Abstract
Background:
Globally, a rising trend has been observed in the prevalence of thyroid disorders, with many demographic and geographic factors influencing its epidemiology. Nonetheless, some cases often go undetected due to the inconsistent and non-specific nature of the clinical symptoms. Therefore, we aimed to determine the trend and relationship between various pathological findings in thyroid disease patients and their demographic factors to aid clinicians in making a prompt diagnosis and treatment plan.
Methods:
A descriptive correlational study was conducted from January 2020 to May 2022 at Jinnah Postgraduate Medical Center, Karachi. We collected data via random sampling from 258 patients suffering from thyroid disorders. We evaluated baseline patient characteristics, along with, thyroid scan and fine needle aspiration cytology (FNAC) reports, and local thyroid gland examination findings.
Results:
Out of 258 participants, 192 (74.4%) were females, whereas 66 (25.6%) were males, giving a female: male ratio of 2.9: 1. On local examination, 167 (64.7%) were found to have a solitary nodule, 79 (30.6%) had multinodular goiter. Findings revealed that benign follicular lesions had the highest prevalence (35.3%). Moreover, among the cancerous growth, papillary carcinoma presented the highest cases (12.4%). Of 258 cases, 24 patients had non-surgical interventions, while most (234) had surgical interventions. Total thyroidectomy was the most common procedure opted for by 45.3% (n = 117) of the participants, followed by lobectomy 70 (27.1%), near total thyroidectomy 43 (13.2%), modified radical neck dissection 5 (1.9%).
Conclusion:
Our study showed that nearly all thyroid-related pathologies were more prevalent amongst females than males, with the majority having an acute to sub-acute clinical presentation. Multinodular goiter was a prominent finding indicating a greater need for screening tools and access to healthcare facilities, especially in rural areas, to allow future studies to compare provinces accurately.
Keywords: Thyroid, epidemiology, demographic, Pakistan, multinodular goiter
Plain Language Summary
Trends of Pathological Findings in Patients with Thyroid Diseases
The thyroid gland plays a critical role in the body’s developmental and metabolic processes. There has been a worldwide rise in thyroid related diseases. This has been attributed to different factors including geography, smoking, genetics etc. However, often due to the non specific nature of disease, the condition often goes undiagnosed until an advanced disease stage, often causing complications. In this study, we aimed to assess the trends and relationship between the different clinical and pathological findings in thyroid disease patients from Pakistan. About 9.7% of our patients were suffering from hypothyroid while a 28.7% suffered from hyperthyroidism while a remaining majority of 61.6% individuals remained euthyroid. Ultrasound findings showed that 96.8% patients has a thyroid mass/nodule or goiter with the highest proprtion of these individuals being found in the middle age (30-50 years) group. Further majority of the diseased population comprised of females. A greater proportion of our patient population required surgical intervention with total thyroidectomy being the most common procedure (45.3%). It is of great importance to continue researching modern trends, presentation and management protocols for thyroid disease, adding to the existing literature.
Introduction
The thyroid gland is one of the most significant endocrine organs in charge of controlling cellular metabolism, essential for the body’s healthy growth and development. 1 Any interference with the hypothalamic-pituitary-thyroid (HPT) axis can cause an imbalance in the thyroid hormones’ normal modulation, eventually aiding in the emergence of thyroid disease. 2 Thyroid dysfunction (hyperthyroidism, hypothyroidism, and subclinical hypo/hyperthyroidism) and structural diseases are the two major categories for thyroid diseases (goiter, benign nodules, and malignant neoplasms).
The incidence of thyroid disorders has increased over the past 3 decades, which could negatively affect populations.3,4 For example, in Pakistan, the prevalence of hypothyroidism and hyperthyroidism is 4.1% and 5.1%, respectively, whereas the prevalence of subclinical hyperthyroidism and subclinical hypothyroidism is 5.8% and 5.4%, respectively.5 -7 Additionally, over 10 years in India, the incidence rate of thyroid cancer rose 62% and 48% in women and men, respectively. 8
Owing to the largely inconsistent and often vague clinical symptoms, the diagnosis of thyroid dysfunction primarily depends on biochemical confirmation, with serum thyroid stimulating hormone (TSH) levels being the most reliable indicator of thyroid status. 4
If undiagnosed or untreated, dangerous complications can occur, such as thromboembolism, osteoporosis, congestive heart failure, delirium, and conduction defects, including atrial fibrillation and death. 9
While thyroid ailments impact a significant proportion of the world, the frequency and type of thyroid disease depend upon various demographic and geographic factors, including iodine intake. 10 In addition, several studies have noted the effect of age, gender, ethnicity, smoking, drug exposure, and other risk factors on the levels of TSH and thyroid disease epidemiology.11,12
Given the extensive incidence of thyroid disorders being reported in Pakistan with gradually advancing geographical variation, this study aims to highlight the incidence of common thyroid diseases, their findings, and their correlation with gender and age to help identify disease patterns and help evaluate the efficacy of diagnostic tests in the population of Pakistan.
Methodology
We conducted a descriptive correlational study in which we retrospectively studied thyroid reports and examination findings of patients to determine the types and frequencies of different neoplastic and non-neoplastic thyroid lesions. This study was approved by the Ethics Committee of Ziauddin University (0030621MNY5) and the Review Board of Jinnah Postgraduate Medical Centre (F.2-81/2022-GENL/208/JPMC). Samples were taken from the Department of Medicine/Oncology, Jinnah Postgraduate Medical Center (JPMC), Karachi, one of Pakistan’s largest government-run tertiary care hospitals.
Sample size for the study was calculated with an estimated prevalence of thyroid disease in Pakistan that is being 10%. 5 At 95% confidence level, and 5% margin of error, the minimum required sample size for the study was calculated to be 139 patients.
Our study was from January 2020 to May 2022, with a sample size of 258 participants recruited via random sampling. Both male and female patients aged between 5 and 70 and from rural and urban areas were included in this study. The patient population was divided into 2 age groups: children (aged 5-18 years) and adults (18-70 years). We excluded patients presenting with pathologies apart from thyroid-related ones.
The study was conducted by evaluating reports of inpatient admissions, including complete thyroid profile, thyroid scan, Fine Needle Aspiration Cytology (FNAC) findings, and clinical findings obtained during a comprehensive local examination of the thyroid gland. In addition, secondary data regarding demographics, past medical history, family history, and clinical details pertaining to each sampled participant’s disease was collected from their hospital file. Data was accessed after obtaining permission from the institute’s surgery department. Excel data sheet and IBM SPSS software version 20.0 were used to analyze the statistical data obtained.
Results
After meeting our study’s inclusion criteria, we enrolled patient samples comprising 258 participants. The sociodemographic and clinical parameters of the participants are presented in Table 1. Out of 258 participants, 192 (74.4%) were females, whereas 66 (25.6%) were males, giving a female: male ratio of 2.9:1. The age of the patients ranged from 5 to 70 years, with a mean age of 37.9 years. 5.8% (n = 15) of the population were children (aged less than 18 years), and 94.2% (n = 243) were adults (18-50+ years). The demographic of the patients was divided into 2 sections: Rural and Urban. A vast majority of 193 (74.8%) of the sample belonged to urban, and 65 (25.2%) were from rural regions. Furthermore, all of the patients had undergone preliminary local examination of the thyroid in order to ensure reliability, of which 113 (43.8%) were found to have a solitary nodule, 95 (36.8%) had multinodular goiter, 95 (36.8%) had diffuse enlargement, whereas the remainder of patients had normal findings. Additionally, 67 out of the 258 patients had palpable lymph nodes, whilst the remaining 191 participants had non-palpable lymph nodes. Finally, the clinical status was assessed and came about as euthyroid for 159 (61.6%) of the participants, hyperthyroid for 74 (28.7%), and hypothyroid for only 25 (9.7%) persons.
Table 1.
Sociodemographic and clinical parameters of patients.
| Parameters | Frequency | Percentage | |
|---|---|---|---|
| Gender | Male | 66 | 25.6 |
| Female | 192 | 74.4 | |
| Age (Y) | <18 | 15 | 5.8 |
| 18-30 | 72 | 27.9 | |
| 30-50 | 122 | 47.3 | |
| >50 | 49 | 19.0 | |
| Residence | Rural | 65 | 25.2 |
| Urban | 193 | 74.8 | |
| Duration of onset of symptoms (Y) | <1 | 108 | 41.9 |
| 1-10 | 121 | 46.9 | |
| 10-20 | 25 | 9.7 | |
| >20 | 4 | 1.6 | |
| Local examination | Diffused goiter | 42 | 16.3 |
| Multinodular goiter | 95 | 36.8 | |
| Solitary nodule | 113 | 43.87 | |
| Lymph nodes | Palpable | 67 | 25.97 |
| Not palpable | 191 | 74.03 | |
| Non-available examinations | 8 | 3.1 | |
| Clinical status | Euthyroid | 159 | 61.6 |
| Hypothyroid | 25 | 9.7 | |
| Hyperthyroid | 74 | 28.7 | |
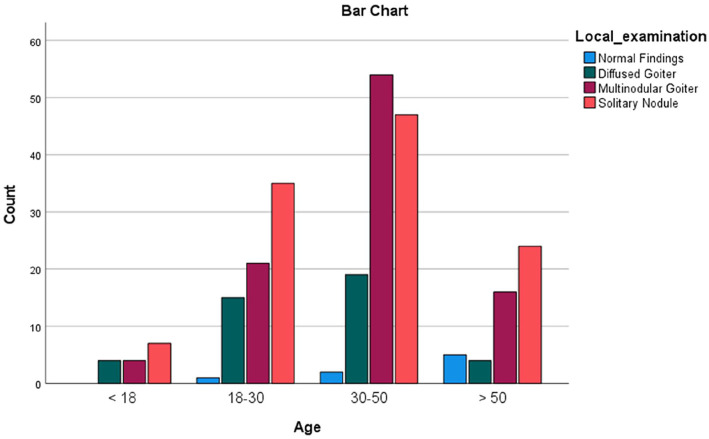
Furthermore, we categorized age into 4 major groups, namely, children and adolescents (<18 years), young adults (18-30 years), middle-aged adults (30-50 years), as well as old-age adults (aged 50 years and above). Hence, this enabled us to make age-wise comparisons based on the local examination findings. Figure 1 illustrates and correlates these findings with the corresponding age groups. According to our results, nearly half of the participants (n = 122) belong to the middle-aged adult group, among which the majority of them had multinodular goiter (n = 54). Moreover, the majority of the diffused thyroid goiter (n = 15 and 19) were present in young adult and middle-aged adult groups, respectively. In contrast to this, the elderly age group reported only 4 cases of findings consistent with diffuse goiter.
Figure 1.
Age distribution of local examination findings of the neck.
Furthermore, Table 2 shows the gender distribution of patients with respect to thyroid lesion based on the ultrasound findings, which exhibits the conclusions obtained from the cases. According to the ultrasound findings, 28.7% of the total sample presented with nodules in one lobe, out of which 73.0% were in females, in contrast to 27.0% in males. Moreover, 23.6% of participants had multinodular goiter, of which female participants formed the majority (86.9%).
Table 2.
Frequency and gender distribution of common pathologies associated with the thyroid gland based on ultrasound imaging.
| Pathologies | Frequency | Gender | |
|---|---|---|---|
| n (%) | Male | Female | |
| n (%) | n (%) | ||
| One lobe enlargement | 2 (0.8) | 0 (0.0) | 2 (100) |
| Both lobes enlargement | 42 (16.3) | 11 (26.2) | 31 (73.8) |
| Parathyroid enlargement | 2 (0.8) | 1 (50.0) | 1 (50.0) |
| Multinodular goiter | 61 (23.6) | 8 (13.1) | 53 (86.9) |
| Mass lesion in one lobe | 20 (7.8) | 8 (40.0) | 12 (60.0) |
| Mass lesions in both lobes | 34 (13.2) | 10 (29.4) | 24 (70.5) |
| Nodule in one lobe | 74 (28.7) | 20 (27.0) | 54 (73.0) |
| Nodule in both lobes | 17 (6.6) | 3 (17.6) | 14 (82.4) |
| Total | 252 (100.0) | 61 (24.2) | 191 (75.8) |
FNAC was done in cases that warranted histopathological correlation. Table 3 shows that our findings revealed that findings suggestive of benign follicular lesions had the highest prevalence (35.3%). Moreover, among the cancerous growth, papillary carcinoma presented the highest cases (12.4%), while medullary and follicular carcinomas were 5.4% and 4.3% respectively. At the same time, the prevalence of diffuse and multi-nodular goiter based on the FNAC findings was 15.9% and 23.3%, respectively. FNAC findings for 5 patients (1.8%) were not available. Of 258 cases, 24 patients had non-surgical interventions whereas the remainder (234) had surgical interventions, citing cosmetic reasons, patient will and improved quality of life . Total thyroidectomy was the most common procedure opted for by 45.3% (n = 117) of the participants, followed by lobectomy 70 (27.1%), near total thyroidectomy 43 (13.2%), modified radical neck dissection 5 (1.9%). The majority of the benign follicular nodule had undergone lobectomy (68.1%). Among the cancerous growths (follicular carcinoma, papillary carcinoma, and medullary carcinoma), the majority of them had undergone total thyroidectomy (91.0%, 59.4%, and 42.8%), respectively. Whereas near-total thyroidectomy was most commonly performed on patients presenting with medullary carcinoma (21.4%).
Table 3.
Prevalence of FNAC findings with respect to Surgical and non-surgical interventions.
| FNAC findings | Prevalence | Surgical intervention | Non-surgical intervention | ||||
|---|---|---|---|---|---|---|---|
| Lobectomy | Near total thyroidectomy | Total thyroidectomy | Parathyroidectomy | Modified radical neck dissection | |||
| Benign follicular nodule | 91 (35.3%) | 62 (68.1%) | 7 (7.7%) | 9 (9.8%) | 0 | 0 | 13 (14.3) |
| Diffuse goiter | 41 (15.9%) | 3 (7.3%) | 9 (22.0) | 29 (70.7%) | 0 | 0 | 0 |
| Multinodular goiter | 60 (23.3%) | 2 (3.3%) | 14 (18.3) | 44 (26.4%) | 0 | 0 | 0 |
| Follicular carcinoma | 11 (4.3%) | 1 (9.0%) | 0 | 10 (91.0%) | 0 | 0 | 0 |
| Papillary carcinoma | 32 (12.4%) | 0 | 1 (3.1%) | 19 (59.4%) | 0 | 4 (12.5%) | 8 (25.0%) |
| Medullary carcinoma | 14 (5.4%) | 1 (7.1%) | 3 (21.4%) | 6 (42.8%) | 0 | 1 (7.1%) | 3 (21.4%) |
| Parathyroid adenoma | 4 (1.6%) | 1 (25.0%) | 0 | 0 | 3 (75.0%) | 0 | 0 |
| N/A | 5 (1.8%) | 0 | 0 | 0 | 0 | 0 | 5 (100%) |
| Total | 258 (100%) | 70 (27.1%) | 34 (13.2%) | 117 (45.3%) | 3 (1.2%) | 5 (1.9%) | 24 (9.3%) |
Discussion
We investigated trends in the incidence of various thyroid pathologies using data representing the rural and urban populations of Pakistan. It is hoped that by highlighting the most common thyroid pathologies in Pakistan, clinicians will be able to redirect their center of focus and decide on suitable plans of action, management, and treatment tailored to each patient’s needs. According to the findings of our study, the prevalence of multinodular goiter rose from the lowest age group to the highest age group. A study conducted in Germany 13 produced similar results where, from the lowest to the oldest age group, the prevalence of goiter rose for both men and women, rising from 3.5% to 27.7% for males and 4.5% to 25.1% for females.
Another study by Khattak et al 14 in Germany found that the prevalence of thyroid nodules rose between SHIP-0 (1997-2001) and SHIP-TREND (2008-2012), with a more significant increase in females. The highest prevalence occurred in males aged 60 to 69 and females aged 50 to 59, concurrent with the results of our study which revealed solitary nodule as the most common thyroid pathology in almost all age groups, including adults aged 50 years and above. All thyroid pathologies were more common in females than males in our study, especially in the 30 to 50 age group, which accounted for roughly half of our sample size. A possible explanation for this could be the interaction of the thyroid gland with female reproductive hormones, released from puberty onward, which may lead to the onset of thyroid diseases and the formation of thyroid nodules. 15 Rapid physiological variations in estrogen levels during pregnancy and menopause can affect thyroid-binding protein concentrations and circulating thyroid hormone levels due to estrogen’s immunomodulatory effects.16,17 Moreover, since estrogen receptors are present in thyroid tissues, it can significantly accelerate the proliferation of thyroid cancer cells, promoting dysplasia and progression to thyroid malignancy.18,19
There has been a considerable rise in the incidence of thyroid cancer in various countries over the past few decades. 20 The majority of thyroid cancer patients in Pakistan manifest as multinodular goiters (59%), according to a study by Zuberi et al. 21 FNAC reports in our study reveal papillary cancer as the most common histological subtype found in both genders, a finding consistent with a global study comparing the geographical and temporal variation of thyroid cancer incidence by subtype in 25 countries. 22 There could be multiple reasons attributing to this rising trend of thyroid cancer incidence, particularly in Pakistan. Firstly, extensive use of advanced diagnostic modalities such as high-resolution thyroid ultrasonography and fine-needle aspiration has greatly improved diagnostic sensitivity. 23 Secondly, the study site for this research is one of Pakistan’s biggest Government-run tertiary care hospitals, catering to most of the rural and urban areas of both Sindh and Balochistan. It is likely that this enhanced healthcare access significantly contributed to better and earlier detection of all thyroid pathologies, including malignancy.
It has been suggested that the rising trend in thyroid cancer incidence is not a true rise but rather due to the overdiagnosis of small, localized papillary tumors from advanced diagnostic techniques. 24 Overdiagnosis involves identifying early-stage cancer through screening, where some cases might never progress to advanced stages or show clinical symptoms. 25 Between 2008 and 2012, overdiagnosis was responsible for approximately 93% of the new thyroid cancer cases in women in South Korea, 87% in China, 84% in Italy and Croatia, and 83% in France. 15 This same study observed that across all the countries analyzed, overdiagnosis was more prevalent in women than men, mirroring the consistent gender disparity in incidence with a female-to-male ratio of roughly 3:1, which was also noted in our study while comparing the incidence of common thyroid pathologies between genders. 15 The overdiagnosis hypothesis is supported by increasing thyroid cancer incidence with stable or declining mortality rates,26,27 along with new thyroid cancer cases, especially small tumors, correlating with the frequency of ultrasound, CT, and other diagnostic exams being performed. 28 However, our study’s data limitations necessitate further research into diagnostic methods, tumor characteristics (size, stage), treatments, and mortality rates to affirm the overdiagnosis hypothesis, particularly in Pakistan.
According to our results, 234 out of 258 patients underwent surgical intervention, with total thyroidectomy being the most preferred choice of surgery for almost half the cases, especially patients with follicular carcinoma. Thyroidectomy should be the primary treatment choice if there is a confirmed or suspected presence of thyroid cancer, 29 and it is generally indicated for patients with hyperthyroidism experiencing local compressive symptoms due to a large goiter, suspicious or malignant thyroid nodules, or moderate to severe Graves’ ophthalmopathy. In patients with Graves’ disease, total thyroidectomy is the recommended surgical procedure since it carries a lower risk of recurrent hyperthyroidism compared to subtotal thyroidectomy. 30 It is also important to note that most of the benign follicular nodule patients in our study had undergone lobectomy/hemithyroidectomy, which may also be effective, especially in older patients with comorbidities for whom invasive surgical approaches should be avoided. 31
The NHANES 1999 to 2018 study examined 57 540 participants and found that the age-standardized prevalence of thyroid disease among US adults rose from 1999 to 2003, stabilized between 2003 and 2014, and increased again from 2014 to 2018, with the highest rates seen in individuals aged ⩾60 years, women, and non-Hispanic Whites. Multiple regression analysis indicated that age, female gender, body mass index (BMI), higher education, and income levels were individually linked to an elevated risk of thyroid disease. 32 Given the continuous global rise in thyroid disease incidence, monitoring its occurrence and analyzing trends are essential for advancing disease prevention and treatment strategies. This information also supports informed decision-making for health administrative authorities and enables the proper allocation of medical and financial resources. Further information on relevant characteristics, including iodine intake, BMI, menstrual and pregnancy factors, family history, and environmental factors is necessary to thoroughly understand the risk factors and specific trends.
Strengths and Limitations
One of the significant strengths of this study is that an ethnically diverse population visits the tertiary care hospital from where the samples were taken. Therefore, our sample size included not only the urban population but also people from rural, thus making the analysis more representative and accounting for differences in urban and rural socio-economic differences. In addition, the sample was representative of both genders and a wide age range (from children to old adults were part of the sample size) over 3 years.
However, due to the hospital’s location in the heart of the busiest metropolitan in the country, the sample size consisted primarily of urban residents. Nonetheless, post-surgical histopathological findings could not be correlated due to the implications of COVID-19 lockdown thereby causing patients being lost to follow up. Another limitation was that despite a large sample size, the female: male ratio was 2.9:1. A study that builds on the current study’s limitations needs to be conducted, ideally including an equal number of people from all provinces to account for some differences.
Conclusion
Our article highlights the incidence of some of the common thyroid pathologies in Pakistan. There is a need for regular thyroid inspection in the region along with the implementation of disease-preventative precautions such as iodized salt, etc. We further highlighted the efficacy of FNAC in diagnosing and subsequently treating thyroid pathologies. There is further a need to make clinicians and diagnostic and treatment modalities more available to the public to allow disease prevention and cure.
Acknowledgments
None.
Footnotes
ORCID iD: Sajjad Ali  https://orcid.org/0000-0002-8024-5942
https://orcid.org/0000-0002-8024-5942
Declarations
Ethics Approval: This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Jinnah Sindh Medical University (F.2-81/2022-GENL/208/JPMC, on 7th July 2022) and the Ethics Committee of Ziauddin University (0030621MNY5).
Consent for Publication: A written formal consent was taken from the participants and/or their guardians for participants of age less then 18 years.
Author Contributions: All authors have contributed equally to this study.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Competing Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of Data and Material: The data that support the findings of this study are available on request from the corresponding author.
References
- 1. Rasheed H, Elahi S, Syed Z, Rizvi NB. Trend of thyroid dysfunction associated with visible goiter. J Sci Res. 2009;39. [Google Scholar]
- 2. Shah N, Ursani TJ, Shah NA, Raza HMZ. Prevalence and manifestations of hypothyroidism among population of Hyderabad, Sindh, Pakistan. Pure Appl Biol. 2021;10:668-675. [Google Scholar]
- 3. Dal Maso L, Panato C, De Paoli A, et al. Trends in thyroid function testing, neck ultrasound, thyroid fine needle aspiration, and thyroidectomies in north-eastern Italy. J Endocrinol Invest. 2021;44:1679-1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Taylor PN, Albrecht D, Scholz A, et al. Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol. 2018;14:301-316. [DOI] [PubMed] [Google Scholar]
- 5. Ullah F, Ali SS, Tahir H. Clinical spectrum of thyroid disorders: an experience at a tertiary care hospital in Peshawar. Pak J Med Res. 2022;61:56-62. [Google Scholar]
- 6. Qureshi IS, Khalid S, Jabeen S, et al. Frequency of different thyroid disorders among females attending sir Ganga ram Hospital, Lahore. Asian J Allied Health Sci. 2020;4:20-28. [Google Scholar]
- 7. Iqbal MA, Naseem Z, Qureshy A, Shahid A, Roohi N. Prevalence and manifestations of thyroidal dysfunction in Central Punjab Pakistan (a case study). Sci Int. 2016;28:3959-3963. [Google Scholar]
- 8. Sekkath Veedu J, Wang K, Lei F, Chen Q, Huang B, Mathew A. Trends in thyroid cancer incidence in India. J Clin Oncol. 2018;36(15_suppl). doi:10.1200/jco.2018.36.15_suppl.e18095 [Google Scholar]
- 9. Devereaux D, Tewelde SZ. Hyperthyroidism and thyrotoxicosis. Emerg Med Clin North Am. 2014;32:277-292. [DOI] [PubMed] [Google Scholar]
- 10. Bjoro T, Holmen J, Kruger O, et al. Prevalence of thyroid disease, thyroid dysfunction and thyroid peroxidase antibodies in a large, unselected population. The health study of nord-Trondelag (HUNT). Eur J Endoc. 2000;143:639-647. [DOI] [PubMed] [Google Scholar]
- 11. Wiersinga WM. Smoking and thyroid. Clin Endocrinol. 2013;79:145-151. [DOI] [PubMed] [Google Scholar]
- 12. González-Rodríguez LA, Felici-Giovanini ME, Haddock L. Thyroid dysfunction in an adult female population: a population-based study of Latin American vertebral osteoporosis study (LAVOS)-Puerto Rico Site hypothyroidism in LAVOS-Puerto Rico site. Endocr Pract. 2013;32:57. [PMC free article] [PubMed] [Google Scholar]
- 13. Reiners C, Wegscheider K, Schicha H, et al. Prevalence of thyroid disorders in the working population of Germany: ultrasonography screening in 96,278 unselected employees. Thyroid. 2004;14:926-932. [DOI] [PubMed] [Google Scholar]
- 14. Khattak RM, Ittermann T, Nauck M, Below H, Völzke H. Monitoring the prevalence of thyroid disorders in the adult population of Northeast Germany. Popul Health Metr. 2016;14:39-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li M, Maso LD, Vaccarella S. Global trends in thyroid cancer incidence and the impact of overdiagnosis. Lancet Diabetes Endocrinol. 2020;8:468-470. [DOI] [PubMed] [Google Scholar]
- 16. del Ghianda S, Tonacchera M, Vitti P. Thyroid and menopause. Climacteric. 2014;17:225-234. [DOI] [PubMed] [Google Scholar]
- 17. Takyar M, Rahmani M, Amouzegar A, et al. Parity and incidence of thyroid autoimmunity: a population-based Tehran thyroid study. Thyroid. 2020;30:1186-1192. [DOI] [PubMed] [Google Scholar]
- 18. Park J, Park H, Kim TH, et al. Trends in childhood thyroid cancer incidence in Korea and its potential risk factors. Front Endocrinol. 2021;12:681148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lee ML, Chen GG, Vlantis AC, et al. Induction of thyroid papillary carcinoma cell proliferation by estrogen is associated with an altered expression of Bcl-xl. Cancer J. 2005;11:113-121. [DOI] [PubMed] [Google Scholar]
- 20. Vaccarella S, Franceschi S, Bray F, et al. Worldwide thyroid-cancer epidemic? The increasing impact of overdiagnosis. New Engl J Med. 2016;375:614-617. [DOI] [PubMed] [Google Scholar]
- 21. Zuberi LM, Yawar A, Islam N, Jabbar A. Clinical presentation of thyroid cancer patients in Pakistan–AKUH experience. J Pak Med Assoc. 2004;54:526. [PubMed] [Google Scholar]
- 22. Miranda-Filho A, Lortet-Tieulent J, Bray F, et al. Thyroid cancer incidence trends by histology in 25 countries: a population-based study. Lancet Diabetes Endocrinol. 2021;9:225-234. [DOI] [PubMed] [Google Scholar]
- 23. Brito JP, Davies L. Is there really an increased incidence of thyroid cancer? Curr Opin Endocrinol Diabetes Obes. 2014;21:405-408. [DOI] [PubMed] [Google Scholar]
- 24. Wartofsky L. Increasing world incidence of thyroid cancer: increased detection or higher radiation exposure? Hormones. 2010;9:103-108. [DOI] [PubMed] [Google Scholar]
- 25. Xu L, Cao ZX, Weng X, Wang CF. Global thyroid cancer incidence trend and age-period-cohort model analysis based on global burden of disease study from 1990 to 2019. Front Endocrinol. 2023;14:1133098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cheng F, Xiao J, Shao C, et al. Burden of thyroid cancer from 1990 to 2019 and projections of incidence and mortality until 2039 in China: findings from global burden of disease study. Front Endocrinol. 2021;12:738213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Li M, Brito JP, Vaccarella S. Long-term declines of thyroid cancer mortality: an international age-period-cohort analysis. Thyroid. 2020;30:838-846. [DOI] [PubMed] [Google Scholar]
- 28. Ahn HS, Kim HJ, Welch HG. Korea’s thyroid-cancer “epidemic”–screening and overdiagnosis. New Engl J Med. 2014;371:1765-1767. [DOI] [PubMed] [Google Scholar]
- 29. Ross DS, Burch HB, Cooper DS, et al. 2016 American thyroid association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016;26:1343-1421. [DOI] [PubMed] [Google Scholar]
- 30. Guo Z, Yu P, Liu Z, Si Y, Jin M. Total thyroidectomy vs bilateral subtotal thyroidectomy in patients with Graves’ diseases: a meta-analysis of randomized clinical trials. Clin Endocrinol. 2013;79:739-746. [DOI] [PubMed] [Google Scholar]
- 31. Wang Z, Vyas CM, Van Benschoten O, et al. Quantitative analysis of the benefits and risk of thyroid nodule evaluation in patients ⩾70 years old. Thyroid. 2018;28:465-471. [DOI] [PubMed] [Google Scholar]
- 32. Zhang X, Wang X, Hu H, et al. Prevalence and trends of thyroid disease among adults, 1999-2018. Endocr Pract. 2023;29:875-880. [DOI] [PubMed] [Google Scholar]