Abstract
The use of medicinal plants in the management of microbial infections is significant to the health of the indigenous people in many Angolan communities. The present study provides a comprehensive overview of medicinal plants used for the management of microbial infections in Angola. Relevant information was extracted from research articles published and associated with the use of medicinal plants in the management of microbial infections in Angola (from January 1976 to November 2023). Data or information were gathered from the literature sourced from Wiley Online, SciFinder, Google Scholar, Web of Science, Scopus, ScienceDirect, BMC, Elsevier, SpringerLink, PubMed, books, journals and published M.Sc. and Ph.D. thesis. A total of 27 plant species, representing 19 families, were recorded in this study. Hypericaceae (11%), Lamiaceae (11%), Malvaceae (11%), Phyllanthaceae (11%), Fabaceae (16%) and Rubiaceae (16%) were the most predominant families. The leaves are the most used parts (96%), followed by bark (74%) and root (70%). The data revealed that medicinal plants continue to play significant roles in the management of microbial infections in Angola. In order to explore the benefits of the therapeutic potential of indigenous medicinal plants for diseases related to infections; further scientific research studies are important to produce data on their effectiveness using appropriate test models. This approach might assist with the continuing drive regarding the integration of Angolan traditional medicine within mainstream healthcare systems.
Keywords: Angolan medicinal plants, antimicrobial activity, antibacterial activity, botanical description, distribution, taxonomy, ethnobotany, phytochemistry, pharmacology
1. Introduction
Infectious diseases remain a crucial problem in global public health and are one of the leading causes of death worldwide [1]. According to the literature reports, these ailments are responsible for 17 million deaths per year worldwide [2,3]. Treatment of microbial infections is becoming a challenge due to the emergence of bacterial pathogens resistant to all antimicrobial drugs [4]. Therefore, there is a need to discover new alternative antimicrobial constituents with improved activity. Traditional herbal medicine has played an essential role as antibiotics in various developing countries [5]. Medicinal plants have long been considered a natural source of novel remedies of high value to mankind [6]. Natural medicinal plants are proven to have beneficial effects and have been used globally for healing various diseases [7]. Medicinal plants are a rich source of phytochemicals and have been used for their antiviral, antifungal, and antibacterial activities for many years [8]. Plants that exhibited the presence of antibacterial components provided data, which led to the development of novel antimicrobial medications [9]. About 80% of people worldwide depend on traditional plants or herbs for their primary healthcare [10]. Fortunately, some plant products, either in the form of raw materials or isolated compounds, have been tested for possible antimicrobial and antibacterial therapy in Africa, but the number of plants and isolated bioactive compounds with potential antimicrobial properties is very limited, and their antimicrobial and antibacterial activities have not yet been scientifically validated [11]. The present study is a review of medicinal plants used to treat microbial and bacterial infections in Angola. The information presented in this review may be used as a guide to formulate new and effective medicinal drugs used to treat microbial infections.
1.1. Traditional Medicine in Angola
Angola is the largest country in Southern Africa, with an estimated population of over 37.2 million, according to the Angola Population (2024)—Worldometer [12]. The Republic of Angola (Figure 1) covers an area of 1,246,700 km2 (481,400 square miles) in Southwest Central Africa. Its western boundary is 1650 km along the Atlantic Ocean and it is bordered by Namibia in the south, the Democratic Republic of Congo in the north and northeast, and Zambia in the east [13]. Furthermore, Angola is the second richest country with respect to endemic plants in continental Africa [14]. The total number of vascular plants in Angola is approximately 6850 species, of which 14.8% are endemic and frequently used in traditional medicine [15,16]. The rich flora of Angola suggests enormous potential for the discovery of new secondary plant metabolites with therapeutic value. There are only a few reports and studies documenting the traditional use of plants in different regions of Angola [17,18,19,20,21,22]. Therefore, there is a need to conduct ethnobotanical, ethnomedicinal and ethnopharmacological studies, document the diversity of medicinal plants and related ethnomedicinal knowledge of traditional healers or herbalists in Angola.
Figure 1.

Angola’s geographic location in Africa (provided by Country Reports Org 2005 (https://www.countryreports.org/country/angola.htm), accessed on 4 March 2024).
A wealth of Angolan ethnic knowledge has been transferred from generation to generation [23,24]. Many Angolans rely on plant-based medicinal treatment for primary healthcare [23,24,25]. This is because Angola’s healthcare system is poor, compared to other sub-Saharan countries in Africa. The lack of essential public health facilities, especially in rural areas, is a major challenge resulting in the importance of traditional practitioners and herbal medicines. In Angola, as in several other countries, the use of plants is an important cultural phenomenon, with some ailments recognised as specifically requiring traditional medicine [22]. Different plant parts are frequently used to treat, manage and control various diseases or sicknesses, such as acute respiratory, cholera, diarrhoea, malaria, tetanus and yellow fever, which affect their patients [22,26]. This is because most medicinal plants are inexpensive, accessible and easy to prepare [27].
1.2. The Burden of Antimicrobial Resistance
Antimicrobial resistance (AMR) is a major global health threat and directly impacts economic growth worldwide [28]. However, low- and middle-income countries, especially in Africa, bear the biggest burden of the negative outcomes of antimicrobial resistance [29]. Antimicrobial resistance occurs when microorganisms (bacteria, viruses, fungi and parasites) grow or develop in the presence of drugs invented to prevent or kill them [30]. This results in therapeutic failure, increased disease spread, severe sickness, disability, and high mortality rates, which negatively influence the global management and control of infectious diseases [31]. Infections caused by antimicrobial-resistant microorganisms are reported to result in approximately 700,000 deaths worldwide annually [31]. The higher burden on low- and middle-income countries, including Africa, is attributed to poor water sanitation, less access to quality antibiotics, insufficient water supply, less access to the best public health facilities, and travelling [32,33,34]. According to estimates, 5.00 million people died in 2019 from antimicrobial-resistant-related causes, of which 1.3 million deaths were directly associated with bacterial AMR globally [31]. In the African continent, over 1.05 million deaths were associated with antimicrobial resistance, and 250,000 deaths were due to antimicrobial resistance [35]. The number of deaths associated with antimicrobial resistance in Africa is greater than those caused by HIV/AIDS (639,554), malaria (594,348), and tuberculosis (424,000), marking a pivotal shift in the health problems facing the African continent [35]. Four major pathogenic microorganisms (Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus, and Streptococcus pneumoniae) contributed to more than 100,000 deaths in the WHO African region [35]. Furthermore, in Angola, 5300 deaths were due to AMR and 22,700 deaths were associated with antimicrobial resistance [36]. The number of AMR deaths in Angola is greater than deaths from malaria, neglected tropical diseases, neoplasms, enteric infections, sexually transmitted infections, HIV/AIDS, and neonatal and maternal disorders [36]. The five leading pathogens for deaths associated with AMR in Angola were Group B Streptococcus (1600), Staphylococcus aureus (2200), Escherichia coli (3100), Klebsiella pneumoniae (3800), and Streptococcus pneumoniae (4800) [36]. More than a few antibiotics such as Carbapenem (such as imipenem and meropenem), Fluoroquinolone (such as ciprofloxacin), Methicillin, Penicillins (such as ampicillin), Vancomycin, and third-generation cephalosporin (such as ceftriaxone and cefotaxime) widely used globally for treating Enterobacteriaceae, Escherichia coli, Group B Streptococcus, Pseudomonas aeruginosa, Staphylococcus aureus, Klebsiella pneumoniae and Streptococcus pneumoniae strains, respectively, have encountered problems and challenges in their efficacy due to antimicrobial resistance [37,38]. According to the World Health Organization [39], drug-resistant diseases could cause 10 million deaths each year by 2050 and damage the global economy significantly [39]. Furthermore, WHO predicts that antimicrobial resistance will cost an additional USD 1 trillion in healthcare by 2050 if sufficient measures are not fulfilled [40]. Unfortunately, the burden is estimated to be higher in Sub-Saharan Africa, and this calls for necessary measures and interventions to limit the threat [28,40]. Thus, future strategies to prevent AMR must focus on fostering international collaboration with high-income countries to build better health facilities and laboratories in countries that are faced with significant infrastructural challenges; train more laboratory workers or scientists and offer them a reasonable remuneration; educate the public about improving the practice of infection prevention and control (IPC) measures at food handling industries or establishments, home and healthcare facilities; increase the healthcare workers; and increase the public’s knowledge of antibiotics and antimicrobial resistance [41].
2. Results and Discussion
2.1. Medicinal Plants Used for Microbial Infections in Angola
This review highlights 27 plant species representing 19 different plant families that are widespread in all areas of Angola. The leaves are the most used parts (96%), followed by bark (74%) and root (70%). The predominant families are Hypericaceae (11%), Lamiaceae (11%), Malvaceae (11%), Phyllanthaceae (11%), Fabaceae (16%) and Rubiaceae (16%). Information or data about the medicinal plants presented include taxonomic names, family, plant part(s) used and traditional uses (Table 1).
2.1.1. Acanthus montanus (Nees) T. Anderson
Acanthus monthanus is a shrub widely distributed in Angola, Chad, Zambia, Sierra Leone and Benin [42]. It belongs to the Acanthaceae family which consists of approximately ~2500 species in ~250 genera [43]. A. monthanus is used to treat many diseases like cystitis, pains, endometritis, urogenital infections, aches, leucorrhoea, urethral pain, urinary disease and furuncle [44]. Numerous pharmacological properties of this plant including antipyretic, spasmolytic, anti-inflammatory, antimicrobial, and analgesic have been well-documented [45,46,47]. Okoli et al. (2008) showed that the aqueous root extract of Acanthus montanus had antimicrobial activities at concentrations of 50 and 100 mg/mL, with zone of inhibition diameters of 10.0 ± 0.32 and 10.0 ± 0.27; and 19.3 ± 0.18 and 15.0 ± 0.32 against Staphylococcus aureus and Pseudomonas aeruginosa strains, respectively [48]. In addition, Okoli et al. (2008) indicated that the antimicrobial efficacy of the aqueous root extracts of Acanthus montanus may be due to the presence of alkaloids, carbohydrates, saponins, glycosides, and terpenoids [48]. Medicinal plants that have alkaloids and glycosides are claimed to exhibit antimicrobial effects [49,50].
2.1.2. Abelmoschus esculentus (L.) Moench
Abelmoschus esculentus (“Lady’s Finger”), also known as Okra worldwide, belongs to the family Malvaceae, estimated to contain ~4224 species in ~244 genera [51]. It has various reported biological properties like antidiabetic, antimicrobial, antioxidant, and anti-inflammatory activity [52,53]. These properties are due to the carotene, chlorophyll and phenolic compounds found in A. esculentus [53]. A. esculentus can be used to treat depression, ulcers, sore throats, pulmonary inflammations, and gastrointestinal irritations [54]. Islam (2019) showed that essential oils: cyclohexanol, citral, β-sitosterol, 3β-galactoside, p-tolualdehyde and α-terpenylacetate isolated from the seeds and pods of Abelmoschus esculentus have antibacterial activity [55]. In another study, fresh water and lyophilised extracts of the A. esculentus (Okra) pods were effective against Mycobacterium sp., Staphylococcus aureus, Xanthobacter Py2, Escherichia coli, Rhodococcus opacus, Rhodococcus erythropolis, and Mycolicibacterium aurum at a concentration of 97.7 mg/mL. The identified saturated fatty acids (palmitic and stearic acids) may be responsible for the antibacterial activity of the fresh water and lyophilised extracts [56].
2.1.3. Aframomum alboviolaceum (Ridl.) K.Schum.
Aframomum alboviolaceum is part of the family Zingiberaceae, comprised of ~52 genera and more than 1300 species; extensively distributed in Sierra Leone to Sudan, south to Angola, Malawi, Zambia, and Mozambique [57]. All plant parts are used to cure headache, cough, fever, amoebic dysentery, haemorrhoids, gastritis, myoma, pruritis, hypertension, filarial, malaria, pruritus, and gastritis [58,59,60]. Ethnopharmacological studies have shown antihelminthic, antimalarial, antiparasitic, antioxidant, antimicrobial, anti-sickling, and anticancer properties from Afromomum alboviolaceum [58,59,60]. Phytochemical evaluation of A. alboviolaceum leaves using thin layer chromatography revealed various metabolites such as iridoids, anthocyanins, tannins, coumarins, phenolic acids, flavonoids, and anthraquinones in this species [61]. It has also been shown that A. alboviolaceum contains alkaloids, anthocyanines, and triterpenes [62]. Olagoke and Amusat (2019) showed that volatile compounds present in the leaves of A. alboviolaceum have antimicrobial potential against Staphylococcus aureus, Pseudomonas aeruginosa, Escherichia coli, Candida albicans, Bacillus subtilis, and Aspergillus niger at 100%, 50% and 25%, as well as moderate inhibition at 12.5 and 6.25% [63].
2.1.4. Alchornea cordifolia (Schumach. & Thonn.) Müll.Arg.
Alchornea cordifolia is a small tree in the Euphorbiaceae family, containing ~6745 species in ~218 genera [64,65]. It is distributed throughout tropical Africa [64,66]. The plant is used in Africa to treat venereal diseases, malaria, diarrhoea, wounds, cuts, sores, coughs, colds, eye problems, pigmentation problems, gastrointestinal, headaches, rheumatic pains, urinary disorders, as well as inflammatory disorders, and fungal, parasitic, bacterial, and parasitic disorders [67,68,69,70]. Some reports on the pharmacological activities of A. cordifolia have confirmed anti-inflammatory, antiviral, anti-diarrhoeal, hepaprotective, and antidiabetic activity [71,72,73,74,75]. Furthermore, several antimicrobial tests of the plant showed its efficacy against a wide variety of microorganisms such as skin, gastrointestinal, urinary tract and respiratory pathogens [65,76,77,78], therefore supporting the medicinal use of the plant species for the management of such diseases. The biological activities of Alchornea cordifolia were due to terpenoids, flavonoids, tannins, steroid glycosides, phenolic acids, saponins, imidazopyrimidine, alkaloids, and fatty acids, carbohydrates [79]. Essien et al. (2015) showed that volatile compounds such as 28.0% benzaldehyde, 25.3% methyl salicylate, 21.4% citronellol, 15.5% β-caryophyllene, 7.4% α-phellandrene, 5.7% terpinolene, 5.5% 1,8-cineole, and 5.3% (E,E)-α-farnesene in the essential oil of A. cordifolia fruits contributed to the antifungal potential against Staphylococcus aureus, Aspergillus niger and Bacillus cereus, with MIC values of 78 μg/mL, 156 μg/mL and 156 μg/mL, respectively [64].
2.1.5. Aloe buettneri A. Berger
Aloe buettneri (Asphodelaceae, which includes about ~900 known species and ~40 genera) is a flowering succulent plant species that has been traditionally utilised in West Africa to treat wounds, vitiligo, malaria, rheumatism, insect bites, burns and worm sores [80]. This plant has a wide variety of chemical constituents, including polyphenols, tannins, flavonoids, sterols, terpenoids, saponins, alkaloids and carbohydrates [81]. However, the bioactive compounds and their bioactivities are not well known or described. The extracts of A. buettneri have a wide variety of pharmacological activities, such as antioxidant, gastric antisecretory, anti-ulcer, and anti-inflammatory [82,83]. Kombate et al. (2022) found that the ethanol–water mixture (5:5. v/v) leaf extract had antimicrobial activity, with inhibition zones of 18.20 ± 0.10 and 14.24 ± 0.17 mm against Cutibacterium acnes and Pseudomonas aeruginosa at a concentration of 250 mg/mL [81]. Kombate et al. (2022) also indicated that A. buettneri gave the best activity with 31.25 mg/mL for minimum microbicidal concentrations and 15.625 mg/mL for MICs (minimum inhibitory concentrations) against Klebsiella pneumoniae [81]. Their phytochemical screening results showed the presence of saponosides, triterpenes, carbohydrates, tannins, flavonoids, polyphenols, and alkaloids in the ethanol–water mixture (5:5. v/v) leaf extract of A. buettneri, which explained the antimicrobial activities [81]. A few literature studies have shown that saponins, tannins, flavonoids, triterpenoids and polyphenolic compounds are also known to have antimicrobial activities [84,85,86]. Therefore, the secondary metabolites found in the ethanol–water mixture (5:5. v/v) leaf extract of A. buettneri may have acted on their own or in synergy to inhibit the tested pathogenic microorganisms.
2.1.6. Annona stenophylla Engl. & Diels
Annona stenophylla belongs to the Annonaceae family, which includes about ~108 genera and ~2400 known species. Many people worldwide use A. stenophylla to treat coughs, wounds, helminthiasis, cancer, dysentery, diarrhoea, headache, asthma, fever, malaria, dermatitis, mental disorders, diabetes, and peptic ulcers [87,88,89]. Annona species are characterised by biological activities such as anti-inflammatory, hypoglycaemic, antimicrobial, anticholinesterase, analgesic, antioxidant, antiparasitic, anticonvulsant, antiplatelet, hepato-protective, anxiolytic, cytotoxicity, and antiproliferative; these activities are usually attributed to the presence of quinones, sesquiterpene lactones, sterols, essential oils, acetogenins, alkaloids, and terpenes [88,90,91]. Munodawafa (2008) and Munodawafa et al. (2013) assessed the antibacterial effects of methanol root and leaf extracts of A. stenophylla against Pseudomonas aeruginosa, Escherichia coli, and Staphylococcus aureus [92]. They showed that the root extract was active against Pseudomonas aeruginosa with an inhibition zone ranging from 2.8 to 3.0 mm, whereas the leaf extract was active against Staphylococcus aureus with an inhibition zone ranging from 1.0 to 1.5 mm. Furthermore, Munodawafa (2008) and Munodawafa et al. (2013) determined the antifungal effects of methanol root and leaf of A. stenophylla against Aspergillus niger and Candida albicans [92]. Their results showed that the root extract of A. stenophylla showed activities against pathogenic microorganisms with inhibition zones ranging from 1.5 to 3.8 mm. Plant secondary metabolites: coumarins, alkaloids, cardiac glycosides, anthraquinone derivatives, tannins, saponins, and flavonoids identified in the methanol root and leaf extracts of A. stenophylla by phytochemical screening could have contributed separately or in combination to the potent antibacterial and antifungal activities of this plant [92].
2.1.7. Bridelia ferruginea Benth.
Bridelia ferruginea (Phyllanthaceae) grows in the rainforests or savannahs of Africa, Australia, and Southern Asia [93]. Phyllanthaceae comprises about ~2000 species grouped into ~60 genera. The roots, fruits, leaves and bark of the “woody shrub” are commonly prepared traditionally for managing dysentery, arthritis, cough, rashes, constipation, epilepsy, diarrhoea, diuretic, chronic diabetes, asthma, gout, intestinal disorders, thrush, dysentery, gastralgias, rheumatisms, sexually transmitted diseases, contusion, oral infections, bladder disorders, skin diseases, and anaemia [94]. Biological studies on several B. ferruginea extracts support its use as an antipyretic, anthelmintic, antityphoid, antioxidant, analgesic, antimicrobial, anti-inflammatory, antidiabetic, and antiplasmodial properties in different parts of Africa [95,96,97,98,99,100,101,102]. Different chemical compounds reported to be found in B. ferruginea extracts include tannins, triterpenes, saponins, alkaloids, flavonoids, cardiac glycosides, phenolics, and phytosterols [103]. A recent study by Afolayan et al. (2019) showed that β-sitosterol glucoside, rutin, quercitrin, myricitrin, isoquercetin, isomericitrin, myricetin, kaempferide-3-O-β-D-glucoside, corilagin, vomifoliol, lutein, 6β-hydroxy-(20R)-24-ethylcholest-4,22-dien-3-one, 6β-hydroxy-(20R)-24-ethylcholest-4-en-3-one, oleic acid, stearic acid and palmitic acid were isolated and identified from the methanolic leaf extracts of B. ferruginea [104]. Myricitrin was the only compound that showed antibacterial activities against Escherichia coli with an IC50 value of 1.123 μM. [104]. Irobi et al. (1994) showed that phenols and tannins in B. ferruginea might be responsible for the antimicrobial activities against Candida albicans, Escherichia coli, Proteus vulgaris, Klebsiella pneumoniae, Staphylococcus epidermidis, Staphylococcus aureus, Proteus mirabilis, Streptococcus lactis and Streptococcus pyogenes at a concentration of 5 mg/mL [105].
2.1.8. Canarium schweinfurthii Engl.
Canarium schweinfurthii (Burseraceae (~19 genera and about ~540 species) is a species of a large tree found in tropical Africa that can be used to treat roundworm infections, skin affections, dysentery, eczema, diarrhoea, dysentery, haemorrhoids, venereal diseases, hypertension, malaria, fever, gonorrhoea, chest pains, stomach complaints, pulmonary affections, ulcers, leprosy, coughs and wounds [106,107,108,109]. The plant has numerous critical biological activities, such as antidiabetic, antibacterial, antifungal, analgesic, antiparasitic, anti-inflammatory and antioxidant [110]. This plant has been reported to have several active metabolites such as sterols, fatty acids, saponins, triterpenes, alkaloids, flavonoids, tannins, anthraquinones, polyphenols, and coumarins [111,112,113]. According to Dzotam et al. (2016), C. schweinfurthii extracts had antimicrobial activities against Escherichia coli, Enterobacter aerogenes, Klebsiella pneumoniae, Pseudomona aeruginosa and Providencia stuartii, with minimum inhibitory concentration values that were between 64 to 1024 μg/mL [114]. Qualitative phytochemical analysis showed that the methanol C. schweinfurthii extracts contained saponins, sterols, triterpenes, tannins, anthraquinones, flavonoids, polyphenols and alkaloids [114]. Therefore, the antimicrobial effects of this plant could be due to the differences in their chemical composition as well as in the mode of action of their bioactive compounds. Nagawa et al. (2015) revealed that the main compounds found in essential oil of Canarium schweinfurthii resin were mostly α-thujene, γ-terpinene, β-pinene, p-cymene, β-phellandrene, α-phellandrene, α-pinene, sabinene, nerolidol octyl acetate, n-octanol, limonene and α-terpineol [115]. However, these compounds could not be tested for their biological activities due to small amounts of the compounds after qualitative chemical analysis. Several research studies reported that α-thujene, γ-terpinene, β-pinene, p-cymene, β-phellandrene, α-phellandrene, α-pinene, sabinene, nerolidol octyl acetate, n-octanol, limonene and α-terpineol were responsible for the antimicrobial activities of several essential oils found in medicinal plants [116,117,118,119,120,121,122]. Consequently, the strong antimicrobial activity of Canarium schweinfurthii might be due to the presence of these main compounds found in the essential oils of this plant.
2.1.9. Chromolaena odorata (L.) R.M.King & H.Rob.
Chromolaena odorata (Asteraceae) is mainly found in tropical and subtropical areas of Texas, Florida, Mexico, Australia, and Asia. Asteraceae is a large family of flowering plants that consists of over ~32,000 known species in over ~1900 genera [123,124]. Various therapeutic and medicinal properties of C. odorata, which include antioxidant, anthelmintic, antimicrobial, antimalarial, analgesic, antispasmodic, anti-inflammatory, and antipyretic, have been reported [125,126,127]. It is widely used for malaria, coughs, colds, toothache, stomach problems, diarrhoea, stomach ulcers, wounds, dysentery, skin infections, and bacterial and fungal infections. This plant has many components like saponins, tannins, coumarins, steroids, terpenoids, cardiac glycosides, and flavonoids [128,129]. Atindehou et al. (2013) demonstrate that the cyclohexane, dichloromethane, ethyl acetate and butanol leaf extracts of C. odorata had antibacterial activity ranging from 0.156 to 1.25 mg/mL against Vibrio cholerae, Shigella sonnei, Salmonella enterica, and Klebsiellaoxytoca microorganisms [130]. The best antibacterial activity was obtained against V. cholerae strain with MIC values of 0.156 mg/mL and 0.312 mg/mL for the dichloromethane and butanol extracts, respectively [130]. Atindehou et al. (2013) also characterised two flavonoids: sinensetin (3’,4’,5,6,7-pentamethoxyflavone) and scutellareintetramethyl ether (4’,5,6,7-tetramethoxyflavone) using bioassay-guided isolation by chemical and pharmacological approaches. However, the antibacterial activity of these compounds could not be tested due to insufficient amounts of material after chemical analysis [130]. In addition, other research studies have shown that these two flavonoids have antibacterial properties [131,132]. Kil et al. (2009) reported that the antimicrobial properties of several medicinal plant extracts are due to the high quality of the flavonoids [133]. Flavonoids have a very large and diverse antibacterial activity, and they inhibit numerous microorganisms with different intensities depending on the pathogenic microorganism and the environment in which it is found; flavonoids are also able to prevent the growth of various microorganisms [134,135,136]. Therefore, the two flavonoids isolated from C. odorata could be used as markers of the antibacterial activities of this plant species.
2.1.10. Clerodendrum splendens G.Don
Clerodendrum splendens (Lamiaceae (~7200 species in ~236 genera) is found in tropical Western Africa [137]. It is a climbing shrub that exhibits anti-inflammatory, antioxidant, antibacterial, and antifungal activities [138,139], and this has provided a scientific basis for its folkloric use in the treatment of numerous infectious conditions such as bruises, vaginal thrush, various skin infections and wound healing [138]. Preliminary phytochemical analysis of extracts showed the presence of unsaturated sterols, carbohydrates, glycosides, alkaloids, triterpenoids, tannins and flavonoids [140]. The methanol aerial extracts of C. splendens exhibited very good antifungal and antibacterial activities against the pathogenic bacteria tested with the minimum inhibitory concentrations (MIC) ranging from 64 to 256 μg/mL against Candida albicans, Klebsiella pneumoniae, Proteus mirabilis, Staphylococcus aureus, Streptococcus faecalis, Bacillus subtilis, Escherichia coli, and Pseudomonas aeruginosa using the micro-well dilution method [138]. Gbedema et al. (2010) reported that the methanol aerial extracts of C. splendens contained reducing sugars, phytosterols, tannins, terpenoids, alkaloids and flavonoids, which could be responsible for the high antifungal and antibacterial activities [138].
2.1.11. Combretum racemosum P.Beauv.
Combretum racemosum belongs to the Combretaceae family, which consists of approximately ~600 species in ~20 genera [141]. The straggling shrub is widely spread across Africa to Senegal, Sudan, Nigeria, Kenya, Angola and the Democratic Republic of the Congo (ex-Zaïre) [141]. C. racemosum has been used for many years in African traditional therapeutic practices for the treatment of wounds, haemorrhoids, roundworms, gastro-intestinal affections, coughs, toothache, tuberculosis, genito-urinary, male sterility and bleeding during pregnancy [142,143,144,145]. Moreover, the antiulcer, vasorelaxant, anti-inflammatory, antimicrobial, antitrypanosomal, and antitrypanosomal effects of the C. racemosum extracts have been proven in modern biological studies [146,147,148,149]. Gossan et al. (2016) isolated betulinic acid, 28-O-β-D-glucopyranosyl-2α,3β,21β,23-tetrahydroxyolean-18-en-28-oate, 11 (3-O-β-acetyl-ursolic acid), terminolic acid, quadranoside, and arjungenin from the ethyl acetate extracts of C. racemosum. These metabolites showed moderate antibacterial activity against Enterococcus faecalis, Escherichia coli and Staphylococcus aureus, with minimum inhibitory concentrations that ranged from 64 to 256 μg/mL [141]. Therefore, these compounds were responsible for the antibacterial activities of ethyl acetate extracts of this plant species.
2.1.12. Dioscorea praehensilis Benth.
Dioscorea praehensilis (Dioscoreaceae family with about ~715 species in ~9 genera) is a species of yam in the genus Dioscorea growing in tropical and subtropical areas of West Africa [150]. D. praehensilis is used by different ethnic groups and geographical areas to treat health problems, such as diabetes, stomach pains, rheumatism, haemorrhoids, coughs, skin infections, and diarrhoea [151,152]. Modern research has proven that Dioscorea praehensilis has a variety of biological activities, such as antidiabetic, anti-tumour, anti-inflammatory, and antibacterial activities [150]. The biological activities of D. praehensilis were mostly due to the presence of tannins, terpenoids, steroids, saponins, flavonoids, alkaloids, and anthocyanins [153]. Furthermore, Sautour et al. (2004) used mplc (medium-pressure liquid chromatography) column chromatography on silica gel to isolate 26-O-β-D-glucopyranosyl-22-methoxy-3β,26-di-hydroxy-25(R)-furost-5-en-3-O-α-L-rhamnopyranosyl-(1→4)-α-L-rhamnopyranosyl-(1→4)-[α-L-rhamnopyranosyl-(1→2)]-β-D-glucopyranoside; dioscin; and diosgenin 3-O-α-L-rhamnopyranosyl-(1→4)-α-L-rhamnopyranosyl-(1→4)-[α-L-rhamnopyranosyl-(1→2)]-β-D-glucopyranoside from the rhizomes of D. praehensilis. Dioscin showed antifungal activity against Candida tropicalis (MIC = 25.0 µg/mL), Candida glabrata (MIC = 12.5 µg/mL) and Candida albicans (MIC = 12.5 µg/mL) using the broth dilution test [150]. Diosgenin 3-O-α-L-rhamnopyranosyl-(1→4)-α-L-rhamnopyranosyl-(1→4)-[α-L-rhamnopyranosyl-(1→2)]-β-D-glucopyranoside had low activity; whereas 26-O-β-D-glucopyranosyl-22-methoxy-3β,26-di-hydroxy-25(R)-furost-5-en-3-O-α-L-rhamnopyranosyl-(1→4)-α-L-rhamnopyranosyl-(1→4)-[α-L-rhamnopyranosyl-(1→2)]-β-D-glucopyranoside was not active [150].
2.1.13. Erythrina abyssinica Lam.
Erythrina abyssinica belongs to the plant family of the Fabaceae, with about 765 genera and nearly 20,000 known species ~765 genera and nearly ~20,000 known species [154,155,156]. The deciduous leguminous tree is found in Eastern DRC, Southern Africa and East Africa [157,158,159]. E. abyssinica is traditionally used to treat diseases such as malaria, tuberculosis, cancer, diabetes, leprosy, syphilis, back pain, yellow fever, anaemia, inflammatory diseases, venereal diseases, sexually transmitted diseases, skin infections, diarrhoea, epilepsy, urinary tract infections, pregnancy-related conditions, vomiting, soft tissue, hepatitis, central nervous system (CNS)-related disorders, helminthiasis, pneumonia, infertility, bacterial and fungal infections [25,160,161,162,163]. Preliminary phytochemical testing of several solvent extracts of E. abyssinica indicated the existence of flavonoids, phenols, terpenoids, chalcones, aromatic hydrocarbons, alkaloids, saponins, quinones and tannins as the major medicinal secondary metabolites [164,165]. Also, chemical compounds in this species possess antifungal, antioxidant, antimycobacterial, anti-HIV, anti-inflammatory, anticancer, antiviral, antihelmintic, antianemic, antibacterial, antiplasmodial, antiobesity, antidiabetic, antipyretic, and hepatoprotective bioactivities [166]. Antimicrobial activities of E. abyssinica crude extracts have been extensively assessed using the microbroth dilution assay against Staphylococcus aureus ATCC 25922 [167]. The existence of antimicrobial activities of E. abyssinica was attributed to 2′-methoxy-nor-glycyrrisoflavanone, 2′,3′,4′,7-tetrahydroxy-5′-prenylflavanone and 1,5,4′-trihydroxy-5′-prenylchalcone isolated from the plant. These pure compounds from E. abyssinica dichloromethane stem bark extracts were found active against Staphylococcus aureus (ATCC 25922) with a zone of inhibition of 15 mm at a concentration of 100 µg/mL [167]. Chitopoa et al. (2019) showed that the hexane, ethyl acetate, dichloromethane, ethanol, and methanol crude extracts of this plant had strong antifungal and antibacterial activities with MICs values of 3 and 10,000 μg/mL against different bacteria. Antimicrobial activity was noticed in most crude extracts, with the ethyl acetate crude extract showing the highest inhibition zone of 25 mm against Candida albicans, and the hexane and dichloromethane crude extracts were the most potent with minimum inhibitory concentrations of 62.5 μg/mL [168]. However, the hexane extract showed the highest inhibition zone of 23 mm against Staphylococcus aureus, while the dichloromethane was found to be the most active with a minimum inhibitory concentration of 15.6 μg/mL against Candida albicans [168]. Variation in the degree of activity in the E. abyssinica crude extracts might be due to the high quantity of terpenoids, which are known to possess antimicrobial, antifungal, and antibacterial activities [169,170,171].
2.1.14. Gardenia ternifolia Schumach. & Thonn.
Gardenia ternifolia is a tree found in Angola, Senegal, Uganda, Ethiopia, Kenya, Botswana, Namibia, and Mozambique. It belongs to the Rubiaceae family, which consists of ~13,500 species in ~620 genera, and is one of the largest of the angiosperm family [172]. G. ternifolia is used to manage diabetes, malaria, sexually transmitted diseases, ascites, hepatitis, wounds, tooth decay, onchocerciasis, hypertension, haemorrhoids, leprosy, blood pressure, female infertility, skin diseases, diarrhoea, liver, cancer, sickle cell disease, rheumatism and yellow fever [25,173,174,175,176,177,178,179,180,181,182,183]. All parts of G. ternifolia are known to have antimicrobial, antitheilerial, antibiotic, antipain, anti-inflammatory, antisickling, antimalarial, antidiabetic, antileishmanial, larvicidal, antioxidant, hepatoprotective and cytotoxicity properties [184]. These pharmacological properties of G. ternifolia are attributed to saponins, steroids, alkaloids, terpenoids and polyphenols (tannins, coumarins and flavonoids) identified in different parts of G. ternifolia [174]. Ternifoliaoside A, β-sitosterol, β-stigmasterol-glucoside, 3β,23,24–trihydroxyurs-12-en-28-oic acid, 3β,19 α,23,24–tetrahydroxyurs-12-en-28-oic acid, lippianoside B, silphioside F, copteroside B and 24(24′)[Z]-dehydroamarasterone B were isolated from the roots of Gardenia ternifolia [185]. Ternifoliaoside A showed a very sensitive antibacterial effect on Escherichia coli (15.40 ± 2 mm) and Salmonnela typhi (20.1 ± 2 mm) at a concentration of 25 mg/mL using the Muller–Hinton agar diffusion method [185]. No effect was shown on Escherichia coli, Vibrion cholorae, Salmonella typhi and Staphilococus aureaus with compounds β-sitosterol and 24(24′)[Z]-dehydroamarasterone B at 25 mg/mL [185]. Furthermore, 3β,19 α,23,24–tetrahydroxyurs-12-en-28-oic acid exhibited the effect on Staphylococcus aureus (12.2 ± 2 mm) and Pseudomonas aeruginosa (15.6 ± 2 mm) at a concentration of 25 mg/mL [185].
2.1.15. Gloriosa superba L.
Gloriosa superba is a flowering plant in the Colchicaceae family that includes ~285 species in ~15 genera. G. superba grows naturally throughout the sub-Saharan countries in the African continent to South Africa as well as in Madagascar [186,187]. It is also distributed in South Central China, Sri Lanka, Indonesia, and Southeast Asian countries. The alkaloid-rich plant has long been used in the treatment of wounds, gout, infertility, snakebite, cholera, ulcers, colic, arthritis, kidney problems, sprains, typhus, itching, smallpox, cancer, leprosy, sexually transmitted diseases, bruises, haemorrhoids, skin problems, nocturnal emission [188,189,190,191,192]. Ethnopharmacological studies have shown anthelmintic, antimicrobial, antibacterial, and antioxidant properties from Gloriosa superba [192]. Mustefa et al. (2024) showed that G. superba has antibacterial properties. Their results showed that 3-hydroxy-5-methoxy-benzoic acid, 3-hydroxymethyl phenol and desmosterol isolated from the chloroform and methanol extracts using silica gel column chromatography had potent in vitro antibacterial against Klebsiella pneumoniae, with inhibition zone values of (11.33 ± 1.15, 11.33 ± 1.53, and 12.33 ± 0.58, mm, respectively), at 1000 μg/mL. In addition, 3-hydroxy-5-methoxy-benzoic acid and desmosterol showed promising zone of inhibition against Pseudomonas aeruginosa strain (14 ± 1.00 and 14 ± 1.73 mm, respectively), at 100 μg/mL [193]. However, rutinose, sucrose, and 4-methoxy caffeic acid heptyl ester isolated from the same extracts did not display any activity [193].
2.1.16. Harungana madagascariensis Lam. ex Poir.
Harungana madagascariensis belongs to the family Hypericaceae, comprising ~700 known species in ~9 genera. H. madagascariensis is distributed throughout the tropics and subtropics (Mauritius, Madagascar, and Africa growing on the edges of wet forests [194]. Furthermore, the plant is considered an antibiotic, anti-inflammatory, antimicrobial, anti-protozoan, anti-sickling, immunomodulatory, antioxidant, and enzyme inhibition effects, as well as cytotoxicity [195,196,197], and is used for the treatment of asthma, anaemia, tuberculosis, angina, syphilis, dysentery, gonorrhoea, parasitic skin diseases, hypertension, toothache, dysmenorrhea, hepatitis, ulcer, river blindness, malaria, diarrhoea, fever, yellow fever, chest pains and wounds [194,198,199]. Phytochemical investigation of H. madagascariensis has shown that the species contains metabolites such as anthracenic derivatives, saponins, tannins, flavonoids, alkaloids, and glycosides [195,196]. Moulari et al. (2006) showed that 3-O-α-L-rhamnoside-5,7,3′,4′-tetrahydroxydihydroflavonol (astilbin) contributed to the strong antibacterial activity against Staphylococcus epidermidis, Micrococcus luteus, Moraxella sp., and Acinetobacter sp., with minimal inhibitory quantity (MIQ) values of 50, 25, 50 and 50 µg, respectively [195]. Tankeo et al. (2016) isolated betulinic acid, ferruginin A, madagascin, and kaempferol-3-O-β-D-glucopyranoside from the methanol leaf and stem bark crude extracts of H. madagascariensis using silica gel column chromatography [200]. Ferruginin A had significant antibacterial activity, with MIC values below 10 µg/mL against Enterobacter cloacae (BM67), Klebsiella pneumoniae (K2 and Kp55), Pseudomonas aeruginosa (PA01), Enterobacter aerogenes (ATCC13048 and EA294), and Escherichia coli (ATCC10536) [200]. However, betulinic acid, madagascin and kaempferol-3-O-β-D-glucopyranoside showed poor inhibitory effects (MIC > 128 µg/mL) against all tested bacteria [200].
2.1.17. Hymenocardia acida Tul.
Hymenocardia acida is a plant of the Phyllanthaceae family that is found in tropical Africa [201]. H. acida is used to treat chest complaints, diarrhoea, toothaches, smallpox, hypertension, headaches, rheumatic pains, abdominal tumours, jaundice, menstrual pains, abscesses, muscular pains and arthritis [202]. Phytochemical testing of the plant species showed the existence of carbohydrates, saponins, terpenes, glycosides, sterols, phenols, flavonoids and tannins [203]. Biological activities reported on the plant include antitumour, antiulcer, anti-HIV, antitrypanosomal, antiplasmodial, and antimicrobial, as well as cytotoxicity [204,205]. Six stilbenoid compounds (hymenocardichromene A–F) and one chromane stilbenoid (hymenocardichromanic acid) were isolated from the leaf extracts of H. acida using semipreparative HPLC [206]. Hymenocardchromanic acid showed the best antibacterial activity compared to the other compounds at 8 μg/mL against methicillin-resistant Staphylococcus aureus (MRSA-108), whereas the other compounds were moderately active [206]. Moreover, Agbidye et al. (2020) demonstrated that the methanol stem bark and root extracts of H. acida had potent antibacterial and fungal effects against Staphylococcus aureus, Streptococcus pyogenes, and Candida albicans at 1.0 × 103 mg/mL, respectively [207]. However, none of the leaf extracts demonstrated antibacterial and antifungal effects against the tested pathogenic microorganisms [207]. Agbidye et al. (2020) further showed that ethyl isoallocholate, γ-sitosterol, β-sitosterol, lupeol, stigmasterol and friedelin tentatively identified by GC-MS spectral technique contributed to the strong antibacterial and fungal effects of the methanol stem bark and root extracts of H. acida [207].
2.1.18. Lannea edulis (Sond.) Engl var.edulis.
Lannea edulis is a small deciduous shrub broadly used to treat malaria, gonorrhoea, angina pectoris, sexually transmitted diseases, dizziness, dysmenorrhea, schistosomiasis, bilharzia, gastrointestinal problems, diarrhoea, sore eyes, amenorrhea and to dilate the birth canal in Southern and East Africa [208,209,210,211,212,213,214]. L. edulis belongs to the Anacardiaceae family, comprising ~800 species in ~81 genera spread across tropical and subtropical regions in Africa, China, India, Indochina, and the Saudi Arabian Peninsula [215]. Ethnopharmacological studies showed that Lannea edulis extracts and constituents have antimalarial, antihyperglycemic, anti-human immunodeficiency virus, anthelmintic, antioxidant, antimicrobial, and antihyperlipidemic activities, as well as cytotoxicity [208,213,216,217,218,219,220,221]. In Malawi and South Africa, the seeds of Vigna unguiculata are mixed with the roots of Lannea edulis to treat blood urine and bilharzia [210,222,223]. However, in Malawi, the stem bark of Piliostigma thonningii is mixed with the stem bark of Lannea edulis to treat bilharzia [224]. The phytochemical screening of the genus Lannea showed that the species contains metabolites such as saponins, alkaloids, polyphenols, flavonoids, tannins, cardiac glycosides, and steroids from different plant parts of L. edulis [220,221]. Munodawafa et al. (2013) reported the antimicrobial properties of the leaf of L. edulis [218]. In their study, they found that the methanol crude extracts of L. edulis leaves were active against Pseudomonas aeruginosa, Escherichia coli, Aspergillus niger, Staphylococcus aureus, and Candida albicans, with MIC values that ranged from 2.5 to 5.0 mg/mL. The antimicrobial activity might be contributed to by the presence of alkaloids, coumarins, anthraquinone derivatives, cardiac glycosides, flavonoids, saponins and tannins detected in the methanol extracts of L. edulis. Medicinal plants that have flavonoids, alkaloids, and glycosides have been reported to possess antimicrobial activities [49].
2.1.19. Lippia multiflora Moldenke
Lippia multiflora is a member of the Verbenaceae family, which includes about ~200 species of grasses, shrubs and small trees, usually found in an extensive ecological range throughout South and Central American countries and tropical West African regions [225,226]. Traditionally, L. multiflora is used for nausea, stomach aches, fevers, coughs, gastrointestinal disturbances, colds, enteritis, and as a laxative [227]. Various pharmacological activities have been reported for L. multiflora, among which are in vitro antimalarial, antiviral, antifungal, analgesic, antipyretic, anti-inflammatory, antimicrobial, and antifungal [228,229]. Phytochemical research on this plant has resulted in the isolation of carvacrol using an accelerated gradient chromatography technique with silica gel as an adsorbent [230]. Samba et al. (2020) demonstrated that volatile components present in L. multiflora have antibacterial effects against Escherichia coli, Pseudomonas aeruginosa and Staphylococcus aureus [226].
2.1.20. Morinda lucida Benth.
Morinda lucida (“brimstone tree”) is a medicinal plant species in the Rubiaceae family which has been extensively used as medicine for decades in Central and West Africa for the treatment of conditions such as sickle cell disease, fever, cognitive disorders, typhoid fever, trypanosomiasis, malaria, parasitic worms, inflammation, cancer, hypertension, and diabetes [231,232]. Various compounds, including tannins, alkaloids, phenols, anthraquinones, fatty acids, saponins, flavonoids, anthraquinones, sterols, terpenoids, iridoids, polyphenols, and cardiac glycosides, have been isolated from different plant parts of Morinda lucida [233,234,235,236]. The in vitro scientific research studies on various extracts and pure components of Morinda lucida support the acclaimed biological properties of the plant, such as antioxidant, antimalarial, immunostimulatory, antimicrobial, anti-inflammatory, antidiabetic, hypotensive, anti-sickling, antileishmanial, antitrypanosomal, antifungal, antionchocercal, and antiproliferative [237]. Bata et al. (2023) proved that α and β-amyrin fractionated using column chromatography were responsible for the antibacterial activity of the active fraction of M. lucida methanol leaf against some multidrug-resistant Enterobacteriaceae (Escherichia coli, Providencia species, Enterobacter, Serratia, Pragia, and Klebsiella), with zones of inhibition that ranged from 15 to 18 mm [238].
2.1.21. Nauclea latifolia Sm.
Nauclea is a tropical evergreen tree belonging to the Rubiaceae family. They are generally distributed in tropical areas in Africa [239]. Many African countries use Nauclea latifolia to treat fever, malaria, dental problems, ascites, toothaches, infectious diseases, hypertension, diarrhoea, dysentery, colic, epilepsy, wounds, hernia, vomiting and health promotion [240,241,242]. N. latifolia has such as anti-inflammatory, antioxidant, and antidiabetic activity [240,241,242]. N. latifolia contains phytochemicals such as carbohydrates, alkaloids, tannins, anthocyanins, saponins, phlobatannins, glycosides, terpenoids, and cardiac glycosides [239]. Chabi-Sika et al. (2022) assessed the antimicrobial activity of the ethanolic crude extract of N. latifolia. Their results showed that the extract had activity against Streptococcus pneumoniae (ATCC 496190) and Pseudomonas aeruginosa (ATCC 27853) with an MIC of 1.25 mg/mL and inhibition diameter of 19 ± 1.33 mm [243]. Phytochemical analysis revealed the presence of flavonoids, O-heterosides, C-heterosides, saponosides, anthocyanins, and mucilages [243]. These secondary metabolites, identified within the ethanolic crude extract of N. latifolia, are well known for their biological activities. Saponosides and flavonoids are recognised for their diversified antimicrobial, antibacterial, and antifungal activities.
2.1.22. Pachira glabra Pasq.
The Pachira glabra is frequently distributed on wetlands near rivers and lakes. It belongs to the Malvaceae family and is native to the tropical regions of Africa, South America and Southern Mexico [244]. All parts of P. glabra are used to treat diarrhoea, stomach pain, and dysentery [245]. Pachira glabra is known to have antimicrobial, insecticidal, antimycobacterial, antioxidant and anti-helicobacter pylori activities [246,247]. These pharmacological properties are attributed to the presence of flavonoids, tannins, terpenoids, steroids, fatty acids, and coumarins in aerial and underground parts of P. glabra [248]. The antimicrobial activity of the Pachira glabra extracts using agar diffusion and broth microdilution methods has been reported, and the results showed that this plant has moderate to potent antimicrobial activity against Micrococcus spp., Proteus spp., and Citrobacter youagae with inhibition zones and MIC’s ranging from 13.7 to 24.0 mm and 0.3 to 2.5 mg/mL, respectively [249]. Thirty-three compounds with 98.40% of total contents from the essential oil of P. glabra contributed to the antimicrobial activity of the extracts [249].
2.1.23. Piliostigma thonningii (Schum.) Milne-Redh.
Piliostigma thonningii is a leguminous plant that belongs to the Fabaceae family. It is used for numerous medicinal purposes in different African countries [250]. The decoction of the leaves and stem bark of P. thonningii are used for the management of malaria, ulcers, cough, sore throat, diarrhoea, bronchitis, toothache, leprosy, pyrexia, arthritis, heart pain, wounds, and gingivitis [251]. Its twigs and roots are used in the management of fever, dysentery, cough, skin diseases and wound infections [252]. The underground and aerial parts of P. thonningii are reported to possess antibacterial, anti-inflammatory, antilipidemic, and antihelminthic activities [253]. Antimicrobial evaluation of 50 % ethyl acetate leaf extracts from P. thonningii was active against Escherichia coli, Staphylococcus epidermidis, Staphylococcus aureus, and methicillin-resistant Staphylococcus aureus with MIC values below 500 µg/mL [254]. Akinpelu and Obuoto (2000) demonstrated that the methanol stem extract of P. thonningii had activity against Staphylococcus aureus (NCIB 8588), Shigella dysenteriae (LIO), Serratia marcescens (NCIB 1377), Pseudomonas aeruginosa (NCIB 950), Proteus vulgaris (NCIB 67), Escherichia coli (NCIB 86), Corynebacterium pyogenes (LIO), and Bacillus subtilis (NCIB 3610) at a concentration of 20 mg/mL [255]. Phytochemical studies on P. thoningii extracts showed the occurrence of distinct chemical components that accommodate the activities of this herbal plant. Among the identified chemical classes were diterpenes, saponins, volatile oils, terpenes, alkaloids, tannins, flavonoids, and carbohydrates [255].
2.1.24. Piper umbellatum L.
Piper umbellatum (Piperaceae (~3600 species in ~5 genera) is broadly distributed in Brazil, Mexico, Bolivia, Peru, Central America, the West Indian Islands, and South America. The neotropical plant has also been introduced to Southeast Asia and Africa [256]. P. umbellatum is used in traditional medicine in various preparation forms for the treatment of colic, malaria, diarrhoea, dysentery, digestive problems, peptic ulcer, dyspepsia, pains, constipation, fever, intestinal parasites, stomach ache, urinary tract infections, bruises, wound healing, swelling, inflammation, rheumatism, and gastrointestinal diseases [257]. Phytochemical studies of Piper umbellatum have demonstrated the presence of terpenes, steroids, flavonoids and alkaloids [258]. Other studies have shown that crude extracts and isolated compounds derived from Piper umbellatum extracts contain a variety of biological activities, including anti-atherogenic, antibacterial, antimalarial, anti-inflammatory, analgesic, antioxidant, antifungal, anti-leishmanial, and antitrypanosomal, as well as cytotoxicity [259]. Okunrobo et al. (2011) demonstrated that carbohydrates, alkaloids, cardiac glycosides, tannins and saponins present in the methanol extract of P. umbellatum, as well as the n-hexane, chloroform and n-butanol fractions of the extract might be responsible for the antimicrobial activity against all the test pathogenic microorganisms (Staphylococus aureus, Psuedomonas aeruginosa, Candida albicans and Escherichia coli), with MIC values < 25 mg/mL [260].
2.1.25. Psorospermum febrifugum Spach
Psorospermum febrifugum (Hypericaceae) is a plant species in the genus Psorospermum growing in Mozambique, Angola, Ethiopia, Zimbabwe and Guinea [261,262]. P. febrifugum has been used to treat various ailments, including epilepsy, skin diseases, wounds, scabies, eczema, pimples, leprosy, malaria, tuberculosis, pneumonia, poison, dysentery, dysmenorrhoea, whooping cough, skin rashes, syphilis, haemorrhoids, and stomach disorders; as well as opportunistic diseases such as watery blisters in genital areas, cryptococcal meningitis, and herpes [17,21,22,263,264,265]. Many phytochemicals, such as alkaloids, flavonoids, xanthones, steroids, anthraquinones, tannins, glycosides, terpenoids, and phenols, have also been isolated from the Psorospermum febrifugum, making it an important resource for biological drug and applications discovery [266,267,268]. Biological information from in vitro studies showed that P. febrifugum phytochemicals and extracts contain biological effects such as anticancer, anxiolytic, antipsoriatic, anti-inflammatory, antitrypanosomal, acaricidal, antimicrobial, antioxidant, and antimalarial, which affirmed the traditional usage of the plant [262,269,270,271,272,273]. Nambooze (2019) demonstrated that P. febrifugum had noteworthy antibacterial activity [274]. The ethyl acetate stem bark crude extract displayed the highest zone of inhibition of 18.3 ± 0.07 mm and 19.1 ± 0.14 mm against Staphylococcus aureus and Streptococcus pyogenes, respectively [274]. Phytochemical screening of ethyl acetate extract proved the existence of tannins, carbohydrates, reducing sugar, phenols, and terpenoids. Furthermore, Nambooze (2019) isolated, identified and characterised oleanolic acetate acid, betulinic acid and oleanolic acid from the ethyl acetate extract; a promising antibacterial activity was exhibited by all three metabolites [274]. Oleanolic acetate acid displayed the lowest zone of inhibitions of 8.1 ± 0.14 mm and 6.5 ± 0.2 mm against Pseudomonas aeruginosa and Staphylococcus aureus, whereas betulinic acid showed a moderate zone of inhibition [274]. Oleanolic acid displayed the highest zone of inhibition of (14.2 ± 0.07 mm) against Staphylococcus aureus and Streptococcus pyogenes. Additionally, Mpinda et al. (2018) proved that the extracts of P. febrifugum demonstrated growth inhibition of Klebsiella pneumoniae with the minimum inhibitory concentrations between 6.3 and 25 mg/mL [271]. This may be due to synergistic or additive effects of the compound mixtures in the extracts.
2.1.26. Syzygium guineense Wall.
Syzygium guineense belongs to the Myrtaceae family, which contains approximately ~4000 species of trees and shrubs in ~140 genera. S. guineense is distributed in various parts of Africa [275]. The stem bark and root mixtures of S. guineense are used to manage stomach aches, diarrhoea, diabetes mellitus, and typhoid fever and are anthelmintic [276]. Syzygium guineense has been reported to possess antioxidant, anti-inflammatory, antifungal, and antibacterial activities [276]. Mavanza et al. (2023) showed that flavonoids, glycosides, terpenoids, phenolics saponins, steroids, alkaloids, quinones, and tannins identified in S. guineense extracts by phytochemical analysis could be responsible for the antibacterial properties observed in this plant against Bacillus subtilis (10.67 mm), Escherichia coli (14.33 mm), Staphylococcus aureus (15.00 mm) and Salmonella enterica typhii (9.33 mm) [277]. Antibacterial properties observed in S. guineense extract against Bacillus subtilis, Escherichia coli, Staphylococcus aureus, and Salmonella enterica typhii produced inhibition zones of 10.67, 14.33, 15.00, and 9.33 mm, respectively [277]. Qualitative analysis of chemical compounds of S. guineense extracts showed the presence of flavonoids, glycosides, terpenoids, phenolics saponins, steroids, alkaloids, quinones, and tannins [277]. Terminolic acid, 28-β-glucopyranosyl ester, oleanolic acid, arjunolic acid, 6-hydroxyasiatic acid, asiatic acid, and 2-hydroxyoleanolic acid were isolated from the S. guineense leaf extracts using column chromatography over silica gel [278]. Asiatic acid and terminolic acid showed significant antibacterial activity against Escherichia coli, Bacillus subtilis and Shigella sonnei with MICs of 3, 0.5, and 30 μg for asiatic acid and 5, 0.75, and 30 μg for terminolic acid. Arjunolic acid and 6-hydroxyasiatic acid were less active with MICs of 6, 3, and 50 μg against Escherichia coli and Bacillus subtilis, whereas oleanolic acid, 2-hydroxyursolic acid, arjunolic acid and 28-β-glucopyranosyl ester had no activity against Escherichia coli and Bacillus subtilis [278].
2.1.27. Vitex doniana Sweet
Vitex doniana is a tree native to the Afrotropics (Sub-Saharan Africa including Madagascar), Southern Arabian Peninsula, and Western India. The Vitex genus belongs to the family Lamiaceae [279]. In folk medicine, the root, stem bark, leaf and fruit pulp are used to treat diseases such as malaria, jaundice, cancer, anaemia, malnutrition, dysentery, leprosy, gonorrhoea, diarrhoea, rickets, ancylostomiasis, backaches, gastrointestinal disorders, respiratory diseases fevers, stiffness, headache, rash, chickenpox, measles, hemiplegia fever, wounds, eye troubles, colic, burns, kidney troubles stomach complaints, liver diseases, leprosy, and to control bleeding after childbirth [25,280,281]. Vitex doniana has been reported to have antibacterial, anti-hepatotoxic, anti-dysentery, and antimalarial activities [280]. Several studies have reported that hydroxycinnamic acid, allicins saponins, terpenoids and flavonoids found in the crude extracts of V. doniana could be responsible for the antimicrobial effectiveness of Vitex doniana against pathogenic bacteria such as Staphylococcus aureus, Escherichia coli, Shigella dysenteriae, Bacillus subtilis, Pseudomonas aeruginosa and Salmonella typhii [282,283,284,285,286]. Sonibare et al. (2009) proved that 31.13% β-phellandrene, 28.3% phytol, and 12.6% β-caryophyllene found in the leaf essential oil of V. doniana have antimicrobial activity against Proteus mirabilis, Bacillus subtilis and Candida albicans [287]. In another study, Owolabi et al. (2022) demonstrated that 23.57% incensyl acetate, 16.87% phytol, 12.34% (E)-β-caryophyllene, and 9.73% phytone present in V. doniana have noteworthy antifungal effectiveness against Aspergillus niger with MIC of 78.1 μg/mL [288].
3. Materials and Methods
3.1. Selection of Published Articles
A literature search on medicinal plants used in the management of microbial infections in Angola was conducted by gathering information or data from books, journals, published M.Sc. and Ph.D. theses, as well as different electronic databases such as Wiley Online, ScienceDirect, Scopus, SciFinder, Web of Science, BMC, Elsevier, Google Scholar, SpringerLink, and PubMed. The following keywords, “Angola”, “Plants used for treating illnesses possibly related to infections”, “Plants used for treating infectious diseases”, “Plants used in treating infections/infectious diseases/microbial infections in Angola”, “Microbial infections”, “Infectious diseases ”, “Angola/Angolan plants”, “Angolan medicinal plants”, “Angolan traditional medicine”, “Angolan and antimicrobial plants”, “Antimicrobial/Antimicrobial plants”, “Angolan and antibacterial plants”, “Antibacterial/Antibacterial plants”, “Angolan and antifungal plants”, “Antifungal/Antifungal plants”, “Traditional/Traditional knowledge”, “Traditional medicine”, “Traditional medicinal plants”, “Medicinal plants”, “Medicinal herbs”, “Indigenous/Indigenous knowledge”, “Plants/Herbal/Medicine/Remedies”, “Ethnobotany/Ethnobotanical”, “Ethnopharmacology/Ethnopharmacological”, “Ethnomedicine/Ethnomedicinal”, and “Phytomedicine” were used to search for relevant articles.
3.2. Selection Criteria
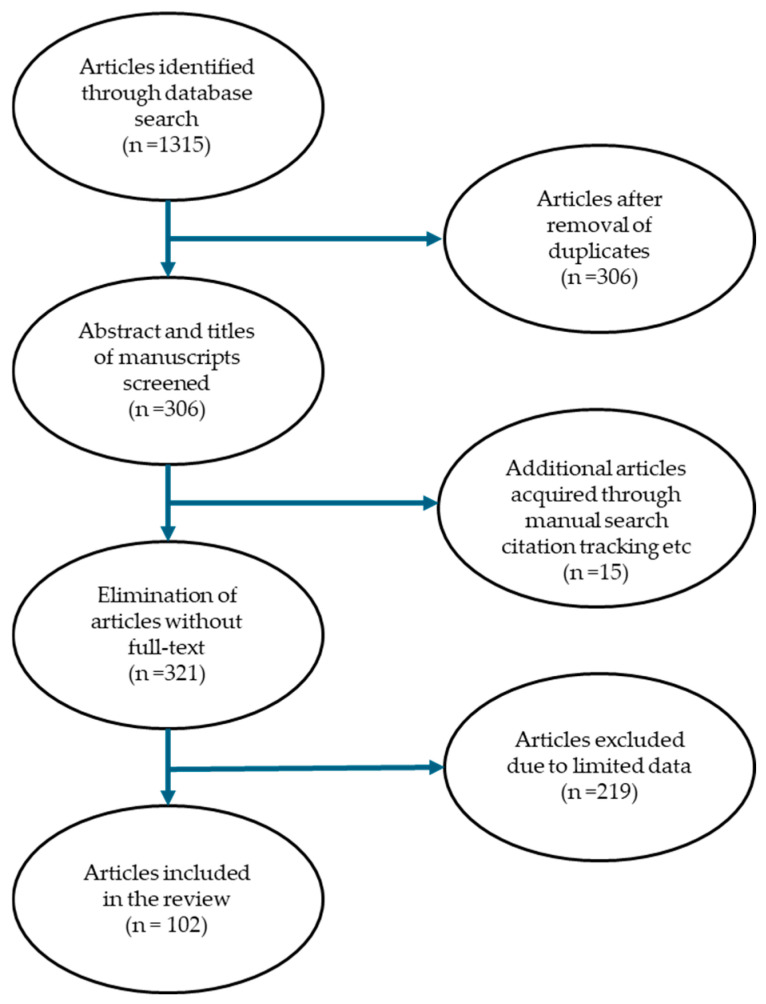
The main inclusion criterion was published research articles related to the use of plants for managing diseases related to infections, with duration from January 1976 to November 2023. The scientific name of the plant had to be provided. The exclusion criteria were published studies or articles not written in the English language. Furthermore, published studies or articles that did not have information on Angolan medicinal plants used for treating infections, microbial infections and illnesses related to infections, and abstract-only accessed published articles. Four-step selection criteria were employed to identify the published articles included in this study. Step 1: the importance of studies was checked based on the titles and abstracts of the published articles. Step 2: titles and abstracts of the published articles were critically evaluated to match the inclusion criteria. The inclusion criteria were published studies or articles written in the English language, published studies or articles with information on Angolan medicinal plants used for treating infections, microbial infections and illnesses related to infections, and the provision of the scientific name of the medicinal plant. Step 3: the full text of the identified published papers obtained by the authors was assessed and screened based on the information or data acquired in the previous step (step 2) to make an informed decision as to whether to add or reject these publications in this review. Step 4: the remaining full-text published articles that met the inclusion criteria were thoroughly inspected. In total, 102 published articles were included in this study (Figure 2). The scientific names for the plants were validated using recognised databases, including Plants of the World Online (https://powo.science.kew.org/, accessed on 6 May 2024), The Plant List (http://www.plantlist.org/, accessed on 6 May 2024) and The World Flora Online (WFO) (http://www.worldfloraonline.org/, accessed on 6 May 2024) [289,290,291].
Figure 2.
An overview of the procedure applied for the identification of 102 articles included in this review.
Table 1.
Angolan medicinal plants used for microbial and bacterial infections.
| Species | Family | Part(s) Used | Traditional Uses | References |
|---|---|---|---|---|
| Acanthus montanus (Nees) T. Anderson | Acanthaceae | Root | Cystitis, pains, endometritis, urogenital infections, aches, leucorrhoea, urethral pain, urinary disease and furuncle | [43,44] |
| Abelmoschus esculentus (L.) Moench | Malvaceae | Leaves, fruits, seeds, pods | Depression, ulcers, sore throats, pulmonary inflammations and gastrointestinal irritations | [51,54] |
| Aframomum alboviolaceum (Ridl.) K. Schum. | Zingiberaceae | Leaves | Cure headache, cough, fever, amoebic dysentery, haemorrhoids, gastritis, myoma, pruritis, hypertension, filarial, malaria, pruritus, and gastritis | [57,58,59,60] |
| Alchornea cordifolia (Schumach. & Thonn.) Müll.Arg. | Euphorbiaceae | Whole plant | Venereal diseases, malaria, diarrhoea, wounds, cuts, sores, coughs, colds, eye problems, pigmentation problems, gastrointestinal, headaches, rheumatic pains, urinary disorders; as well as inflammatory disorders, fungal, parasitic, bacterial, parasitic, and disorders | [64,65,67,68,69,70] |
| Aloe buettneri A. Berger | Asphodelaceae | Root, leaves | Wounds, vitiligo, malaria, rheumatism, insect bites, burns and worm sores | [80] |
| Annona stenophylla Engl. & Diels | Annonaceae | Root, leaves | Coughs, wounds, helminthiasis, cancer, dysentery, diarrhoea, headache, asthma, fever, malaria, dermatitis, mental disorders, diabetes, and peptic ulcers | [87,88,89] |
| Bridelia ferruginea Benth. | Phyllanthaceae | Root, stem bark, leaves, fruits | Dysentery, arthritis, cough, rashes, constipation, epilepsy, diarrhoea, diuretic, chronic diabetes, asthma, gout, intestinal disorders, thrush, dysentery, gastralgias, rheumatisms, sexually transmitted diseases, contusion, oral infections, bladder disorders, skin diseases, and anaemia | [93,94] |
| Canarium schweinfurtii Engl. | Burseraceae | Stem bark, resin, leaves | Roundworm infections, skin-affections, dysentery, eczema, diarrhoea, dysentery, haemorrhoids, venereal diseases, hypertension, malaria, fever, gonorrhoea, chest pains, stomach complaints, pulmonary affections, ulcers, leprosy, coughs and wounds | [106,107,108,109] |
| Chromolaena odorata (L.) R.M.King & H.Rob. | Asteraceae | Leaves | Malaria, coughs, colds, toothache, stomach problems, diarrhoea, stomach ulcers, wounds, dysentery, skin infections, bacterial and fungal infections | [123,124,128,129] |
|
Clerodendrum splendens G.Don |
Lamiaceae | Whole plant | Bruises, vaginal thrush, various skin infections and wound healing | [137,138] |
| Combretum racemosum P.Beauv. | Fabaceae | Whole plant | Wounds, haemorrhoids, roundworms, gastro-intestinal affections, coughs, toothache, tuberculosis, genito-urinary, male sterility and bleeding during pregnancy | [141,142,143,144,145] |
| Dioscorea praehensilis Benth. | Dioscoreaceae | Whole plant | Diabetes, stomach pains, rheumatism, haemorrhoids, coughs, skin infections, and diarrhoea | [150,151,152] |
| Erythrina abyssinica Lam. | Fabaceae | Whole plant | Malaria, tuberculosis, cancer, diabetes, leprosy, syphilis, back pain, yellow fever, anaemia, inflammatory diseases, venereal diseases, sexually transmitted diseases, skin infections, diarrhoea, epilepsy, urinary tract infections, pregnancy-related conditions, vomiting, soft tissue, hepatitis, central nervous system (CNS)-related disorders, helminthiasis, pneumonia, infertility, bacterial and fungal infections | [25,154,155,156,160,161,162,163] |
| Gardenia ternifolia Schumach. & Thonn. | Rubiaceae | Whole plant | Diabetes, malaria, sexually transmitted diseases, ascites, hepatitis, wounds, tooth decay, onchocerciasis, hypertension, haemorrhoids, leprosy, blood pressure, female infertility, skin diseases, diarrhoea, liver, cancer, sickle cell disease, rheumatism and yellow fever | [25,172,173,174,175,176,177,178,179,180,181,182,183] |
| Gloriosa superba L. | Colchicaceae | Whole plant | Wounds, gout, infertility, snakebite, cholera, ulcers, colic, arthritis, kidney problems, sprains, typhus, itching, smallpox, cancer, leprosy, sexually transmitted diseases, bruises, haemorrhoids, skin problems, and nocturnal emission | [186,187,188,189,190,191,192] |
| Harungana madagascariensis Lam. ex Poir. | Hypericaceae | Stem bark, leaves | Asthma, anaemia, tuberculosis, angina, syphilis, dysentery, gonorrhoea, parasitic skin diseases, hypertension, toothache, dysmenorrhea, hepatitis, ulcer, river blindness, malaria, diarrhoea, fever, yellow fever, chest pains and wounds | [194,198,199] |
| Hymenocardia acida Tul. | Phyllanthaceae | Root, stem bark, leaves | Chest complaints, diarrhoea, toothaches, smallpox, hypertension, headaches, rheumatic pains, abdominal, tumours, jaundice, menstrual pains, abscesses, muscular pains and arthritis | [201,202] |
| Lannea edulis (Sond.) Engl. var. edulis | Anacardiaceae | Root, rootbark, stem bark, leaves | Malaria, gonorrhoea, angina pectoris, sexually transmitted diseases, dizziness, dysmenorrhea, schistosomiasis, bilharzia, gastrointestinal problems, diarrhoea, sore eyes, amenorrhea and to dilate birth canal | [208,209,210,211,212,213,214] |
| Lippia multiflora Moldenke | Verbenaceae | Leaves | Nausea, stomach aches, fevers, coughs, gastrointestinal disturbances, colds, and enteritis | [226,227] |
| Morinda lucida Benth. | Rubiaceae | Root, stem bark, leaves | Sickle cell disease, fever, cognitive disorders, typhoid fever, trypanosomiasis, malaria, parasitic worms, inflammation, cancer, hypertension, and diabetes | [231,232] |
| Nauclea latifolia Sm. | Rubiaceae | Whole plant | Fever, malaria, dental problems, ascites, toothaches, infectious diseases hypertension, diarrhoea, dysentery, colic, epilepsy, wounds, hernia, vomiting and health promotion | [239,240,241,242] |
| Pachira glabra Pasq. | Malvaceae | Stem bark, leaves, seeds | Diarrhoea, stomach pain, and dysentery | [244,245] |
| Piliostigma thonningii (Schum.) Milne-Redh. | Fabaceae | Root, stem bark, leaves | Malaria, ulcers, cough, sore throat, diarrhoea, bronchitis, toothache, leprosy, pyrexia, arthritis, heart pain, wounds, and gingivitis | [250,252] |
| Piper umbellatum L. | Piperaceae | Whole plant | Colic, malaria, diarrhoea, dysentery, digestive problems, peptic ulcer, dyspepsia, pains, constipation, fever, intestinal parasites, stomach ache, urinary tract infections, bruises, wound healing, swelling, inflammation, rheumatism, and gastrointestinal diseases | [256,257] |
| Psorospermum febrifugum Spach | Hypericaceae | Whole plant | Epilepsy, skin diseases, wounds, scabies, eczema, pimples, leprosy, malaria, tuberculosis, pneumonia, poison, dysentery, dysmenorrhoea, whooping cough, skin rashes, syphilis, haemorrhoids, and stomach disorders; as well as opportunistic diseases such as watery blisters in genital areas, cryptococcal meningitis, and herpes | [17,21,22,261,262,263,264,265] |
| Syzygium guineense Wall. | Myrtaceae | Stem bark, leaves, fruits, seeds | Stomach ache, diarrhoea, diabetes mellitus, and typhoid fever | [275,276] |
| Vitex doniana Sweet | Lamiaceae | Whole plant | Malaria, jaundice, cancer, anaemia, malnutrition, dysentery, leprosy, gonorrhoea, diarrhoea, rickets, ancylostomiasis, backaches, gastro-intestinal disorders, respiratory diseases fevers, stiffness, headache, rash, chickenpox, measles, hemiplegia fever, wounds, eye troubles, colic, burns, kidney troubles stomach complaints, liver diseases, leprosy, and to control bleeding after childbirth | [25,279,280,281] |
4. Conclusions and Future Perspectives
This review focused on the use of medicinal plants in the management of microbial infections in Angola. A total of 27 plant species, representing 19 families, were documented in this study. The medicinal plants recorded in this study may assist researchers in developing novel medicines for the treatment of infectious diseases in Angola, on the African continent and beyond. This review provided data for scientific considerations in the search for novel natural-based drug development for the management of infectious diseases. There is a need to perform a comprehensive isolation of the bioactive compounds in the identified medicinal plants for biological analysis purposes and to determine their therapeutic properties. Furthermore, extensive preclinical and clinical trials are needed to investigate the therapeutic potential of medicinal plants for microbial infections. The employment of toxicological methods to validate the safety of the biologically active compounds isolated from the medicinal plants recorded or documented in this study is highly recommended.
Author Contributions
Conceptualisation, D.T., N.M., I.T.M., T.L. and M.M.; data curation, D.T.; writing—original draft preparation, D.T.; writing—review and editing, D.T., N.M., I.T.M., T.L. and M.M. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Nasir B., Fatima H., Ahmed M., Haq I.U. Recent trends and methods in antimicrobial drug discovery from plant sources. Austin. J. Microbiol. 2015;1:1002 [Google Scholar]
- 2.Hajjeh R.A., Relman D., Cieslak P.R., Sofair A.N., Passaro D., Flood J., Johnson J., Hacker J.K., Shieh W.J., Hendry R.M., et al. Surveillance for Unexplained Deaths and Critical Illnesses. Emer. Inf. Dis. 2002;8:145. doi: 10.3201/eid0802.010165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray C.J., Ikuta K.S., Sharara F., Swetschinski L., Aguilar G.R., Gray A., Han C., Bisignano C., Rao P., Wool E., et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet. 2022;399:629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boutayeb A. Handbook of Disease Burdens and Quality of Life Measures. Springer Nature; Berlin, Germany: 2010. The impact of infectious diseases on the development of Africa; pp. 1171–1188. [DOI] [Google Scholar]
- 5.Vaou N., Stavropoulou E., Voidarou C., Tsigalou C., Bezirtzoglou E. Towards advances in medicinal plant antimicrobial activity: A review study on challenges and future perspectives. Microorganisms. 2021;9:2041. doi: 10.3390/microorganisms9102041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ozioma E.O.J., Chinwe O.A.N. Herbal medicines in African traditional medicine. Herb. Med. 2019;10:191–214. [Google Scholar]
- 7.Albahri G., Badran A., Hijazi A., Daou A., Baydoun E., Nasser M., Merah O. The therapeutic wound healing bioactivities of various medicinal plants. Life. 2023;13:317. doi: 10.3390/life13020317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elshafie H.S., Camele I., Mohamed A.A. A comprehensive review on the biological, agricultural and pharmaceutical properties of secondary metabolites based-plant origin. Int. J. Mol. Sci. 2023;24:3266. doi: 10.3390/ijms24043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chassagne F., Samarakoon T., Porras G., Lyles J.T., Dettweiler M., Marquez L., Salam A.M., Shabih S., Farrokhi D.R., Quave C.L. A systematic review of plants with antibacterial activities: A taxonomic and phylogenetic perspective. Front. Pharmacol. 2021;11:586548. doi: 10.3389/fphar.2020.586548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mintah S.O., Asafo-Agyei T., Archer M.A., Junior P.A.A., Boamah D., Kumadoh D., Appiah A., Ocloo A., Boakye Y.D., Agyare C. Pharmacognosy-Medicinal Plants. IntechOpen; London, UK: 2019. Medicinal plants for treatment of prevalent diseases; pp. 1–19. [DOI] [Google Scholar]
- 11.Atanasov A.G., Zotchev S.B., Dirsch V.M., Supuran C.T. Natural products in drug discovery: Advances and opportunities. Nat. Rev. Drug Dis. 2021;20:200–216. doi: 10.1038/s41573-020-00114-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Angola Population Worldometer. 2024. [(accessed on 22 January 2024)]. Available online: http://www.worldometers.info.
- 13.Lautenschläger T., Neinhuis C., Heinze C., Göhre A., Monizi M., Pedro M., Mandombe J.L., Bránquima M.F., Ditsch B. New records for the flora of Angola: Observations from Uíge and Cuanza Norte. Plant Ecol. Evol. 2020;153:132–142. doi: 10.5091/plecevo.2020.1625. [DOI] [Google Scholar]
- 14.Canga I.L.V., Vita P., Oliveira A., Pinho C., González M. Ethnopharmacological study of medicinal plants from the province of Cuanza Norte (Angola) Rev. Contexto Saúde. 2022;22:e13336. doi: 10.21527/2176-7114.2022.46.13336. [DOI] [Google Scholar]
- 15.Goyder D.J., Gonçalves F.M.P. Biodiversity of Angola. Springer; Cham, Switzerland: 2019. The flora of Angola: Collectors, richness and endemism; pp. 79–96. [DOI] [Google Scholar]
- 16.Catarino S., Goyder D., Darbyshire I., Costa E., Figueira R., Duarte M.C., Romeiras M.M. Species diversity and endemicity in the Angolan Leguminosae flora. Front. Ecol. Evol. 2022;10:871261. doi: 10.3389/fevo.2022.871261. [DOI] [Google Scholar]
- 17.Göhre A., Toto-Nienguesse Á.B., Futuro M., Neinhuis C., Lautenschläger T. Plants from disturbed savannah vegetation and their usage by Bakongo tribes in Uíge, Northern Angola. J. Ethnobiol. Ethnomed. 2016;12:42. doi: 10.1186/s13002-016-0116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mawunu M., Bongo K., Eduardo A., Vua M.M.Z., Ndiku L., Mpiana P.T. Contribution à la connaissance des produits forestiers non ligneux de la Municipalité d’Ambuila (Uíge, Angola): Les plantes sauvages comestibles [Contribution to the knowledge of no-timber forest products of Ambuila Municipality (Uíge, Angola): The wild edible plants] Int. J. Inn. Sci. Res. 2016;26:190–204. [Google Scholar]
- 19.Urso V., Signorini M.A., Tonini M., Bruschi P. Wild medicinal and food plants used by communities living in Mopane woodlands of southern Angola: Results of an ethnobotanical field investigation. J. Ethnopharm. 2016;177:126–139. doi: 10.1016/j.jep.2015.11.041. [DOI] [PubMed] [Google Scholar]
- 20.Heinze C., Ditsch B., Congo M.F., Lautenschläger T., Neinhuis C. First ethnobotanical analysis of useful plants in Cuanza Norte, North Angola. Res. Rev. J. Bot. Sci. 2017;6:44–53. [Google Scholar]
- 21.Lautenschläger T., Monizi M., Pedro M., Mandombe J.L., Bránquima M.F., Heinze C., Neinhuis C. First large-scale ethnobotanical survey in the province of Uíge, northern Angola. J. Ethnobiol. Ethnomed. 2018;14:51. doi: 10.1186/s13002-018-0238-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Novotna B., Polesny Z., Pinto-Basto M.F., Van Damme P., Pudil P., Mazancova J., Duarte M.C. Medicinal plants used by ‘root doctors’, local traditional healers in Bié province, Angola. J. Ethnopharmacol. 2020;260:112662. doi: 10.1016/j.jep.2020.112662. [DOI] [PubMed] [Google Scholar]
- 23.Soares M.O., Vinha A.F., Coutinho F., Pires P.C. Antimicrobial natural products. In: Méndez-Vilas A., editor. Microbial Pathogens and Strategies for Combating Them: Science, Technology and Education. Volume 2. Formatex Research Center; Badajoz, Spain: 2013. pp. 946–950. [Google Scholar]
- 24.Santos E.S., Luís Â., Gonçalves J., Rosado T., Pereira L., Gallardo E., Duarte A.P. Julbernardia paniculata and Pterocarpus angolensis: From ethnobotanical surveys to phytochemical characterization and bioactivities evaluation. Molecules. 2020;25:1828. doi: 10.3390/molecules25081828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mawunu M., António D., Vita P., Ngbolua K.N., Luyeye L., Ndiku L., Luzolawo P.M., Francisco N.M. Ethnobotanical Survey of Herbal Teas Consumed in Uíge Province, Angola: Part 1. Ethnobot. Res. Appl. 2023;26:23. doi: 10.32859/era.26.23.1-27. [DOI] [Google Scholar]
- 26.Vahekeni N., Neto P.M., Kayimbo M.K., Mäser P., Josenando T., da Costa E., Falquet J., van Eeuwijk P. Use of herbal remedies in the management of sleeping sickness in four northern provinces of Angola. J. Ethnopharm. 2020;256:112382. doi: 10.1016/j.jep.2019.112382. [DOI] [PubMed] [Google Scholar]
- 27.Miranda J.J.M. Phytomedicine. Academic Press; Cambridge, MA, USA: 2021. Medicinal plants and their traditional uses in different locations; pp. 207–223. [DOI] [Google Scholar]
- 28.Anyaegbunam Z.K.G., Mba I.E., Doowuese Y., Anyaegbunam N.J., Mba T., Aina F.A., Chigor V.N., Nweze E.I., Eze E.A. Antimicrobial resistance containment in Africa: Moving beyond surveillance. Biosaf. Health. 2024;6:50–58. doi: 10.1016/j.bsheal.2023.12.003. [DOI] [Google Scholar]
- 29.Dikoumba A.C., Onanga R., Mangouka L.G., Boundenga L., Ngoungou E.B., Godreuil S. Molecular epidemiology of antimicrobial resistance in central africa: A systematic review. Access Microbiol. 2023;5:000556-v5. doi: 10.1099/acmi.0.000556.v5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morrison L., Zembower T.R. Antimicrobial resistance. Gastrointest. Endosc. Clin. 2020;30:619–635. doi: 10.1016/j.giec.2020.06.004. [DOI] [PubMed] [Google Scholar]
- 31.Kariuki S., Kering K., Wairimu C., Onsare R., Mbae C. Antimicrobial resistance rates and surveillance in sub-Saharan Africa: Where are we now? Infect. Drug Resist. 2022;15:3589–3609. doi: 10.2147/IDR.S342753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Iwu-Jaja C.J., Jaca A., Jaja I.F., Jordan P., Bhengu P., Iwu C.D., Okeibunor J., Karamagi H., Tumusiime P., Fuller W., et al. Preventing and managing antimicrobial resistance in the African region: A scoping review protocol. PLoS ONE. 2021;16:e0254737. doi: 10.1371/journal.pone.0254737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moyo P., Moyo E., Mangoya D., Mhango M., Mashe T., Imran M., Dzinamarira T. Prevention of antimicrobial resistance in sub-Saharan Africa: What has worked? What still needs to be done? J. Infect. Public Health. 2023;16:632–639. doi: 10.1016/j.jiph.2023.02.020. [DOI] [PubMed] [Google Scholar]
- 34.Karambwe S., Traoré A.N., Potgieter N. Epidemiology of Cefotaxime-Hydrolysing β-Lactamase-Producing Escherichia coli in Children with Diarrhoea Reported Globally between 2012 and 2022. Microorganisms. 2024;12:171. doi: 10.3390/microorganisms12010171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Institute for Health Metrics and Evaluation (IHME) Antimicrobial Resistance Leads to More Deaths and Illnesses in the WHO African Region Than Anywhere Else. 2023. [(accessed on 11 March 2024)]. Available online: https://www.healthdata.org/news-events/newsroom/news-releases/
- 36.Institute for Health Metrics and Evaluation (IHME) The Burden of Antimicrobial Resistance (AMR) in Angola. 2023. [(accessed on 18 March 2024)]. Available online: https://www.healthdata.org/sites/default/files/2023-09/Angola.pdf.
- 37.Henson S.P., Boinett C.J., Ellington M.J., Kagia N., Mwarumba S., Nyongesa S., Mturi N., Kariuki S., Scott J.A.G., Thomson N.R., et al. Molecular epidemiology of Klebsiella pneumoniae invasive infections over a decade at Kilifi County Hospital in Kenya. Int. J. Med. Microbiol. 2017;307:422–429. doi: 10.1016/j.ijmm.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kishore M., Kaushik M. Antimicrobial resistance: A global health threat. Int. J. Sci. Res. 2006;13:2277–8179. doi: 10.36106/ijsr. [DOI] [Google Scholar]
- 39.World Health Organization (WHO) New Report Calls For Urgent Action to Avert Antimicrobial Resistance Crisis. Joint News Release. Apr 29, 2019. [(accessed on 25 March 2024)]. Available online: https://www.who.int/news/item/29-04-2019-new-report-calls-for-urgent-action-to-avert-antimicrobial-resistance-crisis.
- 40.Mestrovic T., Aguilar G.R., Swetschinski L.R., Ikuta K.S., Gray A.P., Weaver N.D., Han C., Wool E.E., Hayoon A.G., Hay S.I., et al. The burden of bacterial antimicrobial resistance in the WHO European region in 2019: A cross-country systematic analysis. Lancet Public Health. 2022;7:e897–e913. doi: 10.1016/S2468-2667(22)00225-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kimang’a A.N. A situational analysis of antimicrobial drug resistance in Africa: Are we losing the battle? Ethiop. J. Health Sci. 2012;22:135–143. [PMC free article] [PubMed] [Google Scholar]
- 42.Huxley A.J. The New Royal Horticultural Society Dictionary of Gardening. Macmillan Press Ltd.; London, UK: 1992. Acanthus montanus plant description and geographical distribution; p. 1. [Google Scholar]
- 43.Matos P., Batista M.T., Figueirinha A. A review of the ethnomedicinal uses, chemistry, and pharmacological properties of the genus Acanthus (Acanthaceae) J. Ethnopharmacol. 2022;293:115271. doi: 10.1016/j.jep.2022.115271. [DOI] [PubMed] [Google Scholar]
- 44.Didie V.S. Plant remedies from the Democratic Republic of Congo. Medicinal Plants Database, African Research Museum. 2005. [(accessed on 8 April 2024)]. Available online: https://scholar.google.com.sg/scholar?hl=en&as_sdt=0%2C5&q=Plant+remedies+from+the+Democratic+Republic+of+Congo.+Medicinal+Plants+Database%2C+African+Research+Museum.+2005&btnG=
- 45.Adeyemi O.O., Okpo S.O., Young-Nwafor C.C. The relaxant activity of the methanolic extract of Acanthus montanus on intestinal smooth muscles. J. Ethnopharm. 1999;68:169–173. doi: 10.1016/S0378-8741(99)00084-7. [DOI] [PubMed] [Google Scholar]
- 46.Adeyemi O.O., Okpo S.O., Okpaka O. The analgesic effect of the methanolic extract of Acanthus montanus. J. Ethnopharm. 2004;90:45–48. doi: 10.1016/j.jep.2003.09.021. [DOI] [PubMed] [Google Scholar]
- 47.Asongalem E.A., Foyet H.S., Ekobo S., Dimo T., Kamtchouing P. Antiinflammatory, lack of central analgesia and antipyretic properties of Acanthus montanus (Ness) T. Anderson. J. Ethnopharmacol. 2004;95:63–68. doi: 10.1016/j.jep.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 48.Okoli C.O., Akah P.A., Onuoha N.J., Okoye T.C., Nwoye A.C., Nworu C.S. Acanthus montanus: An experimental evaluation of the antimicrobial, anti-inflammatory and immunological properties of a traditional remedy for furuncles. BMC Complement. Alt. Med. 2008;8:27. doi: 10.1186/1472-6882-8-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dubale S., Kebebe D., Zeynudin A., Abdissa N., Suleman S. Phytochemical screening and antimicrobial activity evaluation of selected medicinal plants in Ethiopia. J. Exp. Pharmacol. 2023;15:51–62. doi: 10.2147/JEP.S379805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Anam E.M. Pentacyclic triterpenoids from Acanthus montanus (Acanthaceae) Indian J. Chem. 1997;36B:110–113. [Google Scholar]
- 51.Guebebia S., Espinosa-Ruiz C., Zourgui L., Cuesta A., Romdhane M., Esteban M.Á. Effects of okra (Abelmoschus esculentus L.) leaves, fruits and seeds extracts on European sea bass (Dicentrarchus labrax) leukocytes, and their cytotoxic, bactericidal and antioxidant properties. Fish Shellfish Immunol. 2023;138:108799. doi: 10.1016/j.fsi.2023.108799. [DOI] [PubMed] [Google Scholar]
- 52.Sindhu R.K., Puri V. Phytochemical, nutritional and pharmacological evidences for Abelmoschus esculentus (L.) J. Phytopharmacol. 2016;5:238–241. doi: 10.31254/phyto.2016.5606. [DOI] [Google Scholar]
- 53.Durazzo A., Lucarini M., Novellino E., Souto E.B., Daliu P., Santini A. Abelmoschus esculentus (L.): Bioactive components’ beneficial properties—Focused on antidiabetic role—For sustainable health applications. Molecules. 2018;24:38. doi: 10.3390/molecules24010038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hu L., Yu W., Li Y., Prasad N., Tang Z. Antioxidant activity of extract and its major constituents from okra seed on rat hepatocytes injured by carbon tetrachloride. BioMed Res. Int. 2014;2014:341291. doi: 10.1155/2014/341291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Islam M.T. Phytochemical information and pharmacological activities of Okra (Abelmoschus esculentus): A literature-based review. Phytother. Res. 2019;33:72–80. doi: 10.1002/ptr.6212. [DOI] [PubMed] [Google Scholar]
- 56.de Carvalho C.C., Cruz P.A., da Fonseca M.M.R., Xavier-Filho L. Antibacterial properties of the extract of Abelmoschus esculentus. Biotechnol. Bioprocess Eng. 2011;16:971–977. doi: 10.1007/s12257-011-0050-6. [DOI] [Google Scholar]
- 57.Taylor E.L., Taylor T.N., Krings M. Paleobotany: The Biology and Evolution of Fossil Plants. Academic Press; Cambridge, MA, USA: 2009. [(accessed on 15 April 2024)]. Available online: https://books.google.co.za/books. [Google Scholar]
- 58.Ashande C.M., Lukoki F.L., Tshilanda D.D., Tshibangu D.S., Mpiana P.T. A mini review on the phytochemistry and pharmacology of Aframomum alboviolaceum (Zingiberaceae) South Asian Res. J. Nat. Proc. 2021;4:24–35. [Google Scholar]
- 59.Titanji V.P., Zofou D., Ngemenya M.N. The antimalarial potential of medicinal plants used for the treatment of malaria in Cameroonian folk medicine. Afr. J. Trad. Complement. Altern. Med. 2008;5:302. [PMC free article] [PubMed] [Google Scholar]
- 60.Bongo G., Inkoto C., Masengo C., Tshiama C., Lengbiye E., Djolu R., Kapepula M., Ngombe K., Mbemba T., Tshilanda D., et al. Antisickling, antioxidant and antibacterial activities of Afromomum alboviolaceum (Ridley) K. Schum, Annona senegalensis Pers. and Mondia whitei (Hook. f.) Skeels. Am. J. Lab. Med. 2017;2:52–59. doi: 10.11648/j.ajlm.20170204.13. [DOI] [Google Scholar]
- 61.Nkoto L.C., Bongo N.G., Kapepula M.P., Masengo A.C., Gbolo Z.B., Tshiama C., Ngombe N.K., Bekomo J.I., Mbemba T.F., Mpiana P.T. Microscopic features and chromatographic fingerprints of selected congolese medicinal plants: Aframomum alboviolaceum (Ridley) K. Schum, Annona senegalensis Pers. And Mondia whitei (Hook. f.) Skeels. Emer. Life Sci. Res. 2018;4:1–10. [Google Scholar]
- 62.Djeussi D.E., Noumedem J.A., Seukep J.A., Fankam A.G., Voukeng I.K., Tankeo S.B., Nkuete A.H., Kuete V. Antibacterial activities of selected edible plants extracts against multidrug-resistant Gram-negative bacteria. BMC Complement. Alt. Med. 2013;13:164. doi: 10.1186/1472-6882-13-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Olagoke O.O., Amusat M.A. GC/MS Analysis and evaluation of antimicrobial performance of Aframomum latifolium leaf essential oil from South West Nigeria. Int. J. Trend Sci. Res. Dev. 2019;4:189–191. [Google Scholar]
- 64.Essien E.E., Newby J.S., Walker T.M., Setzer W.N., Ekundayo O. Characterization and antimicrobial activity of volatile constituents from fresh fruits of Alchornea cordifolia and Canthium subcordatum. Medicines. 2015;3:1. doi: 10.3390/medicines3010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Noundou X.S., Krause R.W.M., Van Vuuren S.F., Ndinteh D., Olivier D.K. Antibacterial effects of Alchornea cordifolia (Schumach. and Thonn.) Müll. Arg extracts and compounds on gastrointestinal, skin, respiratory and urinary tract pathogens. J. Ethnopharmacol. 2016;179:76–82. doi: 10.1016/j.jep.2015.12.043. [DOI] [PubMed] [Google Scholar]
- 66.Keay R.W.J. Trees of Nigeria. Oxford Press; London, UK: 1989. [Google Scholar]
- 67.Manga H.M., Brkic D., Marie D.E.P., Quetin-Leclercq J. In vivo anti-inflammatory activity of Alchornea cordifolia (Schumach. & Thonn.) Müll. Arg.(Euphorbiaceae) J. Ethnopharmacol. 2004;92:209–214. doi: 10.1016/j.jep.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 68.Bayor M.T., Ansah C., Duwiejua M., Abaitey A.K. Alchornea Cordifolia (Euphorbiaceae), the Major Constituent of Antiasthmatic Herbal Formulations in Ghana, Stimulates β-adrenoceptors. J. Ghana Sci. Ass. 2008;10:1–11. doi: 10.4314/jgsa.v10i2.18025. [DOI] [Google Scholar]
- 69.Ansah C., Oppong E., Woode E. Subacute oral toxicity assessment of Alchornea cordifolia (Schumach and Thonn) Müll Arg (Euphorbiaceae) extract in rats. Trop. J. Pharm. Res. 2011;10:587–594. doi: 10.4314/tjpr.v10i5.7. [DOI] [Google Scholar]
- 70.Akoto C.O., Acheampong A., Boakye Y.D., Akwata D., Okine M. In vitro anthelminthic, antimicrobial and antioxidant activities and FTIR analysis of extracts of Alchornea cordifolia leaves. J. Pharm. Phytochem. 2019;8:2432–2442. [Google Scholar]
- 71.Agbor G.A., Léopold T., Jeanne N.Y. The antidiarrhoeal activity of Alchornea cordifolia leaf extract. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2004;18:873–876. doi: 10.1002/ptr.1446. [DOI] [PubMed] [Google Scholar]
- 72.Mavar-Manga H., Haddad M., Pieters L., Baccelli C., Penge A., Quetin-Leclercq J. Anti-inflammatory compounds from leaves and root bark of Alchornea cordifolia (Schumach. & Thonn.) Müll. Arg. J. Ethnopharmacol. 2008;115:25–29. doi: 10.1016/j.jep.2007.08.043. [DOI] [PubMed] [Google Scholar]
- 73.Mohammed R.K., Ibrahim S., Atawodi S.E., Eze E.D., Suleiman J.B., Malgwi I.S. Anti-diabetic and haematological effects of n-butanol fraction of Alchornea cordifolia leaf extract in streptozotocin-induced diabetic wistar rats. Sci. J. Biol. Sci. 2013;2:45–53. [Google Scholar]
- 74.Jacob J.M., Olaleye M.T., Olugbuyiro J.A.O. Hepatoprotective effect of Alchornea cordifolia leaf on liver damage in albino rats. Int. J. Appl. Sci. Biotechnol. 2014;2:217–221. doi: 10.3126/ijasbt.v2i2.10473. [DOI] [Google Scholar]
- 75.Odimegwu D.C., Okoye F.B.C., Nworu S.C., Esimone C.C. Anti-respiratory syncytial virus activities of leaf extracts of Alchornea cordifolia and Alchornea floribunda. Afr. J. Pharm. Pharmacol. 2018;12:97–105. [Google Scholar]
- 76.Ajali U. Antibacterial activity of Alchornea cordifolia stem bark. Fitoterapia. 2000;71:436–438. doi: 10.1016/S0367-326X(00)00131-3. [DOI] [PubMed] [Google Scholar]
- 77.Adeshina G.O., Onaolapo J.A., Ehinmidu J.O., Odama L.E. Phytochemical and antimicrobial studies of the ethyl acetate extract of Alchornea cordifolia leaf found in Abuja, Nigeria. J. Med. Plants Res. 2010;4:649–658. [Google Scholar]
- 78.Joseph N., Sorel N.E.M., Kasali F.M., Emmanuel M.M. Phytochemical screening and antibacterial properties from extract of Alchornea cordifolia (Schumach. &Thonn.) Müll. Arg. J. Pharm. Phytochem. 2015;4:176–180. [Google Scholar]
- 79.Boniface P.K., Ferreira S.B., Kaiser C.R. Recent trends in phytochemistry, ethnobotany and pharmacological significance of Alchornea cordifolia (Schumach. & Thonn.) Muell. Arg. J. Ethnopharmacol. 2016;191:216–244. doi: 10.1016/j.jep.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 80.Metowogo K., Agbonon A., Eklu-Gadegbeku K., Aklikokou A.K., Gbeassor M. Anti-ulcer and anti-inflammatory effects of hydroalcohol extract of Aloe buettneri A. Berger (Lilliaceae) Trop. J. Pharm. Res. 2008;7:907–912. doi: 10.4314/tjpr.v7i1.14676. [DOI] [Google Scholar]
- 81.Kombate B., Metowogo K., Kantati Y.T., Afanyibo Y.G., Fankibe N., Halatoko A.W., Yao S.A., Eklu-Gadegbeku K., Aklikokou K.A. Phytochemical screening, antimicrobial and antioxidant activities of Aloe buettneri, Mitracarpus scaber and Hannoa undulata used in Togolese Cosmetopoeia. J. Drug Deliv. Ther. 2022;12:19–24. doi: 10.22270/jddt.v12i2-S.5409. [DOI] [Google Scholar]
- 82.Metowogo K., Eklu-Gadegbeku K., Agbonon A., Aklikokou K.A., Gbeassor M. Gastroprotective effect of hydroalcoholic extract of Aloe buettneri. Iran. J. Pharm. Res. IJPR. 2011;10:69. [PMC free article] [PubMed] [Google Scholar]
- 83.Kossi M., Amégnona A., Messanvi G., Kwashie E.G. Antioxidant and gastric antisecretory properties of hydoalcoholic extract of Aloe buettneri A. Berger (Lilliaceae) [(accessed on 22 April 2024)];Pharm. Méd. Trad. Afr. 2012 16 Available online: http://publication.lecames.org. [Google Scholar]
- 84.Daglia M. Polyphenols as antimicrobial agents. Curr. Opin. Biotechnol. 2012;23:174–181. doi: 10.1016/j.copbio.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 85.Bouarab Chibane L., Degraeve P., Ferhout H., Bouajila J., Oulahal N. Plant antimicrobial polyphenols as potential natural food preservatives. J. Sci. Food Agric. 2019;99:1457–1474. doi: 10.1002/jsfa.9357. [DOI] [PubMed] [Google Scholar]
- 86.O’Rourke A., Beyhan S., Choi Y., Morales P., Chan A.P., Espinoza J.L., Dupont C.L., Meyer K.J., Spoering A., Lewis K., et al. Mechanism-of-action classification of antibiotics by global transcriptome profiling. Antimicrob. Agents Chemother. 2020;64:e01207-19. doi: 10.1128/AAC.01207-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Quílez A.M., Fernández-Arche M.A., García-Giménez M.D., De la Puerta R. Potential therapeutic applications of the genus Annona: Local and traditional uses and pharmacology. J. Ethnopharmacol. 2018;225:244–270. doi: 10.1016/j.jep.2018.06.014. [DOI] [PubMed] [Google Scholar]
- 88.Aziz A., Taha H., Ismail N.H., Yusof F.Z.M., Bakar M.Z.A. Therapeutic potential of plant species derived from some Annonaceae genus. Int. J. Agric. For. 2016;6:214–221. [Google Scholar]
- 89.Simo M.K., Nguepi M.D., Sameza M.L., Toghueo R.K., Fekam F.B., Froldi G. Cameroonian medicinal plants belonging to Annonaceae family: Radical scavenging and antifungal activities. Nat. Prod. Res. 2018;32:2092–2095. doi: 10.1080/14786419.2017.1363753. [DOI] [PubMed] [Google Scholar]
- 90.Formagio A.S.N., Vieira M.C., Volobuff C.R.F., Silva M.S., Matos A.I., Cardoso C.A.L., Foglio M.A., Carvalho J.E. In vitro biological screening of the anticholinesterase and antiproliferative activities of medicinal plants belonging to Annonaceae. Braz. J. Med. Biol. Res. 2015;48:308–315. doi: 10.1590/1414-431x20144127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Maroyi A. Annona stenophylla Engl. & Diels: Review of its botany, medicinal uses and biological activities. J. Pharm. Sci. Res. 2019;11:3385–3390. [Google Scholar]
- 92.Munodawafa T. Master’s Dissertation. University of Zimbabwe; Harare, Zimbabwe: 2008. Screening of Some Traditional Medicinal Plants from Zimbabwe for Biological and Antimicrobial Activity. [Google Scholar]
- 93.Awodele O., Amagon K.I., Agbo J., Prasad M.N.V. Toxicological evaluation of the aqueous stem bark extract of (Euphorbiaceae) in rodents. Interdis. Toxicol. 2015;8:89–98. doi: 10.1515/intox-2015-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Magassouba F.B., Diallo A., Kouyaté M., Mara F., Mara O., Bangoura O., Camara A., Traoré S., Diallo A.K., Zaoro M., et al. Ethnobotanical survey and antibacterial activity of some plants used in Guinean traditional medicine. J. Ethnopharmacol. 2007;114:44–53. doi: 10.1016/j.jep.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 95.Olajide O.A., Makinde J.M., Okpako D.T., Awe S.O. Studies on the anti-inflammatory and related pharmacological properties of the aqueous extract of Bridelia ferruginea stem bark. J. Ethnopharmacol. 2000;71:153–160. doi: 10.1016/S0378-8741(99)00201-9. [DOI] [PubMed] [Google Scholar]
- 96.Olajide O.A., Okpako D.T., Makinde J.M. Anti-inflammatory properties of Bridelia ferruginea stem bark Inhibition of lipopolysaccaride-induced septic shock and vascular permeability. J. Ethnopharmacol. 2003;88:221–224. doi: 10.1016/S0378-8741(03)00219-8. [DOI] [PubMed] [Google Scholar]
- 97.Akuodor G.C., Mbah C.C., Anyalewechi N.A., Idris-Usman M., Iwuanyanwu T.C., Osunkwo U.A. Pharmacological profile of aqueous extract of Bridelia ferruginea stem bark in the relief of pain and fever. J. Med. Plants Res. 2011;5:5366–5369. [Google Scholar]
- 98.Mbah C.C., Akuodor G.C., Anyalewechi N.A., Iwuanyanwu T.C., Osunkwo U.A. In vivo antiplasmodial activities of aqueous extract of Bridelia ferruginea stem bark against Plasmodium berghei berghei in mice. Pharm. Biol. 2012;50:188–194. doi: 10.3109/13880209.2011.592537. [DOI] [PubMed] [Google Scholar]
- 99.Oloyede O., Ekiti A., Ojo O.A., Onikanni S., Basiru A. In-vitro antioxidant activities of the stem bark extract fractions of Bridelia ferruginea. J. Biol. Agric. Healthc. 2014;4:1–7. [Google Scholar]
- 100.Adebayo O.A., Joshua O.B. Evaluation of anthelmintic potential of aqueous extract of the stem bark of Bridelia ferruginea (benth) euphorbiaceae. J. Pharmaceut. Res. Int. 2018;24:1–6. doi: 10.9734/JPRI/2018/28940. [DOI] [Google Scholar]
- 101.Onyenibe N.S., Udogadi N.S. Evaluation of antidiabetic role of Bridelia ferruginea methanol leaf extract in streptozocin induced diabetic male wistar rats. Pharm. Pharmacol. Int. J. 2019;7:264–269. [Google Scholar]
- 102.Dada E.O., Akinyele B.T. In-vivo anti-typhoid activities of ethanol stem bark extract of Bridelia ferruginea (wild) in albino rats infected with Salmonella typhi. J. Adv. Med. Pharm. Sci. 2020;22:10–20. doi: 10.9734/jamps/2020/v22i530170. [DOI] [Google Scholar]
- 103.Abubakar L., Bagna E.A., Dogarai B.B.S. Effects of column fractions on the leaves extract of Bridelia ferruginea on bacteria. Bayero J. Pure Appl. Sci. 2017;10:137–141. doi: 10.4314/bajopas.v10i1.28S. [DOI] [Google Scholar]
- 104.Afolayan M., Srivedavyasasri R., Asekun O.T., Familoni O.B., Ross S.A. Chemical and biological studies on Bridelia ferruginea grown in Nigeria. Nat. Prod. Res. 2019;33:287–291. doi: 10.1080/14786419.2018.1440225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Irobi O.N., Moo-Young M., Anderson W.A., Daramola S.O. Antimicrobial activity of bark extracts of Bridelia ferruginea (Euphorbiaceae) J. Ethnopharmacol. 1994;43:185–190. doi: 10.1016/0378-8741(94)90041-8. [DOI] [PubMed] [Google Scholar]
- 106.Koudou J., Abena A.A., Ngaissona P., Bessière J.M. Chemical composition and pharmacological activity of essential oil of Canarium schweinfurthii. Fitoterapia. 2005;76:700–703. doi: 10.1016/j.fitote.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 107.Yousuf S., Kamdem R.S.T., Wafo P., Ngadjui B.T., Fun H.K. A cocrystal of 3α-hydroxytirucalla-8, 24-dien-21-oic acid and 3β-fluorotirucalla-7, 24-dien-21-oic acid (0.897:0.103) Acta Crystallogr. Sect. E Struct. Rep. Online. 2011;67:o1015–o1016. doi: 10.1107/S1600536811011159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kuete V. Medicinal Spices and Vegetables from Africa. Academic Press; Cambridge, MA, USA: 2017. Canarium schweinfurthii; pp. 379–384. [DOI] [Google Scholar]
- 109.Sokoudjou J.B., Atolani O., Njateng G.S.S., Khan A., Tagousop C.N., Bitombo A.N., Kodjio N., Gatsing D. Isolation, characterization and in vitro anti-salmonellal activity of compounds from stem bark extract of Canarium schweinfurthii. BMC Complement. Med. Ther. 2020;20:316. doi: 10.1186/s12906-020-03100-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Obame L.C., Koudou J., Kumulungui B.S., Bassolé I.H., Edou P., Ouattara A.S., Traoré A.S. Antioxidant and antimicrobial activities of Canarium schweinfurt6hii Engl. Essential oil from Centrafrican Republic. Afr. J. Biotechnol. 2007;6:2319–2323. doi: 10.5897/AJB2007.000-2363. [DOI] [Google Scholar]
- 111.Ngameni B., Fotso G.W., Kamga J., Ambassa P., Abdou T., Fankam A.G., Voukeng I.K., Ngadjui B.T., Abegaz B.M., Kuete V. Medicinal Plant Research in Africa. Elsevier; Amsterdam, The Netherlands: 2013. Flavonoids and related compounds from the medicinal plants of Africa; pp. 301–350. [DOI] [Google Scholar]
- 112.Poumale H.M.P., Hamm R., Zang Y., Shiono Y., Kuete V. Medicinal Plant Research in Africa. Elsevier; Amsterdam, The Netherlands: 2013. Coumarins and related compounds from the medicinal plants of Africa; pp. 261–300. [DOI] [Google Scholar]
- 113.Wansi J.D., Devkota K.P., Tshikalange E., Kuete V. Medicinal Plant Research in Africa. Elsevier; Amsterdam, The Netherlands: 2013. Alkaloids from the medicinal plants of Africa; pp. 557–605. [DOI] [Google Scholar]
- 114.Dzotam J.K., Touani F.K., Kuete V. Antibacterial activities of the methanol extracts of Canarium schweinfurthii and four other Cameroonian dietary plants against multi-drug resistant Gram-negative bacteria. Saudi J. Boil. Sci. 2016;23:565–570. doi: 10.1016/j.sjbs.2015.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nagawa C., Böhmdorfer S., Rosenau T. Chemical composition and anti-termitic activity of essential oil from Canarium schweinfurthii Engl. Ind. Crop. Prod. 2015;71:75–79. doi: 10.1016/j.indcrop.2015.03.078. [DOI] [Google Scholar]
- 116.Buitrago D., Velasco J., Díaz T., Morales A. Chemical composition and antibacterial activity of the essential oil of Monticalia Imbricatifolia Schultz (Asteraceae) Rev. Latinoam. Química. 2012;40:13–18. [Google Scholar]
- 117.Krist S., Banovac D., Tabanca N., Wedge D.E., Gochev V.K., Wanner J., Schmidt E., Jirovetz L. Antimicrobial activity of nerolidol and its derivatives against airborne microbes and further biological activities. Nat. Prod. Comm. 2015;10:1934578X1501000133. doi: 10.1177/1934578X1501000133. [DOI] [PubMed] [Google Scholar]
- 118.Zaibet W., Laouer H., Amira S., Flamini G., Ramdani M., Akkal S. Chemical composition and biological activities of Daucus aureus essential oils from eastern Algeria. J. Chil. Chem. Soc. 2015;60:2722–2728. doi: 10.4067/S0717-97072015000400017. [DOI] [Google Scholar]
- 119.Guimarães A.C., Meireles L.M., Lemos M.F., Guimarães M.C.C., Endringer D.C., Fronza M., Scherer R. Antibacterial activity of terpenes and terpenoids present in essential oils. Molecules. 2019;24:2471. doi: 10.3390/molecules24132471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Julaeha E., Herlina T., Nurzaman M., Mayanti T., Kurnia D., Sari E. The antibacterial effect of β-pinene derived from Citrus aurantifolia peel against oral Streptococcus mutans ATCC 25175. Padjadjaran J. Dent. 2021;33:88–93. doi: 10.24198/pjd.vol33no1.29200. [DOI] [Google Scholar]
- 121.Tiji S., Rokni Y., Benayad O., Laaraj N., Asehraou A., Mimouni M. Chemical composition related to antimicrobial activity of Moroccan Nigella sativa L. extracts and isolated fractions. Evid. Complement. Alt. Med. 2021;2021:8308050. doi: 10.1155/2021/8308050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Brandes A., Dunning M., Langland J. Antimicrobial activity of individual volatile compounds from various essential oils. Molecules. 2024;29:1811. doi: 10.3390/molecules29081811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zachariades C., Strathie L.W., Retief E., Dube N. Progress towards the biological control of Chromolaena odorata (L.) RM King & H. Rob.(Asteraceae) in South Africa. Afr. Entomol. 2011;19:282–302. [Google Scholar]
- 124.Omokhua A.G., McGaw L.J., Chukwujekwu J.C., Finnie J.F., Van Staden J. A comparison of the antimicrobial activity and in vitro toxicity of a medicinally useful biotype of invasive Chromolaena odorata (Asteraceae) with a biotype not used in traditional medicine. S. Afr. J. Bot. 2017;108:200–208. doi: 10.1016/j.sajb.2016.10.017. [DOI] [Google Scholar]
- 125.Vijayaraghavan K., Ali S.M., Maruthi R. Studies on phytochemical screening and antioxidant activity of Chromolaena odorata and Annona squamosa. Int. J. Innov. Res. Sci. Eng. Technol. 2013;2:2319–8753. [Google Scholar]
- 126.Omokhua A.G., McGaw L.J., Finnie J.F., Van Staden J. Chromolaena odorata (L.) RM King & H. Rob.(Asteraceae) in sub-Saharan Africa: A synthesis and review of its medicinal potential. J. Ethnopharmacol. 2016;183:112–122. doi: 10.1016/j.jep.2015.04.057. [DOI] [PubMed] [Google Scholar]
- 127.Panda D., Dash S.K., Dash G.K. Qualitative phytochemical analysis and investigation of anthelmintic and wound healing potentials of various extracts of Chromolaena odorata Linn. collected from the locality of Mohuda village, Berhampur (South Odisha) Int. J. Pharm. Sci. Res. 2010;1:122–126. [Google Scholar]
- 128.Anyasor G.N., Aina D.A., Olushola M., Aniyikaye A.F. Phytochemical constituent, proximate analysis, antioxidant, antibacterial and wound healing properties of leaf extracts of Chromolaena odorata. Ann. Biol. Res. 2011;2:441–451. [Google Scholar]
- 129.Lavanya G., Brahmaprakash G.P. Ph.D. Dissertation. University of Agricultural Sciences; Bangalore, Karnataka State, India: 2010. Phytochemical Screening and Antimicrobial Activity of Compounds from Selected Medicinal and Aromatic Plants. [Google Scholar]
- 130.Atindehou M., Lagnika L., Guérold B., Strub J.M., Zhao M., Van Dorsselaer A., Marchioni E., Prévost G., Haikel Y., Taddéi C., et al. Isolation and identification of two antibacterial agents from Chromolaena odorata L. active against four diarrheal strains. Adv. Microbiol. 2013;3:115–121. doi: 10.4236/aim.2013.31018. [DOI] [Google Scholar]
- 131.Nganso Y.O.D., Tchana E.M.S., Kahouo A.D., Abah K., Fomena H., Mamoudou H. Inhibitory effect and antimicrobial activity of secondary metabolites of Khaya senegalensis (Desr.) A. Juss.(Meliaceae) Sci. J. Chem. 2020;10:81–94. [Google Scholar]
- 132.Shehu Isah T.U., Akande J. Antimalarial and antibacterial properties of some selected species of Asteraceae family. Int. J. Novel Res. Phy. Chem. Math. 2023;10:20–35. [Google Scholar]
- 133.Kil H.Y., Seong E.S., Ghimire B.K., Chung I.M., Kwon S.S. Antioxidant and antimicrobial activities of crude sorghum extract. Food Chem. 2009;115:1234–1239. doi: 10.1016/j.foodchem.2009.01.032. [DOI] [Google Scholar]
- 134.AL-Habib A., AL-Saleh E., Safer A., Afzal M. Bactericidal effects of grape seed extracts on methicillin resistant Staphylococcus aureus (MRSA) J. Toxicol. Sci. 2010;35:357–364. doi: 10.2131/jts.35.357. [DOI] [PubMed] [Google Scholar]
- 135.Kumar K.A., Narayani M., Subanthini A., Jayakumar M. Antimicrobial activity and phytochemical analysis of citrus fruit peels-utilization of fruit waste. Int. J. Eng. Sci. Tech. 2011;3:5414–5421. [Google Scholar]
- 136.Souza J.G., Toledo A.G., Santana C.B., Santos C.V., Mallmann A.P. Chemical composition and antibacterial activity of essential oil and leaf extracts of Zanthoxylum caribaeum Lam. against serotypes of Salmonella. Rev. Bras. Saude Prod. Anim. 2017;18:446–453. doi: 10.1590/s1519-99402017000300005. [DOI] [Google Scholar]
- 137.Wang J.H., Luan F., He X.D., Wang Y., Li M.X. Traditional uses and pharmacological properties of Clerodendrum phytochemicals. J. Trad. Complement. Med. 2018;8:24–38. doi: 10.1016/j.jtcme.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Gbedema S.Y., Emelia K., Francis A., Kofi A., Eric W. Wound healing properties and kill kinetics of Clerodendron splendens G. Don, a Ghanaian wound healing plant. Pharm. Res. 2010;2:63. doi: 10.4103/0974-8490.62948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Fleischer T.C., Mensah A.Y., Oppong A.B., Mensah M.L.K., Dickson R.A., Annan K. Antimicrobial and anti-inflammatory activities of the leaves of Clerodendrum splendens leaves. Pharm. Commun. 2011;1:85–89. [Google Scholar]
- 140.Shehata A.H., Yousif M.F., Soliman G.A. Phytochemical and pharmacological investigations of Clerodendron splendens G. Don growing in Egypt. Egypt. J. Biomed. Sci. 2001;7:145–163. [Google Scholar]
- 141.Gossan D.P.A., Magid A.A., Yao-Kouassi P.A., Josse J., Gangloff S.C., Morjani H., Voutquenne-Nazabadioko L. Antibacterial and cytotoxic triterpenoids from the roots of Combretum racemosum. Fitoterapia. 2016;110:89–95. doi: 10.1016/j.fitote.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 142.Kola K.A., Benjamin A.E. Comparative antimicrobial activities of the leaves of Combretum micranthum and C. racemosum. Glob. J. Med. Sci. 2002;1:13–17. [Google Scholar]
- 143.de Morais Lima G.R., De Sales I.R.P., Caldas Filho M.R.D., De Jesus N.Z.T., de Sousa Falcão H., Barbosa-Filho J.M., Cabral A.G.S., Souto A.L., Tavares J.F., Batista L.M. Bioactivities of the genus Combretum (Combretaceae): A review. Molecules. 2012;17:9142–9206. doi: 10.3390/molecules17089142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mgbemena I.C. Screening of Ethanol extract of Combretum racemosum and Euphorbia hirta leaves for possible activity on Trypanosoma brucei brucei infected mice. Sch. Acad. J. Biosci. 2016;4:725–731. [Google Scholar]
- 145.Wande O.M., Babatunde S.B. In vitro screening of ten Combretaceae plants for antimalarial activities applying the inhibition of beta-hematin formation. Int. J. Biol. Chem. Sci. 2017;11:2971–2981. doi: 10.4314/ijbcs.v11i6.33. [DOI] [Google Scholar]
- 146.Eze J.I., Anosa G.N., Ozota C.A. In vitro and in vivo trypanocidal activity of Combretum racemosum leaves. Afr. J. Biotechnol. 2012;11:10611–10616. [Google Scholar]
- 147.Manga F.N., El Khattabi C., Fontaine J., Berkenboom G., Duez P., Nzunzu J.L., Pochet S. Vascular effects and antioxidant activity of two Combretum species from Democratic Republic of Congo. J. Ethnopharmacol. 2012;142:194–200. doi: 10.1016/j.jep.2012.04.039. [DOI] [PubMed] [Google Scholar]
- 148.Schepetkin I.A., Kouakou K., Yapi A., Kirpotina L.N., Jutila M.A., Quinn M.T. Immunomodulatory and hemagglutinating activities of acidic polysaccharides isolated from Combretum racemosum. Int. Immunopharmacol. 2013;15:628–637. doi: 10.1016/j.intimp.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Babatunde S., Moyinoluwa O., Oluwatosin A., Eigege W., Shreyans J.K. Bioguided isolation of an antioxidant compound from Combretum racemosum P. Beav leaf. Int. J. Biol. Chem. Sci. 2014;8:2339–2346. doi: 10.4314/ijbcs.v8i5.36. [DOI] [Google Scholar]
- 150.Sautour M., Mitaine-Offer A.C., Miyamoto T., Dongmo A., Lacaille-Dubois M.A. Antifungal steroid saponins from Dioscorea cayenensis. Planta Medica. 2004;70:90–92. doi: 10.1055/s-2004-815467. [DOI] [PubMed] [Google Scholar]
- 151.Kumar S., Das G., Shin H.S., Patra J.K. Dioscorea spp. (a wild edible tuber): A study on its ethnopharmacological potential and traditional use by the local people of Similipal Biosphere Reserve, India. Front. Pharmacol. 2017;8:52. doi: 10.3389/fphar.2017.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Obidiegwu J.E., Lyons J.B., Chilaka C.A. The Dioscorea Genus (Yam)—An appraisal of nutritional and therapeutic potentials. Foods. 2020;9:1304. doi: 10.3390/foods9091304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ngelinkoto P.M., Lokassa A.M.K., Bulumuka B., Maliani J.K., Ngondo M.M., Mbuli R.L., Mukoko J.B., Mukeba F.B. Phytochemical study and anti-nutritional factors in stems of Dioscorea praehensilis Benth (Dioscoreaceae) J. Bot. Res. 2021;3:1–10. doi: 10.30564/jbr.v3i4.3455. [DOI] [Google Scholar]
- 154.Bein E., Habte B., Jaber A., Birnie A., Tengnas B. Useful trees and shrubs useful trees and shrubs in Eritrea: Identification, propagation and management for agricultural and pastoral communities. Regional Soil Conservation Unit, Nairobi. Am. J. Plant Sci. 1996;12:422. [Google Scholar]
- 155.Machumi F., Bojase-Moleta G., Mapitse R., Masesane I., Majinda R.R. Radical scavenging-flavonoids from Erythrina abysinica. Nat. Prod. Comm. 2006;1:287–292. [Google Scholar]
- 156.Mukaratirwa-Muchanyereyi N., Gusha C., Mujuru M., Guyo U., Nyoni S. Synthesis of silver nanoparticles using plant extracts from Erythrina abyssinica aerial parts and assessment of their anti-bacterial and anti-oxidant activities. Res. Chem. 2022;4:100402. [Google Scholar]
- 157.Olila D., Bukenya-Ziraba R., Kamoga D. Bio-prospective studies on medicinal plants used in the treatment of poultry diseases in Uganda. Res. J. Pharmacol. 2007;1:56–60. [Google Scholar]
- 158.Bekalo T.H., Woodmatas S.D., Woldemariam Z.A. An ethnobotanical study of medicinal plants used by local people in the lowlands of Konta Special Woreda, Southern nations, nationalities and peoples regional state, Ethiopia. J. Ethnobiol. Ethnomed. 2009;5:26. doi: 10.1186/1746-4269-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Gakuubi M., Wanzala W. A survey of plants and plant products traditionally used in livestock health management in Buuri district, Meru County, Kenya. J. Ethnobiol. Ethnomed. 2012;8:39. doi: 10.1186/1746-4269-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Lagu C., Kayanja F.I.B. A Bird’s-Eye View of Veterinary Medicine. IntechOpen; London, UK: 2012. In vitro antimicrobial activity of crude extracts of Erythrina abyssinica and Capsicum annum in poultry diseases control in the South western agroecological zone of Uganda; pp. 597–614. [DOI] [Google Scholar]
- 161.Lagu C., Kayanja F.I.B. Insights from Veterinary Medicine. IntechOpen; London, UK: 2013. The in vitro antihelminthic efficacy of Erythrina abyssinica extracts on Ascaridia galli; pp. 269–281. [DOI] [Google Scholar]
- 162.Bunalema L., Kirimuhuzya C., Tabuti J.R.S., Waako P., Magadula J.J., Otieno N., Orodho J.A., Okemo P. The efficacy of the crude root bark extracts of Erythrina abyssinica on rifampicin resistant Mycobacterium tuberculosis. Afr. Health Sci. 2011;11:587–593. [PMC free article] [PubMed] [Google Scholar]
- 163.Manyarara T., Chifamba J., Tarugarira F. Antifungal activity of Ziziphus mucronata and Erythrina abyssinica bark crude ex-tracts on Cryptococcus neofomans and Candida albicans species. Br. J. Pharm. Res. 2016;10:1–11. doi: 10.9734/BJPR/2016/23843. [DOI] [Google Scholar]
- 164.Musyoka T.M., Nyamai D.W., Arika W.M., Juma K.K., Nzioka M.D., Maina D., Waithaka S.K., Ngugi M.P., Orinda G.O., Karau G.M., et al. In vivo antianaemic effect and safety of aqueous extracts of Erythrina abyssinica and Zanthoxylum usambarensis in mice models. J. Hematol. Rom. Dis. 2016;4:1000242. [Google Scholar]
- 165.Mosisa G. Master’s Thesis. Jimma University; Jimma, Ethiopia: 2017. Evaluation of Stem Bark of Erythrina abyssinica for Antimicrobial and Termiticidal Principles. [Google Scholar]
- 166.Obakiro S.B., Kiprop A., Kigondu E., K’Owino I., Odero M.P., Manyim S., Omara T., Namukobe J., Owor R.O., Ga-vamukulya Y., et al. Traditional medicinal Uses, phytoconstituents, bioactivities, and toxicities of Erythrina abyssinica Lam. ex DC.(fabaceae): A systematic review. Evid. Based Complement. Alt. Med. 2021;2021:513484. doi: 10.1155/2021/5513484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Irungu S. Master’s Thesis. Kenyatta University; Nairobi, Kenya: 2012. Isolation and Characterization of Antimicrobial Compounds from the Plants Erythrina abyssinica DC. and Chasmanthera Dependens Hochst. [Google Scholar]
- 168.Chitopoa W., Muchachaa I., Mangoyi R. Evaluation of the antimicrobial activity of Erythrina abyssinica leaf extract. J. Microbiol. Biochem. Technol. 2019;11:413 [Google Scholar]
- 169.Wagate C.G., Mbaria J.M., Gakuya D.W., Nanyingi M.O., Kareru P.G., Njuguna A., Gitahi N., Macharia J.K., Njonge F.K. Screening of some Kenyan medicinal plants for antibacterial activity. Phyther. Res. Int. J. Dev. Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2010;24:150–153. doi: 10.1002/ptr.2866. [DOI] [PubMed] [Google Scholar]
- 170.Ochung A. Ph.D. Thesis. Maseno University; Kisumu, Kenya: 2016. Phytochemical Investigations of Lonchocarpus eriocalyx (Harms), Alysicarpus ovalifolius (Schumach) and Erythrina abyssinica (DC) for Antiplasmodial, Larvicidal, Mosquitocidal and Antimicrobial Activities. [Google Scholar]
- 171.Korir K., Bii C., Kiiyukia C., Mutai C. Antimicrobial activities of Clutia abyssinic and Erythrina abyssinica plants extracts used among the Kipsigis community of Bomet district in Kenya. Nat. Prod. 2011;7:247–252. [Google Scholar]
- 172.Mongrand S., Badoc A., Patouille B., Lacomblez C., Chavent M., Bessoule J.J. Chemotaxonomy of the Rubiaceae family basedon leaf fatty acid composition. Phytochemistry. 2005;66:549–559. doi: 10.1016/j.phytochem.2004.12.021. [DOI] [PubMed] [Google Scholar]
- 173.Karou S.D., Tchacondo T., Djikpo Tchibozo M.A., Abdoul-Rahaman S., Anani K., Koudouvo K., Batawila K., Agbonon A., Simpore J., de Souza C. Ethnobotanical study of medicinal plants used in the management of diabetes mellitus and hypertension in the Central Region of Togo. Pharm. Boil. 2011;49:1286–1297. doi: 10.3109/13880209.2011.621959. [DOI] [PubMed] [Google Scholar]
- 174.Maroyi A.A. Gardenia ternifolia Schum. & Thonn.(Rubiaceae): Review of medicinal uses, phytochemistry and biological activities. Int. J. Res. Pharm. Sci. 2020;11:5876–5885. [Google Scholar]
- 175.Traore M.S., Baldé M.A., Diallo M.S.T., Baldé E.S., Diané S., Camara A., Diallo A., Balde A., Keïta A., Keita S.M., et al. Ethnobotanical survey on medicinal plants used by Guinean traditional healers in the treatment of malaria. J. Ethnopharm. 2013;150:1145–1153. doi: 10.1016/j.jep.2013.10.048. [DOI] [PubMed] [Google Scholar]
- 176.Baldé A.M., Traoré M.S., Diallo M.S.T., Vlietinck A., Pieters L. Ethnobotanical survey, antimicrobial and anticomplement activities of Guinean medicinal plants traditionally used in the treatment of inflammatory diseases in Conakry and Dubreka. J. Plant Sci. 2015;3:11–19. [Google Scholar]
- 177.Dahiru Y.Y.D. Effect of aqueous leaves extract of Gardenia ternifolia plant on carbon tetrachloride-induced hepatotoxicity in rats. IOSR J. Pharm. Biol. Sci. 2015;10:73–82. [Google Scholar]
- 178.Mpiana P.T., Ngbolua K.T.N., Tshibangu D., Mwanangombo D.T., Tsalu P.V. Sickle Cell Desease: Genetics, Managements and Prognosis. NOVA; Hauppauge, NY, USA: 2015. Antisickling and radical scavenging activities of anthocyanin extracts from the leaves of Gardenia ternifolia subsp. Jovis-Tonantis (Welw.) Verdc.(Rubiaceae) pp. 61–77. [Google Scholar]
- 179.Holaly G.E., Simplice K.D., Charlemagne G., Kodjovi A., Kokou A., Tchadjobo T., Amegnona A., Komlan B., Jacques S. Ethnobotanical study of plants used in the treatment of diabetes in the traditional medicine of Maritime Region, Togo. Pan Afr. Med. J. 2015;20:437. doi: 10.11604/pamj.2015.20.437.5660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Roger T., Pierre-Marie M., Igor V.K. Phytochemical screening and antibacterial activity of medicinal plants used to treat typhoid fever in Bamboutos division, West Cameroon. J. Appl. Pharm. Sci. 2015;5:034–049. doi: 10.7324/JAPS.2015.50606. [DOI] [Google Scholar]
- 181.Farah H.M., El Amin T.H., Khalid H.S., Hassan S.M., El Hussein A.R.M. In vitro activity of the aqueous extract of Gardenia ternifolia fruits against Theileria lestoquardi. J. Med. Plants Res. 2012;6:5447–5451. [Google Scholar]
- 182.Ngbolua K.N., Mihigo S.O., Liyongo C.I., Ashande M.C., Tshibangu D.S.T., Zoawe B.G., Baholy R., Fatiany P.R., Mpiana P.T. Ethno-botanical survey of plant species used in traditional medicine in Kinshasa city (Democratic Republic of the Congo) Trop. Plant Res. 2016;3:413–427. [Google Scholar]
- 183.Tshibangu D.S., Divakar S., Ramanathan M., Syamala G.G., Ngbolua K.N., Mudogo V., Tshilanda D.D., Gbolo B.Z., Mpiana P. In vitro screening of the leaf extracts from Gardenia ternifolia (Forest Gardenia) for their anticancer activity. J. Complement. Altern. Med. Res. 2016;1:1–7. doi: 10.9734/JOCAMR/2016/28348. [DOI] [Google Scholar]
- 184.Nureye D., Assefa S., Nedi T., Engidawork E. In vivo antimalarial activity of the 80 methanolic root bark extract and solvent fractions of Gardenia ternifolia Schumach. & Thonn.(Rubiaceae) against Plasmodium berghei. Evid. Based Complement. Alt. Med. 2018;2018:9217835. doi: 10.1155/2018/9217835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Bernard D., Hassana Y., Djaouda M., Mathieu M., Romeo W.B., Benoît K., Wahab A.T. Antibacterial effects of a new triterpenoid saponin from roots of Gardenia ternifolia Schumach. & Thonn (Rubiaceae) Res. Chem. 2022;4:100366. [Google Scholar]
- 186.Ghosh B., Mukherjee S., Jha T.B., Jha S. Enhanced colchicine production in root cultures of Gloriosa superba by direct and indirect precursors of the biosynthetic pathway. Biotechnol. Lett. 2002;24:231–234. doi: 10.1023/A:1014129225583. [DOI] [Google Scholar]
- 187.Singh A.K. Flower Crops: Cultivation and Management. New India Publishing; Delhi, India: 2006. [(accessed on 29 April 2024)]. Available online: https://books.google.com. [Google Scholar]
- 188.Sensarma P., Pal D.C., Naya P., Bakshi D.N.G., editors. A Lexicon of Medicinal Plants in India. Naya Prokash; Calcutta, India: 2001. pp. 86–187. ISBN 10: 8185421692/ISBN 13: 9788185421698. [Google Scholar]
- 189.Sivakumar G. Gloriosa superba La very useful medicinal plant. [(accessed on 13 May 2024)];Ethnomed. Pharm. 2002 7:465–482. Available online: https://cir.nii.ac.jp/crid/1570572700706835200. [Google Scholar]
- 190.Megala S., Elango R. Bioactive compounds analysis tuber and seed of Gloriosa superba GC–MS method. Int. J. Rec. Sci. Res. 2012;3:871–873. [Google Scholar]
- 191.Nadkarni A.K. Mumbai: Bombay Popular Prakashan. Volume 1. Popular Prakashan Pvt Ltd.; Mumbai, India: 1976. Indian materia medica; pp. 165–166. [Google Scholar]
- 192.Budhiraja A., Nepali K., Kaul S., Dhar K.L. Antimicrobial and cytotoxic activities of fungal isolates of medicinal plant Gloriosa superba. Int. J. Recent Adv. Pharm. Res. 2012;2:37–45. [Google Scholar]
- 193.Mustefa I., Endale M., Eswaramoorthy R. Antibacterial and antioxidant compounds from root extracts of Gloriosa superba Linn: A combined experimental and computational study. Ethiop. J. Sci. Sust. Dev. 2024;11:98–113. [Google Scholar]
- 194.Longo F., Fogue S.K., Dimo T. Vasodilatory effects of aqueous extract from Harungana madagascariensis stem bark in isolated rat aorta: The roles of endothelium and K+ channels. Am. J. Ethnomed. 2018;5:8. [Google Scholar]
- 195.Moulari B., Pellequer Y., Lboutounne H., Girard C., Chaumont J.P., Millet J., Muyard F. Isolation and in vitro antibacterial activity of astilbin, the bioactive flavanone from the leaves of Harungana madagascariensis Lam. ex Poir.(Hypericaceae) J. Ethnopharmacol. 2006;106:272–278. doi: 10.1016/j.jep.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 196.Happi G.M., Tiani G.L.M., Gbetnkom B.Y.M., Hussain H., Green I.R., Ngadjui B.T., Kouam S.F. Phytochemistry and pharmacology of Harungana madagascariensis: Mini review. Phytochem. Lett. 2020;35:103–112. doi: 10.1016/j.phytol.2019.11.015. [DOI] [Google Scholar]
- 197.Asogwa F.C., Apebende C.G., Ugodi G.W., Ebo P., Louis H., Ikeuba A.I., Asogwa C.J., Gber T.E., Ikot I.J., Owen A.E. Anti-inflammatory, immunomodulatory and DFT evaluation of the reactivity indexes of phytochemicals isolated from Harungana madagascariensis. Chem. Afr. 2023;6:1349–1361. doi: 10.1007/s42250-022-00569-0. [DOI] [Google Scholar]
- 198.Iwalewa E.O., Suleiman M.M., Mdee L.K., Eloff J.N. Antifungal and antibacterial activities of different extracts of Harungana madagascariensis stem bark. Pharm. Biol. 2009;47:878–885. doi: 10.1080/13880200903029316. [DOI] [Google Scholar]
- 199.Mawunu M., Garcia Z., Manuel S.P., Pedro N.J.C., Mampasi N., Guillame N.M., Ngbolua K.N., Ndiku L., Luyeye L. Biodiversity and ethnobotany of medicinal plants of the small Songo City, Angola. J. Qual. Healthc. Eco. 2022;5:000290. doi: 10.23880/jqhe-16000290. [DOI] [Google Scholar]
- 200.Tankeo S.B., Damen F., Sandjo L.P., Celik I., Tane P., Kuete V. Antibacterial activities of the methanol extracts, fractions and compounds from Harungana madagascariensis Lam. ex Poir.(Hypericaceae) J. Ethnopharm. 2016;190:100–105. doi: 10.1016/j.jep.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 201.Shimbe R.Y., Tor-Anyiin T.A., Khan M.E., Anyam J.V. β-sitosterol from Hymenocardia acida root extract and its antimicrobial activity. [(accessed on 20 May 2024)];J. Chem. Soc. Nig. 2016 41:76–81. Available online: https://www.journals.chemsociety.org.ng/index.php/jcsn/article/view/51. [Google Scholar]
- 202.Abu A.H., Uchendu C.N. Effect of aqueous ethanolic extract of Hymenocardia acida stem bark on oestrous cycle of albino rats. J. Med. Plants Res. 2011;5:1280–1283. [Google Scholar]
- 203.Shimbe R.Y., Tor-Anyiin T.A. Phytochemical and antibacterial studies of Hymenocardia acida roots. J. Chem. Soc. Nig. 2014;39:119–122. [Google Scholar]
- 204.Vonthron-Sénécheau C., Weniger B., Ouattara M., Bi F.T., Kamenan A., Lobstein A., Brun R., Anton R. In vitro antiplasmodial activity and cytotoxicity of ethnobotanically selected Ivorian plants. J. Ethnopharm. 2003;87:221–225. doi: 10.1016/S0378-8741(03)00144-2. [DOI] [PubMed] [Google Scholar]
- 205.Hoet S., Opperdoes F., Brun R., Adjakidjé V., Quetin-Leclercq J. In vitro antitrypanosomal activity of ethnopharmacologically selected Beninese plants. J. Ethnopharm. 2004;91:37–42. doi: 10.1016/j.jep.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 206.Starks C.M., Williams R.B., Norman V.L., Rice S.M., O’Neil-Johnson M., Lawrence J.A., Eldridge G.R. Antibacterial chromene and chromane stilbenoids from Hymenocardia acida. Phytochemistry. 2024;98:216–222. doi: 10.1016/j.phytochem.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 207.Agbidye I.G., Msughter A.Q., Chinelo N.J., Iortyom S.D. Phytochemical screening and antimicrobial analysis of Hymenocardia acida. Chem. Res. J. 2020;5:81–93. [Google Scholar]
- 208.Mølgaard P., Nielsen S.B., Rasmussen D.E., Drummond R.B., Makaza N., Andreassen J. Anthelmintic screening of Zimbabwean plants traditionally used against schistosomiasis. J. Ethnopharm. 2001;74:257–264. doi: 10.1016/S0378-8741(00)00377-9. [DOI] [PubMed] [Google Scholar]
- 209.Amusan O.O., Dlamini P.S., Msonthi J.D., Makhubu L.P. Some herbal remedies from Manzini region of Swaziland. J. Ethnopharmacol. 2002;79:109–112. doi: 10.1016/S0378-8741(01)00381-6. [DOI] [PubMed] [Google Scholar]
- 210.Kritzinger Q. Ph.D. Thesis. University of Pretoria; Pretoria, South Africa: 2005. Antimicrobial Activity and Fumonisins Associated with Cowpea (Vigna unguiculata) [Google Scholar]
- 211.Maroyi A. Medicinal uses, biological and chemical properties of wild grape (Lannea edulis): An indigenous fruit plant of Tropical Africa. Asian J. Pharm. Clin. Res. 2019;12:16–20. doi: 10.22159/ajpcr.2019.v12i9.34580. [DOI] [Google Scholar]
- 212.Christenhusz M.J., Byng J.W. The number of known plants species in the world and its annual increase. Phytotaxa. 2016;261:201–217. doi: 10.11646/phytotaxa.261.3.1. [DOI] [Google Scholar]
- 213.Sigidi M.T. Ph.D. Thesis. University of Venda; Thohoyandou, South Africa: 2017. Selection and Evaluation of Ten Medicinal Plants Used in the Vembe District for Life-Threatening Infections. [Google Scholar]
- 214.Magwede K., Van Wyk B.E., Van Wyk A.E. An inventory of Vhavenḓa useful plants. S. Afr. J. Bot. 2019;122:57–89. doi: 10.1016/j.sajb.2017.12.013. [DOI] [Google Scholar]
- 215.Malú Q., Caldeira G.I., Catarino L., Indjai B., da Silva I.M., Lima B., Silva O. Ethnomedicinal, chemical, and biological aspects of Lannea species—A Review. Plants. 2024;13:690. doi: 10.3390/plants13050690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sohni Y.R., Davis C.L., Deschamps A.B., Kale P.G. Frameshift mutations in Salmonella induced by the extracts of medicinal herbs Lannea edulis (Sond.) Engl. and Monotes glaber Sprague. Environ. Mol. Mut. 1995;25:77–82. doi: 10.1002/em.2850250111. [DOI] [PubMed] [Google Scholar]
- 217.Queiroz E.F., Kuhl C., Terreaux C., Mavi S., Hostettmann K. New Dihydroalkylhexenones from Lannea edulis. J. Nat. Prod. 2003;66:578–580. doi: 10.1021/np0202428. [DOI] [PubMed] [Google Scholar]
- 218.Munodawafa T., Chagonda L.S., Moyo S.R. Antimicrobial and phytochemical screening of some Zimbabwean medicinal plants. J. Biol. Act. Prod. Nat. 2013;3:323–330. doi: 10.1080/22311866.2013.782759. [DOI] [Google Scholar]
- 219.Chivengwa C., Mandimutsira T., Gere J., Magogo C., Chikanza I., Vidmar J., Chingwaru W. Inhibition of Escherichia coli and Salmonella spp. by Traditional Phytomedicines That Are Commonly Used to Treat Gastroenteritis in Zimbabwe. Int. J. Pharmacol. Pharm. Sci. 2016;3:1. [Google Scholar]
- 220.Banda M. Master’s Dissertation. University of Zambia; Lusaka, Zambia: 2018. Assessing the Anti-Hyperglycemic and Antihyperlipidemic Effects of an Aqueous Extract of Lanne aedulis in Alloxan-Induced Diabetic Rats. [Google Scholar]
- 221.Banda M., Nyirenda J., Muzandu K., Sijumbila G., Mudenda S. Antihyperglycemic and antihyperlipidemic effects of aqueous extracts of Lanne aedulis in alloxan-induced diabetic rats. Front. Pharmacol. 2018;9:1099. doi: 10.3389/fphar.2018.01099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Gelfand M., Drummond R.B., Mavi S., Ndemera B. The Traditional Medical Practitioner in Zimbabwe: His Principles of Practice and Pharmacopoeia. Vol. 17. Mambo Press; Gweru, Zimbabwe: 1985. [(accessed on 27 May 2024)]. pp. 345–346. Available online: https://lccn.loc.gov/86980486. [Google Scholar]
- 223.Wyk B.E., Gericke N. People’s Plants: A Guide to Useful Plants of Southern Africa. Briza Publications; Pretoria, South Africa: 2007. [(accessed on 3 June 2024)]. Available online: https://www.cabidigitallibrary.org. [Google Scholar]
- 224.Minja M.M. Medicinal plants used in the promotion of animal health in Tanzania. Rev. Sci. Tech. (Int. Off. Epizoot.) 1994;13:905–925. doi: 10.20506/rst.13.3.800. [DOI] [PubMed] [Google Scholar]
- 225.Oladimeji F.A., Orafidiya L.O., Okeke I.N. Physical properties and antimicrobial activities of leaf essential oil of Lippia multiflora Moldenke. Int. J. Aromather. 2004;14:162–168. doi: 10.1016/j.ijat.2004.09.011. [DOI] [Google Scholar]
- 226.Samba N., Aitfella-Lahlou R., Nelo M., Silva L., Coca R., Rocha P., Lopez Rodilla J.M. Chemical composition and antibacterial activity of Lippia multiflora Moldenke essential oil from different regions of Angola. Molecules. 2020;26:155. doi: 10.3390/molecules26010155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Oladimeji F.A., Orafidiya O.O., Ogunniyi T.A.B., Adewunmi T.A. Pediculocidal and scabicidal properties of Lippia multiflora essential oil. J. Ethnopharmacol. 2000;72:305–311. doi: 10.1016/S0378-8741(00)00229-4. [DOI] [PubMed] [Google Scholar]
- 228.Abena A.A., Atipo-Ebata J.K., Diatewa M. Psychopharmacological properties of crude extract and essential oil of Lippia multiflora. L’encephale. 2001;27:360–364. [PubMed] [Google Scholar]
- 229.Abena A.A., Diatewa M., Gakosso G., Gbeassor M., Hondi-Assah T.H., Ouamba J.M. Analgesic, antipyretic and anti-inflammatory effects of essential oil of Lippia multiflora. Fitoterapia. 2003;74:231–236. doi: 10.1016/S0367-326X(03)00029-7. [DOI] [PubMed] [Google Scholar]
- 230.Kunle O., Okogun J., Egamana E., Emojevwe E., Shok M. Antimicrobial activity of various extracts and carvacrol from Lippia multiflora leaf extract. Phytomedicine. 2003;10:59–61. doi: 10.1078/094471103321648674. [DOI] [PubMed] [Google Scholar]
- 231.Adewole K.E., Attah A.F., Adebayo J.O. Morinda lucida Benth (Rubiaceae): A review of its ethnomedicine, phytochemistry and pharmacology. J. Ethnopharm. 2021;276:114055. doi: 10.1016/j.jep.2021.114055. [DOI] [PubMed] [Google Scholar]
- 232.Oladeji O.S., Oluyori A.P., Dada A.O. Antiplasmodial activity of Morinda lucida Benth. Leaf and bark extracts against Plasmodium berghei infected mice. Saudi J. Biol. Sci. 2022;29:2475–2482. doi: 10.1016/j.sjbs.2021.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Ogunlana O.E., Ogunlana O., Farombi O.E. Morinda lucida: Antioxidant and reducing activities of crude methanolic stem bark extract. Adv. Nat. Appl. Sci. 2008;2:49–54. [Google Scholar]
- 234.Lawal H.O., Etatuvie S.O., Fawehinmi A.B. Ethnomedicinal and pharmacological properties of Morinda lucida. J. Nat. Prod. 2012;5:93–99. [Google Scholar]
- 235.Zimudzi C., Gwenhure L.F., Kunonga N., Kativu S., Jere J. Phytochemical screening, cytotoxicity and anti-inflammatory activities of the Zimbabwean endemic plant Phyllanthus serpentinicola Radcl.-Sm.(Phyllanthaceae) J. Appl. Pharm. Sci. 2012;2:050–053. doi: 10.7324/JAPS.2012.21010. [DOI] [Google Scholar]
- 236.Oladeji O.S., Oyebamiji A.K. Stellaria media (L.) Vill.—A plant with immense therapeutic potentials: Phytochemistry and pharmacology. Heliyon. 2020;6:e04150. doi: 10.1016/j.heliyon.2020.e04150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Kazeem M.I., Adamson J.O., Ogunwande I.A. Modes of inhibition of a-amylase and a-glucosidase by aqueous extract of Morinda lucida Benth. leaf. BioMed Res. Int. 2013;2013:1–6. doi: 10.1155/2013/527570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Bata M.M., Adeshina G.O., Onaolapo J.A., Musa A.M., Mshelia E.H., Salihu M.S., Muammar D.L., Sadam A.A., Dauda G. Antibacterial Activity of A and Β Amyrin Isolated from Morinda lucida Against Some Multidrug Resistant Enterobacteriaceae. 2023. [(accessed on 10 June 2024)]. Available online: https://ssrn.com/abstract=4627522.
- 239.Okwu D.E., Uchenna N.F. Exotic multifaceted medicinal plants of drugs and pharmaceutical industries. Afr. J. Biotechnol. 2019;8:7271–7282. [Google Scholar]
- 240.Ayeleso A.O., Oguntibeju O.O., Brooks N.L. In vitro study on the antioxidant potentials of the leaves and fruits of Nauclea latifolia. Sci. World J. 2014;2014:437081. doi: 10.1155/2014/437081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Boucherle B., Haudecoeur R., Queiroz E.F., De Waard M., Wolfender J.L., Robins R.J., Boumendjel A. Nauclea latifolia: Biological activity and alkaloid phytochemistry of a West African tree. Nat. Prod. Rep. 2016;33:1034–1043. doi: 10.1039/C6NP00039H. [DOI] [PubMed] [Google Scholar]
- 242.Iheagwam F.N., Israel E.N., Kayode K.O., DeCampos O.C., Ogunlana O.O., Chinedu S.N. Nauclea latifolia Sm. Leaf extracts extenuates free radicals, inflammation, and diabetes-linked enzymes. Oxid. Med. Cell. Long. 2020;2020:5612486. doi: 10.1155/2020/5612486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Chabi-Sika K., Sina H., Boya B., Mama-Sirou I., Kpangon L., Salami H.A., Kelomey A., Roko G., Assogba S.A., Adoko M.Y., et al. Phytochemical Screening and antimicrobial Activity of Sarcocephalus latifolius Smith roots extracts. Biotechnol. J. Int. 2022;26:54–62. doi: 10.9734/bji/2022/v26i6665. [DOI] [Google Scholar]
- 244.Rodrigues A.P., Pastore G.M. A review of the nutritional composition and current applications of Monguba (Pachira aquatica Aubl.) plant. J. Food Comp. Anal. 2021;99:103878. doi: 10.1016/j.jfca.2021.103878. [DOI] [Google Scholar]
- 245.Whesu O.A., Ogunbamowo P.O., Bankole S.O., Awotedu O.L., Oyediran R.I. Antibacterial activity and chemical profiling of Bombax glabrum (Pasq.) A. Robyns leaves. J. Med. Herbs. 2021;12:57–65. [Google Scholar]
- 246.Gamal El-Din M.I., Youssef F.S., Ashour M.L., Eldahshan O.A., Singab A.N.B. Comparative analysis of volatile constituents of Pachira aquatica Aubl. and Pachira glabra Pasq., their antimycobacterial and antihelicobacter pylori activities and their metabolic discrimination using chemometrics. J. Essent. Oil Bear. Plants. 2018;21:1550–1567. doi: 10.1080/0972060X.2019.1571950. [DOI] [Google Scholar]
- 247.Rodrigues A.P., Pereira G.A., Tomé P.H.F., Arruda H.S., Eberlin M.N., Pastore G.M. Chemical composition and antioxidant activity of Monguba (Pachira aquatica) seeds. Food Res. Int. 2019;121:880–887. doi: 10.1016/j.foodres.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 248.El-Din M.I.G., Youssef F.S., Ashour M.L., Eldahshan O.A., Singab A.N.B. New γ-pyrone glycoside from Pachira glabra and assessment of its gastroprotective activity using an alcohol-induced gastric ulcer model in rats. Food Funct. 2020;11:1958–1965. doi: 10.1039/C9FO02800E. [DOI] [PubMed] [Google Scholar]
- 249.Lawal O.A., Ogunwande I.A., Salvador A.F., Sanni A.A., Opoku A.R. Pachira glabra Pasq. Essential oil: Chemical constituents, antimicrobial and insecticidal activities. J. Oleo Sci. 2014;63:629–635. doi: 10.5650/jos.ess13179. [DOI] [PubMed] [Google Scholar]
- 250.Makosa M., Sithole S., Mukanganyama S. Evaluation of the antimicrobial effect of the extracts of the pods of Piliostigma thonningii (schumach.) milne-redh.(Fabaceae) Adv. Pharmacol. Pharm. Sci. 2021;2021:6616133. doi: 10.1155/2021/6616133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Ighodaro O.M., Agunbiade S.O., Omole J.O., Kuti O.A. Evaluation of the chemical, nutritional, antimicrobial and antioxidant-vitamin profiles of Piliostigma thonningii leaves. Res. J. Med. Plant. 2012;6:537–543. doi: 10.3923/rjmp.2012.537.543. [DOI] [Google Scholar]
- 252.Asuzu I.U., Gray A.I., Waterman P.G. The anthelmintic activity of D-3-O-methylchiroinositol isolated from Piliostigma thonningii stem bark. Fitoterapia. 1999;70:77–79. doi: 10.1016/S0367-326X(98)00006-9. [DOI] [Google Scholar]
- 253.Ibewuike J.C., Ogungbamila F.O., Ogundaini A.O., Okeke I.N., Bohlin L. Anti-inflammatory and antibacterial activities of C-methylflavonols from Piliostigma thonningii. Phytother. Res. 1997;11:281–284. doi: 10.1002/(SICI)1099-1573(199706)11:4<281::AID-PTR281>3.0.CO;2-9. [DOI] [Google Scholar]
- 254.Marquardt P., Vissiennon C., Schubert A., Birkemeyer C., Ahyi V., Fester K. Phytochemical analysis, in vitro anti-inflammatory and antimicrobial activity of Piliostigma thonningii leaf extracts from Benin. Planta Medica. 2020;86:1269–1277. doi: 10.1055/a-1229-4565. [DOI] [PubMed] [Google Scholar]
- 255.Akinpelu D.A., Kolawole D.O. Phytochemistry and antimicrobial activity of leaf extract of Piliostigma thonningii (Schum.) Sci. Focus. 2004;7:64–70. [Google Scholar]
- 256.Roersch C.M. Piper umbellatum L.: A comparative cross-cultural analysis of its medicinal uses and an ethnopharmacological evaluation. J. Ethnopharm. 2010;131:522–537. doi: 10.1016/j.jep.2010.07.045. [DOI] [PubMed] [Google Scholar]
- 257.Arunachalam K., Damazo A.S., Macho A., da Silva Lima J.C., Pavan E., de Freitas Figueiredo F., Oliveira D.M., Cechinel-Filho V., Wagner T.M., de Oliveira Martins D.T. Piper umbellatum L.(Piperaceae): Phytochemical profiles of the hydroethanolic leaf extract and intestinal anti-inflammatory mechanisms on 2, 4, 6 trinitrobenzene sulfonic acid induced ulcerative colitis in rats. J. Ethnopharmacol. 2020;254:112707. doi: 10.1016/j.jep.2020.112707. [DOI] [PubMed] [Google Scholar]
- 258.Agbor G.A., Vinson J.A., Sortino J., Johnson R. Antioxidant and anti-atherogenic activities of three Piper species on atherogenic diet fed hamsters. Exp. Toxicol. Pathol. 2012;64:387–391. doi: 10.1016/j.etp.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 259.da Silva Jr I.F., de Oliveira R.G., Soares I.M., da Costa Alvim T., Ascêncio S.D., de Oliveira Martins D.T. Evaluation of acute toxicity, antibacterial activity, and mode of action of the hydroethanolic extract of Piper umbellatum L. J. Ethnopharm. 2014;151:137–143. doi: 10.1016/j.jep.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 260.Okunrobo L.O., Imafidon K.E., Uwaya J.O., Oloton E., Okebhagbe M.O. Phytochemical screening and antimicrobial evaluation of the methanol extract and fractions of the leaves of Piper umbellatum Linn (Piperaeceae) J. Pharm. Bioresour. 2011;8:123–128. doi: 10.4314/jpb.v8i2.9. [DOI] [Google Scholar]
- 261.Chase M.W., Christenhusz M.J., Fay M.F., Byng J.W., Judd W.S., Soltis D.E., Mabberley D.J., Sennikov A.N., Soltis P.S., Stevens P.F. An update of the Angiosperm Phylogeny Group classification for the orders and families of flowering plants: APG IV. Bot. J. Linn. Soc. 2016;181:1–20. [Google Scholar]
- 262.Asogwa F.C., Ibezim A., Ntie-Kang F., Asogwa C.J., Okoye C.O. Anti-psoriatic and immunomodulatory evaluation of Psorospermum febrifugum Spach and its phytochemicals. Sci. Afr. 2020;7:e00229. doi: 10.1016/j.sciaf.2019.e00229. [DOI] [Google Scholar]
- 263.Aumeeruddy M.Z., Mahomoodally M.F. Traditional herbal therapies for hypertension: A systematic review of global ethnobotanical field studies. S. Afr. J. Bot. 2020;135:451–464. doi: 10.1016/j.sajb.2020.09.008. [DOI] [Google Scholar]
- 264.Dzoyem J.P., Tchuenteu R.T., Mbarawa K., Keza A., Roland A., Njouendou A.J., Assob J.C.N. Ethnoveterinary Medicine: Present and Future Concepts. Springer; Cham, Switzerland: 2020. Ethnoveterinary medicine and medicinal plants used in the treatment of livestock diseases in Cameroon; pp. 175–209. [DOI] [Google Scholar]
- 265.Mollel J.T., Said J.S., Masalu R.J., Hannoun C., Mbunde M.V., Nondo R.S., Bergström T., Trybala E. Anti-respiratory syncytial virus and anti-herpes simplex virus activity of six Tanzanian medicinal plants with extended studies of Erythrina abyssinica stem bark. J. Ethnopharmacol. 2022;292:115204. doi: 10.1016/j.jep.2022.115204. [DOI] [PubMed] [Google Scholar]
- 266.Epifano F., Fiorito S., Genovese S. Phytochemistry and pharmacognosy of the genus Psorospermum. Phytochem. Rev. 2013;12:673–684. doi: 10.1007/s11101-013-9274-8. [DOI] [PubMed] [Google Scholar]
- 267.Olujimi O.O., Bamgbose O., Arowolo T., Steiner O., Goessler W. Elemental profiles of herbal plants commonly used for cancer therapy in Ogun State, Nigeria. Part I. Microchem. J. 2014;117:233–241. doi: 10.1016/j.microc.2014.06.022. [DOI] [Google Scholar]
- 268.Chinweze J.N., Abugu H.O., Okoye C.O.B. Antioxidant activity of Psorospermum febrifugum and Harungana madagascariensis (Hypericaceae) stem bark ethanolic extracts. J. Chem. Pharm. Res. 2020;12:50–59. [Google Scholar]
- 269.Moto F.C.O., Talla E., Taiwe G.S., Ngoupaye G.T. Anxiolytic-like Effects of the Decoction of Psorospermum febrifugum in Mice. Asian J. Pharm. Health Sci. 2013;3:607–614. [Google Scholar]
- 270.Tamokou J.D.D., Chouna J.R., Fischer-Fodor E., Chereches G., Barbos O., Damian G., Benedec D., Duma M., Efouet A.P.N., Wabo H.K., et al. Anticancer and antimicrobial activities of some antioxidant-rich Cameroonian medicinal plants. PLoS ONE. 2013;8:e55880. doi: 10.1371/journal.pone.0055880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Mpinda C., Meyer D., Lyantagaye S. In vitro antimicrobial activity of extracts of some plant species used in the management of HIV/AIDS in Tanzania. Tanzan. J. Sci. 2018;44:179–190. [Google Scholar]
- 272.Alain A., Hamidou C.F., Louise A., Aimée D.K.A.C., Witabouna K.M. Plants used in Côte d’Ivoire (West Africa) against ticks: Evaluation for acaricidal activity against Rhipicephalus (Boophilus) microplus. Vet. Parasitol. Reg. Stud. Rep. 2022;35:100780. doi: 10.1016/j.vprsr.2022.100780. [DOI] [PubMed] [Google Scholar]
- 273.Ajao A.A.N., Moteetee A.N. Psorospermum febrifugum Spach (Hypericaceae): Ethnomedicine, phytochemistry, and pharmacological activity of an underexplored plant. Sci. Afr. 2023;22:e01934. [Google Scholar]
- 274.Nambooze J. Ph.D. Dissertation. Makerere University; Kampala, Uganda: 2019. Isolation and Structural Elucidation of Antibacterial Triterpenoids Compounds from Stem Bark of Psorospermum febrifugum (Spach var. Febrifugum) [Google Scholar]
- 275.Kamsala R.V., Lepakshi B.M., Padma Y., Raju R.R.V. Studies on antimicrobial and antioxidant properties of leaf extracts of Syzygium alternifolium (Wt.) Walp. Int. J. Pharm. Pharm. Sci. 2015;7:139–143. [Google Scholar]
- 276.Chirchir D.K., Cheplogoi P.K., Omolo J.O. Chemical characterization of Syzygium guineense (Myrtaceae) stem bark extracts. J. Pharm. Phytochem. 2019;8:278–282. [Google Scholar]
- 277.Mavanza S.A., Omwenga G.I., Ngugi M.P. Antibacterial and phytochemical effects of ethanol extracts of Syzygium guineense (Willd.) DC barks and Mangifera indica L. seeds. J. Adv. Biotechnol. Exp. Ther. 2023;6:337–349. doi: 10.5455/jabet.2023.d130. [DOI] [Google Scholar]
- 278.Djoukeng J.D., Abou-Mansour E., Tabacchi R., Tapondjou A.L., Bouda H., Lontsi D. Antibacterial triterpenes from Syzygium guineense (Myrtaceae) J. Ethnopharm. 2005;101:283–286. doi: 10.1016/j.jep.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 279.Amo-Mensah J., Darko G., Borquaye L.S. Anti-inflammatory and antioxidant activities of the root and bark extracts of Vitex grandifolia (Verbanaceae) Sci. Afr. 2020;10:e00586. doi: 10.1016/j.sciaf.2020.e00586. [DOI] [Google Scholar]
- 280.Amah U.J., Okogeri O. Nutritional and phytochemical properties of Wild Black Plum (Vitex doniana) seed from Ebonyi state. Int. J. Hort. Agric. Food Sci. 2019;3:32–36. doi: 10.22161/ijhaf.3.1.5. [DOI] [Google Scholar]
- 281.Adjei S., Amponsah I.K., Bekoe S.O., Harley B.K., Mensah K.B., Mensah A.Y., Baah M.K., Fosu-Mensah G. Fruits of Vitex doniana sweet: Toxicity profile, anti-inflammatory and antioxidant activities, and quantification of one of its bioactive constituents oleanolic acid. Heliyon. 2021;7:e07910. doi: 10.1016/j.heliyon.2021.e07910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Kilani A.M. Antibacterial assessment of whole stem bark of Vitex doniana against some Enterobactriaceae. Afr. J. Biotechnol. 2006;5:958–959. [Google Scholar]
- 283.Eze E.A., Nwuche C.O., Ugwu A.M. In-vitro antibacterial activity of bioactive plant extracts against methicillin-resistant strains of Staphylococcus aureus. Bio-Research. 2009;7:441–445. doi: 10.4314/br.v7i1.45469. [DOI] [Google Scholar]
- 284.Nwachukwu E., Uzoeto H.O. Antimicrobial activities of leaf of Vitex doniana and Cajanus cajan on some bacteria. Researcher. 2010;2:37–47. [Google Scholar]
- 285.Osuagwu G.G.E., Eme C.F. The phytochemical composition and antimicrobial activity of Dialium guineense, Vitex doniana and Dennettia tripetala leaves. Asian J. Nat. Appl. Sci. 2013;2:69–81. [Google Scholar]
- 286.Ifeanacho M.O., Ogunwa S.C., Amadi P.U. Phytochemical composition of Vitex doniana. Anal. Chem. Lett. 2019;9:863–875. doi: 10.1080/22297928.2020.1722221. [DOI] [Google Scholar]
- 287.Sonibare O.O., Effiong I., Oladosu I.A., Ekundayo O. Chemical constituents and antimicrobial activity of the essential oil of Vitex doniana sweet (Verbernaceae) J. Essen. Oil Bear. Plants. 2009;12:185–188. doi: 10.1080/0972060X.2009.10643709. [DOI] [Google Scholar]
- 288.Owolabi M.S., Ogundajo L.A., Satyal P., Dosoky N.S., Abdulhakam W., Olubukola D.S.R., Setzer W.N. Vitex doniana L. growing in Southwestern Nigeria: Leaf essential oil composition and antimicrobial activity. Nat. Prod. Commun. 2022;17:1934578X221141777. doi: 10.1177/1934578X221141777. [DOI] [Google Scholar]
- 289.Plants of the World Online. 2024. [(accessed on 6 May 2024)]. Available online: https://powo.science.kew.org/
- 290.Plant List. 2024. [(accessed on 6 May 2024)]. Available online: http://www.plantlist.org.
- 291.World Flora Online (WFO) 2024. [(accessed on 6 May 2024)]. Available online: http://www.worldfloraonline.org/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.