Abstract
Kinesiophobia, the fear of movement, can significantly impede an individual’s ability to engage in daily activities. This fear often stems from past traumatic experiences or witnessing others in pain, leading to an increased fear of injury. This study aimed to evaluate the psychometric properties of the Persian version of the Tampa Scale for Kinesiophobia among Iranian post-surgery patients. A methodological study conducted in 2023 involved a sample of 400 post-surgery patients selected through convenience sampling. The translated scale underwent psychometric evaluation, including network analysis, exploratory and confirmatory factor analysis for construct validity, as well as assessments for convergent and discriminant validity. Internal consistency of the scale was also assessed. The mean age of the participants was 44.38 (SD = 13.49) years and the majority of them (77.8%) were women. Exploratory factor analysis with Promax rotation identified two factors explaining 60.28% of the variance, comprising 17 items. The final model was confirmed after necessary adjustments in confirmatory factor analysis. Both convergent and discriminant validity were established, and alpha and omega coefficients of the subscales were above 0.7. The Persian version of the Tampa Scale for Kinesiophobia showed robust psychometric properties among Iranian post-surgery patients, serving as a valuable tool for evaluating and addressing kinesiophobia in this population. These findings enhance the understanding and management of kinesiophobia within the Iranian healthcare context.
Keywords: Fear of movement, Kinesiophobia, Network analysis, Psychometrics, Reliability, Validity
Subject terms: Diagnosis, Health services, Psychology
Introduction
Pain after surgery is a common experience for hospitalized patients1. According to the US Institute of Medicine, 80% of patients experience postoperative pain2, and studies have shown that a wide range of surgical procedures, including both soft tissue and hard tissue surgeries, can result in postoperative pain1,3–5. Despite advances in understanding the mechanisms of pain generation, identifying its prevalence, and methods of managing it, inadequate pain control remains common. This can lead to consequences such as increased mortality, the development of chronic pain, impaired function, surgical recovery disturbances, and decreased quality of life1.
One of the consequences patients may experience following pain, including postoperative pain, is kinesiophobia. Kinesiophobia is an unreasonable fear of movement and injury due to the perceived danger of pain6 and is a psychological construct in the Fear Avoidance Model7. In fact, following an acute pain experience, individuals may become trapped in a cycle of disability and suffering due to emotional, cognitive, behavioral, and functional responses to pain8. One component of this model, movement avoidance, occurs when pain is perceived as a threat, leading to avoidance, disability, and depression7.
Kinesiophobia affects 51 to 70 percent of chronic pain sufferers8. Individuals with this form of phobia tend to overreact to potential or actual threats and engage in avoidance behaviors that prevent injury or re-injury9. Initially, kinesiophobia was primarily associated with musculoskeletal pain and injuries, but over the years, research has been expanded to include other consequences related to kinesiophobia10. According to some studies, kinesiophobia can serve as a predictor of reduced quality of life, increased pain, and disability10,11. On the other hand, in other types of phobias, the patient is aware of the irrationality of their fear, but this is not the case with kinesiophobia, where the individual believes that the fear, resulting in decreased movement, is a healthy response, even though this decreased movement leads to numerous adverse effects8. Additionally, fear of movement and subsequently reduced mobility in surgical patients is associated with irreversible consequences such as thromboembolic events12 and immobility that leads to poor therapeutic outcomes13. Therefore, accurate measurement and appropriate management of kinesiophobia are essential.
Various tools have been designed to assess fear of movement, including the Fear-Avoidance Beliefs Questionnaire (FABQ)14, Kinesiophobia Causes Scale (KCS)15, and Fear-Avoidance Components Scale (FACS)16. One of the oldest available tools for measuring this construct is The Tampa Scale for Kinesiophobia (TSK)17. This 17-item questionnaire was initially designed to “distinguish between non-excessive fear and phobia related to movement in patients with chronic musculoskeletal pain”18. It is a commonly accepted model that is comprised of two factors: somatic focus and activity avoidance. Responses options include a 5-point Likert scale ranging from 0 (completely disagree) to 4 (completely agree). Items 4, 8, 12, and 16 are reverse-scored10. Shortened versions of TSK, the 13, 11, 6 and 4-item versions, have also been developed19–22.
This questionnaire has been translated and validated in various patient populations, in patients with temporomandibular disorders23, neck pain24, knee surgery25, chronic pain26, in anterior shoulder instability27, in patients with acute and chronic back pain6,19,28,29, children and adolescents undergoing major surgery30. The questionnaire exists in the following languages: Italian, Japanese, Swedish, Turkish, Chinese, Norwegian, Spanish, Greek, and Dutch6,10,31,32. In Iran, the Persian version of this questionnaire has been psychometrically evaluated in populations with chronic nonspecific low-back pain (17 and 11-item versions)19, in patients with neck pain (17-item version)24, and in patients with low-back pain (17-item version)29. However, a similar study focused on the psychometric properties of this questionnaire in surgical patients was not found. Therefore, this study aimed to psychometrically evaluate (construct, convergent and discriminant validity and reliability) of the 17-item version of The Tampa Scale for Kinesiophobia questionnaire in patients undergoing surgery.
Methods
Sample size and data collection
This cross-sectional methodological study was conducted between October 2023 and February 2024. A sample of 400 Iranian adults who had undergone surgery were recrited. A minimum sample size of 200 cases has been recommended for psychometric studies33. This decision was made to enhance statistical power and ensure more reliable estimates, as larger samples reduce the risk of Type I and Type II errors, unstable factor structures and improve generalizability across diverse populations34. Furthermore, recruiting 400 participants allowed us to fulfill the requirement for two different samples necessary for assessing construct validity effectively.
The participants were chosen using a convenience sampling method, which involved selecting individuals who were readily accessible and willing to participate in the study. While this approach can introduce potential selection bias and limit generalizability, we implemented a random selection process within this convenience sample. Thus participants were randomly selected from those available at the time of data collection, which aimed to enhance the representativeness of our sample relative to the broader population of surgical patients.
The research setting consisted of hospitals affiliated with Mazandaran University of Medical Sciences that have surgical wards, located in the city of Amol, Mazandaran, Iran. To access the research sample, the researcher visited the surgical wards of selected hospitals, and patients were chosen based on the inclusion criteria. The demographic questionnaire and TSK-P were completed by the patients with the guidance of the researcher.
Inclusion and exclusion criteria
The inclusion criteria for participants in this study were as follows: participants must be at least 18 years old, able to communicate in Farsi, literate, willing to volunteer for the study, and currently hospitalized in surgical wards after a surgical procedures, including orthopedic, abdominal, or thoracic surgeries. Exclusion criteria were determined based on medical history and self-reported information collected during the initial screening process. Patients were excluded if they had:
Cognitive disorders or reduced level of consciousness: These conditions could impair the patient’s ability to understand and accurately respond to the questionnaire items, compromising data validity.
Mental illnesses: Such as schizophrenia or anxiety disorders, which could independently influence fear-avoidance beliefs and responses.
Significant medical conditions: Including heart diseases (e.g., unstable angina), cerebrovascular diseases, neurological disorders, or rheumatoid arthritis, as these could directly impact physical function and pain experience.
Pregnancy or cancer: These conditions may require specialized medical management that could affect the patient’s physical and psychological status.
Substance use disorders: Drug addiction or dependencies could influence pain perception, coping mechanisms, and responses on the kinesiophobia scale.
The original version of the scale
The original version of TSK was conceptualized and developed by Miller17. This scale has been developed to assess the components of fear of movement. It has 17 items with a Likert scale scoring based on a four-point scale from 1 to 4: (I strongly disagree = 1), (I somewhat disagree = 2), (I somewhat agree = 3), (I strongly agree = 4). The scoring of items 4, 8, 12, and 16 is reversed. The total score ranges from 17 to 68 points. Also, it should be declared that the original version of this scale was designed for adults and adolescents. Two phases were used to assess the psychometric qualities and usefulness of the “Persian version of Tampa Scale for Kinesiophobia (TSK-P)”.
Translation
Subsequently, the scale was translated from English to Persian following the Gudmundsson35 translation protocol. Two proficient English-Persian translators independently translated the TSK into Persian. An expert panel, comprised of some authors of this article and two professional translators, meticulously reviewed and amalgamated the two translations to create a Persian version of the TSK.
To validate this translation, a qualified Persian-English translator, who were not involved in the initial translation, performed a back-translation of the TSK-P into English. This back-translated version was then reviewed by our expert panel, which discussed any discrepancies and ensured that both versions maintained conceptual equivalence. The panel’s involvement was crucial in refining item wording and ensuring cultural relevance for Iranian surgical patients. Finally, this revised version was approved by all members of the expert panel.
Normal distribution, outliers, and missing data
Skewness (± 3) and kurtosis (± 7) were used to individually investigate the univariate distribution of data. Also, the multivariate normality distribution was assessed by the Mardia coefficient of multivariate kurtosis (< 8). Mahalanobis d-squared (p < 0.001) was used to determine whether there were any multivariate outliers36. We employed the multiple imputation method to assess the presence of missing data37. The analysis confirmed that there were no missing values, indicating that all participants responded completely to the scale.
Construct validity
To test construct validity, the original dataset (n = 400) was randomly divided into two datasets with 200 cases each. With the first random dataset (n = 200), we employed Maximum Likelihood Exploratory Factor Analysis (MLEFA) with Promax rotation and Kaiser normalization. The choice of MLEFA was based on its effectiveness in estimating factor structures from continuous data, providing more reliable parameter estimates compared to other techniques such as Principal Component Analysis (PCA). MLEFA is particularly advantageous when assumptions of normality are met38, which aligns with our dataset characteristics. Furthermore, using Promax rotation allowed us to explore potential correlations among factors, facilitating a clearer understanding of the underlying dimensions of kinesiophobia.
To ensure that the data were suitable for factor analysis, we assessed the Kaiser–Meyer–Olkin (KMO) measure, which was found to be greater than 0.8, and conducted Bartlett’s test of sphericity, which yielded a significant result (p < 0.001)39. These tests confirmed the appropriateness of our dataset for factor analysis. For factor extraction, we employed parallel analysis, a robust method that involves generating a random correlation matrices to simulate data. This technique allowed us to compare the eigenvalues obtained from our actual data with those derived from the simulated datasets. Specifically, we conducted 1000 iterations to establish a 95th percentile cutoff for eigenvalues. Factors with eigenvalues greater than this threshold were considered meaningful and retained for further analysis. This approach minimizes the risk of over-extraction by ensuring that only those factors that exceeded chance levels were included in our model40.
Also, the Eigenvalues of more than 1, communalities of more than 0.2, and factor loadings of more than 0.3 were used for the factorability41,42. A communality threshold of 0.2 is generally deemed acceptable, especially in preliminary analyses, as it signifies that a factor accounts for at least 20% of the variability in an item, which is adequate for initial evaluations43. Likewise, a factor loading of 0.3 is commonly recognized as the minimum threshold, indicating a moderate relationship between an item and its underlying factor44.
Eigenvalues (λ) are the sum of squared factor loadings (SSL) across all items (k) for each factor. This represents the amount of variance in each item that can be explained by the analysis. To calculate the percentage of total variance explained by the factor, the Eigenvalue is divided by the total number of items45. The MLEFA was performed using SPSS version 27.
The exploratory graph analysis (EGA) methods were conducted to determine the factor structure. In the field of network psychometrics, EGA is a new method that determines the number of factors underlying multivariate data. EGA generates a network plot, which is a visual guide that displays how many factors should be kept, which items cluster together, and how strongly they are related46.
EGA offers several advantages over traditional factor analysis methods. Notably, it does not depend on rotation techniques that can produce varying results based on subjective choices. This feature allows for a more stable representation of the underlying structure. Furthermore, EGA has been demonstrated to provide comparable or superior performance in estimating dimensionality under various conditions, especially when item correlations are high or when dealing with smaller item sets47. The network plots produced by EGA facilitate easier interpretation by visually representing item interconnections and clustering patterns.
EGA generates a network plot, which visually displays the number of factors that are retained, based on the items that cluster together, and the strength of their relationship47. The estimation of EGA involves representing items as nodes, defining edges as the partial correlation between the nodes, and identifying communalities as clusters of connected nodes in multivariate data using undirected network models. EGA was estimated by applying the Graphical Least Absolute Shrinkage Optimization (GLASSO) method. This method involved the following steps48:
Identification of network nodes: The variables identified in the study as network nodes, representing the entities or concepts we wanted to analyze.
Construction of the network: The nodes were connected with links, representing the relationships or associations between the variables.
Descriptive analysis: Tools used in network science were employed to analyze the topology of the network, such as node centrality, clustering, and other measures.
Centrality measures: Including strength, closeness, and betweenness, were calculated to determine the importance of each node in the network.
Clustering analysis was performed to identify groups of nodes with similar characteristics or relationships.
Comparison of networks: Networks from different groups or conditions were compared to identify any significant differences in the structure and relationships between the variables48,49.
The following centrality and clustering measures were used for the network analysis:
Betweenness: This measure indicates the number of times a node lies on the shortest path between other nodes, revealing its role as a bridge between different parts of the network.
Closeness: Centrality measures the average distance between a node and all other nodes in the network, indicating its ability to reach other nodes quickly.
Strength: Centrality measures the sum of the weights of the connections of a node, indicating its overall influence in the network.
Expected influence: This metric estimates the potential impact of a node on the network, taking into account its strength and the centrality of its neighboring nodes.
Barabási: This centrality measure is derived from the Barabási-Albert model, which focuses on the growth and evolution of networks.
Onnela: This centrality measure is based on the Onnela-Kim centrality, which assesses the significance of a node based on its connectivity and the connectivity of its neighbors.
WS: The WS centrality measure, also known as the HITS algorithm, identifies nodes that serve as both authorities (highly connected to other nodes with high authority) and hubs (highly connected to other nodes with high hub scores).
Zhang: This centrality measure is built upon the Zhang-Zhou centrality, which evaluates the importance of a node in terms of its connectivity and the centrality of its neighbors. In this study, the EGA was conducted using JASP 0.18.3.0 software.
Confirmatory factor analysis (CFA)
In the next step, the factor structure obtained from MLEFA was analyzed and confirmed by conducting (CFA based on the second random dataset (n = 200) using AMOS version 27. The following model fit indices were used to assess the model fit: Parsimony Comparative Fit Index (PCFI), Parsimony Normed Fit Index (PNFI) and Comparative Fit Index (CFI) > 0.5, Normed Fit Index (NFI), and Incremental Fit Index (IFI) was > 0.9; that of Root Mean Square Error of Approximation (RMSEA) was < 0.08; and for Minimum Discrepancy Function divided by degrees of freedom (CMIN/DF) < 3 was considered good36,50.
Convergent, discriminant validity
For convergent validity, composite reliability (CR) should be greater than 0.7, and Average Variance Extracted (AVE) should be greater than 0.5 for each construct. Fornell and Larcker51 stated that for psychological constructs, if AVE is less than 0.5, but CR is more than 0.7, the convergent validity can be considered acceptable.
For discriminant validity, this study used the heterotrait-monotrait ratio (HTMT) of the correlations criterion, where the HTMT ratio between all constructs should be less than 0.85 to achieve discriminant validity52.
Reliability
A Cronbach’s alpha (α) and McDonald’s omega (Ω) along with Composite Reliability (CR) and Maximum Reliability (MaxR) values exceeding 0.7, indicated satisfactory internal consistency and construct reliability for the scale39.
Ethical approval
The Ethics Committee of Mazandaran University of Medical Sciences (Sari, Iran) approvedithis study (Ethics code: IR.MAZUMS.REC.1402.601). The participants were given a thorough explanation of the study’s goals and methods, as well as assurances that their participation was entirely voluntary. Written informed consent forms for participation in the study were filled out by patients or their caregivers. All procedures adhered to the appropriate guidelines and regulations.
Results
Demographic characters
The mean age of the participants was 44.38 (SD = 13.49) years. Among the participants 192 (48%) were women and 208 (52%) were men. Most people (n = 268, 67%) had an education level lower than a diploma. In the present study, 93 participants (23.25%) reported a history of having undergone surgery. The majority of participants were married (n = 334, 83.5%), and the mean body mass index (BMI) was 26.17 (SD = 4.31).
The independent t-test results demonstrated that there was no significant difference in kinesiophobia scores between male (mean = 46.35, SD = 14.88) and female participants (mean = 46.45, SD = 15.34), with p > 0.05. Furthermore, the Pearson correlation analysis indicated no significant relationship between kinesiophobia scores and the age of participants who underwent surgery (p > 0.05). These results imply that demographic factors such as gender and age do not significantly impact kinesiophobia levels in this population.
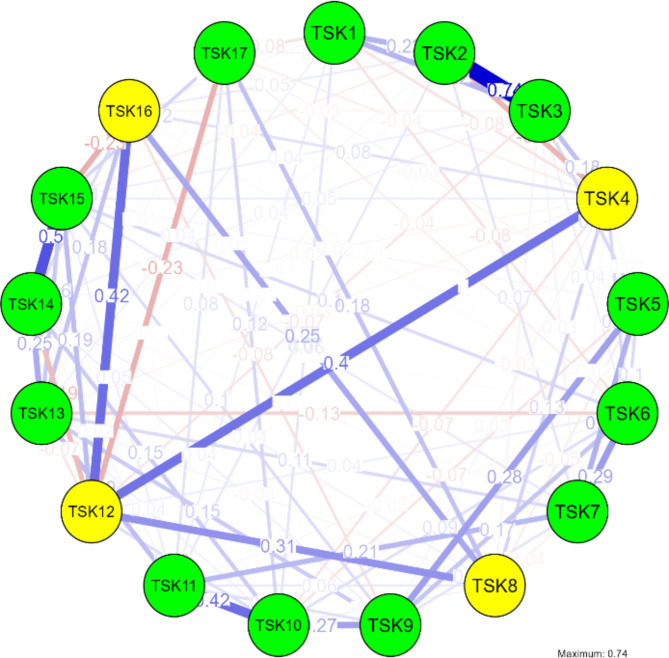
MLEFA
The results of MLEFA with Promax with Kaiser Normalization rotation using the first random dataset (n = 200) extracted three factors accounting for 60.28% of the variance comprising 17 items. Moreover, the results of the KMO (0.955) and Bartlett’s test of sphericity (p < 0.001, chi-square = 6649.181, df = 136) showed the sampling was adequate and appropriate for factor analysis. The detailed results of the MLEFA are shown in Table 1. Also, the EGA is shown in Fig. 1.
Table 1.
The result of MLEFA on the two factors Persian version of Tampa Scale for Kinesiophobia (n = 200).
| Factor | Items (Q) | Factor loading | h2 | λ | % Variance | Reliability |
|---|---|---|---|---|---|---|
| Fear and avoidance of pain-related injuries | TSK11. I wouldn’t have this much pain if there weren’t something potentially dangerous going on in my body | 0.958 | 0.881 | 7.51 | 44.17 |
α = 0.973 Ω = 0.975 |
| TSK9. I am afraid that I might injure myself accidentally | 0.948 | 0.857 | ||||
| TSK10. Simply being careful that I do not make any unnecessary movements is the safest thing I can do to prevent my pain from worsening | 0.932 | 0.849 | ||||
| TSK15. I can’t do all the things normal people do because it’s too easy for me to get injured | 0.930 | 0.814 | ||||
| TSK7. Pain always means I have injured my body | 0.928 | 0.828 | ||||
| TSK13. Pain lets me know when to stop exercising so that I don’t injure myself | 0.891 | 0.821 | ||||
| TSK14. It’s really not safe for a person with a condition like mine to be physically active | 0.888 | 0.850 | ||||
| TSK6. My accident has put my body at risk for the rest of my life | 0.796 | 0.514 | ||||
| TSK5. People aren’t taking my medical condition seriously enough | 0.794 | 0.644 | ||||
| TSK3. My body is telling me I have something dangerously wrong | 0.776 | 0.793 | ||||
| TSK2. If I were to try to overcome it, my pain would increase | 0.754 | 0.783 | ||||
| TSK1. I’m afraid that I might injury myself if I exercise | 0.671 | 0.707 | ||||
| TSK17. No one should have to exercise when he/she is in pain | 0.448 | 0.430 | ||||
| Perception of pain and physical activity | TSK12. Although my condition is painful, I would be better off if I were physically active | − 0.953 | 0.853 | 2.74 | 16.11 |
α = 0.896 Ω = 0.896 |
| TSK16. Even though something is causing me a lot of pain, I don’t think it’s actually dangerous | − 0.800 | 0.632 | ||||
| TSK. My pain would probably be relieved if I were to exercise | − 0.785 | 0.674 | ||||
| TSK. Just because something aggravates my pain does not mean it is dangerous | − 0.779 | 0.580 |
h2 Communalities, λ Eigenvalues.
Fig. 1.
Exploratory graph analysis by network analysis.
Network analysis
Centrality measures:
TSK1 has a high negative betweenness and closeness centrality, indicating its importance in connecting other variables in the network.
TSK4 and TSK12 have high positive betweenness and closeness centrality, suggesting their strong influence and connection to other variables in the network.
TSK17 has high negative betweenness and low closeness centrality, indicating its limited influence and connection to other variables in the network.
Clustering measures:
TSK1 has positive Barrat and Zhang clustering measures, indicating its tendency to form clusters or communities within the network.
TSK3 has negative Barrat and Onnela clustering measures, suggesting its low tendency to form clusters within the network.
TSK12 has high positive Barrat and Onnela clustering measures, indicating its strong tendency to form clusters or communities within the network (Tables 2, and 3).
Table 2.
Centrality measures per variable.
| Variable | Network | |||
|---|---|---|---|---|
| Betweenness | Closeness | Strength | Expected influence | |
| TSK1 | − 0.917 | − 2.104 | − 1.565 | − 1.605 |
| TSK2 | − 0.051 | − 0.472 | 0.413 | 0.336 |
| TSK3 | − 0.267 | − 0.662 | 0.683 | 1.392 |
| TSK4 | 2.113 | 1.309 | 0.497 | − 0.988 |
| TSK5 | − 0.267 | − 1.064 | − 1.448 | − 0.743 |
| TSK6 | − 0.267 | − 0.294 | − 0.341 | − 0.525 |
| TSK7 | − 0.592 | − 0.958 | − 0.695 | 0.569 |
| TSK8 | − 0.917 | − 0.724 | − 0.634 | − 0.168 |
| TSK9 | 0.166 | − 0.182 | − 0.201 | 0.870 |
| TSK10 | 0.598 | 0.323 | 0.379 | 0.745 |
| TSK11 | − 0.592 | − 0.273 | − 0.233 | 1.213 |
| TSK12 | 2.655 | 1.750 | 2.472 | 0.234 |
| TSK13 | 0.057 | 0.641 | 0.176 | 0.131 |
| TSK14 | − 0.484 | 0.933 | 0.122 | 0.307 |
| TSK15 | − 0.592 | 0.939 | 1.180 | 0.910 |
| TSK16 | 0.274 | 1.031 | 0.450 | − 0.375 |
| TSK17 | − 0.917 | − 0.191 | − 1.256 | − 2.302 |
Table 3.
Clustering measures per variable.
| Variable | Network | |||
|---|---|---|---|---|
| Barrat | Onnela | WS | Zhang | |
| TSK1 | 1.216 | − 0.965 | 0.969 | 2.153 |
| TSK2 | 1.305 | 0.338 | 1.495 | 0.292 |
| TSK3 | − 1.483 | − 1.054 | − 0.136 | 0.054 |
| TSK4 | − 0.262 | − 0.408 | − 0.983 | 0.446 |
| TSK5 | − 0.486 | − 0.353 | 0.050 | − 0.679 |
| TSK6 | − 0.018 | − 0.679 | − 0.347 | − 0.898 |
| TSK7 | − 0.575 | − 1.017 | − 1.045 | − 1.084 |
| TSK8 | − 1.359 | − 0.212 | − 1.133 | 1.597 |
| TSK9 | 0.272 | 1.830 | 1.495 | − 0.533 |
| TSK10 | − 1.425 | − 0.076 | − 0.607 | − 1.443 |
| TSK11 | − 0.827 | − 0.647 | − 1.483 | − 1.296 |
| TSK12 | 1.297 | 2.542 | 1.145 | − 0.128 |
| TSK13 | 0.289 | − 0.460 | − 0.157 | − 0.080 |
| TSK14 | 1.717 | 0.297 | 1.583 | 0.667 |
| TSK15 | 0.069 | 0.866 | − 0.506 | − 0.151 |
| TSK16 | 0.678 | 0.602 | 0.269 | 1.236 |
| TSK17 | − 0.409 | − 0.603 | − 0.607 | − 0.153 |
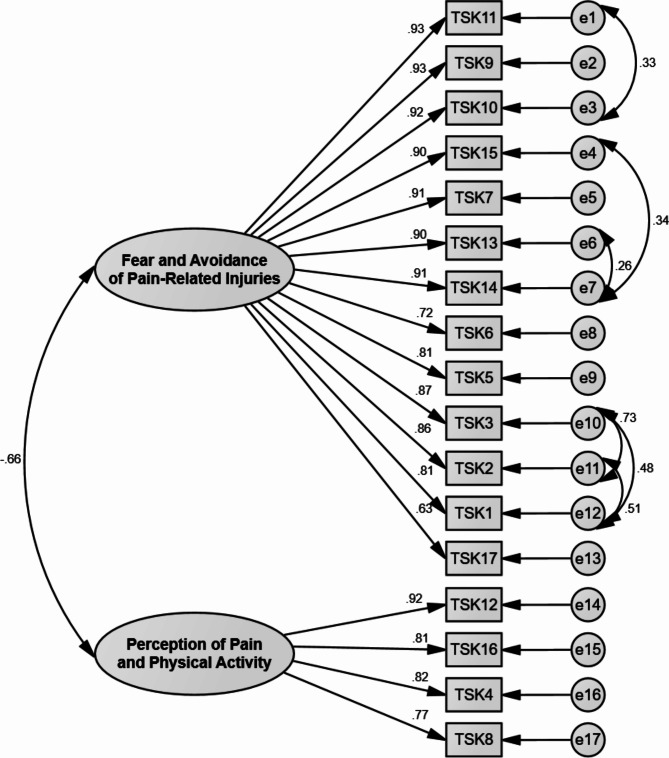
CFA
The CFA was conducted to confirm and validate the factor structure obtained from MLEFA using the second random dataset (n = 200). In the analysis section of the confirmatory factor analysis, correlations were drawn between the following pairs of errors to refine the model: errors 1 and 3, 4 and 7, 6 and 7, 10 and 11, 10 and 12, and 11 and 12 (Fig. 2). The results showed that the data fit the model well as evidenced by (χ2(112) = 237.022, p < 0.001, χ2/df = 2.116, PCFI = 0.769, PNFI = 0.783, CFI = 0.966, IFI = 0.9661, TLI = 0.959, RMSEA (90% C.I.): 0.074 [0.073, 0.086].
Fig. 2.
The results of the CFA and factor loadings.
Convergent, discriminant validity and reliability
The results showed that AVE for factor Fear and Avoidance of Pain-Related Injuries and Perception of Pain and Physical Activity were 0.737 and 0.689 respectively, indicating good convergent validity. As for discriminant validity, the results of the HTMT ratio showed that the correlation between Fear and Avoidance of Pain-Related Injuries and Perception of Pain and Physical Activity (0.685) was lower than 0.85, demonstrating good discriminant validity for the two constructs. As for construct reliability, Cronbach’s alpha, McDonald’s Omega, CR, and MaxR for all constructs were greater than 0.7, demonstrating good internal consistency and construct reliability. Also, McDonald’s Omega of all of the latent variables was in the acceptable range (Tables 1 and 4).
Table 4.
The results of the convergent validity and construct reliability (n = 200).
| Factors | CR | MaxR | AVE |
|---|---|---|---|
| Fear and avoidance of pain-related injuries | 0.973 | 0.980 | 0.737 |
| Perception of pain and physical activity | 0.898 | 0.914 | 0.689 |
Discussion
The present study evaluated the psychometric properties of the TSK in a sample of Iranian adult surgical patients. The findings of this study indicated that the TSK demonstrated both reliability and validity.
Cultural factors significantly influence the concept of kinesiophobia in patients who have undergone surgery. Kinesiophobia, defined as an irrational fear of movement due to concerns about pain or re-injury, can be shaped by various cultural beliefs and societal norms that dictate how individuals perceive pain, recovery, and physical activity.
In many cultures, including Iranian culture, beliefs about fate and spirituality can affect how individuals interpret pain and recovery. For instance, Iranian patients may view their experiences with pain as a spiritual test of faith, which can lead to a stoic approach to suffering and a reluctance to express vulnerability. This perspective may contribute to a higher tolerance for pain but could also exacerbate kinesiophobia if patients fear that movement might jeopardize their spiritual or physical well-being45.
Cultural norms regarding independence and self-reliance can further complicate the experience of kinesiophobia. In societies where there is a stigma associated with appearing weak or dependent on others, patients may be less likely to seek help or express fears related to their recovery53. This can lead to increased anxiety about movement and a greater likelihood of developing kinesiophobia as patients avoid activities that they perceive might expose them to judgment.
The interplay between cultural context and psychosocial factors such as anxiety, depression, and social support is crucial in understanding kinesiophobia. Cultural perceptions of mental health can affect how individuals express these emotions and seek help. In cultures where mental health problems are stigmatized, individuals may be less likely to acknowledge their fears or seek psychological support, thereby exacerbating kinesiophobia54.
The relationship between demographic factors such as gender and age with kinesiophobia in surgical patients is complex and has been explored in various studies55. In our research, we found no significant differences in kinesiophobia scores between male and female participants, nor was there a correlation with age. This finding is consistent with the work of Aleksić et al.55, which highlighted that while older age and female sex are often associated with higher levels of kinesiophobia, their influence can vary significantly across different populations and contexts. Specifically, they noted that factors such as lower education levels and negative coping styles may play a more critical role in predicting kinesiophobia than age or gender alone56. Additionally, a study by Silva et al.57 found that kinesiophobia levels did not significantly differ between genders in elderly females with chronic musculoskeletal pain, suggesting that sociocultural factors might influence these experiences. Furthermore, Higuchi et al.56 emphasized that while older adults may experience higher kinesiophobia due to declining cognitive and physical abilities, this does not uniformly apply to all surgical populations. These findings indicate that while age and gender are commonly considered risk factors for kinesiophobia, their impact may not be as pronounced in out surgical contexts, necessitating further investigation into how these demographic variables interact with psychological factors influencing kinesiophobia.
The results of the EFA revealed that the Persian version of the TSK consisted of two factors and exhibited adequate stability in assessing kinesiophobia in postoperative patients. This 17-item scale with two factors accounted for 60.28% of the total variance in kinesiophobia among Iranian surgical patients.
It is noteworthy that the TSK has been translated into various languages and utilized with participants presenting diverse medical conditions. Consequently, studies conducted in different countries have identified 2 or 3-factor structures, as well as 5-factor structures, in different versions, with varying levels of explained variances for this scale31,58,59. Gómez-Pérez et al., in the results of their initial factor analysis on the 17-item scale, found factor loadings below 0.3 for the reverse-scored items (items 4, 8, 12, and 16) and subsequently removed these items31. The results of the study by Houben et al., also showed that the reverse-scored items had weak inter-item correlations and, in the initial factor analysis, did not load together with other items on the same factor. Instead, they grouped together in a separate factor. As a result, they also removed these four items and conducted factor analysis using the 13-item version60. Similarly, Jafari et al., in their item analysis on Persian-version of the scale, achieved a better Cronbach’s alpha for the entire scale by removing these four items. As a result, they excluded these items in further analyses and examined the 13-item version29. However, in the present study, these four items were retained as they demonstrated acceptable factor analysis results. These discrepancies underscore the influence of cultural context and patient characteristics on the psychometric evaluation of the TSK. Consistent with prior research, the current study’s findings support the notion that the TSK possesses satisfactory psychometric properties.
The internal consistency analysis of the TSK yielded satisfactory results. Notably, the utilization of McDonald’s Omega in this study is advantageous as it is independent of sample size and the number of items61. The results of Askary-Ashtiani el al. study on the Persian version of the scale indicated a Cronbach’s alpha in the range of 0.77 to 0.7824. This level of alpha is lower than the Cronbach’s alpha obtained in the present study. In another study conducted on the Persian version of this scale, Jafari et al.'s study29, the overall Cronbach’s alpha for the 17-item version was 0.796. By removing 4 items, these researchers achieved a higher overall alpha of 0.831. In contrast, in the present study, both factors had an overall alpha higher than 0.8 with all 17 items included.
The first factors identified in the scale pertain to Fear and Avoidance of Pain-Related Injuries. It is well-established that fear and avoidance beliefs are closely linked to the perception of pain, particularly in cases of chronic pain62. Anticipation of severe pain often results in heightened vigilance and monitoring of pain sensations, potentially rendering even mild pain intolerable63. Items associated with this factor suggest that patients’ perceptions regarding postoperative pain may lead them to restrict their activities, thereby increasing the risk of postoperative immobility complications. Consequently, healthcare professionals should prioritize pain management in the immediate postoperative period and provide patients with appropriate guidance on postoperative activity levels to mitigate such risks.
The second factor, namely Perception of Pain and Physical Activity, highlights the significance of pain perception as a defensive mechanism signaling potential harm to tissues and hazardous conditions64.
The items associated with this factor underscores the importance of proper perception of pain post-surgery in facilitating effective planning for physical activity in patients. Consequently, pre-surgical interviews conducted by nurses can offer insights into patients’ anticipated pain perceptions post-surgery, enabling the reinforcement of positive attitudes toward pain. Moreover, addressing negative perceptions can be achieved through educational interventions, aiding patients in maintaining their physical activity levels following surgery.
The correlations drawn between the errors of items 10 and 11, 14 and 15, 13 and 14, as well as 1 and 2, and 1 and 3 in the TSK were instrumental in refining the confirmatory factor analysis model. These specific error correlations suggest that certain items may share common variance beyond what is accounted for by the underlying constructs of the scale. This finding aligns with the theoretical framework of kinesiophobia, which posits that fears related to movement and potential injury can manifest in interconnected ways among various items on the TSK. By addressing these correlations, we enhance the scale’s construct validity and ensure a more accurate representation of the psychological dimensions of kinesiophobia in surgical patients. This refinement is crucial for improving the assessment’s sensitivity to detect fear-related behaviors that may hinder rehabilitation outcomes.
In the modification of CFA, the interpretation of error measurement correlations is critical for understanding the underlying structure of the data. When specific items in a measurement model exhibit correlated errors, it suggests that these items share variance that is not accounted for by the latent constructs being measured. This shared variance may arise from common contextual factors, similar wording, or other systematic influences affecting responses65.
Including these error correlations in the CFA model can enhance its fit by acknowledging these additional relationships, thereby improving the model’s overall explanatory power. However, it also indicates potential redundancy among items, which could complicate the interpretation of the constructs. Ultimately, recognizing and addressing correlated errors helps refine the measurement model, leading to more accurate assessments of the psychological dimensions being studied, such as kinesiophobia in surgical patients66.
The study’s findings also indicate that the items within this scale demonstrate robust convergent and divergent validity. Items that reflect a particular construct should converge or share a high proportion of variance in common, known as convergent validity, while discriminant validity refers to the degree to which a construct is genuinely different from other constructs36.
Furthermore, the internal consistency coefficients of the scales dimensions reveal that the items within each factor exhibited strong internal correlations, elucidating and measuring a broader concept effectively. In essence, the items within each dimension sufficiently capture and assess a specific concept.
Conclusion
The Persian version of the TSK demonstrated acceptable construct validity and reliability. The scale is comprised of two factors encompassing 17 items, collectively explaining 60.28% of the total variance of kinesiophobia observed in post-surgery patients. This instrument holds potential utility for healthcare professionals, including doctors and nurses, in the identification of kinesiophobia among pre-surgical patients. By utilizing the TSK scale, healthcare providers can effectively educate patients before the surgery to mitigate fear, thereby reducing the risk of immobility-related complications post-surgery. It is recommended that future studies evaluate other psychometric properties of the Persian version of the scale in Persian-speaking populations.
Limitations
The lack of evaluation of other psychometric properties, such as test–retest reliability and responsiveness of the scale, is also considered another limitation of this research. The utilization of a four-point scale in the TSK restricts respondents’ ability to convey neutral opinions, potentially biasing the data towards either agreement or disagreement. This constrained-choice format may fail to fully grasp the subtleties of participants’ fear of movement, thereby impacting the accuracy of the results and their applicability to wider demographics. Subsequent research endeavors could enhance their methodology by implementing an odd-numbered scale to accommodate a neutral response alternative.
Clinical implications
Enhanced pre-operative management
The findings of the study offer valuable insights for healthcare professionals in identifying and effectively managing kinesiophobia in patients by preparing then for surgery. By addressing this fear of movement, healthcare providers can potentially reduce complications and enhance the overall recovery process.
Optimized rehabilitation programs
The study emphasizes the significance strategies to kinesiophobia into post-operative rehabilitation programs. By doing so, patients can experience improvements in their functional capacity and overall quality of life.
Tailoring interventions
By pinpointing specific factors and indicators associated with kinesiophobia, healthcare professionals can develop targeted interventions tailored to each patient’s needs. For instance, implementing pre-operative inspiratory muscle training can effectively address kinesiophobia and lead to better outcomes for patients undergoing surgery.
Supplementary Information
Acknowledgements
We sincerely thank all the patients who participated in this study; their cooperation was invaluable in advancing our research. This article stems from research project code 18553, with ethical approval IR.MAZUMS.REC.1402.601, from the Student Research Committee of Mazandaran University of Medical Sciences. We also express our gratitude to Mazandaran University of Medical Sciences for their support and approval of this project.
Author contributions
Performance of data gathering: Poorya Nowrozi; Planning and supervision of the work: Hamid Sharif-Nia; Performance of the analysis: Hamid Sharif-Nia; Manuscript draft: Reza Fatehi, Sima Hejazi, and Esmail Hosseinzadeh; and comment on the final manuscript: Erika Sivarajan Froelicher and All authors.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-78407-1.
References
- 1.Gan, T. J. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J. Pain Res.10, 2287–2298 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Medicine Committee on Advancing Pain Research, Care and Education. The National Academies Collection: Reports funded by National Institutes of Health. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research (National Academies Press (US), 2011). [PubMed]
- 3.Apfelbaum, J. L., Chen, C., Mehta, S. S. & Gan, T. J. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth. Analg.97(2), 534–540 (2003). [DOI] [PubMed] [Google Scholar]
- 4.Gan, T. J., Habib, A. S., Miller, T. E., White, W. & Apfelbaum, J. L. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr. Med. Res. Opin.30(1), 149–160 (2014). [DOI] [PubMed] [Google Scholar]
- 5.Gerbershagen, H. J. et al. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology118(4), 934–944 (2013). [DOI] [PubMed] [Google Scholar]
- 6.Georgoudis, G., Raptis, K. & Koutserimpas, C. Cognitive assessment of musculoskeletal pain: validity and reliability of the Greek version of the Tampa scale of kinesiophobia in patients suffering from chronic low back pain. Maedica (Bucur)17(4), 826–832 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldberg, P. et al. Kinesiophobia and its association with health-related quality of life across injury locations. Arch. Phys. Med. Rehabil.99(1), 43–48 (2018). [DOI] [PubMed] [Google Scholar]
- 8.Bordeleau, M. et al. Treatments for kinesiophobia in people with chronic pain: A scoping review. Front. Behav. Neurosci.16, 933483 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luque-Suarez, A., Martinez-Calderon, J. & Falla, D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br. J. Sports Med.53(9), 554–559 (2019). [DOI] [PubMed] [Google Scholar]
- 10.Liu, H. et al. Fear of movement/(re)injury: an update to descriptive review of the related measures. Front. Psychol.12, 696762 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong, W. S., Chow, Y. F., Chen, P. P., Wong, S. & Fielding, R. A longitudinal analysis on pain treatment satisfaction among Chinese patients with chronic pain: predictors and association with medical adherence, disability, and quality of life. Qual. Life Res.24(9), 2087–2097 (2015). [DOI] [PubMed] [Google Scholar]
- 12.Higgins, R. M., Helm, M., Gould, J. C. & Kindel, T. L. Preoperative immobility significantly impacts the risk of postoperative complications in bariatric surgery patients. Surg. Obes. Relat. Dis.14(6), 842–848 (2018). [DOI] [PubMed] [Google Scholar]
- 13.Cao, J. et al. Factors associated with death in bedridden patients in China: A longitudinal study. PLoS One15(1), e0228423 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waddell, G., Newton, M., Henderson, I., Somerville, D. & Main, C. J. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain52(2), 157–168 (1993). [DOI] [PubMed] [Google Scholar]
- 15.Knapik, A., Saulicz, E. & Gnat, R. Kinesiophobia—introducing a new diagnostic tool. J. Hum. Kinet.28, 25–31 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neblett, R., Mayer, T. G., Hartzell, M. M., Williams, M. J. & Gatchel, R. J. The Fear-avoidance Components Scale (FACS): development and psychometric evaluation of a new measure of pain-related fear avoidance. Pain Pract.16(4), 435–450 (2016). [DOI] [PubMed] [Google Scholar]
- 17.Miller, R. P., Kori, S. H. & Todd, D. D. The Tampa Scale: a measure of kinisophobia. Clin. J. Pain7(1) (1991).
- 18.Hudes, K. The Tampa Scale of Kinesiophobia and neck pain, disability and range of motion: a narrative review of the literature. J. Can. Chiropr. Assoc.55(3), 222–232 (2011). [PMC free article] [PubMed] [Google Scholar]
- 19.Mohsen, A., Farshad, O., Aliyeh, D., Akbarzadeh, B. A. Comparison of psychometric properties of the original and brief version of the Tampa Scale for kinesiophobia. J. Mod. Rehab. 17(3) (2023).
- 20.Eiger, B., Errebo, M., Straszek, C. L. & Vaegter, H. B. Less is more: reliability and measurement error for three versions of the Tampa Scale of Kinesiophobia (TSK-11, TSK-13, and TSK-17) in patients with high-impact chronic pain. Scand. J. Pain23(1), 217–224 (2023). [DOI] [PubMed] [Google Scholar]
- 21.Le Carré, J. et al. Development and Validation of Short Forms of the Pain Catastrophizing Scale (F-PCS-5) and Tampa Scale for Kinesiophobia (F-TSK-6) in musculoskeletal chronic pain patients. J. Pain Res.16, 153–167 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dupuis, F., Cherif, A., Batcho, C., Massé-Alarie, H. & Roy, J. S. The Tampa Scale of Kinesiophobia: a systematic review of its psychometric properties in people with musculoskeletal pain. Clin. J. Pain39(5), 236–247 (2023). [DOI] [PubMed] [Google Scholar]
- 23.Aguiar, A. S., Bataglion, C., Visscher, C. M., Bevilaqua Grossi, D. & Chaves, T. C. Cross-cultural adaptation, reliability and construct validity of the Tampa scale for kinesiophobia for temporomandibular disorders (TSK/TMD-Br) into Brazilian Portuguese. J. Oral Rehabil.44(7), 500–510 (2017). [DOI] [PubMed] [Google Scholar]
- 24.Askary-Ashtiani, A., Ebrahimi-Takamejani, I., Torkaman, G., Amiri, M. & Mousavi, S. J. Reliability and validity of the Persian versions of the fear avoidance beliefs questionnaire and Tampa Scale of Kinesiophobia in patients with neck pain. Spine (Phila Pa 1976) 39(18), E1095–E1102 (2014). [DOI] [PubMed]
- 25.Cai, L. et al. Cross-cultural adaptation, reliability, and validity of the Chinese version of the Tampa Scale for kinesiophobia-11 among patients who have undergone total knee arthroplasty. J. Arthroplasty34(6), 1116–1121 (2019). [DOI] [PubMed] [Google Scholar]
- 26.French, D. J., France, C. R., Vigneau, F., French, J. A. & Evans, R. T. Fear of movement/(re)injury in chronic pain: a psychometric assessment of the original English version of the Tampa scale for kinesiophobia (TSK). Pain127(1–2), 42–51 (2007). [DOI] [PubMed] [Google Scholar]
- 27.van Iersel, T. P., Larsen van Gastel, M., Versantvoort, A., Hekman, K. M. C., Sierevelt, I. N., Broekman, B. F. P. et al. The modified Tampa-scale of kinesiophobia for anterior shoulder instability. Arthrosc. Sports Med. Rehabil.5(4), 100768 (2023). [DOI] [PMC free article] [PubMed]
- 28.Swinkels-Meewisse, E., Swinkels, R., Verbeek, A., Vlaeyen, J. & Oostendorp, R. Psychometric properties of the Tampa Scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Manual Therapy8(1), 29–36 (2003). [DOI] [PubMed] [Google Scholar]
- 29.Jafari, H., Ebrahimi, I., Salavati, M., Kamali, M. & Fata, L. Psychometric properties of Iranian version of Tampa Scale for kinesiophobia in low back pain patients. USWR11(1) (2010).
- 30.Rosenbloom, B. N. et al. Fear of movement in children and adolescents undergoing major surgery: A psychometric evaluation of the Tampa Scale for Kinesiophobia. Eur. J. Pain24(10), 1999–2014 (2020). [DOI] [PubMed] [Google Scholar]
- 31.Gómez-Pérez, L., López-Martínez, A. E. & Ruiz-Párraga, G. T. Psychometric properties of the Spanish version of the Tampa Scale for Kinesiophobia (TSK). J. Pain12(4), 425–435 (2011). [DOI] [PubMed] [Google Scholar]
- 32.Haugen, A. J., Grøvle, L., Keller, A. & Grotle, M. Cross-cultural adaptation and validation of the Norwegian version of the Tampa scale for kinesiophobia. Spine (Phila Pa 1976) 33(17), E595–E601 (2008). [DOI] [PubMed]
- 33.MacCallum, R. C., Widaman, K. F., Zhang, S. & Hong, S. Sample size in factor analysis. Psychol. Methods4(1), 84–99 (1999). [Google Scholar]
- 34.Wolf, E. J., Harrington, K. M., Clark, S. L. & Miller, M. W. Sample size requirements for structural equation models: an evaluation of power, bias, and solution propriety. Educ. Psychol. Meas.76(6), 913–934 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gudmundsson, E. Guidelines for translating and adapting psychological instruments. Nord. Psychol.61(2), 29–45 (2009). [Google Scholar]
- 36.Hair Jr, J., Black, W., Babin, B. & Anderson, R. Multivariate Data Analysis, 8th edn (Cengage Learning EMEA, 2018).
- 37.Patrician, P. A. Multiple imputation for missing data. Res. Nurs. Health25(1), 76–84 (2002). [DOI] [PubMed] [Google Scholar]
- 38.Muthén, L. K. & Muthén, B. O. How to use a Monte Carlo study to decide on sample size and determine power. Struct. Equ. Model.9(4), 599–620 (2002). [Google Scholar]
- 39.Yaghoobzadeh, A. et al. Cross-cultural adaptation and psychometric evaluation of the Herth Hope Index within a sample of Iranian older peoples. Int. J. Aging Hum. Dev.89(4), 356–371 (2019). [DOI] [PubMed] [Google Scholar]
- 40.Çokluk Bökeoğlu, Ö. & Koçak, D. Using Horn’s parallel analysis method in exploratory factor analysis for determining the number of factors. Educ. Sci. Theory Pract. 16(2) (2016).
- 41.Sharif Nia, H. et al. Psychometric evaluation of the Persian version of religious orientation scale in iranian patients with cancer. J. Religion Health60(5), 3658–3674 (2021). [DOI] [PubMed] [Google Scholar]
- 42.Plichta Kellar, S. & Kelvin, E. Munro’s Statistical Methods for Health Care Research, 6th edn (Wolter Kluwer, 2012).
- 43.Hair, J., Anderson, R., Black, B. & Babin, B. Multivariate Data Analysis (Pearson Education, 2016).
- 44.Field, A. Discovering Statistics Using IBM (SPSS Statistics: North American Edition: SAGE Publications, 2017).
- 45.Sharif-Nia, H. et al. Statistical concerns, invalid construct validity, and future recommendations. Nurs. Pract. Today11(1), 16–21 (2024). [Google Scholar]
- 46.Golino, H. et al. Investigating the performance of exploratory graph analysis and traditional techniques to identify the number of latent factors: A simulation and tutorial. Psychol. Methods25(3), 292 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Golino, H. F. & Epskamp, S. Exploratory graph analysis: A new approach for estimating the number of dimensions in psychological research. PLoS One12(6), e0174035 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Borsboom, D. et al. Network analysis of multivariate data in psychological science. Nat. Rev. Methods Primers1(1), 58 (2021). [Google Scholar]
- 49.Hevey, D. Network analysis: a brief overview and tutorial. Health Psychol. Behav. Med.6(1), 301–328 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hosseini, L., Sharif Nia, H. & Ashghali, F. M. Development and psychometric evaluation of family caregivers’ hardiness scale: a sequential-exploratory mixed-method study. Front. Psychol.13, 807049 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fornell, C. & Larcker, D. F. Evaluating structural equation models with unobservable variables and measurement error. J. Market. Res.18(1), 39–50 (1981). [Google Scholar]
- 52.Henseler, J., Ringle, C. M. & Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Market. Sci.43(1), 115–135 (2015). [Google Scholar]
- 53.Morley, S., Eccleston, C. & Williams, A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain80(1–2), 1–13 (1999). [DOI] [PubMed] [Google Scholar]
- 54.Longo, U. G. et al. Preoperative and postoperative kinesiophobia influences postoperative outcome measures following anterior cruciate ligament reconstruction: a prospective study. J. Clin. Med.12(14), 4858 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Aleksić, M. et al. Understanding kinesiophobia: predictors and influence on early functional outcomes in patients with total knee arthroplasty. Geriatrics9(4), 103 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Higuchi, D., Kondo, Y., Watanabe, Y. & Miki, T. Sex differences in the mediating effect of kinesiophobia on chronic pain, dysesthesia, and health-related quality of life in Japanese individuals aged 65 years old and older treated with surgery for lumbar spinal stenosis. J. Pain Res. 1845–1854 (2022). [DOI] [PMC free article] [PubMed]
- 57.Silva, N. S., Abreu, S. S. E. & Suassuna, P. D. Kinesiophobia and associated factors in elderly females with chronic musculoskeletal pain: pilot study. Rev. Dor. 17(3), 188–191 (2016).
- 58.Mintken, P. E., Cleland, J. A., Whitman, J. M. & George, S. Z. Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with shoulder pain. Arch. Phys. Med. Rehab.91(7), 1128–1136 (2010). [DOI] [PubMed] [Google Scholar]
- 59.Siqueira, F. B., Teixeira-Salmela, L. F., Magalhães, L. C. Analysis of the psychometric properties of the Brazilian version the tampa scale for kinesiophobia. Acta Ortopédica Brasileira 15, 19–24 (2007).
- 60.Houben, R. M., Leeuw, M., Vlaeyen, J. W., Goubert, L. & Picavet, H. S. Fear of movement/injury in the general population: factor structure and psychometric properties of an adapted version of the Tampa Scale for Kinesiophobia. J. Behav. Med.28(5), 415–424 (2005). [DOI] [PubMed] [Google Scholar]
- 61.Hoseinzadeh, E., Sharif-Nia, H., Ashktorab, T. & Ebadi, A. Development and psychometric evaluation of nurse’s intention to care for patients with infectious disease scale: an exploratory sequential mixed method study. BMC Nurs.23(1), 65 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sharif-Nia, H. et al. The Persian version of the fear-avoidance beliefs questionnaire among Iranian post-surgery patients: a translation and psychometrics. BMC Psychol.12(1), 390 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zale, E. L. & Ditre, J. W. Pain-related fear, disability, and the fear-avoidance model of chronic pain. Curr. Opin. Psychol.5, 24–30 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen, Y.-C. et al. Transcriptional regulator PRDM12 is essential for human pain perception. Nat. Genet.47(7), 803–808 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brown, T. A. Confirmatory Factor Analysis for Applied Research, 2nd edn (Guilford Publications, 2015).
- 66.Byrne, B. M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming (Lawrence Erlbaum Associates, 2001).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.