Abstract
Background: Effective hospital discharge planning is crucial, particularly in educating caregivers on handling medical devices. This education helps manage the patient’s signs and symptoms, prevents post-discharge complications, and reduces early readmissions. This study aimed to understand aspects involved in the acquisition of mastery by home caregivers, in handling care of a patient who just underwent gastrostomy, after educational intervention during hospitalization and telemonitoring upon return home. Methods: Qualitative descriptive study. It followed 15 caregivers of people with percutaneous endoscopic gastrostomy. The intervention took place between November 2022 and July 2023 in the neuromusculoskeletal unit of a Brazilian university hospital. Results: The educational intervention had four stages. In stage 1, caregivers felt confused and uncertain about managing PEG. By stage 2, they expressed a desire to be capable of handling care, especially in the event of potential complications, and showed increased awareness and engagement. Stage 3 highlighted the effectiveness of hands-on training with feedback from professionals. In stage 4, during monitoring, several complications were noted, including granuloma formation in the stoma, tube obstruction, and accidental tube loss. However, caregivers demonstrated the ability to handle these situations, indicating the effectiveness of the training and telemonitoring interventions. Conclusions: Nursing professionals should consider various factors when training caregivers in a hospital setting, including providing adequate space, allocating sufficient time for educational interventions, offering both theoretical and practical demonstrations, ensuring effective communication, and taking into account the caregivers’ context, as they play a direct role in acquiring a safe and effective skill set.
Keywords: gastrostomy, hospitalization, hospital to home transition, family caregiver
1. Introduction
Percutaneous endoscopic gastrostomy (PEG) is a minimally invasive surgical procedure where a catheter is inserted directly into the stomach for feeding. It is widely recommended for use when long-term enteral nutrition is required, due to inadequate oral intake, which may occur due to neurological conditions affecting swallowing, such as stroke, motor neuron disease, and demyelinating diseases, among others [1,2].
The benefits of this device include ease of insertion, shorter hospitalization time, early start of nutritional support, better cost-effectiveness, and safety during feeding. However, complications can occur when specific guidance is not provided to the patient/caregiver for handling, such as adequate care and management, aiming at continuity at home [3].
The most common complications are mechanical and related to catheter obstruction, leakage related to stoma hypergranulation [4], and buried bumper syndrome, an uncommon adverse event, resulting from the tight positioning of the “pulley”, the external structure of the PEG tube, against the abdominal wall, causing swelling, erythema of the surrounding tissues, leaks around the tube, resistance and/or abdominal pain with the infusion of food [5]. Problems related to the gastrointestinal tract itself, such as nausea, vomiting, increased gastric residual volume, abdominal distension, diarrhea, and infection at the site of the surgical wound are also mentioned [6,7].
Furthermore, there may also be accidental loss of the tube, resulting in closure of the stoma and the need for a new approach. In the case of people dependent on the public health system, this demand causes and intensifies serious problems, such as when they need to return to the hospital for a new treatment. Stoma closure can occur between 24 and 72 h; however, this occlusion, in some cases, can occur between four and eight hours [8,9].
For this reason, health professionals must manage discharge, implementing transitional care from the moment the PEG is indicated, with support from the multidisciplinary team, with the nurse as the protagonist. In this care, assertive guidance and health education for affected people and/or their caregivers are necessary, through training in handling the tube, recognition and management of complications that can be referred and/or handled by the caregiver, skin care, and oral hygiene (regardless of whether or not the oral diet is maintained), as many people may be bedridden and need continued care.
Such actions are essential, as caregivers of people using PEG have problems due to the lack of training post discharge and express difficulties in dealing with onerous responsibilities related to food and stoma care at home [6,10].
Therefore, preparing these people for continuity of care is important, especially in the Brazilian context, where there is difficulty in providing support in primary care, with limited coverage of Primary Health Units (UBS) and Family Health Units (USF) for clarification of residual doubts that arise after returning home and assistance in the face of possible complications [11,12]. Preventable adverse events directly impact the quality and continuity of care and, consequently, early (re)hospitalizations [6,13]. Training throughout hospitalization and follow-up after discharge raise awareness and engagement, which are important properties that help in the acquisition of mastery [14,15].
Mastery is an important result indicator, characterized by the mastery of new skills and the ability to manage situations in the new context of intense transformations. Mastery is supported by self-confidence, the ability to make decisions, and knowledge and cognitive ability. It also depends on personal characteristics, formal and informal supports, situational awareness and engagement to adapt. These elements influence a smooth transition from hospital to home, providing continuity of care [16].
Fundamental points must be identified so that they can be addressed and enhanced in health education during hospitalization, while also considering the relevance of ongoing education for the care team, whose view must go beyond hospitalization, valuing life contexts for understanding and adequate training based on individual needs.
Therefore, the objective of the study was to understand aspects involved in the acquisition of mastery, by home caregivers, of handling gastrostomy care after an educational intervention during hospitalization and telemonitoring upon the return home.
2. Materials and Methods
2.1. Design and Setting
This is a descriptive and qualitative study whose interest was to understand the aspects related to the phenomenon of “acquisition of mastery by caregivers in continued care with gastrostomy, after educational practices during hospitalization and telemonitoring upon returning home”.
The scope of mastery was considered to be the development of skills to provide routine care, the interpretation of basic signs and symptoms of complications and skin injuries in contact with the device, the development of skills and abilities for decision-making in the face of complications, and the need to request help from members of the monitoring team and/or health services to search for information and resolve doubts.
The situations reported and discussed here refer to follow-ups between November 2022 and July 2023 in the neuromusculoskeletal unit of a large public university hospital, a reference in medium and high complexity care, whose services occur exclusively through the Brazilian Public Health System (SUS) [17].
2.2. Population
The researchers selected the sample from a university research and extension project that monitors high-dependency people, according to the Fugulin scale classification [18], and their family members/caregivers during hospitalization and after discharge through telemonitoring, considering caregivers who met the following inclusion criteria: (1) caregivers of adults or older people with gastrostomy who were discharged from the hospital to their home; (2) those who were present, during hospitalization, for health education carried out by the project team; and (3) those who did not have continuous formal support for carrying out PEG care. As a result, 15 caregivers met the inclusion criteria for this research.
2.3. Information about the Fugulin Scale and Academic Project
The Fugulin scale, developed and validated by a Brazilian nurse, is a tool used in the context of Brazilian health services to assess the level of nursing care required by hospitalized patients. The scale evaluates various aspects of patient dependence, including mental status, oxygenation, vital signs, motility, ambulation, feeding, body care, elimination, and therapy [18].
The main project aimed to identify the individual and specific needs of highly dependent individuals (adults and older people), as well as the needs of their family members and other caregivers. The objective was to plan the transfer of care to the patient’s home, with subsequent monitoring for three months after discharge. The monitoring plan involved weekly calls in the first month after discharge, fortnightly calls in the second month, and a single call in the third month, to assess the patient’s adaptation and the acquisition of care mastery. All people who agreed to participate in the project signed a consent form, and their data were organized in an Excel spreadsheet.
2.4. Educational Intervention
The educational intervention focused on providing health education to family caregivers of people using a PEG tube (or who would undergo a surgical procedure for its insertion) due to dysphagia related to an underlying neurological disease. These individuals were classified as having high dependence and low autonomy in care [18,19].
The educational activities took place in the ward on a previously agreed day and time, lasting approximately 40 min, according to the caregivers’ demands and skills, before or after tube installation, depending on the availability of caregivers and the team responsible for providing guidance. The caregivers’ time in relation to receiving the indication of the device and elaborating the situation was also respected.
The educational intervention planning and execution took place in four stages:
2.4.1. Stage 1—Instructing Caregivers about the Device
When a person was eligible for the intervention, the first contact was made by the matrix project team. The study was then presented to the caregivers, and if they accepted the invitation, their sociodemographic data were collected, organized, and stored in Excel spreadsheets.
Patients could be included in the matrix project upon admission or during hospitalization if their degree of dependence reached the inclusion criterion score of 21 to 26 points on the Fugulin scale [18,19]. At the study unit, the indication for the placement of a PEG tube occurred after evaluation by the care team, particularly speech therapy professionals, after rehabilitation attempts.
After identifying the need for the PEG procedure and scheduling the placement, the research team planned the best time for the first orientation meeting with the family. During this initial meeting, the care team’s previous guidance regarding the indications, instructions related to the tube, and the importance and necessity of its use were reinforced and reviewed. Any doubts that arose were addressed, and emotional support was provided regarding the anxieties and insecurities presented by the caregivers. Finally, the best day and time for the educational intervention on the use of the PEG was scheduled.
2.4.2. Stage 2—Training Caregivers to Handle the Tube
For the educational intervention, the number of meetings scheduled depended on the participant’s demand. This phase aimed to provide an understanding of care regarding cleaning techniques; administration of diet, liquids and medications; as well as guidance on fixing the tube; managing complications (leaks, signs of infections, loss of the tube, obstructions); and organizing material for care. Additionally, guidelines were provided related to oral hygiene care, skin care, and the correct positioning of the patient in the bed at home, which is essential for the care of bedridden people with dysphagia and functional dependence.
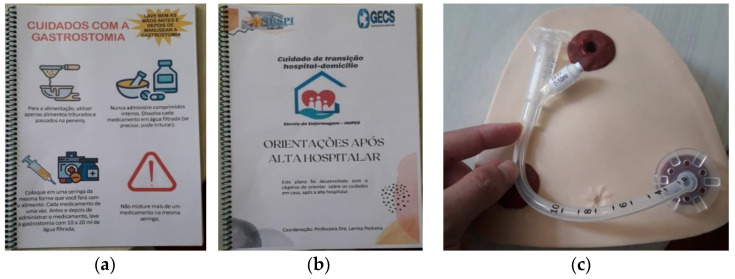
To create a realistic simulation and promote better understanding, the researchers used an anatomical piece of the abdominal region with an attached PEG tube, as well as a 60 mL syringe, gauze, and drinking water. Scientifically supported booklets created by the main research team (Figure 1) were also used to reinforce and illustrate the guidelines, and were later sent via messaging application for observation, reading, and discussion of any doubts.
Figure 1.
Resources used for educational activities with caregivers Scheme 2024. (a) a booklet about gastrostomy care. (b) a booklet of “Guidelines after hospital discharge”. (c) “anatomical specimen of abdominal region with gastrostomy tube used during practical training”.
2.4.3. Stage 3—Feedback Provided during and after Training
During the training sessions, feedback was provided to the caregivers regarding the skills acquired, encouraging them and identifying points to improve the guidance. Specific information was highlighted, such as the consistency of the food to avoid tube obstruction, the ideal temperature to administer the diet, the rate at which the diet should be administered, ways to clean before and after administering food and medications, and the identification and recognition of complications related to the tube and skin.
After the training, the caregivers were invited to view the tube on their family member, as the tube model they would be using at home was often different from the one used during the training. Immediately after the gastrostomy procedure was performed, the telemonitoring follow-up method began, which would continue for three months, with the first call occurring in the first week after discharge.
2.4.4. Stage 4—Follow-Up after Discharge to Observe the Outcome of Interest
The follow-up after discharge was conducted through telemonitoring, which involved seven calls over a three-month period and did not prevent the caregivers from contacting the project team at other times, in case of doubts, either by phone calls or via messaging application. During each follow-up call, a form was filled out with the results, and the caregivers were able to raise any doubts or questions, which were then addressed and clarified by the project team.
2.5. Data Collection and Analysis
To analyze the outcome of interest, forms from the matrix project were used to collect sociodemographic data: sex, age, education, profile (formal or family), time providing care, awareness of the health status of the person under care, formal support on a specific or informal basis, confidence about continuity of care, number of calls received during telemonitoring, and use of an application to exchange messages. During the telemonitoring after discharge, additional information was collected using the matrix project monitoring form, such as the use of a support network (informal or formal), doubts about home care and prescriptions from health professionals, and other demands.
All of the data were organized in an Excel spreadsheet for analysis and discussion of the content based on the Transitions Theory, a mid-range nursing theory proposed by the Egyptian-American Nurse Dr. Afaf Ibrahim Meleis [16]. The information in the text was described according to the Consolidated Criteria for Reporting Qualitative Research (COREQ), translated and validated version for the Portuguese language [20].
2.6. Ethical Considerations
The matrix project was approved by the Ethics Committee of the University Hospital Professor Edgard Santos at the Federal University of Bahia under opinion 5.282.090. This approval was in compliance with resolutions no. 466/2012 [21] and no. 510/2016 [22], which determine specific guidelines and ethics for human and social sciences research.
3. Results
Between November 2022 and July 2023, the research team monitored 52 people with high dependency on care admitted to the neuromusculoskeletal ward. Of these, 17 underwent gastrostomy due to severe dysphagia after neurological impairment from a stroke, and 15 caregivers met the inclusion criteria for this section, as exemplified in Table 1.
Table 1.
Characterization of caregivers participating in the educational intervention. Salvador, Bahia, Brazil, 2023.
| Code Name | Sex/ Age |
Level of Education/ Occupation/ Location and Area of Residence |
Caregiver Profile/ Time Spent Caring |
Aware of the Situation | Formal Support on a Timely Basis/ Informal Support |
Safety for Hospital Discharge/ Telemonitoring Calls |
Use of Messaging App for Residual Doubts |
|---|---|---|---|---|---|---|---|
| C1 | F/ 42 |
Unfinished elementary school/ no defined occupation/ inland city/urban |
Formal/ >12 months |
Yes | No Yes |
Insecure/ 5 calls |
Yes |
| C2 | F/ 67 |
Finished undergraduate degree/ social worker/ capital/urban |
Family member/ <6 months |
Yes | Yes Yes |
Insecure/ 12 calls |
Yes |
| C3 | F/ 58 |
Finished undergraduate degree/ pharmacist/capital/urban |
Family member/ <6 months |
Yes | Yes Yes |
Insecure/ 9 calls |
Yes |
| C4 | F/ 57 |
Finished elementary school/ housewife/ inland city/rural |
family member/ <6 months |
Yes | No Yes |
Insecure/ 7 calls |
Yes |
| C5 | F/ 57 |
Finished high school/ hairdresser/ inland city/urban |
Family member/ >12 months |
Yes | No Yes |
Insecure/ 4 calls |
Yes |
| C6 | F/ 30 |
sales consultant/ inland city/urban |
Family member/ <6 months |
Yes | No Yes |
Insecure/ 8 calls |
Yes |
| C7 | M/ 52 |
Unfinished elementary school/ mason/ capital/urban |
Family member/ <6 months |
Yes | No Yes |
Insecure/ 3 calls |
No |
| C8 | F/ 65 |
Unfinished elementary school/ housewife/ inland city/urban |
Family member/ 6 to 12 months |
Yes | No Yes |
Insecure/ 7 calls |
Yes |
| C09 | F/ 43 |
Unfinished elementary school/ housewife/ inland city/rural |
Family member/ <6 months |
Yes | No Yes |
Insecure/ 6 calls |
Yes |
| C10 | F/ 20 |
Finished high school/ e-commerce businesswoman/ capital/urban |
Family member/ >12 months |
Yes | No Yes |
Insecure/ 5 calls |
Yes |
| C11 | M/ 39 |
Finished undergraduate degree/ pharmacy assistant/ inland city/rural |
Family member/ <6 months |
Yes | Yes Yes |
Insecure/ 4 calls |
Yes |
| C12 | M/ 45 |
Unfinished elementary school/ driver/ inland city/ rural |
Family member/ <6 months |
Yes | No Yes |
Insecure/ 7 calls |
Yes |
| C13 | F/ 52 |
Finished high school/ housewife/ inland city/urban |
Family member/ >12 months |
Yes | No Yes |
Secure/ 2 calls |
No |
| C14 | F/ 43 |
Finished elementary school/ housewife/ inland city/urban |
Family member/ <6 months |
Yes | No Yes |
Insecure/ 12 calls |
Yes |
| C15 | F/ 25 |
Unfinished higher education/ gastronomy student/ inland city/rural |
Family member/ <6 months |
Yes | Yes Yes |
Insecure/ 8 calls |
Yes |
All patients who needed a PEG tube were bedridden and dependent on care for Basic Activities of Daily Living (BADL) and Instrumental Activities of Daily Living (IADL). The educated caregivers had no prior knowledge about the PEG tube, but they all had a basic education and a good understanding of learning.
In the first stage of instruction, after the indication for gastrostomy, it was noticed that the health condition and recommended therapy had an impact on the caregivers, most of whom were family members. They were scared and afraid of managing the PEG, mainly in continuing care safely. The most frequent doubts were related to the indication of PEG instead of the use of the nasoenteral tube, its possible repercussions in the face of frailty, and the possibility of the patient returning to the functional capacity of swallowing and eating after the PEG procedure.
In the second stage, the caregivers were invited to training, which was conducted in an external area to avoid distractions. It was noticed that the participants were aware and engaged in caring for and safely managing the device at home, as they wanted to be prepared for possible complications and act on them. The doubts reported were related to a better understanding of tube care, and the need to share knowledge with other people in the family on whom they counted for support.
In the third stage, the feedback enhanced the caregivers’ engagement for continuity of care. When the caregivers realized that they were making progress, they demonstrated satisfaction with the training, greater confidence, and less fear related to possible adverse events. These reactions were evident in the more fluid and elaborate reports, questions consistent with their social and economic realities, and less resistance to learning when compared to the initial approach.
In the fourth stage, through telemonitoring, it was noticed that the first month after hospital discharge was the most critical period for the caregivers, especially the first and second weeks, considering that these people were getting adapted to family dynamics for shared care, along with work. Some caregivers (C2, C3, C4, and C6)—Table 1 had to give up their work activities and dedicate themselves to this care on top of their other usual responsibilities.
In these cases, despite instructions throughout hospitalization and follow-up, complications arose related to the formation of granulomas in the PEG insertion stoma of seven people receiving care (C2, C3, C4, C5, C8, C11, and C12)—Table 1, tube obstruction in three (C2, C3, and C14), and accidental loss of the tube in two (C6 and C7)—Table 1, which occurred twice in the same person (C6)—Table 1. Regarding these incidents, there was real-time contact with the telemonitoring team, who, in stages, redid the guidelines provided at the hospital, resolving the problem and referring patients to health units, as shown in Table 2.
Table 2.
Characterization of patient complications, effectiveness of training and remote monitoring actions, and recorded outcomes. Salvador, Bahia, Brazil, 2023.
| Code Name | Complications of the Patient | Effectiveness of Training and Telemonitoring Interventions | Results Observed |
|---|---|---|---|
| C2; C3; C4; C5; C8; C11; C12 | Granuloma in the PEG insertion stoma |
|
|
| C2; C3; C14 | PEG obstruction |
|
|
| C6; C7 | Accidental loss of tube |
|
|
|
|
It should be noted that caregivers were aware of their difficulties and limits related to care. Through support from the matrix project team, hospital professionals, and other professionals on a specific basis (Primary Health Care and Home Care), they managed to develop the necessary skills for care and management, especially in the face of complications, assertively seeking out members of the research team and/or health services. The exceptions were C7 and C13 (Table 1), who, despite not having formal support, chose not to continue with telemonitoring, thus resulting, for example, in pneumonia, due to bronchoaspiration of food, and death two months after C7’s family member was discharged from hospital.
4. Discussion
The first stage of the training process revealed the emotional fragility of the caregivers, resulting from fear and uncertainty. This factor was also evidenced in a study of caregivers of older people undergoing PEG in Taiwan, where the risks and benefits of this feeding route were not specified by health professionals, leaving caregivers worried, confused, and insecure about individually consenting to the procedure, resulting in prolongation of hospitalization time and greater exposure to adverse events related to nasoenteric tube use [23].
In the present study, the caregivers had information about the need for gastrostomy, although the communication with the unit’s care team was insufficient in some cases (C2, C3, C4, C8, and C14—Table 1), requiring further explanations from the research care team. Insufficient communication to resolve caregivers’ doubts can negatively impact the acquisition of necessary skills and mastery, which are important outcome indicators for a healthy hospital-to-home transition [16].
This finding is supported by a study that identified factors associated with the cognitive, emotional, psychomotor, and relational skills of caregivers in home care, which emphasized that efficient communication between health professionals and caregivers was essential for them to continue with home care in a planned and safe manner [24]. Intercommunication contributed to the acquisition of new skills, obtaining relevant information about caring, and, consequently, acquiring mastery [24].
Combined with insufficient communication, the emotional and physical exhaustion resulting from the caregivers’ stay in the hospital can have a negative impact on the understanding of information. In the context of the participants in this study, the majority (C4, C5, C6, C8, C9, C12, C13, C14, and C15—Table 1) were from municipalities located in the inland areas of the state, and with a weak informal support network (C8, C12, C14, and C15—Table 1) to share monitoring throughout hospitalization. This situation led to exhaustion, with physical and mental fatigue in caregivers, who also demonstrated a feeling of insecurity regarding the continuity of care, demanding, after discharge, in addition to conventional calls, interactions with text message via app to promote emotional support and ensure greater safety, and resolve residual doubts related to tube care and management of signs and symptoms indicative of complications.
Discharge planning specifically for the continuity of care with PEG for bedridden people with high care dependency should be carried out throughout the hospitalization and continued after returning home. This is because it is during hospitalization that there is an opportunity to get closer to the people involved, knowing their context for planning aligned to their needs. It is crucial to establish transitional care that focuses on the individual and their family, as this is important when a person is discharged from the hospital and returns home. At this point, the person takes on care responsibilities that were previously handled by healthcare professionals, and these responsibilities should now be taken on by the support network [25,26]. However, the support network is often confused and insecure about medication reconciliation, use of devices, and management of signs and symptoms.
The interaction among affected people, family caregivers, and the healthcare team strengthens process indicators in the transition of care. These indicators include understanding the affected person’s health condition and the need for continuity of care, connecting with the healthcare team, considering guidelines and strategies as a form of support, and interacting and inter-relating through the exchange of experiences. These indicators are important for developing confidence and coping strategies in the new context [16]. This interaction also contributes to a collaborative relationship in teaching care, in this case, PEG. A study effectively demonstrated the significance of interaction between nurses and young adults during the care transition process, observing that when healthcare professionals prioritize operational tasks over building relationships with patients, the latter feel insecure, objectified, and helpless, leading to distrust, low adherence, and abandonment of care plans [27].
In this study, nine caregivers (C1, C2, C3, C4, C6, C7, C9, C14, and C15—Table 1) received training before the insertion of the PEG tube into their family members. This training took place on the hospital’s external premises, in a calm environment, without the movement of professionals or other interference, using accessible language and no technical terms. This organization contributed to ensuring that there were no interruptions and distractions, resulting in better learning at the end of the health education.
This finding is supported by a study that explored the experiences of gastrostomy insertion from the perspective of affected people and informal caregivers, which found that participants did not absorb the information provided and/or were unprepared for the practical aspects related to food administration [28]. This was attributed to the lack of guidance before creating the gastrostomy (pre-surgical period) and the inadequate training environment, as they were trained within a neurological ward that was busy and had distractions [28].
Another investigation with caregivers of people undergoing PEG in a university hospital in Turkey observed that the content of the training provided during hospitalization was insufficient and short, making information comprehension difficult [6]. Caregivers were afraid and stressed during the training, as they were not confident that they would be able to reproduce the care, and they pointed out that training should not only occur once and verbally, but rather with practical and demonstrative experiences [6].
In this study, the training did not have a defined end time and varied depending on the caregiver’s acquisition of skills. Furthermore, the realistic simulation with an anatomical piece promoted an interactive and participatory space between caregivers and the team carrying out the educational intervention. This is a practical, repetitive teaching method that influences the ability to understand, engage in the search for information, and clarify residual doubts [29], allowing the development of mastery and prevention of complications related to inadequate care.
During the intervention, caregivers had space to share doubts and concerns, and from there, received clarifications. Subsequently, they were invited to train and demonstrate learning through speech and practice on the anatomical piece under supervision, receiving feedback on their skill and knowledge acquisition, thus driving the decision as to when training could be completed. Studies have shown that feedback is an essential strategy in the process of evaluating learning and skill acquisition [30]. When positive, it can motivate and involve caregivers; however, when negative, it works as a starting point for reorganizing the educational action, with new attempts to put the desired skill into practice [30].
After the family member was discharged, monitoring continued via telemonitoring through telephone calls, audio and/or videos via messaging app, aiming to ensure good adaptation at home. In the cases reported here, this monitoring resulted in a better understanding of the need to use the tube, its safe and appropriate handling, safety in managing signs and symptoms, cognitive ability in the face of complications, clarification of doubts, qualified listening, and emotional support. Furthermore, monitoring promoted a feeling of security in caregivers and allowed for better engagement perceived by feedback on messages and guidance.
The positive impact of this care was observed, as all caregivers demonstrated insecurity and anguish regarding discharge before the intervention. A study revealed that telemonitoring favored the maintenance of bonds and adherence to treatment; supported self-care; and provided confidence and support for hospitalized people and their socio-family network [31]. This technology has the potential for engagement, making the affected person and their caregivers protagonists of the therapeutic process [31].
The first month after discharge, specifically the first week, was a delicate period of intense transformations and new meanings for caregivers, due to fear and apprehension of what could happen, of not being able to manage care, which included tube management. Furthermore, these people were still faced with the need to align this reality with work and restructure family dynamics to share assistance. This fact was particularly noticeable in those who had played the role of caregiver for less than 6 months (C2, C3, C4, C6, C7, C9, C11, C12, C14, and C15—Table 1), who made an average of 7.6 phone calls, that is, 3.6 more than those who had been providing care for more than 12 months (C1, C5, C10, and C13—Table 1, possibly because they lacked experience and perceived, in telemonitoring, the opportunity to acquire knowledge and provide safer care.
Regarding the aspect of having telephone contact in the first week after discharge, the authors discuss the importance of this approach to understand how the hospital–home transition occurred, and whether there were doubts related to care. If the caregiver seems insecure for any reason, professionals must assess their needs and act on them [32].
In this study, all caregivers experienced the transition in the health–illness process, and in addition, seven (C2, C3, C5, C6, C7, C14, and C15—Table 1) experienced situational transitions. Transitions in the health–disease process resulted from the transition from hospital to home, while situational transitions occurred due to the addition or subtraction of people in the environment and/or redefinition of roles in the family context [16].
The situational transitions contributed to four caregivers (C2, C3, C4, and C6—Table 1) giving up their work, leisure and self-care activities, resulting in emotional fragility and musculoskeletal pain related to this role. These setbacks can interfere with engagement and interaction with professionals to discuss doubts, due to the lack of time resulting from exclusive and routine care. Moreover, ergonomic diseases and repetitive strain injuries are situations that can occur in people who provide intense and continuous care for bedridden and dependent individuals [33], interfering with the time and quality of care provided.
Regarding the occurrence of accidental loss of the tube, telemonitoring, when activated, provided support by giving guidelines related to cleaning the ostium with warm water, protecting with gauze and immediate transfer to the local hospital, according to recommendations, as the municipality in which the patient was located did not have Emergency Services activated [34]. On both occasions of this incident, there was rapid and timely response to the displacement, considering that the family member was aware that the PEG orifice could occlude according to the guidelines provided at the hospital. The problem related to the gastrostomy tube obstruction was also resolved when telemonitoring was activated, with instructions through video call via the application. In both situations, guidance regarding complications occurred in real time, with resolution of the problem.
Regarding granuloma care, the guidance was to use 20% sodium chloride (NaCl) due to its ease of access in Primary Health Units and/or lower cost in local drugstores. The practice consisted of moistening gauze with 20% NaCl and applying it around the lesion for a period of five to ten minutes, with it behaving like a hypertonic dressing. The hypertonic solution causes an osmotic imbalance, in which the cells lose fluids to the more solute-concentrated medium (gauze with 20% NaCl), reducing the hypergranulation tissue [35]. The therapeutic effects were satisfactory after guidance and monitoring.
In all cases presented, the caregivers were aware of the family member’s health status. This awareness is characterized when that event gains meaning, promoting engagement to address the situation. This was realized through the sending of photos and videos of caregivers manipulating the tube, real-time video calls to answer questions and/or share progress in rehabilitation and recovery, as well as the search for additional information provided by the UBS team as per observed in the C2, C3, C4, C7, and C14 (Table 1) situations.
A study involving 21 caregivers in Turkey observed that a lack of awareness interfered with the acquisition of mastery, leading these people to make unsafe and hasty decisions in the face of incidents [6]. As an example, they unblocked the PEG with pieces of wire and injected saline solution into the tube [6]. In cases of leakage, a situation that may occasionally occur, they fixed plaster to the parts of the tube that drained liquids or cut these parts and reinserted the tube [6]. In view of the above, we can see the importance of discharge management promoted by the multidisciplinary team and follow-up after return home, to ensure an effective hospital–home transition, adaptation, and continuity of care.
This study is valuable for nursing professionals as it encourages reflection on clinical practice in the hospital environment, the barriers that need to be overcome, and how actions for discharge planning impact the awareness and engagement of caregivers in the home environment. It highlights the need for follow-up to clarify any remaining doubts and preventive practices, resulting in person- and family-centered care, maintenance of autonomy, continuity of care at home, reduction of unfavorable health outcomes, early readmissions, and a decrease in hospital costs.
This study has limitations due to the specific target population and the fact that its findings may not be widely applicable. While this study did not face this issue, it is important to note that not all patients and caregivers have access to the internet or suitable mobile devices for remote monitoring. Therefore, nurses should use hospital time to plan a safe and effective discharge and provide training and health education. The success of telemonitoring depends, in part, on the skills acquired in the hospital. Additionally, to improve monitoring outcomes, it is important to customize a call plan based on the patient’s profile, considering their pre-existing conditions and the skills of the caregivers.
5. Conclusions
The process for home caregivers to acquire mastery in gastrostomy management involves a series of aspects that can influence whether or not the transition is safe. These include the use of appropriate spaces for training; the provision of personalized time for each caregiver; a combination of theoretical and practical demonstrations with constant feedback; transparent, welcoming, and accessible communication; and continuous monitoring of adaptation, especially during the first month after hospital discharge, since complications arose despite the educational intervention. Still, the caregivers demonstrated mastery in managing them.
In addition, it was observed that the physical and emotional exhaustion caused by the lack of knowledge about the device, the experience of accompanying the family member in the hospital, and a weak support network influenced the acquisition of mastery through the greater insecurity of these people regarding the continuity of care. The specific details of the procedure, such as its restrictions and possible complications, are also factors that should be considered, as they can promote insecurity in caregivers.
To ensure a safe transition in situations involving people using a gastrostomy device, the multidisciplinary team must begin discharge planning from the beginning of the hospitalization, setting aside enough time to explain the procedure and its purpose and to carry out simulated training adjusted to the reality of each caregiver, strengthening them with educational material. In this scenario, nursing plays a leading role, given its proximity, frequency of contact, and constant communication with patients and their caregivers.
Author Contributions
Conceptualization, J.M.d.S. and L.C.P.; Data curation, J.M.d.S., L.C.P. and L.C.V.; Formal analysis, J.M.d.S. and L.C.P.; Funding acquisition, J.O.; Investigation, L.C.P.; Methodology, J.M.d.S., L.C.P., R.P.G. and M.A.A.d.S.; Supervision, L.C.P. and R.P.G.; Writing—original draft, J.M.d.S., L.C.P., R.P.G., M.A.A.d.S., C.R.S.L.B., J.O., R.N.D.L.R., A.R.S., V.A.d.S., I.S.P., J.L.P.S. and L.C.V.; Writing—review and editing, J.M.d.S., L.C.P., R.P.G., M.A.A.d.S., C.R.S.L.B., J.O., R.N.D.L.R., A.R.S., V.A.d.S., J.L.P.S. and L.M.S.d.O. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was conducted in accordance with the guidelines set by the Ethics Committee of the University Hospital Professor Edgard Santos at the Federal University of Bahia. It was approved under protocol code 5.282.090 on 9 March 2022.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author. They can also be shared with the journal for review upon request.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This work has been supported by the following Brazilian research agencies: Fundação de Amparo à Pesquisa do Estado da Bahia (FAPESB)—Process number 084.0508.2024.0001182-91, announcement FAPESB 02/2022; Coordenação de Aperfeiçoamento de Pessoal de Nível Superior–Brazil (CAPES)–Finance Code 001; and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ) Funding Code APP0025/2023 research grant. Funding for this article was partially provided by T37MD008647 from the National Institute on Minority Health and Health Disparities. The views expressed in this publication do not necessarily reflect the official policies of the Department of Health and Human Services, nor does the mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Kurien M., Andrews R.E., Tattersall R., McAlindon M.E., Wong E.F., Johnston A.J., Hoeroldt B., Dear K.L., Sanders D.S. Gastrostomies Preserve But Do Not Increase Quality of Life for Patients and Caregivers. Clin. Gastroenterol. Hepatol. 2017;15:1047–1054. doi: 10.1016/j.cgh.2016.10.032. [DOI] [PubMed] [Google Scholar]
- 2.Dietrich C.G., Schoppmeyer K. Percutaneous endoscopic gastrostomy—Too often? Too late? Who are the right patients for gastrostomy? World J. Gastroenterol. 2020;26:2464–2471. doi: 10.3748/wjg.v26.i20.2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clarke E., Pitts N., Latchford A., Lewis S. A large prospective audit of morbidity and mortality associated with feeding gastrostomies in the community. Clin. Nutr. 2017;36:485–490. doi: 10.1016/j.clnu.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Emmons D. Reducing outpatient gastrostomy tube complications. Nutr. Clin. Pract. 2022;37:351–360. doi: 10.1002/ncp.10686. [DOI] [PubMed] [Google Scholar]
- 5.Huynh G., Chan M., Huynh H.Q. Buried bumper syndrome. VideoGIE. 2020;5:104–106. doi: 10.1016/j.vgie.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sezer R.E., Ozdemir Koken Z., Senol Celik S. Home Percutaneous Endoscopic Gastrostomy Feeding: Difficulties and Needs of Caregivers, Qualitative Study. J. Parenter. Enter. Nutr. 2020;44:525–533. doi: 10.1002/jpen.1612. [DOI] [PubMed] [Google Scholar]
- 7.Friginal-Ruiz A.B., Lucendo A.J. Percutaneous Endoscopic Gastrostomy: A Practical Overview on Its Indications, Placement Conditions, Management, and Nursing Care. Gastroenterol. Nurs. Off. J. Soc. Gastroenterol. Nurses Assoc. 2015;38:354–366; quiz 367–368. doi: 10.1097/SGA.0000000000000150. [DOI] [PubMed] [Google Scholar]
- 8.Muoki D. Patient education on PEG tube care at home. Nursing. 2023;53:11–12. doi: 10.1097/01.NURSE.0000919008.15130.5c. [DOI] [PubMed] [Google Scholar]
- 9.DeLegge M.H. Gastrostomy Tubes: Complications and Their Management. [(accessed on 12 July 2024)]. Available online: https://www.medilib.ir/uptodate/show/2552.
- 10.Esenay F.I., Sezer T.A., Kursun S., Gülez Gedik G. Problems Experienced by Family of Child with Percutaneous Endoscopic Gastrostomy. Güncel Pediatri. 2016;14:110–115. doi: 10.4274/jcp.62634. [DOI] [Google Scholar]
- 11.de Castro Hadad A.C.A., de Oliveira Jorge A. Continuidade do cuidado em rede e os movimentos de redes vivas nas trajetórias do usuário-guia. Saúde Debate. 2018;42:198–210. doi: 10.1590/0103-11042018s416. [DOI] [Google Scholar]
- 12.Mauro A.D., Cucolo D.F., Perroca M.G. Hospital—Primary care articulation in care transition: Both sides of the process. Rev. Esc. Enferm. USP. 2021;55:e20210145. doi: 10.1590/1980-220x-reeusp-2021-0145. [DOI] [PubMed] [Google Scholar]
- 13.Sezer R.E., Talas M.S. In Home Caregivers’ Experiences with Percutaneous Endoscopic Gastrostomy Patients: A Qualitative Review. Gastroenterol. Nurs. Off. J. Soc. Gastroenterol. Nurses Assoc. 2021;44:268–277. doi: 10.1097/SGA.0000000000000541. [DOI] [PubMed] [Google Scholar]
- 14.Schweitzer M., Aucoin J., Docherty S.L., Rice H.E., Thompson J., Sullivan D.T. Evaluation of a Discharge Education Protocol for Pediatric Patients with Gastrostomy Tubes. J. Pediatr. Health Care. 2014;28:420–428. doi: 10.1016/j.pedhc.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 15.da Silva Rodrigues T.F.C., Cardoso L.C.B., da Silva Rêgo A., Silva E.S., de Fátima Araújo Lopes Elias M., Radovanovic C.A.T. Educational intervention to increase the skill of informal caregivers: A quasi-experimental pilot study. Texto Contexto Enferm. 2021;30:e20200152. doi: 10.1590/1980-265x-tce-2020-0152. [DOI] [Google Scholar]
- 16.Meleis A.I., Sawyer L.M., Im E.-O., Hilfinger Messias D.K., Schumacher K. Experiencing Transitions: An Emerging Middle-Range Theory. Adv. Nurs. Sci. 2000;23:12. doi: 10.1097/00012272-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 17.de Almeida L.B., Fernandes V.A. Produção científica do Complexo Hospitalar Universitário Professor Edgard Santos (1973–2022) An. 29º Congr. Bras. Bibliotecon. Doc. Cienc. Inform. 2022;1:1–13. [Google Scholar]
- 18.Fugulin F.M.T., Gaidzinski R.R., Kurcgant P. Sistema de classificação de pacientes: Identificação do perfil assistencial dos pacientes das unidades de internação do HU-USP. Rev. Lat. Am. Enferm. 2005;13:72–78. doi: 10.1590/S0104-11692005000100012. [DOI] [PubMed] [Google Scholar]
- 19.Vandresen L., de Pires D.E.P., Lorenzetti J., de Andrade S.R. Classificação de pacientes e dimensionamento de profissionais de enfermagem: Contribuições de uma tecnologia de gestão. Rev. Gaúcha Enferm. 2018;39:e2017. doi: 10.1590/1983-1447.2018.2017-0107. [DOI] [PubMed] [Google Scholar]
- 20.Souza V.R.D.S., Marziale M.H.P., Silva G.T.R., Nascimento P.L. Translation and validation into Brazilian Portuguese and assessment of the COREQ checklist. Acta Paul Enferm. 2021;34:eAPE02631. doi: 10.37689/acta-ape/2021AO02631. [DOI] [Google Scholar]
- 21.Novoa P.C.R. O que muda na Ética em Pesquisa no Brasil: Resolução 466/12 do Conselho Nacional de Saúde. Einstein. 2014;12:vii–vix. doi: 10.1590/S1679-45082014ED3077. [DOI] [Google Scholar]
- 22.Lordello S.R., da Silva I.M. Resolução no 510/2016 do Conselho Nacional de Saúde: Um panorama geral. Rev. SPAGESP. 2017;18:06–15. [Google Scholar]
- 23.Yeh L., Fetzer S.J., Chen S.-Y., Lu F.-H., Chuang C.-H., Chen C.-H. Percutaneous endoscopic gastrostomy placement: Caregiver decision making in Taiwan. J. Formos. Med. Assoc. 2013;112:99–104. doi: 10.1016/j.jfma.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 24.Santos F.G.T.D., Zulin A., Cardoso L.C.B., de Cassia Nogueira Sanches R., da Silva Rêgo A., Girardon-Perlini N.M.O., Radovanovic C.A.T. Factors associated with the skills of informal caregivers in home care. Rev. Bras. Enferm. 2022;75:e20210744. doi: 10.1590/0034-7167-2021-0744. [DOI] [PubMed] [Google Scholar]
- 25.Menezes T.M.O., Oliveira A.L.B., Santos L.B., Freitas R.A., Pedreira L.C., Veras S.M.C.B. Hospital transition care for the elderly: An integrative review. Rev. Bras. Enferm. 2019;72((Suppl. S2)):294–301. doi: 10.1590/0034-7167-2018-0286. [DOI] [PubMed] [Google Scholar]
- 26.Santos J.L.P., Pedreira L.C., Coifman A.H.M., Santos J.M., Pessoa L.S.C., Souza M.A.A. Nursing team strategies for caring for older adults in the hospital-home transition: An integrative review. Acta Paul. Enferm. 2024;37:eAPE01904. doi: 10.37689/acta-ape/2024ar001904. [DOI] [Google Scholar]
- 27.Gillie G.G., Tarabeih M. “A Bridge Over Troubled Water”: Nurses’ Leadership in Establishing Young Adults’ Trust Upon the Transition to Adult Renal-Care—A DualPerspective Qualitative Study. J. Pediatr. Nurs. 2020;53:41–48. doi: 10.1016/j.pedn.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 28.Stavroulakis T., Baird W.O., Baxter S.K., Walsh T., Shaw P.J., McDermott C.J. The impact of gastrostomy in motor neurone disease: Challenges and benefits from a patient and carer perspective. BMJ Support. Palliat. Care. 2016;6:52–59. doi: 10.1136/bmjspcare-2013-000609. [DOI] [PubMed] [Google Scholar]
- 29.Kaneko R.M.U., de Moraes Lopes M.H.B. Realistic health care simulation scenario: What is relevant for its design? Rev. Esc. Enferm. USP. 2019;53:e03453. doi: 10.1590/s1980-220x2018015703453. [DOI] [PubMed] [Google Scholar]
- 30.de Godoi Montes L., Rodrigues C.I.S., de Azevedo G.R. Assessment of feedback for the teaching of nursing practice. Rev. Bras. Enferm. 2019;72:663–670. doi: 10.1590/0034-7167-2018-0539. [DOI] [PubMed] [Google Scholar]
- 31.Camara G.D., Porciúncula L. Cuidado coordenado em um programa de telemonitoramento pós-alta hospitalar. APS Rev. 2022;4:187–195. doi: 10.14295/aps.v4i3.248. [DOI] [Google Scholar]
- 32.Gomes T.J.B., da Silva Ferreira B.A., Baixinho C.L., Ferreira Ó.M.R. Algorithm for transitional care for caregivers of dependent older adults: A validation study. Rev. Bras. Enferm. 2021;74:e20200625. doi: 10.1590/0034-7167-2020-0625. [DOI] [PubMed] [Google Scholar]
- 33.Gomes N.P., Pedreira L.C., Gomes N.P., de Oliveira Souza Fonseca E., Reis L.A.D., de Andrade Santos A. Health-related consequences of caring for dependent relatives in older adult caregivers. Rev. Esc. Enferm. USP. 2019;53:e03446. doi: 10.1590/s1980-220x2018002303446. [DOI] [PubMed] [Google Scholar]
- 34.Ministério da Saúde . Caderno de Atenção Domiciliar. 1st ed. Volume 2 Heidêr Aurélio Pinto; Brasília, Brazil: 2012. [Google Scholar]
- 35.Silva S.E.R., Nunes R.S.O., Silva B.S.V., Simões E.A.P. Utilização da solução hipertônica de Cloreto de Sódio em granulomas periestomais de traqueostomias. Braz. J. Dev. 2023;9:9783–9793. doi: 10.34117/bjdv9n3-062. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author. They can also be shared with the journal for review upon request.