Abstract
Aims
Distal femoral osteotomies (DFOs) are commonly used for the correction of valgus deformities and lateral compartment osteoarthritis. However, the impact of a DFO on subsequent total knee arthroplasty (TKA) function remains a subject of debate. Therefore, the purpose of this study was to determine the effect of a unilateral DFO on subsequent TKA function in patients with bilateral TKAs, using the contralateral knee as a self-matched control group.
Methods
The inclusion criteria consisted of patients who underwent simultaneous or staged bilateral TKA after prior unilateral DFO between 1972 and 2023. The type of osteotomy performed, osteotomy hardware fixation, implanted TKA components, and revision rates were recorded. Postoperative outcomes including the Forgotten Joint Score-12 (FJS-12), Tegner Activity Scale score, and subjective knee preference were also obtained at final follow-up.
Results
A total of 21 patients underwent bilateral TKA following unilateral DFO and were followed for a mean of 31.5 years (SD 11.1; 20.2 to 74.2) after DFO. The mean time from DFO to TKA conversion was 13.1 years (SD 9.7) with 13 (61.9%) of DFO knees converting to TKA more than ten years after DFO. There was no difference in arthroplasty implant systems employed in both the DFO-TKA and TKA-only knees (p > 0.999). At final follow-up, the mean FJS-12 of the DFO-TKA knee was 62.7 (SD 36.6), while for the TKA-only knee it was 65.6 (SD 34.7) (p = 0.328). In all, 80% of patients had no subjective knee preference or preferred their DFO-TKA knee. Three DFO-TKA knees and two TKA-only knees underwent subsequent revision following index arthroplasty at a mean of 12.8 years (SD 6.9) and 8.5 years (SD 3.8), respectively (p > 0.999).
Conclusion
In this self-matched study, DFOs did not affect subsequent TKA function as clinical outcomes, subjective knee preference, and revision rates were similar in both the DFO-TKA and TKA-only knees at mean 32-year follow-up.
Cite this article: Bone Jt Open 2024;5(11):1013–1019.
Keywords: Distal femoral osteotomy, Total knee arthroplasty, Bilateral total knee arthroplasties, DFO, Osteotomy, total knee arthroplasty (TKA), distal femoral osteotomy, knees, Osteotomies, clinical outcomes, bilateral TKAs, Forgotten Joint Score, arthroplasty implant, valgus deformities, arthroplasty
Introduction
Limb mechanical malalignment significantly impacts the distribution of loading forces on cartilage and subchondral bone within the knee, potentially exacerbating the progression of unilateral osteoarthritis in the setting of coronal deformity. In younger patients, unicompartmental osteoarthritis can pose a challenging problem as treatment with total knee arthroplasty (TKA) has been shown to result in inferior outcomes and increased rates of complications and revisions.1,2 Osteotomies performed around the knee help to address these issues and play a pivotal role in redistributing compartmental loads. These not only provide pain relief but also hold the potential to delay or even avoid the need for a TKA.3,4
Distal femoral osteotomies (DFOs) are typically used for correction of valgus deformities to offload the lateral compartment of the knee.5,6 Prior studies have demonstrated long-term joint preservation and favourable clinical outcomes after DFO.7,8 Although DFOs are joint-preserving techniques, many patients are expected to progress in terms of degenerative disease and ultimately undergo TKA. For example, Sternheim et al9 reported a 90% survival rate at ten years post-DFO, while at 20 years this decreased to 22%. Therefore, it is important to carefully weigh the advantages of joint-preserving techniques, such as a DFO, against their potential implications on the outcomes of subsequent procedures.
To date, there have been few studies reporting outcomes of TKA after prior DFO. Most studies have a limited number of patients without control groups.10-12 Therefore, the purpose of this study was to determine the effect of a unilateral DFO on subsequent TKA function in patients with bilateral TKAs, using the contralateral knee as a self-matched control group. We hypothesized that patients would demonstrate similar outcomes, implants used, and revision rates when comparing patients’ DFO-TKA knee with their contralateral TKA-only knee.
Methods
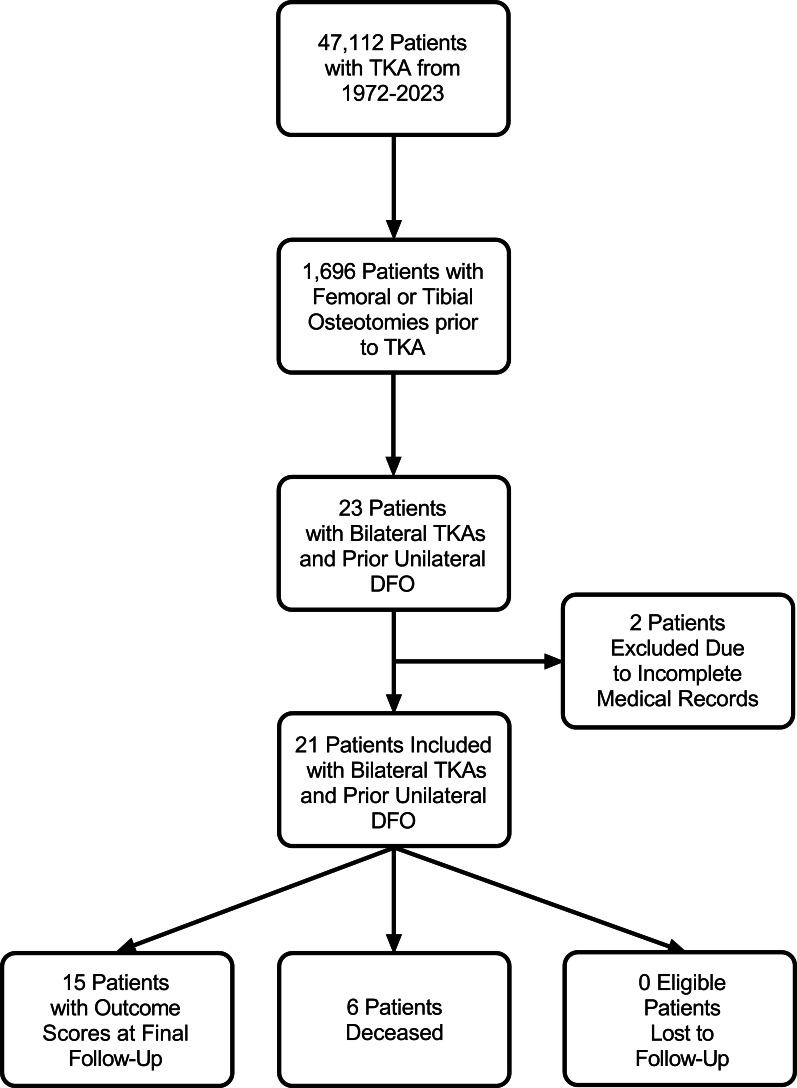
All patients who underwent TKA at a single academic institution from 1972 to 2023 were reviewed following approval from our Institutional Review Board (Mayo Clinic IRB #15-000601). Inclusion criteria consisted of patients who underwent simultaneous or staged bilateral TKA after prior unilateral DFO. A total of 21 patients were included in this study (Figure 1). Two patients were excluded due to incomplete medical records, resulting in an overall follow-up rate of 91.3% (21/23).
Fig. 1.
Patient screening and enrollment based on inclusion criteria. DFO, distal femoral osteotomy; TKA, total knee arthroplasty.
Clinical and demographic data were obtained from the Mayo Clinic Total Joint Registry.13 This registry prospectively records demographics, operative data, and postoperative complications.13 Patients underwent DFO from 1946 to 2001 with 85.7% (18/21) being performed at Mayo Clinic and 14.3% (3/21) being performed at outside institutions. All primary DFO-TKAs were performed at the Mayo Clinic from 1990 to 2010. Overall, 78% (19/21) of the TKAs without prior osteotomy were performed at the Mayo Clinic from 1976 to 2017, while 9.5% (2/21) were performed at outside institutions during 1996 and 2003. The type of osteotomy performed (opening- vs closing-wedge), osteotomy hardware fixation (plate and screws vs staples), when and if osteotomy hardware was removed, implanted TKA components (presence of femoral and tibial stems, implant constraint, polyethylene thickness), and revision rates were recorded. Postoperative outcomes including Forgotten Joint Score-12 (FJS-12),14 Tegner Activity Scale score,15 and subjective knee preference were also obtained. Subjective knee preference was acquired by asking, “Which knee would you consider to be the better knee?”
Statistical analysis
Data were extracted with continuous variables being reported as mean (SD), while categorical variables were reported as frequencies with percentages. Median values were also reported for time from DFO to DFO-TKA, DFO-TKA to final follow-up, TKA-only to final follow-up, and DFO to final follow-up. Differences between continuous variables were evaluated using a paired t-test. Differences between categorical variables were evaluated using a χ2 (chi-squared test) test. A post-hoc power analysis was performed using G*Power version 3.1 (Heinrich-Heine-Universtät, Germany).16 The achieved power was 0.829 and 0.901 for detecting a statistical difference with an effect size of 0.55 when using a paired t-test and chi-squared test, respectively. Kaplan-Meier curves were used to evaluate the probability of survival from DFO to TKA and from TKA to revision surgery. All data were analyzed using R statistical software v. 4.3.1 (R Foundation for Statistical Computing, Austria). A p-value < 0.05 was considered statistically significant.
Results
The overall mean follow-up of the study (initial DFO to final follow-up) was 31.5 years (SD 11.1) (median 29.7 years; IQR 26.6 to 32.6) (Figure 2). The mean age at the time of DFO was 47.8 years (SD 8.7), with 52.4% of patients (11/21) being female. All DFOs were performed for correction of valgus deformity. Medial closing-wedge osteotomies were performed a majority of the time (71.4%, 15/21) in comparison to lateral opening-wedge osteotomies (28.6%, 6/21). Plate and screws were most commonly used for DFO fixation (85.7%, 18/21) while staples were used only 14.3% (3/21) of the time (Table I). Excluding hardware removal, no patients underwent revision after DFO.
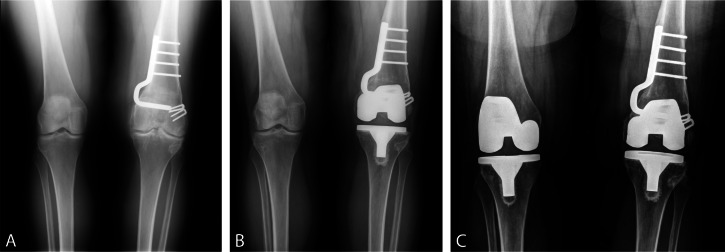
Fig. 2.
Anteroposterior radiographs of a 48-year-old female with a) a valgus deformity of the left knee treated with a medial closing-wedge distal femoral osteotomy with plate and screws and a staple for femoral fixation. b) Subsequently after 15.2 years, the left knee underwent conversion to total knee arthroplasty (TKA). c) Finally, the right knee, without any prior knee osteotomy, underwent primary TKA 10.4 years after prior contralateral TKA.
Table I.
Patient demographics and distal femoral osteotomy characteristics.
| Variable | Data |
|---|---|
| Mean age, yrs (SD) | |
| DFO | 45.8 (10.8) |
| TKA following DFO | 58.9 (9.7) |
| Contralateral TKA | 60.4 (8.4) |
| Sex, n (%) | |
| Female | 11 (52.4) |
| Male | 10 (47.6) |
| DFO laterality, n (%) | |
| Left | 7 (33.3) |
| Right | 14 (66.7) |
| Osteotomy performed, n (%) | |
| Lateral opening-wedge | 5 (23.8) |
| Medial closing-wedge | 16 (76.2) |
| Osteotomy fixation, n (%) | |
| Plate and screws | 17 (81.0) |
| Staples | 3 (14.3) |
| Both | 1 (4.8) |
DFO, distal femoral osteotomy; TKA, total knee arthroplasty.
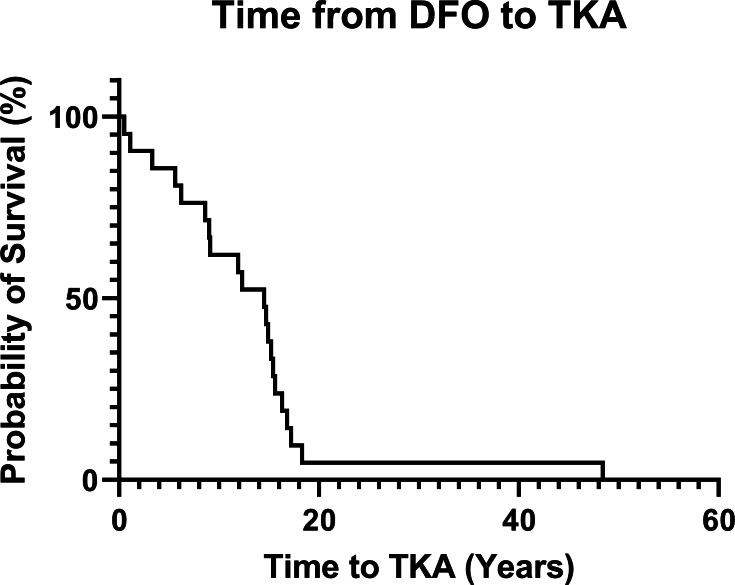
The mean time from DFO to TKA conversion was 13.1 years (SD 9.7) (median 14.5 years, IQR 8.6 to 15.6), with 13/21 patients (61.9%) of patients converting to TKA more than ten years after DFO (Figure 3). Patients had similar age at the time of their bilateral arthroplasties, with a mean age of 58.9 years (SD 9.7) at the time of DFO-TKA and 60.4 years (SD 8.4) for the contralateral TKA-only side (p = 0.287). A total of four of 21 patients (19%) underwent simultaneous bilateral TKA. Overall, five of 21 patients (24%) did not undergo hardware removal, while three (14.3%) underwent hardware removal prior to TKA. Furthermore, ten of 21 patients (48%) had their DFO hardware completely removed at the time of TKA, while three (14.3%) had partial removal of hardware at the time of TKA. In all, five of 21 patients (24%) with DFO-TKA knees had stemmed femoral components in comparison to two of 21 patients (9.5%) for the TKA-only knee (p = 0.408, chi-squared test). Overall, two of 21 patients (10%) with DFO-TKA knees had a stemmed tibial component, while no TKA-only knees had a stemmed tibial component (p = 0.469). In addition, 20 of the 21 DFO-TKA knees (95%) and all the TKA-only knees employed posterior-stabilized implant systems (p > 0.999, chi-squared test). The mean polyethylene insert for DFO-TKA knees was 13.5 mm (SD 3.9), while for TKA-only knees it was 11.9 mm (SD 2.8) (p = 0.032, paired t-test) (Table II).
Fig. 3.
Kaplan-Meier curve showing probability of survival after distal femoral osteotomy prior to total knee arthroplasty conversion. DFO, distal femoral osteotomy; TKA, total knee arthroplasty.
Table II.
Hardware removal and components used at the time of distal femoral osteotomy and total knee arthroplasty, and contralateral total knee arthroplasty.
| Variable | DFO-TKA | Contralateral TKA | p-value |
|---|---|---|---|
| DFO hardware removal, n (%) | N/A | N/A | |
| Prior to TKA | 3 (14.3) | ||
| Complete removal at time of TKA | 10 (47.6) | ||
| Partial removal at time of TKA | 3 (14.3) | ||
| None | 5 (23.8) | ||
| Stemmed femoral component, n (%) | 0.408* | ||
| Yes | 5 (23.8) | 2 (9.5) | |
| No | 16 (76.2) | 19 (90.5) | |
| Stemmed tibial component, n (%) | 0.469* | ||
| Yes | 2 (9.5) | 0 (0.0) | |
| No | 19 (90.5) | 21 (100.0) | |
| TKA implant constraint, n (%) | > 0.999* | ||
| Posterior-stabilized | 20 (95.6) | 21 (91.3) | |
| Varus-valgus | 1 (4.3) | 0 (0.0) | |
| Mean polyethylene insert, mm (SD) | 13.5 (3.9) | 11.9 (2.8) | 0.032†‡ |
Chi-squared test.
Paired t-test.
Statistical significance.
DFO, distal femoral osteotomy; N/A, not applicable; TKA, total knee arthroplasty.
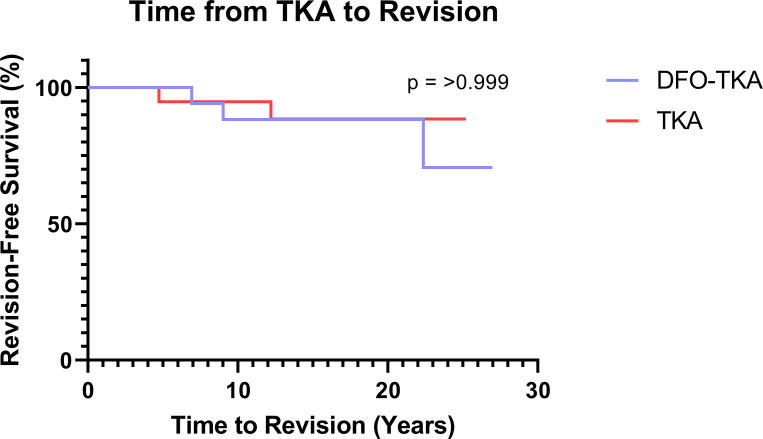
The mean follow-up after DFO-TKA was 18.5 years (SD 6.6) (median 19.1 years, IQR 15.8 to 22.5), while the mean follow-up after the contralateral TKA was 16.8 years (SD 6.0) (median 17.9 years, IQR 13.7 to 20.7). Six patients were deceased at the time of final follow-up. Postoperative outcome scores were obtained from the remaining 15 patients who were eligible for follow-up. The mean FJS-12 of the DFO-TKA knee was 62.7 (SD 36.6), while for the TKA-only knee it was 65.6 (SD 34.7) (p = 0.328, paired t-test). The mean Tegner Activity Scale score was 2.8 (SD 1.5). Ten patients (66.7%) had no subjective knee preference and rated both knees as being the same in terms of pain and function, two (13.3%) preferred their DFO-TKA knee, and three (20.0%) preferred their TKA-only knee. Three DFO-TKA knees (14.3%) underwent subsequent revision after their primary TKA: one for mid-flexion instability at 6.9 years during which the patient was also converted to a varus-valgus constraint insert, one for polyethylene wear and femoral periarticular osteolysis at 22.4 years, and one for patellar component loosening at nine years. Two TKA-only knees (9.5%) underwent subsequent revision: one for aseptic tibial component loosening at 4.7 years and the other for polyethylene wear at 12.2 years. There was no significant difference in revision rates between the DFO-TKA and TKA-only knees (p > 0.999) (Figure 4).
Fig. 4.
Kaplan-Meier curve showing probability of survival from revision surgery after primary total knee arthroplasty. DFO, distal femoral osteotomy; TKA, total knee arthroplasty.
Discussion
This self-matched cohort study followed patients who underwent unilateral DFO and subsequently bilateral TKA at a mean overall follow-up of 31.5 years. The main findings were that DFO effectively delayed conversion to TKA at a mean of 13.1 years. Additionally, prior DFO did not affect postoperative TKA outcomes as both the DFO-TKA and TKA-only knees had comparable FJS-12 scores (p = 0.328), and 80.0% of patients either had no subjective knee preference or preferred their DFO-TKA knee. Similarly, there was no difference in the revision rates of both the DFO-TKA and TKA-only knees (p > 0.999).
Previous studies have similarly demonstrated favourable clinical outcomes and long-term success of DFO in joint preservation. For example, Sternheim et al7 and Shivji et al9 demonstrated a ten-year survival rate after DFO of 90% and 89%, respectively. A separate study showed significant preoperative to postoperative improvements across multiple outcome scores after DFO with no patients undergoing TKA conversion at a mean follow-up of 7.1 years (2 to 14.2).17 Notably, no significant difference in outcomes or TKA conversion were seen based on surgical technique (opening- vs closing-wedge DFO).8 The most commonly reported complication after DFO is hardware removal;8,18 however, only three patients (14.3%) in our current study underwent hardware removal prior to TKA conversion.
Although the literature is limited, a few notable studies have demonstrated favourable clinical outcomes after DFO-TKA. Only one study performed a similar matched analysis comparing outcomes of patients who underwent DFO-TKA to a matched control group who underwent primary TKA without prior osteotomy. The authors found that at a median follow-up of 42 months there was no significant difference in postoperative outcome scores. However, there was significantly more lateral intraoperative laxity, intraoperative complications, and need for screw support in the tibial component due to severe lower limb deformity.19 While this prior study was limited by follow-up, ours demonstrated comparable clinical outcomes between both knees at a minimum of 20.2 years after DFO-TKA. Additionally, while this study performed a matched analysis based on a limited number of variables, our study is novel in that the patients were able to serve as their own controls, eliminating confounding from comorbidities and other variables. Chalmers et al12 examined 29 patients who underwent DFO-TKA and found that Knee Society Scores significantly improved preoperatively to postoperatively with a ten-year survival of 88%, however this study lacked a control group. Notably, Hevesi et al20 performed a similar self-matched cohort study with patients who underwent bilateral TKAs after prior unilateral proximal tibial osteotomy (PTO). The authors demonstrated comparable results to our current study, with no significant differences in clinical outcomes between knees and 81% of patients having either no subjective knee preference or preferring their PTO-TKA knee. In contrast, a prior case series found that patients who underwent DFO-TKA had inferior results compared to patients who underwent TKA without a prior DFO.10 However, this study included fewer than ten patients, and the surgical techniques and preoperative planning for DFOs have advanced considerably since this study was published over 20 years ago.10,21
The impact of a prior DFO on the type of arthroplasty implant system was statistically non-significant, as over 95.0% of both the DFO-TKA and TKA-only knees in our current study received posterior-stabilized implants. However, it is important to note that the polyethylene insert size was significantly larger for the DFO-TKA knees. As mentioned previously, Hevesi et al’s20 self-matched cohort comparing PFO-TKA and TKA-only knees similarly reported a significant larger polyethylene insert size in the PFO-TKA knees with no difference observed in the implant systems used between both knees. Chalmers et al12 and Kosashvili et al22 also demonstrated that most knees were stable intraoperatively with posterior-stabilized components. However, both studies reported that over 15% of knees required either femoral or tibial stemmed components, similar to our cohort with 23.8% of DFO-TKA knees employing a femoral stem.
While DFO-TKA knees exhibit comparable clinical outcomes and arthroplasty implant systems, they can present a considerably greater challenge surgically. For example, a prior DFO may result in substantially more bone loss, altered joint line, and difficult exposure due to scarring, which can increase the risk of resultant instability, limb malalignment, and patellar maltracking.23,24 A prior study found that it was challenging to balance the DFO knee in 13% of patients who underwent primary TKA, with these patients instead requiring a varus-valgus constraint.12 Nelson et al10 reported that in order to create a neutral mechanical axis in DFO knees undergoing primary TKA, that more resection of bone was necessary from the distal aspect of the lateral femoral condyle in relation to the distal aspect of the medial femoral condyle, which is the opposite of typical surgical preparation for a primary TKA. However, with the advent of navigation and robotic platforms, it may be easier to avoid hardware removal and achieve kinematic alignment.25,26
The present study is not without limitations. While our study had a mean follow-up of 32 years following DFO, we do remain limited by the small sample size. However, DFOs are uncommon procedures, and it is exceedingly rare for patients to subsequently undergo bilateral TKAs with extended follow-up.27 Additionally, post-hoc power analysis demonstrated that the study was adequately powered to detect statistical differences between both knees. Six patients were deceased at final follow-up, limiting conclusions drawn from postoperative outcome scores. Nevertheless, this suggests that comparable DFO-TKA and TKA-only outcomes are commonly observed for the life of the implant and the patient. Our institution serves as a tertiary referral centre, with approximately 2,500 TKAs being performed annually by surgeons with substantial technical expertise for complex primary TKAs.20 Thus, it is likely that well-experienced surgeons played a vital role in the outcomes observed. Finally, our results are susceptible to the biases inherent to retrospective reviews including not identifying all eligible patients, incomplete recordkeeping, and the inability to determine surgeons’ implant constraint algorithm and alignment strategy.
In conclusion, in this self-matched study, DFOs did not affect subsequent TKA function as clinical outcomes, subjective knee preference, and revision rates were similar in both the DFO-TKA and TKA-only knees at mean 32-year follow-up.
Take home message
- Patients undergoing distal femoral osteotomy followed by eventual total knee arthroplasty may expect similar clinical outcomes, subjective knee preference, and revision rates to primary knee arthroplasty without prior osteotomy.
- These findings are clinically relevant in that they support distal femoral osteotomy for the treatment of knee malalignment without compromising future arthroplasty clinical outcome.
Author contributions
S. C. Clark: Data curation, Formal analysis, Methodology, Writing – original draft
X. Pan: Data curation, Formal analysis, Writing – original draft
D. B. F. Saris: Conceptualization, Supervision, Writing – review & editing
M. J. Taunton: Conceptualization, Supervision, Writing – review & editing
A. J. Krych: Conceptualization, Supervision, Writing – review & editing
M. Hevesi: Conceptualization, Project administration, Supervision, Writing – review & editing
Funding statement
The authors disclose receipt of the following financial or material support for the research, authorship, and/or publication of this article: Support from the Foderaro-Quattrone Musculoskeletal-Orthopaedic Surgery Research Innovation Fund.
ICMJE COI statement
M. Hevesi reports a consulting fee from Vericel; and payment for educational events from Smith & Nephew, Arthrex, Medwest Associates, and Foundation Medical, all of which are unrelated to this work. A. J. Krych discloses royalties from and being a paid consultant for Arthrex; and having a leadership, fiduciary, or board role for the American Journal of Sports Medicine, Arthroscopy Association of North America, International Cartilage Repair Society, and Springer, all of which are unrelated to this paper. D. B. F. Saris declares being a paid consultant for Phoenix Kinetic and Relive Biotechnologies; and having a leadership, fiduciary, or board role for the American Academy of Orthopaedic Surgeons (AAOS), the Institute of Corporate Responsibility and Sustainability, and Cartilage, all of which are also unrelated. M. J. Taunton reports receiving royalties and consulting fees from Enovis; receiving publishing royalties from the Journal of Arthroplasty; and having a leadership, fiduciary, or board role for AAOS and the Journal of Arthroplasty, all of which are unrelated to this work.
Data sharing
The datasets generated and analyzed in the current study are not publicly available due to data protection regulations. Access to data is limited to the researchers who have obtained permission for data processing. Further inquiries can be made to the corresponding author.
Ethical review statement
Study approved via Institutional Review Board (Mayo Clinic IRB# 15-000601).
Open access funding
The open access fee for this paper was funded by Mayo Clinic, Rochester, Minnesota, USA.
© 2024 Clark et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Contributor Information
Sean C. Clark, Email: clarsc9@gmail.com.
Xuankang Pan, Email: pan.xuankang@mayo.edu.
Daniel B. F. Saris, Email: saris.daniel@mayo.edu.
Michael J. Taunton, Email: taunton.michael@mayo.edu.
Aaron J. Krych, Email: krych.aaron@mayo.edu.
Mario Hevesi, Email: hevesi.mario@mayo.edu.
Data Availability
The datasets generated and analyzed in the current study are not publicly available due to data protection regulations. Access to data is limited to the researchers who have obtained permission for data processing. Further inquiries can be made to the corresponding author.
References
- 1. Walker-Santiago R, Tegethoff JD, Ralston WM, Keeney JA. Revision total knee arthroplasty in young patients: higher early reoperation and rerevision. J Arthroplasty. 2021;36(2):653–656. doi: 10.1016/j.arth.2020.08.052. [DOI] [PubMed] [Google Scholar]
- 2. Ayers DC, Yousef M, Yang W, Zheng H. Age-related differences in pain, function, and quality of life following primary total knee arthroplasty: results from a FORCE-TJR (Function and Outcomes Research for Comparative Effectiveness in Total Joint Replacement) cohort. J Arthroplasty. 2023;38(7 Suppl 2):S169–S176. doi: 10.1016/j.arth.2023.04.005. [DOI] [PubMed] [Google Scholar]
- 3. Peng H, Ou A, Huang X, et al. Osteotomy around the knee: the surgical treatment of osteoarthritis. Orthop Surg. 2021;13(5):1465–1473. doi: 10.1111/os.13021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Capella M, Sabatini L, Bosco F, et al. A novel geometrical planning method to restore knee joint obliquity in double-level osteotomies. Arch Orthop Trauma Surg. 2023;143(11):6685–6693. doi: 10.1007/s00402-023-04997-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ismailidis P, Schmid C, Werner J, et al. Distal femoral osteotomy for the valgus knee: indications, complications, clinical and radiological outcome. Arch Orthop Trauma Surg. 2023;143(10):6147–6157. doi: 10.1007/s00402-023-04923-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fürmetz J, Patzler S, Wolf F, et al. Tibial and femoral osteotomies in varus deformities - radiological and clinical outcome. BMC Musculoskelet Disord. 2020;21(1):201. doi: 10.1186/s12891-020-03232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shivji FS, Foster A, Risebury MJ, Wilson AJ, Yasen SK. Ten-year survival rate of 89% after distal femoral osteotomy surgery for lateral compartment osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2021;29(2):594–599. doi: 10.1007/s00167-020-05988-5. [DOI] [PubMed] [Google Scholar]
- 8. Diaz CC, Lavoie-Gagne OZ, Knapik DM, Korrapati A, Chahla J, Forsythe B. Outcomes of distal femoral osteotomy for valgus malalignment: a systematic review and meta-analysis of closing wedge versus opening wedge techniques. Am J Sports Med. 2023;51(3):798–811. doi: 10.1177/03635465211051740. [DOI] [PubMed] [Google Scholar]
- 9. Sternheim A, Garbedian S, Backstein D. Distal femoral varus osteotomy: unloading the lateral compartment: long-term follow-up of 45 medial closing wedge osteotomies. Orthopedics. 2011;34(9):e488–90. doi: 10.3928/01477447-20110714-37. [DOI] [PubMed] [Google Scholar]
- 10. Nelson CL, Saleh KJ, Kassim RA, et al. Total knee arthroplasty after varus osteotomy of the distal part of the femur. J Bone Joint Surg Am. 2003;85-A(6):1062–1065. doi: 10.2106/00004623-200306000-00012. [DOI] [PubMed] [Google Scholar]
- 11. Cameron HU, Park YS. Total knee replacement after supracondylar femoral osteotomy. Am J Knee Surg. 1997;10(2):70–71. [PubMed] [Google Scholar]
- 12. Chalmers BP, Limberg AK, Athey AG, Perry KI, Pagnano MW, Abdel MP. Total knee arthroplasty after distal femoral osteotomy long-term survivorship and clinical outcomes. Bone Joint J. 2019;101-B(6):660–666. doi: 10.1302/0301-620X.101B6.BJJ-2018-1334.R2. [DOI] [PubMed] [Google Scholar]
- 13. Berry DJ, Kessler M, Morrey BF. Maintaining a hip registry for 25 years. Clin Orthop Relat Res. 1997;344(344):61. doi: 10.1097/00003086-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 14. Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty. 2012;27(3):430–436. doi: 10.1016/j.arth.2011.06.035. [DOI] [PubMed] [Google Scholar]
- 15. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 16. Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 17. Haunschild ED, Gilat R, Aghogho E, et al. Functional outcomes and survivorship of distal femoral osteotomy with cartilage restoration of the knee. J Cartilage Joint Preservation. 2021;1(1):100004. doi: 10.1016/j.jcjp.2021.100004. [DOI] [Google Scholar]
- 18. Chahla J, Mitchell JJ, Liechti DJ, et al. Opening- and closing-wedge distal femoral osteotomy: a systematic review of outcomes for isolated lateral compartment osteoarthritis. Orthop J Sports Med. 2016;4(6):2325967116649901. doi: 10.1177/2325967116649901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gaillard R, Lording T, Lustig S, Servien E, Neyret P. Total knee arthroplasty after varus distal femoral osteotomy vs native knee: similar results in a case control study. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3522–3529. doi: 10.1007/s00167-017-4487-9. [DOI] [PubMed] [Google Scholar]
- 20. Hevesi M, Wilbur RR, Keyt LK, et al. Total knee arthroplasty function at 25 years following proximal tibial osteotomy: paired outcomes of bilateral TKAs following unilateral osteotomy. J Bone Joint Surg Am. 2022;104-A(6):552–558. doi: 10.2106/JBJS.21.00761. [DOI] [PubMed] [Google Scholar]
- 21. Gao L, Madry H, Chugaev DV, et al. Advances in modern osteotomies around the knee. J Exp Ortop. 2019;6(1):9. doi: 10.1186/s40634-019-0177-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kosashvili Y, Gross AE, Zywiel MG, Safir O, Lakstein D, Backstein D. Total knee arthroplasty after failed distal femoral varus osteotomy using selectively stemmed posterior stabilized components. J Arthroplasty. 2011;26(5):738–743. doi: 10.1016/j.arth.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 23. Windsor RE, Insall JN, Vince KG. Technical considerations of total knee arthroplasty after proximal tibial osteotomy. J Bone Joint Surg Am. 1988;70-A(4):547–555. [PubMed] [Google Scholar]
- 24. Seo S-S, Nha K-W, Kim T-Y, Shin Y-S. Survival of total knee arthroplasty after high tibial osteotomy versus primary total knee arthroplasty: a meta-analysis. Medicine (Baltimore) 2019;98(30):e16609. doi: 10.1097/MD.0000000000016609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Siddiqi A, Horan T, Molloy RM, Bloomfield MR, Patel PD, Piuzzi NS. A clinical review of robotic navigation in total knee arthroplasty: historical systems to modern design. EFORT Open Rev. 2021;6(4):252–269. doi: 10.1302/2058-5241.6.200071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shah SM. After 25 years of computer-navigated total knee arthroplasty, where do we stand today? Arthroplasty. 2021;3(1):41. doi: 10.1186/s42836-021-00100-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rosso F, Margheritini F. Distal femoral osteotomy. Curr Rev Musculoskelet Med. 2014;7(4):302–311. doi: 10.1007/s12178-014-9233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed in the current study are not publicly available due to data protection regulations. Access to data is limited to the researchers who have obtained permission for data processing. Further inquiries can be made to the corresponding author.