Abstract
The exposome encompasses the full range of environmental exposures throughout a person’s lifetime and plays an important role in cardiovascular health. Interactions with the social, natural, and built components of the exposome significantly impact cardiovascular disease prevalence and mortality. Robust data analytics, including machine learning and geospatial analysis, have advanced our understanding of how these factors converge to influence cardiovascular disease risk. The integration of multiomics platforms and advanced computational approaches enhances our ability to characterize the exposome, leading to targeted public health interventions and innovative risk reduction strategies aimed at improving cardiovascular health globally. These multiomics platforms that integrate factors such as genomics, epigenomics, clinical data, social factors, environmental factors, and wearable technology will characterize the exposome in greater detail concerning cardiovascular health. In this review, we aimed to elucidate the components of the exposome and discuss recent literature regarding their relationship to cardiovascular health.
Keywords: exposome, electronic health data, big data
Introduction
Understanding the exposome is essential for advancing our knowledge of cardiovascular health. The exposome encompasses the full range of exposures a person encounters throughout their lifetime, including physical and chemical factors, living and working environments, occupation, and food security. Defining and understanding the impact of different components of the cardiovascular exposome (Figure 1) has become an emerging field supported by robust data.1 For example, studies have demonstrated the causal impact of various environmental factors such as air pollution, noise pollution, and light pollution on cardiovascular disease prevalence. Air pollution is recognized as one of the leading causes of morbidity and mortality worldwide, often indirectly through cardiovascular disease.2,3 The Global Burden of Disease study revealed that these types of environmental exposures are responsible for the vast majority of cardiovascular disease burden in Africa and South Asia.1,2
Figure 1.
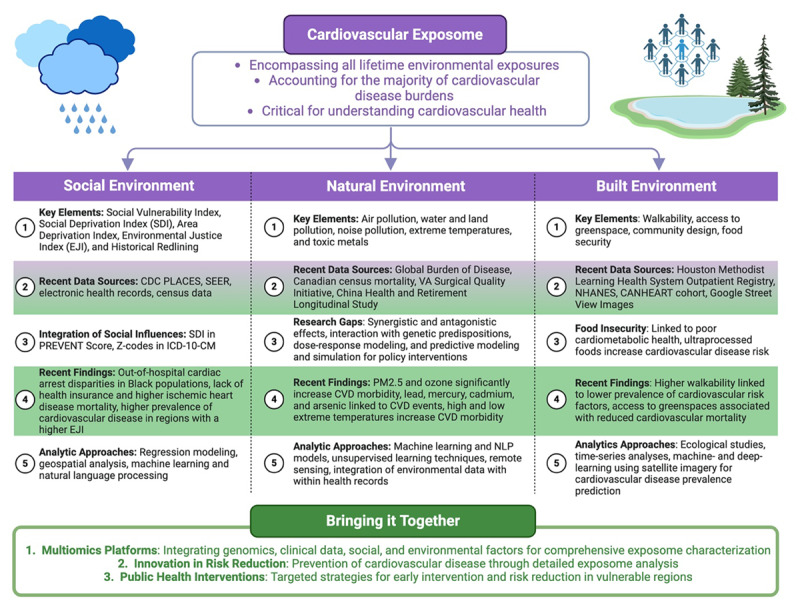
Overview of the cardiovascular exposome and its components. SDI: social deprivation index; CVD: cardiovascular disease; NLP: natural language processing: PM2.5: fine particulate matter smaller than 2.5 micrometers in diameter
The exposome refers to the totality of exposures individuals encounter and encompasses a wide range of internal and external factors. Historically, capturing the exposome has been challenging due to limited historical data. However, with growing recognition of the cardiovascular exposome’s complex impact, we propose categorizing it into three distinct domains: social, natural, and built environments. The social environment component includes factors such as socioeconomic distress, vulnerability, environmental justice, and access to health care. The natural environment encompasses pollution of air, water, and land as well as extreme temperatures. Finally, the built environment consists of human-designed spaces where people live and engage in daily activities, highlighting aspects such as walkability, access to greenspace, and community design.
In this review, we outline important data sources for each exposome category and discuss findings of recent literature as to how this component of the exposome may affect cardiovascular health and disease. This paper also introduces the characterization of environmental exposures in relation to cardiovascular prevention, prevalence, and outcomes.1
Data Analytics in the Social Environment
The social environment significantly impacts cardiovascular health through factors such as systemic racism, marginalization, discrimination, economic status, and social deprivation. Recent studies have investigated various social quantification methods and their relationship to cardiovascular health (Table 1). These methods include the Social Vulnerability Index, Social Deprivation Index (SDI), and Area Deprivation Index, which have been explored across the wide cardiovascular health spectrum, from diagnosis and prevention to management and prognostic implications.4,5,6,7,8,9,10,11,12,13,14,15 These indices quantify the magnitude of many social influences, such as household composition, transportation, financial status, and minority racial and ethnic status. Given the recognized importance of quantifying social influences in cardiovascular care, the updated risk prognostication scoring system, the Predicting Risk of Cardiovascular Disease Events (PREVENT) Score, has incorporated the SDI into its algorithm for predicting future cardiovascular events.16
Table 1.
Studies investigating the association between the social environment and cardiovascular outcomes. CDC: Centers for Disease Control and Prevention; ATSDR: Agency for Toxic Substances and Disease Registry; CMS: Centers for Medicare and Medicaid Services; SVI: Social Vulnerability Index; CVD: cardiovascular disease; AMI: acute myocardial infarction; HF: heart failure; IHD: ischemic heart disease; CPR: cardiopulmonary resuscitation
|
| ||||
|---|---|---|---|---|
| STUDY | STUDY PLACE/YEAR | DATABASE UTILIZED | INDEX | ASSOCIATION WITHIN THE CARDIOVASCULAR EXPOSOME |
|
| ||||
| The Association Between Neighborhood Social Vulnerability and Cardiovascular Health Risk Among Black/African American Women in the InterGEN Study | USA/2021 | InterGEN Study, CDC/ATSDR | SVI | Neighborhood social vulnerability and increased cardiovascular risk factor prevalence among Black women |
|
| ||||
| Neighborhood-level Social Vulnerability and Prevalence of Cardiovascular Risk Factors and Coronary Heart Disease | USA/2023 | CDC Behavioral Risk Factor Surveillance System database (BRFSS), CDC/ATSDR | SVI | SVI and increased cardiovascular risk factors and prevalence of coronary heart disease |
|
| ||||
| Impact of Social Vulnerability on Comorbid Cancer and Cardiovascular Disease Mortality in the United States | USA/2022 | CDC WONDER, CDC/ATSDR | SVI | Social vulnerability and increased mortality attributed to comorbid cancer and CVD |
|
| ||||
| Impact of the Social Vulnerability Index on Pulmonary Embolism Mortality | USA/2023 | CDC WONDER, CDC/ATSDR | SVI | SVI and disproportionate patterns of pulmonary embolism-related mortality in US counties |
|
| ||||
| Impact of social vulnerability on comorbid COVID-19 and acute myocardial infarction mortality in the United States | USA/2023 | CDC WONDER, CDC/ATSDR | SVI | SVI and increased comorbid COVID-19 and AMI mortality |
|
| ||||
| Mortality trends, disparities, and social vulnerability in cardiac arrest mortality in the young: A cross-sectional analysis | USA/2024 | CDC WONDER, CDC/ATSDR | SVI | SVI and worse cardiac arrest outcomes in the young |
|
| ||||
| Association Between Social Vulnerability Index and Cardiovascular Disease: A Behavioral Risk Factor Surveillance System Study | USA/2022 | CDC BRFSS, CDC/ATSDR | SVI | SVI and greater self-reported prevalent cardiovascular comorbidities and atherosclerotic cardiovascular disease |
|
| ||||
| Social Vulnerability and Premature Cardiovascular Mortality Among US Counties, 2014 to 2018 | USA/2021 | CDC WONDER, CDC/ATSDR | SVI | SVI and increased premature CVD mortality across US counties |
|
| ||||
| Social Vulnerability and Cardiovascular-Related Mortality Among Older Adults in the United States | USA/2024 | CDC WONDER, CDC/ATSDR | SVI | SVI and greater CVD-related mortality in older adults |
|
| ||||
| Social Vulnerability and Location of Death in Heart Failure in the United States | USA/2023 | CDC WONDER, CDC/ATSDR | SVI | SVI and disparities in trends in location of death in patients with HF |
|
| ||||
| Impact of Social Vulnerability and Demographics on Ischemic Heart Disease Mortality in the United States | USA/2023 | CDC WONDER, CDC/ATSDR | SVI | SVI and disparities in IHD mortality |
|
| ||||
| Development and Validation of the American Heart Association’s PREVENT Equations | USA/2024 | The Chronic Kidney Disease Prognosis Consortium | Predicting Risk of CVD EVENTs (PREVENT) score, SDI | Risk estimation of total CVD for US adults 30 to 79 years of age without CVD at baseline |
|
| ||||
| County-level variation in healthcare coverage and ischemic heart disease mortality | USA/2024 | CDC WONDER, CDC PLACES | Healthcare coverage deficiency | Healthcare coverage deficiency and increased IHD mortality from IHD |
|
| ||||
| Association of Environmental Injustice and Cardiovascular Diseases and Risk Factors in the United States | USA/2024 | CDC PLACES, CDC/ATSDR | Environmental Justice Index | Environmental injustice and increased prevalence of CVD risk factors |
|
| ||||
| Historical neighborhood redlining and bystander CPR disparities in out-of-hospital cardiac arrest | USA/2024 | Cardiac Arrest Registry to Enhance Survival (CARES) | Redlining | Historical redlining and reduced bystander CPR |
|
| ||||
| Influence of social vulnerability index on Medicare beneficiaries’ expenditures upon discharge | USA/2024 | CMS database, CDC/ATSDR | SVI | Social vulnerability and greater healthcare costs among Medicare beneficiaries |
|
| ||||
Data sources for studying social influences on the cardiovascular exposome include numerous registries. Census data, used for nationally representative samples, helps test complex social hypotheses and their impact on cardiovascular outcomes. The Centers for Disease Control and Prevention Population-Level Analysis and Community Estimates (PLACES) dataset, Surveillance, Epidemiology, and End Results (SEER) dataset, and electronic health records are valuable sources of such social influences. The Centers for Disease Control and Prevention’s PLACES dataset utilizes data from the American Community Survey to obtain 5-year estimates of various social factors, which include housing crowding, internet access, housing costs, poverty rates, educational attainment, and unemployment rates.17 For example, one recent analysis found a higher rate of ischemic heart disease mortality in regions with a greater lack of health insurance.18 Additionally, the SEER dataset, introduced by the National Cancer Institute, provides data on cancer statistics, including incidence rates, survival, and mortality-related outcomes. A multitude of studies have investigated cardiovascular outcomes in relation to patients with malignancies using the SEER dataset.19,20,21,22,23
The Environmental Justice Index (EJI) is another quantification method that incorporates many social variables, such as the Social Vulnerability Index, and includes various environmental factors obtained from the US Census Bureau, the US Mine Safety and Health Administration, and the US Environmental Protection Agency.24 A recent study aggregated prevalence rates of cardiovascular diseases within census tracts into quartiles of the EJI and compared the prevalence of cardiovascular diseases through risk ratios by multivariable Poisson regression models.25 This study found a greater prevalence of cardiovascular disease burden in US regions with a higher EJI. Another method to quantify the impact of social influences on cardiovascular health includes historical redlining, a practice that previously classified neighborhoods for mortgage risk primarily driven by racial segregation. One recent analysis evaluated the impact of historical redlining on out-of-hospital cardiac arrest bystander involvement. Using data from the Cardiac Arrest Registry to Enhance Survival, the study found that historical segregation practices led to reduced rates of bystander cardiopulmonary resuscitation.26
Furthermore, since 2015, efforts have led to the integration of social determinants coding within the International Classification of Diseases system through Z-codes within ICD-10-CM, classified as Z55 to Z65.27 These codes represent psychosocial and socioeconomic factors, with the goal of identifying health risks associated with a patient’s social context. Z-coding domains include housing situation, economic circumstances, educational attainment, occupational exposures, employment status, and physical and social environments. Although Z-coding has been significantly underutilized, studies revealed an association between Z-coding documentation and increased prevalence of hypertension, greater comorbidity burden, and increased pharmaceutical costs.28,29
Analytic approaches to exploring social influences on the cardiovascular exposome include structural equation modeling and multiple regression, which are frequently used in ecological studies. However, many studies in this area are cross-sectional or retrospective, showing numerous associations without establishing causality, thus limiting the interpretability of the results. Regression modeling with appropriate control for confounding variables is crucial for identifying the independent effects of social factors on cardiovascular health; however, it continues to have limitations. Future efforts directed at cohort studies are therefore vital for understanding how social determinants directly impact cardiovascular health and tracking changes over time to establish causal relationships.
Geospatial analysis is also an important tool for exploring the spatial distribution of social determinants of cardiovascular health. One study used a geographic information system analysis of a multisite and multiyear cohort investigating out-of-hospital cardiac arrest outcome disparities, revealing significant racial and socioeconomic disparities in out-of-hospital cardiac arrest outcomes, particularly impacting Black populations in the US.30 Furthermore, it also revealed that university hospital settings, as opposed to safety net hospitals that primarily serve Black populations with lower socioeconomic status, had higher income commercially and the lowest odds of death among Medicare-insured patients. Through the integration of geographic information systems with population health data, it becomes easier to visualize and analyze geographical patterns that correlate social determinants with cardiovascular health. This approach can identify higher-risk areas to enable targeted public health interventions and appropriate resource allocation, ultimately guiding policymakers to implement effective strategies that promote healthcare equity. For example, although social vulnerability has been associated with higher overall Medicare expenditures,31 there is no robust evaluation about whether cardiovascular care-related expenditures are affected by social vulnerability.
Finally, advancements in innovative analytic techniques such as machine learning algorithms and natural language processing (NLP) have significantly enhanced our ability to handle large and complex datasets, allowing for nuanced hypothesis testing.32 For example, NLP approaches can extract meaningful and prognostically relevant information from unstructured data sources, providing valuable insights into social factors. NLP methods can include rule-based algorithms, deep-learning techniques, and supervised machine learning. Among the various types of NLP, one study revealed that machine-learning approaches are commonly applied to social factors, including substance use and homelessness, rule-based methods for housing and transportation factors, and deep-learning for cardiovascular risk factors utilizing complex datasets.32,33,34,35,36,37 One study in 2021 assessed rehospitalization risk in populations with acute myocardial infarction using NLP methods, particularly evaluating the impact of various social factors including social support systems and housing.38 Similarly, one study used the open-source Canary NLP system to explore the capability of this algorithm to detect multiple cardiovascular comorbidities including stroke, hypertension, dyslipidemia, diabetes, and coronary artery disease, resulting in an accurate and predictive model.39
Data Analytics in the Natural Environment
The natural environment influences cardiovascular health, particularly through factors such as air pollution, water and land pollution, and extreme temperatures (Table 2).40,41,42 For example, recent studies have investigated the impact of environmental factors within the exposome on increased atrial fibrillation risk,43 an underrecognized phenomenon. Additionally, numerous studies have established a strong association between air pollution and cardiovascular disease.2 The Global Burden of Disease study, for instance, identified air pollution as a leading environmental health risk.2 Specifically, fine particulate matter smaller than 2.5 micrometers in diameter, known as PM2.5, is a major component of air pollution.44 The relationship between PM2.5 and cardiovascular diseases is well-documented. While chronic exposures to PM2.5 have shown a significant impact on cardiovascular health outcomes,45 acute and shorter-term exposures can also lead to a considerable increase in cardiovascular morbidity.46,47 For instance, a Canadian study found that for each 1 µg/m3 increase in PM2.5, there was a 25% increase in the 10-year hazard ratio for cardiovascular mortality.48 Among the cardiovascular disorders, cerebrovascular disease morbidity and mortality also play a prominent role as being significantly influenced by PM2.5 exposure.49 One study exploring a US veteran cohort that has undergone coronary artery bypass grafting found that patients living in regions with higher ambient PM2.5 were associated with higher rates of 10-year cardiovascular events.50 Furthermore, high blood pressure has also been identified in US regions with air pollution that has exceeded the World Health Organization guidelines.51
Table 2.
Studies investigating the association between the natural environment and cardiovascular (CV) outcomes. CDC: Centers for Disease Control and Prevention; ATSDR: Agency for Toxic Substances and Disease Registry; CABG: coronary artery bypass graft
|
| ||||
|---|---|---|---|---|
| STUDY | STUDY PLACE/YEAR | DATABASE UTILIZED | INDEX | ASSOCIATION WITHIN THE CV EXPOSOME |
|
| ||||
| Long-term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project | Europe/2014 | European Study of Cohorts for Air Pollution Effects (ESCAPE) | Ambient air pollution | Long-term exposure to airborne pollutants and increasing incidence of acute coronary events |
|
| ||||
| Short-Term Exposure to Ambient Air Pollution and Mortality From Myocardial Infarction | China/2021 | National mortality surveillance system in Hubei province | Ambient air pollution | Short-term exposure to air pollution and worse myocardial infarction outcomes |
|
| ||||
| Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: a Canadian national-level cohort study | Canada/2012 | 1991–2001 Canadian census mortality | Ambient air pollution | Long-term exposure to ambient PM2.5 and greater cardiovascular mortality |
|
| ||||
| Spatiotemporal Trends of Stroke Burden Attributable to Ambient PM2.5 in 204 Countries and Territories, 1990–2019: A Global Analysis | Global/2023 | Global Burden of Disease study 2019 | Ambient air pollution | Ambient PM2.5 exposure and greater stroke burden |
|
| ||||
| Disparities in Excess Blood Pressure Across the U.S. Associated With Air Pollution Exceeding WHO Guidelines | USA/2024 | CDC/ATSDR Social Vulnerability Index | Ambient air pollution | Air pollution and racial disparities in excess blood pressure |
|
| ||||
| Air Pollution and Adverse Cardiovascular Events After Coronary Artery Bypass Grafting | USA/2024 | VA Surgical Quality Initiative Project (VASQIP) | Ambient air pollution | Increased major adverse cardiovascular events and air pollution after CABG |
|
| ||||
| Exposure to ambient air pollution and the incidence of congestive heart failure and acute myocardial infarction: A population-based study of 5.1 million Canadian adults living in Ontario | Canada/2019 | Ontario Population Health and Environment Cohort (ONPHEC) | Ambient air pollution | Air pollution and greater incidence of congestive heart failure and myocardial infarction |
|
| ||||
| Long-term exposure to ozone and cardiovascular mortality in China: a nationwide cohort study | China/2022 | China Chronic Disease and Risk Factors Surveillance (CCDRFS) | Ozone | Long-term exposure to ozone and increased cardiovascular mortality |
|
| ||||
| Long-Term Exposure to Ozone and Fine Particulate Matter and Risk of Premature Coronary Artery Disease: Results from Genetics of Atherosclerotic Disease Mexican Study | Mexico/2022 | Genetics of Atherosclerotic Disease (GEA) study | Ozone and Fine Particulate Matter | Long-term exposure to ozone and PM2.5 and worse premature coronary artery disease outcomes |
|
| ||||
| Association of Blood Lead level with Elevated Blood Pressure in Hypertensive Patients | USA/2021 | NHANES | Lead | Blood lead levels and increased prevalence of hypertension |
|
| ||||
| Quantifying lead-attributable cardiovascular disease burden in the United States | USA/2024 | The 2019 Global Burden of Disease Study | Lead | Lead-related cardiovascular burden disparities |
|
| ||||
| Outdoor artificial light at night and incident cardiovascular disease in adults: A national cohort study across China | China/2024 | China Health and Retirement Longitudinal Study (CHARLS) | Light pollution | Outdoor artificial light at night and increased risk of cardiovascular disease |
|
| ||||
Ozone, another independent risk predictor of cardiovascular mortality, has been shown to affect cardiometabolic health in both short- and long-term exposures.52,53,54 The combined presence of ozone with other air pollutants can amplify adverse health effects through changes in chemical half-life, potentially disrupting the blood-brain barrier and causing endothelial dysfunction.48 Furthermore, toxic metals such as arsenic, mercury, lead, and cadmium also play a major role in the natural environment’s impact on cardiovascular health.55 These metals have been linked to various cardiometabolic diseases. For example, lead exposure, which remains particularly high in middle- to low-income countries, significantly increases blood pressure and is associated with cardiovascular mortality.56,57 Lead, mercury, cadmium, and arsenic exposure have also been linked to an increase in cardiovascular disease-related mortality.58,59,60 Lastly, extreme temperatures, whether below or above the optimal range, have been widely associated with increased cardiovascular morbidity and mortality.2
Despite current knowledge about the impact of the natural environment on the cardiovascular exposome, significant gaps remain in this area of research. While many of the studies have revealed the individualistic effects of pollutants, there is minimal understanding of the synergistic or potentially antagonistic effects when multiple pollutants are presented at various levels. This is supported by one study that revealed the synergistic impact of noise pollution combined with air pollution, as both of these factors converge at the vascular level to promote oxidative stress and inflammation, thus contributing to the cardiovascular risk factor burden.61 Furthermore, mechanistic understandings regarding genetic predispositions and their respective interaction with environmental factors are important to effectively identify vulnerable populations. These populations, including those with existing health conditions and economically disadvantaged groups, may be more susceptible to increasing hazardous exposure. Additionally, while most of the studies investigating the impact of the natural exposome on cardiovascular health are retrospective and cross-sectional, more longitudinal studies that track environmental exposures over an entire life course may yield detailed insights regarding exposome-related early-life, adolescence, and adult-related outcomes.62 Longitudinal studies would also facilitate dose-response modeling that may quantify the relationship between exposure levels and health outcomes more precisely over a prolonged period of time.
A recent study used data from the China Health and Retirement Longitudinal Study to explore the impact of artificial light exposure, obtained from satellite image data, on incident cardiovascular disease.63 They found that both low and high outdoor artificial light exposure were associated with greater rates of cardiovascular disease. This study emphasizes the crucial role of remote sensing technologies in monitoring environmental exposures. Satellite data can provide detailed information on air quality, temperature variations, and land use changes over time. By integrating this data with health records, longitudinal studies become feasible.63 This integration may also enable increasingly accurate predictive modeling techniques, aiding future predictions of cardiovascular events based on environmental data. These models can potentially simulate various scenarios, such as changes in pollution levels due to policy interventions, and predict their impact on cardiovascular health.
Machine learning and artificial intelligence algorithms could enhance our understanding of the relationship between the natural environment and cardiovascular health. One study evaluated the performance of multiple artificial intelligence models using nitrogen dioxide levels from ground-based monitoring systems and found that these models accurately forecasted nitrogen dioxide levels, potentially impacting future monitoring system approaches.64 Furthermore, unsupervised learning techniques like clustering can group similar exposure profiles to determine their respective impact on cardiovascular health. Ultimately, while many cardiovascular outcomes have shown an association with poor natural exposome environments, the implementation of science and translation into effective public health policies remain poorly understood.
Data Analytics in the Built Environment
The built environment, encompassing human-designed spaces where people live and engage in daily activities, is increasingly recognized as a significant factor that impacts cardiometabolic health (Table 3).65 The built environment significantly influences cardiovascular health by shaping behavioral risk factors associated with cardiovascular disease. Key attributes, such as promoting active lifestyles, providing access to recreational spaces and greenspace, encouraging walkability, and ensuring food security, all play a crucial role in this relationship.
Table 3.
Studies investigating the association between the built environment and cardiovascular outcomes.
|
| ||||
|---|---|---|---|---|
| STUDY | STUDY PLACE/YEAR | DATABASE UTILIZED | INDEX | ASSOCIATION WITHIN THE CARDIOVASCULAR EXPOSOME |
|
| ||||
| Favorable Neighborhood Walkability is Associated With Lower Burden of Cardiovascular Risk Factors Among Patients Within an Integrated Health System: The Houston Methodist Learning Health System Outpatient Registry | USA/2023 | Houston Methodist Learning Health System Outpatient Registry | Walkability | Reduced neighborhood walkability and increased cardiovascular risk factors |
|
| ||||
| Interaction between neighborhood walkability and traffic-related air pollution on hypertension and diabetes: The CANHEART cohort | Canada/2019 | CANHEART cohort | Walkability | Reduced walkability and increased traffic-related air pollution and greater cardiovascular risk factor prevalence |
|
| ||||
| Greenspace seems protective of both high and low blood pressure among residents of an Alpine valley | Austria/2018 | Environmental Health Impact Assessment | Greenspace | Residential greenspace and disparities in abnormal blood pressures |
|
| ||||
| Long-term secondary prevention of cardiovascular disease with a Mediterranean diet and a low-fat diet (CORDIOPREV): a randomized controlled trial | Spain/2022 | CORDIOPREV | Mediterranean diet, low-fat diet | Effectiveness of the Mediterranean and low-fat diet on secondary cardiovascular prevention |
|
| ||||
| Food Insecurity Is Associated With Cardiovascular and All-Cause Mortality Among Adults in the United States | USA/2020 | US National Health and Nutrition Examination Survey | Food insecurity | Adult food insecurity and worse cardiovascular disease outcomes |
|
| ||||
| Food Environment Quality and Cardiovascular Disease Mortality in the United States: a County-Level Analysis from 2017 to 2019 | USA/2024 | CDC WONDER, County Health Rankings compilation | Food environment index | Food environment quality and greater cardiovascular mortality burden |
|
| ||||
Key elements of the built environment include walkability, access to greenspace, and community design. For example, using data from the Houston Methodist Learning Health System Outpatient Registry, the relationship between cardiovascular risk factors and neighborhood walkability were explored.66 Using a cross-sectional design, this study identified that patients who resided in the most walkable regions had the least prevalence of cardiovascular risk factors—including hypertension, obesity, diabetes, and dyslipidemia—regardless of the presence of clinical atherosclerotic coronary disease.66 Furthermore, a cross-sectional study using data from the Cardiovascular Health in Ambulatory Care Research Team (CANHEART) cohort investigated the relationship between neighborhood walkability and cardiovascular disease risk factors67 and found that lower walkability was also associated with higher rates of hypertension and diabetes.67 This reflects that actively targeting factors associated with improved cardiovascular health, well-being, and quality of life should be encouraged within the exposome framework, a concept recently coined as the “benignome,” in contrast to the “pollutome” which relates to chemical and physical pollutants.68
Access to greenspaces—areas with shrubs, grass, trees, or other vegetation—offers cardiovascular protection through encouraging physical activity and social interaction while also mitigating noise and air pollution exposure. For example, increased residential greenery correlated with increased protection against both high and low blood pressure69 and reduced cardiovascular mortality.70 Another aspect of the built environment impacting cardiovascular health is food insecurity, characterized by limited access to sufficient and nutritious food. Over 10% of American adults experience food insecurity, which is linked to poor cardiometabolic health.71 Moreover, one study investigated the impact of food insecurity on 27,188 individuals who participated in the US National Health and Nutrition Examination Survey.72 It found that participants with low food security had higher rates of all-cause and cardiovascular disease-related mortality compared to participants with higher food security, regardless of adjustment for other demographic and socioeconomic variables.72 Another retrospective analysis examined the impact of the food environment index, a measure of food insecurity and food deserts, on cardiovascular mortality73 and found that a lower food environment index was associated with higher cardiovascular mortality, with the most pronounced effect in counties with greater income inequality and a predominantly African-American population. A corroborating retrospective cohort analysis revealed that food deserts were associated with a higher proportion of residing US veterans with established atherosclerotic cardiovascular disease and subsequently higher risks of all-cause mortality and cardiac events.74
Mechanisms related to food insecurity and cardiovascular health are likely multifactorial. Populations with a lower socioeconomic status may have a greater tendency to consume cheaper, calorie-dense foods, which may lead to insulin resistance and adipose tissue deposition, along with the emotional and physiological stress associated with food insecurity. Additionally, the financial burden from healthcare costs can negatively affect financial security, potentially leading individuals to opt for more affordable food choices. Similarly, the consumption of ultra processed foods, which are industrially produced and often energy-dense, has surged in both middle- and high-income countries.75 Ultra processed foods are linked to poor cardiovascular health outcomes, contributing to the development of diabetes, obesity, hypertension, and hyperlipidemia.76
Advancements in artificial intelligence, similar to those in the social and natural components of the exposome, have progressed considerably in recent years. For example, a recent study used satellite imagery of different US cities to investigate its predictive capabilities regarding the prevalence of chronic kidney disease, cerebrovascular disease, and coronary heart diseases.77 This study built a model that accurately estimated the census-level burden of cardiometabolic disease prevalence by utilizing a deep learning network consisting of Google Street View features. Subsequently, machine learning models were used for prevalence prediction, resulting in appropriately predictive models.77 Another cross-sectional study used Google Street View images to create a machine vision-based model of the built environment in order to estimate the prevalence of coronary heart disease at a census-tract level.78 Using activation maps, convolutional neural networks, and linear mixed-effects models, these deep-learning algorithms predicted 63% of the coronary heart disease prevalence independent of census-tract level population demographics.
Ultimately, the research paradigm related to evaluating the impact of the built environment on the cardiovascular exposome has shown promising advancements. Machine- and deep-learning algorithms can provide valuable information about healthier living conditions, focusing on city planning initiatives that promote cardiovascular health. Longitudinal approaches are still lacking, which could differentiate the impact of short- and long-term walkability on cardiovascular disease. Additionally, the analysis of cardiovascular risk factor prevalence before and after modifications to the built environment, such as bike lanes, new parks, and other features, has been less investigated. These studies could be conducted using time-series analyses or timed pre- and post-intervention studies.
Conclusion
Increased use of computational approaches in medical data-driven analyses has advanced our understanding of the exposome, revealing a myriad of important components. Recent advancements in understanding the cardiovascular exposome have revealed significant, independent associations with the prevalence and management of cardiovascular disease. Despite these promising developments, there is still a gap in the creation of platforms that utilize poly-social and exposomal variables for risk assessment as well as in the formulation of updated health-related policies. Such a platform will improve our understanding of the details that encompass various exposome facilitators, developing fingerprints related to CVD prevention, prevalence, and treatments categorized through spatiotemporal neighborhoods. Data-driven multiomics platforms that integrate factors such as genomics, epigenomics, clinical data, social factors, environmental factors, radiologic data, and wearable technology will characterize the exposome in greater detail concerning cardiovascular health. Such an approach would enable targeted public health interventions and early intervention in vulnerable regions, thereby fostering innovation in risk reduction strategies.
Key Points
Exposome Impact: Emphasizes the comprehensive impact of environmental and socioeconomic factors on cardiovascular health.
Data Analytics Role: Highlights the essential role of advanced data analytics in understanding and managing cardiovascular disease risks.
Public Health Strategies: Supports the development of targeted public health interventions to reduce cardiovascular disease prevalence based on exposome insights.
Acknowledgements
Central illustration completed with BioRender.com. All tables & figures are original.
Contributor Information
Ashutosh Sabharwal, Email: ashu@rice.edu.
Sadeer Al-Kindi, Email: sal-kindi@houstonmethodist.org.
Funding Information
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing Interests
The authors have no competing interests to declare.
References
- 1.Motairek I, Makhlouf MHE, Rajagopalan S, Al-Kindi S. The Exposome and Cardiovascular Health. Can J Cardiol. 2023;39:1191–1203. 2023. Sep;39(9):1191-1203. doi: 10.1016/j.cjca.2023.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020. Oct 17;396(10258):1223-1249. doi: 10.1016/S0140-6736(20)30752-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landrigan PJ, Fuller R, Acosta NJR, et al. The Lancet Commission on pollution and health. Lancet. 2018. Feb 3;391(10119):462-512. doi: 10.1016/S0140-6736(17)32345-0 [DOI] [PubMed] [Google Scholar]
- 4.Basile Ibrahim B, Barcelona V, Condon EM, Crusto CA, Taylor JY. The Association Between Neighborhood Social Vulnerability and Cardiovascular Health Risk Among Black/African American Women in the InterGEN Study. Nurs Res. 2021;70(5S Suppl 1):S3-S12. doi: 10.1097/NNR.0000000000000523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bevan G, Pandey A, Griggs S, et al. Neighborhood-level Social Vulnerability and Prevalence of Cardiovascular Risk Factors and Coronary Heart Disease. Curr Probl Cardiol. 2023. Aug;48(8):101182. doi: 10.1016/j.cpcardiol.2022.101182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganatra S, Dani SS, Kumar A, et al. Impact of Social Vulnerability on Comorbid Cancer and Cardiovascular Disease Mortality in the United States. JACC CardioOncol. 2022. Sep 20;4(3):326-337. doi: 10.1016/j.jaccao.2022.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ibrahim R, Tirambulo C, Wig, R, Kim, RY, Benn BS, Low SW. Impact of the Social Vulnerability Index on Pulmonary Embolism Mortality. CHEST Pulmonary. 2023. Jun;1(1):100006. doi: 10.1016/j.chpulm.2023.100006 [DOI] [Google Scholar]
- 8.Ibrahim R, Pham HN, Sainbayar E, Ferreira JP. Impact of social vulnerability on comorbid COVID-19 and acute myocardial infarction mortality in the United States. Am Heart J Plus. 2023. Dec 26:38:100357. doi: 10.1016/j.ahjo.2023.100357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ibrahim R, Sainbayar E, Pham HN. Public health initiatives: Addressing social vulnerability in research and practice. J Investig Med. 2024. Jan;72(1):159-161. doi: 10.1177/10815589231207799 [DOI] [PubMed] [Google Scholar]
- 10.Ibrahim R, Shahid M, Srivathsan K, Sorajja D, Deshmukh A, Lee JZ. Mortality trends, disparities, and social vulnerability in cardiac arrest mortality in the young: A cross-sectional analysis. J Cardiovasc Electrophysiol. 2024. Jan;35(1):35-43. doi: 10.1111/jce.16112 [DOI] [PubMed] [Google Scholar]
- 11.Jain V, Al Rifai M, Khan SU, et al. Association Between Social Vulnerability Index and Cardiovascular Disease: A Behavioral Risk Factor Surveillance System Study. J Am Heart Assoc. 2022. Aug 2;11(15):e024414. doi: 10.1161/JAHA.121.024414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan SU, Javed Z, Lone AN, et al. Social Vulnerability and Premature Cardiovascular Mortality Among US Counties, 2014 to 2018. Circulation. 2021. Oct 19;144(16):1272-1279. doi: 10.1161/CIRCULATIONAHA.121.054516 [DOI] [PubMed] [Google Scholar]
- 13.Minhas AMK, Kobo O, Mamas MA, et al. Social Vulnerability and Cardiovascular-Related Mortality Among Older Adults in the United States. Am J Med. 2024. Feb;137(2):122-127.e1. doi: 10.1016/j.amjmed.2023.10.012 [DOI] [PubMed] [Google Scholar]
- 14.Pham R, Gorodeski EZ, Al-Kindi S. Social Vulnerability and Location of Death in Heart Failure in the United States. Curr Probl Cardiol. 2023. Jul;48(7):101689. doi: 10.1016/j.cpcardiol.2023.101689 [DOI] [PubMed] [Google Scholar]
- 15.R. Ibrahim MS, Tirambulo C.V.G., et al. Impact of Social Vulnerability and Demographics on Ischemic Heart Disease Mortality in the United States. JACC Adv. 2023. Aug 24;2(7):100577. doi: 10.1016/j.jacadv.2023.100577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khan SS, Matsushita K, Sang Y, et al. Development and Validation of the American Heart Association’s PREVENT Equations. Circulation. 2024. Feb 6;149(6):430-449. doi: 10.1161/CIRCULATIONAHA.123.067626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CDC [Internet]. PLACES. Washington, DC: US Department of Health & Human Services; c2024. PLACES: Local Data for Better Health; 2024. [cited 2024 Sep 29]. Available from: https://wwwcdcgov/places [Google Scholar]
- 18.Ibrahim R, Habib A, Terrani K, et al. County-level variation in healthcare coverage and ischemic heart disease mortality. PLoS One. 2024. Jan 26;19(1):e0292167. doi: 10.1371/journal.pone.0292167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun S, Wang W, He C. Cardiovascular Mortality Risk among Patients with Gastroenteropancreatic Neuroendocrine Neoplasms: A Registry-Based Analysis. Oxid Med Cell Longev. 2021. Jun 26:2021:9985814. doi: 10.1155/2021/9985814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Felix AS, Bower JK, Pfeiffer RM, Raman SV, Cohn DE, Sherman ME. High cardiovascular disease mortality after endometrial cancer diagnosis: Results from the Surveillance, Epidemiology, and End Results (SEER) Database. Int J Cancer. 2017. Feb 1;140(3):555-564. doi: 10.1002/ijc.30470 [DOI] [PubMed] [Google Scholar]
- 21.Liao J, Zhou Z. Long-term cardiovascular mortality risk in patients with bladder cancer: a real-world retrospective study of 129,765 cases based on the SEER database. Front Cardiovasc Med. 2023. Nov 9:10:1142417. doi: 10.3389/fcvm.2023.1142417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Antwi-Amoabeng D, Meghji Z, Thakkar S, et al. Survival Differences in Men and Women With Primary Malignant Cardiac Tumor: An Analysis Using the Surveillance, Epidemiology and End Results (SEER) Database From 1973 to 2015. J Am Heart Assoc. 2020. May 18;9(10):e014846. doi: 10.1161/JAHA.119.014846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shi T, Jiang C, Zhu C, Wu F, Fotjhadi I, Zarich S. Insurance disparity in cardiovascular mortality among non-elderly cancer survivors. Cardiooncology. 2021. Mar 20;7(1):11. doi: 10.1186/s40959-021-00098-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.CDC [Internet]. Washington, DC: US Department of Health & Human Services; c2024. Environmental Justice Index (EJI); 2022. [cited 2024 Sep 28]. Available from: https://www.atsdr.cdc.gov/placeandhealth/eji/index.html [Google Scholar]
- 25.Khadke S, Kumar A, Al-Kindi S, et al. Association of Environmental Injustice and Cardiovascular Diseases and Risk Factors in the United States. J Am Heart Assoc. 2024. Apr 2;13(7):e033428. doi: 10.1161/JAHA.123.033428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Motairek I, Rvo Salerno P, Chen Z, et al.; CARES Surveillance Group. Historical neighborhood redlining and bystander CPR disparities in out-of-hospital cardiac arrest. Resuscitation. 2024. Aug;201:110264. doi: 10.1016/j.resuscitation.2024.110264 [DOI] [PubMed] [Google Scholar]
- 27.Kostick K. From V codes to Z codes: transitioning to ICD-10 (updated). J AHIMA. 2011. Nov-Dec;82(11):60-3. [PubMed] [Google Scholar]
- 28.CMS [Internet]. Baltimore, MD: Centers for Medicare and Medicaid Services; c2024. Mathew, J HC, Khau M, Codes, Z. Utilization Among Medicare Fee-for-Service (FFS) Beneficiaries in 2017. CMS OMH Data Highlight No. 17, 2020. [cited 2024 Sep 28]. Available from: https://www.cms.gov/files/document/cms-omh-january2020-zcode-data-highlightpdf.pdf [Google Scholar]
- 29.Guo Y, Chen Z, Xu K, et al. International Classification of Diseases, Tenth Revision, Clinical Modification social determinants of health codes are poorly used in electronic health records. Medicine (Baltimore). 2020. Dec 24;99(52):e23818. doi: 10.1097/MD.0000000000023818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Monlezun DJ, Samura AT, Patel RS, Thannoun TE, Balan P. Racial and Socioeconomic Disparities in Out-Of-Hospital Cardiac Arrest Outcomes: Artificial Intelligence-Augmented Propensity Score and Geospatial Cohort Analysis of 3,952 Patients. Cardiol Res Pract. 2021. Nov 24:2021:3180987. doi: 10.1155/2021/3180987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ibrahim R, Lin L, Sainbayar E, et al. Influence of social vulnerability index on Medicare beneficiaries’ expenditures upon discharge. J Investig Med. 2024. Aug;72(6):574-578. doi: 10.1177/10815589241247791 [DOI] [PubMed] [Google Scholar]
- 32.Patra BG, Sharma MM, Vekaria V, et al. Extracting social determinants of health from electronic health records using natural language processing: a systematic review. J Am Med Inform Assoc. 2021. Nov 25;28(12):2716-2727. doi: 10.1093/jamia/ocab170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feller DJ, Bear Don’t Walk Iv OJ, Zucker J, Yin MT, Gordon P, Elhadad N. Detecting Social and Behavioral Determinants of Health with Structured and Free-Text Clinical Data. Appl Clin Inform. 2020. Jan;11(1):172-181. doi: 10.1055/s-0040-1702214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lybarger K, Ostendorf M, Yetisgen M. Annotating social determinants of health using active learning, and characterizing determinants using neural event extraction. J Biomed Inform. 2021. Jan;113:103631. doi: 10.1016/j.jbi.2020.103631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rajendran S, Topaloglu U. Extracting Smoking Status from Electronic Health Records Using NLP and Deep Learning. AMIA Jt Summits Transl Sci Proc. 2020. May 30:2020:507-516. [PMC free article] [PubMed] [Google Scholar]
- 36.Stemerman R, Arguello J, Brice J, Krishnamurthy A, Houston M, Kitzmiller R. Identification of social determinants of health using multi-label classification of electronic health record clinical notes. JAMIA Open. 2021. Feb 9;4(3):ooaa069. doi: 10.1093/jamiaopen/ooaa069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Houssein EH, Mohamed RE, Ali AA. Heart disease risk factors detection from electronic health records using advanced NLP and deep learning techniques. Sci Rep. 2023. May 3;13(1):7173. doi: 10.1038/s41598-023-34294-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reeves RM, Christensen L, Brown JR, et al. Adaptation of an NLP system to a new healthcare environment to identify social determinants of health. J Biomed Inform. 2021. Aug;120:103851. doi: 10.1016/j.jbi.2021.103851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berman AN, Biery DW, Ginder C, et al. Natural language processing for the assessment of cardiovascular disease comorbidities: The cardio-Canary comorbidity project. Clin Cardiol. 2021. Sep;44(9):1296-1304. doi: 10.1002/clc.23687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Al-Kindi S, Silversides, C. Environmental Considerations in Cardiovascular Risk Assessment and Prevention. JACC Adv. 2023. May 26;2(3):100361. doi: 10.1016/j.jacadv.2023.100361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rajagopalan S, Brook RD, Salerno P, et al. Air pollution exposure and cardiometabolic risk. Lancet Diabetes Endocrinol. 2024. Mar;12(3):196-208. doi: 10.1016/S2213-8587(23)00361-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Al-Kindi S, Brook RD, Rajagopalan S. Green cardiovascular care: a call for sustainable transformation of cardiovascular practices. Eur Heart J. 2024. Mar 7;45(10):744-747. doi: 10.1093/eurheartj/ehad844 [DOI] [PubMed] [Google Scholar]
- 43.Wass SY, Hahad O, Asad Z, et al. Environmental Exposome and Atrial Fibrillation: Emerging Evidence and Future Directions. Circ Res. 2024. Apr 12;134(8):1029-1045. doi: 10.1161/CIRCRESAHA.123.323477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sagheer U, Al-Kindi, S, Abohashem S, et al. Environmental Pollution and Cardiovascular Disease: Part 1 of 2: Air Pollution. JACC Adv. 2023. Dec 28;3(2):100805. doi: 10.1016/j.jacadv.2023.100805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cesaroni G, Forastiere F, Stafoggia M, et al. Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ. 2014. Jan 21:348:f7412. doi: 10.1136/bmj.f7412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mustafic H, Jabre P, Caussin C, et al. Main air pollutants and myocardial infarction: a systematic review and meta-analysis. JAMA. 2012. Feb 15;307(7):713-21. doi: 10.1001/jama.2012.126 [DOI] [PubMed] [Google Scholar]
- 47.Liu Y, Pan J, Fan C, et al. Short-Term Exposure to Ambient Air Pollution and Mortality From Myocardial Infarction. J Am Coll Cardiol. 2021. Jan 26;77(3):271-281. doi: 10.1016/j.jacc.2020.11.033 [DOI] [PubMed] [Google Scholar]
- 48.Crouse DL, Peters PA, van Donkelaar A, et al. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: a Canadian national-level cohort study. Environ Health Perspect. 2012. May;120(5):708-14. doi: 10.1289/ehp.1104049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bo Y, Zhu Y, Zhang X, et al. Spatiotemporal Trends of Stroke Burden Attributable to Ambient PM2.5 in 204 Countries and Territories, 1990–2019: A Global Analysis. Neurology. 2023. Aug 15;101(7):e764-e776. doi: 10.1212/WNL.0000000000207503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Deo S, Elgudin Y, Motairek I, et al. Air Pollution and Adverse Cardiovascular Events After Coronary Artery Bypass Grafting: A 10-Year Nationwide Study. JACC Adv. 2023. Dec 21;3(2):100781. doi: 10.1016/j.jacadv.2023.100781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Al-Kindi S, Rajagopalan S, Salerno P, et al. Disparities in Excess Blood Pressure Across the U.S. Associated With Air Pollution Exceeding WHO Guidelines. JACC Adv. 2024. Mar 20;3(7):100876. doi: 10.1016/j.jacadv.2024.100876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bai L, Shin S, Burnett RT, et al. Exposure to ambient air pollution and the incidence of congestive heart failure and acute myocardial infarction: A population-based study of 5.1 million Canadian adults living in Ontario. Environ Int. 2019. Nov;132:105004. doi: 10.1016/j.envint.2019.105004 [DOI] [PubMed] [Google Scholar]
- 53.Niu Y, Zhou Y, Chen R, et al. Long-term exposure to ozone and cardiovascular mortality in China: a nationwide cohort study. Lancet Planet Health. 2022. Jun;6(6):e496-e503. doi: 10.1016/S2542-5196(22)00093-6 [DOI] [PubMed] [Google Scholar]
- 54.Wang M, Sampson PD, Sheppard LE, Stein JH, Vedal S, Kaufman JD. Long-Term Exposure to Ambient Ozone and Progression of Subclinical Arterial Disease: The Multi-Ethnic Study of Atherosclerosis and Air Pollution. Environ Health Perspect. 2019. May;127(5):57001. doi: 10.1289/EHP3325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pan Z, Gong T, Liang P. Heavy Metal Exposure and Cardiovascular Disease. Circ Res. 2024. Apr 26;134(9):1160-1178. doi: 10.1161/CIRCRESAHA.123.323617 [DOI] [PubMed] [Google Scholar]
- 56.Alghasham AA, Meki AR, Ismail HA. Association of Blood Lead level with Elevated Blood Pressure in Hypertensive Patients. Int J Health Sci (Qassim). 2011. Jan;5(1):17-27. [PMC free article] [PubMed] [Google Scholar]
- 57.Vaziri ND. Mechanisms of lead-induced hypertension and cardiovascular disease. Am J Physiol Heart Circ Physiol. 2008. Aug;295(2):H454-65. doi: 10.1152/ajpheart.00158.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Abdulhai F, Motairek I, Mirzai S, et al. Quantifying lead-attributable cardiovascular disease burden in the United States. Curr Probl Cardiol. 2024. Jun;49(6):102565. doi: 10.1016/j.cpcardiol.2024.102565 [DOI] [PubMed] [Google Scholar]
- 59.Hu XF, Lowe M, Chan HM. Mercury exposure, cardiovascular disease, and mortality: A systematic review and dose-response meta-analysis. Environ Res. 2021. Feb;193:110538. doi: 10.1016/j.envres.2020.110538 [DOI] [PubMed] [Google Scholar]
- 60.Lamas GA, Navas-Acien A, Mark DB, Lee KL. Heavy Metals, Cardiovascular Disease, and the Unexpected Benefits of Chelation Therapy. J Am Coll Cardiol. 2016. May 24;67(20):2411-2418. doi: 10.1016/j.jacc.2016.02.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kuntic M, Hahad O, Al-Kindi S, et al. Pathomechanistic Synergy Between Particulate Matter and Traffic Noise-Induced Cardiovascular Damage and the Classical Risk Factor Hypertension. Antioxid Redox Signal. 2024. Jul 11. doi: 10.1089/ars.2024.0659 [DOI] [PubMed] [Google Scholar]
- 62.Hahad O, Al-Kindi S. The Prenatal and Early Life Exposome: Shaping Health Across the Lifespan. JACC Adv. 2024. Jan 5;3(2):100807. doi: 10.1016/j.jacadv.2023.100807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hu X, Wang LB, Jalaludin B, et al. Outdoor artificial light at night and incident cardiovascular disease in adults: A national cohort study across China. Sci Total Environ. 2024. Mar 25:918:170685. doi: 10.1016/j.scitotenv.2024.170685 [DOI] [PubMed] [Google Scholar]
- 64.AlShehhi A, Welsch R. Artificial intelligence for improving Nitrogen Dioxide forecasting of Abu Dhabi environment agency ground-based stations. J Big Data. 2023;10(1):92. doi: 10.1186/s40537-023-00754-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rajagopalan S, Vergara-Martel A, Zhong J, et al. The Urban Environment and Cardiometabolic Health. Circulation. 2024. Apr 16;149(16):1298-1314. doi: 10.1161/CIRCULATIONAHA.123.067461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Makram OM, Nwana N, Nicolas JC, et al. Favorable Neighborhood Walkability is Associated With Lower Burden of Cardiovascular Risk Factors Among Patients Within an Integrated Health System: The Houston Methodist Learning Health System Outpatient Registry. Curr Probl Cardiol. 2023. Jun;48(6):101642. doi: 10.1016/j.cpcardiol.2023.101642 [DOI] [PubMed] [Google Scholar]
- 67.Howell NA, Tu JV, Moineddin R, et al. Interaction between neighborhood walkability and traffic-related air pollution on hypertension and diabetes: The CANHEART cohort. Environ Int. 2019. Nov;132:104799. doi: 10.1016/j.envint.2019.04.070 [DOI] [PubMed] [Google Scholar]
- 68.Hahad O, Al-Kindi S, Lelieveld J, Munzel T, Daiber A. Supporting and implementing the beneficial parts of the exposome: The environment can be the problem, but it can also be the solution. Int J Hyg Environ Health. 2024. Jan;255:114290. doi: 10.1016/j.ijheh.2023.114290 [DOI] [PubMed] [Google Scholar]
- 69.Dzhambov AM, Markevych I, Lercher P. Greenspace seems protective of both high and low blood pressure among residents of an Alpine valley. Environ Int. 2018. Dec;121(Pt 1):443-452. doi: 10.1016/j.envint.2018.09.044 [DOI] [PubMed] [Google Scholar]
- 70.Keith RJ, Hart JL, Bhatnagar A. Greenspaces And Cardiovascular Health. Circ Res. 2024. Apr 26;134(9):1179-1196. doi: 10.1161/CIRCRESAHA.124.323583 [DOI] [PubMed] [Google Scholar]
- 71.Delgado-Lista J, Alcala-Diaz JF, Torres-Pena JD, et al. Long-term secondary prevention of cardiovascular disease with a Mediterranean diet and a low-fat diet (CORDIOPREV): a randomised controlled trial. Lancet. 2022. May 14;399(10338):1876-1885. doi: 10.1016/S0140-6736(22)00122-2 [DOI] [PubMed] [Google Scholar]
- 72.Sun Y, Liu B, Rong S, et al. Food Insecurity Is Associated With Cardiovascular and All-Cause Mortality Among Adults in the United States. J Am Heart Assoc. 2020. Oct 20;9(19):e014629. doi: 10.1161/JAHA.119.014629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Parekh T, Xue H, Al-Kindi S, Nasir K, Cheskin LJ, Cuellar AE. Food Environment Quality and Cardiovascular Disease Mortality in the United States: a County-Level Analysis from 2017 to 2019. J Gen Intern Med. 2024. Feb;39(2):176-185. doi: 10.1007/s11606-023-08335-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lloyd M, Amos ME, Milfred-Laforest S, et al. Residing in a Food Desert and Adverse Cardiovascular Events in US Veterans With Established Cardiovascular Disease. Am J Cardiol. 2023. Jun 1:196:70-76. doi: 10.1016/j.amjcard.2023.03.010 [DOI] [PubMed] [Google Scholar]
- 75.Poti JM, Braga B, Qin B. Ultra-processed Food Intake and Obesity: What Really Matters for Health-Processing or Nutrient Content? Curr Obes Rep. 2017. Dec;6(4):420-431. doi: 10.1007/s13679-017-0285-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Juul F, Vaidean G, Parekh N. Ultra-processed Foods and Cardiovascular Diseases: Potential Mechanisms of Action. Adv Nutr. 2021. Oct 1;12(5):1673-1680. doi: 10.1093/advances/nmab049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen Z, Dazard JE, Khalifa Y, et al. Deep Learning-Based Assessment of Built Environment From Satellite Images and Cardiometabolic Disease Prevalence. JAMA Cardiol. 2024. Jun 1;9(6):556-564. doi: 10.1001/jamacardio.2024.0749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen Z, Dazard JE, Khalifa Y, Motairek I, Al-Kindi S, Rajagopalan S. Artificial intelligence-based assessment of built environment from Google Street View and coronary artery disease prevalence. Eur Heart J. 2024. May 7;45(17):1540-1549. doi: 10.1093/eurheartj/ehae158 [DOI] [PMC free article] [PubMed] [Google Scholar]


