Abstract
Background:
Charles Bonnet syndrome (CBS) refers to the experience of visual hallucinations occurring secondary to sight loss. Although there is an increasing amount of research on this phenomenon, CBS remains a lesser-known outcome of visual impairment, with limited research into the impact on the patient.
Objectives:
To explore the experiences and opinions of visually impaired military veterans with CBS regarding the impact of visual hallucinations.
Design:
Semi-structured qualitative interviews.
Methods:
Forty-six telephone interviews were conducted with members of Blind Veterans UK, a charity for visually impaired ex-service men and women. One-hundred and fifteen individuals at the charity with CBS were identified and invited to a semi-structured interview (participation rate – 40%). Qualitative data was transcribed and analysed using thematic analysis.
Results:
Four overarching themes were identified: (1) impact of CBS (2) understanding and management of CBS (3) awareness of CBS (4) recommendations. Negative impact of CBS included feelings of fear, annoyance and disruptions to daily life and quality of life. Negative appraisal of CBS was not necessarily related to negative hallucination content. Participants expressed the value of increased awareness amongst patients and health care professionals. Knowledge and understanding of CBS provided reassurance and was considered an effective strategy to mitigate the negative impact of the condition.
Conclusion:
Regardless of hallucination content, CBS has a substantial impact on the lives of people with visual impairment. Increased awareness and information can help to support individuals to manage their CBS more effectively. However, the findings from this study cannot be generalized to people without a military background so further research is required to understand and optimize support for military veterans and civilians with CBS.
Keywords: Charles Bonnet syndrome, hallucinations, veterans
Introduction
Charles Bonnet syndrome (CBS) is a condition where individuals with visual impairment experience simple and/or complex visual hallucinations, despite having no cognitive or neurodegenerative condition. 1 Simple hallucinations are common 2 and may include flashes of light, dots and patterns, whereas complex hallucinations may include formed images of people, animals and detailed landscapes. 3 Prevalence estimates vary; however, it is generally considered that 11%–15% of patients with sight loss experience CBS. 4 Globally, it is estimated that there are 47 million individuals currently living with CBS, 5 and it is projected that there are as many as 1 million cases in the United Kingdom (UK). 6 The precise pathophysiology remains unknown; however, the primary mechanism is considered to be alterations in functional connectivity or cortical excitability as the visual system adapts to reduced input. 7 Although pharmacological treatments and other interventions have been proposed,8–10 evidence regarding their effectiveness is limited. 8
Despite its prevalence, awareness of the condition amongst healthcare professionals (HCPs) is low.11,12 In one study of 499 Canadian family physicians, more than half (54.7%) indicated they were not at all aware of CBS, despite almost three-quarters (72.8%) attending to patients with visual hallucinations within the last year. 11 Family physicians and general practitioners (GPs) have limited training on CBS, and there have been calls for increased education and awareness amongst all HCPs regarding the condition. 8 Limited awareness of CBS extends also to patients with visual impairment, 13 which often results in a hesitancy in speaking to HCPs for fear of being labelled ‘insane’. 14
The impact of CBS can be highly heterogenous. Patients may report feeling unperturbed by their hallucinations, or even enjoy their occurrence. 15 Conversely, hallucinations can cause a negative impact, partly due to their disruptive effects on daily activities. 16 For some, visual hallucinations can be troubling, particularly when they first occur, even though patients generally understand that the images are not real. 15 Hallucinations that are long-lasting or constant have been described as being ‘irritating’. 16 A study by Randeblad et al., demonstrated that glaucoma patients with CBS reported significantly reduced vision-related quality of life compared to patients without CBS. 17 However, it was unclear which aspects of CBS were more significantly associated with lower quality of life. Patients with CBS also report issues with mental health, whereby an increased incidence of anxiety 18 and depressive symptoms 19 have been identified, as well as a greater use of medication to manage these symptoms. 20
Limited research has explored factors that are associated with troubling or concerning hallucinations. Hallucination content has been explored in relation to structural changes in the brain, 21 whereby functional magnetic resonance imaging (fMRI) indicates hallucinations may reflect the functional specialization of the activated region. For example, hallucinations of colours, faces, textures and objects correlate with cerebral activity in the ventral extrastriate visual cortex. 19 Despite an association between non-CBS related auditory hallucinations and life events, particularly in military veterans with post-traumatic stress disorder (PTSD),22,23 the role of personal experiences in hallucination content has not been taken into consideration. In fact, there is very limited research on hallucinations and personal experiences, outside of CBS, where the data are even more scarce.
There is estimated to be ~12,000 visually impaired military veterans in the UK. The health profile of military veterans is considered unique, partly due to their increased risk of sensory loss,24,25 and the impact of adverse occupational exposure on their mental health. 26 In addition, CBS is associated with an increased risk of experiencing mental health problems, such as anxiety, 27 and mental health conditions occur more frequently among military veterans than the general populations. 28 Taken together, this evidence suggests CBS occurring in military veterans may have a more detrimental impact on mental health amongst this cohort. From a lived experience perspective, it is interesting to understand the nature of visual hallucinations and their impact. The aim of this study was to qualitatively investigate the impact and management of CBS amongst a sample of visually impaired military veterans. In addition, we aimed to gain insights into how veterans with CBS would like care to be improved in the future, to help address and reduce the negative impact of the condition.
Methods
Study design
The study was reviewed and approved by London-Fulham Research Ethics Committee (21/PR/0693). To date, studies on CBS have mainly been survey-based using closed-ended questions, with limited qualitative research providing a detailed understanding of lived experiences. 29 A qualitative design was used where beneficiaries of Blind Veterans UK were recruited to a semi-structured telephone interview. Blind Veterans UK is a charity based in the United Kingdom providing lifelong support and rehabilitation to veterans living with sight loss. Eligible members are military veterans who lost their sight in service or having acquired sight loss after leaving the armed forces. The sight loss criteria for membership is Snellen visual acuity (VA) of equal to or worse than 6/60 in one eye and 6/24 in the other, or to have been issued a certificate of vision impairment (i.e. official documentation from an eye care specialist in the United Kingdom used to certify someone as sight impaired). Veterans with preserved VA but substantial visual field loss may also be admitted through a review process with the charity’s ophthalmic consultant. The study was designed and reported following the guidance of the Consolidated Criteria for Reporting Qualitative Research. 30
Participants: Beneficiaries at Blind Veterans UK with a record of CBS were invited to the study. Participants were recruited from a database of charity members who had previously been screened and identified as living with CBS using the Charles Bonnet Syndrome Screening Questionnaire. 31 A total of 461 suspected cases of CBS were present in the database, wherein 115 had undergone screening and case confirmation and were invited to the interview. Participants were contacted only once to take part and those that were unavailable were not recontacted. Participants that reported experiencing simple hallucinations (e.g. shapes and patterns), complex hallucinations (e.g. faces, people, animals) or both 32 were considered to have CBS and were included in the study. Participants were not included in the study if they experienced only photopsia and basic visual phenomena such as flashes of light as these could be due to other conditions such as retinal detachment.
A total of 46 interviews were conducted and analysed. The participants were predominantly male (n = 39; 84.8%) and none lived alone. The average age of participants was 79.9 years and most lived in England (n = 43; 93.48%). The age and gender profile of our sample was representative of the overall population of beneficiaries at Blind Veterans UK. Participant demographics, including main military branch, are shown in Table 1.
Table 1.
Participant demographic information with percentage frequencies.
| Sex | N (%) |
| Male | 39 (84.8%) |
| Female | 7 (15.2%) |
| Age | Mean years (SD) |
| 79.9 (11.7) | |
| Marital status | N (%) |
| Single | 1 (2.17%) |
| Married | 26 (56.52%) |
| Widowed | 13 (28.26%) |
| Divorced | 2 (4.35%) |
| Partner | 2 (4.35%) |
| Military branch | N (%) |
| The British Army | 21 (45.65%) |
| Royal Navy | 9 (19.57%) |
| Royal Airforce | 14 (30.43%) |
| Visual acuitya,b | LogMAR (SD) |
| Average better eye visual acuity | 1.0 logMAR (0.9) |
| Average worse eye visual acuity | 1.8 logMAR (0.9) |
| Underlying conditions b | N (%) |
| Age related Macular Degeneration | 24 (52.17%) |
| Glaucoma | 10 (21.73%) |
| Retinal pigmentosa | 2 (4.35%) |
| Diabetic retinopathy | 2 (4.35%) |
| Other | 4 (8.7%) |
| Not available | 4 (8.7%) |
Based on n = 42 as visual acuity information was not available for four participants.
Information based on records from when participants first joined Blind Veterans UK and may have changed since.
SD, standard deviation.
Data collection
Participants underwent one semi-structured interview via telephone, lasting for approximately 40 min. Data were collected between August to November 2023. Interviews were conducted by author LDF, a female hospital-based counsellor with training in psychology. No relationship was established between the researcher and the participants prior to beginning the study. An interview topic guide was developed which included open-ended questions about the phenomenology of hallucinations and individuals’ appraisal of their CBS. Audio-recorded interviews were transcribed using a transcription service (Sterling Transcription Ltd. www.sterlingtranscription.co.uk).
Data analysis
Data saturation was defined as the point where no new information was coded during transcript analysis, which was based on the judgement of the research team and indicated further data collection or analysis was unnecessary. Transcripts were analysed thematically using the qualitative data analysis software (NVivo12 www.qsrinternational.com/nvivo12). Transcripts were read and re-read by one author (SD) to identify key themes and patterns in each interview. Content analysis was completed by coding meaningful tests to form ‘nodes’ and once completed for all interviews, an analytical framework was created by grouping nodes together to form themes, allowing for better interpretation of the data. The nodes and themes were reviewed independently by another researcher (CC) and disagreements were taken to a third researcher (LJ), who also reviewed the analytical framework. The final framework for the analysis was agreed upon by all the researchers.
Results
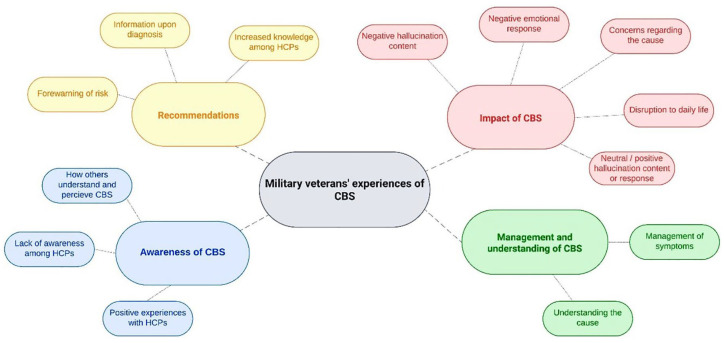
Four major themes were identified: (1) impact of CBS (2) management and understanding of CBS (3) awareness of CBS (4) recommendations. Figure 1 displays a diagram of the major themes and corresponding subthemes.
Figure 1.
Diagram illustrating the major and subthemes identified in the interviews.
(1) Impact of CBS
Negative emotional responses to CBS
Many participants expressed a strong emotional response to their hallucinations. It was common for hallucinations to disrupt daily life causing feelings of confusion, fear and concern during an episode of CBS:
I wouldn’t know what room I was in. I was just totally confused and very frightened. Extremely frightened. –P40
It frightened the life out of me. I just could not move, I felt like I was going to fall down this hole that was on both sides of me. –P19
In addition to disrupting daily life, it was common for participants to feel frightened due to the fearsome content of their hallucinations. These negative hallucinations were described by 17 out of 46 participants. Images which evoked a fearful response were often macabre or alarming in nature, such as screaming faces, mythological creatures, and puppets:
What I see now is a face. It’s a screaming face, that’s all. Rushes at me from the left, straight up to me. There’s no sound but it’s screaming. –P6
I see a smashed face, all bleeding and blood pouring from a face. –P11
I’ve seen killers, these killers and they’re sitting in the room with me. –P24
I was seeing gargoyles, those things you have on buildings, those awful creatures. –P21
There were cases where hallucinations were described as ‘tormenting’ participants and causing a negative impact, including when trying to enjoy hobbies:
The one that worries me most of all is the one that torments me, it’s hundreds of little puppets, wooden puppets and the little girl ones all dressed in pretty dresses. I’m a football fan, so when I’m watching football all these dozens of little puppets mingle in with the footballers. –P9
A further concern was that hallucinations were associated with cognitive or neurological problems, thus, cultivating a belief among participants that they were not of sound mind:
‘Sometimes I don’t know if I’m in a waking dream or it’s Charles Bonnet or I’m just losing the plot altogether.’ –P3
I wondered what was happening, was I going mad or something? –P8
Negative emotional responses were exacerbated when participants struggled to distinguish between reality and their hallucinations. At times, a feeling about the presence of another being would manifest:
I just get this feeling that they’re there. I’ve only got to hear something scurrying about. It could be the kids playing next door and things like that but I’m thinking, where is it. Where is it? –P27
From my point of view it’s an annoyance and it makes you wonder, to a certain extent, what you really are seeing and what you are imagining. Whether things are real images or not. –P13
Feelings of annoyance and exhaustion were also described. These reactions followed occasions where hallucinations were disruptive to daily life, or causing frustration due to their persistence:
This Charles Bonnet thing it was a nuisance at first, it really was, it was a pain because I couldn’t see people’s faces, I could portray another face on top of them. –P24
It was really frustrating. I can understand why it’s your brain that’s putting these things into you, but sometimes I wish I could get rid of them, and you can’t get rid of them. It can get frustrating sometimes. –P29
I was wiped out from having these constant images in my eyesight. You can’t escape it. It’s there all the time. You shut your eyes; it’s still there. –P45
Further examples of CBS causing disruption were evident when participants described potentially hazardous situations, whereby hallucinations had caused distraction or were interfering with their field of vision:
Well, I love cooking. I can be cooking, and all of a sudden, a pattern comes in front of me, and I can’t see what I’m doing. –P42
It’s dangerous in the street because I have to cross two very busy roads when I leave this house to get to where I want to go to. The bus stop, the shops, the bank, the library or whatever. With traffic coming up and you’re seeing other things you’re not really paying much attention. –P36
Additionally, participants expressed a concern regarding their quality of life and progressive severity of their CBS as their vision worsens:
What worried me that basically my quality of life had gone because of this wretched complaint. –P12
I’ve totally lost the vision in my left eye now, so it’s just my right eye, and yet the images do seem to be getting more realistic. Again, trying to get from A to B by myself, it can be very distracting, but they said there’s nothing they can do about it at the moment –P3
Although many participants did not describe hallucinations that were upsetting or fear-inducing in nature, concerns remained regarding the wider impact of hallucinations on activities of daily living and well-being.
Neutral or positive responses to hallucinations
In contrast, several participants described positive feelings towards hallucinations such as feelings of fascination or joy:
The visions that I could see, the colours and the butterflies – it’s still hard to explain now, but it was fantastic. −P16
People have asked me what I can see, I explain it’s like you’ve got a beautiful net over you with all coloured lights on it. Yeah, it makes you look very good. −P23
Circumstances where participants felt positive or neutral appeared to be linked to the content of their hallucinations. In some case, vivid colours or pleasant scenery such as flowers and plants were described:
I can describe it as a wallpaper. It’s a blue with darker blue or purple like stipples. – P2
I used to look at the apple tree and all of a sudden there’d be something else there instead of the apple tree. It’s a plant of some sort, it’s a plant with flowers on it. – P22
I’ve had the experience of a dog that jumped off the chair and it walked over to me wagging its tail . . . Then I’ve seen a cat, not all black, but a smoky black cat. −P2
The last ones I really saw was, there was an elderly person in a big, purple gown, and there was four little children, all in purple, with a hoodie on. −P28
In these situations, participants relished their CBS episodes which sometimes brought comforting feelings:
Oh, it was incredible. It was a fantastic journey. −P16
I’m quite happy with the coloured lights floating around, that’s okay. That’s what I usually go to sleep with. -P35
It was lovely waking up in the night, opening your eyes up and seeing the net in the room. -P37
Interestingly, a small proportion reported experiencing military-related hallucinations. These images typically related to items or memories from serving in the armed forces which were generally described in neutral terms:
When I see the rock formations, that was like being in the army, I used to do mountaineering. −P29
It looks like the radar screen that I looked at. I watched the path of planes going across the screen, you know, when they took off. −P36
Although, most participants did not believe that their military background impacted on their hallucinations:
I don’t think my experience in the military or the fire service has made any difference to my Charles Bonnet. –P6
(2) Management and understanding of CBS
Management of symptoms
Twenty-eight participants described their experiences of managing and coping with hallucinations. Amongst these, some used management techniques recommended to them by their HCP, such as closing their eyes or distracting themselves when a hallucination appears in the hope it would alleviate the symptoms:
I’ve just got to look away, shut my eyes −P2
I thought, well, I’ll look away. I’ll put my head down. Then I’d look back and it’d be gone. If I moved my head or my eyes rapidly from side to side, they would go. −P6
We just have to do our exercises that I’ve been told to do, and hopefully it subsides. −P18
Participants also described interacting with their hallucinations as a mitigation strategy, or to reaffirm their understanding that the images were not real:
Well, I talk to them, I ask them a question, who are you, what do you want? Then they’re gone. On one occasion I did feel threatened, and I struck out, but again there was nothing there. −P15
I would want to step in front of it because for me, I always remember the lady at the [hospital] told me the coping mechanism is to reach out and try and touch it. This was my idea, if I stand in front of it, it’s not going to touch me because it’s not real −P46
Another common strategy for managing hallucinations was using head movements or distraction techniques. However, the effectiveness of this approach was variable.
The only way to get rid of it is if you stay looking at it, it’ll stay there. You have to look away and look at something else and go back to see if it’s gone. −P22
I used to sort of screw my eyes up and then look again, but that doesn’t make any difference because they’re not in your eyes, they’re actually in your head, so it makes no difference. −P26
I tried to move my head up and down and that, but it works sometimes. It doesn’t work others. −P29
I always try and do something. Okay, I put the sewing machine on, I’m keeping my mind occupied, and things like that. −P11
Understanding of CBS
Many participants reported that accepting their condition and gaining an understanding of it was the most effective way of coping with CBS. This was due to the reduction of fear about what was happening and attempting to stay rational in their response to hallucinations:
Yeah, that’s how I cope with it. I just think to myself they’re not there, you’re just being silly. −P27
But I know it’s nothing – it’s not real. As long as you can tell people, keep reminding yourself it’s not real. −P45
In general, feelings of positivity stemmed from a sense of relief after being diagnosed with CBS, as this allowed participants to gain an understanding of what they were living with, removing the fear that they were ‘going crazy’.
You give something a name; you tend to be able to live with it a bit better. −P40
I know exactly how I felt, I felt relieved. I have to be honest, I felt so relieved when they told me because then you’re thinking, so I’m not crazy then. −P46
Despite a number of management techniques being described, these were not always effective or helpful to mitigate the impact of CBS. Understanding and accepting their diagnosis was, however, described as helpful for the management of the negative feelings associated with the condition.
(3) Awareness of CBS
There was recognition of an overall lack of awareness among HCPs abut CBS, leading to limited information provision to patients. Thirty-eight participants described having experiences with clinicians that did not have an understanding of CBS and/or associated management strategies. This appeared to be most common amongst GPs:
I mentioned it to my GP, and she had never heard of it. −P4
I was dead shocked when my GP said, I don’t know nothing about it. He said, I’ve heard of it, but I don’t know nothing about it. −P18
On the other hand, participants described ophthalmologists and optometrists as being more aware of CBS:
I think it’s no use getting the GPs to do it, because they’re just going to refer you to an eye specialist anyway. But I think perhaps opticians seem to understand it far better. −P6
Participants also expressed concerns about the lack of awareness of visual impairment and CBS among other people, leading to a reluctance to disclose their hallucinations out of concerns for how they would be perceived:
It is a bit irritating, I don’t tell many people about it, because they don’t understand me about being blind, never mind anything else. They say all the right things like, oh dear, and isn’t that a shame, and how do you manage, but really, they haven’t got a clue. −P26
(4) Recommendations
A range of recommendations were proposed by participants based on their lived experiences of CBS and their interactions with HCPs. First, concerns were raised over practitioners’ lack of awareness of CBS, whereby many participants believed that future experiences for patients could be improved if practitioners had greater knowledge of the condition:
Increased knowledge of Charles Bonnet syndrome, especially in an eye department. Like I had somebody there to explain things to me, but not everybody’s going to be that fortunate. −P16
I think across the board, an hour to two, just on Charles Bonnet, just to give them a little bit of understanding. −P18
Second, participants recalled their own experiences of being diagnosed and receiving little or no information regarding CBS:
Well when I mentioned it to the doctors, they didn’t explain a great deal, they just said that’s what you’ve got, Charles Bonnet and that’s all, he never gives information. −P19
It’s been dismissed in a one-word sentence, that’s it, you’ve got it, we can’t do anything about it, get on with it, basically. −P40
To address this, participants felt that clinicians could provide patients with more information on CBS when they are diagnosed with their visual impairment to forewarn them about the risk and what to expect:
I think just information really. It’s like anything, if you’ve got a heads up of what might happen, you’re not as alarmed about it. −P3
Something that could be improved, when people go blind or they know they’re going to go blind, I think Charles Bonnet ought to be mentioned to people so they know what to expect, and don’t get frightened by it. −P40
The positive experiences described by participants who had received helpful information and support from clinicians underline the need for more information-provision at the point of diagnosis:
They said to me, the problem you’ve got, you’re not going mad, you’ve got Charles Bonnet syndrome. This is something that happens to you when you’re losing your sight because your brain compensates and gives you these images to see, he said. That was it. He said it affects people in different ways. Sometimes you get coloured lights going across your eyes and things like this. Which I’d had for some time. −P12
That was a real good experience. [The optometrist] was the first person who I actually felt confident that, thank goodness, I’ve got someone here that is listening to me and could possibly help me through this situation. –P45
Learning that CBS is a common complication of sight loss was also a source of comfort for participants:
It’s nice to know that other people have got it. It doesn’t make me feel as if I’m quite loopy. –P36
Finally, to facilitate greater knowledge of CBS, participants described the importance of disclosing what they are going through and participating in research and being able to contribute towards the understanding of CBS:
I do think that when we have these things, we should try to help other people before they get it. It really is not a comfortable thing to have. —P21
Unfortunately, there’s no cure for it, but just remember - talk about it. Talk about it to friends, neighbours. If necessary, to a talking therapist, if that helps. But just accept it as part of your blindness, and not to be so terrified of it. –P40
To improve the experiences of patients diagnosed with CBS in the future, participants believed that greater knowledge is needed amongst HCPs and patients themselves, and that there should be additional support and information at the point when individuals are first diagnosed with their visual impairment.
Discussion
Previous research shows that hallucinations that are scary in nature are more likely to bring about negative emotions. 14 This study highlights that visual hallucinations experienced by a sample of visually impaired military veterans with CBS do not need to be negative in content for the impact to be significant. The causes of positive or negative hallucination content have been explored previously in the context of auditory hallucinations, where negative voices have been associated with adverse life experiences, such as earlier traumatic life-events, physical or sexual abuse. 22 Besides few cases using neuroimaging assessment, 19 little research has been done to understand the mechanisms responsible for the content of visual hallucinations. Participants’ appraisal of their hallucination content was often neutral, even the military related hallucinations were neutral, and usually depicted scenery or equipment rather than scary or trauma-related imagery. A negative impact remained due to their frequency, disruption to daily life and concerns about a psychological cause, referring to them as ‘frightening’, ‘exhausting’ or ‘worrying’. Our findings align with previous studies identifying a negative impact of CBS,1,33 due to fears and disruption to daily living, 16 including an increased risk of depressive symptoms and a loss of independence. 19 Over a third of participants described negative hallucinations, such as bloodied faces and puppets. These hallucinations evoked a strong emotional response and were described as ‘tormenting’ or ‘freaky’. Nonetheless, the findings from this study suggest that the content of the hallucinations is seldom the only cause of a negative emotional response, which may arise from a lack of understanding and awareness of CBS amongst participants, peers, and HCPs.
An underlying theme present throughout the current findings was the importance of awareness of CBS. Awareness had a significant impact on participant responses to CBS and provided a basis for the most effective management of hallucinations, as well as being a priority area for the future recommendations. Upon receiving an accurate diagnosis of CBS and information about the condition, fear was reduced. In line with previous research, 40 participants in this study highlighted the benefits of forewarning about CBS at the point of diagnosis with a visual impairment. This is consistent with previous research showing the importance of patient awareness in avoiding the negative effects of CBS. 18 For example, Cox and Ffytche 16 showed that patients with a lack of prior knowledge of CBS were more likely to have negative outcomes than those who had prior knowledge, regardless of hallucination content. 16 Moreover, once patients understood that their hallucinations were caused by the brain adjusting to sight loss, participants expressed a greater ability to cope with their CBS. Yet, previous research suggests that patients are hesitant to speak to medical professionals due to the fear of being misdiagnosed and labelled with a psychiatric condition. 34 Visual hallucinations have a broad differential diagnosis such as schizophrenia, seizures 35 and other conditions with overlapping symptoms. A diagnosis of CBS may also be impeded by associations between visual hallucinations and lewy body dementia.36,37 Indeed, a major concern for participants was the fear that the hallucinations were due to a neurodegenerative or psychiatric condition (‘feeling like they were going crazy’).
Although this has not been explored in research, military veterans may be particularly reluctant to discuss their hallucinations with an HCP. Previous research on health-seeking behaviours among veterans with musculoskeletal and psychological conditions has found a significant culture of under-reporting,38,39 while pre-conditioning and military training may equip veterans to be more resilient to distressing hallucinations. 40 Notably, military veterans may be at an elevated risk of certain neurological conditions,41–43 which may increase diagnostic uncertainty and misdiagnosis when visual hallucinations present amongst this cohort. Moreover, veterans experiencing CBS who are aware of their increased risk of neurological problems may be reluctant to seek medical assistance due to fears of receiving this diagnosis, or concerns about misdiagnosis. A recent meta-analysis reported that female gender is a risk factor for CBS, 29 which has also been reported elsewhere. 44 However, these findings could be due to ‘male-gender behaviour’ where men, particularly veterans in the age group of our participants, could be less likely to report symptoms than women. 43 Participants in our study reported a lack of discussion with their HCP regarding CBS, but this could also be explained by a reluctance from the participants’ perspective too.
A diagnosis of CBS in military veterans may also be more difficult due to the prevalence of post-traumatic stress disorder (PTSD) in veteran populations. Approximately 10% of patients diagnosed with PTSD will experience auditory or visual hallucinations; however, the hallucinations are often accompanied by symptoms of psychosis (50%–90% of cases). 46 As discussed, people with CBS will have no psychological symptoms but the presence of hallucinations and a military background may result in misdiagnoses. Similarly, in previous research, 11 HCPs encountering patients with visual hallucinations typically referred them to counselling or psychiatric services more often than referring to an eye care professional. Practitioners also expressed a need for more education on CBS that they could then provide to patients. 11 In the current study, eye care practitioners were felt to be more informed about CBS than GPs and were reported to have provided better support to participants, underlining the need for further training HCPs on CBS and its impact. 47
As well as a diagnosis and awareness of CBS, participants described using a range of management and coping strategies, but the effectiveness of these was mixed. Exercises described in previous research include frequent blinking or rapid eye movements, changing light levels to increase visual input and alerting/distraction techniques. 48 However, there is limited evidence for the effectiveness of these techniques, despite participants in our study employing them. The theoretical underpinning for these exercises relate to behavioural principles in cognition and have been described as being effective for auditory hallucinations, where distractions inhibit hallucinations as attentional resources are redirected due to the introduction of competing stimuli. 49 Additionally, research on visual hallucinations in neurodegenerative conditions suggests a relationship with altered sensory input (bottom-up information) and existing knowledge (top-down information) in the visual system. 50 Further research is required on distraction techniques to generate an evidence base regarding the effectiveness of this strategy for visual hallucinations. The most effective management strategy described by our participants was having a greater awareness of CBS.
The findings from our study suggest there was a limited impact of military experience on CBS, and the feelings towards military-related hallucinations were equivalent to those relating to non-military-related hallucinations. This finding is consistent with previous research that hallucination content is influenced by the visual environment due to images generally being embedded in existing scenes, rather than personal experiences. 51
Several recommendations can be drawn from the study to improve CBS management in the future. Based on these findings, the following recommendations (Table 2) are provided:
Table 2.
Recommendations for how CBS management can be improved in the future.
| Recommendations |
| • Provide patients with information about CBS at the time of diagnosis with a visual impairment (forewarning). |
| • Improve training among HCPs interacting with people with visual impairment to increase awareness and ensure sufficient and accurate information is provided to patients with CBS. Educational materials and CPD training would provide practitioners with sufficient information to be able to support patients at onset of symptoms. |
| • Referral to counselling or community support groups where necessary. Patients should be pointed to peer support groups or non-profit organisations such as Esme’s Umbrella (www.charlesbonnetsyndrome.uk/about) which aim to highlight the lesser-known aspects of CBS. |
| • More research is required to determine the efficacy of existing and alternative management strategies for hallucinations. |
CBS, Charles Bonnet syndrome; CPD, Continuing professional development; HCP, healthcare professionals.
This study has limitations. First, we included only visually impaired military veterans from a specific UK based charity. This was primarily due to funding from the Military Veterans’ Health Innovation Fund seeking to fund research specific to the needs and recommendations for UK military veterans. Therefore, the findings from this study cannot be generalized to other people with visual impairment and no military experience. Second, as the participants in this study were all military veterans, it is important to consider PTSD as a factor that may affect the study findings. Although a question on ‘military related hallucinations’ was included to help identify potential PTSD, no specific PTSD assessments were completed. Similarly, although participants with a known diagnosis of dementia were excluded, information about what medications participants were taking was not collected, and it is known that some medications can cause hallucinations. Another limitation of this study was the lack of visual field data and updated VA information. Members of Blind Veterans UK undergo ophthalmic screening when joining the charity, but do not undergo repeated assessments. Therefore, the VA for the participants in this study may have been outdated and visual field data was not collected. Additionally, we recruited only those who were members of a charity who are therefore already in a position of receiving care/rehabilitation. This cohort could differ from those who are not engaged with charities. There was also a low participation rate (46/115; 40%), meaning that the findings may not be generalizable to the population. Lastly, participants average age was ~80 years; thus, the findings may not be representative of younger people’s experiences.
CBS has potential to considerably impact on the lives of people with visual impairment. Aside from distressing hallucination content, the impact of CBS can be affected by individual appraisals of hallucinations, disruption to daily life, and uncertainty surrounding the cause of the hallucinations. The condition may be managed through behavioural techniques with varying degrees of success. Yet the most effective strategy appeared to be staying informed about CBS and understanding the normalcy of experiencing hallucinations as a consequence of sight loss. Experiences can be improved in the future by providing patients with information about CBS at the time of diagnosis of their visual impairment and increasing education among practitioners. These recommendations may help to bolster resilience and reduce the negative effects of CBS on patients’ mental health and in turn could improve patients’ quality of life.
Acknowledgments
We would like to thank Blind Veterans UK for their assistance with recruitment for this study. We would also like to acknowledge the contributions from all of the participants that took part in this study and provided valuable insights.
Footnotes
ORCID iDs: Sonali Dave  https://orcid.org/0000-0002-2420-3991
https://orcid.org/0000-0002-2420-3991
Lee Jones  https://orcid.org/0000-0002-8030-1211
https://orcid.org/0000-0002-8030-1211
Mariya Moosajee  https://orcid.org/0000-0003-1688-5360
https://orcid.org/0000-0003-1688-5360
Renata SM Gomes  https://orcid.org/0000-0002-9197-8279
https://orcid.org/0000-0002-9197-8279
Contributor Information
Sonali Dave, BRAVO VICTOR, Research, London, UK; City, University of London, Department of Optometry and Visual Sciences, UK.
Lee Jones, BRAVO VICTOR, Research, London, UK; University College London, Institute of Ophthalmology, London, UK.
Matthew Lee, BRAVO VICTOR, Research, London, UK; Blind Veterans UK, London, UK.
Lara Ditzel-Finn, BRAVO VICTOR, Research, London, UK; Great Ormond Street Hospital for Children, NHS Foundation Trust, London, UK.
Claire Castle, BRAVO VICTOR, Research, London, UK.
Nikki Heinze, BRAVO VICTOR, Research, London, UK.
Judith Potts, Esme’s Umbrella, London, UK.
Mariya Moosajee, University College London, Institute of Ophthalmology, London, UK; Moorfields Eye Hospital NHS Foundation Trust, London, UK; The Francis Crick Institute, London, UK.
Renata S. M. Gomes, Northumbria University, Northern Hub for Veterans and Military Families Research, Newcastle, UK.
Declarations
Ethics approval and consent to participate: This study was reviewed and approved by London-Fulham Research Ethics Committee (21/PR/0693). Informed verbal consent to participate was obtained for all participants.
Consent for publication: All participants provided informed consent for the publication of anonymised data and quotes to be used in the publication of this study.
Author contributions: Sonali Dave: Formal analysis; Validation; Visualization; Writing – original draft; Writing – review & editing.
Lee Jones: Conceptualisation; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing – review & editing.
Matthew Lee: Conceptualisation; Data curation; Investigation; Methodology; Project administration; Resources; Writing – review & editing.
Lara Ditzel-Finn: Data curation; Investigation; Methodology; Project administration; Resources; Writing – review & editing.
Claire Castle: Formal analysis; Supervision; Validation; Writing – review & editing.
Nikki Heinze: Supervision; Validation; Visualization; Writing – review & editing.
Judith Potts: Conceptualisation; Validation; Writing – review & editing.
Mariya Moosajee: Conceptualisation; Validation; Writing – review & editing.
Renata S. M. Gomes: Conceptualisation; Funding acquisition; Grant Management; Validation; Writing – review & editing.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Office of Veteran Affairs (OVA) Veterans’ Health Fund. The competitive grant was awarded and managed by the Defence and Security Accelerator (DASA), Ministry of Defence, United Kingdom.
Competing interests: The authors declare that there is no conflict of interest.
Availability of data and materials: Anonymised data may be made available upon request.
References
- 1. Jones L, Ditzel-Finn L, Enoch J, et al. An overview of psychological and social factors in Charles Bonnet syndrome. Ther Adv Ophthalmol 2021; 13: 25158414211034715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Urwyler P, Nef T, Müri R, et al. Visual hallucinations in eye disease and Lewy body disease. Am J Geriatr Psychiatry 2016; 24(5): 350–358. [DOI] [PubMed] [Google Scholar]
- 3. Ffytche DH. Visual hallucinatory syndromes: past, present, and future. Dialogues Clin Neurosci 2007; 9(2): 173–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Manford M, Andermann F. Complex visual hallucinations. Clinical and neurobiological insights. Brain 1998; 121(Pt.10): 1819–1840. [DOI] [PubMed] [Google Scholar]
- 5. Subhi Y, Nielsen MA, Scott DAR, et al. Prevalence of Charles Bonnet syndrome in low vision: a systematic review and meta-analysis. Ann Eye Sci 2022; 7: 12. [Google Scholar]
- 6. Potts J. Charles Bonnet Syndrome: so much more than just a side effect of sight loss. Ther Adv Ophthalmol 2019; 11: 2515841419886257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Firbank MJ, daSilva Morgan K, Collerton D, et al. Investigation of structural brain changes in Charles Bonnet Syndrome. Neuroimage Clin 2022; 35: 103041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eperjesi F, Akbarali N. Rehabilitation in Charles Bonnet syndrome: a review of treatment options. Clin Exp Optom 2004; 87(3): 149–152. [DOI] [PubMed] [Google Scholar]
- 9. Holroyd S, Sabeen S. Successful treatment of hallucinations associated with sensory impairment using gabapentin. J Neuropsychiatry Clin Neurosci 2008; 20(3): 364–366. [DOI] [PubMed] [Google Scholar]
- 10. daSilva Morgan K, Schumacher J, Collerton D, et al. Transcranial direct current stimulation in the treatment of visual hallucinations in Charles Bonnet syndrome: a randomized placebo-controlled crossover trial. Ophthalmology 2022; 129(12): 1368–1379. [DOI] [PubMed] [Google Scholar]
- 11. Gordon KD, Felfeli T. Family physician awareness of Charles Bonnet syndrome. Fam Pract 2018; 35(5): 595–598. [DOI] [PubMed] [Google Scholar]
- 12. Voit M, Jerusik B, Chu J. Charles Bonnet Syndrome as another cause of visual hallucinations. Cureus 2021; 13(1): e12922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Singh A, Subhi Y, Sørensen TL. Low awareness of the Charles Bonnet syndrome in patients attending a retinal clinic. Dan Med J 2014; 61(2): A4770. [PubMed] [Google Scholar]
- 14. Menon GJ. Complex visual hallucinations in the visually impaired: a structured history-taking approach. Arch Ophthalmol 2005; 123(3): 349–355. [DOI] [PubMed] [Google Scholar]
- 15. Carpenter K, Jolly JK, Bridge H. The elephant in the room: understanding the pathogenesis of Charles Bonnet syndrome. Ophthalmic Physiol Opt 2019; 39(6): 414–421. [DOI] [PubMed] [Google Scholar]
- 16. Cox TM, ffytche DH. Negative outcome Charles Bonnet syndrome. Br J Ophthalmol 2014; 98(9): 1236–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Randeblad P, Singh A, Peters D. Charles Bonnet syndrome adversely affects vision-related quality of life in patients with glaucoma. Ophthalmol Glaucoma 2024; 7(1): 30–36. [DOI] [PubMed] [Google Scholar]
- 18. Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Surv Ophthalmol 2003; 48(1): 58–72. [DOI] [PubMed] [Google Scholar]
- 19. Jackson ML, Bassett K, Nirmalan PK. Charles Bonnet hallucinations: Natural history and risk factors. Int Congress Ser 2005; 1282: 592–595. [Google Scholar]
- 20. Geueke A, Morley MG, Morley K, et al. Anxiety and charles bonnet syndrome. J Visual Impairment Blindness 2012; 106(3): 145–153. [Google Scholar]
- 21. Ffytche DH, Howard RJ, Brammer MJ, et al. The anatomy of conscious vision: an fMRI study of visual hallucinations. Nat Neurosci 1998; 1(8): 738–742. [DOI] [PubMed] [Google Scholar]
- 22. Larøi F, Thomas N, Aleman A, et al. The ice in voices: understanding negative content in auditory-verbal hallucinations. Clin Psychol Rev 2019; 67: 1–10. [DOI] [PubMed] [Google Scholar]
- 23. Crompton L, Lahav Y, Solomon Z. Auditory hallucinations and PTSD in ex-POWS. J Trauma 2017; 18(5): 663–678. [DOI] [PubMed] [Google Scholar]
- 24. Raza Z, Hussain SF, Gomes RSM. Prevalence of dual sensory impairment in veterans: a rapid systematic review. Front Rehabil Sci 2024; 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lucas JW, Zelaya CE. Hearing difficulty, vision trouble, and balance problems among male veterans and nonveterans. Natl Health Stat Report 2020(142): 1–8. [PubMed] [Google Scholar]
- 26. Inoue C, Shawler E, Jordan CH, et al. Veteran and military mental health issues. StatPearls. Treasure Island (FL): StatPearls Publishing, 2024. [PubMed] [Google Scholar]
- 27. Bou Khalil R, Richa S. [Psychiatric, psychological comorbidities of typical and atypical Charles-Bonnet syndrome]. Encephale 2011; 37(6): 473–480. [DOI] [PubMed] [Google Scholar]
- 28. Rhead R, MacManus D, Jones M, et al. Mental health disorders and alcohol misuse among UK military veterans and the general population: a comparison study. Psychol Med 2022; 52(2): 292–302. [DOI] [PubMed] [Google Scholar]
- 29. Niazi S, Krogh Nielsen M, Singh A, et al. Prevalence of Charles Bonnet syndrome in patients with age-related macular degeneration: systematic review and meta-analysis. Acta Ophthalmol 2020; 98(2): 121–131. [DOI] [PubMed] [Google Scholar]
- 30. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19(6): 349–357. [DOI] [PubMed] [Google Scholar]
- 31. Cantin S, Duquette J, Dutrisac F, et al. Charles Bonnet syndrome: development and validation of a screening and multidimensional descriptive questionnaire. Can J Ophthalmol 2019; 54(3): 323–327. [DOI] [PubMed] [Google Scholar]
- 32. Ffytche DH. Visual hallucinations and the Charles Bonnet syndrome. Curr Psychiatry Rep 2005; 7(3): 168–179. [DOI] [PubMed] [Google Scholar]
- 33. Gilmour G, Schreiber C, Ewing C. An examination of the relationship between low vision and Charles Bonnet syndrome. Can J Ophthalmol 2009; 44(1): 49–52. [DOI] [PubMed] [Google Scholar]
- 34. Kester EM. Charles Bonnet syndrome: case presentation and literature review. Optometry 2009; 80(7): 360–366. [DOI] [PubMed] [Google Scholar]
- 35. Borruat FX. [Visual hallucinations and illusions, symptoms frequently misdiagnosed by the practitioner]. Klin Monbl Augenheilkd 1999; 214(5): 324–327. [DOI] [PubMed] [Google Scholar]
- 36. Brucki SMD, Takada LT, Nitrini R. Charles Bonnet syndrome: case series. Dement Neuropsychol 2009; 3(1): 61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kaya D, Dokuzlar O, Kaya M, et al. An elderly patient with Charles Bonnet Syndrome misdiagnosed as Lewy Body Dementia. Acta Neurol Belg 2020; 120(4): 1011–1013. [DOI] [PubMed] [Google Scholar]
- 38. Smith L, Westrick R, Sauers S, et al. Underreporting of musculoskeletal injuries in the US Army: findings from an infantry brigade Combat Team Survey Study. Sports Health 2016; 8(6): 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Warner CH, Appenzeller GN, Grieger T, et al. Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Arch Gen Psychiatry2011; 68(10): 1065–1071. [DOI] [PubMed] [Google Scholar]
- 40. McDaniel JT, Hascup ER, Hascup KN, et al. Psychological resilience and cognitive function among older military veterans. Gerontol Geriatr Med 2022; 8: 23337214221081363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hussain SF, Raza Z, Cash ATG, et al. Traumatic brain injury and sight loss in military and veteran populations – a review. Mil Med Res 2021; 8(1): 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Raza Z, Hussain SF, Ftouni S, et al. Dementia in military and veteran populations: a review of risk factors—traumatic brain injury, post-traumatic stress disorder, deployment, and sleep. Mil Med Res 2021; 8(1): 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Raza Z, Hussain SF, Foster VS, et al. Exposure to war and conflict: The individual and inherited epigenetic effects on health, with a focus on post-traumatic stress disorder. Front Epidemiol 2023; 3: 1066158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Abdulhussein D, Jones L, Dintakurti SH, et al. Practice patterns in reporting and documentation of Charles Bonnet syndrome: a retrospective review following COVID-19. Ther Adv Ophthalmol 2024; 16: 25158414241232285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma 2023; 15(4): 665–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Quidé Y. Dissociation, trauma and the experience of visual hallucinations in post-traumatic stress disorder and schizophrenia. BJPsych Open 2023; 9(1): e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. O’Brien J, Taylor JP, Ballard C, et al. Visual hallucinations in neurological and ophthalmological disease: pathophysiology and management. J Neurol Neurosurg Psychiatry 2020; 91(5): 512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Best J, Liu PY, Ffytche D, et al. Think sight loss, think Charles Bonnet syndrome. Ther Adv Ophthalmol 2019; 11: 2515841419895909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Shergill SS, Murray RM, McGuire PK. Auditory hallucinations: a review of psychological treatments. Schizophr Res 1998; 32(3): 137–150. [DOI] [PubMed] [Google Scholar]
- 50. Thomas GEC, Zeidman P, Sultana T, et al. Changes in both top-down and bottom-up effective connectivity drive visual hallucinations in Parkinson’s disease. Brain Commun 2023; 5(1): fcac329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Blom JD. Leroy’s elusive little people: a systematic review on lilliputian hallucinations. Neurosci Biobehav Rev 2021; 125: 627–636. [DOI] [PubMed] [Google Scholar]