Abstract
We report the case of a 38-year-old patient with an undocumented history of lung disease who presented with Kartagener's syndrome diagnosed on CT scan in the context of lupus erythematosus. Kartagener's syndrome is a distinct entity among primary ciliary dyskinesias, but its association with lupus has not been described in the literature.
Keywords: Kartagener's syndrome, Computed tomography, Lupus
Introduction
Kartagener's syndrome is a unique entity among primary ciliary dyskinesias (PCD), characterized by a triad: sinusitis, bronchiectasis, and complete or incomplete situs inversus [1]. It is a rare congenital disease with autosomal recessive inheritance, occurring in approximately 1 in 15,000 individuals [2]. Airway infections associated with this pathology typically manifest in childhood [2]. We report the case of a 38-year-old female patient with a history of pulmonary pathology, lupus and Kartagener syndrome diagnosed by CT scan.
Case report
The patient, a 38-year-old woman with a history of undocumented respiratory pathology, presented with productive cough and respiratory distress, necessitating a thoracic CT scan.
Clinical examination revealed a fever of 38°C, bronchial rales and skin lesions of lupus origin.
Biological investigations revealed leukopenia with a leukocyte count of 2000/µL and high antinuclear antibodies.
The thoracic CT revealed dextrocardia (Fig. 1) associated with cylindrical bronchiectasis (Fig. 2). Given these anomalies, an additional abdominal scan was performed, showing complete situs inversus with the liver on the left and the spleen on the right (Fig. 3). These findings led to the suspicion of Kartagener's syndrome, prompting a sinus CT scan, which confirmed pansinusitis (Fig. 4). The diagnosis of Kartagener's syndrome in the context of lupus was therefore made on the basis of the triad of bronchiectasis, situs inversus and sinusitis.
Fig. 1.
Coronal reconstruction of a thoracic CT scan demonstrating dextrocardia.
Fig. 2.
Cylindrical bronchiectasis on coronal reconstruction of a chest CT scan.
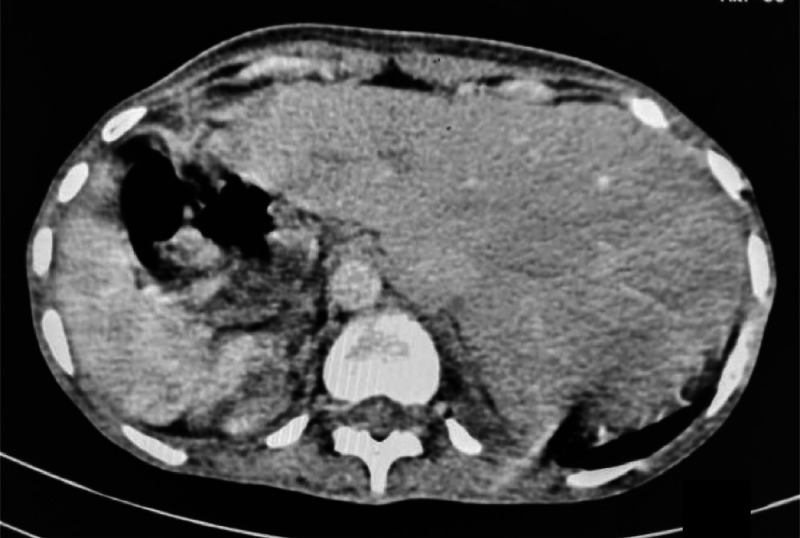
Fig. 3.
Axial slice of an abdominal CT scan showing a situs inversus with the liver on the left and the spleen on the right.
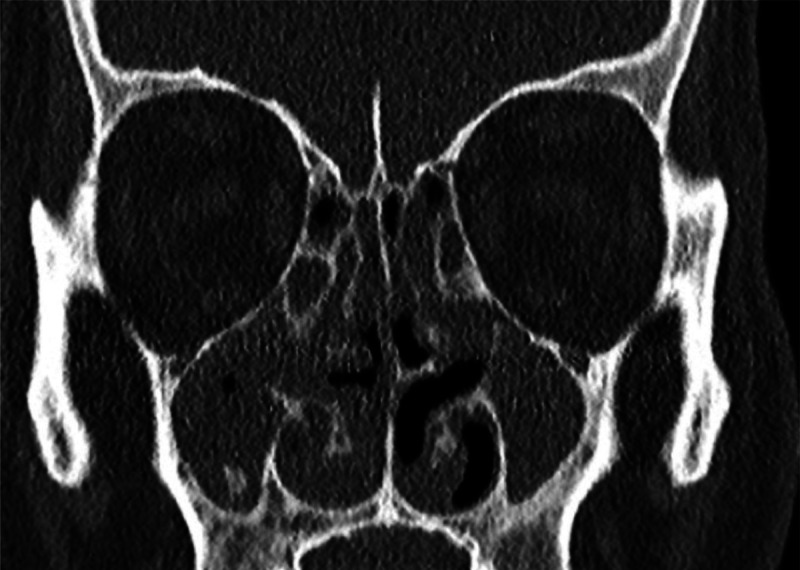
Fig. 4.
CT scan of the facial sinuses with coronal reconstruction showing polypoidal thickening of the mucosa of the facial sinuses.
Treatment consisted of respiratory physiotherapy, antibiotic therapy based on amoxicillin-clavulanic acid 1 g x 3/day and hydroxycloroquine 200 mg: 2 tablets/day.
Discussion
Kartagener's syndrome was first described by Manes Kartagener in 1935. The syndrome, named after him, includes chronic sinusitis, situs inversus, and bronchiectasis [3]. Kartagener's syndrome accounts for 50% of primary ciliary dyskinesias (PCD). It is a rare genetic disorder with autosomal recessive inheritance, although X-linked or dominant inheritance patterns have also been described [3]. It involves mutations in genes encoding dynein on chromosomes 5, 9, and 7, leading to morphological and/or functional ciliary anomalies [4]. The age at diagnosis varies, with the disease typically being identified in childhood [[5], [6], [7]]. In our case, the diagnosis was made at the age of 38. The clinical presentation of Kartagener's syndrome is dominated by respiratory symptoms beginning in childhood. These symptoms, present in all patients, are characterized by their chronicity and annual recurrence [1]. They include chronic bronchial congestion, daily productive cough with mucopurulent secretions, and phases of exacerbations and superinfections. Imaging, particularly thoraco-abdominal and sinus CT scans, is crucial for diagnosis, revealing the diagnostic triad of bronchiectasis, complete or incomplete situs inversus, and chronic sinusitis. The association between Kartagener syndrome and lupus has not been described in the literature, despite our searches in pub Med and Google scholar.
Comprehensive management of Kartagener's syndrome primarily involves bronchial drainage physiotherapy, antibiotics for superinfection, and appropriate vaccination against influenza and pneumococci [3,5].
Conclusion
Kartagener's syndrome is a rare congenital pathology with nonspecific clinical presentation. Imaging, particularly CT, is essential for diagnosis, as demonstrated in our patient. However, it is not known to be associated with lupus, according to the literature.
Patient consent
Written informed consent for the publication of this case report was obtained from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Prisca Gabrielle AE, Honjaniaina R, Christian T, Narindra Lova Hasina RNO, Ahmad A. Toux chronique révélant un syndrome de kartagener à propos d'un cas. J Func Vent Pulm. 2017;23(8):44–48. doi: 10.12699/jfvp.8.23.2017.44. [DOI] [Google Scholar]
- 2.Escudier E, Tamalet A, Prulière-Escabasse V, Roger G, Coste A. Dyskinésie ciliaire primitive. Revue Française d'Allergol et D'Immunol Clin. 2006;46(6):530–537. doi: 10.1016/j.allerg.2006.08.010. [DOI] [Google Scholar]
- 3.Ludovic M. Formes cliniques de la dyskinésie ciliaire primitive des bronches chez l'enfant: à propos de 13 observations. Thèse de Médecine Nancy (France) 2000;137:217. [Google Scholar] [Google Scholar]
- 4.Doumbia A, Koné Y, Koné A, Maïga O, Dembélé A. Syndrome de Kartagener de découverte fortuite au cours d'un bilan d'infécondité du couple à propos d'un cas. Pan Afr Med J. 21 août. 2019;33:316. doi: 10.11604/pamj.2019.33.316.16919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El Alaoui Abdelilah. Le syndrome de Kartagener: prototype de dyskinésie ciliaire primitive. Thèse de Médecine Maroc. 2014;182:127. [Google Scholar]
- 6.Melki B, Hamdi B, Berraies A, El Bey R, Ammar J, Hamzaoui A. Syndrome de kartagener: à propos de 6 cas. Revue Des Maladies Respirat. 2015 Jan;32(Supplément):A142–A2143. Doi : 10.1016/j.rmr.2014.10.081
- 7.Bemba E, Lee P, Odzili I, Franck A, Mongo N, Solange F, et al. Syndrome de Kartagener chez une adolescente. J Fran Viet Pneu. 2015;18(6):1–60. doi: 10.12699/jfvp.6.18.2015.33. [DOI] [Google Scholar]