Abstract
When a severe medial wall defect is present in revision total hip arthroplasty (THA), simple bone grafting (BG) may not be sufficient, and trabecular metal (TM) augmentation is often necessary. We aimed to evaluate whether there were differences in outcomes of revision THA with medial wall defects depending on the use of TM augmentation. Between 2009–2021, 130 patients were classified into two groups: 80 patients undergoing bone grafting (BG group) and 50 patients undergoing both bone grafting and TM augmentation (BG/TM group). We evaluated the postoperative center of rotation (COR) position and changes in vertical and horizontal COR at last follow-up. Additionally, we categorized the fate of the transplanted bone graft into four groups: unchanged, initially changed, resorption-no further intervention, and resorption-revision. The mean horizontal COR changes were −3.50 mm in the BG group and −1.07 mm in the BG/TM group (p = 0.005). In the BG/TM group, a higher proportion of the patients showed unchanged or only initial changes when compared to the BG group (88.0% and 65.0%, respectively). The BG/TM group showed more favorable results regarding horizontal changes in the COR and fate of the bone graft. Therefore, for revision THA in patients with severe medial wall defects, the combined use of bone graft and TM augmentation can be a suitable option.
Subject terms: Medical research, Outcomes research
Introduction
The rate of total hip arthroplasty (THA) is rapidly increasing due to the rise in hip fractures and diseases resulting from the aging population. Alongside this rise in THA procedures, revision THA have been increasing, owing to more extensive use of THA, lower age indications for surgery, and longer life expectancy1,2. Compared to primary THA, revision THA presents greater challenges, including dealing with previous scars, implant compatibility, bone defects, inadvertent bone loss during component or cement removal, and infection.
Despite improvements in acetabular liners, aseptic implant loosening remains the main cause of THA revision3–5. In cases of severe acetabular bone deficiency, central segmental deficiencies (medial wall absent) connecting to the pelvic cavity can be encountered. When a medial wall defect is present, achieving a stable fixation of the acetabular cup becomes difficult. The treatment goal for these patients is to restore the center of rotation (COR) and ensure a robust acetabular cup fixation by filling the defect area with bone grafts. However, this process is highly challenging and demands specialized skills. Additionally, in cases of substantial defects, simple bone grafting (BG) may not be sufficient, and trabecular metal (TM) augmentation is often necessary, with several studies reporting favorable outcomes6–12.
TM augmentation was introduced to improve biological fixation and is commonly used in revision surgeries when the contact surface between the implant and host bone is insufficient due to osteolysis. TM offer several advantages, including high porosity (up to 80%), resembling cancellous bone, which promotes vascularization and bone ingrowth, and a low elastic modulus, which helps reduce stress shielding around the acetabulum13. Additionally, the high friction coefficient, which increases the shear strength at its interface with bone, provides excellent initial stability13,14. Moreover, this technique simplifies and expedites the procedure without the risk of bone resorption following grafting. These combined features make TM augmentation suitable for treating bone loss in revision THA.
Despite this, no study has compared the results between simple BG and TM augmentation in revision THAs with acetabular medial wall defects. Therefore, we aimed to compare and analyze the clinical and radiological outcomes of two types of revision THAs in patients with acetabular medial wall defects: one group underwent only BG (BG group), and the other group underwent both BG and TM augmentation (BG/TM group). We hypothesized that the BG/TM group would show better radiological results regarding changes in the COR and fate of the graft than the BG group.
Materials and methods
Study population
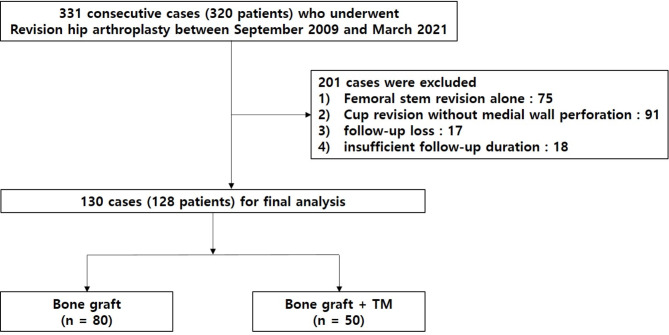
This study was a single-center, retrospective, comparative cohort study that enrolled patients who underwent revision THA between September 2009 and March 2021. In total, 331 revision procedures were conducted at our tertiary university hospital. Inclusion criteria for this study were as follows: patients who underwent revision THA with acetabular medial wall defects and those who had a minimum follow-up of 2 years. Of the 331 hips, 75 who only underwent femoral stem replacement and 91 who underwent acetabular revision surgery without medial wall defects were excluded. Seventeen patients who were lost to follow-up, despite extensive efforts to contact them to return for radiological evaluation, were excluded. Eighteen patients were further excluded because of insufficient follow-up period within 2 years or incomplete medical records. After the exclusion, 130 hips with a minimum follow-up of 2 years were finally included in the study. The patients were classified into two groups based on the treatment they received for their medial acetabular defect. The first group underwent only BG in the acetabular defect area, and the second group underwent both BG and TM augmentation. The BG and BG/TM groups consisted of 80 and 50 hips, respectively (Fig. 1).
Fig. 1.
Flowchart of the study.
No difference in age, sex, body mass index, bone mineral density, revision type, and American Society of Anesthesiologists status was observed. Mean follow-up periods were 5.6 years in the BG group and 5.7 years in the BG/TM group (Table 1). Aseptic cup loosening was the most common cause in each group (p = 0.052). The Paprosky classification was used to classify acetabular bone deficiency. In the BG group, type 3A (52.5%) bone defect classification was the most common, while in the BG/TM group, type 3B (56.0%) was the most common. There was a statistically significant difference between the two groups (p = 0.003).
Table 1.
Preoperative demographics.
| Variables | Total | BG only | BG/TM button | P Value |
|---|---|---|---|---|
| Number | 130 | 80 | 50 | |
| Age, mean ± SD, years | 62.9 ± 9.9 | 62.3 ± 10.8 | 64.9 ± 7.4 | 0.132 |
| Gender | 1.000 | |||
| Female | 55 (42.3%) | 34 (42.5%) | 21 (42.0%) | |
| Male | 75 (57.7%) | 46 (57.5%) | 29 (58.0%) | |
| BMI, mean ± SD, kg/m2 | 24.8 ± 3.1 | 24.0 ± 2.9 | 26.2 ± 3.0 | 0.505 |
| BMD, mean ± SD, T-score | − 1.2 ± 1.3 | − 1.3 ± 1.4 | − 1.0 ± 1.5 | 0.284 |
| Follow-up, mean ± SD, years | 5.6 ± 2.5 | 5.6 ± 2.7 | 5.7 ± 1.9 | 0.449 |
| Cause for revision | 0.052 | |||
| Cup loosening | 79 (60.8%) | 50 (62.5%) | 29 (58.0%) | |
| Bipolar cup migration | 27 (20.8%) | 20 (25.0%) | 7 (14.0%) | |
| Periprosthetic joint infection | 24 (18.4%) | 10 (12.5%) | 14 (28.0%) | |
| Revision type | 0.366 | |||
| Total component | 20 (15.4%) | 10 (12.5%) | 10 (20.0%) | |
| Isolated cup revision | 110 (85.6%) | 70 (87.5%) | 40 (80.0%) | |
| Laterality | 0.039 | |||
| Right | 75 (57.7%) | 40 (50.0%) | 35 (70.0%) | |
| Left | 55 (42.3%) | 40 (50.0%) | 15 (30.0%) | |
| Surgical approach | ||||
| Posterolateral | 130 (100%) | 80 (100%) | 50 (100%) | 1.000 |
| ASA classification | 0.555 | |||
| 1 | 35 (26.9%) | 24 (30.0%) | 11 (22.0%) | |
| 2 | 76 (58.5%) | 44 (55.0%) | 32 (64.0%) | |
| 3 | 19 (14.6%) | 12 (15.0%) | 7 (8.0%) | |
| Paprosky classification of acetabular bone defect | 0.003 | |||
| 2C | 12 (9.3%) | 12 (15.0%) | 0 (0.0%) | |
| 3A | 64 (49.2%) | 42 (52.5%) | 22 (44.0%) | |
| 3B | 54 (41.5%) | 26 (32.5%) | 28 (56.0%) |
BG, bone graft; TM, trabecular metal; SD, standard deviation; BMI, body mass index; BMD, bone mineral density; ASA, American Society of Anesthesiologists.
Surgical technique and postoperative management
All operations were performed by an experienced arthroplasty surgeon using a posterolateral approach in the lateral decubitus position. For all the patients, the appropriate cup position and extent of BG were predicted using a preoperative template. The goal for the cup placement was to restore the native COR if possible. During the surgery, fluid culture was conducted after capsulotomy, and specimens from the hip joint capsule and implant area were collected for frozen biopsy to reconfirm the absence of current infections. After removal of the acetabular component, acetabular granulation tissue and osteolytic lesions were thoroughly removed, and pulsatile lavage was performed. Femoral head allografts, frozen and stored under –80℃ after collection and radiation sterilization at a dose of 25 kGy, were prepared to achieve cup positioning in the native COR. For the medial defect site, allografts were placed alone or combined with an augment (TM Acetabular Revision System; Zimmer Biomet, Warsaw, IN, USA). In the BG group, morselized allograft was impacted above the pelvic membrane in the medial wall defect site. It was placed with an appropriate strength to prevent excessive intrusion into the pelvic cavity, and the strength was gradually increased while packing the defect site. Additionally, reaming on reverse was performed intermittently to enhance impaction efficiency (Fig. 2). In the BG/TM group, a TM augment was used to cover the medial wall before impacted BG. Reaming the acetabulum on reverse was performed to ensure proper impaction of the morselized allografts (Fig. 3).
Fig. 2.
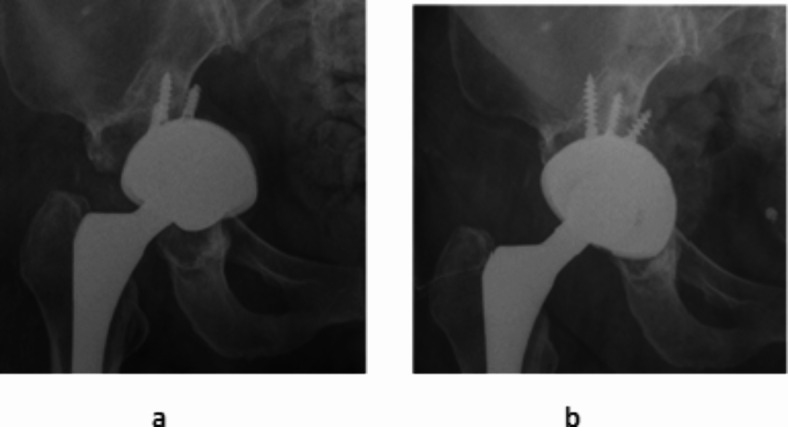
(a) A preoperative anteroposterior (AP) radiograph showing a Paprosky IIC acetabular defect, (b) A postoperative anteroposterior (AP) radiograph showing reconstruction of the acetabular defect using only bone grafting.
Fig. 3.
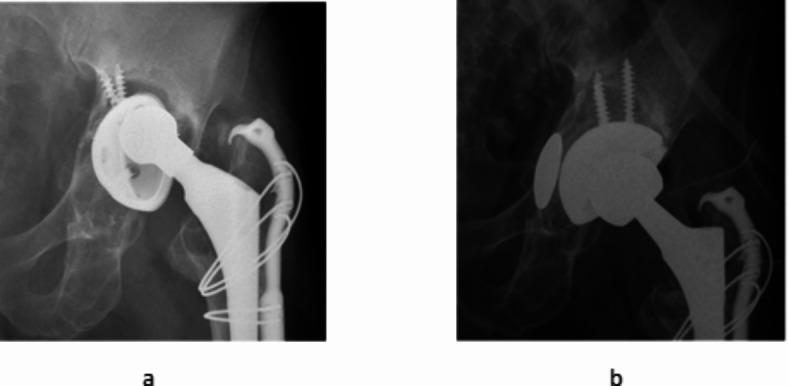
(a) A preoperative AP radiograph showing a Paprosky IIIA acetabular defect, (b) A postoperative AP radiograph showing the use of a trabecular metal restrictor with bone graft for reconstruction of the acetabular defect.
A cementless acetabular cup and highly cross-linked polyethylene (HXLPE) liner were used in all the patients. The acetabular cups used were the Trilogy (Zimmer Biomet, Warsaw, IN, USA) cup and G7 (Zimmer Biomet), and no difference in usage frequency was noted between the two groups. Cup fixation was achieved using the press fitting technique with an available peripheral rim, and in cases where the peripheral rim was lost or in poor condition, line-to-line fixation was allowed. There was no difference in the composition of cup fixation techniques between the two groups (Table 2) (p = 0.075). Initial stability was achieved through a minimum of two transacetabular screw fixations. The HXLPE liners used were Longevity (Zimmer Biomet) for the Trilogy cup and E1 (Zimmer Biomet): Vitamin E infused polyethylene for the G7 cup. The PE options included standard, elevated wall, and dual mobility bearings, and there was not a difference in composition ratio between the two groups (p = 0.119) (Table 2). Postoperatively, all the patients were prescribed subcutaneous low molecular weight heparin as thromboprophylaxis. On postoperative day two, the patients were instructed to walk with partial weight-bearing with the aid of crutches or walker, with full weight-bearing as tolerated. There was no difference in postoperative rehabilitation methods between the two groups.
Table 2.
Operative data.
| Variables | Total (n = 130) | BG only (n = 80) | BG/TM (n = 50) | P Value |
|---|---|---|---|---|
| Acetabular component (Zimmer Biomet) | 1.000 | |||
| Trilogy®, HXLPE (Longevity®) | 72 (55.4%) | 44 (55.0%) | 28 (56.0%) | |
| G7®, VEPE (E1®) | 58 (44.6%) | 36 (45.0%) | 22 (44.0%) | |
| Fixation technique | 0.075 | |||
| Press-fit | 111 (85.4%) | 72 (90.0%) | 39 (78.0%) | |
| Line-to-line fixation | 19 (14.6%) | 8 (10.0%) | 11 (22.0%) | |
| PE options | 0.119 | |||
| Standard PE | 61 (46.9%) | 32 (40.0%) | 29 (58.0%) | |
| Elevated PE | 16 (12.3%) | 12 (15.0%) | 4 (8.0%) | |
| Dual mobility | 53 (40.8%) | 36 (45.0%) | 17 (34.0%) | |
| Transacetabular screw, mean ± SD, n | 2.8 ± 0.7 | 3.0 ± 0.7 | 2.6 ± 0.7 | 0.002 |
| Cup anteversion, mean ± SD, ° | 17.1 ± 6.1 | 17.6 ± 6.1 | 16.4 ± 6.3 | 0.621 |
| Cup inclination, mean ± SD, ° | 44.8 ± 1.5 | 44.8 ± 1.6 | 44.9 ± 1.2 | 0.943 |
| Cup size, mean ± SD, mm | 58.4 ± 5.0 | 58.3 ± 4.6 | 58.7 ± 6.1 | 0.617 |
| Prosthetic femoral head | 0.054 | |||
| Cobalt-chromium | 62 (47.7%) | 44 (55.0%) | 18 (36.0%) | |
| Ceramic (Biolox delta, CeramTec) | 68 (52.3%) | 36 (45.0%) | 32 (64.0%) | |
| Neck length, mean ± SD, mm | 1.3 ± 4.4 | 1.3 ± 4.4 | 1.2 ± 3.8 | 0.492 |
| Operating time, mean ± SD, min | 138.4 ± 28.8 | 130.6 ± 28.1 | 151.4 ± 26.0 | 0.227 |
| Hospital stay, mean ± SD, day | 14.1 ± 5.6 | 14.4 ± 6.4 | 13.7 ± 2.3 | 0.059 |
BG, bone graft; TM, trabecular metal; HXLPE, highly cross-linked polyethylene; VEPE, vitamin E infused polyethylene; SD, standard deviation.
Methods of assessment
Anteversion and inclination of the acetabular cup were measured using PolyWare Rev. 7 (Draftware Developers Inc. Vevay, IN, USA)15. A postoperative radiological review was performed at 6 weeks, 3, 6, and 12 months, and annually thereafter. Standard radiographs, with additional Judet views, were used to detect periprosthetic osteolysis. Radiolucent lesions of ≥ 2 mm around the prosthetic components that were not immediately present postoperatively denoted osteolysis16. Changes in inclination of > 5° and vertical or horizontal migration of the acetabular component of ≥ 2 mm were defined as acetabular component loosening17. To observe any changes in cup position and COR, we compared the images obtained immediately postoperatively with those taken at the last follow-up. We evaluated the COR position in comparison to unaffected contralateral hip, and assessed the differences in vertical and horizontal COR at the last follow-up (Fig. 4). If the contralateral hip was abnormal, we used the Ranawat triangle method to determine the anatomic COR18. Additionally, we categorized the fate of the transplanted bone graft into four groups: unchanged, initially changed, resorption-no further intervention, and resorption-revision19. Medical records and radiographs of the patients were analyzed to determine reoperation and postoperative complication, such as dislocation, periprosthetic fracture, and deep joint infection. Operating times and hospital stay among the two groups were also collected. Modified Harris Hip Score (mHHS) was used to assess the patient-reported outcomes (PROM).
Fig. 4.
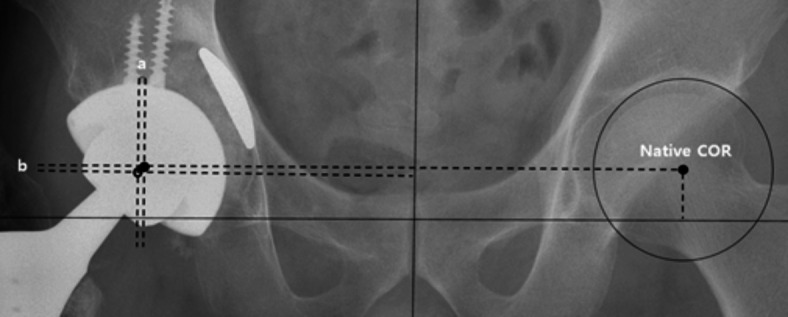
Illustrate showing the method of measuring the difference (a: horizontal and b: vertical) of the center of rotation (COR) position compared to the native COR of unaffected contralateral hip.
Statistical analysis
Summary data are expressed as means ± standard deviations for continuous variables, and as number and frequencies (%) for categorical variables. Continuous variables with non-normal distribution were analyzed using the Mann–Whitney U-test, whereas those with normal distribution were analyzed using independent t-tests. Categorical data were statistically analyzed using the chi-square test or Fisher’s exact test (n < 40 or t < 1). Statistical analysis was performed using SPSS software (version 24.0; IBM Corp., Armonk, NY, USA). A P-value of < 0.05 was considered statistically significant.
Ethics approval and informed consent
This study followed the World Medical Association Declaration of Helsinki and strengthening the reporting of observational studies in epidemiology (STROBE) guidelines for cohort studies. All procedures performed in studies involving human participants were in accordance with ethical standards, patient information was reviewed by the university human subjects committee and informed consent exemption was obtained from the IRB of our affiliated institutions (Pusan National University Yangsan Hospital, Approval No. 55-2023-068). All experimental protocols were approved by our institutional committee (Pusan National University Yangsan Hospital, Approval No. 55-2023-068).
Results
We compared two groups divided according to their use of porous metal augments to cover medial wall defect of the acetabulum (BG only and BG/TM groups). In osteolysis, radiolucent lines, implant loosening, and cup position changes, no significant differences were observed between the two groups. When comparing the COR, the mean vertical COR, mean vertical COR change, and mean horizontal COR in both the groups did not show any significant differences.
However, a more significant horizontal change in COR was observed in the BG group (p = 0.005). Specifically, the mean horizontal COR changes were − 3.50 mm (range, − 5 to 0 mm) in the BG group and − 1.07 mm (range, − 4 to 0 mm) in the BG/TM group (negative values indicate more medial migration) (p = 0.005). Additionally, a significant difference in the fate of the bone graft (p = 0.021), with a higher frequency of resorption without further intervention, was observed in the BG only group compared to that in the BG/TM group (18 patients, 22.5% in the BG only group; 3 patients, 6.0% in the BG/TM group). In contrast, in the BG/TM group, a higher proportion of patients showed unchanged or only initial changes compared to the BG only group (44 patients, 88.0% in the BG/TM group; 52 patients, 65.0% in the BG only group), although the BG group had a higher proportion of bone resorption requiring a revision group compared to the BG/TM group (10 patients, 12.5% in the BG only group; 3 patients, 6.0% in the BG/TM group). Reoperations occurred in 15 patients. Complications, including dislocation, periprosthetic fracture, and deep joint infection were observed in five, two, and four patients, respectively. No significant differences were observed in reoperation rates or the composition of complications between the two groups. The mean mHHS at the last follow-up was 89.1, and no significant differences were noted between the two groups (Table 3). The mean operation time was slightly longer in the BG/TM group compared to that in the BG only group, but was not statistically different, and the hospital stay also showed no significant difference (Table 2).
Table 3.
Postoperative outcomes in both groups.
| Variables | Total (n = 130) | BG only (n = 80) | BG/TM (n = 50) | P Value |
|---|---|---|---|---|
| Radiologic outcome at the last FU | ||||
| Osteolysis | 4 (3.1%) | 4 (5.0%) | 0 (0.0%) | 0.278 |
| Radiolucent line | 12 (9.2%) | 8 (10.0%) | 4 (8.0%) | 0.943 |
| Implant loosening | 19 (14.6%) | 12 (15.0%) | 7 (14.0%) | 1.000 |
| Cup position change | 40 (30.8%) | 22 (27.5%) | 18 (36.0%) | 0.409 |
| Center of rotation (COR) | ||||
| Vertical COR, mean ± SD, mm | 2.35 ± 4.47 | 2.08 ± 4.22 | 2.79 ± 5.25 | 0.102 |
| Vertical COR change, mean ± SD, mm | 1.87 ± 3.65 | 1.65 ± 3.96 | 2.21 ± 2.64 | 0.913 |
| Horizontal COR, mean ± SD, mm | 0.08 ± 3.59 | 0.13 ± 3.38 | 0.00 ± 4.26 | 0.456 |
| Horizontal COR change, mean ± SD, mm | -2.57 ± 1.79 | -3.50 ± 1.96 | -1.07 ± 1.47 | 0.005 |
| Graft fate | 0.021 | |||
| Unchanged | 66 (50.8%) | 38 (47.5%) | 28 (56.0%) | |
| Initial change | 25 (19.2%) | 14 (17.5%) | 16 (32.0%) | |
| Resorption-no further intervention | 26 (20.0%) | 18 (22.5%) | 3 (6.0%) | |
| Resorption-revision | 13 (10.0%) | 10 (12.5%) | 3 (6.0%) | |
| Reoperation | 15 (11.5%) | 12 (15.0%) | 3 (6.0%) | 0.200 |
| Complications | ||||
| Dislocation (%) | 5 (3.8%) | 2 (2.5%) | 3 (6.0%) | 0.589 |
| Periprosthetic fracture (%) | 2 (1.5%) | 2 (2.5%) | 0 (0.0%) | 0.693 |
| Deep joint Infection (%) | 4 (3.1%) | 4 (5.0%) | 0 (0.0%) | 0.278 |
| mHHS at the last FU, mean ± SD | 89.1 ± 9.1 | 88.5 ± 9.8 | 90.1 ± 9.5 | 0.245 |
BG, bone graft; TM, trabecular metal; FU, follow-up; COR, center of rotation; SD, standard deviation; mHHS, modified Harris hip score.
Discussion
Revision THA has been increasing with the rise in primary THA. Severe acetabular bone deficiencies can complicate acetabular cup fixation and restoration of COR. In severe defects of the acetabulum, in which simple BG may not be sufficient, TM augmentation is often necessary, with several studies reporting favorable outcomes6–12. Eachempati et al. conducted an assessment of the use of TM augments in the reconstruction of severe Paprosky IIIA and IIIB acetabular defects during revision THA. In their study, 41 patients were followed-up for an average of 39.4 months, revealing a 100% survivorship at the latest follow-up, with no reported failures8. Löchel et al. reported the long-term outcomes of revision THA using TM shell augmentation in a study with a mean follow-up period of 10.2 years. Among the 62 hips that underwent acetabular revision, the overall survival of the acetabular component was 92.5%, and mHHS at the latest follow-up was 81 points20. Jenkins et al. presented findings from a study involving 85 hips that underwent revision THA with TM augmentation, with a minimum of 5-year follow-up. Survival rate was 97%, and satisfactory hip function was maintained at a minimum of 5 years after an index revision surgery6. Abolghasemian et al. studied 34 patients with failed hip replacement using TM augments with a mean follow-up period of 64.5 months. In their analysis, the COR of the hip was restored in 27 (79.4%) patients. PROM at the final follow-up were excellent based on the Oxford hip score, demonstrating a 5-year survival rate of 91.1% in a group with severely deficient acetabula21. In cases of acetabular medial wall defect, Deng et al. evaluated 40 consecutive revision THA cases using metal disc augments for medial acetabular wall reconstruction. The mean follow-up period was 35.8 months, and 96.8% of patients with a minimum of 2-year follow-up were stable radiographically. Final clinical scores were satisfactory based on the HHS and Western Ontario and McMaster Universities Arthritis Index9.
However, to the best of our knowledge, no studies compared the outcomes of simple BG versus BG with TM augmentation during revision THAs in patients with acetabular medial wall defects. Several studies demonstrated that using TM augmentation is effective in restoring COR of the hip, but none have evaluated change of COR postoperatively9,10,21.
We aimed to compare and analyze the clinical and radiological outcomes of two groups based on different augmentation methods for revision THAs among patients with acetabular medial wall defects. Both groups showed low reoperation and complication rates, and the rates of these in the two groups were similar. PROMs, as measured by mHHS, were similar in both groups at the last follow-up, with an average score of 89.1. This suggests satisfactory functional outcomes. Both groups also exhibited similar rates of osteolysis, radiolucent lines, implant loosening, and cup position changes. However, a more substantial horizontal change in the COR was observed in the BG group, suggesting that the BG/TM augmentation may offer better stability in terms of COR alignment. Additionally, in the BG/TM group, more patients showed unchanged or only initial changes in the fate of the graft, but the BG only group had a higher rate of bone resorption requiring revision than the BG/TM group. These findings indicate that TM augmentation may contribute to better graft stability. Based on the Paprosky classification in both groups, the BG/TM group generally exhibited more severe bone defects than the BG only group. Nevertheless, by providing buttress support, the use of TM augments may prevent medial migration of the acetabular cups and enable a more compact impaction of allograft bone. The BG/TM group yielded favorable results regarding changes in the COR and fate of the bone graft.
This study demonstrated that using TM augmentation in revision THAs among patients with medial wall defects prevents medialization of the cup and provides a positive effect in terms of the fate of the allograft bone. However, when considering subsequent re-revision THAs, there may be issues related to bone stock depletion and potential problems associated metal debris and reactions with surrounding soft tissues.
This study has some limitations. First, this study is a retrospective cohort study with relatively small sample size, but it is meaningful, as there is a lack of studies comparing BG and TM/BG groups in revision THA among patients with severe medial wall defect, which are not very common. Second, this study has inherent selection bias, particularly due to differences in severity of bone defects between the two groups. Although it is difficult to consider this a fair comparison under identical conditions, it is noteworthy that better outcomes were achieved in the BG/TM group with more significant bone defects. Third, we sought to compare the outcomes between groups that received bone grafts only for medial wall defects and those that also used TM augments. Although TM augments of various forms were utilized during surgery for Paprosky type 3A or 3B defects to reconstruct large superior segmental bone defects, these aspects were not separately analyzed within this study, potentially introducing noise into the results. Given the small overall sample size and the revision setting, accurate matching analysis was challenging, leading to the decision that attempting such analysis could introduce more bias through overmatching or improper matching. Fourth, the postoperative rehabilitation method may have influenced the outcomes. Although cup fixation was performed on morselized bone, firm fixation was confirmed intraoperatively using multiple transacetabular screws. Therefore, rehabilitation began with partial weight-bearing, progressing to weight-bearing as tolerated. However, a cup position change was observed in 40 cases (30.8%). If partial weight-bearing or non-weight-bearing ambulation had been maintained as the rehabilitation method, more favorable outcomes in terms of cup position stability might have been observed across both groups, potentially reducing any difference between them. Fifth, the relatively short follow-up period limits the assessment of implant durability and detection of potential complications related to the augments. Finally, implant selection and augmentation methods were based on surgeon preference. We could not suggest an absolute indication to use TM augmentation. Further studies should be conducted to establish standardized protocols that may offer more specific guidance on TM augmentation strategies in patients with severe medial wall defects during revision THA.
In conclusion, the BG/TM group exhibited clinical and radiological outcomes similar to those of the BG only group, but showed more favorable results regarding horizontal changes in the COR and fate of the bone graft. Therefore, for revision THA in patients with severe medial wall defects, the combined use of bone graft and TM augmentation can be a suitable option.
Acknowledgements
This work was supported by a 2-year study grant from the Pusan National University
Author contributions
W.C.S. and K.T.S. designed the research. M.U.D., S.W.K. and J.J.K. conducted the search. W.C.S., M.U.D. and S.M.L. had full access to the study data and carried out all analysis. M.U.D. wrote the draft of this paper. W.C.S. and S.M.L. revised the article critically.
Funding
The authors did not receive any outside funding or grants in support of the study or during the preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
Data availability
The data utilized are accessible from the corresponding author upon reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lee, J. M. & Kim, T. H. Acetabular cup revision arthroplasty using morselized impaction allograft. Hip Pelvis.30, 65–77 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahmoud, A. N., Sundberg, M. & Flivik, G. Comparable results with porous metal augments in combination with either cemented or uncemented cups in revision hip arthroplasty: An analysis of one hundred forty-seven revisions at a mean of five years. J. Arthroplasty32, 1612–1617 (2017). [DOI] [PubMed] [Google Scholar]
- 3.Ulrich, S. D. et al. Total hip arthroplasties: What are the reasons for revision?. Int. Orthop.32, 597–604 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Böhm, P. & Bischel, O. Femoral revision with the Wagner SL revision stem: Evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J. Bone Joint Surg. Am.83, 1023–1031 (2001). [PubMed] [Google Scholar]
- 5.Weeden, S. H. & Paprosky, W. G. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J. Arthroplasty.17, 134–137 (2002). [DOI] [PubMed] [Google Scholar]
- 6.Jenkins, D. R., Odland, A. N., Sierra, R. J., Hanssen, A. D. & Lewallen, D. G. Minimum five-year outcomes with porous tantalum acetabular cup and augment construct in complex revision total hip arthroplasty. J. Bone Joint Surg. Am.99, e49 (2017). [DOI] [PubMed] [Google Scholar]
- 7.Nehme, A., Lewallen, D. G. & Hanssen, A. D. Modular porous metal augments for treatment of severe acetabular bone loss during revision hip arthroplasty. Clin. Orthop. Relat. Res.429, 201–208 (2004). [DOI] [PubMed] [Google Scholar]
- 8.Eachempati, K. K. et al. Results of trabecular metal augments in Paprosky IIIA and IIIB defects: A multicentre study. Bone Joint. J.100-B, 903–908 (2018). [DOI] [PubMed] [Google Scholar]
- 9.Deng, W. et al. Medial wall reconstruction using metal disc augments in revision total hip arthroplasty. Int. Orthop.47, 1203–1212 (2023). [DOI] [PubMed] [Google Scholar]
- 10.Zhou, B. et al. The utilization of metal augments allows better biomechanical reconstruction of the hip in revision total hip arthroplasty with severe acetabular defects: A comparative study. J. Arthroplasty33, 3724–3733 (2018). [DOI] [PubMed] [Google Scholar]
- 11.Weeden, S. H. & Schmidt, R. H. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J. Arthroplasty.22, 151–155 (2007). [DOI] [PubMed] [Google Scholar]
- 12.Humphrey, T. J. et al. The dome technique for managing massive anterosuperior medial acetabular bone loss in revision total hip arthroplasty: Short-term outcomes. Hip Pelvis.35, 122–132 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shen, X., Qin, Y., Li, Y., Tang, X. & Xiao, J. Trabecular metal versus non-trabecular metal acetabular components for acetabular revision surgery: A systematic review and meta-analysis. Int. J. Surg.100, 106597 (2022). [DOI] [PubMed] [Google Scholar]
- 14.Bobyn, J. D., Stackpool, G. J., Hacking, S. A., Tanzer, M. & Krygier, J. J. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J. Bone Joint Surg. Br.81, 907–914 (1999). [DOI] [PubMed] [Google Scholar]
- 15.Shin, W. C., Moon, N. H., Jeon, S. B. & Suh, K. T. Comparison of surgical outcomes between standard and elevated-rim highly cross-linked polyethylene acetabular liners in primary total hip arthroplasty with minimum 15-year follow-up: Single-center, retrospective cohort study. J. Arthroplasty.35, 1290–1296 (2020). [DOI] [PubMed] [Google Scholar]
- 16.Joshi, R. P., Eftekhar, N. S., McMahon, D. J. & Nercessian, O. A. Osteolysis after Charnley primary low-friction arthroplasty. A comparison of two matched paired groups. J. Bone Joint Surg. Br.80, 585–590 (1998). [DOI] [PubMed] [Google Scholar]
- 17.Cruz-Pardos, A., García-Rey, E. & García-Cimbrelo, E. Total hip arthroplasty with use of the cementless Zweymüller alloclassic system: A concise follow-up, at a minimum of 25 years, of a previous report. J. Bone Joint Surg. Am.99, 1927–1931 (2017). [DOI] [PubMed] [Google Scholar]
- 18.Ranawat, C. S., Dorr, L. D. & Inglis, A. E. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J. Bone Joint Surg. Am.62, 1059–1065 (1980). [PubMed] [Google Scholar]
- 19.Oommen, A. T., Krishnamoorthy, V. P., Poonnoose, P. M. & Korula, R. J. Fate of bone grafting for acetabular defects in total hip replacement. Indian. J. Orthop.49, 181–186 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Löchel, J., Janz, V., Hipfl, C., Perka, C. & Wassilew, G. I. Reconstruction of acetabular defects with porous tantalum shells and augments in revision total hip arthroplasty at ten-year follow-up. Bone Joint J.101-B, 311–316 (2019). [DOI] [PubMed] [Google Scholar]
- 21.Abolghasemian, M. et al. Combined trabecular metal acetabular shell and augment for acetabular revision with substantial bone loss: A mid-term review. Bone Joint. J.95-B, 166–172 (2013). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data utilized are accessible from the corresponding author upon reasonable request.