (i.e., routine tests based on the age were considered waste), and
⁃ defined which “Value Added” activities must be included for each surgery.
Continuous flow
Innovation
Technology was a fundamental driver for lean implementation to ensure continuous flows. A continuous flow was ensured through the following steps: (i) the computerization of the hospitalization proposal, (ii) the surgery planning was scheduled based on the stratification of patients by the administrative offices, and (iii) a change in the physical space of the PA with the possibility of choosing between the hospital setting and innovative options, e.g., “tele preoperative”.
Establish pull
Organization
It was necessary to move from a push logic (Figure 2(a)) to a pull logic, where the pre-operative assessment was conducted by the anesthesiology and surgery visits. The PA was re-organized with a patient’s convocation depending on the anesthesiology and surgery visits (Figure 2(b)). In this way, the anesthesiologists can conclude their consultation in a day.
Figure 2.
PA before (a) and after (b) the re-organization.
Continuous improvement
Governance
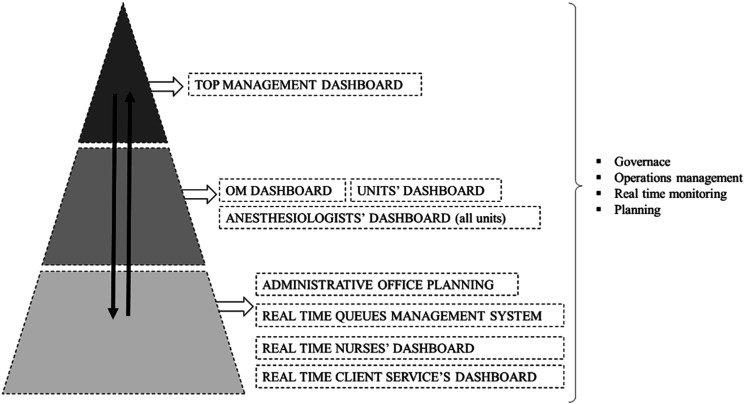
Another relevant driver is represented by the governance of results for both the project and the future operability. The 15 teams identified a pyramid system of dashboards, thus creating a preoperative performance management model (PPMM) with a strategic vision and a drill down logic (Figure 3).
Figure 3.
The preoperative performance management model (PPMM) – a pyramid system of dashboards.
How to assess the impacts of lean management implementation in the preoperative assessment
Impacts
Patient
Despite this study does not assess clinical health outcomes, some positive results are reported also in the patient’s sphere.
The clinical contribution allowed to increase appropriateness of care (identifying the right clinical pathway for each patient). Through the stratification according to the clinical risk and the surgery, 40 preoperative pathways were identified. Patients receive only the appropriate tests and visits according to their clinical condition and the surgical intervention programmed.
Efficiency
The reduction of those activities without value for patients or the organization as well as the related reduction of the “No value added” time were used as proxy of efficiency. Consistently, the use of Chest X-rays was reduced from about 41% in 2019 to 14% in 2021 (only revised units) and cardiac visits decreased from 49% in 2019 to 37% in 2021 (decreasing overproduction).
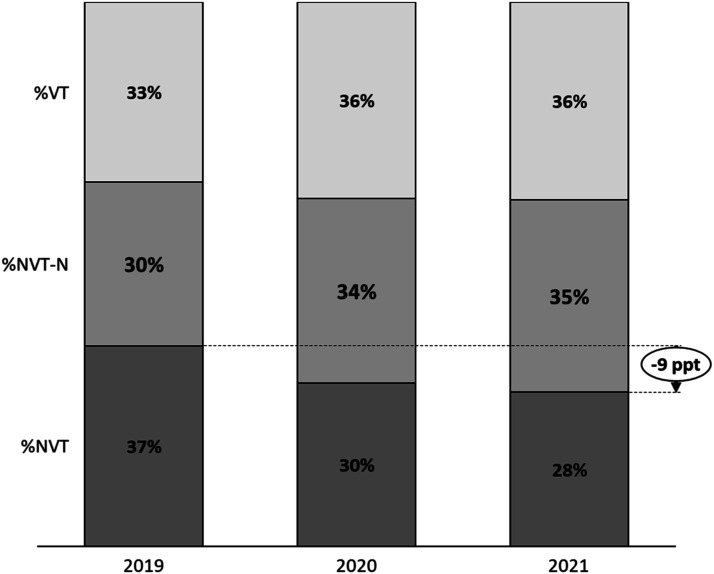
Figure 4 shows the percentage of Value Time, No-Value Time-Necessary and No-Value Time on Total Time during 2019, 2020 and 2021. Considering all the units and only the day of the “standard” PA (days dedicated to additional tests were excluded), VT increased from 33% in 2019 to 36% and to reduce NVT from 37% in 2019 to 28%, during 2021.
Figure 4.
% of TV, NVT-N and NVT during 2019, 2020 and 2021.
Sustainability
The hospital achieved pioneering status in the field of “tele-preoperative” procedures, with 2500 instances implemented in the year 2021. This initiative led to enhanced empowerment of both personnel and processes. The implementation of computerized systems, particularly for hospitalization proposals, yielded not only positive clinical outcomes but also notable sustainability benefits. These benefits included improved availability of data and hospitalization proposals, the elimination of paper-based documentation, and the reduction of duplicate records. By the year 2021, a total of 2298 hospitalization proposals had been successfully transitioned to the computerized system.
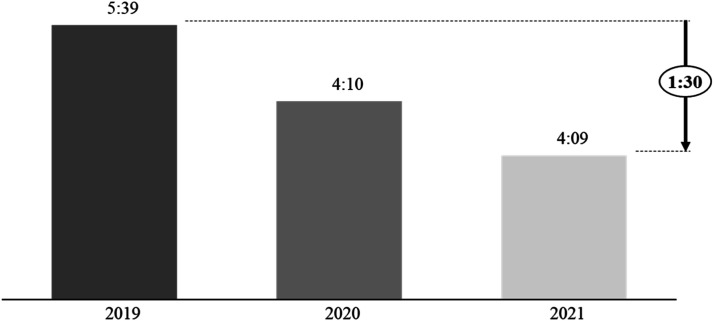
Time
The pull logic allowed reduce the length of stay and waiting times perceived by patients as waste of time. From 2019 to 2021, the average time spent by patients in PA decreased. Considering all the units and only the day of the “standard” PA, the average hours spent per year were reduced from 5:39 h in 2019 to 4:09 h in 2021, with 1:30 h less (Figure 5).
Figure 5.
Average time spent by patients for PA.
Learning and growth
The PPMM allowed to monitor and discuss about PA’s performance, thus ensuring continuous improvement and planning. It enabled to give top-down feedbacks, but also to obtain monthly bottom-up suggestions for improvement, with a continuous exchange. During the first 12 months the multidisciplinary groups met 1 h per month, and thereafter twice a year, to discuss the results.
Discussion
The PA is a crucial service in healthcare organizations worldwide. An efficient and effective functioning is fundamental to ensure the correct management of surgical patients, influencing the entire peri-operative pathway.
Despite the suitability of lean methods and philosophy implementation with PA’s problem solving, literature about its application in this field is scarce. This work stands out as the first providing a theoretical framework to implement a lean re-organization in PAs with a socio-technical approach. Differently from previous literature reviews and case studies, it represents the first work with a single application to PA, it provides a socio-technical framework with pillars and impacts related to the model of lean principles, it draws from a real and concrete implementation in a hospital setting, thus contributing to the literature on lean management implementation. Consistently, positive impacts (reported with qualitative and quantitative measures) have been obtained in all the areas. Moreover, it contributes suggesting that innovation favors sustainability, 23 and that the re-organization of the PA can be itself a driver of innovation by facilitating the adoption of new working methods, such as “tele preoperative”.
Lean is a tools-based approach 30 and the PA’s re-organization used lean tools to increase the sustainability of results. However, the presented case suggests that the hospital embraced a holistic lean implementation within an organizational culture of quality improvement.18,19 Continuous improvement contributes to staff education/growth, and organizational learning. 19 The re-organization had a patient-centered focus both from a clinical (i.e., necessary medical tests) 1 and organizational perspective (i.e., reduced waiting times). 24
In February 2020, the pandemic completely changed the hospital life and increased the treated patients’ complexity. The PA re-organization was a driver also during SARS-COV-2. This led to less time spent in hospital with less risk of infections, especially due to COVID-19.
Moreover, one of the novelties of lean implementation in the PA is that this hospital function cannot be considered as a single-process adoption. Preoperative admissions include several different surgical units and pathways according to the specific surgical interventions. For this reason, embracing lean adoption in this complex service requires a holistic, hospital-wide approach.
Limitations of this study are due to the complexity of detecting and analyzing all the relevant outcomes and providing indicators. Despite triangulation was used, further research should deepen the clinical outcomes and use different data collection methodologies such as interviews or surveys to provide data for more accurate statistical analysis. Efficiency data, such as costs, should be further analyzed. Moreover, the results are based on a single hospital setting. To generalize the model, other studies should test the framework.
Practical implications
This work provides a framework to implement a lean re-organization with a socio-technical approach. It provides a validation of the framework through a real single case-study. A circular model, able to connect each lean principle to a concrete driver for lean implementation and an outcome measure to report results, is provided. The pillars identified should drive successful re-organizations in PAs through lean principles.
This study also suggests that all the improvements must be supported by a culture of quality, shared by everyone in the healthcare organization.
Acknowledgments
The authors thank Prof. Maurizio Cecconi for the clinical conceptualization and the anesthesiology team for the support. We are grateful to surgeons for their collaboration. Thanks to nurses, cardiologists, all clinical consultants, operations management team, statistical office, customer service, medical direction for the support in the implementation phase. Special appreciations to the IT and clinical flows office. Thanks to Hospital Direction for the commitment. The authors acknowledge Professor Marta Marsilio of the University of Milan for her helpful support and comments in the draft’s revision.
Footnotes
Contributions: All authors have read and approved the manuscript. The authors’ contributions are the following: GG: conceptualized project, conceived the study, methodology, writing, data analysis and review; MP: scientific supervision, conceived the study, methodology, data analysis, writing, review and editing; PM: conceptualized project, conceived the study and review and MRC: data analysis and review.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Giulia Goretti https://orcid.org/0000-0003-4241-2540
References
- 1.García-Miguel F, Serrano-Aguilar P, López-Bastida J. Preoperative assessment. Lancet 2003; 362(9397): 1749–1757. Available at: https://www.jaypeedigital.com/book/9789351521792/chapter/ch3 [DOI] [PubMed] [Google Scholar]
- 2.O’Neill F, Carter E, Pink N, et al. Routine preoperative tests for elective surgery: Summary of updated NICE guidance. BMJ 2016; 354: 1–4. Available at: 10.1136/bmj.i3292 [DOI] [PubMed] [Google Scholar]
- 3.Radnor ZJ, Holweg M, Waring J. Lean in healthcare: The unfilled promise? Soc Sci Med 2012; 74(3): 364–371. Available at: https://linkinghub.elsevier.com/retrieve/pii/S0277953611000979 [DOI] [PubMed] [Google Scholar]
- 4.Hallam CRA, Contreras C. Lean healthcare: scale, scope and sustainability. Int J Health Care Qual Assur 2018; 31(7): 684–696. [DOI] [PubMed] [Google Scholar]
- 5.Coffey C, Cho ES, Wei E, et al. Lean methods to improve operating room elective first case on-time starts in a large, urban, safety net medical center. Am J Surg 2018; 216(2): 194–201. Available at: https://linkinghub.elsevier.com/retrieve/pii/S0002961018302678 [DOI] [PubMed] [Google Scholar]
- 6.Fiorillo A, Sorrentino A, Scala A, et al. Improving performance of the hospitalization process by applying the principles of lean thinking. TQM J 2021; 33(7): 253–271. Available at: https://www.emerald.com/insight/content/doi/10.1108/TQM-09-2020-0207/full/html [Google Scholar]
- 7.Franklin J, Franklin T. Improving preoperative throughput. J PeriAnesthesia Nurs 2017; 32(1): 38–44. Available at: https://linkinghub.elsevier.com/retrieve/pii/S1089947215004645 [DOI] [PubMed] [Google Scholar]
- 8.Ali KAG, Haaen R, Ibrahim RAES, et al. Effect of lean management strategies on the quality of perioperative nursing roles. Egypt J Heal Care 2020; 11(3): 431–454. Available at: https://ejhc.journals.ekb.eg/article_119025.html [Google Scholar]
- 9.Torabi SA, Pour SH, Shamsi GN. Lean healthcare. In: Operations Research Applications in Health Care Management. Cham: Springer, 2018, pp. 543–568. Available at: http://link.springer.com/10.1007/978-3-319-65455-3_21 [Google Scholar]
- 10.Radnor ZJ, Holweg M, Waring J. Lean in healthcare: The unfilled promise? Soc Sci Med 2012; 74(3): 364–371. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0277953611000979 [DOI] [PubMed] [Google Scholar]
- 11.D’Andreamatteo A, Ianni L, Lega F, et al. Lean in healthcare: A comprehensive review. Health Pol 2015; 119(9): 1197–1209. Available at: https://linkinghub.elsevier.com/retrieve/pii/S0168851015000366 [DOI] [PubMed] [Google Scholar]
- 12.Antony J, Sunder MV, Sreedharan R, et al. A systematic review of lean in healthcare: a global prospective. Int J Qual Reliab Manag 2019; 36(8): 1370–1391. [Google Scholar]
- 13.Henrique DB, Filho MG, Marodin G, et al. A framework to assess sustaining continuous improvement in lean healthcare. Int J Prod Res 2021; 59(10): 2885–2904. Available at: DOI: 10.1080/00207543.2020.1743892. [DOI] [Google Scholar]
- 14.Centauri F, Mazzocato P, Villa S, et al. System-wide lean implementation in health care: A multiple case study. Heal Serv Manag Res 2018; 31(2): 60–73. Available at: http://journals.sagepub.com/doi/10.1177/0951484818768226 [DOI] [PubMed] [Google Scholar]
- 15.Marsilio M, Pisarra M. Lean management in health care: a review of reviews of socio-technical components for effective impact. J Health Organ Manag 2021; 35(4): 475–491. Available at: https://www.emerald.com/insight/content/doi/10.1108/JHOM-06-2020-0241/full/html [DOI] [PubMed] [Google Scholar]
- 16.Sales-Coll M, de Castro R, Hueto-Madrid JA. Improving operating room efficiency using lean management tools. Prod Plan Control, 2021; 23: 1–14. Available at: https://www.tandfonline.com/doi/full/10.1080/09537287.2021.1998932 [Google Scholar]
- 17.Shah R, Ward PT. Defining and developing measures of lean production. J Oper Manag 2007; 25(4): 785–805. Available at: http://doi.wiley.com/10.1016/j.jom.2007.01.019 [Google Scholar]
- 18.Poksinska B. The current state of lean implementation in health care. Qual Manag Health Care 2010; 19(4): 319–329. Available at: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00019514-201010000-00007 [DOI] [PubMed] [Google Scholar]
- 19.Al-Balushi S, Sohal AS, Singh PJ, et al. Readiness factors for lean implementation in healthcare settings – a literature review. .J Health Organ Manag. In: Sloan AF, Kathryn JT. (eds), 2013; 28: 135–153. Available at: https://www.emerald.com/insight/content/doi/10.1108/JHOM-04-2013-0083/full/html [DOI] [PubMed] [Google Scholar]
- 20.Dellve L, Strömgren M, Williamsson A, et al. Health care clinicians’ engagement in organizational redesign of care processes: The importance of work and organizational conditions. Appl Ergon 2018; 68: 249–257. [DOI] [PubMed] [Google Scholar]
- 21.Leksic I, Stefanic N, Veza I. The impact of using different lean manufacturing tools on waste reduction. Adv Prod Eng Manag 2020; 15(1): 81–92. Available at: http://apem-journal.org/Archives/2020/Abstract-APEM15-1_081-092.html [Google Scholar]
- 22.Tlapa D, Tortorella G, Fogliatto F, et al. Effects of lean interventions supported by digital technologies on healthcare services: a systematic review. Int J Environ Res Public Health 2022; 19(15): 9018. Available at: https://www.mdpi.com/1660-4601/19/15/9018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Balta M, Valsecchi R, Papadopoulos T, et al. Digitalization and co-creation of healthcare value: A case study in occupational health. Technol Forecast Soc Change 2021: 168; 120785. DOI: 10.1016/j.techfore.2021.120785. [DOI] [Google Scholar]
- 24.Trakulsunti Y, Trakoonsanti L. The use of Lean tools to reduce inpatient waiting time in a Thai public hospital: an action research study. Leadersh Heal Serv 2021; 34(2): 84–97. [DOI] [PubMed] [Google Scholar]
- 25.Pinheiro MG, Misaghi M. Proposal of a framework of lean governance and management of enterprise IT. In: Proceedings of the 16th International Conference on Information Integration and Web-based Applications & Services. New York, NY, USA: ACM, 2014: 554–558. Available at: https://dl.acm.org/doi/10.1145/2684200.2684367 [Google Scholar]
- 26.Rosa A, Marolla G, Lega F, et al. Lean adoption in hospitals: the role of contextual factors and introduction strategy. BMC Health Serv Res 2021; 21(1): 889. Available at: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-021-06885-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yin RK. Case study research: Design and methods. 3rd ed, Thousand Oaks, CA, USA: Sage Publications, 2003. [Google Scholar]
- 28.National Institute for Health and Care Excellence. Available at: https://www.nice.org.uk/guidance/ng45/resources/colour-poster-pdf-2423836189
- 29.Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 2005; 242(3): 326–343. Available at: https://journals.lww.com/00000658-200509000-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parkhi SS. Lean management practices in healthcare sector: a literature review. Benchmarking An Int J 2019; 26(4): 1275–1289. Available at: https://www.emerald.com/insight/content/doi/10.1108/BIJ-06-2018-0166/full/html [Google Scholar]