Abstract
Multiple sclerosis is a chronic inflammatory demyelinating disease of the central nervous system. BCG-PSN is one of the immunomodulators to treat urticaria. We report the case of a 37-year-old woman who developed neurological symptoms following BCG-PSN treatment for urticaria, and whose MRI showed signs suggestive of multiple sclerosis.
Keywords: Multiple sclerosis, BCG-PSN, Urticaria, MRI, Case report
Introduction
Multiple sclerosis (MS) is a chronic inflammatory demyelinating disease of the central nervous system (CNS). MS as a multifactorial immune-mediated disease is influenced by genetic and environmental factors. The pathological characteristic of MS is the demyelinating lesions in the CNS, which may be accompanied by neuraxial damage [1]. Urticaria is a mast cell-driven, limited edema reaction caused by dilation and increased permeability of small blood vessels in the skin and mucous membranes. Clinical manifestations include pruritic masses of varying size. The lifetime incidence of acute urticaria is approximately 20% [2]. Bacillus Calmette-Guérin polysaccharide ribonucleic acid (BCG-PSN) is one of the immunomodulators to treat urticaria. It is a mixture of nucleic acids and polysaccharides obtained from Mycobacterium bovis by the hot phenol method [3]. It had been reported in case reports that Mycobacterium tuberculosis (MTB) is a significant but neglected factor involved in the pathogenic mechanisms of MS [4]. However, it is unclear whether BCG-PSN can also cause MS. Here, we describe a case of multiple sclerosis after BCG-PSN treatment.
Case report
A 37-year-old woman was admitted to our department, because of unfavorable speech with crooked corners of the mouth for 5 days. She was diagnosed with hives 10 years ago. Two months ago, she developed hives after the upper respiratory infection. She sought treatment at the dermatology department and received oral treatment with epinastine hydrochloride capsules, ketotifen fumarate tablets, levamisole hydrochloride tablets, and thymidine enteric-coated capsules. In addition, she received intramuscular BCG-PSN injections. During her treatment, she developed dizziness and weakness, which persisted without relief and was not taken seriously or treated. She stopped the above treatment after 2 months of medication. Five days before the first time that the patient is seen in the clinic, she presented with a slight lack of fluency in speech, together with a slight tilting of the corners of the mouth to the left and drooling from the right side of the mouth after exertion. The above symptoms persisted. She presented to the local community hospital with a diagnosis of peripheral facial nerve palsy and was treated with oral ribavirin tablets for antiviral and oral vitamin B1 tablets and mecobalamin tablets for nerve nutrition. Three days later, her speech disfluency was worse than before, along with impaired finger movement in both hands. She visited local municipal hospital and perfected magnetic resonance imaging (MRI), which suggested multiple abnormal signal shadows in the cranium. She was then admitted to our hospital for further diagnosis and treatment. She had no fever, blurred vision, numbness of the limbs, or urinary or fecal disturbances throughout the course of the disease. Physical examination showed dysphagia, right-sided facial paralysis, right limbs muscle strength grade 4, right Babinski's sign positive.
After being admitted to our hospital, blood tests demonstrated antinuclear antibody (ANA) positive (1:320). Cell-based assays (CBA) showed that serum and cerebrospinal fluid (CSF) MOG-IgG, AQP4-IgG were negative. CSF examination showed total protein concentration and white cell count are normal, which with positive intrathecal oligoclonal bands (unmatched in the serum), and the IgG index was elevated (39.40 mg/L; normal range, <34.00 mg/L). Brain MRI showed multiple abnormal signals in the bilateral frontal and occipital lobes, right temporal lobe (Fig. 1, Fig. 2, Fig. 3). With gadolinium, all lesions were enhanced. (Fig. 4). The cervical and thoracic cord MRI were normal (Fig. 5). The diagnosis of MS was established according to the 2017 McDonald criteria: 1 clinical relapse, periventricular and cortical typical brain MS-like lesions, and a positive test for oligoclonal bands in the CSF.
Fig. 1.
MRI was completed 6 days after the onset of neurologic symptoms. T2 flair images showed multiple foci of hyperintense in bilateral frontal and occipital lobes, right temporal lobe.
Fig. 2.
T2WI showed multiple hyperintense lesions in the right temporal lobe, bilateral frontal and occipital lobes.
Fig. 3.
Brain MRI of the sagittal sequence revealing multiple hypointense lesions at the periventricular and subcortical matter on T1WI.
Fig. 4.
Annular enhancement lesions in the bilateral frontal and occipital lobes, right temporal lobe.
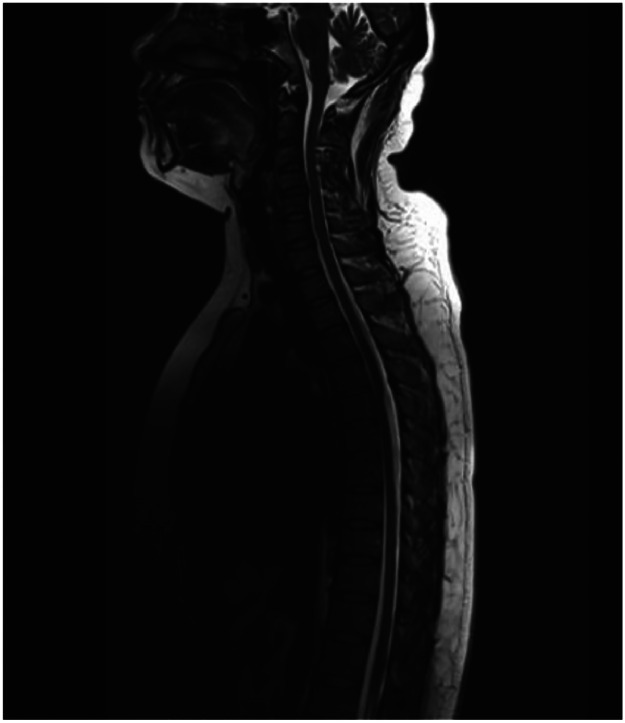
Fig. 5.
No abnormal signal on cervical cord and thoracic cord MRI.
After being given a high dose of methylprednisolone intravenously (1000 mg × 3 days), her symptoms alleviated. Then she received oral prednisone taper therapy. After 6 months, we re-evaluated the patient's condition. Fortunately, she didn't have a clinical relapse and got better. Her brain MRI revealed no new T2 lesions or enhancing lesions.
Discussion
Considering the clinical manifestations, CSF positive intrathecal oligoclonal bands, and brain MRI results, this patient was finally diagnosed with MS after other diagnoses were excluded. With no certain aetiology, this disease is influenced by genetic and environmental factors. Since the pathogenesis of MS is immune-mediated, it has been suggested that infectious diseases are possible triggers of the onset of the disease [1]. After excluding other possible factors, we considered that the onset of this patient's disease might be related to the injection of BCG-PSN.
BCG-PSN plays a crucial role in Th1/Th2 balance in patients with urticaria. BCG-PSN has the capability to harmonize the CD4 and CD8 subsets of T cells and the Th1 and Th2 subtypes of helper T cells [5]. BCG-PSN promotes Th1 activation, production of IFN-γ and IL-2, and inhibits IL-4 and IL-10, thereby regulating the Th1/Th2 balance [6]. IgE plays an important role in the pathogenesis of urticaria, which can be enhanced by IL-4 through B-cell division [7]. IFN-γ inhibits this transformation, thereby halting the production of specific IgE. IL-2 promotes the production of IFN-γ. IL-10 depresses IFN-γ activity, leaving the previous IL-4 to function in the IgE cascade, which may lead to reduced production of proinflammatory cytokines and chemokines [6]. Consequently, promotion of IL-2 and inhibition of IL-10 production can inhibit IgE production and restore the abnormal skin symptoms of urticaria.
Experimental autoimmune encephalomyelitis (EAE) is a model for studying MS. EAE was induced in male mice using murine myelin oligodendrocyte glycoprotein (MOG) peptides combined with heat-inactivated MTB and pertussis toxin [8]. EAE formation involves immunization by a MOG peptide emulsified in complete Freund's adjuvant (CFA) containing inactivated MTB.
The antigenic component of MTB activates dendritic cells, which promotes the process of cytokine production by T cells. This process boosts the Th1 response through toll-like receptors. Studies have shown that the number and species of MTB are associated with the formation of EAE [9]. MTB is a possible pathogenetic causes of autoimmune diseases. It was found that Mycobacterium avium subspecies paratuberculosis (MAP) has 100% sequence homology with MTB [10]. In studies of MS, antibodies against BOLF1 and MAP-4027 were found to cross-react with IRF5 [11]. This leads to the conclusion that multiple sclerosis may develop through MTB-related antigens. However, further experimental confirmation of this result is necessary. The most accepted mechanism leading to MS is that MTB infection triggers inflammatory demyelinating in the CNS through immune mediation [4].
In summary, the possible mechanisms for the development of MS after BCG-PSN treatment are likely related to T-cell activation and cross immune reactions. There are no reports of inflammatory demyelinating disease of CNS caused by BCG-PSN injections and this hypothesis needs further experimental confirmation. We need to consider the possibility of triggering MS after the use of immunomodulators.
Authors’ contributions
All authors have made important contributions to the manuscript and have approved the final version of the manuscript.
Patient consent
An informed consent was obtained from the patient.
This work was approved by the ethics committee of the Shanxi Provincial People's Hospital of the Shanxi Medical University.
Footnotes
Acknowledgments: This work was supported by the Shanxi Key Laboratory of Brain Disease Control (202104010910014) and the Research Project of Shanxi Province Health Commission (2020TD25).
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Filippi M, Bar-Or A, Piehl F, Preziosa P, Solari A, Vukusic S, et al. Multiple sclerosis. Nat Rev Dis Primers. 2018;4(1):43. doi: 10.1038/s41572-018-0041-4. [DOI] [PubMed] [Google Scholar]
- 2.Zuberbier T, Abdul Latiff AH, Abuzakouk M, Aquilina S, Asero R, Baker D, et al. The international eaaci/ga2len/euroguiderm/apaaaci guideline for the definition, classification, diagnosis, and management of urticaria. Allergy. 2022;77(3):734–766. doi: 10.1111/all.15090. [DOI] [PubMed] [Google Scholar]
- 3.Sun J, Hou J, Li D, Liu Y, Hu N, Hao Y, et al. Enhancement of hiv-1 DNA vaccine immunogenicity by bcg-psn, a novel adjuvant. Vaccine. 2013;31(3):472–479. doi: 10.1016/j.vaccine.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 4.Han K, Wang Y, Li S, Ye T, Li M, Wang J. Ophthalmoplegia with a focal lesion in the interpeduncular fossa as the initial symptoms of multiple sclerosis: 3-year follow-up. J Int Med Res. 2024;52(1) doi: 10.1177/03000605231208570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiong C, Li Q, Lin M, Li X, Meng W, Wu Y, et al. The efficacy of topical intralesional bcg-psn injection in the treatment of erosive oral lichen planus: A randomized controlled trial. J Oral Pathol Med. 2009;38(7):551–558. doi: 10.1111/j.1600-0714.2009.00796.x. [DOI] [PubMed] [Google Scholar]
- 6.Li N, Cao N, Niu YD, Bai XD, Lu J, Sun Y, et al. Effects of the polysaccharide nucleic acid fraction of bacillus calmette-guérin on the production of interleukin-2 and interleukin-10 in the peripheral blood lymphocytes of patients with chronic idiopathic urticaria. Biomed Rep. 2013;1(5):713–718. doi: 10.3892/br.2013.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Du Toit G, Prescott R, Lawrence P, Johar A, Brown G, Weinberg EG, et al. Autoantibodies to the high-affinity ige receptor in children with chronic urticaria. Ann Allergy Asthma Immunol. 2006;96(2):341–344. doi: 10.1016/s1081-1206(10)61245-8. [DOI] [PubMed] [Google Scholar]
- 8.Kohs TCL, Fallon ME, Oseas EC, Healy LD, Tucker EI, Gailani D, et al. Pharmacological targeting of coagulation factor xi attenuates experimental autoimmune encephalomyelitis in mice. Metab Brain Dis. 2023;38(7):2383–2391. doi: 10.1007/s11011-023-01251-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cossu D, Tomizawa Y, Momotani E, Yokoyama K, Hattori N. Adjuvant activity of mycobacterium paratuberculosis in enhancing the immunogenicity of autoantigens during experimental autoimmune encephalomyelitis. J Vis Exp. 2023;(195) doi: 10.3791/65422. [DOI] [PubMed] [Google Scholar]
- 10.Gremese E, Tolusso B, Bruno D, Alivernini S, Ferraccioli G. Infectious agents breaking the immunological tolerance: The holy grail in rheumatoid arthritis reconsidered. Autoimmun Rev. 2022;21(6):103102. doi: 10.1016/j.autrev.2022.103102. [DOI] [PubMed] [Google Scholar]
- 11.Cossu D, Mameli G, Galleri G, Cocco E, Masala S, Frau J, et al. Human interferon regulatory factor 5 homologous epitopes of epstein-barr virus and mycobacterium avium subsp. Paratuberculosis induce a specific humoral and cellular immune response in multiple sclerosis patients. Mult Scler. 2015;21(8):984–995. doi: 10.1177/1352458514557304. [DOI] [PubMed] [Google Scholar]