Abstract
Background
This study aims to evaluate the efficacy and clinical outcomes of Nice knot-assisted fixation in the management of comminuted and displaced clavicle fractures.
Methods
A systematic search was conducted across multiple electronic databases, including PubMed, Embase, Cochrane Library, China Biology Medicine (CBM) database, CNKI, Wanfang, and VIP database, to identify studies comparing Nice knot-assisted fixation with traditional surgical treatment for displaced midshaft clavicle fractures. The primary outcomes assessed included fracture healing times, hospitalization days, complications, and functional outcomes. Secondary outcomes such as intraoperative blood loss, operative time, incision length, and fluoroscopy time were also evaluated. Data were analyzed using random-effects models, and summary statistics including Mean Difference (MD), risk ratios (RRs) and theirs’ 95% confidence intervals (CIs) were calculated.
Results
Screening of the literature yielded a total of 11 studies meeting the inclusion criteria, involving 754 patients. Meta-analysis of the pooled data demonstrated a significant advantage of Nice knot-assisted fixation over traditional surgical treatment in terms of operative time (MD = -11.53, 95% CI: -18.16 to -4.91, p = 0.0006) and blood loss (MD = -14.19, 95% CI: -20.93 to -7.45, p = 0.00001). Additionally, Nice knot-assisted fixation was associated with reduced fracture healing time (MD = -0.63, 95% CI: -1.12 to -0.14, p = 0.01) rather than hospitalization days (MD = -0.47, 95% CI: -1.14 to 0.21, p = 0.18) and complications (RR = 0.48, 95% CI: 0.23 to 1.01, p = 0.05) compared to traditional surgical treatment. Moreover, nice knot-assisted fixation was associated with increased constant-murley score and Neer score, and reduced visual analogue scale (VAS) score compared to traditional surgical treatment.
Conclusion
This study highlights that Nice knot assistance offers advantages in reducing intraoperative blood loss, shortening operation time, and achieving favorable postoperative outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-024-08012-w.
Keywords: Clavicle fractures, Nice knot, Fixation, Meta-analysis, Clinical outcomes, Surgical technique
Introduction
Clavicle fractures are a common orthopedic injury, accounting for approximately 5–10% of all fractures [1]. While many clavicle fractures can be managed conservatively, surgical intervention is often necessary for complex or displaced fractures to promote optimal healing and restore function. However, despite advancements in surgical techniques, challenges such as nonunion, refracture, and infection continue to complicate the management of clavicle fractures, particularly those involving comminution or displacement [2].
Comminuted midshaft clavicle fractures present a particularly challenging clinical scenario, often requiring precise reduction and stable fixation to prevent complications and promote optimal healing. Traditional treatment methods, including open reduction and internal fixation with plates and screws, have shown variable outcomes and are associated with risks such as hardware failure and infection. Management strategies for such fractures have evolved over the years, with a focus on achieving stable fixation while minimizing soft tissue disruption and promoting early mobilization. Among the various techniques employed, the Nice knot has emerged as a promising adjunctive approach, offering advantages in both reduction and fixation [3].
The Nice knot is a modification of the traditional square knot used in surgical suturing [4]. The Nice knot technique involves the use of doubled sutures to create a secure and stable construct [5, 6], aiding in fracture reduction and maintaining alignment during plate fixation [7]. The development of the Nice knot represents a significant advancement in surgical techniques for clavicle fracture fixation [8, 9]. Several recent studies have investigated the clinical outcomes of employing Nice knots as a supportive measure in the treatment of midshaft clavicle fractures, particularly in cases of comminution and displacement. By doubling the suture material, the Nice knot enhances knot security and stability, providing a reliable method for fracture reduction and fixation [7].
The application of the Nice knot in clavicle fracture fixation offers several advantages over traditional techniques. Its enhanced frictional grip reduces the risk of knot failure and suture slippage, improving the stability of the fixation construct. This is particularly important in the treatment of comminuted fractures, where achieving and maintaining reduction can be challenging. In addition to its clinical benefits, the Nice knot also offers biomechanical advantages in fracture reduction and fixation [7]. By creating multiple friction points, the Nice knot enhances stability and resistance to displacement, promoting optimal healing. Several recent studies have investigated the clinical outcomes of Nice knot-assisted fixation in the treatment of comminuted midshaft clavicle fractures. On the contrary, the Nice knot technique can be technically demanding and may extend surgical time. It has a steep learning curve, with risks of knot slippage and limited long-term evidence compared to other methods. Additionally, it may not be suitable for all patients, especially those with specific anatomical variations or underlying conditions.
There is limited evidence on its long-term benefits compared to traditional methods. While some studies have reported favorable outcomes with Nice knot-assisted fixation, such as improved fracture reduction and stability, there is a need for a comprehensive evaluation of its clinical effectiveness. Wu et al. (2021) [10] evaluated the use of doubled-suture Nice knot augmented plate fixation and reported favorable outcomes in terms of fracture reduction and stability. Similarly, Hong et al. (2021) [11] compared Nice knots with traditional methods as an auxiliary reduction-fixation technique and found advantages in achieving and maintaining anatomical reduction.
This meta-analysis aims to fill this gap by systematically assessing the clinical outcomes of the Nice knot technique versus traditional fixation methods. By synthesizing data from multiple studies, it seeks to provide a robust evaluation of the Nice knot’s efficacy and offer insights into its overall impact on clavicle fracture management. This comprehensive approach will help clarify the advantages and drawbacks of the Nice knot technique and inform clinical practice guidelines.
Materials and methods
This study adhered to the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) guidelines [12]. Since this study involved the analysis of existing literature and did not directly involve human participants or animals, ethical approval was not required. All data were extracted from publicly available sources, and patient confidentiality was maintained throughout the study.
Literature search
A comprehensive search was conducted across multiple electronic databases, including PubMed, Embase, Cochrane Library, China Biology Medicine (CBM) database, CNKI, Wanfang, and VIP database, to identify relevant studies examining the efficacy of Nice knot-assisted fixation for displaced midshaft clavicle fractures. The search strategy included combinations of keywords such as “Nice knot”, “surgical methods” or “surgery”, and “clavicle fracture”. Throughout the identification process, there were no limitations based on language. The last search update occurred on May 31, 2024. Two separate investigators, referred to as investigator A and investigator B, independently and without knowledge of each other’s assessments, conducted the preliminary screening and evaluation of the studies retrieved according to the predefined criteria. The titles and abstracts of the papers were examined, and those that did not fit the scope of the research were discarded. The remaining articles then underwent an exhaustive evaluation. Furthermore, reference lists from relevant articles, including reviews, meta-analyses, and studies that met inclusion criteria, were manually inspected by two separate investigators to locate any additional studies that might have been missed in the initial database search [13]. The manual examination of references was performed following the above screening process.
Inclusion criteria
Studies were included if they met the following criteria: (1) clinical studies evaluating the use of Nice knot-assisted fixation for displaced midshaft clavicle fractures compared to traditional methods, (2) included randomized controlled trials (RCTs) or observational studies comparing surgical treatment with Nice knot-assisted fixation to traditional surgical treatment, and (3) reported outcomes related to fracture healing, cosmetic results, intraoperative parameters, or postoperative complications. When overlapping datasets were encountered across various publications, preference was given to the study either providing the most thorough data or having the latest publication date.
Exclusion criteria
Studies were excluded if they were duplicates, conference abstracts, letters, editorials, or non-peer-reviewed articles. Study that did not provide the necessary data in the control group was also excluded.
Data extraction
Two independent reviewers extracted relevant data from the included studies, including study characteristics (e.g., author, publication year), patient demographics (age, sex), intervention details, follow-up, inclusion period, outcome measures, and effect estimates. Any discrepancies were resolved through discussion or consultation with a third reviewer.
Quality assessment
The evaluation of the quality of non-randomized trials is crucial in order to assess the validity and reliability of the study findings. The methodological quality was performed by using MINORS scale [14], commonly used in non-randomized controlled trials, with a total of 12 items. 0–2 points for each item, with a total score of 24 points. 0 indicates that it has not been reported; 1 indicates that it has been reported but the information is insufficient; A score of 2 indicates that it has been reported and provided sufficient information. Studies with low methodological quality were considered for sensitivity analysis or subgroup analysis to assess their impact on the overall results.
Publication bias
Potential publication bias was assessed using funnel plots and statistical tests, such as Egger's test, where appropriate. Sensitivity analyses were conducted to evaluate the robustness of the results and assess the impact of publication bias on the overall findings.
Statistical analysis
Statistical analyses were performed using appropriate software packages, such as RevMan software version 5.0. A two-tailed P-value < 0.05 was considered statistically significant. Quantitative synthesis of the extracted data was performed using appropriate statistical methods including Mean Difference (MD), risk ratios (RRs) and theirs’ 95% confidence intervals (CIs) [15]. Meta-analytic techniques, such as random-effects models, were used to estimate summary effect sizes and their corresponding 95% confidence intervals. Heterogeneity among the studies was assessed through statistical methods (Cochran's Q test, I2statistic) [16–18]. Where relevant, subgroup analyses or meta-regression were employed to investigate potential sources of variability [19]. Meta-regressions involving variations in study time, size of patient populations, inclusion period, MINORS scores, and surgical techniques were performed to explore the source of the high heterogeneity. Sensitivity analysis was performed by excluding studies one by one [15].
Results
Study inclusion and exclusion
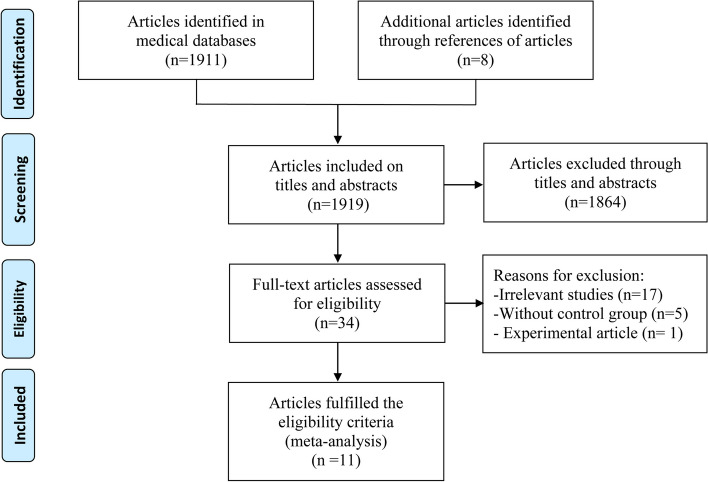
The electronic database search yielded a total of 1911 records, with an additional 8 studies identified through the manual examination of reference lists from relevant articles. Out of the combined 1919 records, 1864 were excluded due to duplication or lack of relevance based on their titles and abstracts. This filtering process left 34 articles, of which 17 were deemed irrelevant, five lacked a control group [4, 20–23], and one was classified as an experimental study [7], resulting in their exclusion. Ultimately, after thorough evaluation, 11 studies [8, 10, 11, 24–31] encompassing 754 patients were selected as suitable for quantitative analysis. The detailed inclusion procedure and exclusion rationale are illustrated in Fig. 1.
Fig. 1.
Flow diagram of the literature search and selection process
Search results and included participants
The included studies, published between 2019 and 2023, had sample sizes ranging from 36 to 100. In total, 11 studies [8, 10, 11, 24–31] were analyzed to assess the effectiveness and clinical outcomes of Nice knot-assisted fixation compared to traditional surgical techniques in managing comminuted and displaced clavicle fractures. Various types of studies were included.
According to the MINORS score, 4 (36.4%) [8, 11, 25, 30], 2 (18.2%) [10, 27], 3 (27.3%) [24, 26, 29], and 2 (18.2%) [28, 31] studies scored 15, 13, 12, and 11, respectively. The MINORS score for these studies averaged 12.5, ranging from 11 to 15. The scores of each included study are presented in Table 1. Detailed methodological characteristics, procedural features, and demographic data of the participants in the selected studies are presented in Table 1.
Table 1.
Basic Information of the Included Studies
| Author | Year | Group | Number of cases | Male/Female | Age (range, yrs) | Fixation method | Inclusion period | Study type | Follow-up (month) | MINORS score |
|---|---|---|---|---|---|---|---|---|---|---|
| Xu, et al | 2023 | T | 12 | 9/3 | 42.5 ± 11.9 (22–57) | Nice knot + plate | 2022.1-2022.12 | R | 10.1 ± 3.5 | 12 |
| C | 24 | 16/8 | 40.3 ± 10.9 (17–57) | Lag screw + plate | 11.7 ± 4.9 | |||||
| Cheng, et al | 2023 | T | 34 | 19/15 | 38.7 ± 4.4 (21–65) | Nice knot + locking plate | 2021.6-2022.1 | R | NA | 12 |
| C | 32 | 20/12 | 39.8 ± 5.3 (21–65) | Bridge plate | ||||||
| Tian, et al | 2023 | T | 28 | 21/7 | 51.5 ± 13.5 | Nice knot + bridge plate | 2019.1–2021.6 | R | > 12 | 15 |
| C | 34 | 23/11 | 49.6 ± 14.2 | Locking plate | ||||||
| Lin, et al | 2022 | T | 18 | 10/8 | 61.4 ± 8.3 | Nice knot + Locking plate | 2018.1–2021.6 | R | 24 (12–30) | 13 |
| C | 21 | 13/8 | 65.3 ± 7.2 | Lag screw + Locking plate | ||||||
| Cao, et al | 2022 | T | 49 | 22/27 | 20–59 | Nice knot + intramedullary nail | 2017.2–2020.2 | R | NA | 11 |
| C | 47 | 24/23 |
42.41 ± 12.63 19–58 |
Plate | ||||||
| Hong, et al | 2021 | T | 52 | 34/18 |
50.8 ± 11.2 (24–69) |
Nice knot + locking plate | 2016.12–2019.4 | R |
25.8 ± 7.9 (13–40) |
15 |
| C | 49 | 31/18 |
50.9 ± 12.2 (20–71) |
Lag screw + locking plate |
25.9 ± 8.4 (12–40) |
|||||
| Peng, et al | 2021 | T | 50 | 25/25 |
23–50 mean 32.9 |
Nice knot + locking plate | 2019.3–2020.3 | R |
12–18 mean 14 |
12 |
| C | 50 | 23/27 |
20–45 mean 37.2 |
Kirschner wire/lag screw + locking plate | ||||||
| Hu, et al | 2021 | T | 38 | 21/17 | 35.3 ± 10.2 | Nice knot + locking plate | 2014.1–2019.12 | R | NA | 15 |
| C | 37 | 19/18 | 33.3 ± 10.0 | Locking plate | ||||||
| Chen, et al | 2020 | T | 22 | 15/7 | 48.90 ± 12.50 | Nice knot + locking plate | 2017.1–2019.6 | R |
6–15 (10.7 ± 3.5) |
15 |
| C | 25 | 16/9 | 49.84 ± 12.84 | Locking plate | ||||||
| Wu, et al | 2020 | T | 26 | 17/9 |
18–60 mean 41 |
Nice knot + intramedullary nail | 2016.3–2018.1 | R | NA | 13 |
| C | 56 | 42/14 |
20–65 mean 44 |
Plate | ||||||
| Huang, et al | 2019 | T | 25 | 18/7 |
31.6 ± 1.8 (17–64) |
Nice knot + plate | 2015.6–2018.6 | R | NA | 11 |
| C | 25 | 17/8 |
32.2 ± 1.5 (18–66) |
Plate |
T Trial group, C Control group, R Retrospective study, MINORS Methodological index for non-randomized studies, NA Not available
Operative time and blood loss
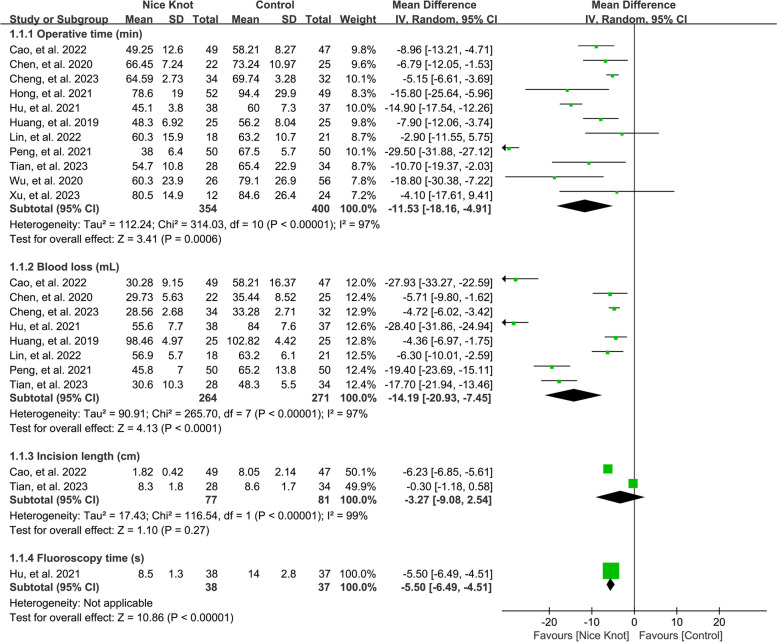
We synthesized results from 11 [8, 10, 11, 24–31] and 8 [8, 25–31] studies, encompassing 754 and 535 cases, respectively, to compare operative time and blood loss between Nice knot-assisted and traditional methods for treating comminuted clavicle fractures. Our pooled analysis indicated that Nice knot-assisted fixation reduced operation time (pooled MD = -11.53, 95% CI: -18.16 to -4.91) and decreased intraoperative blood loss (pooled MD = -14.19, 95% CI: -20.93 to -7.45) compared to conventional methods, as illustrated in Fig. 2. However, the I2 statistic for heterogeneity was 97%, indicating significant variability among the included studies. Meta-regressions involving variations in study time, size of patient populations, inclusion period, MINORS scores, and surgical techniques were performed to explore the source of the high heterogeneity, which indicated that the size of patient population may the source of high heterogeneity (the I2 statistic deceased to 0.001% when the size of patient population is set at 80). Sensitivity analysis, performed by excluding studies one by one, confirmed this trend consistently.
Fig. 2.
Forest plots of the pooled results when assessing the indicators of interest including operative time, blood loss, incision length, and fluoroscopy time
Incision length and fluoroscopy time
Only two studies [25, 28] examined outcomes related to incision length and fluoroscopy time. Our analysis suggested that Nice knots assistance reduced fluoroscopy time but did not significantly affect incision length. The heterogeneity was high, with an I2 statistic of 97%, reflecting substantial variability among the studies. Sensitivity analysis by excluding studies one by one, supported a consistent trend. Meta-regressions were not performed due to the limited records of studies.
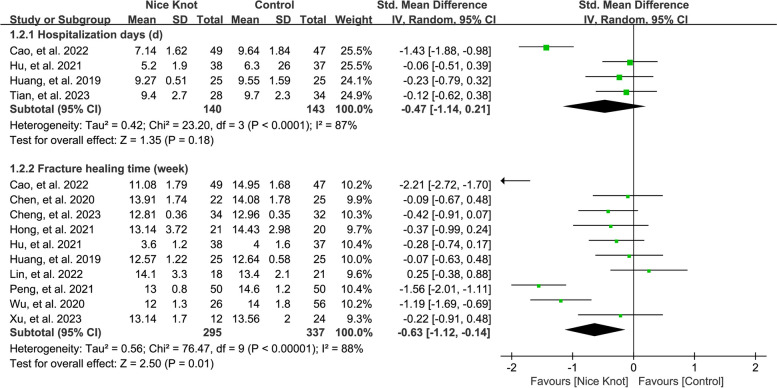
Hospitalization days
Pooling data from 4 studies [8, 25, 28, 31], involving a total of 246 cases, we evaluated the length of hospital stays comparing Nice knots to traditional surgical methods for comminuted clavicle fractures. The pooled analysis showed no significant difference in hospitalization duration (pooled MD = -0.47, 95% CI: -1.14 to 0.21), as depicted in Fig. 3. The I2 statistic for heterogeneity was 87%, indicating considerable heterogeneity. Sensitivity analysis, performed by systematically omitting studies one by one, consistently confirmed this finding.
Fig. 3.
Forest plots of the pooled results when assessing the indicators of interest including complications
Fracture healing time
Results from ten studies [8, 10, 11, 24, 26–31], involving 672 cases, were pooled to evaluate fracture healing time in Nice knots versus traditional methods for comminuted clavicle fractures. Our analysis revealed that Nice knot-assisted fixation shortened the fracture healing period (pooled MD = -0.63, 95% CI: -1.12 to -0.14), as shown in Fig. 3. The I2 statistic was 88%, suggesting significant heterogeneity among the included studies. Sensitivity analysis corroborated a consistent trend. Meta-regressions involving variations in study time, size of patient populations, inclusion period, MINORS scores, and surgical techniques, were performed to explore the source of the high heterogeneity, which indicated that surgical techniques may the source of high heterogeneity (the I2 statistic deceased to 0.001%). Sensitivity analysis, performed by excluding studies one by one, confirmed this trend consistently.
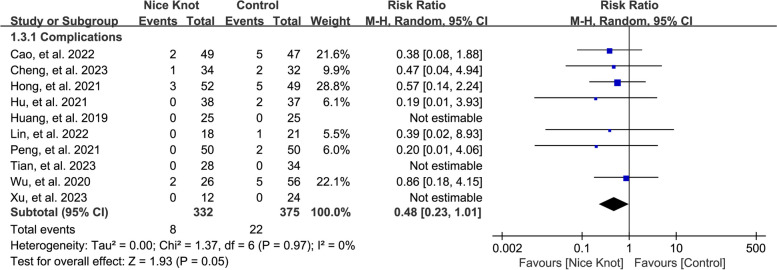
Complications
By aggregating data from ten studies [8, 10, 11, 24–29, 31], involving 707 cases, we assessed complication rates between Nice knots and traditional surgical approaches for treating comminuted clavicle fractures. The pooled analysis indicated no significant difference in complication rates (pooled RR = 0.48, 95% CI: 0.23 to 1.01), as depicted in Fig. 4. The I2 statistic was 0.001%, suggesting negligible heterogeneity. Sensitivity analysis, performed by excluding studies one by one, confirmed a consistent trend across the studies.
Fig. 4.
Forest plots of the pooled results when assessing the indicators of interest including hospitalization days and fracture healing time
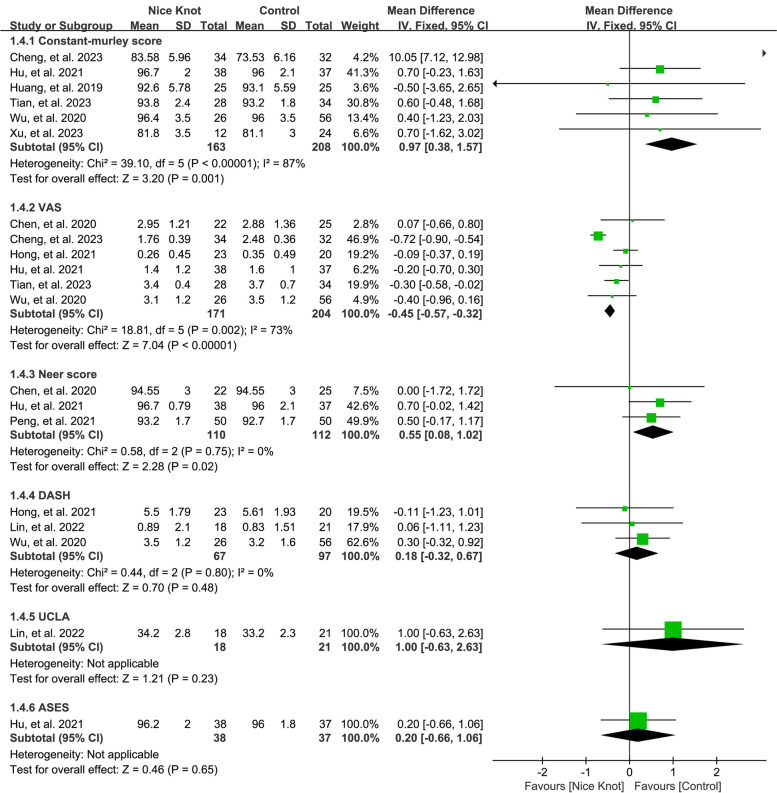
Functional outcomes and pain score
We combined results from six studies [8, 10, 24–26, 31] and six others [8, 10, 11, 25, 26, 30] encompassing 334 and 396 cases respectively, to evaluate the Constant-Murley and VAS scores when comparing Nice knots with traditional surgical methods for comminuted clavicle fractures. The pooled analysis demonstrated that Nice knot-assisted fixation improved the Constant-Murley score (pooled MD = 0.97, 95% CI: 0.38 to 1.57) and reduced VAS scores (pooled MD = -0.45, 95% CI: -0.57 to -0.32), as shown in Fig. 5. The I2 statistic exceeded 50%, indicating substantial heterogeneity. Sensitivity analysis consistently supported these findings. However, a small improvement of constant score (0.97 point) could not represent clinical significance.
Fig. 5.
Forest plots of the pooled results when assessing the indicators of interest including Constant-murley score, neer score, UCLA, VAS, DASH, and ASES
Aggregated data from three studies [8, 29, 30] and three more [10, 11, 27], involving 222 and 22 cases, were used to evaluate Neer score and DASH in Nice knots versus traditional methods. The pooled analysis suggested that Nice knot-assisted fixation enhanced the Neer score (pooled MD = 0.55, 95% CI: 0.08 to 1.02) but did not significantly impact DASH scores (pooled MD = 0.18, 95% CI: -0.32 to 0.67), as shown in Fig. 5. The I2 statistic was 0.001%, indicating minimal heterogeneity. Sensitivity analysis, performed by excluding studies one by one, revealed a consistent trend. Only one study reported outcomes related to UCLA [27] and ASES [8] score, requiring cautious interpretation of these results. The results involving functional outcomes and pain score indicated that both nice knots and traditional surgical methods have satisfactory outcome for the treatment of comminuted clavicle fractures.
Publication bias
Egger’s test results revealed no publication bias when evaluating key indicators such as operative time, blood loss, hospitalization duration, fracture healing time, complications, functional outcomes, and pain scores in the comparison of Nice knots versus traditional surgical methods for comminuted clavicle fractures, as presented in supplementary Figs. 1–4.
Discussion
This meta-analysis comprehensively evaluates the clinical outcomes of Nice knot augmented plate fixation compared to traditional surgical method in the treatment of comminuted midshaft clavicle fractures. By synthesizing evidence from 11 studies, we aim to provide valuable insights into the efficacy and safety of Nice knot augmentation as an auxiliary technique for clavicle fracture management.
One of the key findings of our meta-analysis is the potential reduction in surgical time associated with Nice knot augmented plate fixation compared to traditional single plate fixation. The studies included consistently reported shorter surgical durations in the Nice knot group, suggesting that the use of Nice knots may facilitate a more efficient surgical procedure. The simplified knot tying technique and enhanced stability provided by Nice knots likely contribute to the reduction in surgical time by streamlining the fixation process and minimizing the need for intraoperative adjustments [20].
Our meta-analysis also suggests a possible decrease in intraoperative blood loss with Nice knot augmented plate fixation relative to traditional single plate fixation. This finding indicates that Nice knot augmentation may help to mitigate the risk of excessive bleeding during surgery. The improved control of soft tissue tension and more secure fixation achieved with Nice knots likely contribute to the reduction in intraoperative blood loss by minimizing tissue trauma and vascular injury. Consequently, the use of Nice knots may enhance surgical safety and reduce the need for intraoperative blood transfusions. Indeed, whether the 20 g reduction in blood loss observed with the Nice knot technique impacts the need for blood transfusions is worth considering. While blood transfusion is typically unnecessary for simple clavicle fractures, it may be required in cases with multiple injuries, such as rib fractures or intrathoracic hemorrhage, where minimizing bleeding through clavicular internal fixation becomes crucial. Unfortunately, there is currently no data comparing intraoperative blood transfusion volumes between these two methods.
The analysis of incision length between the two fixation methods shows promising results favoring Nice knot augmented plate fixation [21, 22]. Several studies included in our meta-analysis reported shorter incision lengths in the Nice knot group compared to the traditional single plate group. This finding suggests that the use of Nice knots may allow for smaller incisions while achieving comparable or superior fracture reduction and fixation. The reduced incision length associated with Nice knot augmentation may lead to improved cosmesis, decreased risk of wound complications, and faster postoperative recovery. Our analysis by pooling only two studies [25, 28] suggested that Nice knots assistance reduced fluoroscopy time but did not significantly affect incision length. Moreover, Nice knot could help to reduce soft tissue dissection, and protect the blood supply of fracture block vies by avoiding stripping in the fracture, which could obtain better results.
Our meta-analysis indicates a potential reduction in the length of hospital stay with Nice knot augmented plate fixation compared to traditional single plate fixation [8, 25, 28, 31]. The included studies consistently reported shorter hospital stays in the Nice knot group, suggesting that patients undergoing Nice knot augmentation may experience expedited postoperative recovery and discharge. The shorter hospital stay associated with Nice knot augmentation may lead to cost savings, improved patient satisfaction, and decreased risk of hospital-acquired infections.
Evaluation of postoperative complications is crucial for assessing the safety and efficacy of surgical interventions [8, 10, 11, 24–29, 31]. Our meta-analysis suggests a comparable incidence of postoperative complications, such as implant failure, infection, and malunion, in patients treated with Nice knot augmented plate fixation compared to traditional single plate fixation. The improved biomechanical stability offered by Nice knots may reduce the risk of implant-related complications, while the enhanced soft tissue preservation and reduced surgical trauma associated with Nice knot augmentation may lower the likelihood of wound complications and infection. However, it is important to acknowledge that the incidence of postoperative complications can be influenced by various factors, including patient characteristics, surgical technique, and follow-up duration.
Prompt and effective fracture healing is essential for achieving optimal patient outcomes. Our meta-analysis indicates comparable or shorter time to fracture healing in patients treated with Nice knot augmented plate fixation compared to traditional single plate fixation. The enhanced biomechanical stability provided by Nice knots may promote more rapid callus formation and bone remodeling, facilitating expedited fracture healing [7]. Additionally, the reduced incidence of implant-related complications associated with Nice knot augmentation may contribute to accelerated fracture union. It is obvious that Nice knots also offer potential financial benefits over implants, even though this is not explored in our analysis.
Evaluation of postoperative functional outcomes is essential for assessing the success of surgical interventions in restoring patient mobility and quality of life. Our meta-analysis suggests favorable postoperative functional scores in patients treated with Nice knot augmented plate fixation compared to traditional single plate fixation. The improved biomechanical stability provided by Nice knots likely contributes to better fracture reduction and alignment, leading to enhanced functional recovery. However, results should be interpreted with caution, as a small improvement of 0.97 points in the Constant score may not be clinically significant. We prefer to believe that both the Nice knot and traditional surgical methods show satisfactory outcomes for treating comminuted clavicle fractures, as evidenced by functional outcomes and pain scores.
Despite the valuable insights provided by this meta-analysis, several limitations should be acknowledged. First, the included studies exhibit notable heterogeneity in terms of patient populations, surgical techniques, and outcome measures. This variability could affect the overall reliability and generalizability of our findings. Second, there is variability in the quality of evidence across the included studies, which could introduce potential bias into the meta-analysis results. Additionally, the retrospective nature of many of the studies included in our analysis may impact the robustness of the findings. Retrospective studies are often limited by incomplete data and inherent biases in data collection. The lack of standardized protocols for Nice knot augmentation among the studies further complicates the interpretation of results, as differences in techniques and procedural details may influence outcomes. Moreover, the relatively limited number of studies available for inclusion could restrict the statistical power and precision of our findings. High heterogeneity among the studies, as indicated by our analysis, may obscure true effects and affect the conclusions drawn from the meta-analysis. Lastly, publication bias is a concern, as studies with positive or significant results are more likely to be published compared to those with negative or inconclusive results. This bias may skew the results and affect the overall validity of the meta-analysis. These limitations highlight the need for future research to address these issues, including conducting well-designed, prospective studies with standardized protocols to better assess and validate the findings. Based on the obvious advantages of Nice knots, the efficacy and safety of Nice knot augmentation is as an auxiliary technique for clavicle fracture management. Thus, future research should focus on standardized protocols for the Nice knot technique and longer follow-up periods study need to evaluate long-term outcomes.
Conclusion
This study provides compelling evidence supporting that Nice knot assistance offers advantages in reducing intraoperative blood loss, shortening operation time, and achieving favorable postoperative outcomes.
Supplementary Information
Additional file 1: Supplementary Fig. 1. The results of publication bias when assessing the indicators of interest including operative time, blood loss, incision length, and fluoroscopy time.
Additional file 2: Supplementary Fig. 2. The results of publication bias when assessing the indicators of interest including hospitalization days and fracture healing time.
Additional file 3:Supplementary Fig. 3. The results of publication bias when assessing the indicators of interest including complications.
Additional file 4:Supplementary Fig. 4. The results of publication bias when assessing the indicators of interest including Constant-murley score, neer score, UCLA, VAS, DASH, and ASES.
Acknowledgements
Not applicable.
Abbreviations
- ASES
American shoulder and elbow surgeons
- CBM
China Biology Medicine
- CI
Confidence intervals
- DASH
Disability of the Arm, Shoulder and Hand
- MD
Mean difference
- MINORS
Methodological index for non-randomized studies
- PRISMA
Preferred Reporting Items for a Systematic Review and Meta-analysis
- RCT
Randomized controlled trial
- RR
Risk ratio
- SD
Standard deviation
- VAS
Visual Analogue Scale
Authors’ contributions
LFX, CLJ and LC contributed to the idea of this study. LFX and CLJ searched literatures and screened them independently. LFX, LC, and CLJ screened data and made tables. LFX, DJL, and LLX played an important role in analyzing the outcomes. LFX, DJL, and CLJ conducted the data analyses and made graphs. All authors wrote the first draft and polished and approved the final version. The authors read and approved the final manuscript.
Funding
The design, collection, analysis, and interpretation of the data in the study were financially supported by the Natural Science Foundation of Shandong Province (No.: ZR2021QH307; No.: ZR2021MH013), the Shandong Province Major Scientific and Technical Innovation Project (No.:2021SFGC0502), and the Jinan Clinical Medical Science and Technology Innovation Plan (NO.: 202328065). The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Data availability
All data analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chao Li and Weiwei Cao contributed equally in the planning, construction and writing of the manuscript as the first author.
Contributor Information
Huailin Kou, Email: 15866623279@163.com.
Fanxiao Liu, Email: woshi631@126.com, Email: liufanxiao@sdfmu.edu.cn.
References
- 1.Jeray KJ, Broderick JS, Mullis BH, Everhart J, Tanner SL, Snider BG, et al. Multicenter, prospective, observational study of nonoperative versus operative treatment for high-energy midshaft clavicle fractures. J Orthop Trauma. 2024;38(7):345–50. 10.1097/BOT.0000000000002817. [DOI] [PubMed] [Google Scholar]
- 2.Sabatini CS, Edmonds EW, Nepple JJ, Liotta ES, Hergott K, Quinn M, et al. Nonoperative versus operative treatment of Z-type comminuted clavicle fractures in adolescents: a prospective substratified cohort analysis. J Orthop Trauma. 2024;38(7):351–7. 10.1097/BOT.0000000000002821. [DOI] [PubMed] [Google Scholar]
- 3.Gao Y, Han X, Zhou B, Zhao S, Yu X. A double-suture cerclage reduction technique with Nice knots for comminuted patella fractures (AO/OTA 34-C3). J Orthop Surg Res. 2023;18(1):112. 10.1186/s13018-023-03574-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhong Q, Zhan J, Yang H, Zhu N, Feng R, Yao Y. A new method of nice knot elastic fixation for distal tibiofibular syndesmosis injury. Orthop Surg. 2023;15(3):785–92. 10.1111/os.13635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu J, Chang R, Zhang W, Zhang C, Zhu D, Liu F, et al. Skin stretch suturing with Nice knots in the treatment of small- or medium-sized wounds. J Orthop Surg Res. 2020;15(1):488. 10.1186/s13018-020-02007-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu F, Han S, Liu F, Wang Z, Jia H, Wang F, et al. A modified single-endobutton technique combined with nice knot for treatment of Rockwood type III or V acromioclavicular joint dislocation. BMC Musculoskelet Disord. 2022;23(1):15. 10.1186/s12891-021-04915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedman LGM, Quigley R, Shewman E, Kirsch J, Freehill MT, Garrigues GE. Comparison of mechanical properties between nice knot, modified nice knot, and surgeon’s knot. Clin Biomech (Bristol Avon). 2021;90: 105486. 10.1016/j.clinbiomech.2021.105486. [DOI] [PubMed] [Google Scholar]
- 8.Hu F, Liu X, Liu F, Jia H, Lv X, Wang F, et al. Intraoperative Nice knots assistance for reduction in displaced comminuted clavicle fractures. BMC Musculoskelet Disord. 2021;22(1):467. 10.1186/s12891-021-04348-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kong LP, Yang JJ, Wang F, Liu FX, Yang YL. Minimally invasive open reduction of greater tuberosity fractures by a modified suture bridge procedure. World J Clin Cases. 2022;10(1):117–27. 10.12998/wjcc.v10.i1.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu Y, Kang Y, Rui Y, Liu J, Jun GU, Ma Y, et al. Comparison of clinical efficacy of nice knot assisted intramedullary nailing and plate fixation in the treatment of adult midshaft clavicle fracture. Chin J Hand Surg. 2020;36(6):435. 10.3760/cma.j.cn311653-20200218-00055. [Google Scholar]
- 11.Hong S, Wang W, Guo J, He F, Wang C. The comparison of Nice knots and traditional methods as an auxiliary reduction-fixation technique in pre-contoured locking plate fixation for comminuted Robinson type 2B clavicle fracture: a retrospective study. Med (Baltim). 2021;100(23): e26282. 10.1097/MD.0000000000026282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350: g7647. 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 13.Teng A, Liu F, Zhou D, He T, Chevalier Y, Klar RM. Effectiveness of 3-dimensional shoulder ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. Med (Baltim). 2018;97(37): e12405. 10.1097/MD.0000000000012405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6. 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 15.Liu F, Dong J, Zhou D, Kang Q, Xiong F. Gout is not associated with the risk of fracture: a meta-analysis. J Orthop Surg Res. 2019;14(1):272. 10.1186/s13018-019-1317-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu F, Dong J, Kang Q, Zhou D, Xiong F. Subacromial balloon spacer implantation for patients with massive irreparable rotator cuff tears achieves satisfactory clinical outcomes in the short and middle of follow-up period: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2021;29(1):143–53. 10.1007/s00167-019-05834-3. [DOI] [PubMed] [Google Scholar]
- 17.Liu F, Meng Q, Yin H, Yan Z. Stem cells in Rotator Cuff injuries and reconstructions: a systematic review and meta-analysis. Curr Stem Cell Res Ther. 2019;14(8):683–97. 10.2174/1574888X14666190617143952. [DOI] [PubMed] [Google Scholar]
- 18.Wang X, Zhang W, Dong J, Li L, Xiao Y, Liu F. Three-dimensional sonography has satisfied accuracy for detecting rotator cuff tears. Front Surg. 2024;11:1411816. 10.3389/fsurg.2024.1411816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu F, Dong J, Shen Y, Yun C, Wang R, Wang G, et al. Comparison of PET/CT and MRI in the diagnosis of bone metastasis in prostate Cancer patients: A Network Analysis of Diagnostic studies. Front Oncol. 2021;11:736654. 10.3389/fonc.2021.736654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tangjaroenpaisan Y, Klabklay P, Maliwankul K, Chuaychoosakoon C. Using a nice knot to simplify and strengthen closed reduction in displaced distal clavicle fracture: a technical note. J Surg Case Rep. 2024;2024(6):rjae196. 10.1093/jscr/rjae196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kang Y, Zhang Q, Ma Y, Zhou M, Jia X, Lin F, et al. Clinical effect of nice knot-assisted minimally invasive titanium elastic nail fixation to treat Robinson 2B midshaft clavicular fracture. BMC Musculoskelet Disord. 2024;25(1):59. 10.1186/s12891-024-07197-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu G, Chen YQ, Chen CY, Lin ZX, Xie QY, Ye JJ, et al. Clinical outcomes of doubled-suture nice knot augmented plate fixation in the treatment of comminuted midshaft clavicle fracture. BMC Surg. 2021;21(1):270. 10.1186/s12893-021-01274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen M, Jin X, Fryhofer GW, Zhou W, Yang S, Liu G, et al. The application of the nice knots as an auxiliary reduction technique in displaced comminuted patellar fractures. Injury. 2020;51(2):466–72. 10.1016/j.injury.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Xu T, Ma G, Wu Y, Chang J, Zhang C, Zhou P, et al. Clinical observation of applying nice knot for the treatment in clavicle fractures. J Chin Orthop Res. 2023;8(4):202. 10.19548/j.2096-269x.2023.04.002. [Google Scholar]
- 25.Tian H, Chai L, Song C, Liang X, Qiao B, Zhang K. Comparison of two internal fixations for midshaft clavicle fractures. Orthop J China. 2023;31(8):678. 10.3977/j.issn.1005-8478.2023.08.02. [Google Scholar]
- 26.Cheng C, Xu X, Lu D, Zhu J, Chen N. Comparative study on the efficacy of bridge combined type internal fixation system combined with Nice knot and locking plate in the treatment of comminuted fracture of middle clavicle. Progress Mod Biomed. 2023;23(3):534. 10.1324/j.cnki.pmb.2023.03.027. [Google Scholar]
- 27.Lin X, Wei G, Lin P, Xie J. Comparison of therapeutic effects of nice knot and common screw combined with anatomical locking plate in the treatment of oblique fracture of middle clavicle. Chin J Bone Joint Injury. 2022;37(11):1171. 10.7531/j.issn.1672-9935.2022.11.014. [Google Scholar]
- 28.Cao W, Zhang Y. Comparison of the effect of nice knot assisted intramedullary nail and traditional incision plate in the treatment of middle clavicle fracture in adults. Guizhou Med J. 2022;5:704. [Google Scholar]
- 29.Peng Q, Wen X, Xie X, Li Z, Lin Z, Wang Z, et al. Comparison of therapeutic effects of modified nice knot and kirschner wire combined with plate internal fixation in the treatment of middle and distal clavicle fractures. Chin J Bone Joint Injury. 2021;36(11):1190. 10.7531/j.issn.1672-9935.2021.11.024. [Google Scholar]
- 30.Chen J, Ma J, Ma X, Zhao L, Wan F, Zhang Q, et al. Comparison of the nice knot assisted reduction technique and the traditional reduction technique in the treatment of displaced comminuted midshaft clavicle fracture. Chin J Hand Surg. 2020;8(3):220. 10.3877/cma.j.issn.2095-5790.2020.03.006. [Google Scholar]
- 31.Huang E, Feng Y, Huang C. Clinical observation on adjuvant treatment of comminuted fracture of clavicle terminal with nice node. Fujian Med J. 2019;41(5):62. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Fig. 1. The results of publication bias when assessing the indicators of interest including operative time, blood loss, incision length, and fluoroscopy time.
Additional file 2: Supplementary Fig. 2. The results of publication bias when assessing the indicators of interest including hospitalization days and fracture healing time.
Additional file 3:Supplementary Fig. 3. The results of publication bias when assessing the indicators of interest including complications.
Additional file 4:Supplementary Fig. 4. The results of publication bias when assessing the indicators of interest including Constant-murley score, neer score, UCLA, VAS, DASH, and ASES.
Data Availability Statement
All data analyzed during this study are included in this published article.