Abstract
Introduction
Forearm lacerations could lead to disastrous disabilities, nerve injuries led by the ulna nerve cause severe hand deformity and disfunction with little options to repair.
Case presentation
A young male suffered a distal ulna nerve injury and underwent multiple surgeries over two years. Zancolli-Lasso procedure was done, and major improvement was obtained.
Discussion
A comprehensive approach for claw hand is essential, supple mobile joints and the Bouvier maneuver are the most decisive factors, literature shows that the right procedure will work for the right patient.
Conclusion
The Zancolli procedure could be a simple viable treatment for a compliant patient who suffers from hand clawing and adapted to a weaker pinch.
Keywords: Claw hand, Zancolli, Ulna nerve, Deformity
Highlights
-
•
Overlook on forearm lacerations and peripheral upper limb nerve injuries.
-
•
A unique case of claw hand treated with Zancolli-lasso procedure.
-
•
Review of the literature for claw hand treatment outcomes and indications.
Abbreviations
- MCP
the metacarpophalangeal (MCP) joint
- PIP
The proximal interphalangeal joint
- DASH
the (Disability of Arm-Shoulder-Hand) score.
- ECRB
The extensor carpi radialis brevis
- ERCL
The extensor carpi radialis longus
- FDS
The flexor digitorum superficialis
1. Introduction
Traumatic forearm and wrist lacerations could lead to catastrophic injuries, severe morbidity, and loss of hand function. It is a relatively common occupational injury [1]. The outcomes are not predictable. While the wound's size does not correlate with the effect of disability, the injured structures could predict the disability's severity.
Vascular injuries are the most time-sensitive. However, they can be managed successfully even in complex situations [2]. Tendon injuries are rarely back to normal after being repaired, and usually suffer through rehabilitation and might be complicated with stiffness and tendon adhesiveness [3]. Peripheral nerve injuries are the worst. Primary repair is not predictable even in the simplest laceration, and secondary solutions like grafting, later deformities corrections, and tendon transfers, if applicable, do not give the best outcomes [4,5].
The hand is a unique anatomical, functional unit, not only the outstanding mechanics that work simultaneously to make the most precise movements, controlled by intrinsic and extrinsic muscles that have a unique balance between them, other than the sensitive proprioception function of the hand and looking to nerve injuries as an insult to all these factors might give a good idea of the less favorable outcome associated with it [6,7].
Three major nerves supply the hand. All of which contribute to sensory enervation of the hand. The radial nerve provides the extrinsic extensors. The median nerve gives most of the extrinsic flexors, and a minority of intrinsics of the hand, and the ulnar nerve supplies the ulnar flexors and the majority of intrinsics, including the three hypothenar muscles, the two medial lumbricals, the seven interossei, the adductor pollicis and the deep head of the flexor pollicis brevis [8]. In contrast, an isolated or combined insult to any of these nerves could lead to significant deterioration in hand function. The ulnar nerve is unique with proximal and distal injury patterns, and the distal injury, when chronic, leads to more disability, because of the intact ring and little fingers deep flexor's function and the loss of intrinsics, with characteristic claw hand deformity that could be severe. The exact pathology of clawing is the loss of muscle balance on the digits, as the diminished lumbricals can't flex the MCP and extend the PIP with pure domination of the more powerful flexors, which leads to persistent MCP hyperextension, this with the loss of adduction of the fingers and the thumb manifest in loss of grip strength and pinch and difficulty in performing precise movements [4,9].
Several treatment options are valid for fresh injuries of the ulnar nerve. Still, when the injury is chronic with a lack of reinnervation, the options are limited, physiotherapy is ineffective alone, and surgery is often necessary [9].
This article presents a case of a young male with chronic distal ulnar nerve dysfunction who was treated surgically with a Zancolli procedure. Significant functional improvement utilizing the DASH (Disability of Arm-Shoulder-Hand) score, and correction of the claw hand deformity were obtained.
The article has been reported by SCARE 2023 standards [10].
2. Case presentation
A 25-year-old male attended our clinic complaining of right-hand deformity and weakness of grip, struggling with daily activities, manual work, and numbness of the fourth and fifth digits. His DASH (Disability of Arm-Shoulder-Hand) score was 26.7 [11]. he was right handed, no comorbidities, nonsmoker college student, he mentioned a laceration injury to the distal medial palmar aspect of his forearm two years ago, he was taken to the emergency room of a local hospital where they explored the wound and found an injured flexor carpi ulnaris and a complete cut of the ulnar nerve, the ulnar artery was unharmed, so they did primary repair of the tendon and the nerve with no further details of the technical aspects of the operation, motion was protected with a splint for three weeks and physiotherapy was started afterwards, however the patient complaint of numbness of the two most medial fingers and grip weakness which did not seem to improve by the physiotherapy program, his doctor assured him and required him to stay patient until the passage of six months to see if any signs of reinnervations would occur, because that did not happen his doctor did an ulnar nerve decompression at the same location of initial injury and put the patient under observation, as no improvement were obtained, the patient sought the consultant of another doctor who asked for a nerve conduction study which showed no response of the injured ulnar nerve and supplied muscles, at this point the patient's hand was starting to develop clawing gradually with no marked progress and no response to physiotherapy, the doctor suggested exploration of the nerve and possible grafting with an autograft from the sural nerve, the patient underwent the procedure but for unknown reasons grafting was not done and the patient was assured that this time his injury would recover this time, however it did not, clawing progressed, and after that is when he presented to our clinic two years from the initial injury, on examination there was severe clawing of the hand maximize on the ring and little fingers, a scar on the distal palmar aspect of the forearm apparently from the previous operations, he was unable to fully extends the PIP of his injured fingers unless the MCP was flexed passively-Bouvier sign- [12], there was a mild weakness in pinch formation and adducting the fingers-(Froment sign was positive) Fig. 1, Vid 1.
Fig. 1.
Shows clinical image of the clawing deformity and the scar at the distal volar aspect of the forearm. A video is attached showing the clinical examination.
Fig. 1 shows clinical image of the clawing deformity and the scar at the distal volar aspect of the forearm.
Flexor carpi ulnaris scored [5], Flexor digitorium profundus of the fourth finger [5], Flexor digitorium profundus of the fourth finger [5], Adductor pollicis (0–5), first dorsal interossei (0–5) on Medical Research Council Manual Muscle Testing scale [13].
Thorough discussion was done with patient regarding his situation and treatment options, he was unable to tolerate the clawing of his hand but was adapted to the weakness of the pinch and grip formation, so we decided to go with Zancolli lasso procedure to correct the deformity and explained that procedure to the patient and the rehabilitation process and that it might correct clawing deformity and mildly improve the grip strength, after we obtained informed consent we operated the patient under general anesthesia applying a tourniquet on the upper arm, after disinfecting and draping the limp and inflation of the tourniquet a volar oblique incision was done on the level of the PIP of the fourth finger, and harvesting of the superficialis flexor of the digit was done, a transverse 5 cm incision was done at the distal palmar crease and dissection was done until reaching of the flexor tendons, and the harvested tendon was retracted to the proximal wound and divided into four tails Fig. 2, then dissection was done to reach the A1 pulleys of the digits and the splits of the donner tendon was passed and looped over the pulleys respectfully and sutured under tension with the MCP in 60 degrees of flexion, irrigation and closing the wounds was done, a short arm cast that extend to the fingers was applied for four weeks, after that removing of the cast was done, no wound healing problems was noticed, and a major correction of the clawing was observed, physiotherapy was initiated at this point with focusing on range of motion for two months, strengthening of the muscles was started at three months at the same time that precise hand movement and full grips formation was allowed, evaluation every other month was done with progressive improvement and patient satisfaction, the score was evaluated six months after the operation his DASH score is now 15 and The Patient Rated Wrist/Hand Evaluation is 27 of 100.
Fig. 2.
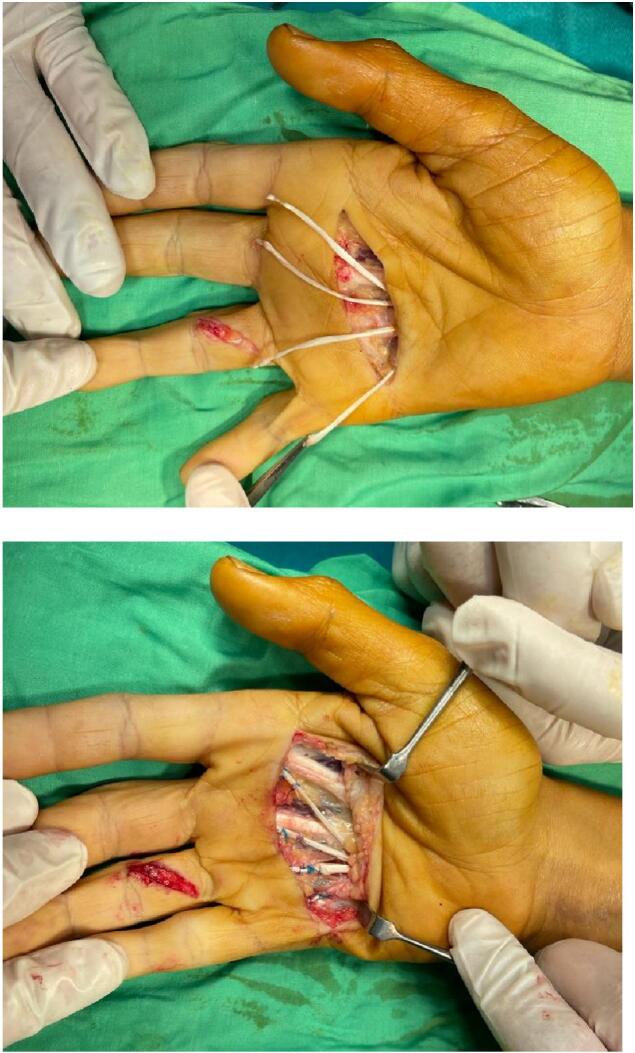
Shows the four tailed donor from the fourth FDS tendon before and after tenodesis to the A1 pulleys.
Fig. 2 shows the four-tailed donor from the fourth FDS tendon before and after tenodesis to the A1 pulleys.
3. Discussion
Chronic nerve deficiency is a complex disabling lesion that leaves the hand with cosmetic and functional impairments. The latter is undoubtedly far more important, as the hand is the most essential functional unit in the musculoskeletal system [6]. Wearing socks, tying a shoe, opening a door, writing ..etc. are all day-to-day activities that require a good range of motion of the digits, good muscles, grasp power, and the ability to oppose and adduct the thumb with sufficient pinch power, restoring these abilities is the mainstay of the desired outcome when dealing with such lesions if there were multiple nerve dysfunctions, a highly trained hand expert is required to obtain the most favorable outcomes, which even then could not always be obtained due to injury and patients related factors [14].
An orthopedic surgeon can successfully deal with a simpler isolated nerve dysfunction, though not necessarily easier; a favorable outcome is more obtainable.
The ulnar nerve of all nerves has a particular situation when it is not functioning, as the significant supplement of intrinsic muscles of the hand. Its injury leads to weakness or loss of all the main functions of the hand, weaker grip, weaker pinch, and difficulty in performing precise hand tasks, especially when the injury is distal to the enervation of the extrinsic hand muscles, a clawing hand deformity will develop causing cosmetic disability as well [15].
Acute ulnar nerve injuries could be repaired. However, the prognosis relies on injury-specific factors. When there is a material loss, primary end-to-end nerve fascicle repair is not viable. An autograft might be necessary, also, there have been other possible options, such as synthetic grafts… etc., but even then, full recovery is not guaranteed. Chronic insufficiency will develop [16,17].
Clawing deformity in variant severity is the mainstay of developed injuries; reconstruction of the impaired functions is the best treatment option. This decision is based on the severity of the deformity, the patient's needs, age, hand dominance, and occupational factors [18].
Loss of thumb adduction leads to weakness of pinch. When it is severe enough, transfer of the extensor carpi radialis brevis, FDS, extensor indicis proprius, abductor polices longus, or brachioradialis extended with a graft is viable to restore thumb adduction. Each surgical technique emphasizes the pulley used as it differs on whether the donor is an extensor or a flexor tendon [19].
When it comes to clawing, restoring the extrinsic and intrinsic muscles' functions is mandatory. Correcting only the intrinsic in a high ulnar injury will worsen deformity following the transfer [18].
In distal injuries, the Bouvier maneuver is crucial in building accurate decisions; if active PIP extension is regained when MCP hyperextension is prevented- the deformity is not fixed, and the extensor slip is intact- a static or dynamic procedure could be chosen, a static procedure is based on hyperextension prevention of the MCP which leads to restoring of PIP extension, it is either tenodesis or MCP volar capsule tightening, the advantage that it is a technically more straightforward working procedure. However, it might stretch with time [20].
A dynamic procedure uses a donor muscle to control MCP flexion. When the Bouvier maneuver is negative, restoring the lumbrical function with a transfer is further indicated to restore PIP extension.
The downsides of such a procedure are the demanding technique, the possibility of swan neck deformity development, and the inability to improve grip strength sufficiently.
Specific considerations must be taken based on the level of injury, as in high ulnar injuries, rings and small finger FDS are not viable donors [14].
In our case, the Bouvier maneuver was positive, and although there was a mild weakness of thumb adduction, it was not a major concern for the patient. He was unwilling to undergo a more invasive procedure, such as brachioradialis transfer, so we decided to go with the Zancolli-Lasso procedure. Based on the outcome we obtained, our decision was correct.
Zancolli- lasso procedure is a simple procedure; it is a modification of the original Zancolli, which is a capsulodesis of the volar MCP joints [21]. The modified technique is based on a split transfer of the fourth or the third fingers superficial flexor into the A1 pulley system -Zancolli recommends transferring each superficial flexor tendon of the digits- it was initially described in 1974 [22] And it was later supported in the literature as Hastings Hill et al. found in 1994 when he studied 12 patients that the Zancolli lasso procedure is an effective, simple procedure for isolated ulnar nerve palsy under the condition it is correctly indicated, the recommended however against it in the thick handed patients with strong, powerful grip requirements [23], and Gupta Vikas et al. found in 2015 when studying the outcomes of 20 patients suffering from a claw hand deformity that 15 obtained good results, and all patients showed increased grip strength six months after the surgery [24].
If the Bouvier maneuver was negative, we would have gone with the Stiles-Bunnell transfer, which is based on a split transfer of two flexor tendons into the lateral bands of the digits to restore PIP extension. It was first described in 1922 but popularized later by Bunnel, who modified the technique by vitalizing each finger's lateral bands with its own FDS. But later, it was found that it is too powerful a transfer that may cause swan neck deformity. Hence, a slit four tails single tendon transfer is the current standard method. However. The vital lesson of this technique is that when the Bouvier maneuver is negative, the lateral bands must be revitalized, regardless of what donor is used [25,26].
If the injury was a high ulnar nerve injury, we would have gone with additional supplementation by surgically synchronizing the profundus flexors with the superficial flexors of the ring and small fingers in the forearm [14].
A major part of the success of this operation is the postoperative period and rehabilitation afterward. We went with the most agreed-on protocol in the literature [27]. We applied a full cylinder cast in wrist flexion, MCP flexion, and PIP extension for three weeks. After that, we applied and handmade MCP extensor splint and allowed the passive motion of the digits for five weeks, then we started a gentle strengthening program for the intrinsic muscles of the hand that became more aggressive after an additional four weeks, precise hand movements and heavy objects lifting was prohibited for three months,
One of the treatment options was to transfer the ECRB/ECRL to the pulleys as a replacement for the FDS. However, the Zancolli technique is more straightforward and has a lower threshold to learn. Although both could be as effective, the technique popularized by Brand has the advantage of utilizing a strong extensor without affecting the power of wrist extension that much. The negatives are the extra incisions needed, the harder technique, and the risk of iatrogenic median nerve injury in case of transferring the ECRL through the carpal tunnel [28,29].
Another transfer that carries the same risk is the palmaris Longus transfer through the carpal tunnel. Although it might have similar functional outcomes to other dynamic transfers, palmaris does not exist in all humans, and the need for a tendon graft is the main downside of this treatment option [30].
In summary, the first step is electing the right patient based on his previous treatment plans and his needs, specifying the exact lesion and other possible concomitant pathologies, and choosing the correct procedure based on clinical examination. While static procedures have many downsides, they still have a role, and dynamic procedures can all correct the deformity, but improving the grip strength requires further complex techniques. The best one is the one that matches the patient's needs, available donors, and the surgeon's expertise, and don't forget to strive to restore digits adduction in case of significant weakness.
4. Conclusion
Zancolli procedure could be a simple viable treatment for a compliant patient who suffers from hand clawing and adapted to a weaker pinch.
The following is the supplementary data related to this article.
Video 1 shows the patient's inability to extend the fourth and fifth digits without preventing MCP hyperextension.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
This study is exempt from ethical approval in our institution.
Funding
This research did not receive any specific grant from any funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The author has no conflicts to disclose.
References
- 1.Sorock G.S., Lombardi D.A., Courtney T.K., Cotnam J.P., Mittleman M.A. Epidemiology of occupational acute traumatic hand injuries: a literature review. Saf. Sci. 2001 Aug;38(3):241–256. [Google Scholar]
- 2.Thai J., Pacheco J., Margolis D., Swartz T., Massey B., Guisto J., et al. Evidence-based comprehensive approach to forearm arterial laceration. Western Journal of Emergency Medicine. 2015 Dec 17;16(7):1127–1134. doi: 10.5811/westjem.2015.10.28327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taras J.S., Gray R.M., Culp R.W. Complications of flexor tendon injuries. Hand Clin. 1994 Feb;10(1):93–109. [PubMed] [Google Scholar]
- 4.Robinson L.R. Traumatic injury to peripheral nerves. Muscle Nerve. 2000 Jun;23(6):863–873. doi: 10.1002/(sici)1097-4598(200006)23:6<863::aid-mus4>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 5.Menorca R.M.G., Fussell T.S., Elfar J.C. Nerve physiology. Hand Clin. 2013 Aug;29(3):317–330. doi: 10.1016/j.hcl.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duncan S.F.M., Saracevic C.E., Kakinoki R. Biomechanics of the hand. Hand Clin. 2013 Nov;29(4):483–492. doi: 10.1016/j.hcl.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Moran CA. Anatomy of the hand. Phys. Ther. 1989 Dec 1;69(12):1007–13. [DOI] [PubMed]
- 8.Maw J., Wong K.Y., Gillespie P. Hand anatomy. Br. J. Hosp. Med. 2016 Mar 2;77(3):C34–C40. doi: 10.12968/hmed.2016.77.3.C34. [DOI] [PubMed] [Google Scholar]
- 9.Woo A., Bakri K., Moran S.L. Management of Ulnar Nerve Injuries. J. Hand Surg. Am. 2015 Jan;40(1):173–181. doi: 10.1016/j.jhsa.2014.04.038. [DOI] [PubMed] [Google Scholar]
- 10.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023 May;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Germann G., Wind G., Harth A. Der DASH-Fragebogen - Ein neues Instrument zur Beurteilung von Behandlungsergebnissen an der oberen Extremität. Handchirurgie Mikrochirurgie Plastische. Chirurgie. 1999 May;31(3):149–152. doi: 10.1055/s-1999-13902. [DOI] [PubMed] [Google Scholar]
- 12.Pai M, Bhardwaj P. Bouvier's Maneuver The Origin and Interpretation.
- 13.Williams M. Manual muscle testing, development and current use. Phys. Ther. 1956 Dec 1;36(12):797–805. [DOI] [PubMed]
- 14.Jones N.F., Machado G.R. Tendon transfers for radial, median, and ulnar nerve injuries: current surgical techniques. Clin. Plast. Surg. 2011 Oct;38(4):621–642. doi: 10.1016/j.cps.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Murovic J.A. Upper-extremity peripheral nerve injuries. Neurosurgery. 2009 Oct;65(4):A11–A17. doi: 10.1227/01.NEU.0000339130.90379.89. [DOI] [PubMed] [Google Scholar]
- 16.Vordemvenne T., Langer M., Ochman S., Raschke M., Schult M. Long-term results after primary microsurgical repair of ulnar and median nerve injuries. Clin. Neurol. Neurosurg. 2007 Apr;109(3):263–271. doi: 10.1016/j.clineuro.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 17.Dahlin L.B. Techniques of peripheral nerve repair. Scand. J. Surg. 2008 Dec 1;97(4):310–316. doi: 10.1177/145749690809700407. [DOI] [PubMed] [Google Scholar]
- 18.BRANDSMA JW, BRAND PW. Claw-finger correction. J. Hand Surg. 1992 Dec 29;17(6):615–21. [DOI] [PubMed]
- 19.Burkhalter W.E. Restoration of power grip in ulnar nerve paralysis. Orthop. Clin. North Am. 1974 Apr;5(2):289–303. [PubMed] [Google Scholar]
- 20.Sapienza A., Green S. Correction of the claw hand. Hand Clin. 2012 Feb;28(1):53–66. doi: 10.1016/j.hcl.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 21.ZANCOLLI EA. Claw-hand caused by paralysis of the intrinsic muscles: a simple surgical procedure for its correction. J. Bone Joint Surg. Am. 1957 Oct;39-A(5):1076–80. [PubMed]
- 22.Zancolli E. Correccion de la “garra” digital por paralysis intrinseca. La operacion del ‘lazo.’ Acta Ortop Latinoam. 1974;1(6):65–71.
- 23.Hastings H., McCollam S.M. Flexor digitorum superficialis lasso tendon transfer in isolated ulnar nerve palsy: a functional evaluation. J. Hand Surg. Am. 1994 Mar;19(2):275–280. doi: 10.1016/0363-5023(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 24.Gupta V., Consul A., Swamy M. Zancolli lasso procedure for correction of Paralytic claw hands. J. Orthop. Surg. 2015 Apr 1;23(1):15–18. doi: 10.1177/230949901502300104. [DOI] [PubMed] [Google Scholar]
- 25.Brand PW. PARALYTIC CLAW HAND. J. Bone Joint Surg. Br. 1958 Nov;40-B(4):618–32. [DOI] [PubMed]
- 26.LITTLER JW. Tendon transfers and arthrodeses in combined median and ulnar nerve paralysis. J. Bone Joint Surg. Am. 1949 Apr;31A(2):225–234. [PubMed] [Google Scholar]
- 27.Duff S.V., Humpl D. 6th edn. Elsevier Mosby; Philadelphia, PA: 2011. Therapist’s Management of Tendon Transfers. Rehabilitation of the Hand and Upper Extremity; p. 786. [Google Scholar]
- 28.Brand PW. PARALYTIC CLAW HAND. J. Bone Joint Surg. Br. 1958 Nov;40-B(4):618–32. [DOI] [PubMed]
- 29.Brand PW. TENDON GRAFTING. J. Bone Joint Surg. Br. 1961 Aug;43-B(3):444–53.
- 30.ANTIA NH. The palmaris longus Motor for Lumbrical Replacement. Hand. 1969 Apr 29;1(2):139–145. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1 shows the patient's inability to extend the fourth and fifth digits without preventing MCP hyperextension.



