Abstract
Background
Arthrodesis serves as the traditional therapeutic approach for advanced distal interphalangeal joint (DIPJ) arthritis. However, the conventional technique may prove insufficient when the excision of pronounced volar and lateral spurs is required. To address this, we innovated the 'smile incision with reverse shotgun approach'. This method enhances joint exposure and yields superior cosmetic results by extending the transverse skin incision over the DIPJ and cleaving the accessory collateral ligament, thereby improving access to the volar and lateral joint margins. This article meticulously elucidates the surgical procedure and presents preliminary results of its implementation.
Method
The clinical data of 22 consecutive patients (36 fingers) who received DIPJ arthrodesis by this procedure during March 2018 to October 2022, with a mean follow-up period of 9.8 months, were reviewed. Patients’ demographics, union rate, complications, radiographic findings, as well as visual analogue scale (VAS) for pain and satisfaction, were collected and analyzed.
Results
Thirty-five of 36 fingers achieved uneventful bony union (97.2%). The average VAS for pain and satisfaction as well as he coronal plane deviation of DIPJ significantly improved after the operation (all, P < 0.05). No skin necrosis, nail deformity, or infection were observed during the follow-up period.
Conclusion
The smile incision and reverse shotgun approach provided excellent DIPJ exposure, high union rate, and cosmetic appearance for DIPJ arthrodesis surgery. This technique may be a good surgical option for DIPJ arthrodesis when more volar part joint preparation and more volar implant insertion sites are necessary.
Keywords: Distal interphalangeal joint arthritis, DIP, Shotgun procedure, Smile incision, Transverse incision
Introduction
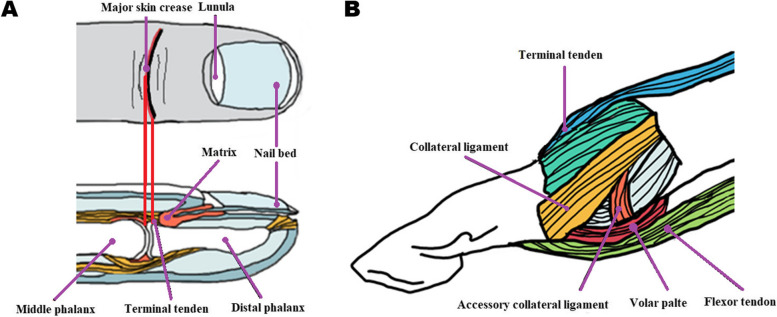
Arthrodesis is the most common surgical treatment for terminal distal interphalangeal joint (DIPJ) arthritis, joint subluxation, and deformity [1–3]. Traditional approaches for a DIPJ include a transverse, H, Y, and lazy S style incisions around the dorsal aspect of DIPJ followed by a dorsal capsulotomy [4–7]. Although these approaches enable effective exposure for DIPJ arthrodesis, they may not provide the adequate exposure required for volar or lateral spur excision, joint preparation or implant insertion when there is a need for more extensive volar or lateral joint surface exposure. To address this issue, we propose a novel technique referred to as the 'smile incision with reverse shotgun procedure' to optimize DIPJ exposure. This procedure involves dividing the accessory collateral ligament (ACL) and applying hyperflexion of more than 120 degrees to the DIPJ (Fig. 1), thereby allowing maximum exposure of the joint, inclusive of the volar rim and the volar capsule. This enhanced exposure facilitates optimal joint surface preparation and implant insertion. To mitigate potential complications such as skin necrosis and nail deformity, the 'smile' incision is strategically executed along the primary, un-bifurcated DIPJ finger crease, which is distanced from the nail germinal matrix (Fig. 2). It is hypothesized that this technique will yield non-inferior surgical outcomes and reduce associated complications. The objective of this article is to provide a comprehensive description of the procedure and to present the preliminary surgical outcomes of this innovative technique.
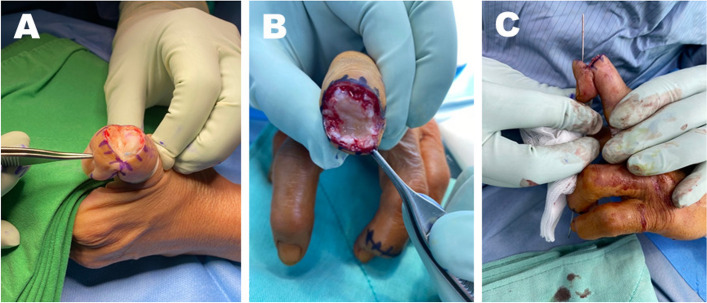
Fig. 1.
Arthrodesis; Fig. 1. The reverse shotgun position facilitates joint preparation and implant insertion: (A) the thumb interphalangeal joint (IPJ) is exposed after transection of extensor tendon and collateral ligaments. (B) The volar IPJ is fully exposed after releasing the accessory collateral ligaments and hyperflexion of the joint greater than 120 degrees as the reverse shot gun position (C) Implant insertion site can be selected under full-field view of joint after complete decortication of the IPJ
Fig. 2.
A Smile-style incision is made along the major skin crease of DIPJ. Incision slightly curves distally until the mid-axial line of the finger. The level of this incision can cover the whole DIPJ and keep a distance from the nail germinal center. B The joint exposure is enlarged gradually after dividing terminal tendon, collateral ligaments, and accessory collateral ligaments, accordingly
Materials and methods
Patient enrollment
After obtaining Institutional Review Board approval, all patients who underwent DIPJ arthrodesis with smile incision and reverse shotgun approach during the study period between March, 2018 and October, 2022 were retrospective reviewed using our institutional registry. The surgical indications for DIPJ arthrodesis include Kellgren and Lawrence grade 3 or more in radiographic arthritic change or joint subluxation of DIPJ with persistent pain or tenderness [8].
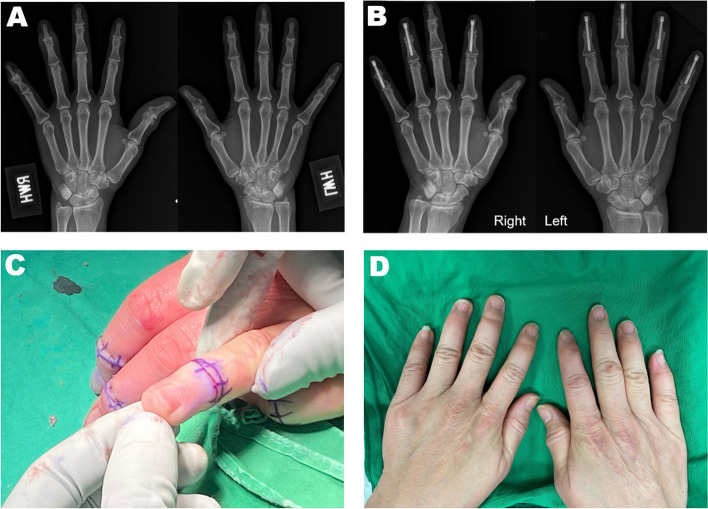
Patients with previous surgery for the same finger, a follow-up period of less than 2 months, or underlying vascular diseases were excluded. The flowchart of patient enrollment is depicted in Fig. 3.
Fig. 3.
The flow chart of patient enrollment
Surgical technique
The surgical procedures were uniformly conducted by a certified hand surgeon, affiliated with a single academic medical institution, and were performed on an outpatient basis, employing regional anesthesia with an arm/digital tourniquet.
The surgical process commenced with a transverse incision made along the dorsal major skin crease of the DIP joint, extending this incision to the mid-axial line of the finger's lateral aspect with a gentle curve towards the distal phalanx (Fig. 2). The dorsal capsule and terminal tendon were then severed at the joint line level to expose the joint. A cautious dissection is crucial at this juncture to prevent damage to the nerves and vessels.
Following this, the dorsal and volar peripheral osteophytes of the middle phalanx's head and the distal phalanx's base were excised. The residual articular surface underwent decortication and dechondrification to correct the coronal plane deviation deformity and create reciprocal surfaces.
For reduction and fixation, a 1-mm (0.035 inch) Kirschner wire (K-wire) was implanted from the distal phalangeal base's center, directed towards the finger's tip and parallel to the nail. The K-wire was then removed, leaving approximately 2-mm of the wire tip jutting out from the distal phalangeal base's joint surface. Following the selection of the central-central position of the DIP joint surface on the middle phalanx, the wire was driven retrogradely across the DIP joint into the middle phalanx. The intramedullary K-wire's depth was then measured to choose a suitable screw length.
Subsequently, while manually sustaining the reduction in full extension (or 10 degrees flexion for the thumb IP joint), an appropriate cannulated drill bit was advanced retrograde along the K-wire path. An appropriate-length headless screw was then inserted to compress the DIP joint. In this series, all thumbs were affixed using a 3.5 mm Dart-Fire Headless Compression Screw (Wright Medical Technology, Memphis TN), whereas all other fingers utilized a 2.5 mm Dart-Fire Headless Compression Screw. The implant and joint alignment's position, size, and length were verified using fluoroscopy.
After the procedure, the extensor tendon was reapproximated using 4–0 absorbable sutures, leaving a 2–3 mm tendon overlap to maintain the extensor tendon's tension. The skin was then closed using 5–0 nylon horizontal mattress sutures, followed by the application of a sterile dressing and a protective splint. The splints were removed four weeks postoperatively.
Sutures were typically removed between 10 to 14 days post-surgery. Physiotherapy was generally deemed unnecessary. Patients underwent routine clinical visits and radiographic assessments to evaluate bony and clinical union.
Clinical and radiographic evaluation
Clinical outcomes were assessed using the visual analog scale (VAS 0–10 cm) for pain and satisfaction at each follow-up appointment postoperatively. The preoperative and the last postoperative VAS were compared. Complications such as infection, skin necrosis, subungual hemorrhage, and nail deformity were recorded.
Radiographic outcomes were assessed using the finger’s anteroposterior and lateral views. Union was defined as bone bridging across the fusion site on 2 standard finger radiographs (anteroposterior, lateral) and no DIPJ movement or pain during clinical examination. Nonunion was defined as no evidence of bone union and DIPJ movement or pain during clinical examination more than 3 months after surgery. Finger coronal plane correction was measured preoperatively and postoperatively according to the description of Gumussuyu et al. [9]. The method for measuring angles is shown in detail in Fig. 4.
Fig. 4.
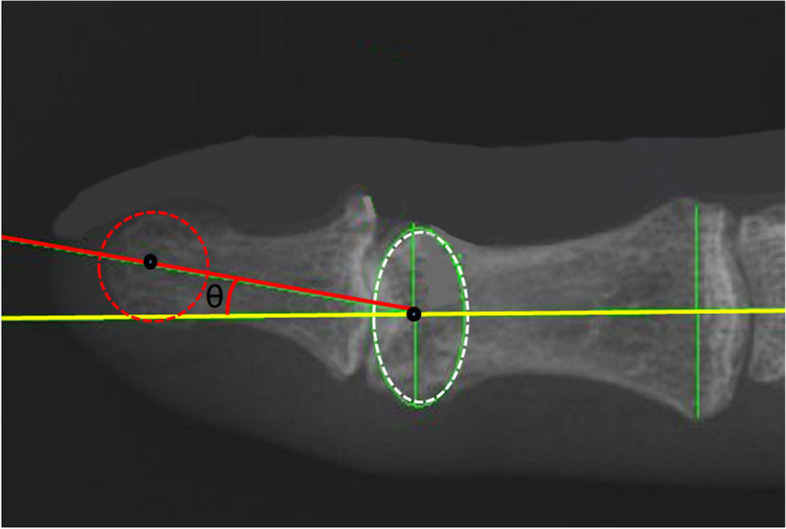
Measurement of DIPJ radial-ulnar deviation on the coronal plane. The yellow line represents the longitudinal axis of the middle phalanx. The red line represents the longitudinal axis of the distal phalanx. The white dotted circle shows the best-fit circle to the head of the middle phalanx. The red dotted circle shows the best-fit circle to the head of the distal phalanx. The joint radial-ulnar deviation is the angle between the red line and the yellow line
Hospital charts were reviewed to collect clinical data. The surgeon examined all patients and radiographs were obtained preoperatively and every month postoperatively until bony union was achieved.
Statistical analysis
Data analysis was performed using SPSS software (Version 22.0; Chicago, Illinois). Univariate analysis was performed using frequencies for descriptive statistics. The Chi-square test was used in the analysis of categorical variables. Paired sample t-test was used in the analysis of preoperative and postoperative variables. Correlations were considered significant if p values were less than 0.05 (two-sided).
Results
Thirty-six fingers that had undergone arthrodesis were included in the analysis with a mean follow-up period of 9.8 months (range, 2 to 21.3 months). Thirty-five of 36 fingers achieved uneventful bone union (97.2%). The average union time was 3 months.
The demographic data of 36 fingers in 22 patients is shown in Table 1. The patients comprised 3 males (13.6%) and 19 females (86.4%). The mean age of the patients was 57 years (range from 41 to 82 years). Painful osteoarthritis was observed in 17 cases, ligament tear with joint subluxation in 9 cases, and rheumatoid arthritis in 10 patients. The affected fingers consisted of 12 thumbs, 7 index fingers, 7 middle fingers, 4 ring fingers, and 6 little fingers. No significant difference was found in demographic data between the union and nonunion groups.
Table 1.
Basic characteristics of 22 patients (36 fingers)
| Characteristics | All (n = 36) |
Union (n = 35) |
Nonunion (n = 1) |
P-value |
|---|---|---|---|---|
| Age, n (%) | ||||
| ≥ 60 years old | 25(69.44) | 25(71.43) | 1(100) | 1.000 |
| < 60 years old | 11(30.56) | 10(28.57) | 0(0) | |
| Gender, n (%) | ||||
| Male | 3(8.33) | 3(8.57) | 0(0) | 1.000 |
| Female | 33(91.67) | 32(91.43) | 1(100) | |
| Side, n (%) | ||||
| Right | 17(47.22) | 17(48.57) | 0(0) | 1.000 |
| Left | 19(52.78) | 18(51.43) | 1(100) | |
| Finger, n (%) | ||||
| Thumb | 12(33.33) | 12(34.29) | 0(0) | 0.372 |
| Index | 7(19.44) | 6(17.14) | 1(100) | |
| Middle | 7(19.44) | 7(20) | 0(0) | |
| Ring | 4(11.11) | 4(11.43) | 0(0) | |
| Little | 6(16.67) | 6(17.14) | 0(0) | |
| Cause, n (%) | ||||
| Osteoarthritis | 17(47.22) | 16(45.71) | 1(100) | 0.563 |
| Joint subluxation | 9(25) | 9(25.71) | 0(0) | |
| Rheumatoid arthritis | 10(27.78) | 10(28.57) | 0(0) | |
| Anesthesia, n (%) | ||||
| LA | 22(61.11) | 22(62.86) | 0(0) | 0.389 |
| GA | 14(38.89) | 13(37.14) | 1(100) | |
Table 2 shows the preoperative and postoperative VAS score for pain and satisfaction. The postoperative VAS score for pain showed significant improvement compared to the preoperative score (6.22 to 0.67, P < 0.001). The postoperative VAS score for satisfaction revealed significant improvement compared to the preoperative score (1.67 to 8.14, P < 0.001).
Table 2.
Comparison of pre-operative and postoperative VAS for pain and satisfaction for 36 fingers
| VAS | Preoperative | Postoperative | p-values |
|---|---|---|---|
|
For pain, Mean ± S.D (Range) |
6.22 ± 0.76 (5–7) | 0.67 ± 0.54 (0–1) | < 0.001 |
| For satisfaction, Mean ± S.D (Range) | 1.67 ± 0.59 (1–2) | 8.14 ± 0.59 (8–9) | < 0.001 |
VAS visual analogue scale
Table 3 shows the preoperative and postoperative finger coronal axis deviation angles. The postoperative coronal axis deviation angles significantly improved compared to the preoperative angles for fingers and thumbs, respectively (10.38° to 3.10° and 24.02° to 3.16°, P = 0.001 and 0.002, respectively).
Table 3.
Comparison of preoperative and postoperative DIPJ deviation in coronal plane
| Coronal axis deviation | Preoperative | Postoperative | p-values |
|---|---|---|---|
| Fingers, Mean ± S.D. (n = 24) | 10.38° ± 9.97° | 3.10° ± 2.26° | 0.001 |
| Thumbs, Mean ± S.D. (n = 12) | 24.02° ± 19.22° | 3.16° ± 1.97° | 0.002 |
Table 4 shows the common complications of DIPJ arthrodesis. One nonunion case was found in our series (1/36, 2.78%). This patient complained of operative finger pain. Screw loosening line was found on the radiograph at the 2-month follow-up visit. She received a revision surgery with meticulous debridement and larger-sized screw (3.5 mm) fixation. Uneventful bone union was achieved 3 months after the operation. Complaint of dorsal distal phalangeal region numbness occurred in 15/36 (41.7%) patients initially after the operation. However, this numbness had mostly subsided (35/36) at 2 months postoperatively. Subungual hemorrhage was also found initially after the operation in 17/36 (47.2%) fingers. However, this complication had subsided in all patients at the final follow-up visit. There were no complaints of pain or inconvenience in daily life among patients with subungual hemorrhage. There were no occurrences of infection, contracted scar, hypertrophic scar, nail deformity, osteomyelitis, superficial infection, fracture, or screw cut out during the follow-up period.
Table 4.
Comparison of complications in the study population (n = 36 cases)
| Complications | |||
|---|---|---|---|
| Postoperative | Final follow-up | Complication rate, n (%) | |
| Scar formation | 0/36 | 0/36 | 0/36 |
| Skin necrosis | 0/36 | 0/36 | 0/36 |
| Nail bed deformity | 0/36 | 0/36 | 0/36 |
| Nonunion | 1/36 | 1/36 | 1/36(2.78%) |
| Osteomyelitis | 0/36 | 0/36 | 0/36 |
| Abnormal hot and cold sensitivity | 0/36 | 0/36 | 0/36 |
| Infection | 0/36 | 0/36 | 0/36 |
| Fracture | 0/36 | 0/36 | 0/36 |
| Amputation | 0/36 | 0/36 | 0/36 |
| Screw cut out | 0/36 | 0/36 | 0/36 |
Discussion
Ensuring adequate surgical exposure of the DIPJ is of paramount importance in the arthrodesis procedure to effectively treat marginal spurs, correct mal-alignment, perform thorough joint preparation, and choose the optimal implant insertion site. Our proposal is that the 'smile incision with reverse shotgun procedure' would provide both satisfactory DIPJ exposure and minimize the incidence of skin and nail complications. This technique, in our study, yielded a 97.2% bone union rate, remarkable finger alignment correction, and significantly improved VAS scores for pain and satisfaction at an average of 9.8 months postoperatively compared with preoperative scores. We observed no instances of infection or complications related to skin or nails.
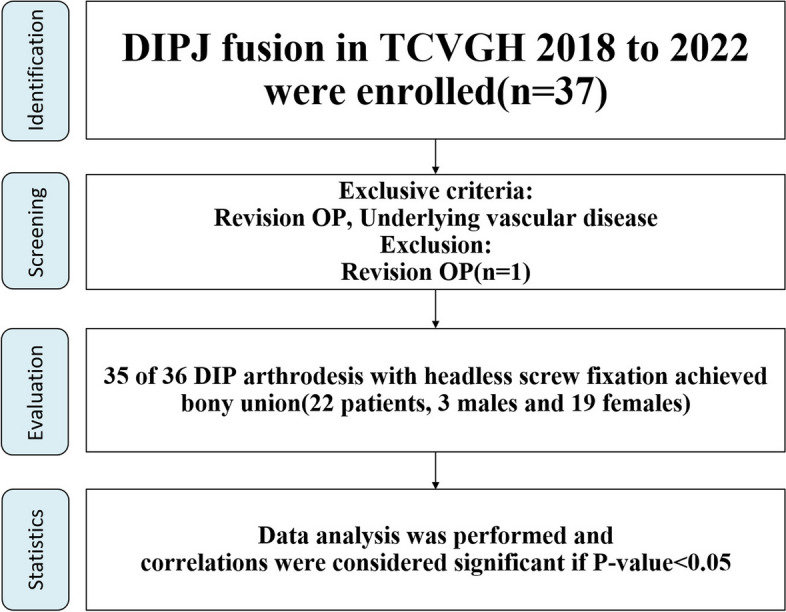
Traditionally, arthrodesis of the DIP joint is performed through a transverse, Y-shape, H-shape, or lazy S-shape around the dorsal aspect of the DIPJ. In contrast, our technique involves an extended simple transverse incision, eschewing the H or Y incision. This avoids the need for a longitudinal incision or sharp-angled skin flap, which frequently result in hypertrophic scars that may restrict joint motion [10, 11]. The "smile incision" begins at the center of the major DIPJ skin crease and then arcs distally towards the lateral aspect of the finger, ensuring a safe distance from the nail germinal matrix. At this juncture, the extensor tendon can be severed at the tendon segment, which is considerably more proximal than the terminal tendon insertion and the nail's germinal matrix [12]. (Fig. 2). The "smile incision" is designed to circumvent direct cutting into the nail germinal matrix. Still, soft tissue dissection should be performed just above the bone surface to avoid damaging the nail germinal matrix. In our series, no skin necrosis, contracted scars, or nail-related complications were observed. This is potentially because the procedure successfully avoids inducing skin ischemia and maintains a safe distance from the nail germinal matrix (Fig. 5).
Fig. 5.
A Preoperative anterior–posterior radiograph shows the advanced osteoarthritis over DIPJ of right index, middle, ring, small finger, left index, middle, ring, and small fingers. B Postoperative 3-month anterior–posterior radiograph shows bone union of the arthrodesis. C Intraoperative photograph of the left hand shows the incisions and skin condition after wound closure. D Postoperative 3-month photograph of bilateral hands shows the well-healed wounds and subsided subungual hematoma
The original shotgun approach was conceived to maximize the exposure of the proximal interphalangeal joint (PIPJ) of the finger by hyperextending the PIPJ. Despite releasing the volar plate, accessory collateral ligament, and the volar part of the collateral ligament, no significant ligament-related complications were noted in the surgical outcomes [13]. In our study, hyperflexion and full joint surface exposure of the DIPJ were achieved by releasing the dorsal capsule, the collateral ligament, and the dorsal part of the accessory collateral ligament. Dorsal DIPJ stability could be reconstructed by implant fixation and subsequent bone union. We found no complications related to blood supply or immediate reduction loss resulting from the release of the accessory collateral ligament. This suggests that neither the blood supply nor the stability of the DIPJ was irreversibly impacted by the release of the accessory collateral ligament and DIPJ hyperflexion of more than 120 degrees in this procedure. However, the dorsal transverse incision does affect venous return, leading to noticeable postoperative swelling. Nevertheless, in all our patients, the swelling typically subsided within an average of two months after the operation, and no cases of massive necrosis were observed.
In this research, headless screws were utilized in all 36 fingers to attain interdigital fixation and inter-fragment compression. Although Kirschner wire is a commonly used implant for DIPJ arthrodesis, the use of a headless screw, which provides inter-fragmental compression, is beneficial for bone union. A biomechanical study suggested that compared to the K-wire, the headless screw exhibited higher stiffness and maximum fracture forces [14, 15]. A systematic review conducted in 2014 deduced that the union rate of patients treated with headless screws was superior to those treated with K-wires (96.1% versus 91.6%)1. In our study, the high bone union rate achieved (35 of 36 patients, translating to 97.2%) was comparable to the union rates reported in existing literature [2, 4, 6, 16–20]. This suggests that the successful bone union rate achieved by the smile incision and reverse shotgun procedure is not inferior to that of traditional incisions employing headless screws. Some authors have reported potential complications from using oversized headless screws, such as fractures at the distal phalangeal tip or thread penetration of the nail bed during screw placement, especially in female patients or in little fingers. If the dorsal cortex is compromised, the nail bed could be damaged, potentially resulting in pain, subungual hematoma, and nail deformity [16, 21, 22]. Iwamoto et al. have reported the potential for symptomatic hardware and nail bed injury when the thread diameter exceeds the anteroposterior diameter of the distal phalanx {Iwamoto, 2013 #19}. In our study, subungual hemorrhage was observed in 17 of the 36 cases (47.2%) in the early postoperative period. Notably, all instances of subungual hemorrhage were due to intraoperative K-wire injury rather than screw oversizing. Nonetheless, by the final follow-up, all incidences of hemorrhage had resolved without residual symptoms. Our experience suggests that such complications can be minimized by opting for more volar screw insertion sites in fingers of smaller diameter and by diligently monitoring the direction of the K-wire using fluoroscopy during surgery.
Another potential issue associated with the use of headless screws is finger length shortening due to interphalangeal compression, which may result in subsequent swan neck deformity [23, 24]. Certain researchers have suggested the utilization of bone grafts derived from Lister's tubercle as a strategy to circumvent the shortening of the finger length [24, 25]. However, the additional bony interface may interfere with the bony union. In our procedure, swan neck deformity can be prevented by overlapping the extension tendon by 2-3 mm during the tendon repair procedure. With this method, swan neck deformity was not observed in our follow-up period.
The various methods, utilized implants, rates of union, rates of complications, and the surgical outcomes that have been reported for DIPJ arthrodesis in the recent decade are comprehensively presented in Table 5 [2, 4, 6, 16–20]. The rates of successful union were found to vary between 91% and 100%. The incidences of significant complications, such as nonunion, fracture, and hardware loosening, ranged from 0 to 14%. This is in contrast to complications like nail dystrophy and skin necrosis, which were reported to have an incidence range of between 11% and 15% [20, 26]. In contrast to studies conducted 15 years ago, recent research has reported no complications related to skin or nails. Most of these studies investigated fewer than 50 cases. The most comprehensive series, involving 102 fingers treated with DIPJ arthrodesis using Arex SCRU2 screws and a transverse incision, reported a union rate of 100%, a remarkably high satisfaction rate (95%, or 97 out of 102 cases), and no skin or nail complications. The authors suggested the low complication rate resulted from the low profile of the Arex SCRU2 screw. However, similar complication-free results were reported in studies using different implants (as seen in Table 5). This implies that the decrease in skin and nail complications might be due to advancements in surgical approaches that prioritize soft tissue preservation.
Table 5.
Approaches, outcomes, implants, and complications in DIP arthrodesis in the literature
| Authors Year |
Digits (n) | Incision | Implants | Union rate, (%) | Union time (months) |
F/U period (months) |
Complications (%) |
|---|---|---|---|---|---|---|---|
| Woo et al. (2022) [4] | 15 | Y-shaped | Multiple screws | 100 | 5.67 | 5.67 |
Skin necrosis (0) Nail deformity (0) Screw removal(13) |
| Auzias et al. (2019) [18] | 22 | H-shaped | Lync implant | 91 | 4.2 | 15 |
Skin necrosis (0) Nail deformity (0) Implant loosening (14) |
| Cox et al. (2014) [6] | 48 | Transverse | Acutrak AcuTwist | 94 | 12 | 12 |
Skin necrosis (0) Nail deformity (0) Nonunion(6) Fracture (2) |
| Song et al. (2012) [16] | 23 | H-shaped | Acutrak screw | 100 | 2.5 | 18 |
Skin necrosis (0) Nail deformity (0) Fixation failure (4) |
|
Han et al. (2014) [2] |
9 | H-shaped | Wiring & K-wire | 100 | 1.9 | 19.6 |
Skin necrosis (0) Nail deformity (0) Wire removal(11) |
|
Iwamoto el al. (2013) [19] |
28 | Y-shaped | Oblique Acutrak screw | 96 | 2.75 | 12 |
Skin necrosis (0) Nail deformity (0) Nonunion(4) |
|
Villani et al (2012) [17] |
102 | Transverse | Arex SCRU2 screw | 100 | 3–6 | 26 |
Skin necrosis (0) Nail deformity (0) Prominent hardware(2) CRPSa(1) Bone callus(1) |
|
Present study (2023) |
36 | Smile | Dart-fire screw | 97 | 3.41 | 9.84 |
Skin necrosis (0) Nail deformity (0) Nonunion(3) |
aCRPS Complex regional pain syndrome
In addition to performing a transverse incision over the DIPJ and transecting the collateral ligament, our method extends the transverse incision to the lateral aspect and releases the accessory collateral ligament, enhancing volar joint exposure. We found that this approach significantly aids in joint preparation and implant insertion without increasing complications. Our surgical method offers an optional treatment technique to enhance surgical outcomes, particularly for inpatients with severe deformities and extensive osteophytes.
However, this study has several limitations. First, our sample size was relatively small, and the follow-up period was short. This could mean that rare or late-onset complications may not have been recorded. Second, as this was a retrospective study, we could not control factors such as patients’ underlying diseases, anesthesia methods, and lifestyle factors. To mitigate this potential bias, we applied the same surgical procedures and postoperative management across all cases. Lastly, we did not directly compare the results of patients who underwent other surgical techniques, so evidence is lacking to definitively show that the smile incision and reverse shotgun approach is superior to other methods.
Despite these limitations, our study is the first to report clinical and radiologic outcomes using the smile incision and reverse shotgun approach for DIPJ arthrodesis. Our results suggest this technique offers a safe and accessible surgical exposure, particularly when more volar joint preparation and more volar implant insertion points are required.
Acknowledgements
We thank K. H. Chen and S.P. Wang for supporting this study.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of TCVGH (CE22238B, 21st, Jun. 2022).
Informed consent statement
Patient consent was waived due to the retrospective design of the study by the Institutional Review Board of TCVGH (CE22238B).
The name of the Internal Review Board (IRB)
Institutional Review Board I &II of Taichung Veterans General Hospital.
Authors’ contributions
Conceptualization, Cheng-En Hsu and Leo Shaw; methodology, Cheng-En Hsu; formal analysis, Yi-Sheng Chiang.; investigation,.; resources, Wei-Chih Wang and Yung-Cheng Chiu; data curation, Yi-Sheng Chiang.; writing—original draft preparation, Yi-Sheng Chiang an Chai-Yu Chang; writing—review and editing, Cheng-En Hsu and Yung-Cheng Chiu; supervision, Yung-Cheng Chiu; project administration, Cheng-En Hsu and Yung-Cheng Chiu.; funding acquisition, Cheng-En Hsu and Yung-Cheng Chiu. All authors have read and agreed to the published version of the manuscript.”
Funding
This research was funded by TCVGH, grant number TCVGH-1115104B”.
Data availability
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yi-Sheng Chiang and Yung-Cheng Chiu co-first authors.
References
- 1.Dickson DR, et al. A systematic review of distal interphalangeal joint arthrodesis. J Hand Microsurg. 2014;6(2):74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Han SH, Cha YS, Song WT. Arthrodesis of distal interphalangeal joints in the hand with interosseous wiring and intramedullary K-wire fixation. Clin Orthop Surg. 2014;6(4):401–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee JK, et al. Distal interphalangeal Joint Arthrodesis using only Kirschner Wires in small distal Phalanges. Handchir Mikrochir Plast Chir. 2021;53(5):462–6. [DOI] [PubMed] [Google Scholar]
- 4.Woo SH, et al. Distal interphalangeal joint arthrodesis with nonaxial multiple small screws: a biomechanical analysis with axial headless compression screw and clinical result of 15 consecutive cases. BMC Musculoskelet Disord. 2022;23(1):504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ko SH, Park JW, Lee TJ. The Inlay Technique with Cortico-Cancellous Olecranon Bone Graft Used for Revision of Failed Distal Interphalangeal Joint Arthrodesis. Medicina (Kaunas). 2022;58(10):1442. [DOI] [PMC free article] [PubMed]
- 6.Cox C, et al. Arthrodesis of the thumb interphalangeal joint and finger distal interphalangeal joints with a headless compression screw. J Hand Surg Am. 2014;39(1):24–8. [DOI] [PubMed] [Google Scholar]
- 7.Wang WC, et al. Functional outcomes and complications of hook plate for bony mallet finger: a retrospective case series study. BMC Musculoskelet Disord. 2021;22(1):281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kohn MD, Sassoon AA, Fernando ND. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474(8):1886–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gumussuyu G, et al. Reliability of subluxation and articular involvement measurements during the assessment of bony mallet finger. Hand Surg Rehabil. 2021;40(1):87–92. [DOI] [PubMed] [Google Scholar]
- 10.Sebastin SJ, et al. Application of the dorsal metacarpal artery perforator flap for resurfacing soft-tissue defects proximal to the fingertip. Plast Reconstr Surg. 2011;128(3):166e–78e. [DOI] [PubMed] [Google Scholar]
- 11.El-Hadidi S, Al-Kdah H. Distal interphalangeal joint arthrodesis with Herbert screw. Hand Surg. 2003;8(1):21–4. [DOI] [PubMed] [Google Scholar]
- 12.Shum C, et al. Examination of the anatomic relationship of the proximal germinal nail matrix to the extensor tendon insertion. J Hand Surg Am. 2000;25(6):1114–7. [DOI] [PubMed] [Google Scholar]
- 13.Cerovac S, Stanley J. Outcome review on the percutaneous release of the proximal interphalangeal joint accessory collateral ligaments. Orthop Rev (Pavia). 2009;1(2): e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Avery, D.M., 3rd, et al., Headless Compression Screw Versus Kirschner Wire Fixation for Metacarpal Neck Fractures: A Biomechanical Study. J Hand Surg Am. 2017. 42(5): 392 e1–392 e6. [DOI] [PubMed]
- 15.Chiu YC, et al. Effect of oblique headless compression screw fixation for metacarpal shaft fracture: a biomechanical in vitro study. BMC Musculoskelet Disord. 2021;22(1):146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Song JH, et al. Distal interphalangeal joint arthrodesis with a headless compression screw: morphometric and functional analyses. Arch Orthop Trauma Surg. 2012;132(5):663–9. [DOI] [PubMed] [Google Scholar]
- 17.Villani F, Uribe-Echevarria B, Vaienti L. Distal interphalangeal joint arthrodesis for degenerative osteoarthritis with compression screw: results in 102 digits. J Hand Surg Am. 2012;37(7):1330–4. [DOI] [PubMed] [Google Scholar]
- 18.Auzias P, et al. Distal interphalangeal joint arthrodesis with the intramedullary Lync((R)) implant: Prospective study of 22 cases. Hand Surg Rehabil. 2019;38(2):114–20. [DOI] [PubMed] [Google Scholar]
- 19.Iwamoto T, et al. An obliquely placed headless compression screw for distal interphalangeal joint arthrodesis. J Hand Surg Am. 2013;38(12):2360–4. [DOI] [PubMed] [Google Scholar]
- 20.Brutus JP, et al. Use of a headless compressive screw for distal interphalangeal joint arthrodesis in digits: clinical outcome and review of complications. J Hand Surg Am. 2006;31(1):85–9. [DOI] [PubMed] [Google Scholar]
- 21.Mintalucci, D., et al., Distal interphalangeal joint bony dimensions related to headless compression screw sizes. J Hand Surg Am, 2014. 39(6): p. 1068–74 e1. [DOI] [PubMed]
- 22.Wyrsch B, et al. Distal interphalangeal joint arthrodesis comparing tension-band wire and Herbert screw: a biomechanical and dimensional analysis. J Hand Surg Am. 1996;21(3):438–43. [DOI] [PubMed] [Google Scholar]
- 23.Jones DB Jr, et al. Arthrodesis as a salvage for failed proximal interphalangeal joint arthroplasty. J Hand Surg Am. 2011;36(2):259–64. [DOI] [PubMed] [Google Scholar]
- 24.Ameline T, et al. Arthrodesis of thumb interphalangeal and finger distal interphalangeal joints using the intramedullary X-Fuse(®) implant: Retrospective analysis of 38 cases. Chir Main. 2015;34(2):67–72. [DOI] [PubMed] [Google Scholar]
- 25.Netscher DT, Hamilton KL. Interphalangeal joint salvage arthrodesis using the lister tubercle as bone graft. J Hand Surg Am. 2012;37(10):2145–9. [DOI] [PubMed] [Google Scholar]
- 26.Stern PJ, Fulton DB. Distal interphalangeal joint arthrodesis: an analysis of complications. J Hand Surg Am. 1992;17(6):1139–45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.