Abstract
Background:
Health care systems are increasingly focused on assessing patient well-being and functioning. The objective of the current analysis was to evaluate a pragmatic question: to what extent and in what way can the PHQ-2, a routinely collected screening measure, be used to help clinicians and a learning health system understand the well-being and functioning of its beneficiaries?
Methods:
The current analysis focused on 2872 Veterans who completed a large-scale longitudinal survey about health and wellness for whom we were able to link survey responses to PHQ-2 scores recorded in their electronic health records (EHR). Regression analyses examined the cross-sectional and longitudinal associations between PHQ-2 scores recorded in the EHR and measures of well-being (life satisfaction, purpose in life, and social health) and functioning (pain severity and interference, physical and mental health, and perceived stress).
Results:
Veterans were aged 65 years on average (11% women). PHQ-2 scores were correlated cross-sectionally with all well-being and functioning measures; however, there was minimal variance accounted for. Changes in the PHQ-2 over time were associated with 3 measures: purpose in life (b = −0.19; 95% CI: −0.34, −0.04), mental health functioning (b = −0.29, 95% CI: −0.54, −0.04), and perceived stress (b = 0.13; 95% CI: 0.02, 0.24).
Conclusions:
The PHQ-2 was minimally associated with patient well-being and functioning, with more work needed on how the PHQ-2 may be used in large health care settings within the context of VA Whole Health. Assessment of well-being is critical as VA’s Whole Health transformation continues, and identifying strategies for well-being measurement is an integral next step.
Key Words: functioning, PHQ-2, Veterans, well-being, Whole Health
The Veterans Health Administration’s (VA) Whole Health System of Care (ie, VA Whole Health) aims to focus patient-provider conversations on “what matters most,” as opposed to “what is the matter with you.”1 This transformation in care delivery coincides with the National Academy of Sciences’2 call to ensure that Whole Health care focuses on optimizing the “physical, behavioral, spiritual, and socioeconomic well-being” of an individual. Although well-being may be defined in different ways,3 in the current research, we define well-being as the “positive state experienced by an individual and societies”4 that includes positive affect, meaning and purpose, and life satisfaction, among other constructs.5,6 Measuring disease-specific symptom severity is important; however, such assessments do not examine how these conditions are affecting functioning (defined in the current manuscript as how health negatively impacts an individual) or how they interfere with experiencing positive emotions (eg, well-being). However, asking health care systems to measure another dimension of patient experiences may be challenging due to time constraints and potential provider and patient burden, which may reduce feasibility.
Various screening measures are already being routinely used during clinical encounters to assess the potential need for patients to be evaluated for other common conditions, including depression, anxiety, and substance use disorders.7–10 Not only are such measures already administered to patients before many medical visits, but in most cases, they are also being integrated into patient electronic health records (EHRs), thereby allowing for easy individual-level and population-level assessment of scores over time. Such measures may, therefore, readily offer a way for health care systems to help capture information on how individuals may score on well-being and functioning; however, the relationship between clinical measures and well-being and functioning assessed in health care systems remains largely unknown.
One alternative to adopting new measures of well-being across health care systems is to utilize existing measures that are already routinely collected. The 2-item Patient Health Questionnaire (PHQ-211) is a psychometrically sound screening tool for depression and is used routinely to screen for depression in VA.9 In 2003, the PHQ-2 was developed from the legacy PHQ-9 assessment,12 and designed as an initial brief screening assessment for depression symptoms. The PHQ-2 has demonstrated good internal consistency,13 test-retest reliability,13 and major depressive disorder (MDD) diagnostic validity,14,15 and is responsive to changes in depression symptoms over time.16 Current US Preventative Services Task Force clinical practice guidelines include screening for depression symptoms in settings where appropriate follow-up can be provided if clinically indicated.17 The VA health care system is one such setting where patient assessment and subsequent follow-up are feasible, and VA clinical practice guidelines for MDD include annual screening for depression using the PHQ-2.9
Given the widespread use of the PHQ-2 within VA and its availability in the VA EHR, the PHQ-2 may be an efficient tool to help capture information on levels of Veteran well-being and functioning across the health care system. The PHQ-2 significantly correlates with the World Health Organization’s (WHO) 5-item well-being index,18 subjective well-being,19 and life satisfaction,20 suggesting that the PHQ-2 may help capture information on well-being when positive emotions are of interest. When the PHQ-2 was introduced, its validity in assessing deficits in functioning was also established.11 Its construct validity has been further established since then. In 2 samples of individuals with anxiety and/or depression, Staples et al13 reported strong correlations between the PHQ-2 and general psychological distress, and small to medium correlations with anxiety. The PHQ-2 also performs well when measuring physical functioning.18,21 Nevertheless, the PHQ-2, by design, focuses on mental distress symptoms (not well-being), and as such, its potential utility in informing levels of well-being assessed in large health care systems may be limited. The objective of the current exploratory analysis was to evaluate a pragmatic question: to what extent and in what way can the PHQ-2, a routinely collected screening measure, be used to help clinicians and a learning health system understand the well-being and functioning of its beneficiaries? To do so, we examined the PHQ-2 and its cross-sectional and longitudinal relationships between well-being (life satisfaction, purpose in life, and social health) and functioning (pain severity and interference, physical and mental health functioning, and perceived stress). Specifically, we expected that the PHQ-2 would be negatively associated with all well-being measures and physical and mental health functioning and positively associated with pain and perceived stress.
METHODS
Overview
Between 2018 and 2021, the VA conducted a longitudinal survey of patient-reported outcomes (the Veterans Health and Life Survey), which was administered to Veterans at 4 time points as part of a larger quality improvement evaluation focused on Whole Health.22 We linked this survey with PHQ-2 scores from the VA EHR collected as part of routine VA care. This linked data resource allowed us to examine the cross-sectional and longitudinal incremental validity of the PHQ-2 and its associations with 3 patient-reported well-being measures (ie, life satisfaction, purpose in life, and social health) and 4 measures of functioning (ie, pain severity and interference, physical and mental health functioning, and perceived stress).
Study Cohort
The current analysis focused on 2872 Veterans who responded to a baseline administration of the Veterans Health and Life Survey and for whom we were able to link PHQ-2 scores documented in the VA EHR within 3 months before or after their baseline survey completion (±90 days). We chose this timeframe based on both quantitative and theoretical reasons. Namely, ±90 days maximizes the number of Veterans in the sample, while scores closer to the time of assessment will likely be more clinically meaningful; clinicians may not have PHQ-2 scores available closer in time than the ±90-day timeframe; and PHQ-2 assessments were approximately evenly distributed within the ±90 days. The Veterans Health and Life Survey was originally designed to assess facets of well-being and functioning among individuals with chronic pain. This survey was conducted as part of a collaboration between VA’s Office of Patient Centered Care and Cultural Transformation (OPCC&CT), the operational office responsible for the diffusion of Whole Health care across the VA health care system, and the Quality Enhancement Research Initiative (QUERI), VA’s implementation arm of its Office of Research and Development (ORD).22
Survey data were collected from Veterans who received care at 1 of the 18 VA Whole Health pilot implementation sites. Because the larger quality improvement evaluation was designed to focus on Veterans with chronic pain who used VA Whole Health services, Veterans were sampled based on (1) having chronic pain, as documented in the EHR (wave 1 sampling: n=1803, 62.8%) or (2) having used VA Whole Health services (wave 2 sampling: n=1069, 37.2%). Additional information regarding data collection is detailed elsewhere.22 For the current analysis, we used baseline and 12-month surveys. A total of 9835 Veterans had valid survey baseline data (designated by answering at least 2 of the 3 pain severity and interference items), with 2872 Veterans having a valid PHQ-2 score documented in the EHR within 3 months before or after the date the baseline survey was returned. Of these 2872 Veterans, 836 also had a valid PHQ-2 score within 3 months before or after their 12-month survey date.
Measures
PHQ-2
The PHQ-2 was obtained from Veterans’ EHR, which is collected as part of routine care. The PHQ-2 is a 2-item depression screener that asks participants the degree to which they experience “Little interest or pleasure in doing things” and “Feeling down, depressed, or hopeless.” Participants rate the items on a 0 (“Not at all”) to 3 (“Nearly every day”) scale. Sum scores are calculated ranging from 0 to 6, and higher scores indicate more depressive symptoms.
Well-Being Measures
All 3 well-being measures were collected using the Veterans Health and Life Survey. (1) Life satisfaction was assessed using 1 item from Cantril’s Ladder.23 Participants indicated where on a ladder (0 “worst possible life” to 10 “best possible life”) they felt their life was currently (ie, “Indicate where on the ladder you feel you personally stand right now”). Higher scores indicate more life satisfaction. (2) Purpose in life was assessed using the Life Engagement Test.24 Participants responded to 6 items (eg, “There is not enough purpose in my life”) on a 5-point Likert scale (“strongly agree” to “strongly disagree”). Scores are summed, with higher scores indicating more purpose in life. (3) Social health was assessed using a modified version of the Medical Outcomes Study Social Support Survey, with the addition of 1 item related to financial support (a total of 8 items were used; eg, “During the last month, did you have someone to love and make you feel wanted”).25 Participants responded on a 5-point Likert scale (“none of the time” to “all of the time”). Scores are averaged, with higher scores indicating greater perceptions of social health.
Measures of Functioning
All 4 measures of functioning were collected using the Veterans Health and Life Survey. (4) Pain severity and interference were assessed using the 3-item pain intensity, interference with enjoyment of life, and interference with general activity scale (PEG26; eg, “What number best describes your pain on average in the past week”). Responses on the PEG items range from 0 to 10. Items are averaged, with higher scores indicating higher levels of pain severity and interference. (5) Physical and (6) mental health functioning were assessed using the 4-item PROMIS-physical health (PROMIS-PH; e.g., “In general, would you say your physical health is”) and mental health (PROMIS-MH; eg, “In general, how would you rate your mental health, including your mood and ability to think”), respectively.27 Participants responded on a 5-point Likert scale, and responses were transformed into T-scores, where 50 represents average functioning across populations, and 10 represents a standard deviation. Higher T-scores indicate higher physical and mental health functioning. (7) Perceived stress was assessed using the 4-item perceived stress scale (eg, “In the last month, how often have you felt that you were unable to control the important things in your life”).28 Participants responded on a 5-point Likert scale (“never” to “very often”). Scores are summed, with higher scores indicating more perceived stress.
Demographic and Health Characteristics
Age, sex, race, ethnicity, number of past-year chronic conditions (ie, Elixhauser comorbidity score29), and past-year diagnoses of chronic pain, PTSD, anxiety, and depression were extracted from EHR. Self-reported marital status, education, and length of chronic pain were collected as part of the Veterans Health and Life Survey.
Data Analyses
We first present sample characteristics of the entire cohort. We then present findings from cross-sectional linear regression analyses, which examined the associations between baseline PHQ-2 scores and each well-being and functioning measure at baseline, adjusting for baseline covariates (ie, age, sex, race, ethnicity, employment, relationship status, number of past-year medical conditions, and past-year chronic pain, anxiety, depression, and posttraumatic stress disorder), for the n = 2872 Veterans who had PHQ-2 scores associated with their baseline survey completion date. Finally, we present longitudinal linear regression analyses, in which we regressed changes in measures of well-being and functioning from baseline to 12 months on changes in PHQ-2 from baseline to 12 months, adjusting for all covariates. To account for missing 12-month data, we used multiple imputations via chained equations (MICE)30 to impute missing values. All variables used in the main linear regression analyses were included in the imputation models. We additionally included outcome variables captured at 6 months post-baseline as auxiliary variables. The final results were based on estimates from 100 imputed datasets combined.31 All regression and multiple imputation analyses were conducted using the R version 4.1.1.32 Because the sample was partially recruited based on chronic pain status, we performed a sensitivity analysis by including an interaction between chronic pain and the PHQ-2 in the regression models. Results showed that chronic pain did not moderate the associations between the PHQ-2 and measures of well-being and functioning. Therefore, we report the original multiple imputation analyses.
RESULTS
Demographic and Health Characteristics
Table 1 includes demographic and health characteristics. Our total sample consisted of 2872 Veterans, with an average age of 65 years (SD=12). Women Veterans accounted for 11% of the sample. Most Veterans were White (80%); 19% were Black or African American, and ≤1% were either American Indian or Alaska Native, Asian, or Native Hawaiian or Other Pacific Islander. Hispanic or Latino/a Veterans accounted for 4% of the sample.
TABLE 1.
Sample Characteristics
| Characteristic | N = 2872* |
|---|---|
| Age | 65 (12) |
| Sex, n (%) | |
| Female | 319 (11) |
| Male | 2553 (89) |
| Race, n (%) | |
| American Indian or Alaska Native | 17 (0.6) |
| Asian | 14 (0.5) |
| Black or African American | 514 (19) |
| Native Hawaiian or Other Pacific Islander | 17 (0.6) |
| White | 2203 (80) |
| Unknown | 107 |
| Ethnicity, n (%) | |
| Hispanic or Latino | 127 (4.4) |
| Not Hispanic or Latino | 2659 (93) |
| Unknown | 86 (3.0) |
| History of PTSD,† n (%) | 674 (23) |
| History of depression† | 349 (12) |
| History of anxiety† | 427 (15) |
| Marital status, n (%) | |
| Divorced | 683 (24) |
| Married or in a civil union | 1750 (61) |
| Single (never married or in a civil union) | 199 (7.0) |
| Separated | 95 (3.3) |
| Widowed | 126 (4.4) |
| Unknown | 19 |
| Count of chronic conditions‡ | 2.79 (1.95) |
| History of chronic pain,† n (%) | 1830 (64) |
| Employment status, n (%) | |
| Homemaker | 12 (0.4) |
| Multiple responses | 700 (25) |
| Not working and not looking for work | 71 (2.5) |
| Not working, but actively looking for work | 55 (1.9) |
| Retired | 781 (27) |
| Student in high school, job training, or college degree program | 11 (0.4) |
| Unable to work due to disability | 661 (23) |
| Working as a volunteer (no pay) | 29 (1.0) |
| Working for pay full-time (30+ h/wk) | 401 (14) |
| Working for pay part-time (<30 h/wk) | 122 (4.3) |
| Unknown | 29 |
| Length of chronic pain, n (%) | |
| Not at all | 59 (2.1) |
| <1 month | 26 (0.9) |
| 1–3 months | 57 (2.1) |
| 3–6 months | 69 (2.5) |
| 6 mo–1 y | 134 (4.8) |
| 1–5 y | 527 (19) |
| More than 5 y | 1901 (69) |
| Unknown | 99 |
Mean (SD); n (%).
Past-year diagnosis found in the electronic health record.
Elixhauser Comorbidity Index.
PHQ-2
Table 2 summarizes the PHQ-2 scores identified for this cohort. For the 2872 patients for whom we identified baseline PHQ-2 scores, the overall average PHQ-2 scores were 0.52 (SD=1.27). For the sample (n=836) of respondents for whom PHQ-2 scores were identified around the time of the baseline survey as well as the 12-month survey, PHQ-2 scores significantly improved over time [M=0.40; SD=1.12 at baseline and M=0.23; SD = 0.82 at 12-months; change = −0.17 (95% CI: 0.09, 0.25); Cohen’s d = −0.15]. PHQ-2 scores identified in the EHR had similar lengths of time in proximity to both the baseline Veterans Health and Life survey and the 12-month survey (baseline median = 45 days; 12-mo median = 47 days). Moreover, the average time between assessments was 384 days (SD=52 days), with a median of 371 days. Table 3 details the distribution of PHQ-2 scores at baseline and 12 months.
TABLE 2.
PHQ-2 and Patient-reported Outcomes Over Time
| Outcome* † | Baseline M (SD) |
12 mo M (SD) |
Change (95% CI) | P | Effect Size (Cohen’s d) |
|---|---|---|---|---|---|
| PHQ-2 (0‒6) | 0.40 (1.12) | 0.23 (0.82) | −0.17 (0.09, 0.25) | <0.001 | −0.15 |
| Well-being | |||||
| Life satisfaction (0‒10) | 6.37 (1.98) | 6.56 (1.93) | 0.18 (0.05, 0.30) | 0.005 | 0.09 |
| Purpose in life (6‒30) | 22.99 (4.62) | 22.71 (4.7) | −0.32 (−0.57, −0.06) | 0.015 | −0.07 |
| Social health (1–5) | 3.47 (1.20) | 3.47 (1.19) | −0.01 (−0.07, 0.05) | 0.721 | −0.01 |
| Functioning | |||||
| PEG Pain (0–10) | 6.17 (2.36) | 6.19 (2.31) | 0.01 (−0.12, 0.14) | 0.864 | 0.00 |
| PROMIS Physical Health Functioning‡ | 38.53 (7.77) | 38.39 (7.51) | −0.03 (−0.40, 0.33) | 0.857 | 0.00 |
| PROMIS Mental Health Functioning‡ | 43.43 (9.09) | 43.54 (9.05) | 0.27 (−0.14, 0.68) | 0.203 | 0.03 |
| Perceived Stress (4‒20) | 5.7 (3.17) | 5.56 (3.19) | −0.12 (−0.31, 0.07) | 0.205 | −0.04 |
Numbers in parentheses indicate the minimum to a maximum range of scale scores, with bolded numbers indicating the worst score.
Values in the table represent those with complete data at baseline and 12 months. Baseline values were as follows: life satisfaction: M=6.14 (SD=2.02); purpose in life: M=22.46 (SD=4.77); social health: M=3.37 (SD=1.17); PEG: M=6.39 (SD=2.34); physical health functioning: M=37.73 (SD=7.44); mental health functioning: M=41.81 (SD=9.36); perceived stress: M=6.14 (SD=3.27).
For PROMIS scales, 50 represents the population norm with lower scores indicating worse functioning and 10 representing 1 SD.
TABLE 3.
Distribution of PHQ-2 Scores at Baseline and 12 Months
| 12 Months | ||||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | Total | |
| Baseline, n (%) | ||||||||
| 0 | 651 (78) | 28 (3.3) | 12 (1.4) | 4 (0.5) | 3 (0.4) | 2 (0.2) | 3 (0.4) | 703 (84) |
| 1 | 30 (3.6) | 2 (0.2) | 3 (0.4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 35 (4.2) |
| 2 | 39 (4.7) | 7 (0.8) | 8 (1.0) | 0 (0) | 1 (0.1) | 1 (0.1) | 1 (0.1) | 57 (6.8) |
| 3 | 9 (1.1) | 1 (0.1) | 1 (0.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 11 (1.3) |
| 4 | 7 (0.8) | 1 (0.1) | 2 (0.2) | 0 (0) | 1 (0.1) | 0 (0) | 0 (0) | 11 (1.3) |
| 5 | 2 (0.2) | 0 (0) | 1 (0.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 3 (0.4) |
| 6 | 8 (1.0) | 1 (0.1) | 3 (0.4) | 1 (0.1) | 0 (0) | 0 (0) | 3 (0.4) | 16 (1.9) |
| Total | 746 (89) | 40 (4.8) | 30 (3.6) | 5 (0.6) | 5 (0.6) | 3 (0.4) | 7 (0.8) | 836 (100) |
Cross-sectional Associations Between PHQ-2 Scores, Well-Being, and Functioning
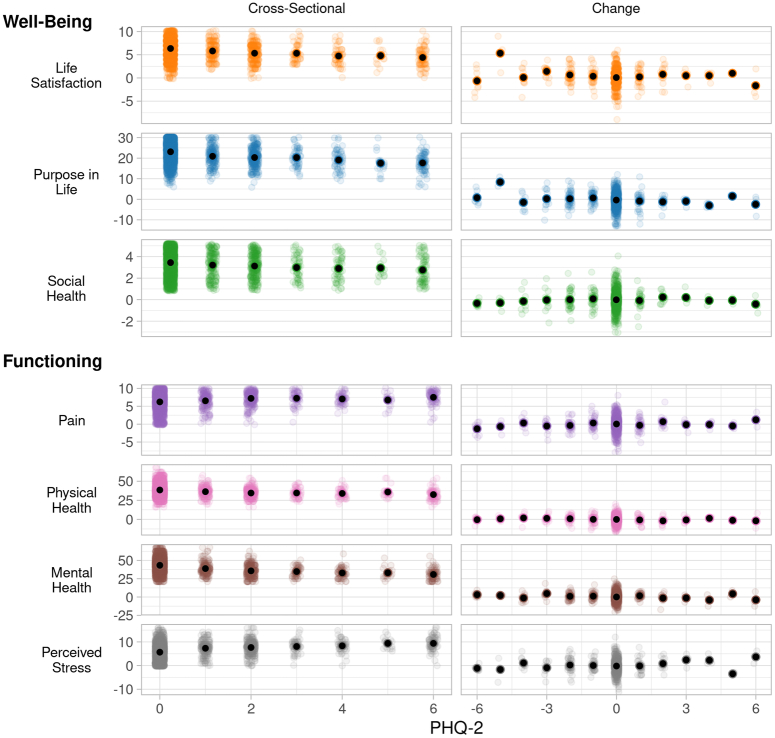
Table 4 summarizes cross-sectional and longitudinal associations of well-being and functioning measures, and Figure 1 shows the visual representation of the results. Higher levels of depressive symptoms were associated with lower levels of well-being, with variance accounted for by the PHQ-2 ranging from r 2 = 0.01 (social health) to r 2 = 0.04 (purpose in life). Similarly, more severe depressive symptoms were associated with poorer functioning across all measures, with variance accounted for by the PHQ-2 ranging from r 2 = 0.01 (pain severity and interference) to r 2 = 0.07 (mental health functioning).
TABLE 4.
Regression Estimates of the Associations of PHQ-2 Scores With Measures of Well-Being and Functioning
| Baseline associations (cross-sectional) | Associations between PHQ-2 mean change and mean change in outcomes (longitudinal) | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcome* | ||||||||
| Well-being | Beta | 95% CI | P | r † (model/PHQ-2) | Beta | 95% CI | P | r † (model/PHQ-2) |
| Life satisfaction (0‒10) | −0.26 | −0.32, −0.21 | <0.001 | 0.13/0.03 | −0.01 | −0.10, 0.07 | 0.808 | 0.01/0.00 |
| Purpose in life (6‒30) | −0.77 | −0.91, −0.64 | <0.001 | 0.14/0.04 | −0.19 | −0.34, −0.04 | 0.013 | 0.02/0.01 |
| Social health (1–5) | −0.09 | −0.13, −0.06 | <0.001 | 0.14/0.01 | 0.03 | −0.01, 0.06 | 0.147 | 0.01/0.00 |
| Functioning | ||||||||
| PEG Pain (0–10) | 0.16 | 0.10, 0.23 | <0.001 | 0.17/0.01 | 0.03 | −0.05, 0.12 | 0.449 | 0.01/0.00 |
| PROMIS Physical Health Functioning‡ | −0.82 | −1.02, −0.61 | <0.001 | 0.19/0.02 | −0.12 | −0.32, 0.09 | 0.268 | 0.01/0.00 |
| PROMIS Mental Health Functioning‡ | −1.75 | −1.99, −1.50 | <0.001 | 0.27/0.07 | −0.29 | −0.54, −0.04 | 0.022 | 0.02/0.01 |
| Perceived Stress (4‒20) | 0.53 | 0.43, 0.62 | <0.001 | 0.17/0.04 | 0.13 | 0.02, 0.24 | 0.026 | 0.02/0.00 |
Numbers in parentheses indicate the minimum to a maximum range of scale scores, with bolded numbers indicating the worst score.
Confidence interval.
For PROMIS scales, 50 represents the population norm, with lower scores indicating worse functioning and 10 representing 1 SD.
PHQ-2 indicates Patient Health Questionnaire-2.
FIGURE 1.
y axis represents well-being or functioning values on their natural scale; x axis represents PHQ-2 scores, with scores ranging from 0 to 6 in the cross-sectional analyses and −6 (improvement in depressive symptoms) to +6 (worsening of depressive symptoms); means are represented by black dots, and colored dots represent individual values reported by Veterans. PHQ-2 indicates Patient Health Questionnaire-2.
Longitudinal Associations Between PHQ-2 Scores, Well-Being, and Functioning
While a total of 113 (13.5%) Veterans saw improvement in PHQ-2 scores over time, 58 (6.9%) Veterans saw a worsening of depressive symptoms. See Table 3 for frequency information on PHQ-2 scores. The largest changes observed in this cohort were improvements in life satisfaction (diff = 0.18; 95% CI: 0.05, 0.30; P = 0.005; Cohen’s d = 0.09) over time and decreased purpose in life (diff = −0.32; 95% CI: –0.57, –0.06; P = 0.015, Cohen’s d = −0.07). There were no significant changes over time in the remaining well-being and functioning measures.
The strongest relationship between change in PHQ-2 scores and well-being was in purpose in life, where an increase in depressive symptoms assessed by the PHQ-2 between baseline and 12 months was associated with less purpose in life over time (b = −0.19, 95% CI: −0.34, −0.04; r 2 = 0.01). All other well-being longitudinal associations were non-signifiacnt (P’s > 0.05).
The strongest relationship between change in PHQ-2 scores and functioning was in mental health functioning, where an increase in depressive symptoms between baseline and 12 months was associated with lower mental health functioning (b = −0.29, 95% CI: −0.54, −0.04; r 2 = 0.01). Increased PHQ-2 scores were also associated with more perceived stress (b = 0.13, 95% CI: 0.02, 0.24; r 2 = 0.00) over time. All other functioning longitudinal associations were nonsignificant (P’s > 0.05).
DISCUSSION
The current analysis is among the first to examine how a widely used screening tool in a large health care system, the PHQ-2, may help inform health care providers and researchers on what to expect regarding well-being and functioning among individuals receiving services. Our results provide foundational evidence that the PHQ-2 minimally corresponds to cross-sectional measures of well-being and functioning. Changes in PHQ-2 scores performed less well as an indicator of change in well-being and functioning over time. Results have important implications for VA, as well as other health care systems, seeking to address patient well-being through clinical care and other services.
The PHQ-2 may have limited ability to help clinicians and learning health systems understand the well-being and functioning of its beneficiaries; however, it is important to place the current results within their context. We did not assess the circumstances under which the PHQ-2 was measured. It may be that individuals are more likely to accurately report distress during some visits (eg, a mental health visit) versus others (eg, a primary care visit). Moreover, most individuals in our sample reported no symptoms on the PHQ-2, and most individuals neither improved nor got worse, as assessed by the PHQ-2. This lack of variability likely contributed to the limited associations between the PHQ-2 and well-being and functioning over time. Monitoring improvement is a critical component of ensuring that Veterans are receiving the care and services they need to optimize well-being and health. When the PHQ-2 is being used to monitor depressive symptoms over time, other measures will likely be needed to capture the trajectory of well-being and functioning. Overall, results highlight how the PHQ-2 likely minimally informs patient functioning and well-being when used as part of a large health care system.
VA has invested a great deal of resources in its Whole Health transformation, including the recent Veterans Health Administration (VHA) Directive 1445, which establishes VA as a “Whole Health System of Care”33; therefore, it is critical that VA understands how to assess well-being for every Veteran “at each phase of their life journey.”34 A first step in assessing receipt of benefit is having an appropriate measure that captures a broad range of well-being constructs efficiently. The recent development of the Well-being Signs, shows promise in this regard35,36; however, it has not been systematically integrated into VA care like the PHQ-2. An ideal brief measure of well-being delivered in large health care systems should be able to predict a significant amount of variance related to positive aspects of “physical, behavioral, spiritual, and socioeconomic well-being,”2 both cross-sectionally and longitudinally.
With these considerations in mind, developing Clinical Practice Guidelines for Promoting Well-Being may be an appropriate next step in the VA Whole Health transformation, and such guidelines could be leveraged by other large health care systems, as well. Clinical Practice Guidelines centered on well-being could clearly define well-being, potentially adopting the World Health Organization’s definition of “a positive state experienced by individuals and societies,”4 and identify which constructs should be considered under the umbrella of well-being within the context of VA Whole Health care. Indeed, a recent VA State of the Art conference on measuring whole person health37 noted more work is needed to determine which constructs should be considered well-being. The current results suggest that measures of functioning (ie, deficits) clearly operate differently than measures of well-being, based on differences in how much variance was accounted for by PHQ-2 scores. Clinical Practice Guidelines for Promoting Well-Being would lay the foundation for mandating yearly well-being screening and indications where further assessment is needed. For instance, if an individual scores low on the Well-Being Signs,35,36 this could trigger a patient-provider conversation on (1) what domains of an individual’s life are contributing to low well-being, (2) which domains the patient would like to focus on to optimize well-being, and the (3) development of a personal health plan38 that includes which resources could help move an individual toward improved well-being. The guidelines could then also designate which treatment team members are most suited to be involved in promoting well-being.
Limitations and Future Directions
The current study was carried out within the context of recruiting a sample of Veterans with chronic pain and/or who used VA Whole Health care, rather than a sample reflecting the general Veteran population, which may limit generalizability. Although we used rigorous methods to account for potential bias associated with missing data, it is still possible that missingness also limited generalizability (eg, individuals more likely to engage with VA are overrepresented). While the use of the PHQ-2 helps reduce patient and provider burden, it may not capture the nuance of an individual’s clinical presentation as the PHQ-9 can. While the ±90-day window for PHQ-2 assessments was chosen for both theoretical and quantitative reasons, stronger associations between the PHQ-2 and measures of well-being and functioning may have been detected if assessed concurrently/closer in time. Furthermore, although the time between PHQ-2 assessments varied between individuals, analyses treated the time between assessments as equal, potentially introducing unexplained variability. Future research could replicate these results with specific populations who have a wider range of depressive symptom severity, particularly in light of the lack of variability in PHQ-2 scores. Life satisfaction was assessed using only 1 item, potentially reducing the accuracy of its measurement. Survey results did not represent all aspects of well-being.5,39,40 Future work could take a more systematic approach to choosing well-being measures and determining whether the PHQ-2 is associated with those measures. For instance, it may be that affect balance, a concept discussed as important to emotional well-being,5 may indeed be strongly associated with the PHQ-2, thus providing clinicians with another avenue in understanding the experiences of an individual. Finally, while outside the scope of the current research, we also recognize that it will be important for future research to understand how changes in functioning and well-being affect each other over time.
CONCLUSIONS
The present analysis combined EHR and survey data to provide evidence that the PHQ-2 minimally helped inform levels of patient well-being and functioning, with limitations. While cross-sectional relationships between the PHQ-2 and well-being and functioning were significant, associations among these measures were small. The current research suggests that more work is needed to better understand how large health care systems can more fully capture well-being and “what matters most” to individuals.
Footnotes
The authors declare no conflict of interest.
Contributor Information
David E. Reed, II, Email: david.reed7@va.gov.
Charles C. Engel, Email: charles.engel@va.gov.
Scott Coggeshall, Email: scott.coggeshall@va.gov.
Martha Michel, Email: martha.michel@va.gov.
Bella Etingen, Email: bella.etingen@va.gov.
Rendelle E. Bolton, Email: rendelle.bolton@va.gov.
Kurt Kroenke, Email: kkroenke@regenstrief.org.
Barbara G. Bokhour, Email: barbara.bokhour@va.gov.
Steven B. Zeliadt, Email: steven.zeliadt@va.gov.
REFERENCES
- 1. Bokhour BG, Haun JN, Hyde J, et al. Transforming the Veterans Affairs to a whole health system of care. Med Care. 2020;58:295–300. [DOI] [PubMed] [Google Scholar]
- 2. National Academies of Sciences E, Medicine. Achieving Whole Health. National Academies Press; 2023. [Google Scholar]
- 3. Lomas T, VanderWeele TJ. The garden and the orchestra: generative metaphors for conceptualizing the complexities of well-being. Int J Environ Res Public Health. 2022;19:14544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Organization WH. Promoting well-being. Accessed November 14, 2023. https://www.who.int/activities/promoting-well-being#:~:text=Well%2Dbeing%20is%20a%20positive,social%2C%20economic%20and%20environmental%20conditions
- 5. Park CL, Kubzansky LD, Chafouleas SM, et al. Emotional well-being: What it is and why it matters. Affect Sci. 2022;4:10–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee MT, McNeely E, Weziak-Bialowolska D, et al. Demographic predictors of complete well-being. BMC Public Health. 2022;22:1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mulvaney-Day N, Marshall T, Downey Piscopo K, et al. Screening for behavioral health conditions in primary care settings: a systematic review of the literature. J Gen Intern Med. 2018;33:335–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yano EM, Chaney EF, Campbell DG, et al. Yield of practice-based depression screening in VA primary care settings. J Gen Intern Med. 2012;27:331–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Affairs USDoV, Department of D. VA/DoD Clinical Practice Guideline for the Management of Major Depressive Disorder. 2022. Accessed October 14, 2024. https://www.healthquality.va.gov/guidelines/MH/mdd/VADoDMDDCPGFinal508.pdf
- 10. Bradley KA, Kivlahan DR, Zhou XH, et al. Using alcohol screening results and treatment history to assess the severity of at-risk drinking in Veterans Affairs primary care patients. Alcohol Clin Exp Res. 2004;28:448–455. [DOI] [PubMed] [Google Scholar]
- 11. Kroenke K, Spitzer RL, Williams JBW. The patient health questionnaire-2. Med Care. 2003;41:1284–1292. [DOI] [PubMed] [Google Scholar]
- 12. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Staples LG, Dear BF, Gandy M, et al. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: the PHQ-2, GAD-2, and K-6. Gen Hosp Psychiatry. 2019;56:13–18. [DOI] [PubMed] [Google Scholar]
- 14. Mitchell AJ, Yadegarfar M, Gill J, et al. Case finding and screening clinical utility of the Patient Health Questionnaire (PHQ-9 and PHQ-2) for depression in primary care: a diagnostic meta-analysis of 40 studies. BJPsych Open. 2016;2:127–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Levis B, Sun Y, He C, et al. Accuracy of the PHQ-2 alone and in combination with the PHQ-9 for screening to detect major depression: systematic review and meta-analysis. JAMA. 2020;323:2290–2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kroenke K, Stump TE, Chen CX, et al. Responsiveness of PROMIS and Patient Health Questionnaire (PHQ) Depression Scales in three clinical trials. Health Qual Life Outcomes. 2021;19:41 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Force USPST. Barry MJ, Nicholson WK, et al. Screening for depression and suicide risk in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2023;329:2057–2067. [DOI] [PubMed] [Google Scholar]
- 18. Dadfar M, Momeni Safarabad N, Asgharnejad Farid AA, et al. Reliability, validity, and factorial structure of the World Health Organization-5 Well-Being Index (WHO-5) in Iranian psychiatric outpatients. Trends Psychiatry Psychother. 2018;40:79–84. [DOI] [PubMed] [Google Scholar]
- 19. Ventura-León J, Sánchez-Villena AR, Caycho-Rodríguez T. Validity evidence and reliability of a subjective well‑being scale. Trends Psychol. 2023. doi: 10.1007/s43076-022-00251-x [DOI] [Google Scholar]
- 20. Mamani-Benito O, Carranza Esteban RF, Castillo-Blanco R, et al. Anxiety and depression as predictors of life satisfaction during pre-professional health internships in COVID-19 times: the mediating role of psychological well-being. Heliyon. 2022;8:e11025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fujii T, Oka H, Katsuhira J, et al. Association between somatic symptom burden and health-related quality of life in people with chronic low back pain. PLoS One. 2018;13:e0193208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bokhour BG, DeFaccio R, Gaj L, et al. Changes in patient-reported outcomes associated with receiving whole health in the Veteran Health Administration (VHA)‘s National Demonstration Project. J Gen Intern Med. 2023;39:84–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cantril H. The Pattern of Human Concerns. Rutgers University Press; 1965. [Google Scholar]
- 24. Scheier MF, Wrosch C, Baum A, et al. The life engagement test: assessing purpose in life. J Behav Med. 2006;29:291–298. [DOI] [PubMed] [Google Scholar]
- 25. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. [DOI] [PubMed] [Google Scholar]
- 26. Krebs EE, Lorenz KA, Bair MJ, et al. Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J Gen Intern Med. 2009;24:733–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hays RD, Bjorner JB, Revicki DA, et al. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18:873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Social Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 29. Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 30. van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Statist Softw. 2011;45:1–67. [Google Scholar]
- 31. Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons, Inc; 1987. [Google Scholar]
- 32. R Core Team. _R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2024. [Google Scholar]
- 33. U.S. Department of Veterans Affairs. VHA Directive 1445: Whole Health System. 2023. Accessed October 14, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=11498
- 34. Kligler B, Khung M, Schult T, et al. What we have learned about the implementation of whole health in the Veterans Administration. J Integr Complement Med. 2023;29:774–780. [DOI] [PubMed] [Google Scholar]
- 35. Transformation OoPCCaC. Well-being signs: a whole health measurement for well-being. 2024. Accessed October 14, 2024. https://www.va.gov/WHOLEHEALTH/professional-resources/clinician-tools/well-being_signs_fact_sheet.pdf
- 36.Vogt DMV, Borowski S, Bokhour B, et al. https://www.healthaffairs.org/content/forefront/beyond-disease-and-dysfunction-asking-patients-their-psychosocial-well-being Beyond disease and dysfunction: asking patients about their psychosocial well-being. 2022. Accessed June 20, 2024.
- 37. Affairs USDoV. Measuring What Matters Most: Whole Person Outcomes & Well Being: State of the Art Conference; 2023.
- 38. Bolton RE, Bokhour BG, Hogan TP, et al. Integrating personalized care planning into primary care: a multiple-case study of early adopting patient-centered medical homes. J Gen Intern Med. 2020;35:428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ryff CD. Flotsam, jetsam, and forward-moving vessels on the sea of well-being: commentary on “emotional well-being: what is it and why it matters”. Affect Sci. 2023;4:49–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Feller SC, Castillo EG, Greenberg JM, et al. Emotional well-being and public health: proposal for a model national initiative. Public Health Rep. 2018;133:136–141. [DOI] [PMC free article] [PubMed] [Google Scholar]