Abstract
Background:
Hyperextension varus tibial plateau fracture (HVTPF) is known to present with concomitant injuries to the posterolateral corner (PLC). However, the exact rate and characteristics of these injuries remain unclear. The primary objective of this study was to explore the rate and characteristics of PLC injuries in HVTPFs. The secondary objective was to investigate the relationship between the fracture morphological features and the associated PLC injuries.
Methods:
Patients with HVTPFs were subdivided into 2 groups: group I (without fracture of the posterior column cortex) and group II (with fracture of the posterior column cortex). Fracture characteristics were summarized qualitatively based on fracture maps and quantitatively based on the counts of morphological parameters. Knee ligamentous and meniscal injuries were assessed using magnetic resonance imaging. The association between fracture characteristics and PLC injuries was analyzed.
Results:
We included a total of 50 patients with HVTPFs in our study: 28 in group I and 22 in group II. The rate of PLC injuries was 28.6% in group I and 27.3% in group II. In group I, patients with PLC injuries showed fracture lines closer to the anterior rim of the medial plateau and had smaller fracture areas. Furthermore, 6 of the 8 patients with PLC injuries in group I also had posterior cruciate ligament injuries.
Conclusions:
The rate of PLC injuries is relatively high in HVTPFs. In HVTPFs without fracture of the posterior column cortex, a small fracture area strongly suggests an accompanying PLC injury, and PLC injury is frequently combined with posterior cruciate ligament injury.
Level of Evidence:
Prognostic Level III. See Instructions for Authors for a complete description of levels of evidence.
Hyperextension varus tibial plateau fracture (HVTPF) is a rare knee fracture pattern that was initially described as an anteromedial tibial plateau fracture1. Subsequent studies have noted that, in some cases, it may also involve tension failure in the posterior column cortex, resulting in a more complicated fracture pattern2. In general, HVTPFs show fracture characteristics with recurvatum and varus (loss of both the posterior tibial slope and the medial tibial plateau angle)2,3.
Recent progress in the treatment of tibial plateau fractures has encouraged orthopaedic surgeons to focus on the associated ligamentous and meniscal injuries in order to provide a comprehensive treatment of this type of knee injury4-6. Specifically, the injury mechanism responsible for HVTPFs can jeopardize the soft tissue of the knee, particularly the posterolateral corner (PLC), which is located on the diagonal side of the tibial plateau1,7-9. In a previous study, a 51% rate of fibular head avulsion fractures was reported in HVTPFs9. However, there is still limited knowledge about the rate and characteristics of concurrent ligamentous injuries. Given the profound role of the PLC in maintaining knee stability, accurate diagnosis and appropriate management are crucial in order to optimize outcomes10,11. Physical examination in patients with combined injuries is often of limited value because it is generally impossible to isolate instability findings as osseous or ligamentous. Therefore, magnetic resonance imaging (MRI) is a convenient and effective method for diagnosing PLC injuries12,13.
We believed that an in-depth study combining computed tomography (CT) and MRI to describe osseous and ligamentous injuries in HVTPFs would have clinical value. The main objectives of our study were (1) to explore the rate and characteristics of PLC injuries in HVTPFs and (2) to investigate the relationship between the fracture morphological features and the associated PLC injuries.
Materials and Methods
Participants
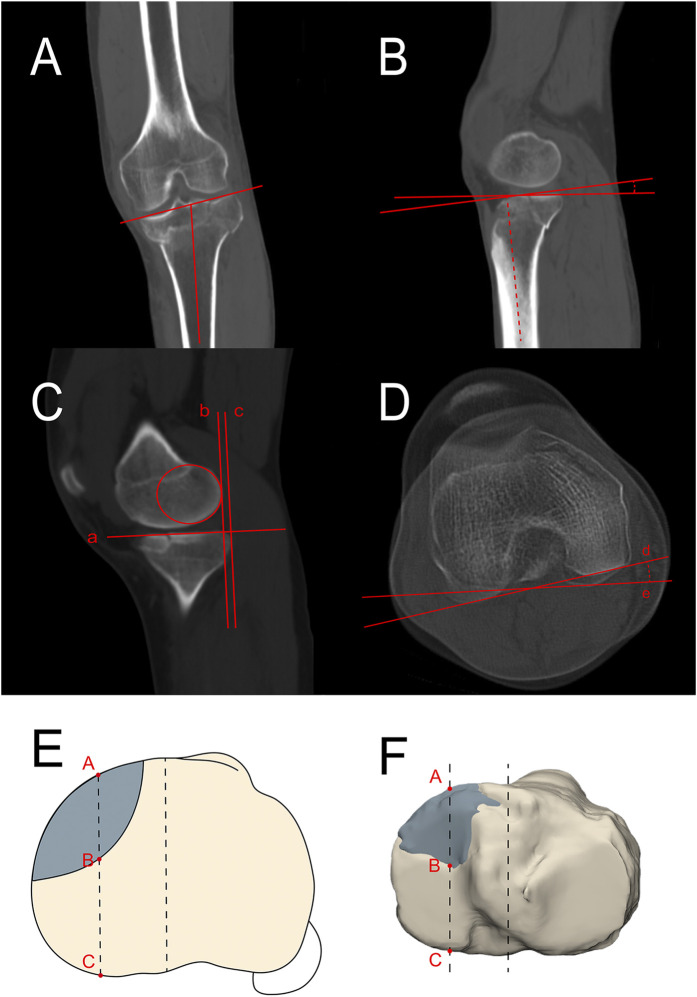
We conducted a search in the PACS (picture archiving and communication system) of a level-I trauma center for CT data of patients who had been diagnosed with the keywords “tibia plateau fracture” between January 2019 and August 2022. The following exclusion criteria were used: (1) polytrauma with an Injury Severity Score of >16; (2) open or pathological fractures; (3) fractures that were concomitant with an ipsilateral tibial shaft, femoral, or patellar non-avulsion fracture; (4) skeletal immaturity (age of <16 years); and (5) other fractures that were not HVTPFs. Patients with HVTPFs were subsequently screened. In accordance with previous research, the HVTPFs were characterized as being fractures that mainly involved the anteromedial articular surface, which could also be combined with or without fracture of the posterior column cortex1,2,9. Patients with HVTPFs with both CT and MRI data were selected from the database, excluding those who had not been treated in our department. Fifty patients were deemed eligible for this study. Since it remains unknown whether fracture of the posterior column cortex is associated with soft-tissue injuries, we subdivided the cases into 2 groups: group I, those without fracture of the posterior column cortex; and group II, those with fracture of the posterior column cortex (Fig. 1).
Fig. 1.
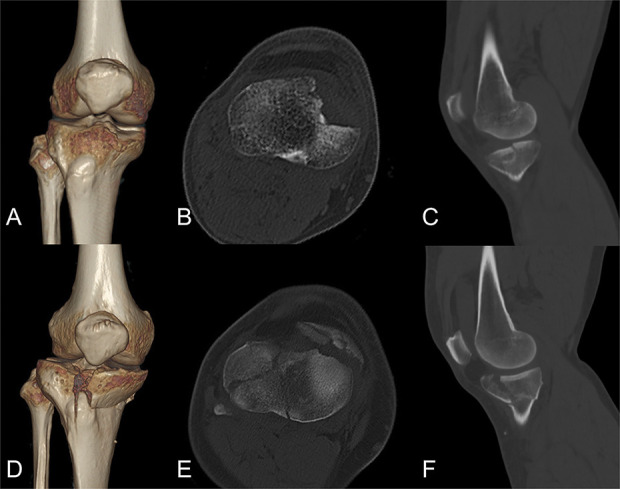
Figs. 1-A through 1-F HVTPFs. Figs. 1-A, 1-B, and 1-C Group-I HVTPFs. Figs. 1-D, 1-E, and 1-F Group-II HVTPFs.
Three-Dimensional Fracture Heat Mapping
As reported in previous studies, the spatial morphology of a tibial plateau fracture has been demonstrated using a 3-dimensional (3D) fracture-mapping technique9,14. CT data of patients with an HVTPF were first used to reconstruct and reduce the fracture fragments with Materialise Mimics software. In order to best fit a 3D template of the proximal part of the tibia and the fibula, additional operations, including rotating, normalizing, translating, and flipping the model, were performed by 3-matic software (Materialise). Then, the osseous markers in the proximal part of the tibia were used to modify the CT data-reconstructed model. Next, smooth curves were selected to draw the fracture lines directly on the surface of the standard 3D model. Lastly, all of the drawn fracture lines were overlapped onto a 3D model to generate a spatial fracture line map. Then, the heat-mapping technique was adopted to show the results of the fracture line maps in a more intuitive way. The graphically superimposed fracture lines were transferred and imported into E3D software (Central South University) to create 3D heat maps, which revealed the frequency of fracture lines with use of different colors (ranging from blue to red, indicating a frequency of low to high, respectively).
Measurement Technique
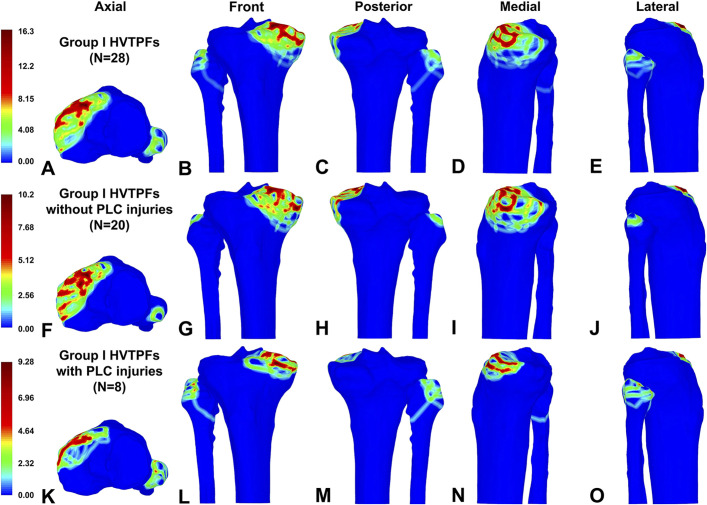
The radiographic data were acquired from a PACS and were subsequently imported into RadiAnt DICOM (Digital Imaging and Communications in Medicine) Viewer (version 2021.2; Medixant) for analysis. In accordance with previous research, osseous parameters, including the medial proximal tibial angle, the medial and lateral posterior tibial slope, the medial and lateral plateau retreat distance, and the rotation angle, were measured based on the CT data15-18 (Fig. 2). The medial and lateral plateau retreat distance was a measure of subluxation. The anterior articular surface loss was measured based on the 3D model of the reduced fracture (Fig. 2). The fracture area ratio was evaluated based on the transverse section of the 3D model of the reduced fracture (see Appendix S1).
Fig. 2.
Figs. 2-A through 2-F Measurements of the medial proximal tibial angle, the medial and lateral posterior tibial slope, the medial and lateral plateau retreat distance, the rotation angle, and anterior articular surface loss. Fig. 2-A The medial proximal tibial angle is the angle between the tibial plateau surface and the long axis of the tibia in coronal images. Fig. 2-B The posterior tibial slope is the angle between the tibial plateau surface and the line perpendicular to the tibial long axis in sagittal images. Fig. 2-C A best-fit circle over the posterior femoral condyle was drawn on sagittal images, and then the line “a” tangent to the medial and lateral tibial plateau was determined. Two parallel lines perpendicular to line “a” were drawn tangent to the posterior margin of the circle and the tibial plateau, marked as line “b” and line “c.” The distance between line b and line c was regarded as the medial and lateral plateau retreat distance. Fig. 2-D Two axial slices were chosen in which the deepest femoral trochlear groove and the posterior tibial plateau notch were clearly observed. Lines “d” and “e” were drawn tangential to the posterior aspect of the femoral condyle and to the tibial plateau, respectively, and the angle between them was the rotation angle. A positive value of the rotation angle indicates internal rotation of the proximal tibia relative to the distal femur. Figs. 2-E and 2-F Based on the 3D model of the reduced fracture, the transverse diameter of the tibial plateau was quartered and a dashed line was drawn perpendicular to the transverse diameter at the medial quarter of the width. The dashed line intersects the anterior rim of the medial tibial plateau at point “A,” the most posterior point on the fracture line (whether displaced or not) at point “B,” and the posterior margin of the medial tibial plateau at point “C.” The anterior articular surface loss was calculated as AB divided by AC.
To determine intraobserver and interobserver reliability using the intraclass correlation coefficient (ICC), 2 observers independently measured each case twice with an interval of 2 weeks. An ICC value of ≥0.75 was defined as good, while an ICC value from 0.50 to 0.74 was defined as moderate19 (see Appendix Table S1).
MRI Acquisition and Interpretation
Following a standard imaging protocol, MRI data were acquired with a 3.0-T MRI scanner. The current study employed T1-weighted, T2-weighted, and proton density sequences. Increased signal intensity within the meniscus indicated meniscal pathology, classified as grades 1 through 420. Only grade-3 and 4 lesions were considered to be meniscal tears. Ligamentous injuries included avulsion fractures and complete midsubstance tears. An avulsion fracture of the ligament was defined as an avulsion fracture of the tibial or femoral footprint. A complete midsubstance tear of a ligament was recognized as a complete disruption of ligamentous fibrous tissue continuity21,22. A PLC injury was defined as a lateral collateral ligament injury and/or a popliteus tendon injury.
Two senior doctors with expertise in musculoskeletal radiology analyzed the MRI data and adopted a panel discussion to resolve disagreements. The radiologists were not informed of the original patient information. Prior to this, in order to assess intraobserver and interobserver reliability using the Cohen kappa coefficient, the observers reviewed all of the cases twice with an interval of 2 weeks. The level of reliability was evaluated based on the kappa values according to the guidelines proposed by Landis and Koch23 (see Appendix Table S2).
Results
Fifty patients with an HVTPF (13 men and 37 women with a mean age of 46.3 years) with available CT and MRI data were included in this study. The demographic characteristics of both groups are documented in Table I.
TABLE I.
Patient Demographic Characteristics
| Group | Total | ||
|---|---|---|---|
| I | II | ||
| No. of fractures | 28 | 22 | 50 |
| Age* (yr) | 44.1 ± 13.1 | 49.1 ± 15.6 | 46.3 ± 14.3 |
| Sex† | |||
| Female | 6 | 7 | 13 |
| Male | 22 | 15 | 37 |
| Side of injury‡ | |||
| Left | 17 | 14 | 31 |
| Right | 11 | 8 | 19 |
| Medial plateau retreat distance* (mm) | 4.7 ± 2.1 | 7.3 ± 3.4 | 5.8 ± 3.0 |
| Lateral plateau retreat distance* (mm) | −1.8 ± 3.0 | 2.3 ± 5.6 | 0.0 ± 4.8 |
| Rotation angle* (deg) | 4.6 ± 3.0 | 4.4 ± 3.2 | 4.5 ± 3.1 |
| Medial proximal tibial angle* (deg) | 85.1 ± 2.6 | 83.9 ± 2.1 | 84.6 ± 2.4 |
| Medial posterior tibial slope* (deg) | 1.0 ± 7.4 | −6.1 ± 7.1 | −2.1 ± 8.0 |
| Lateral posterior tibial slope* (deg) | 6.5 ± 4.3 | −2.9 ± 6.3 | 2.3 ± 7.0 |
The values are given as the mean ± the standard deviation.
The values are given as the number of patients.
The values are given as the number of fractures.
Several osseous morphological parameters were determined (Table I). In particular, the mean medial posterior tibial slope (and standard deviation) was 1.0° ± 7.4° in group I and −6.1° ± 7.1° in group II; the mean lateral posterior tibial slope was 6.5° ± 4.3° in group I and −2.9° ± 6.3° in group II. These results indicated that the 2 groups of HVTPFs, resulting from the same injury-force mechanism, had different osseous morphological characteristics and should be considered as 2 different patterns.
Next, the rate of soft-tissue injuries was determined (Table II). The rate of PLC injuries was 28.6% in group I and 27.3% in group II. The number of patients with combined PLC and posterior cruciate ligament injuries was 6 in group I and 2 in group II.
TABLE II.
Rate of Soft-Tissue Injuries*
| Group I (N = 28) (no. [%]) | Group II (N = 22) (no. [%]) | |
|---|---|---|
| ACL | ||
| Complete midsubstance tear | 2 (7.1) | 0 (0.0) |
| Avulsion fracture | 1 (3.6) | 3 (13.6) |
| PCL | ||
| Complete midsubstance tear | 6 (21.4) | 2 (9.1) |
| Avulsion fracture | 1 (3.6) | 1 (4.5) |
| MCL | ||
| Complete midsubstance tear | 1 (3.6) | 0 (0.0) |
| Avulsion fracture | 1 (3.6) | 0 (0.0) |
| LCL | ||
| Complete midsubstance tear | 4 (14.3) | 2 (9.1) |
| Avulsion fracture | 4 (14.3) | 3 (13.6) |
| PT | ||
| Complete midsubstance tear | 5 (17.9) | 2 (9.1) |
| Avulsion fracture | 0 (0.0) | 0 (0.0) |
| MM | ||
| Anterior horn tear | 2 (7.1) | 3 (13.6) |
| Body tear | 5 (17.9) | 3 (13.6) |
| Posterior horn tear | 8 (28.6) | 3 (13.6) |
| LM | ||
| Anterior horn tear | 1 (3.6) | 2 (9.1) |
| Body tear | 1 (3.6) | 3 (13.6) |
| Posterior horn tear | 2 (7.1) | 2 (9.1) |
ACL = anterior cruciate ligament, PCL = posterior cruciate ligament, MCL = medial collateral ligament, LCL = lateral collateral ligament, PT = popliteus tendon, MM = medial meniscus, and LM = lateral meniscus.
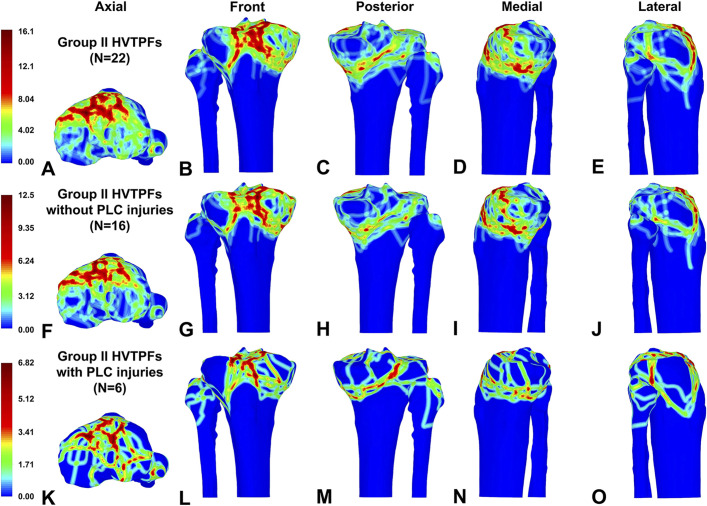
In order to elucidate the role of the PLC in an HVTPF, 3D fracture heat maps were used to visualize the morphology of fracture lines in both groups with or without PLC injury (Figs. 3 and 4). In patients with PLC injuries in group I, the fracture area (hot zone) was smaller and was concentrated on the anterior rim of the medial plateau when compared with those without PLC injuries (Figs. 3-F through 3-O). However, no substantial visualized morphological differences between fractures with and without PLC injuries were demonstrated with heat mapping in patients in group II (Figs. 4-F through 4-O).
Fig. 3.
Figs. 3-A through 3-O Heat mapping and representative views of the fracture line distribution in group-I HVTPFs. Figs. 3-A through 3-E Group-I HVTPFs. Figs. 3-F through 3-J Group-I HVTPFs without PLC injuries. Figs. 3-K through 3-O Group-I HVTPFs with PLC injuries.
Fig. 4.
Figs. 4-A through 4-O Heat mapping and representative views of the fracture line distribution in group-II HVTPFs. Figs. 4-A through 4-E Group-II HVTPFs. Figs. 4-F through 4-J Group-II HVTPFs without PLC injuries. Figs. 4-K through 4-O Group-II HVTPFs with PLC injuries.
In addition to heat mapping, quantitative analyses of several osseous parameters were utilized to further investigate the fracture morphology differences between patients with and without PLC injuries in both of the groups (Table III). In group I, the mean fracture area ratio was 6.2% ± 2.8% in patients with a PLC injury and 16.7% ± 5.6% in patients without a PLC injury; the mean rotation angle was 8.0° ± 3.5° in patients with a PLC injury and 3.2° ± 1.1° in patients without a PLC injury. In group II, the mean rotation angle was 7.0° ± 5.5° in patients with a PLC injury and 3.4° ± 1.0° in patients without a PLC injury.
TABLE III.
Differences in Parameters Between Patients with and without PLC Injury*
| Group I | Group II | |||
|---|---|---|---|---|
| Injury (N = 8) | Noninjury (N = 20) | Injury (N = 6) | Noninjury (N = 16) | |
| Medial plateau retreat distance (mm) | 5.7 ± 1.5 | 4.2 ± 2.2 | 8.8 ± 4.9 | 6.7 ± 2.7 |
| Lateral plateau retreat distance (mm) | −3.4 ± 2.4 | −1.2 ± 3.0 | 4.7 ± 6.2 | 1.4 ± 5.3 |
| Rotation angle (deg) | 8.0 ± 3.5 | 3.2 ± 1.1 | 7.0 ± 5.5 | 3.4 ± 1.0 |
| Medial proximal tibial angle (deg) | 85.1 ± 2.2 | 85.1 ± 2.8 | 83.0 ± 2.2 | 84.3 ± 1.9 |
| Medial posterior tibial slope (deg) | 0.2 ± 4.8 | 1.3 ± 8.3 | −9.4 ± 10.5 | −4.8 ± 5.2 |
| Lateral posterior tibial slope (deg) | 6.6 ± 2.9 | 6.4 ± 4.8 | −3.8 ± 7.7 | −2.6 ± 6.0 |
| Anterior articular surface loss (%) | 15.1 ± 12.6 | 27.7 ± 15.4 | — | — |
| Fracture area ratio (%) | 6.2 ± 2.8 | 16.7 ± 5.6 | — | — |
The values are given as the mean ± the standard deviation. PLC = posterolateral corner.
The relationship between a PLC injury and other soft-tissue injuries was analyzed (see Appendix Table S3). In group I, 6 of 8 patients with PLC injuries had combined posterior cruciate ligament injuries, whereas only 1 of 20 patients without PLC injuries had a posterior cruciate ligament injury.
Discussion
The most important finding of this study was that concomitant PLC injuries were common in patients with HVTPFs. The rate of PLC injuries was the same in patients with and without fracture of the posterior column cortex. The involvement of the posterior column cortex did not influence the rate of PLC injuries. Therefore, it cannot be used as a criterion to rule out PLC injuries. Surgeons should maintain a high level of suspicion for PLC injuries in all patients with HVTPFs.
Patients in group I were mainly characterized by osseous injuries on the anteromedial tibial plateau and had associated PLC injuries on the tension side, as confirmed by previous studies1,8,24,25. Furthermore, we found that the fracture area tended to be smaller in group-I patients with PLC injuries. From a biomechanical point of view, when a knee joint is subjected to hyperextension and varus forces, a collision between the medial femoral condyle and the anteromedial tibial plateau is induced, thereby causing an HVTPF1,8,24. The size of the fracture is determined by which point on the medial tibial plateau touched the medial femoral condyle. Some studies have suggested that if the ligament on the tension side is ruptured initially, the impact site between the femoral condyle and the tibial plateau would shift anteriorly, leading to a reduced fracture area1,24,26. Therefore, for patients with small anteromedial tibial plateau fractures, clinicians should be particularly vigilant for concomitant ligamentous injuries.
HVTPFs in patients in group II were mainly characterized by a decreased posterior tibial slope, coronal plane varus deformity, and posterior-tension osseous injuries. Additionally, a concentration of tension fracture lines was observed on the posterior side of HVTPFs on our heat maps, which, to our knowledge, has not been highlighted in the existing literature9,27. Generally speaking, the tension-side failures in group-II HVTPFs are considered osseous2,28. Accordingly, treatment strategies predominantly target their osseous characteristics, with less emphasis on the management of associated ligamentous injuries; this approach has resulted in poor outcomes2,3,28,29. Nevertheless, in our study, 6 PLC injuries were observed in group-II HVTPFs, a rate of 27.3%. Therefore, we recommend routine evaluation for soft-tissue injuries before and after open reduction and internal fixation of HVTPFs.
Based on the theory of the injury-force mechanism, unique fracture patterns are inextricably linked to specific soft-tissue injuries9. For example, diagonal injuries involving anteromedial tibial plateau fractures and PLC injuries are characteristic consequences of a hyperextension varus injury mechanism. Previous studies have reported that ligamentous injuries in anteromedial tibial plateau fractures are predominantly PLC injuries1,8,9. Li et al. found that 9.5% of patients with combined PLC and posterior cruciate ligament injuries had concomitant anteromedial tibial plateau fractures30. To investigate the relationship between fracture morphology and ligamentous injury in diagonal injuries, we measured the morphological parameters that were related to PLC injuries. In the group-I HVTPFs with PLC injuries, we observed substantial internal rotation of the tibia, which was not consistent with the common phenomenon of isolated PLC injuries with external rotation of the tibia31,32. This difference could be partially explained by the combination of both PLC injuries and anteromedial tibial plateau fractures30. In group-II HVTPFs, morphological parameters were not found to be associated with PLC injuries. We acknowledge that this study may have been underpowered to detect such associations. Severe osseous injuries may obscure the influence of PLC injuries on fracture morphology. It is unknown what the risk of medial tibial plateau displacement is with or without treatment involving the PLC ligaments.
In general, PLC injuries rarely occur in isolation, and concomitant ligamentous injuries are commonly reported11. In this study, PLC injuries were common in both group-I and group-II HVTPFs, which prompted us to further investigate the association between PLC and other ligamentous injuries. Notably, PLC injuries were often combined with posterior cruciate ligament injuries in group-I HVTPFs, which aligns with existing reports1,8. In group-II HVTPFs, 2 of the 6 patients with PLC injuries had combined posterior cruciate ligament injuries. Concomitant injuries to the PLC and posterior cruciate ligament can lead to knee instability, gait abnormalities, and alterations in medial joint contact pressures33-37. It has also been reported that patients with posterior cruciate ligament and PLC injuries who have larger anteromedial fractures tend to develop subsequent varus deformity of the lower extremity30. Based on the aforementioned findings, extra attention should be given to the diagnosis and treatment of posterior cruciate ligament injuries in addition to PLC injuries.
Our study had some limitations. First, given the limited incidence of HVTPFs in the population, patients with both CT and MRI data are extremely rare. Because the sample size of HVTPF cases was small, the findings should be interpreted with caution and may not be generalizable. Second, MRI can yield false positives, and the MRI grading of PLC injuries does not always correspond with the degree of knee laxity. A future goal is a better understanding of which fracture patterns are most closely associated with PLC injury in order to provide selective indications for MRI. Third, the energy of the injuries had not been documented. Additionally, other posterolateral structures such as the biceps femoris and the peroneal nerve were not evaluated. Fourth, there was a lack of follow-up data for the HVTPFs. Finally, it is unclear to what extent soft-tissue injuries affect fracture stability. These are all areas for future studies by our group.
Conclusions
The rate of accompanying PLC injuries is relatively high in HVTPFs. In HVTPFs without fracture of the posterior column cortex, a small fracture area strongly suggests an accompanying PLC injury, and PLC injury is frequently combined with posterior cruciate ligament injury.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/I207).
Acknowledgments
Note: The authors thank Yingqi Zhang for his technical support of the study.
Footnotes
Binghao Wang, MD, and Teng Ye, MD, contributed equally to this work.
Investigation performed at the Department of Orthopaedic Surgery, Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China
Disclosure: This work was sponsored by the National Natural Science Foundation of China (No. 82172521) and the Youth Program of National Natural Science Foundation of China (No. 82002287). The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/I208).
Contributor Information
Binghao Wang, Email: wang.binghao@outlook.com.
Teng Ye, Email: yeteng@sjtu.edu.cn.
Binbin Zhang, Email: binbin_yoyo@163.com.
Yukai Wang, Email: Duncanjames@126.com.
Yi Zhu, Email: tzjzzy@163.com.
References
- 1.Chiba T, Sugita T, Onuma M, Kawamata T, Umehara J. Injuries to the posterolateral aspect of the knee accompanied by compression fracture of the anterior part of the medial tibial plateau. Arthroscopy. 2001. Jul;17(6):642-7. [DOI] [PubMed] [Google Scholar]
- 2.Firoozabadi R, Schneidkraut J, Beingessner D, Dunbar R, Barei D. Hyperextension Varus Bicondylar Tibial Plateau Fracture Pattern: Diagnosis and Treatment Strategies. J Orthop Trauma. 2016. May;30(5):e152-7. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez LJ, Lott A, Konda S, Egol KA. The Hyperextension Tibial Plateau Fracture Pattern: A Predictor of Poor Outcome. J Orthop Trauma. 2017. Nov;31(11):e369-74. [DOI] [PubMed] [Google Scholar]
- 4.Maheshwari J, Pandey VK, Mhaskar VA. Anterior tibial plateau fracture: An often missed injury. Indian J Orthop. 2014. Sep;48(5):507-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chellamuthu G, Chandramohan AK, Zackariya M, Perumal R, Jayaramaraju D, Shanmuganathan R. Uncommon Pattern of Anterior Compression Fractures of the Tibial Plateau: A Report of 7 Cases and Review of Literature. J Orthop Case Rep. 2021. Nov;11(11):39-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li L, Li Y, He Y, Deng X, Zhou P, Li J, Jiang H, Li Z, Liu J. Single-stage arthroscopic-assisted treatment of anteromedial tibial plateau fracture with posterolateral corner injury: a retrospective study. BMC Musculoskelet Disord. 2022. May 5;23(1):420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanders TG, Medynski MA, Feller JF, Lawhorn KW. Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics. 2000. Oct;20(Spec No):S135-51. [DOI] [PubMed] [Google Scholar]
- 8.Bennett DL, George MJ, El-Khoury GY, Stanley MD, Sundaram M. Anterior rim tibial plateau fractures and posterolateral corner knee injury. Emerg Radiol. 2003. Oct;10(2):76-83. [DOI] [PubMed] [Google Scholar]
- 9.Xie X, Zhan Y, Wang Y, Lucas JF, Zhang Y, Luo C. Comparative Analysis of Mechanism-Associated 3-Dimensional Tibial Plateau Fracture Patterns. J Bone Joint Surg Am. 2020. Mar 4;102(5):410-8. [DOI] [PubMed] [Google Scholar]
- 10.Bolog N, Hodler J. MR imaging of the posterolateral corner of the knee. Skeletal Radiol. 2007. Aug;36(8):715-28. [DOI] [PubMed] [Google Scholar]
- 11.LaPrade RF, Wentorf FA, Fritts H, Gundry C, Hightower CD. A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthroscopy. 2007. Dec;23(12):1341-7. [DOI] [PubMed] [Google Scholar]
- 12.Rakhra KS, Delorme JP, Sanders B, Liew A. The diagnostic accuracy of MRI for evaluating the posterolateral corner in acute knee dislocation. Eur Radiol. 2022. Oct;32(10):6752-8. [DOI] [PubMed] [Google Scholar]
- 13.Sanchez-Munoz E, Lozano Hernanz B, Zijl JAC, Passarelli Tirico LE, Angelini FJ, Verdonk PCM, Vuylsteke K, Andrade R, Espregueira-Mendes J, Valente C, Figueroa F, Figueroa D, Maestro Fernández A. Accuracy of Magnetic Resonance Imaging in the Diagnosis of Multiple Ligament Knee Injuries: A Multicenter Study of 178 Patients. Am J Sports Med. 2023. Feb;51(2):429-36. [DOI] [PubMed] [Google Scholar]
- 14.Xie X, Zhan Y, Dong M, He Q, Lucas JF, Zhang Y, Wang Y, Luo C. Two and Three-Dimensional CT Mapping of Hoffa Fractures. J Bone Joint Surg Am. 2017. Nov 1;99(21):1866-74. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y, Luo C, Zhu Y, Zhai Q, Zhan Y, Qiu W, Xu Y. Updated Three-Column Concept in surgical treatment for tibial plateau fractures - A prospective cohort study of 287 patients. Injury. 2016. Jul;47(7):1488-96. [DOI] [PubMed] [Google Scholar]
- 16.Utzschneider S, Goettinger M, Weber P, Horng A, Glaser C, Jansson V, Müller PE. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc. 2011. Oct;19(10):1643-8. [DOI] [PubMed] [Google Scholar]
- 17.Ni QK, Wang XP, Guo Q, Li M, Liu N, Zhang H. High-grade pivot-shift phenomenon after anterior cruciate ligament injury is associated with asymmetry of lateral and medial compartment anterior tibial translation and lateral meniscus posterior horn tears. Knee Surg Sports Traumatol Arthrosc. 2022. Nov;30(11):3700-7. [DOI] [PubMed] [Google Scholar]
- 18.Chen J, Wu C, Ye Z, Zhao J, Xie G. Tibial Tuberosity-Trochlear Groove Distance and Its Components in Patients with and without Episodic Patellar Dislocation: A Study of 781 Knees. J Bone Joint Surg Am. 2022. Mar 16;104(6):504-11. [DOI] [PubMed] [Google Scholar]
- 19.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979. Mar;86(2):420-8. [DOI] [PubMed] [Google Scholar]
- 20.Beals CT, Magnussen RA, Graham WC, Flanigan DC. The Prevalence of Meniscal Pathology in Asymptomatic Athletes. Sports Med. 2016. Oct;46(10):1517-24. [DOI] [PubMed] [Google Scholar]
- 21.Gardner MJ, Yacoubian S, Geller D, Suk M, Mintz D, Potter H, Helfet DL, Lorich DG. The incidence of soft tissue injury in operative tibial plateau fractures: a magnetic resonance imaging analysis of 103 patients. J Orthop Trauma. 2005. Feb;19(2):79-84. [DOI] [PubMed] [Google Scholar]
- 22.Spiro AS, Regier M, Novo de Oliveira A, Vettorazzi E, Hoffmann M, Petersen JP, Henes FO, Demuth T, Rueger JM, Lehmann W. The degree of articular depression as a predictor of soft-tissue injuries in tibial plateau fracture. Knee Surg Sports Traumatol Arthrosc. 2013. Mar;21(3):564-70. [DOI] [PubMed] [Google Scholar]
- 23.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. Mar;33(1):159-74. [PubMed] [Google Scholar]
- 24.Yoo JH, Kim EH, Yim SJ, Lee BI. A case of compression fracture of medial tibial plateau and medial femoral condyle combined with posterior cruciate ligament and posterolateral corner injury. Knee. 2009. Jan;16(1):83-6. [DOI] [PubMed] [Google Scholar]
- 25.Conesa X, Minguell J, Cortina J, Castellet E, Carrera L, Nardi J, Cáceres E. Fracture of the anteromedial tibial plateau associated with posterolateral complex injury: case study and literature review. J Knee Surg. 2013. Dec;26(Suppl 1):S34-9. [DOI] [PubMed] [Google Scholar]
- 26.Tomás-Hernández J, Monyart JM, Serra JT, Vinaixa MR, Farfan EG, García VM, Feliu EC. Large fracture of the anteromedial tibial plateau with isolated posterolateral knee corner injury: case series of an often missed unusual injury pattern. Injury. 2016. Sep;47(Suppl 3):S35-40. [DOI] [PubMed] [Google Scholar]
- 27.Yao X, Hu M, Liu H, Tang J, Yuan J, Zhou K. Classification and morphology of hyperextension tibial plateau fracture. Int Orthop. 2022. Oct;46(10):2373-83. [DOI] [PubMed] [Google Scholar]
- 28.Liu ZY, Zhang JL, Liu C, Cao Q, Shen QJ, Zhao JC. Surgical Strategy for Anterior Tibial Plateau Fractures in Hyperextension Knee Injuries. Orthop Surg. 2021. May;13(3):966-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bu G, Sun W, Lu Y, Cui M, Zhang X, Lu J, Zhang J, Sun J. Complications associated with hyperextension bicondylar tibial plateau fractures: a retrospective study. BMC Surg. 2021. Jun 25;21(1):299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li X, Song G, Li Y, Liu X, Zhang H, Feng H. The “Diagonal” Lesion: A New Type of Combined Injury Pattern Involving the Impingement Fracture of Anteromedial Tibial Plateau and the Injury of Posterior Cruciate Ligament and Posterolateral Corner. J Knee Surg. 2020. Jun;33(6):616-22. [DOI] [PubMed] [Google Scholar]
- 31.Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am. 1976. Mar;58(2):173-9. [PubMed] [Google Scholar]
- 32.Fanelli GC, Larson RV. Practical management of posterolateral instability of the knee. Arthroscopy. 2002. Feb;18(2)(Suppl 1):1-8. [DOI] [PubMed] [Google Scholar]
- 33.Amis AA, Bull AM, Gupte CM, Hijazi I, Race A, Robinson JR. Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2003. Sep;11(5):271-81. [DOI] [PubMed] [Google Scholar]
- 34.DeLee JC, Riley MB, Rockwood CA, Jr. Acute posterolateral rotatory instability of the knee. Am J Sports Med. 1983. Jul-Aug;11(4):199-207. [DOI] [PubMed] [Google Scholar]
- 35.Grood ES, Stowers SF, Noyes FR. Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am. 1988. Jan;70(1):88-97. [PubMed] [Google Scholar]
- 36.Petrigliano FA, Lane CG, Suero EM, Allen AA, Pearle AD. Posterior cruciate ligament and posterolateral corner deficiency results in a reverse pivot shift. Clin Orthop Relat Res. 2012. Mar;470(3):815-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Skyhar MJ, Warren RF, Ortiz GJ, Schwartz E, Otis JC. The effects of sectioning of the posterior cruciate ligament and the posterolateral complex on the articular contact pressures within the knee. J Bone Joint Surg Am. 1993. May;75(5):694-9. [DOI] [PubMed] [Google Scholar]