Abstract
Cardiovascular disease (CVD) represents a significant financial burden on patients and families, compounded by both direct and indirect healthcare costs. The increasing prevalence of CVD, coupled with the rising costs of treatment, exacerbates financial toxicity—defined as the economic strain and associated physical, emotional, and behavioral consequences on patients. This review explores the scope of financial toxicity in CVD care, detailing its prevalence, associated risk factors, and the complex interplay with social determinants of health such as income, insurance status, and comorbidities. Drawing from models in oncology, we highlight key interventions aimed at mitigating financial toxicity, including patient counseling, financial navigation, and enhanced patient-physician cost discussions. By adopting these approaches, healthcare providers can better support patients with CVD in managing both their health and financial well-being, potentially improving clinical outcomes. Future research is needed to develop standardized assessment tools for financial toxicity in CVD and implement system-wide mitigation strategies.
Keywords: financial toxicity, cardiovascular disease, social determinants of health
Introduction
The United States (US) expenditures on cardiovascular disease (CVD) were estimated to be $555 billion in 2016 and are projected to grow to $1.1 trillion by 2035.1 Cardiovascular disease is the leading cause of death (23%) in the US and affects 41.5% of the US population. With this rising cost and disease prevalence, increasing financial burden is being deferred to individual patients and their families in the form of higher deductibles, co-pays, and co-insurance.2 These costs are compounded by the many sources of indirect costs such as transportation and parking fees, childcare, and lower wages due to sick days and morbidity from CVD.3,4,5,6
The impact of such costs on patient well-being are multifactorial and profound. Cost-related medical nonadherence—by missing clinic appointments, reducing or skipping medication doses, or foregoing care altogether—has a direct impact on cardiovascular outcomes, resulting in more frequent emergency room admissions, longer length of stay, and further financial strain.7 Medical debt can further lead to other negative coping behaviors, such as poor diet, social isolation, and poor mental health and has been associated with lower overall survival.8,9,10
The purpose of this review is to define various aspects of financial toxicity in CVD and report on its prevalence, identify risk factors for financial toxicity in CVD, and share ongoing interventions to mitigate financial toxicity in CVD as well as oncology models that may benefit patients with CVD. We hope to provide readers with the tools necessary to assess for financial toxicity at the point-of-care and system-wide and consider various strategies for mitigation.
Financial Hardship, Burden, and Toxicity
Definition
Prior to the early 2010s, a variety of terminology was used to describe the adverse financial conditions due to medical care, including medical bankruptcy, financial strain, and economic hardship.11 Around this time, oncologists led efforts to address the exorbitant financial burden that patients with cancer faced, primarily due to rising costs of medications. The American Society of Clinical Oncology created a Cost of Cancer Care Task Force in 2007 and published the first and only guideline dedicated to cost of care. They emphasized the need to understand the drivers of cost in cancer care and recommended ways to improve physician and patient cost-related communication and education.12 With the enactment of the Affordable Care Act in 2010, approximately 20 to 24 million people gained access to insurance; however, the out-of-pocket cost of medical care has remained high and has led to rising concerns among patients, physicians, advocates, and policymakers.13
With the expanding literature in the past decade primarily in oncology, the terminology regarding financial strain due to medical care has been further standardized. Financial burden refers to the objective medical bills—out-of-pocket cost as it relates to household income. They may include the costs secondary to a medical encounter, which include but are not limited to prescription drug costs, laboratory and imaging tests, procedures, clinic visits, emergency room visits, and hospital admissions.4 In addition, the costs associated with transportation, childcare, and loss in income due to missed hours at work or disability from a medical condition can all impose objective financial strain on patients and their families. Financial hardship refers to the subjective distress patients experience with regard to the financial burden.4 The psychological stress from medical bills is a critical aspect of the patient experience and a link to deferred medical care that is distinct from the actual cost of care.14 Financial toxicity, on the other hand, is the term used to describe the resulting consequences of treatments and disease, such as negative emotional, physical, and behavioral changes. It was first conceptualized, measured, and validated in oncology to describe the comprehensive impact of medical bills on patients’ overall quality of life.4
Assessment Tools and Prevalence
In CVD, the financial burden of care has been investigated via billing data and national health surveys (see Figure 1). The Medical Expenditure Panel Survey (MEPS) was queried to determine the prevalence of financial burden, defined as “high financial burden” if more than 20% of annual post-subsistence income (the difference between income and food-related subsistence expenses) was spent on healthcare expenditure and “catastrophic” if it exceeded 40% of annual post-subsistence income.15 Among 22,521 adults with self-reported coronary or cerebrovascular disease (“atherosclerotic cardiovascular disease” or ASCVD) between 2006 to 2015, the average annual out-of-pocket expenses was $2,227. Almost 3 million families (13.7%) of patients with ASCVD reported high financial burden, with 1 million families (4.9%) reporting catastrophic financial burden.15 Patients with heart failure were also found to have significant burden of out-of-pocket costs ($4,423), with similar proportions experiencing high (14%) and catastrophic (5%) financial burden.16
Figure 1.
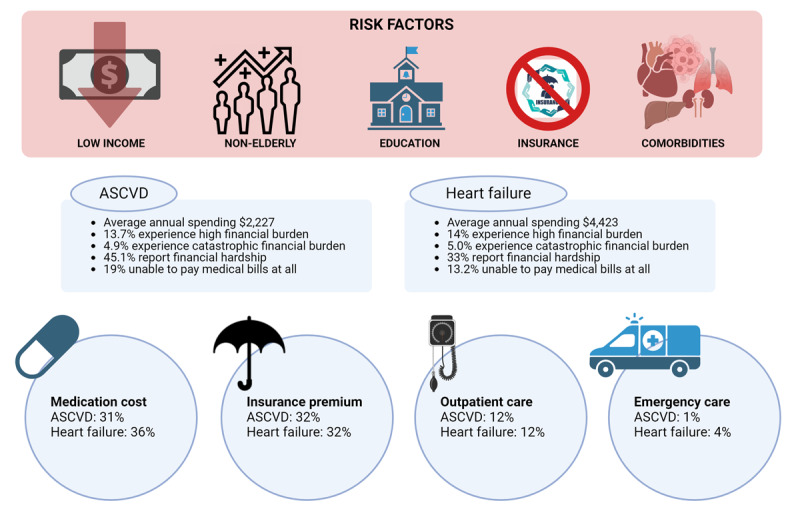
Financial toxicity prevalence and risk factors in cardiovascular disease. ASCVD: atherosclerotic cardiovascular disease
The greater share of the financial burden in CVD has been attributed to medications, specifically to 45% of out-of-pocket spending in ASCVD and 36% in heart failure.15,16 For example, the estimated 2024 co-pay for aldosterone receptor and neprilysin inhibitors is $700/month, proprotein convertase subtilisin/kexin type 9 inhibitor (PCSK9i) is $550/month, and sodium glucose transporter-2 inhibitor (SGLT2i) is $600/month17,18; together, this confers a cost that is almost 60% of the median US income in 2022 according to the US Census Bureau.19 A Medicare data analysis showed the average cost of guideline-directed medical therapy (GDMT) for heart failure ranging from $159 for the three original generic medications including beta-blocker, angiotensin converting enzyme inhibitor (ACEi), and mineralocorticoid receptor antagonist (MRA) to as high as $2,217 when replacing ACEi with angiotensin receptor neprilysin inhibitors and adding SGLT2i.20 Similar discrepancy in estimates were found using claims data from Optum Clinformatics (Optum, Inc.), with higher co-pays estimated for angiotensin receptor neprilysin inhibitors compared with ACEi, regardless of whether the patient had commercial insurance ($828 per year vs. $80.88 per year) or Medicare advantage ($744 per year vs. $30.24 per year).21 SGLT2i were also found to be costly regardless of Medicare or private insurances, with an average cost (according to the MEPS data) of $138 per month or $1,656 per year, which is likely prohibitive for some.22
Valero-Elizondo et al. (2019) first described the prevalence of financial hardship in patients with ASCVD using the National Health Interview Survey (NHIS).23 The survey assessed financial hardship with a binary question regarding “any financial hardship from medical bills” in the past 12 months as well as a binary question on the patient’s “inability to pay medical bills at all.” Interestingly, a much higher prevalence of subjective financial hardship was found: 45.1% compared to objective financial burden estimates (13.7%), with 18.9% reporting being unable to pay medical bills at all. Similarly, for patients with heart failure, 33% reported any financial hardship due to medical bills, and 13.2% were not able to pay bills at all.24 Whether patients receiving care for preventive cardiovascular medicine, valvular disease, or arrhythmias face similar financial burden and hardship is unknown, and out-of-pocket costs have not yet been systematically assessed.
Financial toxicity, the comprehensive impact of medical bills and subjective toll on negative mental, physical, and coping behaviors, is critical to understanding and mitigating the impact of financial stress on patient outcomes. Patients with ASCVD who reported an inability to pay medical bills were more likely to report financial distress (OR 3.60; 95% CI, 2.68-4.82), cost-related medication nonadherence (OR 3.39; 2.44-4.71), as well as food insecurity (OR 2.89; 2.14-3.90).23 Among patients with heart failure, 16% reported foregone care due to medical cost that was associated with more emergency room visits (43% vs 58%, P < .05) as well as $8,027 more out-of-pocket costs annually.7 In fact, CVD patients with public insurance were still more than twice as likely to forego or delay care compared to those with private insurance (OR 2.07; 95% CI, 1.37-3.12).25 Given foregone/delayed care as well as admissions for heart failure are linked to worse clinical outcomes,26 there is a clear unmet need despite expansion of medical insurance coverage in recent years to prevent financial toxicity.
In the world of oncology, several surveys have been validated as patient-reported outcome measure of financial toxicity related to medical care. The most commonly used tool is the Comprehensive Score for Financial Toxicity, or COST.27 This is a comprehensive score that includes 11 items addressing financial status and its impact on patients’ quality of life (see Figure 2). The scale has also been re-validated in patients with diabetes28 and various chronic diseases including cardiometabolic diseases (n = 221 patients).29 The Economic Strain and Resilience in Cancer (ENRICh) measure of financial toxicity is a 15-item scale that was developed to better capture the multiple dimensions of financial toxicity, including the material, psychological, and behavioral impact of financial burden.30 The subsequent brief 4-item questionnaire “ENRICh-4” correlated well with the full scale. It includes items regarding money in savings, debt, subjective stress about finances, and ability to pay bills. ENRICh-4 may lend itself to larger wide-scale screening for early signs of financial toxicity.30
Figure 2.
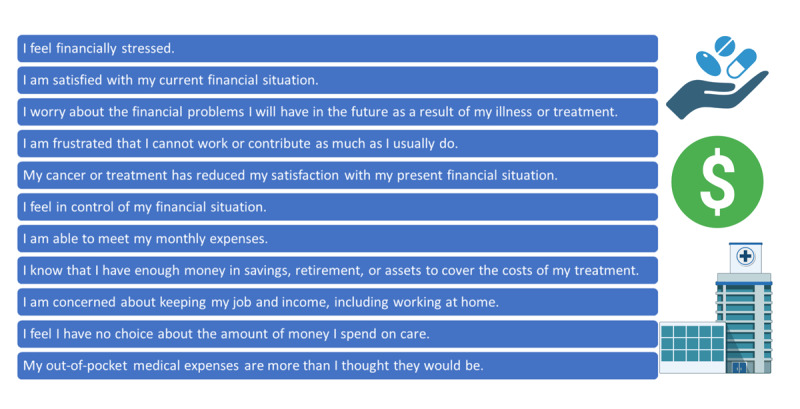
Eleven-item Comprehensive Score for Financial Toxicity (COST).
These validated patient-reported outcome surveys have not yet been applied in cardiovascular disease. The standardization of a definition of financial toxicity and the application of lessons learned from oncology is critical to capture the breadth of the issue as it relates to financial toxicity. With regard to financial burden, transparency regarding out-of-pocket cost is needed across all chronic disease management and will likely require leadership by policymakers in coordinating a nationwide centralized resource and mandating insurance companies to provide data. Efforts are currently underway, including the No Surprises Act, the $2,000 cap on out-of-pocket expenses for Medicare beneficiaries as part of the Inflation Reduction Act 2022, as well as the Medicare Drug Price Negotiation Program.31,32,33 Financial hardship and toxicity, on the other hand, require leadership from health care to implement validated survey tools at a systems level, identify at-risk populations, and advance research in modifiable risk factors and interventions.
Risk Factors
Lower Income Status, Insurance Status, and Youths
Multiple analyses of national health survey data have highlighted several risk factors for financial burden, hardship, and toxicity. Compared with middle/high-income families, low-income families of patients with ASCVD were found to have 10-fold higher odds of reporting catastrophic financial burden (OR 10.78; 95% CI, 8.72-13.33).15 Similarly, low-income families of patients with heart failure had 14-fold higher odds of reporting catastrophic burden (OR 14.2; 95% CI, 5.1-39.5).16 Low-income individuals with ASCVD, compared with higher-income individuals, had 1.34 (95% CI, 1.12-1.59) and 2.24 (95% CI, 1.79-2.80) higher odds of being in families facing any financial hardship from medical bills and an inability to pay medical bills, respectively.23
Several other socioeconomic factors have been shown to be high risk. Female sex and lower than a college education were significantly associated with financial hardship in patients with ASCVD and with heart failure.23,24 Uninsured individuals with ASCVD versus those with insurance had 1.86 (95% CI, 1.46-2.36) and 3.27 (95% CI, 2.49-4.30) higher odds of facing any financial hardship from medical bills and an inability to pay medical bills at all, respectively.23 However, similar analysis in patients with heart failure did not show an association between insurance status and financial hardship, but this may be due to the analysis being underpowered.24
Younger age has been shown to be a consistent demographic risk factor for financial burden, hardship, and toxicity across several chronic comorbidities including CVD. The youth may represent a particularly vulnerable intersection of multiple risk factors, such as lower income and accumulated savings, limited financial literacy and experience, and changing insurance status. Much of the analyses of patients with ASCVD and heart failure have focused on patients aged 18 to 64 years old.16,23,25,34 Among patients with ASCVD, nonelderly patients (< 65 years old) had a higher likelihood of experiencing any financial toxicity (53.1% vs 24.0%), difficulty paying medical bills (45.1% vs 19.9%), and inability to pay bills at all (18.9% vs 6.3%).35 Nonelderly heart failure patients also reported a higher likelihood of experiencing financial hardship (50.2% vs 26.0%, P < .001) with an adjusted OR of 3.11 (95% CI, 2.00-4.83).24 Being nonelderly was a significant risk factor for cost-related nonadherence (ie, delaying prescriptions or taking less than prescribed).15 In screening for at-risk population during the patient encounter, it is important to take into account the younger aged since this is associated with additional socioeconomic vulnerabilities, such as fewer assets, unstable employment, and the need for more under/unemployment issues secondary to CVD-related disabilities.
Family Structure and Caregivers
The financial status of a patient can be intricately linked to and impacted by the overall financial status of the family. Whether the patient has dependent children, income-earning partners, or other family members with chronic diseases can significantly impact the available budget, subjective distress, and ultimately financial decisions regarding medical care. Unfortunately, this factor has not been as thoroughly explored in cardiovascular disease as in other chronic conditions, specifically cancer. Recently, Jewett et al. (2024) found that among patients with cancer, single adults with minor children compared to families with two or more adults without children more often reported financial toxicity on almost all dimensions, financial distress (OR 1.46; 95% CI, 1.36-1.58), reducing prescription costs (OR 1.57; 95% CI, 1.07-2.28), skipping specialist or follow-up care (OR 1.36; 95% CI, 1.16-1.58), and delaying/foregoing care (OR 1.63; 95% CI. 1.16-2.29).36 In patients with ASCVD, family size was significantly associated with financial hardship, with 50% of families having ≥ 3 family members compared with 31.8% of single adult families reporting any financial hardship (P < .001).23 Future prospective studies are needed to better understand how family structure might impact financial toxicity in patients with CVD.
Caregiving is an essential component of financial toxicity experienced by patients with CVD. Due to the significant impairment in their functional status, patients often face costly needs for performing their daily activities of living in the form of informal caregiving, referring to the services provided by family members and friends. According to projections by the American Heart Association, the cost of informal caregiving was estimated to be $616 billion in 2015 and is expected to grow to $1.2 trillion in 2035.37 The elderly and patients who are non-White Hispanic and Black were found to have the highest financial burden of informal caregiving.37 The financial toxicity that ensues as a result of foregone work and wages by partners and its impact on patients with CVD needs to be better studied prospectively. For example, in partners of colorectal cancer survivors, 68.1% reported financial burden, which was significantly associated with worse health-related quality of life.38 On the other hand, the lack of informal caregiving resources from family and friends likely places high financial burden and is an important area for future research.
Multiple Comorbidities
Patients with multiple chronic medical conditions face higher medical bills and are at higher risk of experiencing medical debt and financial hardship. A recent analysis of the billing data from Blue Cross Blue Shield showed that among almost 3 million adults, there was a significant association between having a high burden of comorbidities and medical debt in collections (32% with 7-13 comorbid conditions vs 7.7% with no comorbid conditions).39 The highest incremental debt was posed by severe mental illness ($274) followed by substance use disorders ($268), stroke ($235), congestive heart failure ($234), and liver disease ($228).39 Diabetes is also an important comorbidity to consider in understanding financial toxicity given the high out-of-pocket cost of novel diabetes medications. One in six nonelderly patients with diabetes report not taking medications due to cost.40 In fact, 49.9% with ASCVD and diabetes reported financial hardship from medical bills and were significantly more likely than patients with ASCVD alone, diabetes alone, or neither condition to report financial hardship.34 In analyses of NHIS and MEPS, having multiple comorbidities was consistently shown to increase risk of financial burden, financial hardship, and cost-related nonadherence.7,16,23,24,41,42 Considering the incremental impact of new diagnoses on the financial situation of patients, the burden of comorbidities needs to be further studied in screening and management of financial toxicity.
As aforementioned, financial toxicity has been most thoroughly described in the cancer population. The prioritization of financial toxicity in cancer care is evident in multiple society guidelines,12,43 and recent years have seen an explosion of literature addressing the prevalence, risk factors, and interventions. Several scoping and systematic reviews have summarized the available findings. In 74 observational studies, Smith et al. (2019) found a pooled prevalence of 49% of material or psychologic financial burden of cancer.3 In patients with breast cancer alone, the pooled analysis of 34 studies that described financial toxicity estimated a prevalence of 35.3%.44 Patients with thyroid cancer have also been found to have a financial burden of an average annual cost between $1,425 and 17,000 and reported financial burden to be as high as 50%.45 In another systematic review by Azzani et al. of financial toxicity in cancer patients, the pooled prevalence of catastrophic financial burden was found to be as high as 47% in middle- and high-income countries, with 17% to 31.9% prevalence of financial toxicity as measured by the COST survey.46
Interestingly, having a cancer diagnosis as a comorbidity has not yet been shown to have incremental impact on financial toxicity in the setting of other diagnoses. In analyzing the claims data from Blue Cross Blue Shield, cancer was found to have the smallest incremental increase in rates of medical debt in collections compared with other chronic diseases.39 Similarly, NHIS data regarding patients with ASCVD showed that there was no statistically significant difference between patients with ASCVD only and those with both ASCVD and cancer in the risk of financial toxicity in several domains: difficulty/inability paying bills, financial distress, cost-related medication nonadherence, food insecurity, and delayed/forgone care.42 Of note, there was a signal for higher odds of financial toxicity in patients with ASCVD and cancer compared to those with ASCVD alone when referenced to patients with neither diagnosis. It is possible that some of the binary questions in the NHIS survey are less relevant to cancer patients; for example, those referring to food insecurity in the setting of decreased appetite and nausea secondary to chemotherapy. Future studies are needed to validate tools for assessment of financial toxicity, particularly in patients with ASCVD and cancer who are likely to face high medical bills from each diagnosis.
Comprehensive Social Determinants of Health
A comprehensive understanding of social determinants of health (SDOH) is an important step to fully defining the various risk factors posed by the patient’s socioeconomic status. As described by the Kaiser Family Foundation, there are potentially six domains: economic stability, neighborhood and physical environment, education, food, community and social context, and health care system.47 Valero-Elizondo et al. proposed creating a comprehensive index of SDOH using the data collected in NHIS, which included 34 items that covered these 6 domains and divided the ASCVD population into quartiles.35 Not surprisingly, patients in the lowest quartiles of SDOH were associated with a much higher prevalence of any financial toxicity (68% vs 15% in the highest SDOH quartile) with an 8-fold higher odds after adjusting for age, sex, race/ethnicity, and cardiovascular risk factors and comorbidities.35 Future interventions for screening for and mitigation of financial toxicity could benefit from utilizing such a comprehensive index for targeting the most vulnerable population.
Interventions
Patients with cardiovascular disease face highest out-of-pocket cost burden due to prescription drugs, but the discussion at the point-of-care remains severely limited. The importance of discussing out-of-pocket costs along with clinical benefit have been emphasized in semi-structured interviews.48,49 In a single-center review of 222 patient encounters, cost discussion was found in only 45%, with only 29% bringing up the insurance coverage of medications and 13% specifically about the affordability of co-pays.49 In 23% of the encounters, free samples were discussed but without a plan to continue when the time limited samples ran out.49 Currently, there are a few ongoing trials in CVD with interventions to improve access to care and encourage patient-physician communication regarding out-of-pocket costs. POCKET-COST-HF is a collaborative study between Emory Healthcare and the University of Colorado designed to improve transparency of out-of-pocket cost at the time of treatment decisions during clinic visits.50 Other trials to improve the use of GDMT medications including EPIC-HF (Electronically Delivered, Patient-Activation Tool for Intensification of Medications for Chronic Heart Failure with Reduced Ejection Fraction), which focuses on patient education tools, and PROMPT-MRA (Pragmatic Trial of Messaging to Providers About Treatment With Mineralocorticoid Receptor Antagonists), which uses electronic health record-based alert systems for physicians who have not included an intervention for out-of-pocket costs.
Future interventions to mitigate financial toxicity in CVD can be informed by evidence-based practices from oncology patients. Large-scale screening programs and interventions in oncology have shown improved patient-reported outcomes and quality of life. Figure 3 summarizes various interventions to address financial toxicity, highlighting the potential for similar approaches to be adapted in cardiology.
Figure 3.
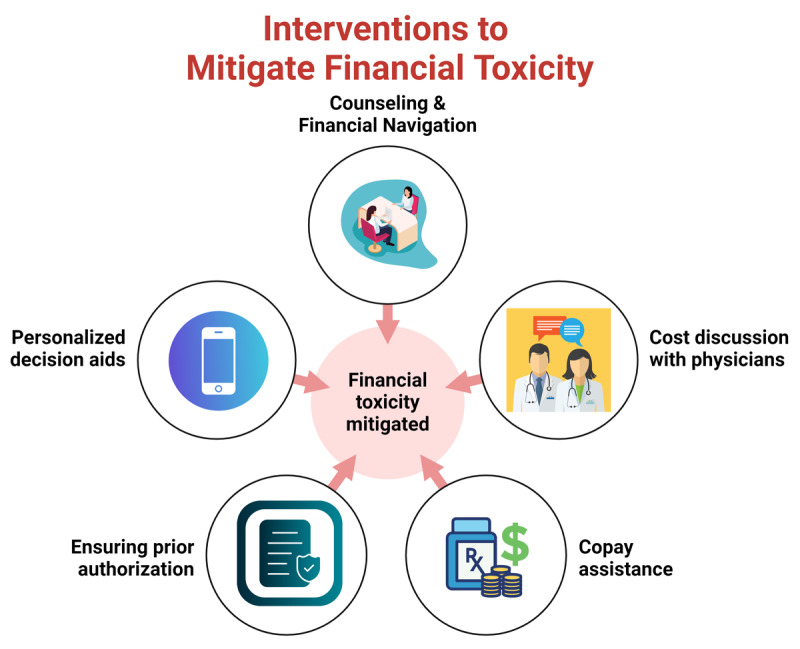
Interventions to address financial toxicity.
Counseling and Financial Navigation
Counseling and financial navigation services provide personalized support to patients, guiding them through the complexities of healthcare costs, insurance coverage, and potential sources of financial aid. This approach has been demonstrated to significantly reduce economic stress and improve patient outcomes, as seen in oncology practices where financial counseling has effectively mitigated financial toxicity.51 Additionally, a feasibility study highlighted the importance of personalized out-of-pocket cost communication and remote financial navigation, showing that such interventions can be successfully adapted and implemented in clinical practice to reduce financial distress.52
Cost Discussion with Physicians
Cost discussions with physicians are another critical intervention. By integrating these discussions into clinical consultations, patients can make informed decisions about their treatment options, balancing clinical efficacy with financial feasibility. This has been shown to improve adherence to treatment plans and reduce the likelihood of financial distress, as demonstrated in a randomized controlled trial that evaluated a mobile application designed to assist patients with managing out-of-pocket costs.53 Additionally, the implementation of mobile apps (ie, the DISCO app) has proven effective in facilitating these crucial cost discussions and enhancing patient-physician communication.54
Co-Pay Assistance
Programs providing co-pay assistance also play a crucial role in reducing the immediate financial burden on patients, enabling them to adhere to prescribed therapies without sacrificing other essential needs. For example, the Levine Cancer Institute Financial Toxicity Tumor Board successfully implemented co-pay assistance programs that provided significant financial relief to patients, reducing their out-of-pocket costs and improving treatment adherence.55 Furthermore, co-pay assistance and patient aid programs were effectively used in statewide insurance coverage pilots for proton therapy, demonstrating their efficacy in mitigating financial burden.56
Ensuring Prior Authorization
Ensuring prior authorization for treatments, particularly for costly medications, is another vital step in preventing unexpected expenses that could lead to financial distress. The establishment of structured programs to manage prior authorizations proactively has been shown to reduce the incidence of insurance denials, thus decreasing financial toxicity for patients. This was clearly demonstrated by the Financial Toxicity Tumor Board, which addressed complex financial issues and secured necessary authorizations, significantly reducing patient expenditures.55
Personalized Decision Aids
Finally, personalized decision aids such as mobile applications and tailored counseling tools have proven effective in empowering patients to navigate complex insurance landscapes and manage out-of-pocket costs. These tools help patients make informed decisions regarding their care, thereby reducing financial toxicity and enhancing overall satisfaction with their healthcare experience. The development and implementation of such tools have been shown to improve patient outcomes by providing critical financial and clinical information at the point of care.54,57
Moreover, financial toxicity interventions have been shown to improve both financial and clinical outcomes in patients with hematologic malignancies, further supporting the efficacy of such interventions.58 These interventions highlight the potential for comprehensive strategies to mitigate financial toxicity in CVD care, ensuring that patients receive the necessary treatments without the added burden of financial hardship.
Conclusion
Current efforts to reduce financial toxicity in cardiology are disjointed, often relying on local resources such as institutional charity care or foundation support. While the burden of medical bills, especially with the introduction of novel therapies, has been recognized, there is a lack of national prioritization to address cost-based discussions in clinical settings. Novel therapies such as SGLT2i, cardiac amyloidosis therapies, and device therapies like leadless pacemakers exacerbate financial hardships for patients with cardiovascular disease.
In the United States, the American College of Oncology has been at the forefront of addressing financial toxicity. They established the Cost of Care Task Force in 2007 and issued a Guidance Statement in 2009, setting several priorities for research, education, and advocacy to address the underlying issues of financial toxicity. These priorities include:
Emphasizing the importance of addressing the cost of care during physician-patient encounters to aid value-based and patient-centered medical decision-making.
Highlighting the lack of comparative effectiveness data among different treatment options, the determination of out-of-pocket payments during clinic visits, and the need for clinicians experienced in facilitating such discussions.
This review highlights the significant burden of financial toxicity in CVD and the gaps in current interventions. The complex interplay between the socioeconomic factors—the patients’ income, education level, insurance status, and the healthcare system—render certain vulnerable populations unable to access the prescribed medical care. By applying lessons learned from oncology, there is an opportunity to develop comprehensive and individualized strategies to mitigate financial toxicity in cardiovascular care, ensuring that patients receive the necessary support to manage both their medical and financial well-being, thereby improving overall patient outcomes.
Key Points
Financial toxicity in cardiovascular disease (CVD) significantly impacts patient outcomes, contributing to medical nonadherence and decline in mental and physical well-being.
The prevalence of financial toxicity in CVD parallels findings in oncology, where financial strain is well-documented and addressed through structured guidelines.
Socioeconomic factors, including income level, insurance status, and younger age, heighten the risk of financial hardship for CVD patients.
Interventions like financial counseling, cost discussions with physicians, and co-pay assistance programs are vital to mitigating the burden.
Applying lessons from oncology can help establish standardized financial toxicity assessment tools and improve outcomes for CVD patients.
Funding Statement
This research is supported in part by the National Institutes of Health through MD Anderson’s Cancer Center Support Grant (CA016672).
Disclosures/Competing Interests
Dr. Palaskas is supported by the Cancer Prevention & Research Institute of Texas (CPRIT) RP200670, the National Institutes of Health/National Cancer Institute 1P01CA261669-01, and the Andrew Sabin Family Foundation and is a consultant for Replimmune and Kiniksa Pharmaceuticals. Dr. Smith receives research support from Genentech. Dr. Deswal is supported in part by the Ting Tsung and Wei Fong Chao Distinguished Chair and has received consultant fees from Bayer. Drs. Kandula and Ali have no disclosures to declare.
References
- 1.Heart [Internet]. Washington, DC: American Heart Association Office of Federal Advocacy; c2024. Cardiovascular Disease: A Costly Burden for America: Projections Through 2035; 2017. [cited 2024 Oct 6]. Available from: https://www.heart.org/-/media/Files/About-Us/Policy-Research/Fact-Sheets/Public-Health-Advocacy-and-Research/CVD-A-Costly-Burden-for-America-Projections-Through-2035.pdf [Google Scholar]
- 2.Abdus S, Keenan PS. Financial Burden of Employer-Sponsored High-Deductible Health Plans for Low-Income Adults With Chronic Health Conditions. JAMA Intern Med. 2018. Dec 1;178(12):1706-1708. doi: 10.1001/jamainternmed.2018.4706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith GL, Lopez-Olivo MA, Advani PG, et al. Financial Burdens of Cancer Treatment: A Systematic Review of Risk Factors and Outcomes. J Natl Compr Canc Netw. 2019. Oct 1;17(10):1184-1192. doi: 10.6004/jnccn.2019.7305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khera R, Valero-Elizondo J, Nasir K. Financial Toxicity in Atherosclerotic Cardiovascular Disease in the United States: Current State and Future Directions. J Am Heart Assoc. 2020. Oct 20;9(19):e017793. doi: 10.1161/JAHA.120.017793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warraich HJ, Ali HJR, Nasir K. Financial Toxicity With Cardiovascular Disease Management: A Balancing Act for Patients. Circ Cardiovasc Qual Outcomes. 2020. Dec;13(12):e007449. doi: 10.1161/CIRCOUTCOMES.120.007449 [DOI] [PubMed] [Google Scholar]
- 6.Luo F, Chapel G, Ye Z, Jackson SL, Roy K. Labor Income Losses Associated With Heart Disease and Stroke From the 2019 Panel Study of Income Dynamics. JAMA Netw Open. 2023. Mar 1;6(3):e232658. doi: 10.1001/jamanetworkopen.2023.2658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas A, Valero-Elizondo J, Khera R, et al. Forgone Medical Care Associated With Increased Health Care Costs Among the U.S. Heart Failure Population. JACC Heart Fail. 2021. Oct;9(10):710-719. doi: 10.1016/j.jchf.2021.05.010 [DOI] [PubMed] [Google Scholar]
- 8.Perrone F, Jommi C, Di Maio M, et al. The association of financial difficulties with clinical outcomes in cancer patients: secondary analysis of 16 academic prospective clinical trials conducted in Italy. Ann Oncol. 2016. Dec;27(12):2224-2229. doi: 10.1093/annonc/mdw433 [DOI] [PubMed] [Google Scholar]
- 9.Ramsey SD, Bansal A, Fedorenko CR, et al. Financial Insolvency as a Risk Factor for Early Mortality Among Patients With Cancer. J Clin Oncol. 2016. Mar 20;34(9):980-6. doi: 10.1200/JCO.2015.64.6620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma SJ, Iovoli AJ, Attwood K, et al. Association of significant financial burden with survival for head and neck cancer patients treated with radiation therapy. Oral Oncol. 2021. Apr:115:105196. doi: 10.1016/j.oraloncology.2021.105196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381-90. doi: 10.1634/theoncologist.2012-0279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meropol NJ, Schrag D, Smith TJ, et al. American Society of Clinical Oncology guidance statement: the cost of cancer care. J Clin Oncol. 2009. Aug 10;27(23):3868-74. doi: 10.1200/JCO.2009.23.1183 [DOI] [PubMed] [Google Scholar]
- 13.Obama B. United States Health Care Reform: Progress to Date and Next Steps. JAMA. 2016. Aug 2;316(5):525-32. doi: 10.1001/jama.2016.9797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang SY, Valero-Elizondo J, Cainzos-Achirica M, Desai NR, Nasir K, Measures of Financial Hardship From Health Care Expenses Among Families With a Member With Atherosclerotic Cardiovascular Disease in the US. JAMA Health Forum. 2022. Jul 22;3(7):e221962. doi: 10.1001/jamahealthforum.2022.1962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khera R, Valero-Elizondo Javier, Okunrintemi V, et al. Association of Out-of-Pocket Annual Health Expenditures With Financial Hardship in Low-Income Adults With Atherosclerotic Cardiovascular Disease in the United States. JAMA Cardiol. 2018. Aug 1;3(8):729-738. doi: 10.1001/jamacardio.2018.1813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang SY, Valero-Elizondo J, Ali HJ, et al. Out-of-Pocket Annual Health Expenditures and Financial Toxicity From Healthcare Costs in Patients With Heart Failure in the United States. J Am Heart Assoc. 2021. Jul 20;10(14):e022164. doi: 10.1161/JAHA.121.022164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.GoodRx [Internet]. Santa Monica, CA: GoodRx; c2024. Entresto fact sheet; 2023. Jun [cited 2024 Oct 6]. Available from: https://www.goodrx.com/entresto/what-is?label_override=undefined [Google Scholar]
- 18.GoodRx [Internet]. Santa Monica, CA: GoodRx; c2024. Jardiance fact sheet; 2023. [cited 2024 Oct 6]. Available from: https://www.goodrx.com/jardiance?utm_campaign=16074693778&utm_content=132584585973&utm_source=google&utm_medium=cpc&utm_term=kwd-819146029810&gclid=CjwKCAjw4_K0BhBsEiwAfVVZ_5E7Cjwb9X8UgxsGVPDsnXGfpMpz72zYIaRN0lNYIcUd17tAyUCA5xoCqsUQAvD_BwE&gclsrc=aw.ds&dosage=10mg&form=tablet&quantity=30&label_override=jardiance [Google Scholar]
- 19.US Census [Internet]. Washington, DC: US Census Bureau; c2024. Guzman G, Kollar M. Income in the United States: 2022; 2023. Sept [cited 2024 Aug 12]. Available from: https://www.census.gov/content/dam/Census/library/publications/2023/demo/p60-279.pdf [Google Scholar]
- 20.Faridi KF, Dayoub EJ, Ross JS, Dhruva SS, Ahmad T, Desai NR. Medicare Coverage and Out-of-Pocket Costs of Quadruple Drug Therapy for Heart Failure. J Am Coll Cardiol. 2022. Jun 28;79(25):2516-2525. doi: 10.1016/j.jacc.2022.04.031 [DOI] [PubMed] [Google Scholar]
- 21.Shore S, Basu T, Kamdar N, et al. Use and Out-of-Pocket Cost of Sacubitril-Valsartan in Patients With Heart Failure. J Am Heart Assoc. 2022. Sep 6;11(17):e023950. doi: 10.1161/JAHA.121.023950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aggarwal R, Vaduganathan M, Chiu N, Bhatt DL. Out-of-Pocket Costs for SGLT-2 (Sodium-Glucose Transport Protein-2) Inhibitors in the United States. Circ Heart Fail. 2022. Mar;15(3):e009099. doi: 10.1161/CIRCHEARTFAILURE.121.009099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Valero-Elizondo J, Khera R, Saxena A, et al. Financial Hardship From Medical Bills Among Nonelderly U.S. Adults With Atherosclerotic Cardiovascular Disease. J Am Coll Cardiol. 2019. Feb 19;73(6):727-732. doi: 10.1016/j.jacc.2018.12.004 [DOI] [PubMed] [Google Scholar]
- 24.Ali HJR, Valero-Elizondo J, Wang SY, et al. Subjective Financial Hardship due to Medical Bills Among Patients With Heart Failure in the United States: The 2014-2018 Medical Expenditure Panel Survey. J Card Fail. 2022. Sep;28(9):1424-1433. doi: 10.1016/j.cardfail.2022.06.009 [DOI] [PubMed] [Google Scholar]
- 25.Bernard D, Fang Z. Financial Burdens and Barriers to Care Among Nonelderly Adults With Heart Disease: 2010-2015. J Am Heart Assoc. 2019. Dec 17;8(24):e008831. doi: 10.1161/JAHA.118.008831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaneko H, Itoh H, Yotsumoto H, et al. Association between the number of hospital admissions and in-hospital outcomes in patients with heart failure. Hypertens Res. 2020. Dec;43(12):1385-1391. doi: 10.1038/s41440-020-0505-2 [DOI] [PubMed] [Google Scholar]
- 27.de Souza JA, Yap BJ, Wroblewski K, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: The validation of the COmprehensive Score for financial Toxicity (COST). Cancer. 2017. Feb 1;123(3):476-484. doi: 10.1002/cncr.30369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel MR, Zhang G, Heisler M, et al. Measurement and Validation of the Comprehensive Score for Financial Toxicity (COST) in a Population With Diabetes. Diabetes Care. 2022. Nov 1;45(11):2535-2543. doi: 10.2337/dc22-0494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pavela G, Fifolt M, Tison SE, Allison M, Burton BS, Ford EW. Re-Validation of the COmprehensive Score for Financial Toxicity (COST): Assessing the Scale’s Utility in Chronic Disease Populations. Health Serv Insights. 2021. Dec 10:14:11786329211057352. doi: 10.1177/11786329211057352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu C, Smith GL, Chen YS, et al. Short-form adaptive measure of financial toxicity from the Economic Strain and Resilience in Cancer (ENRICh) study: Derivation using modern psychometric techniques. PLoS One. 2022. Aug 25;17(8):e0272804. doi: 10.1371/journal.pone.0272804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Foote JHA, Kazi DS. The March Toward Improved Heart Failure Outcomes Requires an Emphasis on Affordability. JACC Heart Fail. 2024. Jul;12(7):1238-1241. doi: 10.1016/j.jchf.2024.04.019 [DOI] [PubMed] [Google Scholar]
- 32.Narasimmaraj PR, Oseran A, Tale A, et al. Out-of-Pocket Drug Costs for Medicare Beneficiaries With Cardiovascular Risk Factors Under the Inflation Reduction Act. J Am Coll Cardiol. 2023. Apr 18;81(15):1491-1501. doi: 10.1016/j.jacc.2023.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kazi DS, DeJong C, Chen R, Wadhera RK, Tseng CW. The Inflation Reduction Act and Out-of-Pocket Drug Costs for Medicare Beneficiaries With Cardiovascular Disease. J Am Coll Cardiol. 2023. May 30;81(21):2103-2111. doi: 10.1016/j.jacc.2023.03.414 [DOI] [PubMed] [Google Scholar]
- 34.Mszar R, Grandhi GR, Valero-Elizondo J, et al. Cumulative Burden of Financial Hardship From Medical Bills Across the Spectrum of Diabetes Mellitus and Atherosclerotic Cardiovascular Disease Among Non-Elderly Adults in the United States. J Am Heart Assoc. 2020. May 18;9(10):e015523. doi: 10.1161/JAHA.119.015523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Valero-Elizondo J, Javed Z, Khera R, et al. Unfavorable social determinants of health are associated with higher burden of financial toxicity among patients with atherosclerotic cardiovascular disease in the US: findings from the National Health Interview Survey. Arch Public Health. 2022. Dec 6;80(1):248. doi: 10.1186/s13690-022-00987-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jewett PI, Purani H, Vogel RI, Parsons HM, Borrero M, Blaes A. Comparisons of financial hardship in cancer care by family structure and among those with and without minor children using nationally representative data. Cancer Med. 2024. Mar;13(6):e7088. doi: 10.1002/cam4.7088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dunbar SB, Khavjou OA, Bakas T, et al. Projected Costs of Informal Caregiving for Cardiovascular Disease: 2015 to 2035: A Policy Statement From the American Heart Association. Circulation. 2018. May 8;137(19):e558-e577. doi: 10.1161/CIR.0000000000000570 [DOI] [PubMed] [Google Scholar]
- 38.Ghazal LV, Abrahamse P, Ward KC, Morris AM, Hawley ST, Veenstra CM. Financial Toxicity and Its Association With Health-Related Quality of Life Among Partners of Colorectal Cancer Survivors. JAMA Netw Open. 2023. Apr 3;6(4):e235897. doi: 10.1001/jamanetworkopen.2023.5897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Becker NV, Scott JW, Moniz MH, Carlton EF, Ayanian JZ. Association of Chronic Disease With Patient Financial Outcomes Among Commercially Insured Adults. JAMA Intern Med. 2022. Oct 1;182(10):1044-1051. doi: 10.1001/jamainternmed.2022.3687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taha MB, Valero-Elizondo J, Yahya T, et al. Cost-Related Medication Nonadherence in Adults With Diabetes in the United States: The National Health Interview Survey 2013-2018. Diabetes Care. 2022. Mar 1;45(3):594-603. doi: 10.2337/dc21-1757 [DOI] [PubMed] [Google Scholar]
- 41.Khera R, Valero-Elizondo J, Das SR, et al. Cost-Related Medication Nonadherence in Adults With Atherosclerotic Cardiovascular Disease in the United States, 2013 to 2017. Circulation. 2019. Dec 17;140(25):2067-2075. doi: 10.1161/CIRCULATIONAHA.119.041974 [DOI] [PubMed] [Google Scholar]
- 42.Valero-Elizondo J, Chouairi F, Khera R, et al. Atherosclerotic Cardiovascular Disease, Cancer, and Financial Toxicity Among Adults in the United States. JACC CardioOncol. 2021. Jun 15;3(2):236-246. doi: 10.1016/j.jaccao.2021.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Agarwal A, Livingstone A, Karikios DJ, Stockler MR, Beale PJ, Morton RL. Physician-patient communication of costs and financial burden of cancer and its treatment: a systematic review of clinical guidelines. BMC Cancer. 2021. Sep 16;21(1):1036. doi: 10.1186/s12885-021-08697-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ehsan AN, Wu CA, Minasian A, et al. Financial Toxicity Among Patients With Breast Cancer Worldwide: A Systematic Review and Meta-analysis. JAMA Netw Open. 2023. Feb 1;6(2):e2255388. doi: 10.1001/jamanetworkopen.2022.55388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Uppal N, Cunningham Nee Lubitz C, James B. The Cost and Financial Burden of Thyroid Cancer on Patients in the US: A Review and Directions for Future Research. JAMA Otolaryngol Head Neck Surg. 2022. Jun 1;148(6):568-575. doi: 10.1001/jamaoto.2022.0660 [DOI] [PubMed] [Google Scholar]
- 46.Azzani M, Atroosh WM, Anbazhagan D, Kumarasamy V, Abdalla MMI. Describing financial toxicity among cancer patients in different income countries: a systematic review and meta-analysis. Front Public Health. 2024. Jan 2:11:1266533. doi: 10.3389/fpubh.2023.1266533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.KFF [Internet]. San Francisco, CA: Kaiser Family Foundation; c2024. Artiga S, Hinton E. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity; 2018. May [cited 2024 July 24]. Available from: https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/ [Google Scholar]
- 48.Dickert NW, Mitchell AR, Venechuk GE, et al. Show Me the Money: Patients’ Perspectives on a Decision Aid for Sacubitril/Valsartan Addressing Out-of-Pocket Cost. Circ Cardiovasc Qual Outcomes. 2020. Dec;13(12):e007070. doi: 10.1161/CIRCOUTCOMES.120.007070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rao BR, Akrobetu DJ, Dickert NW, et al. Deciding Whether to Take Sacubitril/Valsartan: How Cardiologists and Patients Discuss Out-of-Pocket Costs. J Am Heart Assoc. 2023. Apr 4;12(7):e028278. doi: 10.1161/JAHA.122.028278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Montembeau SC, Rao BR, Mitchell AR, et al. Integrating Cost into Shared Decision-Making for Heart Failure with Reduced Ejection Fraction (POCKET-COST-HF): A Trial Providing Out-of-Pocket Costs for Heart Failure Medications during Clinical Encounters. Am Heart J. 2024. doi: 10.1016/j.ahj.2023.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kircher SM, Yarber J, Rutsohn J, et al. Piloting a Financial Counseling Intervention for Patients With Cancer Receiving Chemotherapy. J Oncol Pract. 2019. Mar;15(3):e202-e210. doi: 10.1200/JOP.18.00270 [DOI] [PubMed] [Google Scholar]
- 52.Sadigh G, Coleman D, Switchenko JM, Hopkins JO, Carlos RC. Treatment out-of-pocket cost communication and remote financial navigation in patients with cancer: a feasibility study. Support Care Cancer. 2022. Oct;30(10):8173-8182. doi: 10.1007/s00520-022-07270-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tarnasky AM, Tran GN, Nicolla J, et al. Mobile Application to Identify Cancer Treatment-Related Financial Assistance: Results of a Randomized Controlled Trial. JCO Oncol Pract. 2021. Oct;17(10):e1440-e1449. doi: 10.1200/OP.20.00757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hamel LM, Dougherty DW, Hastert TA, et al. The DISCO App: A pilot test of a multi-level intervention to reduce the financial burden of cancer through improved cost communication. PEC Innov. 2021. Oct 30:1:100002. doi: 10.1016/j.pecinn.2021.100002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Raghavan D, Keith NA, Warden HR, et al. Levine Cancer Institute Financial Toxicity Tumor Board: A Potential Solution to an Emerging Problem. JCO Oncol Pract. 2021. Oct;17(10):e1433-e1439. doi: 10.1200/OP.21.00124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ning MS, Palmer MB, Shah AK, et al. Three-Year Results of a Prospective Statewide Insurance Coverage Pilot for Proton Therapy: Stakeholder Collaboration Improves Patient Access to Care. JCO Oncol Pract. 2020. Sep;16(9):e966-e976. doi: 10.1200/JOP.19.00437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Politi MC, Grant RL, George NP, et al. Improving Cancer Patients’ Insurance Choices (I Can PIC): A Randomized Trial of a Personalized Health Insurance Decision Aid. Oncologist. 2020. Jul;25(7):609-619. doi: 10.1634/theoncologist.2019-0703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Knight TG, Aguiar M, Robinson M, et al. Financial Toxicity Intervention Improves Outcomes in Patients With Hematologic Malignancy. JCO Oncol Pract. 2022. Sep;18(9):e1494-e1504. doi: 10.1200/OP.22.00056 [DOI] [PubMed] [Google Scholar]


