Abstract
Background
Taiwan enacted the Hospice Palliative Care Act in 2000 and the Patient Autonomy Act in 2016. However, medical education has emphasized palliative care skills over ethical and legal integration. This study developed a curriculum for pre-clinical students, focusing on applying these issues in end of life care.
Methods
The participants were fourth-year medical students enrolled in a 1-credit medical ethics and law course at a medical school in Taiwan. The study employed a two-stage design, combining quantitative pretests and posttests with qualitative data obtained through the Know-Want-Learn strategy. The curriculum, called the video-triggered expert-led debrief module, included a video scenario on end of life care, insights shared by three interprofessional experts, and students debrief. In 2021, 168 students participated, and a quantitative questionnaire using a pretest-posttest design was applied to assess the curriculum’s impact on students’ knowledge and attitudes toward end of life care. In 2022, 157 students participated, and the survey used open-ended questionnaires (the Know-Want-Learn strategy) to evaluate what students already knew and what they wanted to know before the module, as well as what they had learned afterward.
Results
In 2021, we collected 166 (98.8%) valid responses in the quantitative questionnaire. Seven of the eight knowledge-based questions and four of the seven learning motivation items showed significant improvement in the posttest (P < 0.05). In 2022, 81 (51.6%) valid responses were obtained from the qualitative questionnaire. Before the module, students’ understanding was superficial and focused on literal meanings. Three themes emerged in what they wanted to know: medical decision-making, ethics and laws, and empathetic communication, with eight subthemes. After the module, three themes and six subthemes were identified in the “what I learned” section. Students reported gaining knowledge related to ethics and laws, and empathetic communication.
Conclusions
The video-triggered expert-led debrief module can effectively teach the application of medical ethics and laws in end of life care. This approach has shown positive results among young medical students. It enhances students’ learning motivation, deepens their understanding of ethics and laws, and empathetic communication. It further encourages them to reflect deeply on the meaning of healthcare.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06304-2.
Keywords: Video triggered, End-of-life care, Know-want-learn strategy
Background
Because of the implementation of the Taskforce of Medical School Curriculum Reform, since 2013, medical education in Taiwan has involved a 6-year rather than a 7-year program. In the 7-year program, after completing the 4-year medical school curriculum, medical students underwent a 1-year clerkship followed by a 2-year internship at a hospital. They graduated from medical school upon completion of this training. By contrast, students participating in 6-year medical programs typically graduate upon successful completion of 2 years of clerkship training following the initial 4-year medical school curriculum. This reduction in the number of years of medical school may influence students’ competency-based education in end of life (EoL) care, including the related ethical and legal knowledge.
EoL care is regarded as a crucial component of medical education [1, 2]; however, the training in this area is often inadequate [3, 4]. Therefore, numerous medical educators have designed specialized courses to equip students with the skills necessary for delivering EoL care and engaging in EoL discussions with patients and their families. For example, utilizing role-playing and group discussions, training with simulated patients, and providing online videos [5–7]. Moreover, medical education experts had developed reliable tools to assess EoL care learning [8]. However, courses for pre-clinical students remain scarce, and those integrating EoL care with ethics and laws are limited by the territoriality of laws and regional cultural values.
This study aims to teach EoL care-related ethical and legal issues before students enter clinical rotations. Medical students generally lack prior clinical experience, and therefore, they have an educational gap in their practical knowledge of EoL care before they enter clinical rotations. If students lack prerequisite knowledge and experience, they are unlikely to apply the methods mentioned in the previously cited articles to their learning. Furthermore, as medical students who have not yet entered clinical practice, it is not appropriate to have them interact directly with patients.
Therefore, in this study, we adopted a video-triggered expert-led debrief (VED) module to teach medical students about the ethical and legal issues related to EoL care. This two-year study first compared the differences in medical students’ understanding and learning motivation through pretests and posttests. Subsequently, based on the students’ reflections, the study examined their initial doubts before the course and whether the module helped address those doubts.
Methods
Participants and study design
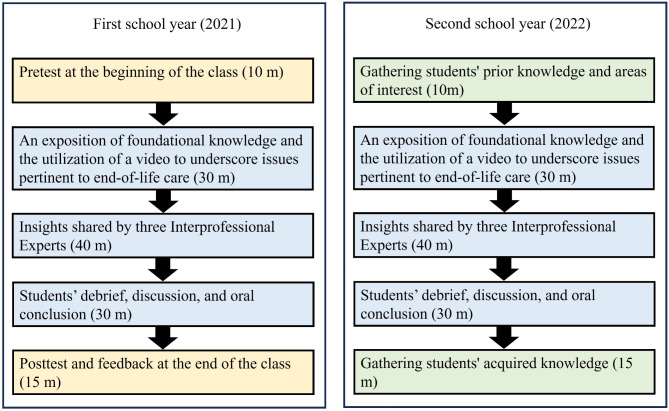
The study participants were fourth-year medical students who were enrolled in a 1-credit mandatory course on medical ethics and law in a 6-year program at a medical school in Taiwan. Convenience sampling was used to recruit medical students who were enrolled in this course from August 2021 to May 2023. The curriculum of this course was developed in accordance with the principles of situational and experiential learning [9, 10]. We developed a comprehensive 100-minute module to cultivate students’ competency in EoL care-related ethical and legal issues; the module was designed to be seamlessly integrated into the curriculum of the medical ethics and law course. The module comprised three sessions: a description of foundational knowledge and a video scenario highlighting the ethical and legal concerns related to EoL care; sharing of insights by three interprofessional experts (IPEs), namely, an EoL care clinician, a medical humanities educator, and a psychosocial counselor; and a structured discourse forum involving the three IPEs and the medical students (Fig. 1).
Fig. 1.
Medical ethics and law curriculum flowchart. The module on medical ethics and law comprised 30 min of video trigger appreciation, 40 min of insights being shared by interprofessional experts, and 30 min of student discussion. Different mechanisms of feedback collection were applied in the first and second school years
This study applied a two-stage approach. In the first year of the study, online quantitative data were collected before and after the module was employed. Eligible students voluntarily completed pretest and posttest questionnaires and a postclass satisfaction survey. In the second year, qualitative data were collected. Students’ feedback was obtained before and after the module by using the Know-Want-Learn (KWL) strategy developed by Ogle in 1986. The focus of this strategy is identifying what students already know (“Know”), what they want to learn (“Want”), and what they have learned from the module (“Learned”) [11].
Measurements
The pretest and posttest questionnaires used to collect quantitative data comprised two parts. The first part of the questionnaire assessed students’ understanding of EoL care-related ethical and legal issues (Additional file 1). It comprised eight multiple-choice questions, with four answer options provided for each question. The questions were primarily authored by Dr. Chih‑Chia Wang, with contributions from three IPEs in the design process. Dr. Wang holds a master’s and PhD in law from Taiwan and has extensive experience in medical disputes and medical ethics and law issues [12–14]. The three experts who contributed to the design are from the fields of EoL care, medical humanities education, and psychology. A questionnaire developed by Hwang and Chang [15] was used in the second part of the questionnaire to assess changes in the students’ learning motivation. It comprises seven items rated on a 5-point scale; the Cronbach’s alpha value for the questionnaire was 0.964. In the postclass satisfaction survey, which was concurrently conducted with the posttest, students were asked to rate their satisfaction with the learning approach as highly dissatisfied, dissatisfied, neutral, satisfied, and highly satisfied. This 5-point scale satisfaction assessment was based on the scale developed by Judy C.R. Tseng et al. [16]. The Cronbach’s alpha value was 0.976 for this survey.
For the qualitative feedback, we used the KWL strategy to collect qualitative data [11]. Before the module, we gathered what students already knew (Know) and what they wanted to know (Want). After the module, we collected what they had learned (Learn). The questionnaire included blank fields, allowing students to write freely.
Statistical analyses
This study employed a two-stage approach for analyses, conducting both quantitative and qualitative analyses. The reliability of the questionnaires was evaluated by calculating Cronbach’s α values, which are an indicator of internal consistency. A Cronbach’s α value equal to or exceeding 0.7 was deemed satisfactory in this study [17].
Quantitative data were evaluated using a two-tailed paired t-test. Statistical analyses were conducted using Version 18.0 of Statistical Product and Service Solutions for Windows (SPSS Inc., Chicago, IL, USA). For qualitative data analysis, we employed thematic analysis to identify and organize themes within the data [18]. Subsequently, the results were categorized by using the inductive method [19].
Results
Quantitative analysis
In the 2021 academic year, 168 students (131 men and 37 women) participated in this study. For the first part of the questionnaire, the multiple-choice section, we collected 166 (98.8%) valid responses. Table 1 presents the results of the analysis of the number of correct responses for each question before and after the test. Significant differences were identified between the pretest and posttest scores for seven questions. The question that did not show significant improvement (P = 0.113) is as follows: “Which of the following descriptions of ‘advance medical directives’ and ‘advance care planning and health-care decision-making documents’ is correct?” The learning motivation scale showed significant improvement (P < 0.05) in four out of seven items in the posttest (Table 2). The satisfaction survey showed that students’ satisfaction scores were all above 4.6 out of 5 (Table 3).
Table 1.
Analysis of correct responses in pre-test and post-test multiple-choice questions (n = 166)
| Multiple-choice question items | Pretest n (%) |
Posttest n (%) |
p value |
|---|---|---|---|
| Q1: According to the Hospice Palliative Care Act, if a patient is unable to express their wishes and if their adult family members do not prefer cardiopulmonary resuscitation for the patient, what is the “priority order” for the nearest relatives? |
104 (62.7) |
119 (71.7) |
0.007* |
| Q2: Which of the following regarding ‘not performing cardiopulmonary resuscitation’ and ‘terminating or withdrawing cardiopulmonary resuscitation’ for terminally ill patients is correct? | 82 (49.4) | 90 (54.2) | <0.001* |
| Q3: According to the Patient Autonomy Act, which description of a medical proxy is correct? | 22 (13.3) | 29 (17.5) | 0.001* |
| Q4: According to the Patient Autonomy Act, who should be involved in advance medical care consultations before advance medical decisions are made? | 98 (59.0) | 105 (63.3) | <0.001* |
| Q5: According to the Patient Autonomy Act, when advance medical directives are in place, in which of the following clinical conditions may health-care institutions or physicians terminate life-sustaining treatment in accordance with the patient’s advance medical directives? | 42 (25.3) | 63 (38.0) | <0.001* |
| Q6: According to the Patient Autonomy Act, who can establish advance medical directives? | 108 (65.1) | 112 (67.5) | <0.001* |
| Q7: Which of the following descriptions of “advance medical directives” and “advance care planning and health-care decision-making documents” is correct? | 32 (19.3) | 36 (21.7) | 0.113 |
| Q8: When discussing the Patient Autonomy Act, which of the following issues is not often compared with? | 82 (49.4) | 85 (51.2) | <0.001* |
*: Indicates a statistically significant difference (p < 0.05)
Table 2.
Learning motivation (n = 166)
| Items | Pretest | Posttest | p value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| 1. I think that the course is interesting and valuable. | 4.43 ± 0.66 | 4.6 ± 0.54 | 0.018* |
| 2. I would like to learn more and observe more in the course. | 4.43 ± 0.67 | 4.55 ± 0.58 | 0.106 |
| 3. The content of the course is worth learning. | 4.45 ± 0.66 | 4.67 ± 0.51 | 0.001* |
| 4. It is important that I sufficiently learn the course content. | 4.49 ± 0.65 | 4.64 ± 0.53 | 0.034* |
| 5. It is important to acquire the course knowledge related to our living environment. | 4.48 ± 0.66 | 4.59 ± 0.54 | 0.141 |
| 6. I will actively search for more information and learn about the topics discussed in the course. | 4.33 ± 0.76 | 4.49 ± 0.62 | 0.064 |
| 7. It is important that everyone take this course. | 4.48 ± 0.67 | 4.62 ± 0.55 | 0.047* |
*: Indicates a statistically significant difference (p < 0.05)
Table 3.
Satisfaction with the learning approach (n = 166)
| Items | Mean ± SD |
|---|---|
| 1. This learning activity helped me to better understand how to identify and classify the features of the target learning objects. | 4.60 ± 0.67 |
| 2. I attempted to identify the differences between the target learning objects in this learning activity. | 4.61 ± 0.67 |
| 3. The goal of this learning activity is difficult to achieve, but I can easily understand the instruction. | 4.63 ± 0.59 |
| 4. Learning in this course was more challenging and interesting than learning through traditional approaches is. | 4.62 ± 0.60 |
| 5. I made new discoveries or gained new information regarding the target learning objects from the course. | 4.64 ± 0.58 |
| 6. I have developed new manners of thinking or thinking styles with respect to learning because of the course. | 4.63 ± 0.60 |
| 7. The course has helped me to learn how to identify the features of the target learning objects. | 4.64 ± 0.61 |
| 8. The course has helped me to identify differences within the target learning objects. | 4.61 ± 0.63 |
| 9. In this course, I learned how to observe the target learning objects from new perspectives. | 4.66 ± 0.61 |
Qualitative analysis
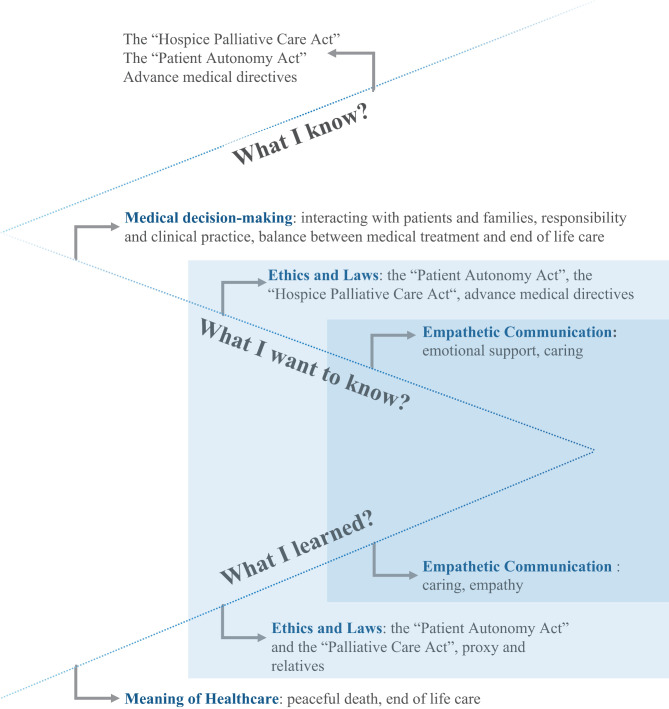
Qualitative data were collected utilizing the KWL strategy, which is based on constructivist philosophy. In the 2022 academic year, 157 medical students (116 men and 41 women) participated in the course, and a total of 81 KWL questionnaires (51.6%) were collected. The following themes were identified on the basis of the students’ feedback (Fig. 2):
Fig. 2.
Student feedback on the EoL care course obtained through the KWL strategy. On the basis of the feedback obtained through the KWL strategy, the student responses were categorized into themes and subthemes. For “What I Know,” three themes were identified: the “Hospice Palliative Care Act”, the “Patient Autonomy Act”, and advance medical directives. For “What I Want to Know,” three themes and eight subthemes were identified; the themes included medical decision-making, ethics and laws, and empathetic communication. For “What I Learned,” three themes and six subthemes were identified; the themes included ethics and laws, empathetic communication, and the meaning of healthscare
Three main themes were identified in the students’ feedback for the “What I know” section: the Hospice Palliative Care Act, the Patient Autonomy Act, and advance medical directives. The data indicated that the students already had a preliminary understanding of these three themes before the module, but their understanding was mostly based on textual interpretation.
The hospice palliative care act
A medical student stated the following regarding EoL care:
EoL care refers to providing relieving and supportive medical care for patients with severe illness, including by relieving symptoms, offering emotional and social support, and respecting patient wishes regarding treatment decisions such as opting out of cardiopulmonary resuscitation (CPR). (Student No. 056)
The patient autonomy act
A medical student stated the following:
According to the Patient Autonomy Act, patients have the right to sign advance medical directives. By establishing advance medical directives, they can decide whether they wish to accept or refuse life-sustaining treatment, artificial nutrition, or other therapies at the EoL. (Student No. 019)
Advance medical directives
A medical student stated the following regarding advance medical directives:
The Patient Autonomy Act empowers patients to establish advance directives. Through these directives, patients can express their wishes regarding life-sustaining treatments, artificial nutrition, and other interventions at the EoL, including whether they wish to accept or refuse them. (Student No. 100)
On the basis of the students’ feedback in the “What I want to know” section, three themes and eight subthemes were identified. The themes were medical decision-making, ethics and laws, and empathetic communication. The students’ responses revealed that they wished to gain insight into practical implementation methods, potential challenges encountered during implementation, opportunities for further education, and strategies for enhancing doctor–patient communication.
Theme 1: Medical decision-making
Interacting with patients and families
A medical student stated the following:
The doctor should first confirm the patient’s wishes regarding their care, especially if they have an advance directive. This document has legal value and supersedes any objections from family members. (Student No. 149)
Responsibility and clinical practice
A medical student asked the following question:
Under what circumstances can a patient choose to forgo life-sustaining treatment and have a peaceful passing? (Student No. 071)
Balance between medical treatment and EoL care
A student stated the following:
Clinicians are facing a growing challenge in terms of maintaining the balance between aggressive medical treatment and EoL care. Maintaining this balance will likely involve considerations beyond medicine. (Student No. 026)
Theme 2: Ethics and laws
The patient autonomy act
A medical student asked the following question:
What are the main rights granted by the Patient Autonomy Act to patients regarding their medical care? (Student No. 110)
The hospice palliative care act
Medical students asked the following questions:
What criteria must a patient meet to qualify for EoL care? (Student No. 039)
Is there any training in Taiwan regarding the relevant legal regulations, including the required course hours for training regarding providing EoL care, that can enable health-care professionals to gain knowledge of EoL care and to understand their responsibilities and obligations within it? (Student No. 036)
Advance medical directives
A medical student asked the following question:
What are the initiation timings, decision-making processes, and final execution processes for advance directives? (Student No. 017)
Theme 3: Empathetic communication
Emotional support
Medical students asked the following questions:
How should psychological and emotional support be provided to patients and their families during EoL care? (Student No. 036)
Caring
Medical students asked the following questions:
How communication with patients regarding legal documents pertaining to life and death be initiated, and who should be responsible for initiating such communication? (Student No. 049)
On the basis of the students’ feedback in the “What I learned section,” three themes and six themes were identified. The three themes were ethics and laws, empathetic communication, and the meaning of healthcare. The students’ responses revealed that the regulatory topics that they wished to know more about had been discussed in class. Additionally, they enhanced their understanding of the medical humanities.
Theme 1: Ethics and laws
The patient autonomy act and the hospice palliative care act
A medical student stated the following:
The Patient Autonomy Act does not adequately cover adolescents. The right to make life-and-death decisions should not be solely determined on the basis of age. (Student No. 002)
Proxies and relatives
A medical student reported the following:
The entities exercising the right to informed consent are as follows: the patient or relative. Relatives are not allowed to hinder health-care institutions or physicians from making decisions on the basis of patients’ wishes regarding medical options. (Student No. 120)
Theme 2: Empathetic communication
Caring
A medical student reported the following:
Medical decision-making is a complex process, and patients’ preferences may evolve over time. As doctors, we play a crucial role in facilitating decision-making by helping patients explore their core values. (Student No. 149)
Empathy
A medical student reported the following:
In health-care settings, empathy involves more than simply thinking from the patient’s perspective. It involves understanding their emotional experience, values, and fears. By cultivating empathy, doctors can more effectively tailor care to meet each patient’s needs. (Student No. 048)
Theme 3: The meaning of health care
Peaceful death
A medical student reported the following:
Survival is a primal instinct, whereas the desire for a good death is a conscious choice. Patients facing terminal illness often hold hope for life but not at the cost of undue suffering. This complex reality is acknowledged in EoL care. The core principle of EoL care is to prioritize patient comfort and well-being to ensure that patients live out their remaining days with as much dignity and peace as possible. (Student No. 120)
EoL care
A medical student stated the following:
The aim of EoL care is to fulfill the physiological, psychological, and social needs of patients. Enhancing the quality of life for both patients and their families is also a key objective. (Student No. 128)
Discussion
Quantitative analysis showed significant progress in the knowledge part (multiple-choice questions), along with strong learning motivation and high satisfaction with the module. Qualitative data supplemented these findings, confirming that we provided the information students sought.
In the first part of the quantitative analysis, we observed that the correct response rates for multiple-choice questions were generally low. This may be attributed to the students’ limited exposure to legal studies, making it challenging to familiarize themselves with specialized terminology within a short timeframe. This likely caused confusion when reading or answering the questions, resulting in lower overall accuracy and limited progress in the posttest. Conversely, some questions (Question 1 and 6) had relatively high correct response rates in the pretest and further significant improvement in the posttest, possibly due to the question stem and options involving fewer legal terms. However, the qualitative analysis showed that students’ vague understanding of legal and ethical issues in EoL care became more defined. In the qualitative analysis, the “What I want to know” and “What I learned” sections shared two common themes: “ethics and laws” and “empathetic communication.” This highlights that the module provided students with the knowledge they were seeking. Additionally, it showed that despite less-than-ideal performance on the multiple-choice questions, students still gained a deeper understanding of relevant issues. Notably, in the “What I learned” section, under the theme of ethics and laws, students expressed a strong grasp of issues regarding the authority of proxies and relatives. This finding also aligns with our quantitative results, where Question 1 showed significant improvement in the posttest.
In the second part of the quantitative analysis, the results indicated that students exhibited a high level of learning motivation prior to the module. This may be attributed to the pre-course introduction, where we provided detailed information regarding the module structure, including its delivery by a diverse group of experts (with background information provided), the use of video-based learning, expert-led interactive sessions, and the focus on developing essential future competencies. We also emphasized that the module was ungraded, with the primary objective being to deepen students’ understanding before entering clinical practice. In the posttest, scores for all learning motivation items increased, and although only four items reached statistical significance, the overall trend suggested an enhancement in students’ motivation. Furthermore, the satisfaction survey indicated that all items received ratings above 4.6, which also supports the observed increase in learning motivation following the module. In addition, the noticeable change in students’ learning attitudes may have been influenced by the concept of embodiment.
The embodied cognition strategy can be used to teach abstract concepts by grounding them in perceptual, motor, and emotional systems [20]. VED creates a well-designed experiential context, enabling the application of the embodied cognition strategy. In the qualitative analysis, the theme of “empathetic communication” appeared in both the “What I want to know” and “What I learned” sections. Before the module, students expressed a desire to understand how to provide psychological and emotional support to patients and their families. After the module, they not only recognized the complexity of medical decision-making but also realized that a physician’s responsibility goes beyond treatment — it includes helping patients explore their core values and make the most ethically aligned choices. Besides, these most ethically aligned choices should not be decided on the basis of the previous and present actions of doctors [21]。The embodied learning facilitated by the VED module may serve as a key stimulus for the components of “knows” and “knows how” in Miller’s pyramid [22]. Moreover, embodiment is a vital component of reflective practice [23]. Another theme in the “What I learned” section, “the meaning of healthcare,” revealed that students came to understand that a “peaceful death” is a conscious choice, and that physicians must prioritize the comfort and dignity of the patient. This reflects the feedback from students’ reflective practice.
Notably, the findings of this study indicate that even before clinical rotations, fourth-year medical students have strong interest in developing patient-communication skills. The postclass reflections revealed that the students understood the crucial role of empathy engagement and the importance of fostering self-awareness among patients in effective physician–patient communication. Interpersonal communication is also emphasized as a core competency by the Accreditation Council for Graduate Medical Education (ACGME), aligning with the findings of this study [24].
Formal curriculum—the prescribed educational format in medical schools—has several weaknesses in terms of EoL care teaching. These weaknesses include inadequate teaching content; minimal coverage of EoL content in medical textbooks; and overreliance on lectures as the primary mode for teaching [25]. Furthermore, inadequate funding, insufficient clinical supervision, a lack of trained faculty, overloaded curricula, and differing views regarding the importance of EoL care education among medical school administrators have adversely affected the quality of EoL care education [4, 26]. Research has indicated that EoL care-related ethical and legal knowledge can be enhanced by implementing well-structured teaching plans [27, 28]. In this study, the use of the VED module may offer a new method for this issue, especially for medical students who have not yet entered clinical practice.
This study has several limitations. First, it included a cohort of fourth-year medical students from a single institution in Taiwan, which limits the generalizability of the results. Second, the high pre-test scores in learning motivation make it difficult to fully rule out a ceiling effect. Third, this study did not assess long-term retention of knowledge or skills, which limits our ability to evaluate the long-term impact of the VED approach. Additionally, although qualitative feedback is valuable, it may not capture the full range of student experiences. Fourth, the study lacked a control group, so it cannot be concluded that the observed improvements were solely attributable to the VED intervention. Furthermore, students’ lower performance in knowledge-based multiple-choice questions may reflect unfamiliarity with legal issues. This suggests that future studies should allow more time for students to understand the background knowledge. Future research should employ longitudinal designs, multi-institutional samples, and more rigorous assessment methods.
Conclusions
The number of hours of EoL care education in medical schools in Taiwan has been reduced, and therefore, integrating EoL care education into Taiwan’s medical curriculum is crucial. In the VED approach, embodied cognition is applied to transform abstract concepts into experiential learning. This approach encourages reflection and empathy in students and has the potential to improve education on ethics and laws related to EoL care.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank their colleagues and the students who contributed to this study. The authors would also like to thank the reviewers and the editor for their comments on this article.
Abbreviations
- VED
Video-triggered expert-led debrief module
- EoL
End-of-life
- KWL
Know-Want-Learn
- IPE
Interprofessional expert
- TSGHIRB
Tri-Service General Hospital Institutional Review Board
- SPSS
Statistical Product and Service Solutions
- MOST
Ministry of Science and Technology
- PMN
Project Management Number
Author contributions
YPC and CCW contributed to the literature review, plan execution, data collection and management, and manuscript writing. DYN contributed to the study design as well as data collection and management, and provided assistance to the principal investigator in the plan execution. JJL and YLT contributed to policy advisory, study design, and manuscript structuring. CPF contributed to policy advisory.
Funding
This work was supported by the Ministry of Education of the Republic of China (Taiwan) (Grant No: PMN1122301) and the National Science and Technology Council of the Republic of China (Grant No: MOST110-2511-H-016-002-MY3).
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to ongoing research but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the Tri-Service General Hospital, National Defense Medical Center (TSGHIRB Nos. B202105040 and 202305042). The survey was executed in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects. All participants were adults with decision-making capacity.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chan HYL, Lee DTF, Woo J. Diagnosing gaps in the development of Palliative and End-of-Life Care: a qualitative exploratory study. Int J Environ Res Public Health. 2019;17(1). [DOI] [PMC free article] [PubMed]
- 2.Machin LL, Latcham N, Lavelle C, Williams RA, Corfield L. Exploring the perceived medical ethics and law training needs of UK Foundation doctors. Med Teach. 2020;42(1):92–100. [DOI] [PubMed] [Google Scholar]
- 3.Wynter K, Brignall R. End-of-life medical education: is it dead and buried? Med Teach. 2020;42(9):1065–6. [DOI] [PubMed] [Google Scholar]
- 4.Horowitz R, Gramling R, Quill T. Palliative care education in U.S. medical schools. Med Educ. 2014;48(1):59–66. [DOI] [PubMed] [Google Scholar]
- 5.Bansal A, Monk A, Norman M, Fingas S. Improving medical students’ confidence in end-of-life consultations. Clin Teach. 2020;17(6):705–10. [DOI] [PubMed] [Google Scholar]
- 6.Parry R, Whittaker B, Pino M, Jenkins L, Worthington E, Faull C. RealTalk evidence-based communication training resources: development of conversation analysis-based materials to support training in end-of-life-related health and social care conversations. BMC Med Educ. 2022;22(1):637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parikh PP, White MT, Buckingham L, Tchorz KM. Evaluation of palliative care training and skills retention by medical students. J Surg Res. 2017;211:172–7. [DOI] [PubMed] [Google Scholar]
- 8.López-García M, Rubio L, Martin-de-Las-Heras S, Suárez J, Pérez-Cárceles MD, Martin-Martin J. Instruments to measure skills and knowledge of physicians and medical students in palliative care: a systematic review of psychometric properties. Med Teach. 2022;44(10):1133–45. [DOI] [PubMed] [Google Scholar]
- 9.Dunin-Borkowska A, Cardoso Pinto AM, Xu J, Bhandari N, Ranasinghe L. Evaluating the utility of a Near-peer Situation-based course to prepare medical students for the UK Foundation Programme: a pilot study. Adv Med Educ Pract. 2023;14:1317–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nagel DA, Penner JL, Halas G, Philip MT, Cooke CA. Exploring experiential learning within interprofessional practice education initiatives for pre-licensure healthcare students: a scoping review. BMC Med Educ. 2024;24(1):139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogle DM. KWL: a teaching model that develops active reading of expository text. Read Teacher. 1986;39(6):564–70. [Google Scholar]
- 12.Wang C-C, 淺談醫預法下的醫療爭議調解制度. 醫療品質雜誌. 2024;18(1):14–9. [Google Scholar]
- 13.Shen R-N, Huang Y-Y, Chen W-W, Wang C-C, 醫療事故預防及爭議處理法中的醫療事故關懷. 醫療品質雜誌. 2024;18(1):20–4. [Google Scholar]
- 14.Wang C-C. Constructing the Prevention of Medical disputes with the Module of three-sections and five-levels and Multi-mechanism. Angle Health Law Rev. 2021(51):107–14.
- 15.Hwang G-J, Yang L-H, Wang S-Y. A concept map-embedded educational computer game for improving students’ learning performance in natural science courses. Comput Educ. 2013;69:121–30. [Google Scholar]
- 16.Chu H-C, Hwang G-J, Tsai C-C, Tseng JC. A two-tier test approach to developing location-aware mobile learning systems for natural science courses. Comput Educ. 2010;55(4):1618–27. [Google Scholar]
- 17.McHorney CA, Ware JE Jr., Lu JF, Sherbourne CD. The MOS 36-item short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40–66. [DOI] [PubMed] [Google Scholar]
- 18.Greg Guest KMM, Emily E. Namey. Applied Thematic Analysis. SAGE Publications, Inc.; 2012.
- 19.Creswell JW. Educational Research: planning, conducting, and evaluating quantitative and qualitative research: Upper Saddle River., NJ: Pearson Education, Inc.; 2008. [Google Scholar]
- 20.Glenberg AM. Embodiment and learning of abstract concepts (such as algebraic topology and regression to the mean). Psychol Res. 2022;86(8):2398. [DOI] [PubMed] [Google Scholar]
- 21.Dominic Wilkinson JHaJS. Medical Ethics and Law: A curriculum for the 21st Century 3rd13th September 2019.
- 22.Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9 Suppl):S63–7. [DOI] [PubMed] [Google Scholar]
- 23.Smears E. Breaking old habits: professional development through an embodied approach to reflective practice. J Dance Somatic Practices. 2009;1:99–110. [Google Scholar]
- 24.Joshi T, Budhathoki P, Adhikari A, Poudel A, Raut S, Shrestha DB. Improving Med Education: Narrative Rev Cureus. 2021;13(10):e18773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Block SD. Medical education in end-of-life care: the status of reform. J Palliat Med. 2002;5(2):243–8. [DOI] [PubMed] [Google Scholar]
- 26.Head BA, Schapmire TJ, Earnshaw L, Chenault J, Pfeifer M, Sawning S, et al. Improving medical graduates’ training in palliative care: advancing education and practice. Adv Med Educ Pract. 2016;7:99–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leung DYP, Chan HYL. Palliative and End-of-Life Care: more work is required. Int J Environ Res Public Health. 2020;17(20). [DOI] [PMC free article] [PubMed]
- 28.Lamont S, Stewart C, Chiarella M. Capacity and consent: knowledge and practice of legal and healthcare standards. Nurs Ethics. 2019;26(1):71–83. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to ongoing research but are available from the corresponding author on reasonable request.