Abstract
This review examines the multifaceted impact of neighborhood-level social determinants of health (SDOH) on cardiovascular disease (CVD) and outlines strategic interventions for mitigating cardiovascular health inequities. Research highlights that environmental and socioeconomic factors within a neighborhood—including education, unemployment, healthcare access, racial segregation, systemic inequities, air quality, housing quality, and other SDOH—influence CVD outcomes. Addressing CVD disparities necessitates a comprehensive strategy that integrates policy reform, enhanced community infrastructure, improved healthcare access, and community empowerment and leverages innovative technology to create equitable health outcomes across diverse populations.
Keywords: zip codes, social determinants of health, cardiovascular health
Introduction
Cardiovascular disease (CVD) remains the leading cause of global mortality and disability,1 influenced not only by traditional risk factors such as smoking, hypertension, dyslipidemia, and diabetes but also by social determinants of health (SDOH), such as socioeconomic status, education, and healthcare access.2 Environmental conditions, including air quality, housing quality, and neighborhood safety, are also crucial in shaping health behaviors and CVD risks.3
Studies highlight the significant impact of zip codes on cardiovascular health, often exceeding the influence of genetic factors.4 For instance, individuals moving to zip codes with prevalent uncontrolled health conditions experience corresponding increases in these comorbidities.5 A Veterans Health Administration cohort analysis showed that relocating to areas with higher rates of uncontrolled health conditions such as hypertension, diabetes, and obesity led to increased incidences of these conditions.5 Additionally, a study involving more than 27,000 patients found that those in the highest quintile of the Area Deprivation Index (ADI) faced greater readmission risks and mortality after cardiovascular hospitalizations, and including ADI in predictive models notably enhanced risk reclassification.6 Another investigation of 49,305 refugees resettled in Denmark from 1986 to 1998 revealed that placement in socioeconomically disadvantaged neighborhoods was linked to increased risks of hypertension, hyperlipidemia, diabetes, and myocardial infarction (MI).7
Addressing cardiovascular health disparities requires a deep understanding of the complex ways through which neighborhood-level SDOH influence CVD. This review explores the several mechanisms through which zip codes impact cardiovascular health disparities and proposes a multifaceted framework for addressing these inequities. The central illustration provides an overview of various neighborhood-level social determinants impacting cardiovascular health along with proposed strategic interventions to mitigate associated health disparities (Figure 1).
Figure 1.
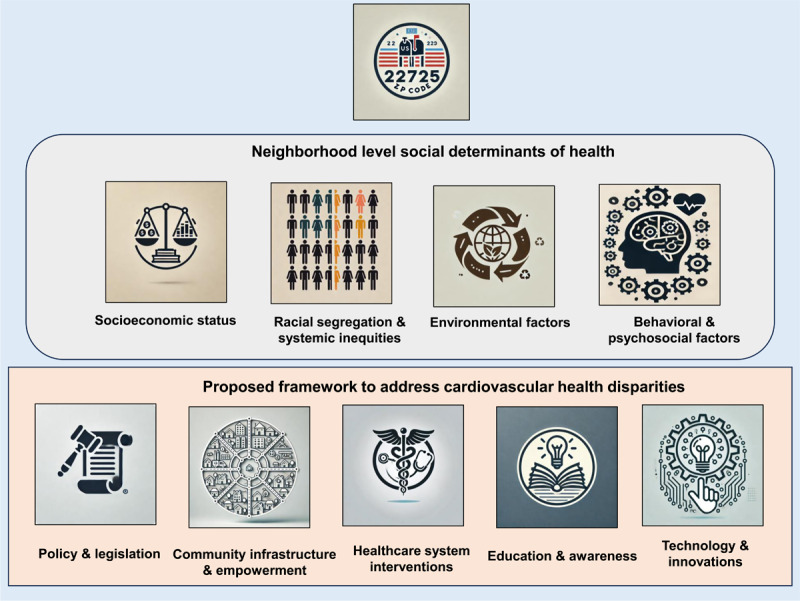
Central illustration shows an overview of neighborhood level social determinants of cardiovascular health and potential solutions to mitigate health disparities.
Neighborhood-level Determinants of Cardiovascular Health
Socioeconomic Status
A clear inverse relationship exists between neighborhood socioeconomic status (SES) and CVD.8 While higher socioeconomic levels are associated with decreased CVD risk, residents in lower-income neighborhoods face substantial obstacles, such as limited access to health care, fewer healthy food options, and inadequate recreational facilities.8,9,10,11 A longitudinal study in Israel found a heightened risk of stroke among individuals in lower SES neighborhoods after MI, attributed to community-induced stress and suboptimal care.12 Another French study observed an inverse relationship between neighborhood deprivation and coronary heart disease (CHD) incidence, only partly explained by traditional CVD risk factors.13 The residents of US counties with higher socioeconomic deprivation, indicated by the Social Deprivation Index and ADI, were shown to be significantly associated with higher rates of premature CVD mortality.10 Both indices accounted for a substantial portion of the variation in county CVD mortality, with the most deprived counties showing smaller reductions in premature CVD mortality over the analyzed period. Another study highlighted that young adults (≤ 45 years) in US counties with high socioeconomic vulnerability indices experienced a > 10% increase in preventable CVD mortality compared with those in more affluent areas.14
Racial Segregation
Neighborhood-level racial segregation significantly increases the risk of CVD, especially within Black communities.15 Studies have shown that Black adults in segregated areas have a 12% greater risk of developing CVD compared with White adults, a disparity driven by inequities in healthcare access, fewer resources, and historical socioeconomic injustices.15,16,17 The National Health and Nutrition Examination Survey (1999-2006) of over 8,000 participants found that Black adults had nearly 3-fold higher odds of hypertension than White adults, but these disparities were notably smaller in areas with low racial segregation.18 The disparities were pronounced in segregated low-poverty areas and most diminutive in non-segregated high-poverty areas. Another study analyzed diabetes mortality between Black and White populations across the 50 most populous US cities; it showed that Blacks had significantly higher mortality rates in 39 out of 41 cities, ranging from 57% higher in Baltimore to 4-fold higher in Washington, DC.17 Economic inequality and segregation were correlated with these disparities. Specifically, adjusting for both Black/White poverty and segregation explained 72.6% of the mortality disparity.
Healthcare Access
Geographic location significantly dictates access to health care, directly influencing cardiovascular outcomes.3,5 Rural areas often lack specialized cardiac care facilities, imposing delays in treatment that can exacerbate health conditions.5,19 For instance, the availability and utilization of aortic valve replacement procedures and a scarcity of transcatheter aortic valve replacement (TAVR) programs in rural regions significantly impact mortality rates.20 A study indicated that individuals in rural counties of Florida traveled an additional 44 miles to receive TAVR and underwent the procedure at rates approximately seven-times lower than those in more densely populated areas.21
Urban residents in poor areas may also face a lack of nearby healthcare facilities and extended wait times, further complicating health management.9 Research shows a notable variation in challenges accessing medical care across US states, with a median difficulty rate of 13% for the general population.19 In US states without expanding Medicaid, 1 in 6 residents reported difficulty accessing care.19 These factors contribute to reduced life expectancy; for example, US rural regions have consistently reported higher age-adjusted mortality rates compared to urban areas, with Black individuals exhibiting higher mortality than other races.22
Environmental Factors
Environment factors such as air quality, housing quality, availability of grocery stores with healthy food choices, the walkability of the area, facilities for physical activities, and the presence of greenspace are linked to achieving optimal cardiovascular health.3,23 Aided by deep learning, a cross-sectional study analyzed 0.53 million Google Street View images from 789 census tracts across seven US cities to measure the built environment’s impact on CHD prevalence.24 Features from these images, interpreted through convolutional neural networks and activation maps, explained 63% of the variance in CHD rates, enhancing predictions over models based solely on demographic and socioeconomic data.24 The analysis identified specific neighborhood characteristics, such as buildings and roads, significantly associated with CHD prevalence.
Another study examined 71,659 US Census tracts and found that neighborhoods in the highest quartile for environmental burden had significantly elevated rates of hypertension, diabetes, obesity, CHD, and stroke compared with those in the lowest quartile.25 The link between environmental burden and cardiovascular health was notably robust in socially vulnerable neighborhoods. On the same note, accelerated urban growth and industrial activities have significantly increased air pollution, posing a critical environmental and health challenge.26 The 2004 American Heart Association (AHA) scientific statement identified a connection between exposure to particulate matter and cardiovascular incidents.27 The 2010 AHA update further emphasized the detrimental effects of particulate matter 2.5 (PM2.5) on cardiovascular health.28 Research has demonstrated the association of acute exposure to PM2.5 with MI, stroke, arrhythmias, and heart failure,29 while prolonged exposure has been shown to reduce life expectancy in populations subjected to high levels of these particles.30
Social Determinants
Neighborhood variations in several other SDOH, such as education, employment opportunities, and income levels, critically shape cardiovascular health.9 Higher educational attainment typically leads to improved health outcomes due to better employment prospects and enhanced access to health care.9,31 Conversely, lower educational achievements can restrict job opportunities, diminishing economic potential and worsening health outcomes.9,32 For instance, a study in Australia and New Zealand revealed that individuals with only primary education face higher risks of cardiovascular and all-cause mortality compared to those with tertiary education, with key risk factors being smoking, obesity, and physical inactivity.8
Additionally, lower education often results in reduced participation in tertiary prevention programs like cardiac rehabilitation, exacerbating health disparities.8,31 Another study conducted in the US and Finland identified a persistent increased risk of nonfatal MI and sudden cardiac death among low-income groups, with findings consistent on both individual and neighborhood scales.11 Another report observed that a $10,000 rise in a neighborhood’s median income corresponded with a 10% decrease in mortality for its residents.33
Similarly, research has highlighted the impact of unemployment on cardiovascular health. A French study found that unemployment in the French population led to a 20% increased risk of CHD, with diet and lifestyle factors such as alcohol consumption and smoking explaining nearly half of this risk.34 Similarly, another US report identified that unemployment was associated with a 35% increased risk of MI in the first year alone, with repeated job losses and extended periods of unemployment compounding this risk.35
Systemic Inequities
Historical systemic injustices, such as redlining, have perpetuated disparities in housing and neighborhood resources.4,12,16,36,37 These practices have historically obstructed homeownership among Black adults and relegated them to resource-poor neighborhoods, fostering conditions conducive to higher CVD rates and mortality.4,36,37 In a US study, veterans residing in historically redlined (grade D) neighborhoods had a 14% higher risk of experiencing cardiovascular events compared with those in lowest-risk (grade A) areas; the risks of MI and all-cause death were increased by 15% and 13%, respectively.36 Furthermore, socioeconomically disadvantaged neighborhoods, often marked by higher pollution levels, have been linked to a 25% increase in the risk of incident CVD and all-cause mortality in Black versus White populations.38 Moreover, neighborhoods with over 60% Hispanic residents experience up to 30% greater exposure to harmful air pollutants such as PM2.5 than areas with lower than 25% Hispanic populations.16
Behavioral and Psychological Factors
Behavioral and psychosocial risk factors such as smoking, physical inactivity, and unhealthy diets are more prevalent in socioeconomically disadvantaged neighborhoods.9 Additionally, residents in these areas often experience higher levels of chronic stress and depression, further exacerbating CVD risks.39 The REGARDS (Reasons for Geographic and Racial Differences in Stroke) study indicated that individuals with an annual income below $35,000 who experience both stress and depressive symptoms faced an approximately 50% increased risk of developing CVD and a 33% increase in all-cause mortality.40 Moreover, research shows that these disparities have a pronounced gender aspect. The WISE (Women’s Ischemic Syndrome Evaluation) study found that women with CHD and low SES incur higher drug costs and suffer more frequent hospitalizations than their higher-income counterparts.41 In Southern Alberta’s healthcare system, the influence of neighborhood SES on the use of cardiac catheterization and the subsequent 30-day mortality rates post-acute coronary syndrome was noted exclusively among women.42
Blueprint for Achieving Equitable Cardiovascular Health
Addressing neighborhood-level SDOH and mitigating CVD risk requires a multidimensional strategy encompassing policy reform, infrastructure enhancement, healthcare improvements, educational initiatives, and community empowerment. The subsequent sections detail these critical elements, providing a framework for potential interventions to enhance cardiovascular health across diverse communities. This approach emphasizes the need for comprehensive, coordinated efforts tailored to the specific needs and contexts of different communities.
Policy and Legislation
Reforming housing policies to enforce fair housing laws is essential for diminishing racial segregation and promoting inclusive communities.36,37 Expanding affordable housing initiatives diversifies neighborhood demographics, thereby reducing health disparities.37 Additionally, enforcing stringent building codes ensures better living conditions, thereby improving health outcomes. Economic revitalization of underserved areas through tax incentives encourages business investment, enhances local employment opportunities, and promotes healthy lifestyles through living wage policies.8,9,11 Expanding Medicaid coverage provides essential healthcare access to underserved populations, and increased funding for community health centers enhances primary care services.19 Implementing stringent air quality standards and regulating industrial pollutants reduce environmental cardiovascular risks,27,28 while urban planning incorporating green spaces promotes physical activity and mitigates urban heat, contributing to cardiovascular health.25
Community Infrastructure
Enhancing public transportation systems, creating bike lanes, and making streets more pedestrian-friendly significantly improve physical activity.7,21,25,33,40,41 Similarly, developing parks and recreational facilities in marginalized areas encourages physical activity, while community centers offering fitness programs cater to all ages and abilities, promoting active lifestyles from a young age.3,11,15,22,25,40,42 Subsidizing transportation costs for low-income residents increases access to health care and healthy food options.5,19,34,43 Addressing food deserts by incentivizing grocery stores in underserved areas, supporting farmers’ markets, and funding community gardens ensures access to nutritious food.13,33,43
Healthcare System Interventions
Increasing the availability of primary care facilities in underserved areas and deploying mobile health clinics and community health workers dramatically improve access to preventative and ongoing care, while establishing satellite clinics for specialized cardiac care reduces travel time for specialized services.44,45 Telehealth initiatives bridge the gap between rural patients and healthcare providers.19 Expanding screening programs for CVD risk factors and integrating workplace and school-based health programs facilitate early identification and mitigation of risk factors as well as support with symptom monitoring and medication adherence.44,45
Education and Awareness
Developing culturally and linguistically appropriate health education materials enhances understanding and engagement in health management.8,9,11,31 Integrating health education into school curricula and community-based health programs empowers individuals to make informed health decisions.31 Smoking cessation programs, community exercise initiatives, and nutrition education significantly influence lifestyle choices and must be accessible and tailored to meet the community’s unique needs.7,9,31,33,35 Leveraging media and social media for targeted public health campaigns raises awareness and effectively educates the public on cardiovascular health.46
Community Empowerment
Supporting the formation of neighborhood health committees and facilitating community-led health assessments empowers residents to identify and act on their health needs.9,47,48 Participatory budgeting for health initiatives ensures community involvement in allocating local health resources.47,48 Providing leadership training for community health advocates and developing mentorship programs for youth builds long-term capacity for community health management.47,48 Establishing support groups for individuals with CVD and at-risk populations provides crucial emotional and practical support, reducing isolation and promoting health-enhancing behaviors.40,48
Technology and Innovation
Utilizing advanced technologies such as a geographical information system (GIS) for resource allocation and neighborhood-level health tracking systems optimizes health interventions.24 Predictive modeling based on SDOH helps anticipate health trends and prepare appropriate responses.49 Mobile apps for health management, wearable technologies for health monitoring, and AI-powered chatbots for health education transform the approach to cardiovascular health management.32 Incorporating health considerations into smart city initiatives, such as air quality monitoring and traffic management, enhances urban living conditions and health outcomes.23
Partnerships and Collaboration
Collaborations across health care, education, housing, and other sectors are crucial for addressing SDOH.9,48 Public-private partnerships and alliances between academia and community organizations amplify the impact of health interventions.50,51 Innovative funding strategies like social impact bonds and community development financial institutions focused on health sustain long-term health initiatives.50,51 Establishing networks for sharing best practices and facilitating collaborations across cities and nations accelerates progress in addressing health disparities.48,50,51
Conclusion
The profound impact of neighborhood-level SDOH on CVD underscores the need for a holistic approach to mitigate cardiovascular health disparities. While this review has detailed the complex interplay between several neighborhood-level SDOH, effective intervention requires implementing targeted healthcare strategies and broader societal changes that address the root causes of health disparities. By fostering community empowerment, leveraging technology and innovation, and enhancing infrastructure, we can create healthier environments that enable all individuals, regardless of zip code, to achieve optimal cardiovascular health.
Key Points
Neighborhood-level social determinants of health, including socioeconomic status, racial segregation, and environmental factors, significantly impact cardiovascular disease (CVD).
Disparities in access to health care, influenced by geographic location and community infrastructure, exacerbate cardiovascular health inequities, especially in rural areas and segregated communities.
Comprehensive interventions that address both individual and neighborhood-level factors are necessary to mitigate CVD disparities effectively.
Multisector collaborations and the integration of advanced technologies, such as GIS and telehealth, are essential for developing sustainable solutions to reduce cardiovascular health inequities.
CME Credit Opportunity
Houston Methodist is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
Houston Methodist designates this Journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Click to earn CME credit: learn.houstonmethodist.org/MDCVJ-20.5.
Acknowledgements
Central illustration was created using DALL.E (ChatGPT: www.chatgpt.com).
Competing Interests
The author has no competing interests to declare.
References
- 1.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017. Sep 16;390(10100):1151-1210. doi: 10.1016/S0140-6736(17)32152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan SU, Javed Z, Lone AN, et al. Social Vulnerability and Premature Cardiovascular Mortality Among US Counties, 2014 to 2018. Circulation. 2021. Oct 19;144(16):1272-1279. doi: 10.1161/CIRCULATIONAHA.121.054516 [DOI] [PubMed] [Google Scholar]
- 3.Bhatnagar A. Environmental Determinants of Cardiovascular Disease. Circ Res. 2017. Jul 7;121(2):162-180. doi: 10.1161/CIRCRESAHA.117.306458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powell-Wiley TM. Disentangling Ancestry From Social Determinants of Health in Hypertension Disparities-An Important Step Forward. JAMA Cardiol. 2021. Apr 1;6(4):398-399. doi: 10.1001/jamacardio.2020.6573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baum A, Wisnivesky J, Basu S, Siu AL, Schwartz MD. Association of Geographic Differences in Prevalence of Uncontrolled Chronic Conditions With Changes in Individuals’ Likelihood of Uncontrolled Chronic Conditions. JAMA. 2020. Oct 13;324(14):1429-1438. doi: 10.1001/jama.2020.14381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson AE, Zhu J, Garrard W, et al. Area Deprivation Index and Cardiac Readmissions: Evaluating Risk-Prediction in an Electronic Health Record. J Am Heart Assoc. 2021. Jul 6;10(13):e020466. doi: 10.1161/JAHA.120.020466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hamad R, Öztürk B, Foverskov E, et al. Association of Neighborhood Disadvantage With Cardiovascular Risk Factors and Events Among Refugees in Denmark. JAMA Netw Open. 2020. Aug 3;3(8):e2014196. doi: 10.1001/jamanetworkopen.2020.14196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woodward M, Peters SA, Batty GD, et al. Socioeconomic status in relation to cardiovascular disease and cause-specific mortality: a comparison of Asian and Australasian populations in a pooled analysis. BMJ Open. 2015. Mar 17;5(3):e006408. doi: 10.1136/bmjopen-2014-006408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic Status and Cardiovascular Outcomes: Challenges and Interventions. Circulation. 2018. May 15;137(20):2166-2178. doi: 10.1161/CIRCULATIONAHA.117.029652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bevan GH, Nasir K, Rajagopalan S, Al-Kindi S. Socioeconomic Deprivation and Premature Cardiovascular Mortality in the United States. Mayo Clin Proc. 2022. Jun;97(6):1108-1113. doi: 10.1016/j.mayocp.2022.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kucharska-Newton AM, Harald K, Rosamond WD, Rose KM, Rea TD, Salomaa V. Socioeconomic indicators and the risk of acute coronary heart disease events: comparison of population-based data from the United States and Finland. Ann Epidemiol. 2011. Aug;21(8):572-9. doi: 10.1016/j.annepidem.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerber Y, Koton S, Goldbourt U, et al. Poor neighborhood socioeconomic status and risk of ischemic stroke after myocardial infarction. Epidemiology. 2011. Mar;22(2):162-9. doi: 10.1097/EDE.0b013e31820463a3 [DOI] [PubMed] [Google Scholar]
- 13.Silhol R, Zins M, Chauvin P, Chaix B. Investigating the spatial variability in incidence of coronary heart disease in the Gazel cohort: the impact of area socioeconomic position and mediating role of risk factors. J Epidemiol Community Health. 2011. Feb;65(2):137-43. doi: 10.1136/jech.2009.087379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khan SU, Kumar P, Arshad A, et al. Social Vulnerability and Potentially Preventable Cardiovascular Deaths Among Younger Adults in the U.S. Counties, 2014-2018. JACC Adv. 2023. Feb 8;2(2):100196. doi: 10.1016/j.jacadv.2022.100196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reddy NM, Mayne SL, Pool LR, et al. Exposure to Neighborhood-Level Racial Residential Segregation in Young Adulthood to Midlife and Incident Subclinical Atherosclerosis in Black Adults: The Coronary Artery Risk Development in Young Adults Study. Circ Cardiovasc Qual Outcomes. 2022. Feb;15(2):e007986. doi: 10.1161/CIRCOUTCOMES.121.007986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones MR, Diez-Roux AV, Hajat A, et al. Race/ethnicity, residential segregation, and exposure to ambient air pollution: the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Public Health. 2014. Nov;104(11):2130-7. doi: 10.2105/AJPH.2014.302135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenstock S, Whitman S, West JF, Balkin M. Racial disparities in diabetes mortality in the 50 most populous US cities. J Urban Health. 2014. Oct;91(5):873-85. doi: 10.1007/s11524-013-9861-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abrahamowicz AA, Ebinger J, Whelton SP, Commodore-Mensah Y, Yang E. Racial and Ethnic Disparities in Hypertension: Barriers and Opportunities to Improve Blood Pressure Control. Curr Cardiol Rep. 2023. Jan;25(1):17-27. doi: 10.1007/s11886-022-01826-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al Rifai M, Mahtta D, Kherallah R, et al. Prevalence and Determinants of Difficulty in Accessing Medical Care in U.S. Adults. Am J Prev Med. 2021. Oct;61(4):492-500. doi: 10.1016/j.amepre.2021.03.026 [DOI] [PubMed] [Google Scholar]
- 20.Gupta T, Kalra A, Kolte D, et al. Regional Variation in Utilization, In-hospital Mortality, and Health-Care Resource Use of Transcatheter Aortic Valve Implantation in the United States. Am J Cardiol. 2017. Nov 15;120(10):1869-1876. doi: 10.1016/j.amjcard.2017.07.102 [DOI] [PubMed] [Google Scholar]
- 21.Damluji AA, Epstein R, Moscucci M, et al. Healthcare access to TAVR procedures by population density: a focus on healthcare disparity in Florida. Circulation. 2019. Nov 11;140 (Suppl_1):A14981-A. [Google Scholar]
- 22.Cross SH, Mehra MR, Bhatt DL, et al. Rural-Urban Differences in Cardiovascular Mortality in the US, 1999-2017. JAMA. 2020. May 12;323(18):1852-1854. doi: 10.1001/jama.2020.2047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Danielli S, Ashrafian H, Darzi A. Healthy city: global systematic scoping review of city initiatives to improve health with policy recommendations. BMC Public Health. 2023. Jul 1;23(1):1277. doi: 10.1186/s12889-023-15908-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Z, Dazard J-E, Khalifa Y, Motairek I, Al-Kindi S, Rajagopalan S. Artificial intelligence-based assessment of built environment from Google Street View and coronary artery disease prevalence. Eur Heart J. 2024. May 7;45(17):1540-1549. doi: 10.1093/eurheartj/ehae158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu M, Patel VR, Salas RN, et al. Neighborhood Environmental Burden and Cardiovascular Health in the US. JAMA Cardiol. 2024. Feb 1;9(2):153-163. doi: 10.1001/jamacardio.2023.4680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan SU, Al-Mallah MH. Air pollution and acute coronary syndrome: The air we breathe. Atherosclerosis. 2024. Mar:390:117453. doi: 10.1016/j.atherosclerosis.2024.117453 [DOI] [PubMed] [Google Scholar]
- 27.Brook RD, Franklin B, Cascio W, et al. Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation. 2004. Jun 1;109(21):2655-71. doi: 10.1161/01.CIR.0000128587.30041.C8 [DOI] [PubMed] [Google Scholar]
- 28.Brook RD, Rajagopalan S, Pope CA 3rd, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010. Jun 1;121(21):2331-78. doi: 10.1161/CIR.0b013e3181dbece1 [DOI] [PubMed] [Google Scholar]
- 29.Pope CA 3rd, Muhlestein JB, May HT, Renlund DG, Anderson JL, Horne BD. Ischemic heart disease events triggered by short-term exposure to fine particulate air pollution. Circulation. 2006. Dec 5;114(23):2443-8. doi: 10.1161/CIRCULATIONAHA.106.636977 [DOI] [PubMed] [Google Scholar]
- 30.Beelen R, Hoek G, van den Brandt PA, et al. Long-term effects of traffic-related air pollution on mortality in a Dutch cohort (NLCS-AIR study). Environ Health Perspect. 2008. Feb;116(2):196-202. doi: 10.1289/ehp.10767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Lancet Public Health. Education: a neglected social determinant of health. Lancet Public Health. 2020. Jul;5(7):e361. doi: 10.1016/S2468-2667(20)30144-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khan SU. Cardiovascular Disease Prevention With mHealth Innovations: Transforming Wellness Through Wireless. Circ Cardiovasc Qual Outcomes. 2024. Jul;17(7):e011005. doi: 10.1161/CIRCOUTCOMES.124.011005 [DOI] [PubMed] [Google Scholar]
- 33.Gerber Y, Weston SA, Killian JM, Therneau TM, Jacobsen SJ, Roger VL. Neighborhood income and individual education: effect on survival after myocardial infarction. Mayo Clin Proc. 2008. Jun;83(6):663-9. doi: 10.4065/83.6.663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Méjean C, Droomers M, van der Schouw YT, et al. The contribution of diet and lifestyle to socioeconomic inequalities in cardiovascular morbidity and mortality. Int J Cardiol. 2013. Oct 15;168(6):5190-5. doi: 10.1016/j.ijcard.2013.07.188 [DOI] [PubMed] [Google Scholar]
- 35.Dupre ME, George LK, Liu G, Peterson ED. The cumulative effect of unemployment on risks for acute myocardial infarction. Arch Intern Med. 2012. Dec 10;172(22):1731-7. doi: 10.1001/2013.jamainternmed.447 [DOI] [PubMed] [Google Scholar]
- 36.Deo SV, Motairek I, Nasir K, et al. Association Between Historical Neighborhood Redlining and Cardiovascular Outcomes Among US Veterans With Atherosclerotic Cardiovascular Diseases. JAMA Netw Open. 2023. Jul 3;6(7):e2322727. doi: 10.1001/jamanetworkopen.2023.22727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Swope CB, Hernández D. Housing as a determinant of health equity: A conceptual model. Soc Sci Med. 2019. Dec:243:112571. doi: 10.1016/j.socscimed.2019.112571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Erqou S, Clougherty JE, Olafiranye O, et al. Particulate Matter Air Pollution and Racial Differences in Cardiovascular Disease Risk. Arterioscler Thromb Vasc Biol. 2018. Apr;38(4):935-942. doi: 10.1161/ATVBAHA.117.310305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Joynt KE, Whellan DJ, O’Connor CM. Depression and cardiovascular disease: mechanisms of interaction. Biol Psychiatry. 2003. Aug 1;54(3):248-61. doi: 10.1016/s0006-3223(03)00568-7 [DOI] [PubMed] [Google Scholar]
- 40.Sumner JA, Khodneva Y, Muntner P, et al. Effects of Concurrent Depressive Symptoms and Perceived Stress on Cardiovascular Risk in Low- and High-Income Participants: Findings From the Reasons for Geographical and Racial Differences in Stroke (REGARDS) Study. J Am Heart Assoc. 2016. Oct 10;5(10):e003930. doi: 10.1161/JAHA.116.003930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shaw LJ, Merz CN, Bittner V, et al. Importance of socioeconomic status as a predictor of cardiovascular outcome and costs of care in women with suspected myocardial ischemia. Results from the National Institutes of Health, National Heart, Lung and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation (WISE). J Womens Health (Larchmt). 2008. Sep;17(7):1081-92. doi: 10.1089/jwh.2007.0596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fabreau GE, Leung AA, Southern DA, et al. Sex, socioeconomic status, access to cardiac catheterization, and outcomes for acute coronary syndromes in the context of universal healthcare coverage. Circ Cardiovasc Qual Outcomes. 2014. Jul;7(4):540-9. doi: 10.1161/CIRCOUTCOMES.114.001021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Campanera M, Gasull M, Gracia-Arnaiz M. Food Security as a Social Determinant of Health: Tackling Inequalities in Primary Health Care in Spain. Health Hum Rights. 2023. Jun;25(1):9-21. [PMC free article] [PubMed] [Google Scholar]
- 44.Takahashi EA, Schwamm LH, Adeoye OM, et al. An Overview of Telehealth in the Management of Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2022. Dec 20;146(25):e558-e568. doi: 10.1161/CIR.0000000000001107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haleem A, Javaid M, Singh RP, Suman R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int. 2021:2:100117. doi: 10.1016/j.sintl.2021.100117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ladeiras-Lopes R, Baciu L, Grapsa J, et al. Social media in cardiovascular medicine: a contemporary review. Eur Heart J Digit Health. 2020. Nov 30;1(1):10-19. doi: 10.1093/ehjdh/ztaa004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Syme SL. Social determinants of health: the community as an empowered partner. Prev Chronic Dis. 2004. Jan;1(1):A02. [PMC free article] [PubMed] [Google Scholar]
- 48.Thompson B, Molina Y, Viswanath K, Warnecke R, Prelip ML. Strategies To Empower Communities To Reduce Health Disparities. Health Aff (Millwood). 2016. Aug 1;35(8):1424-8. doi: 10.1377/hlthaff.2015.1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nasir K, Javed Z, Khan SU, Jones SL, Andrieni J. Big Data and Digital Solutions: Laying the Foundation for Cardiovascular Population Management CME. Methodist Debakey Cardiovasc J. 2020. Oct-Dec;16(4):272-282. doi: 10.14797/mdcj-16-4-272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gondi S, Chokshi DA. Public Health and Payers-Bridging the Gap to Boost Public Health Investment. JAMA Health Forum. 2022. Jul 1;3(7):e222750. doi: 10.1001/jamahealthforum.2022.2750 [DOI] [PubMed] [Google Scholar]
- 51.Crowley R, Mathew S, Hilden D. Health and Public Committee of the American College of Physicians. Modernizing the United States’ Public Health Infrastructure: A Position Paper From the American College of Physicians. Ann Intern Med. 2023. Aug;176(8):1089-1091. doi: 10.7326/M23-0670 [DOI] [PubMed] [Google Scholar]


