Abstract
Background
Tai Chi and Baduanjin are nonpharmacological interventions that are widely applied among cancer patients.
Objective
This meta-analysis aimed to assess the effect of Tai Chi and Baduanjin on breast cancer patients by summarizing and pooling the results of previous studies.
Methods
The PubMed, Embase, Web of Science, Scopus and Cochrane Library and several databases were searched up to December 1, 2023, to identify high-quality RCTs. Relevant terms such as Tai Chi and Baduanjin were used as keywords. Stata 15.0 software and Review Manager (version 5.3; Cochrane Training) were used to screen the studies, extract the data, code the data, and perform the meta-analysis. The mean differences (MDs) and standardized mean differences (SMDs) with 95% CIs were used to calculate continuous variables. The Cochrane risk of bias assessment tool was used to evaluate the risk of bias. The PICOS framework was used to develop the following eligibility criteria: (i) population - breast cancer patients; (ii) intervention - Tai Chi and Baduanjin intervention; (iii) comparison - Tai Chi and Baduanjin group and different intervention (e.g., regular intervention, routine rehabilitation training, waiting list, sham Qigong, usual care, no intervention); (iv) outcomes - cognitive ability, shoulder joint function, anxiety, depression, fatigue, sleep quality, quality of life; and (v) study design - randomized controlled trial.
Results
From January 2013 to December 2023, we included a total of 16 RCTs involving 1247 patients. A total of 647 patients were in the experimental group and were treated with Tai Chi and Baduanjin, while 600 patients were in the control group and were treated with traditional methods. The results of our meta-analysis indicate that Tai Chi and Baduanjin yield outcomes that are comparable to those of traditional treatment methods. Specifically, Tai Chi and Baduanjin significantly increased cognitive function, increased shoulder joint function, improved sleep quality indicators and improved quality of life indicators. Furthermore, Tai Chi and Baduanjin significantly reduced anxiety symptoms, depression symptoms, and fatigue symptoms among breast cancer patients. Sensitivity analysis was performed, a funnel plot was constructed. No publication bias was indicated by Egger’s or Begg’s test.
Conclusion
Overall, Tai Chi and Baduanjin are viable and effective nonpharmacological approaches for treating breast cancer patients, as they yield better results than traditional treatment methods. However, these findings should be interpreted with caution due to the limited number of controlled trials, small sample sizes, and low quality of the evidence.
Systematic review registration
https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42023469301.
Keywords: Tai Chi and Baduanjin, rest breaks, meditation, relaxation, mindfulness, mental health, breast cancer patients
1. Introduction
1.1. Description of the condition
In 2020, the estimated number of new breast cancer cases and deaths increased respectively to 2.3 million(11.6%) and 685,000(6.9%) globally, among which China ranked first in new cases and deaths worldwide, accounting for approximately 18.4% of total new cases and 17.1% of total deaths globally in 2020 (1, 2). The high incidence and mortality rate have imposed a substantial burden on healthcare systems of countries with low resources (3). When women develop breast cancer, they experience a range of related painful experiences, such as anxiety (4, 5), depression (5, 6), fatigue (7–9), cognitive impairment (10, 11), shoulder function impairment (12, 13), sleep problems (14, 15), and poor quality of life (QoL) (16, 17). Conventional treatments such as surgery for breast cancer may have negative effects on survivors of breast cancer (18). Specifically, recent research has shown that surgery may lead to sleep disorders (19), life-threatening bleeding or infections (20), flap necrosis (21) and joint damage (22) in a significant percentage of patients with breast cancer. These side effects negatively affect survivors’ overall well-being and functionality, ultimately affecting their quality of life (17). Moreover, breast cancer survivors may face various complications after conventional treatments, such as surgery (total mastectomy and breast conservation), chemotherapy, and radiotherapy (23). Furthermore, breast cancer has been reported to be a risk factor for depression (6). Due to the alarming increase in the number of breast cancer patients worldwide and the lack of effective drug treatments for these diseases. Therefore, it is highly emergent to develop non-drug therapies and apply in the field of social work for the cancer patients are highly necessary. It may slow the distress of physical and psychological in breast cancer patients to combat personal and socioeconomic problems, to address the alarming increases in the incidences of cancer patients worldwide, and to overcome the lack of effective drug treatments for such diseases.
1.2. Description of the Taiji and Baduanjin invention
Nowadays, people’s attentional capabilities are increasingly strained by environmental factors such as time pressure (24) or multiple task demands (25), or even professional requirements (26). Since multitasking demands preoccupy large parts of people’s daily routines, the question of how to manage or to recover from the strain imposed by overload has become increasingly important, both for researchers and practitioners (27), Especially women (28). Formally, rest breaks are defined as temporal interruptions of an activity, serving the purpose of regenerating mental functions (29, 30). Conceptually, there are three fundamental aspects that are connected to taking a break, depending on the particular context: to find distance, to change activity mode (e.g., from thinking to sensing), and to recover or regain energy levels (31).
The practice of meditation has seen a tremendous increase in the western world since the 60s (32). Scientific interest in meditation has also significantly grown in the past years (33) and increasing evidence suggests the efficacy of meditation in health care and the field of stress management (34) and some potency to enhance positive feelings (35) increase pain tolerance, and reduce anxiety (36). TaiChi and Baduanjin also belong to meditation practice (37), This are different from other physical exercises like light gymnastics (38).
Unlike in western cultures, the Chinese felt that individuals are part of a closely knit collectivity, whether a family or a village, and that the behavior of the individual should be guided by the expectations of the group (39). The relationship view versus the rule stance is well illustrated by the difference between the holistic approach to medicine characteristic of the Chinese and the effort to find effective rules and treatment principles in the West. Surgery was common in the West from a very early period because the idea that some part of the body could be malfunctioning was a natural one to the analytic mind (39). But the idea of surgery was “heretical to ancient Chinese medical tradition, which taught that good health depended on the balance and flow of natural forces throughout the body” (39).
Originating in China, Tai Chi is a mind-body physical activity known as “meditation in motion”, and it has been practiced by the Chinese for centuries (40). Tai Chi is based on Chinese martial arts and integrates meditation elements, thereby enhancing well-being and promoting physical and mental health (41). The gentle, mindful, slow, and continuous movements of Tai Chi make it a preferable complementary program for promoting wellness (42, 43). Considerable empirical evidence supports the numerous health benefits associated with regular Tai Chi practice (44–46). To address these challenges in terms of quality of life and mental health, Baduanjin exercise, known as Qigong exercise, has been recommended as an effective treatment method for patients after surgery (47–49). Baduanjin comprises eight distinct sections of movements that are performed routinely. This traditional Chinese exercise combines controlled breathing with bodily movements, aiming to improve physical fitness and mental well-being. Unlike traditional exercise methods, Baduanjin emphasizes the need for a balanced approach that not only enhances physical strength but also nurtures psychological well-being, focusing on harmonious physical and mental integration (47). Furthermore, Baduanjin exercise is easy to perform without equipment or field restrictions. Baduanjin is free of equipment or field restrictions, so it is easy for people to learn and practice (47). After the founding of the Chinese Health Qigong Association, Baduanjin underwent modifications to accommodate the needs of diverse individuals, particularly those who suffer from physical or psychological sickness (50). To date, people have developed numerous therapeutic methods. Among them, Tai Chi therapy (42, 47) and Baduanjin (47, 51, 52) therapy are nonpharmacological treatment methods that have been advocated due to their lack of side effects.
Recent meta-analyses have shown potential benefits of Taiji therapy for anxiety (53–55), fatigue (56), cognitive impairment (55), shoulder function (54), sleep problems (57, 58) and quality of life (QoL) (59). It is necessary to examine the potential benefits of these therapies. In conclusion, Tai Chi and Baduanjin therapy have been regarded as a positive treatment strategies for breast cancer patients in terms of cognitive function, shoulder joint function, and mental health. Moreover, they have also been widely used in health-related subjects due to their positive effects (59, 60).
1.3. Tai Chi and Baduanjin therapy on breast cancer patients
In addition to genetic factors, ageing (61), family history (62), reproductive factors (63), oestrogen (64), and lifestyle (65) are five significant risk factors for breast cancer. However, lifestyle is the only one of these risk factors that is modifiable. Tai Chi (54, 56) and Baduanjin (47, 60) have garnered increasing recognition as impactful lifestyle choices that can help prevent and improve breast cancer outcomes. It may also serve as a beneficial complement to cancer treatment, reducing the risk of both breast cancer-specific mortality and overall mortality (66, 67). The Tai Chi and Baduanjin interventions are increasingly used in oncology (48) to achieve psychosocial stabilization and provide support for cancer patients (58).
1.4. Research gap and aim
Firstly, there are inconsistent clinical results regarding the effects of Taijiquan and Baduanjin therapy on cognitive ability, fall prevention, shoulder joint ability and mental health. Myers et al. (68) conducted a systematic review of breast cancer patients and reported that Tai Chi improved cognitive ability. Meng et al. (69) conducted a systematic review of breast cancer patients and reported that Baduanjin improved cognitive ability. However, Wei et al. (70) find Tai Chi failed to show any between-group differences in cognitive function. Luo discovered Tai Ji had positive effects on shoulder function and strength of arm in breast cancer patients compared with the non-exercise therapy (54). Fong et al. find Tai Chi showed a favorable effect of on pain and ROM of the shoulder joint, but not on hand grip strength, flexibility, and upper limb function compared with no treatment (71). A study (70) revealed that Taijiquan and Qigong can act as primary interventions for balance training and fall prevention. However, Li reported that there was no significant decrease in falls for strength training or Tai Chi Quan compared to the stretching control group among postmenopausal women receiving chemotherapy (58). Luo et al. reported that Tai Chi therapy was effective for improving mental health in breast cancer patients (72). Ye et al. (73) reported that Baduanjin therapy was effective for improving mental health in breast cancer patients. As reported by several researchers (47, 74, 75), Tai Chi and Baduanjin can significantly improve mental health. However, another observational study detected no significant time × group interaction effects on stress and mental health (76). Therefore, recent meta-analyses have reported conflicting results. Luo et al. (54) discovered that Tai Chi can decrease the fatigue symptom to breast cancer patients while Liu et al. (56) Hold the opposite view. Sameh Gomaa et al. find Tai Chi improved sleep quality and depressive symptoms (77). Wei et al. discovered Tai Chi failed to show any between-group differences in sleep quality and depression symptoms (70). Liu et al. demonstrated that tai chi is no different from conventional supportive care interventions in improving fatigue, sleeping quality, depression symptom at either 3 months or 6 months (54). Clinical data examining the effects of Tai Chi and Baduanjin on cognitive impairment, shoulder function impairment, Prevent falls, mental health fatigue, sleeping quality and depression symptom remain controversial. A more comprehensive review is needed to systematically evaluate the effects of Tai Chi and Baduanjin on the physical and mental health of breast cancer patients.
Secondly, many studies included indicated that Tai Chi and Baduanjin had positive effects on cognitive function, shoulder joint function, depression, anxiety, fatigue, sleep quality, and quality of life, but none included the effect of both Tai Chi and Baduanjin therapy on seven outcome measures. Tai Chi, breast cancer patients, cognitive function, shoulder joint function (54) depression symptom (78), anxiety symptom (79), fatigue symptom (78), sleep quality (80), and quality of life (81). Wei observed Baduanjin exercise has a certain preventive effect on the decline of subjective cognitive ability of breast cancer patients during chemotherapy clearly (70). Baduanjin, breast cancer patients, cognitive function (82), shoulder joint function (58), depression symptom (83), anxiety symptom (83), fatigue symptom (84), sleep quality (70), and quality of life (60). This study investigates the effects of Tai Chi and Baduanjin on the cognitive ability, shoulder joint ability and mental health of breast cancer patients simultaneously.
Thirdly, it is important to investigate not only the effects of Tai Chi and Baduanjin but also the variables that may influence their effectiveness, including duration of treatment and target population. In this research, we used weeks and continental plate to divide Sub-group analysis, which was not available in previous studies. To address this gap, we conducted a comprehensive systematic review and meta-analysis to evaluate the impact of Tai Chi and Baduanjin on training breast cancer patients.
2. Materials and methods
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA, 2020) guidelines, as detailed in the Multimedia Appendix 3 Abstracts checklist and Multimedia Appendix 4 Checklist 2020 (85). The study was also registered in PROSPERO (CRD42023469301).
2.1. Selection criteria
For this study, eligibility criteria were established based on the PICOS principles. (1) P: The subjects had to exhibit at least one indicator of cognitive function, shoulder joint function, or mental health, and they had to be 18 years of age or older. (2) I: Tai Chi and Baduanjin were implemented among breast cancer patients in the experimental group without restrictions on the time of intervention. (3) C: The control group received a different intervention (e.g., regular intervention, routine rehabilitation training, waiting list, sham qigong, usual care, no intervention). (4) O: The outcomes included cognitive function, shoulder joint function and mental health in breast cancer patients. (5) S: The type of study was RCTs. The exclusion criteria were as follows: (1) reviews, case reports, non-RCTs, or articles without full-text availability; (2) animal experiments or duplicate publications; and (3) unavailable or incomplete data. Furthermore, we used the PICOS principles to identify eligible studies ( Multimedia Appendix 1 ). All studies included were published in Chinese or English, and studies that interpreted results from the perspective of breast cancer patients were considered eligible.
2.2. Search strategy
To identify relevant literature, the following databases were searched: the UWE Library database, PubMed, MEDLINE, Embase, the Cochrane Library, Scopus, PsycINFO, SinoMed, Wanfang Data, China National Knowledge Infrastructure (CNKI), Yiigle, Wanfang MED ONLINE, and Web of Science. The search terms varied slightly across databases. Keywords such as “Cognitive Function or Shoulder Joint Function or Mental Health or Depression or Anxiety or Fatigue or Sleep Quality or Quality of life”, and “a pilot study or Randomized Controlled Trial or RCT,” and “Tai Chi and Baduanjin,” as well as “Breast Cancer Patients or Breast Cancer Women” were used to retrieve articles published from January 1, 2013, to December 1, 2023. The “snowball” method was employed to trace the references of the included studies. Moreover, the references of the included studies were manually searched to identify additional eligible articles. Academic unpublished literature was considered ineligible. The retrieval strategy for the PubMed database is provided in Multimedia Appendix 2 .
The search strategies are presented in Figure 1 . Four researchers (Zuo Xinyi, Tang Yong, Chen Yifang and Zhou Zhimiao) screened all the literature for eligibility. After the removal of duplicates, the initial screening of all studies was based on abstracts and titles. Subsequently, the researchers read the full texts of the remaining articles according to the predefined inclusion and exclusion criteria. Finally, they extracted data from the selected literature. Additionally, we retrieved grey literature (opengrey.eu) to further identify related publications.
Figure 1.
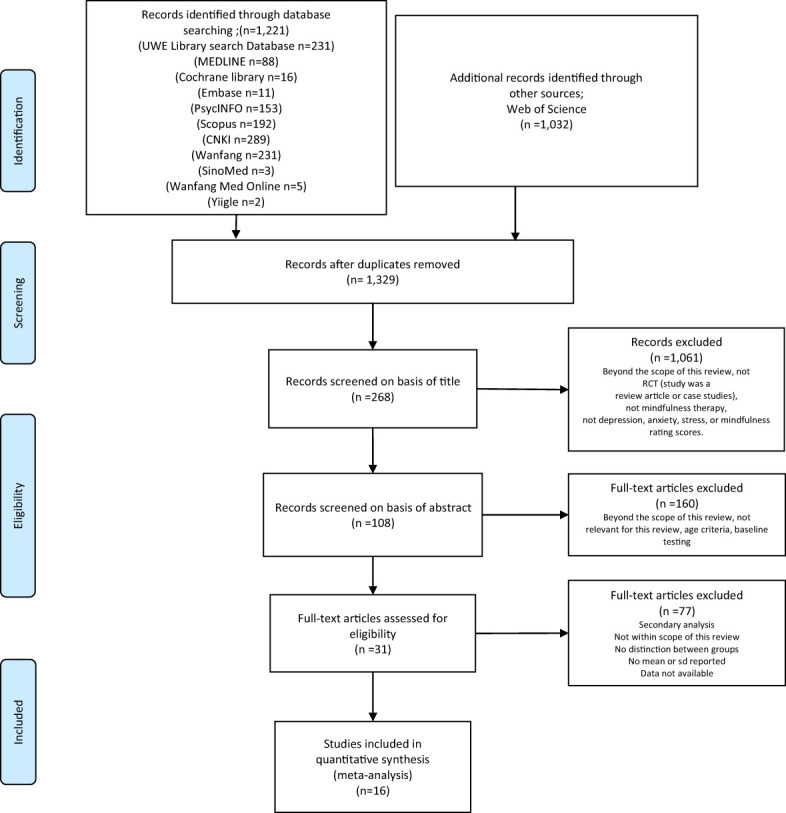
Study selection flowchart (PRISMA, 2020).
2.3. Data extraction
After removing duplicate studies (using EndNote X9), four reviewers (Zuo Xinyi, Tang Yong, Chen Yifang and Zhou Zhimiao) independently screened the abstracts and titles of the studies. Subsequently, the full texts of the remaining studies were evaluated according to the predefined inclusion and exclusion criteria.
The first authors (Zuo Xinyi and Chen Yifang) used a modified version of the data extraction form in the Cochrane Handbook for Systematic Reviews of Interventions (86) to extract study characteristics. They also extracted data on the content, design, and delivery features of the interventions (definitions provided in the “Introduction”) by a modified template version for intervention description as well as replication (TIDieR) checklist and guide (87). On a random sample of three studies, the forms were first tested and then used by the first authors (Zuo Xinyi and Chen Yifang) for the completion of data extraction. Once the study was completed, the accuracy of the process was verified by the second author (Zhou Zhimiao). Finally, through thematic analysis (88), we determined in advance the content of the author, year, country, publication type, study design, sample size, mean age (SD), age, MMSE score, health condition, population group, setting, results as reported in the studies, and conclusions ( Table 1 ); author, year, intervention type, modes of delivery, materials, procedures, activities, and/or processes, format of the intervention delivery, location, duration of intervention, length of sessions, frequency of sessions, intensity, measurement, follow-up, and Jadad score ( Table 2 ).
Table 1.
Study characteristics and findings of the included studies.
| Author(year) | Country | Publication type | Study design | Sample size | Age/Mean age (SD) | Health condition | Population group | Setting | Conclusion | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | IG 1 | CG 2 | IG | CG | The interactive game can improve senile dementia patients` cognitive function and daily living ability. | |||||||
| 1. Han et al., 2017 (89) | China Shanxi | JA 3 | RCT 4 | 60 | 30 | 30 | 39-55(47.83) | 37-55(46.23) | BC 5 | Chemotherapy patients one month after breast cancer surgery | clinical | Baduanjin training can significantly improve the anxiety and of mental health status patients after breast cancer surgery. |
| 2. Li et al.2017 (90) | China Shanxi | JA | RCT | 61 | 31 | 30 | 37-57(47.31) | 34-56(45.43) | BC | Diagnosed breast cancer who requiring radiotherapy after chemotherapy | clinical | Baduanjin intervention can improve the anxiety and depression & improve the quality of life of patients |
| 3 Li et al., 2013 (91) | China Fujian | JA | RCT | N =57 | 29 | 28 | 47(47.56) | 47(47.56) | BC | Pathology confirmed breast cancer, and modified radical operation | clinical | Tai Chi Yunshou training has a certain effect on improving the quality of life of patients. |
| 4 Lv et al., 2015 (92) | China Henan | JA | RCT | N=149 | 100 | 49 | 32-65(48.61) | 32-65(48.61) | BC | Pathologic diagnosis and voluntary modified radical treatment of unilateral breast cancer | clinical | Tai Chi have potential advantages in promoting the postoperative rehabilitation of breast cancer patients and improving the quality of life of patients after surgery. |
| 5 Wang Hongying, 2015 (93) | China Wuhan | JA | RCT | N =149 | 75 | 74 | 43-59(51.4) | 42-58(50.58) | BC | Clinical pathology examination | clinical | The exercise mode of Tai Chi and rehabilitation exercises has a positive effect on improving the mental health of breast cancer patients after surgery. |
| 6 Wang et al., 2016 (94) | China Wuhan | JA | RCT | N=96 | 48 | 48 | 46-60(53.64) | 44-59(51.74) | BC | Confirmed breast cancer on pathological examination, with modified radical resection | clinical | |
| 7 Yang et al., 2022 (95) | China Henan | JA | RCT | N=88 | 44 | 44 | 37-78(58.24) | 36-78(57.86) | BC | Gave surgical resection and postoperative chemotherapy intervention | clinical | Baduanjin exercise can improve post-surgery treatment compliance, limb function, health status, quality of life, mood, nursing satisfaction, and have minimal side effects for breast cancer patients. |
| 8 Liao et al., 2022 (82) | China Guangzhou | JA | RCT | N=68 | 33 | 35 | 46-60(53.12) | 46-63(54.63) | BC | Diagnosis with stage I–III breast cancer for 6 months to 8 years prior to recruitment | clinical | Baduanjin exercise improved the quality of life and sleep of breast cancer patients. |
| 9 Larkey et al., 2015 (96) | The United State | JA | RCT | N =87 | 42 | 45 | 48-66(57.7) | 50-68(59.8) | BC | Diagnosed with Stage 0-III breast cancer | clinical | Both Qigong and Tai Chi can improved depression and sleep dysfunction among breast cancer survivors. |
| 10 Larkey et al., 2016 (97) | The United State | JA | RCT | N =87 | 42 | 45 | 48-66(57.7) | 50-68(59.8) | BC | Diagnosed with Stage 0-III breast cancer | clinical | Both Qigong and Tai Chi could enhance the quality of life, cognitive function, and physical activity patterns in women with a history of breast cancer. |
| 11 Thongteratham et al., 2015 (98) | Thailand | JA | RCT | N=30 | 15 | 15 | 54-65(60.3) | 55-65()61 | BC | First diagnosis with stage 0-IIIb breast cancer | clinical | The study suggests that Tai Chi Qi Qong benefits Thai women with breast cancer. |
| 12 Huang et al., 2016 (99) | China Taiwan | JA | RCT | N=62 | 31 | 31 | 18-65(51.4) | 18-65(51.4) | BC | Adult women with breast cancer who were about to start chemotherapy | clinical | The study preliminarily suggests SQG and NSQG may improve frailty and QOL in breast cancer patients undergoing chemotherapy. |
| 13. Fong et al., 2013 (100) | China HongKong | JA | RCT | N=23 | 11 | 12 | 48-68(58.3) | 49-58(53.8) | BC | Having received a mastectomy with or without adjutant chemotherapy or radiotherapy | clinical | Tai Chi and Qigong training might improve shoulder muscular strength and functional wellbeing in breast cancer survivors. |
| 14 Loh et al., 2014 (101) | Malaysia | JA | RCT | N =64 | 32 | 32 | 18-65(41.5) | 18-65(41.5) | BC | Had a primary diagnosis of early stage (I-II) breast cancer | clinical | Qigong mildly enhanced life quality in cancer survivors. |
| 15 Wei et al., 2022 (70) | China Shanghai | JA | RCT | N =70 | 35 | 35 | 43-60(52) | 50-62(55) | BC | Female patients newly diagnosed with stage I to III BC and scheduled to receive chemotherapy | clinical | This pilot study showed that Baduanjin exercise improves cognition and quality of life in Chinese breast cancer patients undergoing chemotherapy. |
| 16 Chen et al., 2013 (102) | China Shanghai | JA | RCT | N=96 | 49 | 47 | 29-58(45.3) | 25-62(44.7) | BC | Women with stage 0–III breast cancer who were had undergone breast surgery | clinical | Qigong help to improve quality of life and reduce depressive symptoms in women undergoing radiotherapy for breast cancer. |
IG, Intervention Group.
CG, control group.
JA, Journal article.
RCT, Randomized controlled trial.
BC, breast cancer.
Table 2.
Intervention characteristics—Adapted from the template for intervention description and replication (TIDieR) checklist and guide.
| Author, year | Intervention type | Content (what)—the materials, procedures, activities, and/or processes | Delivery (who, where, when, how much)—format of the intervention delivery, the location, duration of intervention, length of sessions, frequency of sessions, intensity |
Measurement | Follow-up | Jadad score | |
|---|---|---|---|---|---|---|---|
| IG a | CG b | ||||||
| 1. Han et al., 2017 (89) | BaDuanJin training | regular intervention | Under the guidance of the head coach, 5 students became auxiliary coaches responsible for guiding patients to perform Eight Section Brocade training in the hospital square until they mastered the correct movements. The discharged patient trains for 20 minutes every afternoon, 5 times a week and daily follow-up. | Format: group Location: public hospital Duration: 3 month Length: 20 min Frequency: 5 times/week Intensity: move follow with the DVD of baduanjin training |
Anxiety: SAS c | Baseline, Post-intervention | 4 |
| 2 Li et al., 2017 (90) | BaDuanJin training | regular intervention | A nurse became the main trainer and led 5 interns jointly conducted a one week Eight Section Brocade training for 31 patients, including group exercises at the hospital square, exercises on CDs published by the Fitness Qigong Management Center of the General Administration of Sport of China, and follow-up on the completion status of patients through phone calls. | Format: group Location: public hospital or Home Duration: 3 month Length: no record Frequency: 5 times/week Intensity: move follow with the DVD of baduanjin training |
Anxiety:SAS Depresstion: SDS d |
Baseline, Post-intervention | 5 |
| 3 Li et al., 2013 (91) | TaiChi cloudyhand | regular intervention | Starting 1-2 weeks after surgery, shoulder joint activities will be carried out, with the arm swinging back and forth centered around the shoulder. Daily activities will gradually be performed. Train 1-3 times a day for 20-30 minutes each time. The experimental group began Tai Chi training 7 days after surgery. Three nurses provide Tai Chi exercise guidance to patients through “Tai Chi Exercise”, helping them master the correct posture of Tai Chi cloud hand movements, and lead patients to 30 minutes of training every day in the hospital’s aerial garden corridor. | Format:group Location: public hospital Duration: 6 month Length: 30min Frequency: 14 times/week Intensity: move follow with nurse order |
Quality of life: WHOQOLBREF e Shoulder joint function: Lovett | day 7, 1 month, 3 month, 6 month. | 5 |
| 4 Lv et al., 2015 (92) | TaiChi & Baduanjin | regular intervention | A week of basic training, after the patient can accurately master the movements and breathing essentials into the exercise intervention period. Practice for 60min and 3 times a week for 6 months. | Format:group Location:community Duration: 3 month Length: 60 min Frequency: 3 times/week Intensity: learn from order and do it by themselves |
Quality of life: SF-36 f Shoulder joint funtion: Constant-murley | day 10, 1 month, 3 month. | 4 |
| 5 Wang Hongying 2015 (93) | TaiChi | Routine rehabilitation training | Transitional training at least twice a day for 20-30 minutes each time. After 10 days, the intervention group patients can undergo Chen’s Tai Chi exercise, once in the morning and once in the evening, for 20 minutes each time. After discharge, the patients still need to follow the exercise until 6 months after surgery. Conduct two phone follow-up or home visits per week to continue routine rehabilitation training and Tai Chi exercise. | Format: group Location: public hospital or Home Duration: 6 month Length: 20min Frequency: 14 times/week Intensity: On-site teaching and broadcast Taijiquan video, the chief nurse on time patrol |
Anxiety: SAS | day 10, 1 month, 3 month, 6 month. | 4 |
| 6 Wang et al., 2016 (94) | Tachi & regular intervention | regular intervention | Tai Chi exercises are jointly developed by Tai Chi trainers and head nurses, including on-site teaching and playing Tai Chi videos. The patient needs to undergo two routine rehabilitation exercises and two Tai Chi exercises per day, each lasting 20 minutes. After discharge, the nurse will conduct telephone follow-up or home visits twice a week to ensure that the patient continues to receive routine rehabilitation training and Tai Chi exercises. | Format: group Location: public hospital or Home Duration: 3 month Length: 20min Frequency: 14 times/week Intensity: learn from order and do it by themselves |
Shoulder joint funtion: Neer Quality of life: FACT-B g |
day 10, 1 month, 3 month, 6 month. | 4 |
| 7 Yang et al., 2022 (95) | Traditional Chinese medicine rehabilitation physiotherapy&Baduanjin | regular intervention | A fitness qigong called Ba Duan Jin have 10 movements that can help patients relax and maintain natural breathing. Before discharge, the therapist will guide the patient and their family to master relevant physical therapy and exercise methods, and develop a training plan to follow up on the patient’s training situation. | Format: group Location: public hospital or Home Duration: 3 month Length: no record Frequency: 7 times/week Intensity: learn from video guided by professional |
Shoulder joint funtion: Constant-murley Quality of life: FACT-B |
Baseline, Post-intervention | 4 |
| 8 Liao et al., 2022 (82) | Baduanjin | usual care | The Baduanjin program was composed of 90 min per session with 2 sessions per week (Monday and Wednesday) for 12 weeks. | Format: group Location: public hospital or Home Duration: 3 month Length: 90 min Frequency: 2 times/week Intensity: learn from 2 experts |
Sleep quality: PSQI Quality of life: EORTC QLQ-c30 h |
Baseline, Post-intervention | 4 |
| 9 Larkey et al., 2015 (96) | TaiChi/Qigong | sham Qigong | This research project has two courses led by a nurse and a professor of exercise physiology. There are two meetings per week in the first two weeks, and only one meeting per week thereafter. Participants are required to practice at home for 30 minutes per week for a total of 5 days, and the frequency, number of minutes, and level of effort of the practice must be recorded. | Format: group Location: Home Duration: 3 month Length: 30 min Frequency: 5 times/week Intensity: learn from 2 experts |
Fatigue: FSI Sleep quality: PSQI Depression: BDI i |
Baseline, Post-Intervention, 3 Month Follow up | 5 |
| 10 Larkey et al., 2016 (97) | TaiChi/Qigong | sham Qigong | Professionals experienced in leading exercise sessions with cancer patients taught both Qingong and Tai Chi Easy56 practices (TCE) exercises interventions. Sessions were sixty minutes long, delivered over 12 weeks, meeting twice a week for the first two weeks to provide the opportunity to learn the practices well, then once a week for the remainder of the period. Participants were asked to practice at home at least 30 minutes a day, 5 days per week and to keep a log of the frequency, minutes of practice and level of exertion. | Format: group Location: Home Duration: 3 month Length: 30 min Frequency: 5 times/week Intensity: learn from 2 experts |
Cognitive function: FACT-cogPCI
j
Quality of life: SF36 |
Baseline, immediately after the 12-week intervention and again at 12 weeks post-intervention. | 6 |
| 11 Thongteratham et al., 2015 (98) | TaiChi/Qigong | usual care | Each 60-minute TCQQ session is divided into three phases: 1) warm-up (extend muscle for 5 minutes), 2) exercise (18-form TCQQ practicing for 45-50 minutes), and cool-down(decreasing exercise to normal for 5-10 minutes). The 18-form TCQQ was grouped into 3 sets (6-form/set) aiming to assist participants’ memory. The participants practiced the 18-forms at the 4th week of the program. A weekly follow-up telephone call was done by the PI to monitor. | Format: group Location: Home Duration: 12 week Length: 60 min Frequency: 5 times/week Intensity: learn from TCQQ.The TCQQ Program was developed by the researchers, based on TC literature and research and was validated by 3 experts, a psychologist, a physical therapy instructor, and an advanced practice nurse (APN) in medical-surgical nursing |
Quality of life: FACT-B Fatigue: FSI k |
Baseline, 6week, 12 week | 6 |
| 12 Huang et al., 2016 (99) | Sporting Qigong | usual care | This study invited two qigong experts, two general surgeons, and two oncology case managers to help patients exercise. Participants were asked to exercise three times a week for 12 weeks, each lasting 30 minutes. The researchers also contacted all participants by phone to encourage them to exercise regularly.The patients were asked to complete finger and palm exercises, shoulder exer_x0002_cises, hand lifting, hair combing, pendulum exercises, wall hand climbing, pulley tugging, chest flies, towel exercises, rod lifting, pushing on the wall, and putting on a brassiere. |
Format: group Location: hospital & home Duration: 12 week Length: 30 min Frequency: 3 times/week Intensity: All participants have received at least one training session before starting their exercise or qigong program. The number of training courses is based on the patient’s ability to fully intervene. They are required to undergo postoperative exercise |
Quality of life: Physical and mental components for QOL | baseline, 1 month, 3 months | 4 |
| 13. Fong et al., 2013 (100) | Tai Chi Internal Qigong | regular intervention | This exercise will be conducted 3 times a week for 1 hour each time. It includes 18 movements aimed at helping the body relax, reduce stress, and enhance breathing awareness. These movements include center of gravity transfer, arm swing, boxing, and mild stretching of various parts of the body, which require breathing control under professional guidance. | Format: group Location: the Sports Training and Rehabilitation Labo_x0002_ratory Duration: 6 month Length: 60 min Frequency: 3 times/week Intensity: trained by experts |
Cognitive fouction: FACT-B Shoulder joint function: Shoulder active Rom |
Baseline, Post-Intervention | 4 |
| 14 Loh et al., 2014 (101) | internal Qigong (Zhi Neng Qigong) programme |
usual care | Invite participants to participate in an 8-week qigong course each week, taught in person by qualified qigong masters. Warm up 10 minutes before each class, followed by 70 minutes of main exercise, and remain calm for 10 minutes at the end of the class. The course includes two 5-minute breaks. This course teaches the basic steps of empowering qigong, including three different starting sequence postures. Attendees need to attend five meetings to master their posture and pace. | Format: group Location: community Duration: 8 week Length: 60 min Frequency: 1 times/week Intensity: trained by experts face to face |
Cognitive function:FACT-B | Baseline, Post-Intervention, Follow-up study (12 month after baseline) | 5 |
| 15 Wei et al., 2022 (70) | BaDuanJin training | usual care | This is a qigong training consisting of 10 postures, with professional trainers providing training guidance and video demonstrations. After the first hospital meeting before starting chemotherapy, it is recommended that patients undergo video exercise at home, 5 times a week for half an hour each time, for a period of 12 weeks. The training includes stretching joints, inhaling and exhaling, 2 minutes of muscle relaxation, and two 12 minute Eight Section Brocade exercises. | Format: group Location: hospital & home Duration: 12 week Length: 30 min Frequency: 5 times/week Intensity: trained by experts and video tape |
Quality of life: FACT-B Anxiety: HADS l Depression: HADS |
pre-intervention, 4 weeks, 8 weeks, and 12 weeks | 3 |
| 16 Chen et al., 2013 (102) | qigong sessions | no intervention | Women in the qigong group attend 5 sessions 40 minute qigong classes per week for 5-6 weeks. These courses are taught by a government licensed master of traditional Chinese medicine and qigong. The number of participants may vary, ranging from 1 to 10. Participants will receive a DVD containing program records of qigong and some printed materials, encouraging them to complete the course without a qigong master. | Format: group Location: hospital & home Duration: 3 month Length: 40 min Frequency: 1 times/week Intensity: trained by experts and video tape |
Cognitive function: FACT-G
m
Depression: CES-D n Sleep quality: PSQI o |
baseline, middle, Last week of treatment, 1 months later, and 3 months later. | 3 |
IG, Intervention Group.
CG, control group.
SAS, self-rating anxiety scale;
SDS, self-rating depressive scale;
WHOQOLBREF, Brief table of quality of life assessment recommendation by WHO;
SF-36, The 36-item Medical Outcomes Survey Short Form;
FACT-B, functional assessment of cancer therapy—breast;
EORTC QLQ-C30, European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30;
BDI, the 20-item Beck Depression Inventory;
Fact-Cog PCI, the Functional Assessment of Cancer Therapy-Cognitive Function perceived cognitive impairment;
FSI, The Fatigue Symptom Inventory;
HADS, hospital anxiety and depression scale;
FACT-G, The Functional Assessment of Cancer Therapy–General;
CES-D, the Center for Epidemiologic Studies-Depression;
PSQI, The Pittsburgh Sleep Quality Index.
The following data were extracted from the included studies: (1) the information of the literature included (name of author, publication year, country, publication type and study design); (2) the characteristics of the subjects (sample size, participant mean age, participant age, Mini-mental State Examination (MMSE) score, participant health conditions and population group); (3) the interventions (setting, intervention type, design (how)—the modes of delivery, content (what)—the materials, procedures, activities, and/or processes, delivery (who, where when, how much)—format of the intervention delivery, the location, duration of intervention, length of sessions, frequency of sessions, intensity); (4) the information on quality of the study (Jadad score); and (5) the main outcomes (results as reported in studies, conclusion, measurement and follow-up).
2.4. Quality and bias assessment
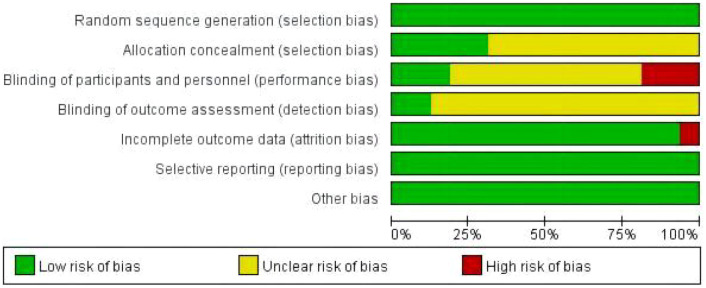
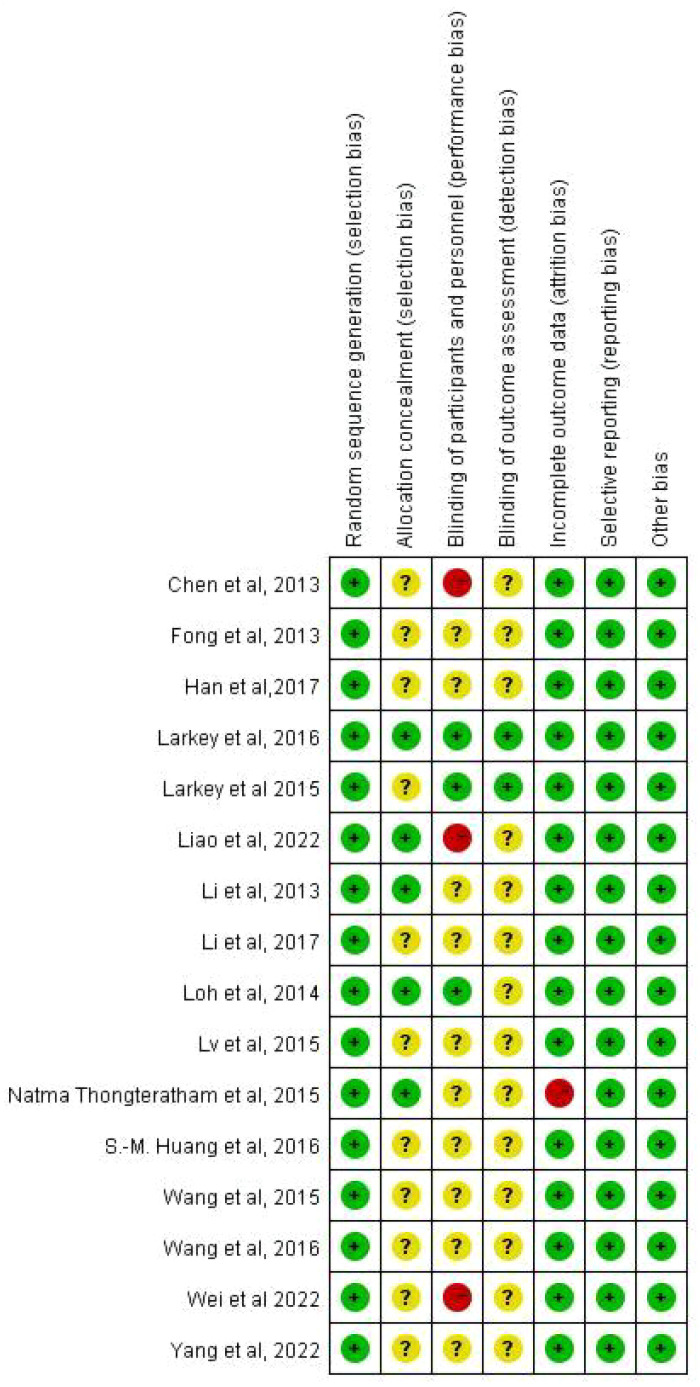
Using the Cochrane Collaboration Risk of Bias tool, authored by Higgins et al. (86) in 2008, four researchers—Zuo Xinyi, Tang Yong, Chen Yifang and Zhou Zhimiao—independently evaluated the potential for bias in the included studies. Furthermore, to assess the overall quality of the literature, we employed the Jadad scale (103). This risk of bias tool encompasses seven distinct domains: 1. allocation concealment, 2. random sequence generation, 3. blinding of subjects and experimenters, 4. blinding of outcome assessors, 5. selective reporting, 6. integration of resulting data, and 7. other potential sources of bias. Each study was classified as having an unclear, low, or high risk of bias for each domain. Additionally, to assess the degree of publication bias, we conducted the Egger and Begg tests; through these comprehensive assessments, we aimed to ensure the reliability and validity of our findings (76).
2.5. Statistical analysis
Data analysis was conducted utilizing Review Manager 5.3 software and Stata 15.1. To visually represent the findings, forest plots were generated. The studies included in the analysis measured outcomes as continuous variables, with the same indicator assessed using diverse tools. To standardize these measurements, the outcomes are expressed as standard mean differences (SMDs). Statistical significance was determined at α = 0.05. Through this rigorous analytical process, we aimed to provide a comprehensive understanding of the results. Heterogeneity was evaluated using I² statistics, with categories defined as high (>75%), moderate (50-75%), low (<50%), or as outlined (104) in 2002. When high heterogeneity was observed, a sensitivity analysis was conducted using the leave-one-out approach to pinpoint potential sources. During this analysis, multiple weeks were compared as subpoints to ensure the robustness of the findings. Additionally, Begg’s test (105) and Egger’s test (106) in 1997 were utilized to assess the likelihood of publication bias, thereby enhancing the overall reliability of our results. When the meta-analysis included at least 10 studies, a funnel plot (107, 108) was used to assess potential publication bias. Specifically, this study focused on examining the standard mean difference (SMD) along with its corresponding 95% confidence interval (CI) (109). If the overall effect yielded a p value less than 0.05, it was interpreted as statistically significant evidence favouring the effects of MBIs.
2.6. Subgroup analyses
We conducted subgroup analyses on the basis of intervention country (inside or outside China) and intervention duration (weeks).
3. Results
3.1. Selection of studies
Figure 1 outlines the study selection process, and the results are presented in Figure 1 . After searching through thirteen databases, a total of 2,253 records were found. All studies were imported into EndNote X8 (Bld, 10063) (110), and duplicates were removed. Following the removal of 924 duplicates and a rigorous screening process that eliminated 1,313 articles, 16 trials (70, 82, 89–102) with 1,256 participants were ultimately included. Studies were excluded if they did not report sd values (75), were missing data for the control group (111), were review articles (68), or were not within the scope of this meta-analysis (112). All the studies included indicated that Tai Chi and Baduanjin had positive effects on cognitive function, shoulder joint function, depression, anxiety, fatigue, sleep quality, and quality of life. The primary outcomes of interest were as follows: cognitive function scores, as assessed by the Functional Assessment of Cancer Therapy-Cognitive Function Perceived Cognitive Impairment (Fact-Cog PCI), The Functional Assessment of Cancer Therapy-Breast (FACT-B), The Functional Assessment of Cancer Therapy-General (FACT-G); shoulder joint function, as assessed by the shoulder active Rom, Lovett Constant-Murley, Neer; depression symptoms, as assessed by the Center for Epidemiologic Studies-Depression (CES-D), the 20-item, Beck Depression Inventory (BDI), self-rating depressive scale (SDS), hospital anxiety and depression scale (HADS); anxiety symptoms, as assessed by the Self-rating Anxiety Scale (SAS), Hospital Anxiety and Depression Scale (HADS); fatigue symptoms, as assessed by the British Standard Institution (BSI), The Fatigue Symptom Inventory (FSI), Multidimensional Fatigue Symptom Scale type: Primary indicator (MFSI-SF); sleep quality, as assessed by the Pittsburgh Sleep Quality Index (PSQI); quality of life, as assessed by the 36-item Medical Outcomes Survey Short Form (SF-36), European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30), Brief table of quality of life assessment recommendation by WHO (WHOQOLBREF), Functional Assessment of Cancer Therapy—Breast(FACT-B), physical components of quality of life and mental components of quality of life.
3.2. Study characteristics
Tables 1 , 2 present the general features of the included studies. All 16 studies were published before 2024. The sample sizes ranged from 11 to 100, and a total of 1247 breast cancer patients over the age of 18 were enrolled, with 654 participants in the experimental group and 602 in the control group. None of the breast cancer patients had been diagnosed with a psychiatric disorder. The interventions were based on Tai Chi and Baduanjin, with durations ranging from 5 weeks to 24 weeks. The weekly intervention time varied between 20 minutes and 90 minutes. Both individual and group training methods were utilized (70, 82, 89–102). All studies (70, 82, 89–102) were further categorized into Tai Chi and Baduanjin therapy.
3.3. Risk of bias and quality assessment
Figures 2 and 3 provides an assessment of the risk of bias. All 16 articles (70, 82, 89–102) provided detailed descriptions of the randomization methods. Four studies reported the blinding method, and all of them were single-blinded trials (82, 89, 91, 95). The dropout rate was reported in two articles (89, 96). The average Jadad score for all included studies was 4.1875, indicating fair to mild quality.
Figure 2.
Risk of bias graph.
Figure 3.
Risk of bias summary of included studies.
3.4. Meta-analyses
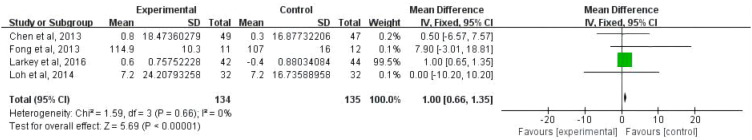
3.4.1. Cognitive function scores
Four studies involving 209 breast cancer patients (141 in the experimental group and 138 in the control group) evaluated the effect of Tai Chi and Baduanjin on cognitive function in breast cancer patients. Due to the utilization of various evaluation tools, the SMD was utilized as the pooled measure for effect size. The pooled results revealed no heterogeneity among the studies (P =.66, I2 = 0%). As shown in Figure 4 , the Tai Chi and Baduanjin groups had significantly higher cognitive ability scores than the control group (SMD 1.00, 95% CI 0.66 to 1.35; P<.00001).
Figure 4.
Forest plot for MMSE scores.
3.4.2. Shoulder joint function scores
Five studies involving 456 breast cancer patients (228 in the experimental group and 228 in the control group) evaluated the effect of Tai Chi and Baduanjin on the Shoulder Joint Function scores of breast cancer patients based on the shoulder active Rom, Lovett Constant-Murley, Neer. Due to the utilization of various evaluation tools, the SMD was utilized as the pooled measure for effect size. The pooled results revealed a high degree of heterogeneity among the studies (P=.07, I2 = 51%), necessitating the use of a random effects model for the meta-analysis. As shown in Supplementary Figure 5 , there were significantly higher shoulder joint function scores in the Tai Chi and Baduanjin groups than in the control group (SMD 7.34, 95% CI 6.32 to 8.35; P<.00001).
3.4.3. Anxiety indicators
Four studies involving 340 breast cancer patients (171 in the experimental group and 169 in the control group) evaluated the effect of Tai Chi and Baduanjin on anxiety symptoms among breast cancer patients based on the SAS and HADS. Due to the utilization of various evaluation tools, the SMD was utilized as the pooled measure for effect size. The pooled results revealed a high degree of heterogeneity among the studies (P<.00001, I2 = 90%), necessitating the use of a random effects model for the meta-analysis. As shown in Supplementary Figure 6 the Tai Chi and Baduanjin groups had significantly lower anxiety scores than the control group (SMD - 2.22, 95% CI - 3.15 to - 1.29; P<.00001).
3.4.4. Depression indicators
Four studies involving 318 breast cancer patients (158 in the experimental group and 160 in the control group) evaluated the effect of Tai Chi and Baduanjin on depression symptoms in breast cancer patients based on the CES-D, BDI, SDS, and HADS. Due to the utilization of various evaluation tools, the SMD was utilized as the pooled measure for effect size. The pooled results revealed a high degree of heterogeneity among the studies (P=.02, I2 = 88%), necessitating the use of a random effects model for the meta-analysis. A shown in Supplementary Figure 7 , the Tai Chi and Baduanjin groups had significantly lower depressions scores than the control group (SMD - 1.44, 95% CI -2.46 to -0.41; P<.006).
3.4.5. Fatigue indicators
Four studies involving 282 breast cancer patients (141 in the experimental group and 141 in the control group) evaluated the effect of Tai Chi and Baduanjin on fatigue symptoms in breast cancer patients based on the BSI, FSI, and MFSI-SF. Due to the utilization of various evaluation tools, the SMD was utilized as the pooled measure for effect size. The pooled results revealed a high degree of heterogeneity among the studies (P=.17, I2 = 41%), necessitating the use of a random effects model for the meta-analysis. As shown in Supplementary Figure 8 , the Tai Chi and Baduanjin groups had lower fatigue scores than the control group (SMD - 1.02, 95% CI -1.52 to -0.53; P<.0001).
3.4.6. Sleep quality indicators
Three studies involving 222 breast cancer patients (110 in the experimental group and 112 in the control group) evaluated the effect of Tai Chi and Baduanjin on sleep quality indicators in breast cancer patients based on the PSQI. Due to the utilization of various evaluation tools, the SMD was utilized as the pooled measure for effect size. The pooled results revealed a high degree of heterogeneity among the studies (P=.001, I2 = 85%), necessitating the use of a random effects model for the meta-analysis. As shown in Supplementary Figure 9 , the Tai Chi and Baduanjin groups had higher sleep quality scores than the control group (SMD - 1.44, 95% CI -2.57 to -0.31; P=.01).
3.4.7. Quality of life indicators
Nine studies involving 749 breast cancer patients (372 in the experimental group and 377 in the control group) evaluated the effect of Tai Chi and Baduanjin on breast cancer patients’ quality of life indicators based on the SF-36, EORTC QLQ-C30, WHOQOLBREF, FACT-B, physical components of quality of life and mental components of quality of life. Due to the utilization of various evaluation tools, the SMD was utilized as the pooled measure for effect size. The pooled results revealed a high degree of heterogeneity among the studies (P=<.0001, I2 = 93%), necessitating the use of a random effects model for the meta-analysis. Supplementary Figure 10 shows that there was a significant increase in the quality-of-life scores of the Tai Chi and Baduanjin groups than the control group (SMD 6.94, 95% CI 5.60 to 8.27; P<.00001).
In conclusion, the included studies used the following assessment tools: the Fact-Cog PCI, FACT-B, FACT-G, shoulder active Rom, Lovett Constant-Murley, Neer, CES-D, BDI, SDS, HADS, SAS, HADS, BSI, FSI, MFSI-SF, PSQI, SF-36, EORTC QLQ-C30, WHOQOLBREF, FACT-B, physical components of quality of life and mental components of quality of life. Seven outcomes were evaluated: cognitive function, shoulder joint function, depression, anxiety, fatigue, sleep quality, and quality of life. The Tai Chi and Baduanjin groups had significantly greater total scores for cognitive function than the control group (CG) (SMD 1.00, 95% CI: [0.66, 1.35], P<.00001, I2 = 0%) ( Figure 4 ). Compared with the control group (CG), the Tai Chi and Baduanjin groups had significantly greater total shoulder joint function scores (SMD 7.34, 95% CI: [6.32, 8.35], P<.00001, I2 = 51%) ( Supplementary Figure 1 ). In addition, the Tai Chi and Baduanjin groups had lower anxiety scores than the CG (SMD - 2.22, 95% CI: [- 3.15, - 1.29], P <.00001, I2 = 90%) ( Supplementary Figure 2 ). The Tai Chi and Baduanjin groups had lower depression levels than the CG (SMD - 1.44, 95% CI: [-2.46, -0.41], P = .006, I2 = 88%) ( Supplementary Figure 3 ). The Tai Chi and Baduanjin groups had lower fatigue levels than the CG (SMD - 1.02, 95% CI: [-1.52, -0.53], P <.0001, I2=41%) ( Supplementary Figure 4 ). The Tai Chi and Baduanjin groups had better sleep quality than the CG (SMD - 1.44, 95% CI: [-2.57, -0.31], P = .01, I2 = 85%) ( Supplementary Figure 5 ). The Tai Chi and Baduanjin groups had better quality of life scores than the CG (SMD - 1.44, 95% CI: [5.60, 8.27], P <.00001, I2 = 93%) ( Supplementary Figure 6 ).
3.5. Subgroup analyses
Analyses of subgroups including shoulder function, anxiety, depression, fatigue, sleep quality, and quality of life scores were performed in accordance with the intervention country (outside China or not) and duration of the intervention (weeks).
3.5.1. Intervention country (China or not in China)
In terms of depression, obvious differences were observed in the SMDs between studies performed in China (70, 90, 102) (P=.002) and studies performed outside of China (96) (P = .67). The Tai Chi and Baduanjin interventions had a significant effect in studies performed in China (SMD = - 1.71, 95% CI: - 2.80 to - 0.62, P = .002) (see Supplementary Figure 7 ). For sleep quality, obvious differences were observed in the SMDs between studies performed in China (82, 102) (P = .01) and studies performed outside of China (96)(P = .49). The Tai Chi and Baduanjin interventions had a significant effect in studies performed in China (SMD = 一1.65, 95% CI: 一2.95 to 一0.35, P = .01) (see Supplementary Figure 8 ). For quality of life, obvious differences were observed in the SMDs between studies performed in China (70, 82, 91, 92, 94, 95, 99) (P <.00001) and studies performed outside of China (94, 97) (P = .23). The Tai Chi and Baduanjin interventions had a significant effect in studies performed in China (SMD = 7.51, 95% CI: 6.09 to 8.93, P <.00001) ( Supplementary Figure 9 ).
3.5.2. Intervention duration (weeks)
In terms of shoulder function, 4 out of the 5 studies indicated a significant effect (91, 92, 94, 95) with an intervention period of ≥10 weeks [SMD = 7.63, 95% CI: (6.59 to 8.67), P <.0001]. For the remaining study (100), the pooled effect was SMD = 1.40 (95% CI: −3.31, 6.11; P = .56) within the intervention period. In contrast to the control treatment, Tai Chi and Baduanjin had different effects on shoulder function based on the intervention duration. There was a significant difference in shoulder function in interventions that lasted for longer than 10 weeks ( Supplementary Figure 10 ).
Among the 4 studies on anxiety indicators, 1 study (93) with an intervention duration > 12 weeks reported a pooled effect of SMD = −4.64 [95% CI: (−6.59 to −2.69)], P <.00001]. For 3 studies (70, 89, 90) in which the intervention duration was ≤ 12 weeks, the pooled effect was SMD = −1.51 [95% CI (−2.577, −0.45), P = .005]. An intervention period of more than 8 weeks was found to have an obvious effect on reducing breast cancer patients’ levels of anxiety ( Supplementary Figure 11 ).
Of the 4 studies regarding depression indicators, 3 studies (70, 90, 96) had an intervention duration of > 8 weeks and reported a pooled effect of SMD = −1.53 [95% CI: (−2.59 to −0.47), P = .005]. For 1 study (102) in which the intervention cycle was ≤ 8 weeks, the pooled effect was SMD = −0.20 [95% CI (−3.98, 3.58), P = .006]. An intervention period of more than 8 weeks was found to have an obvious effect on reducing breast cancer patients’ levels of depression ( Supplementary Figure 12 ).
Among the 4 studies reporting fatigue indicators, 3 (70, 96, 98) had an intervention duration > 8 weeks and reported a pooled effect of SMD = −1.30 [95% CI: (−1.88 to −0.73), P <.00001]. For 1 study (102) in which the intervention cycle was ≤ 8 weeks, the pooled effect was SMD = −0.20 [95% CI (−1.19, 0.79), P = .69]. An intervention period of more than 8 weeks was found to have an obvious effect on reducing breast cancer patients’ levels of fatigue ( Supplementary Figure 13 ).
Among the 3 studies regarding sleep quality indicators, 2 (82, 96) had an intervention duration > 8 weeks and reported a pooled effect of SMD = −2.88 [95% CI: (−4.39 to −1.38), P = .0002]. For 1 study (102) in which the intervention cycle was ≤ 8 weeks, the pooled effect was SMD = 0.40 [95% CI (−1.30, 2.10), P = .65]. An intervention period of more than 8 weeks was found to have increase sleep quality among breast cancer patients ( Supplementary Figure 14 ).
Among the 9 studies reporting quality of life indicators, 1 (150) had an intervention duration > 12 weeks and had a pooled effect of SMD = −7.78 [95% CI: (−17.89 to 2.33), P = .13]. For 8 studies (70, 82, 92, 94, 95, 97–99) in which the intervention cycle was ≤ 12 weeks, the pooled effect SMD = 7.20 [95% CI (5.85, 8.54), P <.00001]. An intervention period of more than 8 weeks was found to have an obvious effect on increasing quality of life among breast cancer patients ( Supplementary Figure 15 ).
3.6. Sensitivity analysis
In the sensitivity analysis ( Table 3 ), the study of Li et al. (90) was excluded, and we observed an obvious change in heterogeneity, which decreased from 91% to 0%. Similarly, when excluding the study by Liao et al. (2022) (82), the heterogeneity level decreased to 0%. Based on these observations, we hypothesize that the outcomes of depression and sleep quality indicators may be the primary sources of heterogeneity in this study. Other potential reasons for heterogeneity include differences in patient populations, inconsistencies in clinical indicators between domestic and overseas studies, and specific treatment methods. The patient characteristics, specific treatment modalities, and applied clinical indicators across the literature are as follows: Li et al. (90), Shanxi (China), aged 37-57 years, breast cancer patients, Baduanjin intervention, shoulder function, anxiety, depression; Liao et al. (2022) (82), Guangzhou (China), aged 46-60 years, breast cancer patients, Baduanjin intervention, sleep quality, and quality of life. The factors mentioned above are all potential sources of heterogeneity in this study.
Table 3.
Sensitivity analysis for depression and sleep quality indicators.
| After excluding the reference | The Result of Heterogeneity: | |||
|---|---|---|---|---|
| Chi² | df | P | I² | |
| Chen et al., 2013 (102) CES-D | 9.03 | 2 | =0.01 | 78% |
| Larkey et al., 2015 (96) BDI | 7.40 | 2 | =0.02 | 73% |
| Li et al., 2017 (90) SDS | 1.81 | 2 | =0.40 | 0% |
| Wei et al., 2022 (70) HADS | 9.48 | 2 | =0.009 | 79% |
| Chen et al., 2013 (102) PSQI | 5.75 | 1 | =0.02 | 83% |
| Larkey et al., 2015 (96) PSQI | 13.35 | 1 | =0.0003 | 93% |
| Liao et al., 2022 (82) PSQI | 0.69 | 1 | =0.41 | 0% |
Sensitivity analysis for depression.
3.7. Publication bias
We conducted a thorough analysis of the funnel plots for cognitive function ( Supplementary Figure 13 ), shoulder function ( Supplementary Figure 14 ), anxiety ( Supplementary Figure 15 ), depression ( Supplementary Figure 16 ), fatigue ( Supplementary Figure 17 ), sleep quality ( Supplementary Figure 18 ), and quality of life ( Supplementary Figure 19 ). The plots were found to be symmetrical, strongly suggesting the absence of publication bias. Furthermore, the P values exceeded.04, indicating a lack of significant publication bias. Additionally, Egger’s regression test (P=.018) and Begg’s test (P=.02) confirmed the absence of publication bias. All in all, it seems challenging to detect, let alone define, publication bias in the present context because the study conditions and designs appear relatively heterogeneous.
4. Discussion
4.1. Principal findings
This study systematically evaluated the efficacy of Tai Chi and Baduanjin in breast cancer patients, drawing upon data from 16 studies with a total of 1247 participants. Our findings revealed that Tai Chi and Baduanjin significantly improved cognitive function (SMD = 1.00), shoulder function scores (SMD = 7.34), sleep quality (SMD = -1.44) and quality of life (SMD = 6.94) and reduced depression (SMD = -1.44), anxiety (SMD = -2.22) and fatigue scores (SMD = -1.02). These findings suggest that Tai Chi and Baduanjin are highly effective alternatives for treating breast cancer patients. However, caution is advised in interpreting these results because of the statistical heterogeneity mentioned in the research. To investigate the impact of individual studies on overall risk, sensitivity analysis was conducted to identify the main sources of heterogeneity. Notably, there were large variations in sample size (range: 11–100), intervention type, intervention duration (range: 5–24 weeks), weekly intervention hours (range: 20–90 min/week), and type of control group. (e.g., regular intervention, routine rehabilitation training, waiting list, sham qigong, usual care, no intervention). We acknowledge that cultural background, measurement instruments, and other confounding factors may have contributed to the heterogeneity observed in this systematic review. To the best of our knowledge, this is the first meta-analysis and systematic review to evaluate the effectiveness of Tai Chi and Baduanjin therapy on seven outcome indicators in breast cancer patients. In our study, Tai Chi and Baduanjin therapy significantly improved cognitive function and shoulder function and alleviated depression, anxiety, fatigue and quality of life symptoms.
4.2. comparison with previous work
Previous studies have explored the effects of Tai Chi and Baduanjin in cognitive ability (69, 70), alleviating shoulder function impairment (55, 59) and improving mental health problems (72, 73) in breast cancer patients. However, previous studies have reported inconsistent findings regarding the effects of Tai Chi and Baduanjin therapy on improving cognitive function (70), shoulder function (71), reducing falls (75), improving stress and mental health problems (81), improving fatigue, sleeping quality, depression symptom (70) in breast cancer patients. To the best of our knowledge, this systematic review included recent literature (2013-2023) and is the first systematic review and meta-analysis to evaluate examined the effect of Tai Chi and Baduanjin of seven outcome indicators in breast cancer patients. In our study, Tai Chi and Baduanjin were found to significantly alleviate anxiety, depression, and sleep problems and improve cognitive impairment, shoulder function impairment, fatigue, and quality of life (QoL). This systematic review also divided subgroup analysis of the weeks and continental plates, which was not available in the previous systematic review.
4.3. Limitations
This study has some limitations that should not be ignored. First, given the nature of systematic reviews, a clear causal relationship cannot be established, as Tai Chi can but only play a supportive role that is preventive and somewhat curative but always in conjunction with other therapeutic methods. Additionally, stress outcome indicators had some impact on the psychological health of breast cancer patients. However, as the only study reported these indicators, a comprehensive comparison could not be made; thus, these indicators were not included in this review. Third, due to the design restrictions in the study, the randomization and blinding methods of the included studies were seldom described in detail. Only five (82, 91, 97, 98, 101) studies were found to detail the randomization method. In contrast, randomization was only mentioned in other studies, and no explanation of the method used was provided. Among them, double-blinding was only implemented in three (96, 97, 101) studies.
4.4. Implications
Complementary therapies, particularly mind-body practice, are interventions with great effectiveness for managing treatment side effects and breast cancer symptoms and side effects of complementary therapies (113). Tai Chi (114) and Baduanjin (115) are therapies that complement each other and integrate physical and psychological components. These ancient Chinese mind-body exercises combine breathing exercises, meditation, relaxation techniques, and physical movement (116). Tai Chi and Qigong are two of the most popular traditional aerobic exercises used to treat breast cancer (42). The most common cancers diagnosed among Chinese females was breast cancer, with an, age-standardized incidence rate(ASIR) of 39.1 per 100,000 (117). Of all countries, China faces the largest economic cost of cancers at INT $6.1 trillion, followed by the US (INT $5.3 trillion) and India (INT $1.4 trillion) (118). Our findings have also found that Tai Chi and Baduanjin can have a positive impact on increasing in cognitive ability, shoulder joint function, quality of life, sleep quality and decreasing in anxiety, depression, fatigue symptom among breast cancer patients. With this in mind, we suggest that nursing home caregivers, social workers, and psychologists consider using Tai Chi and Baduanjin in their work, and collaborate with Tai Chi and Baduanjin professionals, it will both physical and psychological health improvements to the breast cancer patients and reduce the financial burden on our country at the same time.
5. Outlook
In the future, more research is needed to improve participant motivation, reduce dropout rates, and sustain the benefits of Tai Chi and Baduanjin therapy. Given the study limitations, subgroup analyses for intervention types were not feasible. Therefore, it is essential to conduct in depth, stratified comparisons and discussions of different types of interventions. To validate the effectiveness of Tai Chi and Baduanjin therapy for breast cancer patients, researchers should conduct high-quality studies with large sample sizes. All in all, we should recognize that this research is good to stimulate future research on the many possibilities of Tai Chi and its potential therapeutic benefits as a holistic and preventive approach to a healthy lifestyle, as compared to the more analytical and curative focus in Western discussions. And the take-home message is that Tai Chi is a form of mental relaxation capable of restoring attention and inner resources (25), which is movement-oriented, as it focuses on forms of gentle motion particularly beneficial for older individuals or patients aiding the healing process. Finally, it is a social act that promotes the feeling of togetherness by bringing people together in the true sense of the word (39).
6. Conclusion
Overall, Tai Chi and Baduanjin therapy may be associated with an increase in quality of life among breast cancer patients. However, a definitive conclusion could not be reached on the safety and effectiveness of Tai Chi and Baduanjin therapy for improving cognitive ability, shoulder joint abilities, and mental health among breast cancer patients. The overall quality of evidence across all meta-analyses was found to be very low. This was primarily due to concerns about the overall bias within most included studies, high evidence heterogeneity, and reported effect size imprecision. Given these limitations, psychologists, social workers, psychiatrists, and patients should approach Tai Chi and Baduanjin therapy as complementary treatments rather than as replacements for existing interventions. To more robustly evaluate the effectiveness and safety of Tai Chi and Baduanjin for improving specific cognitive abilities, social well-being, and pain among individuals of different age groups, regardless of cognitive status, further reviews and additional studies are needed. It is essential to assess the impact, safety profile, and long-term effects of this therapy to determine its potential as a sustainable and effective intervention in various settings.
Acknowledgments
The authors (XZ, YT, YC and ZZ) have confirmed the submission of this manuscript, the key message of the manuscript, and the uniqueness of the study. We would like to thank the reviewers for their helpful remarks.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by funding from the Shenzhen Philosophy and social science planning project (SZ2024D007) and Shenzhen University-Lingnan University Joint Research Programme (SZU-LU Joint Research Programme) (2023004).
Data availability statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.
Author contributions
CY: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ZX: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. TY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. ZZ: Data curation, Formal analysis, Methodology, Resources, Writing – original draft.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1434087/full#supplementary-material
References
- 1. Jiang J, Jiang S, Ahumada-Canale A, Chen Z, Si L, Jiang Y, et al. Breast cancer screening should embrace precision medicine: evidence by reviewing economic evaluations in china. Adv Ther. (2023) 40(4):1393–417. doi: 10.1007/s12325-023-02450-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin. (2021) 71(3):209–49. doi: 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 3. Azadnajafabad S, Saeedi Moghaddam S, Mohammadi E, Delazar S, Rashedi S, Baradaran HR. Patterns of better breast cancer care in countries with higher human development index and healthcare expenditure: Insights from GLOBOCAN 2020. Front Public Health. (2023) 11:1137286. doi: 10.3389/fpubh.2023.1137286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hashemi S-M, Rafiemanesh H, Aghamohammadi T, Badakhsh M, Amirshahi M, Sari M, et al. Prevalence of anxiety among breast cancer patients: a systematic review and meta-analysis. Breast Cancer. (2020) 27:166–78. doi: 10.1007/s12282-019-01031-9 [DOI] [PubMed] [Google Scholar]
- 5. Wang X, Wang N, Zhong L, Wang S, Zheng Y, Yang B, et al. Prognostic value of depression and anxiety on breast cancer recurrence and mortality: a systematic review and meta-analysis of 282,203 patients. Mol Psychiatry. (2020) 25(12):3186–97. doi: 10.1038/s41380-020-00865-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pilevarzadeh M, Amirshahi M, Afsargharehbagh R, Rafiemanesh H, Hashemi S-M, Balouchi A. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res Treat. (2019) 176:519–33. doi: 10.1007/s10549-019-05271-3 [DOI] [PubMed] [Google Scholar]
- 7. Biering K, Frydenberg M, Pappot H, Hjollund NH. The long-term course of fatigue following breast cancer diagnosis. J Patient-Reported Outcomes. (2020) 4:1–11. doi: 10.1186/s41687-020-00187-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ruiz-Casado A, Alvarez-Bustos A, de Pedro CG, Mendez-Otero M, Romero-Elias M. Cancer-related fatigue in breast cancer survivors: a review. Clin Breast Cancer. (2021) 21(1):10–25. doi: 10.1016/j.clbc.2020.07.011 [DOI] [PubMed] [Google Scholar]
- 9. Son H-M, Park EY, Kim E-J. Cancer-related fatigue of breast cancer survivors: qualitative research. Asian Oncol Nurs. (2020) 20(4):141–9. doi: 10.5388/aon.2020.20.4.141 [DOI] [Google Scholar]
- 10. Dijkshoorn AB, van Stralen HE, Sloots M, Schagen SB, Visser-Meily JM, Schepers VP. Prevalence of cognitive impairment and change in patients with breast cancer: a systematic review of longitudinal studies. Psycho-Oncology. (2021) 30(5):635–48. doi: 10.1002/pon.5623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vardy JL, Stouten-Kemperman MM, Pond G, Booth CM, Rourke SB, Dhillon HM, et al. A mechanistic cohort study evaluating cognitive impairment in women treated for breast cancer. Brain Imaging Behav. (2019) 13:15–26. doi: 10.1007/s11682-017-9728-5 [DOI] [PubMed] [Google Scholar]
- 12. Kikuuchi M, Akezaki Y, Nakata E, Yamashita N, Tominaga R, Kurokawa H, et al. Risk factors of impairment of shoulder function after axillary dissection for breast cancer. Supportive Care Cancer. (2021) 29:771–8. doi: 10.1007/s00520-020-05533-7 [DOI] [PubMed] [Google Scholar]
- 13. Lang AE, Kim SY, Dickerson CR, Milosavljevic S. Measurement of objective shoulder function following breast cancer surgery: A scoping review. Phys Ther Rev. (2020) 25(4):253–68. doi: 10.1080/10833196.2020.1851439 [DOI] [Google Scholar]
- 14. Kwak A, Jacobs J, Haggett D, Jimenez R, Peppercorn J. Evaluation and management of insomnia in women with breast cancer. Breast Cancer Res Treat. (2020) 181:269–77. doi: 10.1007/s10549-020-05635-0 [DOI] [PubMed] [Google Scholar]
- 15. Mogavero MP, DelRosso LM, Fanfulla F, Bruni O, Ferri R. Sleep disorders and cancer: State of the art and future perspectives. Sleep Med Rev. (2021) 56:101409. doi: 10.1016/j.smrv.2020.101409 [DOI] [PubMed] [Google Scholar]
- 16. Mokhatri-Hesari P, Montazeri A. Health-related quality of life in breast cancer patients: review of reviews from 2008 to 2018. Health Qual Life Outcomes. (2020) 18:1–25. doi: 10.1186/s12955-020-01591-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schmidt ME, Scherer S, Wiskemann J, Steindorf K. Return to work after breast cancer: The role of treatment-related side effects and potential impact on quality of life. Eur J Cancer Care. (2019) 28(4):e13051. doi: 10.1111/ecc.13051 [DOI] [PubMed] [Google Scholar]
- 18. Kerr AJ, Dodwell D, McGale P, Holt F, Duane F, Mannu G, et al. Adjuvant and neoadjuvant breast cancer treatments: A systematic review of their effects on mortality. Cancer Treat Rev. (2022) 105:102375. doi: 10.1016/j.ctrv.2022.102375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Leysen L, Lahousse A, Nijs J, Adriaenssens N, Mairesse O, Ivakhnov S, et al. Prevalence and risk factors of sleep disturbances in breast cancersurvivors: systematic review and meta-analyses. Supportive Care Cancer. (2019) 27:4401–33. doi: 10.1007/s00520-019-04936-5 [DOI] [PubMed] [Google Scholar]
- 20. Nomura K, Sakawaki E, Sakawaki S, Yamaoka A, Aisaka W, Okamoto H, et al. Non-surgical treatment of tetanus infection associated with breast cancer skin ulcer: a case report and literature review. BMC Infect Dis. (2021) 21:1–6. doi: 10.1186/s12879-020-05739-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yabe S, Nakagawa T, Oda G, Ishiba T, Aruga T, Fujioka T, et al. Association between skin flap necrosis and sarcopenia in patients who underwent total mastectomy. Asian J Surg. (2021) 44(2):465–70. doi: 10.1016/j.asjsur.2020.11.001 [DOI] [PubMed] [Google Scholar]
- 22. Khan JS, Ladha KS, Abdallah F, Clarke H. Treating persistent pain after breast cancer surgery. Drugs. (2020) 80(1):23–31. doi: 10.1007/s40265-019-01227-5 [DOI] [PubMed] [Google Scholar]
- 23. Riis M. Modern surgical treatment of breast cancer. Ann Med Surg. (2020) 56:95–107. doi: 10.1016/j.amsu.2020.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li F, Liu S, Zhang F, Huang H. Moderating effects of self-efficacy and time pressure on the relationship between employee aging and work performance. Psychol Res Behav Manage. (2022) 2022:1043–54. doi: 10.2147/PRBM.S359624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schumann F, Steinborn MB, Kürten J, Cao L, Händel BF, Huestegge L. Restoration of attention by rest in a multitasking world: Theory, methodology, and empirical evidence. Front Psychol. (2022) 13:867978. doi: 10.3389/fpsyg.2022.867978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Parker SK, Ward MK, Fisher GG. Can high-quality jobs help workers learn new tricks? a multidisciplinary review of work design for cognition. Acad Manage Ann. (2021) 15(2):406–54. doi: 10.5465/annals.2019.0057 [DOI] [Google Scholar]
- 27. Pluta A, Rudawska A. The role of the employees' individual resources in the perception of the work overload. J Organizational Change Manage. (2021) 34(3):590–612. doi: 10.1108/JOCM-08-2020-0241 [DOI] [Google Scholar]
- 28. Nybergh L, Bergström G, Hellman T. Do work-and home-related demands and resources differ between women and men during return-to-work? a focus group study among employees with common mental disorders. BMC Public Health. (2020) 20:1–17. doi: 10.1186/s12889-020-10045-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Singh U, Ghadiri A, Weimar D, Prinz J. “Let’s have a break”: An experimental comparison of work-break interventions and their impact on performance. J Business Res. (2020) 112:128–35. doi: 10.1016/j.jbusres.2020.03.008 [DOI] [Google Scholar]
- 30. Loch F, Hof zum Berge A, Ferrauti A, Meyer T, Pfeiffer M, Kellmann M. Acute effects of mental recovery strategies after a mentally fatiguing task. Front Psychol. (2020) 11:558856. doi: 10.3389/fpsyg.2020.558856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fancourt D, Aughterson H, Finn S, Walker E, Steptoe A. How leisure activities affect health: a narrative review and multi-level theoretical framework of mechanisms of action. Lancet Psychiatry. (2021) 8(4):329–39. doi: 10.1016/S2215-0366(20)30384-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Harrington A, Dunne JD. When mindfulness is therapy: Ethical qualms, historical perspectives. Am Psychol. (2015) 70(7):621. doi: 10.1037/a0039460 [DOI] [PubMed] [Google Scholar]
- 33. Vieten C, Wahbeh H, Cahn BR, MacLean K, Estrada M, Mills P, et al. Future directions in meditation research: Recommendations for expanding the field of contemplative science. PloS One. (2018) 13(11):e0205740. doi: 10.1371/journal.pone.0205740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pinnock R, Ritchie D, Gallagher S, Henning MA, Webster CS. The efficacy of mindful practice in improving diagnosis in healthcare: a systematic review and evidence synthesis. Adv Health Sci Educ. (2021) 26(3):785–809. doi: 10.1007/s10459-020-10022-x [DOI] [PubMed] [Google Scholar]
- 35. Garland EL. Mindful positive emotion regulation as a treatment for addiction: From hedonic pleasure to self-transcendent meaning. Curr Opin Behav Sci. (2021) 39:168–77. doi: 10.1016/j.cobeha.2021.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jinich-Diamant A, Garland E, Baumgartner J, Gonzalez N, Riegner G, Birenbaum J, et al. Neurophysiological mechanisms supporting mindfulness meditation–based pain relief: An updated review. Curr Pain Headache Rep. (2020) 24:1–10. doi: 10.1007/s11916-020-00890-8 [DOI] [PubMed] [Google Scholar]
- 37. Yang GY, Sabag A, Hao WL, Zhang LN, Jia MX, Dai N, et al. Tai Chi for health and well-being: a bibliometric analysis of published clinical studies between 2010 and 2020. Complement Ther Med. (2021) 60:102748. doi: 10.1016/j.ctim.2021.102748 [DOI] [PubMed] [Google Scholar]
- 38. Zhou D-H. Comparative therapeutic exercise: East and west. Am J Chin Med. (1978) 6(04):263–71. doi: 10.1142/S0147291778000356 [DOI] [Google Scholar]
- 39. Nisbett RE, Peng K, Choi I, Norenzayan A. Culture and systems of thought: holistic versus analytic cognition. psychol Rev. (2001) 108(2):291. doi: 10.1037/0033-295X.108.2.291 [DOI] [PubMed] [Google Scholar]
- 40. Leung KCW, Yang YJ, Hui SSC, Woo J. Mind-body health benefits of traditional chinese qigong on women: a systematic review of randomized controlled trials. J Evid Based Complementary Altern Med. (2021) 2021:7443498. doi: 10.1155/2021/7443498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Qi F, Soh KG, Nasiruddin NJM, Leong OS, He S, Liu H. Effect of taichi chuan on health-related physical fitness in adults: a systematic review with meta-analysis. Complementary Therapies Med. (2023) 77:102971. doi: 10.1016/j.ctim.2023.102971 [DOI] [PubMed] [Google Scholar]
- 42. Liu F, Cui J, Liu X, Chen KW, Chen X, Li R. The effect of tai chi and qigong exercise on depression and anxiety of individuals with substance use disorders: a systematic review and meta-analysis. BMC Complementary Med Therapies. (2020) 20:1–11. doi: 10.1186/s12906-020-02967-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Soltero EG, James DL, Han S, Larkey LK. The impact of a meditative movement practice intervention on short-and long-term changes in physical activity among breast cancer survivors. J Cancer Survivorship. (2023), 1–9. doi: 10.1007/s11764-023-01430-0 [DOI] [PubMed] [Google Scholar]
- 44. Chen L-Z, Dai A-Y, Yao Y, Si R, Hu Z, Ge L, et al. Effects of 8-week tai chi chuan practice on mindfulness level. Mindfulness. (2021) 12:1534–41. doi: 10.1007/s12671-021-01622-8 [DOI] [Google Scholar]
- 45. Choo YT, Jiang Y, Hong J, Wang W. Effectiveness of tai chi on quality of life, depressive symptoms and physical function among community-dwelling older adults with chronic disease: A systematic review and meta-analysis. Int J Nurs Stud. (2020) 111:103737. doi: 10.1016/j.ijnurstu.2020.103737 [DOI] [PubMed] [Google Scholar]
- 46. Leung K-CW, Yang Y-J, Hui SS-C, Woo J. Mind-body health benefits of traditional Chinese Qigong on women: a systematic review of randomized controlled trials. Evidence-Based complementary Altern Med. (2021) 2021:1–16. doi: 10.1155/2021/7443498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gong X, Rong G, Wang Z, Zhang A, Li X, Wang L. Baduanjin exercise for patients with breast cancer: A systematic review and meta-analysis. Complementary Therapies Med. (2022) 71:102886. doi: 10.1016/j.ctim.2022.102886 [DOI] [PubMed] [Google Scholar]
- 48. Liu Q, Zhan L, Yan X, Li Y, Wei S. Clinical effects of baduanjin qigong exercise on cancer-related fatigue: A systematic review and meta-analysis. Eur J Integr Med. (2023) 63:102283. doi: 10.1016/j.eujim.2023.102283 [DOI] [Google Scholar]
- 49. Yin J, Tang L, Dishman RK. The efficacy of Qigong practice for cancer-related fatigue: A systematic review and meta-analysis of randomized controlled trials. Ment Health Phys Act. (2020) 19:100347. doi: 10.1016/j.mhpa.2020.100347 [DOI] [Google Scholar]
- 50. Kong L, Ren J, Fang S, He T, Zhou X, Fang M. Effects of traditional Chinese mind-body exercise-baduanjin for type 2 diabetes on psychological well-being: A systematic review and meta-analysis. Front Public Health. (2022) 10:923411. doi: 10.3389/fpubh.2022.923411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mei B, Yuan L, Shu Y. Quantitative evidence of the effect of Baduanjin exercise on quality of life and cardiac function in adults with chronic heart failure. Complement Ther Clin Pract. (2023) 53:101775. doi: 10.1016/j.ctcp.2023.101775 [DOI] [PubMed] [Google Scholar]
- 52. Zhu R, Niu Y, Xu H, Wang S, Mao J, Lei Y, et al. Traditional chinese exercises for cardiovascular diseases: A bibliometric analysis. Perceptual Motor Skills. (2024) 131:514–36. doi: 10.1177/00315125241230599 [DOI] [PubMed] [Google Scholar]
- 53. Deng J, Liu X, Wang Y, Fan J, Yang L, Duan J, et al. The therapeutic effect of taijiquan combined with acupoint pressing on the treatment of anxiety insomnia in college students: A study protocol for a randomized controlled trial. Front Psychiatry. (2022) 13:961513. doi: 10.3389/fpsyt.2022.961513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Luo X-C, Liu J, Fu J, Yin H-Y, Shen L, Liu M-L, et al. Effect of tai chi chuan in breast cancer patients: a systematic review and meta-analysis. Front Oncol. (2020) 10:607. doi: 10.3389/fonc.2020.00607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zhang P, Li Z, Yang Q, Zhou J, Ma X. Effects of taijiquan and qigong exercises on depression and anxiety levels in patients with substance use disorders: a systematic review and meta-analysis. Sports Med Health Sci. (2022) 4(2):85–94. doi: 10.1016/j.smhs.2021.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Liu L, Tan H, Yu S, Yin H, Baxter GD. The effectiveness of tai chi in breast cancer patients: A systematic review and meta-analysis. Complement Ther Clin Pract. (2020) 38:101078. doi: 10.1016/j.ctcp.2019.101078 [DOI] [PubMed] [Google Scholar]
- 57. Li K, Walczak-Kozłowska T, Lipowski M, Li J, Krokosz D, Su Y, et al. The effect of the baduanjin exercise on COVID-19-related anxiety, psychological well-being and lower back pain of college students during the pandemic. BMC Sports Science Med Rehabil. (2022) 14(1):102. doi: 10.1186/s13102-022-00493-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Li W, You F, Wang Q, Shen Y, Wang J, Guo J. Effects of Tai Chi Chuan training on the QoL and psychological well-being in female patients with breast cancer: a systematic review of randomized controlled trials. Front Oncol. (2023) 13:1143674. doi: 10.3389/fonc.2023.1143674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Yao Y, Ge L, Yu Q, Du X, Zhang X, Taylor-Piliae R, et al. The effect of Tai Chi Chuan on emotional health: potential mechanisms and prefrontal cortex hypothesis. Evid Based Complement Alternat Med. (2021) 2021:5549006. doi: 10.1155/2021/5549006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ye XX, Ren ZY, Vafaei S, Zhang JM, Song Y, Wang YX, et al. Effectiveness of baduanjin exercise on quality of life and psychological health in postoperative patients with breast cancer: A systematic review and meta-analysis. Integr Cancer Ther. (2022) 21:15347354221104092. doi: 10.1177/15347354221104092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Momenimovahed Z, Salehiniya H. Epidemiological characteristics of and risk factors for breast cancer in the world. Breast Cancer (Dove Med Press). (2019) 11:151–64. doi: 10.2147/bctt.S176070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Pizzato M, Carioli G, Rosso S, Zanetti R, La Vecchia C. The impact of selected risk factors among breast cancer molecular subtypes: a case-only study. Breast Cancer Res Treat. (2020) 184(1):213–20. doi: 10.1007/s10549-020-05820-1 [DOI] [PubMed] [Google Scholar]
- 63. Figueroa JD, Davis Lynn BC, Edusei L, Titiloye N, Adjei E, Clegg-Lamptey JN, et al. Reproductive factors and risk of breast cancer by tumor subtypes among ghanaian women: A population-based case-control study. Int J Cancer. (2020) 147(6):1535–47. doi: 10.1002/ijc.32929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Pu H, Wen X, Luo D, Guo Z. Regulation of progesterone receptor expression in endometriosis, endometrial cancer, and breast cancer by estrogen, polymorphisms, transcription factors, epigenetic alterations, and ubiquitin-proteasome system. J Steroid Biochem Mol Biol. (2023) 227:106199. doi: 10.1016/j.jsbmb.2022.106199 [DOI] [PubMed] [Google Scholar]
- 65. Lofterød T, Frydenberg H, Flote V, Eggen AE, McTiernan A, Mortensen ES, et al. Exploring the effects of lifestyle on breast cancer risk, age at diagnosis, and survival: the EBBA-life study. Breast Cancer Res Treat. (2020) 182(1):215–27. doi: 10.1007/s10549-020-05679-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Dong J, Wang D, Li H, Ni H. Effects of different chinese traditional exercises on sleep quality and mental health of adults: systematic review and meta-analysis. Sleep Breath. (2024) 28(1):29–39. doi: 10.1007/s11325-023-02881-6 [DOI] [PubMed] [Google Scholar]
- 67. Salam A, Woodman A, Chu A, Al-Jamea LH, Islam M, Sagher M, et al. Effect of post-diagnosis exercise on depression symptoms, physical functioning and mortality in breast cancer survivors: A systematic review and meta-analysis of randomized control trials. Cancer Epidemiol. (2022) 77:102111. doi: 10.1016/j.canep.2022.102111 [DOI] [PubMed] [Google Scholar]
- 68. Myers JS, Mitchell M, Krigel S, Steinhoff A, Boyce-White A, Van Goethem K, et al. Qigong intervention for breast cancer survivors with complaints of decreased cognitive function. Support Care Cancer. (2019) 27(4):1395–403. doi: 10.1007/s00520-018-4430-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Meng T, Hu SF, Cheng YQ, Ye MN, Wang B, Wu JJ, et al. Qigong for women with breast cancer: An updated systematic review and meta-analysis. Complement Ther Med. (2021) 60:102743. doi: 10.1016/j.ctim.2021.102743 [DOI] [PubMed] [Google Scholar]
- 70. Wei X, Yuan R, Yang J, Zheng W, Jin Y, Wang M, et al. Effects of baduanjin exercise on cognitive function and cancer-related symptoms in women with breast cancer receiving chemotherapy: a randomized controlled trial. Support Care Cancer. (2022) 30(7):6079–91. doi: 10.1007/s00520-022-07015-4 [DOI] [PubMed] [Google Scholar]
- 71. Fong SS, Ng SS, Lee H, Pang MY, Luk WS, Chung JW, et al. The effects of a 6-month Tai Chi Qigong training program on temporomandibular, cervical, and shoulder joint mobility and sleep problems in nasopharyngeal cancer survivors. Integr Cancer Therapies. (2015) 14(1):16–25. doi: 10.1177/1534735414556508 [DOI] [PubMed] [Google Scholar]
- 72. Luo X, Zhao M, Zhang Y, Zhang Y. Effects of baduanjin exercise on blood glucose, depression and anxiety among patients with type II diabetes and emotional disorders: A meta-analysis. Complement Ther Clin Pract. (2023) 50:101702. doi: 10.1016/j.ctcp.2022.101702 [DOI] [PubMed] [Google Scholar]
- 73. Ye M, Zheng Y, Xiong Z, Ye B, Zheng G. Baduanjin exercise ameliorates motor function in patients with post-stroke cognitive impairment: A randomized controlled trial. Complement Ther Clin Pract. (2022) 46:101506. doi: 10.1016/j.ctcp.2021.101506 [DOI] [PubMed] [Google Scholar]
- 74. Huang J, Liu H, Chen J, Cai X, Huang Y. The effectiveness of tai chi in patients with breast cancer: An overview of systematic reviews and meta-analyses. J Pain Symptom Manage. (2021) 61(5):1052–9. doi: 10.1016/j.jpainsymman.2020.10.007 [DOI] [PubMed] [Google Scholar]
- 75. Li C, Dong X, Yu L, Yuan K, Yi X, Shen Y, et al. The effects of qigong intervention based on the internet on quality of life and physical fitness in chinese postoperative breast cancer patients: a protocol of randomized controlled trial. Trials. (2023) 24(1):186. doi: 10.1186/s13063-023-07187-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Harbord R, Harris R, Sterne J. Updated tests for small-study effects in meta-analysis. Strata J. (2009) 9:197–210. doi: 10.1177/1536867X0900900202 [DOI] [Google Scholar]
- 77. Gomaa S, West C, Lopez AM, Zhan T, Schnoll M, Abu-Khalaf M, et al. A telehealth-delivered tai chi intervention (TaiChi4Joint) for managing aromatase inhibitor-induced arthralgia in patients with breast cancer during COVID-19: Longitudinal pilot study. JMIR Form Res. (2022) 6(6):e34995. doi: 10.2196/34995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Yao LQ, Kwok SWH, Tan JB, Wang T, Liu XL, Bressington D, et al. The effect of an evidence-based tai chi intervention on the fatigue-sleep disturbance-depression symptom cluster in breast cancer patients: A preliminary randomised controlled trial. Eur J Oncol Nurs. (2022) 61:102202. doi: 10.1016/j.ejon.2022.102202 [DOI] [PubMed] [Google Scholar]
- 79. Zhang JY, Li SS, Meng LN, Zhou YQ. Effectiveness of a nurse-led mindfulness-based tai chi chuan (MTCC) program on posttraumatic growth and perceived stress and anxiety of breast cancer survivors. Eur J Psychotraumatol. (2022) 13(1):2023314. doi: 10.1080/20008198.2021.2023314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Li H, Chen J, Xu G, Duan Y, Huang D, Tang C, et al. The effect of tai chi for improving sleep quality: A systematic review and meta-analysis. J Affect Disord. (2020) 274:1102–12. doi: 10.1016/j.jad.2020.05.076 [DOI] [PubMed] [Google Scholar]
- 81. Gao Z, Ryu S, Chen Y. Effects of tai chi app and facebook health education programs on breast cancer survivors' stress and quality of life in the era of pandemic. Complement Ther Clin Pract. (2022) 48:101621. doi: 10.1016/j.ctcp.2022.101621 [DOI] [PubMed] [Google Scholar]
- 82. Liao J, Chen Y, Cai L, Wang K, Wu S, Wu L, et al. Baduanjin's impact on quality of life and sleep quality in breast cancer survivors receiving aromatase inhibitor therapy: a randomized controlled trial. Front Oncol. (2022) 12:807531. doi: 10.3389/fonc.2022.807531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Hu Y, Xie YD, Xu X, Liu Y, Zhang C, Wang H. Facilitators and barriers of attending BaDuanJin experienced by breast cancer survivors during chemotherapy. Physiother Theory Pract. (2024) 40(3):528–43. doi: 10.1080/09593985.2022.2135977 [DOI] [PubMed] [Google Scholar]
- 84. Kuo C-C, Wang C-C, Chang W-L, Liao T-C, Chen P-E, Tung T-H. Clinical effects of baduanjin qigong exercise on cancer patients: a systematic review and meta-analysis on randomized controlled trials. Evidence-Based Complementary Altern Med. (2021) 2021:1–10. doi: 10.1155/2021/6651238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Tugwell P, Tovey D, Cuella-Garcia CA. “Never let a crisis go to waste”: how science has responded to the COVID-19 pandemic. J Clin Epidemiol. (2021) 131:A5–6. doi: 10.1016/j.jclinepi.2021.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. (2008). doi: 10.1002/9780470712184. [DOI] [Google Scholar]
- 87. Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Bmj. (2014) 348:g1687. doi: 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 88. Cooper HE, Camic PM, Long DL, Panter A, Rindskopf DE, Sher KJ. APA handbook of research methods in psychology, vol 2: Research designs: Quantitative, qualitative, neuropsychological, and biological. American Psychological Association; (2012). doi: 10.1037/13620-000 [DOI] [Google Scholar]
- 89. Han Y, Wang Q, Luo D, Xue J. Effects of ba duan jin training on anxiety and serum-related anxiety proteins in patients who were after breast cancer surgery. J Nursing. (2017) 032(008):42–4. [Google Scholar]
- 90. Li Q, Wang L, Zhang X. Evaluation of the effect of Ba Duan Jin on the mental health and quality of life of patients with breast cancer during radiotherapy after radical surgery. General Care. (2017) 15(18):3. [Google Scholar]
- 91. Li Y, Li L, Wei W. Effect of Tai Chi Cloud Hands on functional rehabilitation of affected limbs in patients who were after breast cancer surgery. Fujian Trad Chinese Med. (2013) 5:57–8. [Google Scholar]
- 92. Lv F, Yu Y, Liang D, Li Z, You W, Zhang B. Effects of Ba Duan Jin and Tai Chi exercises on the quality of life of patients who were with breast cancer after surgery. J Wuhan Instit Phys Educ. (2015) 49(7):80–3. [Google Scholar]
- 93. Wang H. The efficacy of Tai Chi to breast cancer patients on anxiety symptom. Chin Modern Nursing J. (2015) 28:3386–8. [Google Scholar]
- 94. Wang H, Dai S, Hu M, Yu H, Liu S. Effect of Tai Chi on shoulder joint function and quality of life in patients who were after breast cancer surgery. N Knowledge Med. (2016) 26(3):231–3. [Google Scholar]
- 95. Yang Y, Wu F. Effect of traditional Chinese medicine rehabilitation therapy combined with Ba Duan Jin exercise on patients who were after breast cancer surgery. J Guangxi Univ Trad Chin Med. (2023) 26(1):13–7. [Google Scholar]
- 96. Larkey LK, Roe DJ, Weihs KL, Jahnke R, Lopez AM, Rogers CE, et al. Randomized controlled trial of Qigong/Tai chi easy on cancer-related fatigue in breast cancer survivors. Ann Behav Med. (2015) 49(2):165–76. doi: 10.1007/s12160-014-9645-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Larkey LK, Roe DJ, Smith L, Millstine D. Exploratory outcome assessment of Qigong/Tai chi easy on breast cancer survivors. Complementary Therapies Med. (2016) 29:196–203. doi: 10.1016/j.ctim.2016.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Wang R, Huang X, Wu Y, Sun D. Efficacy of qigong exercise for treatment of fatigue: a systematic review and meta-analysis. Front Med. (2021) 8:684058. doi: 10.3389/fmed.2021.684058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Huang S-M, Tseng L-M, Chien L-Y, Tai C-J, Chen P-H, Hung CT, et al. Effects of non-sporting and sporting qigong on frailty and quality of life among breast cancer patients receiving chemotherapy. Eur J Oncol Nurs. (2016) 21:257–65. doi: 10.1016/j.ejon.2015.10.012 [DOI] [PubMed] [Google Scholar]
- 100. Fong SS, Ng SS, Luk W, Chung JW, Chung LM, Tsang WW, et al. Shoulder mobility, muscular strength, and quality of life in breast cancer survivors with and without tai chi qigong training. Evidence-Based complementary Altern Med. (2013) 2013:787169. doi: 10.1155/2013/787169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Loh SY, Lee SY, Murray L. The kuala lumpur qigong trial for women in the cancer survivorship phase-efficacy of a three-arm RCT to improve QOL. Asian Pacific J Cancer Prev. (2014) 15(19):8127–34. doi: 10.7314/APJCP.2014.15.19.8127 [DOI] [PubMed] [Google Scholar]
- 102. Chen Z, Meng Z, Milbury K, Bei W, Zhang Y, Thornton B, et al. Qigong improves quality of life in women undergoing radiotherapy for breast cancer: results of a randomized controlled trial. Cancer. (2013) 119(9):1690–8. doi: 10.1002/cncr.27904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Mohsina S, Gurushankari B, Niranjan R, Sureshkumar S, Sreenath G, Kate V. Assessment of the quality of randomized controlled trials in surgery using jadad score: Where do we stand? J Postgraduate Med. (2022) 68(4):207–12. doi: 10.4103/jpgm.JPGM_104_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21(11):1539–58. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 105. Begg CB, Berlin JA. Publication bias: a problem in interpreting medical data. J R Stat Soc Ser A: Stat Soc. (1988) 151(3):419–45. doi: 10.2307/2982993 [DOI] [Google Scholar]
- 106. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. (1997) 315(7109):629–34. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56(2):455–63. doi: 10.1111/j.0006-341x.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 108. Sterne JA, Becker BJ, Egger M. The funnel plot. In: Publication bias in meta-analysis: Prevention, assessment and adjustments. (2005). p. 73–98. doi: 10.1002/0470870168.ch5 [DOI] [Google Scholar]
- 109. Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Systematic Rev. (2019) 2019:ED000142. doi: 10.1002/14651858.ED000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Ivey C, Crum J. Choosing the right citation management tool: EndNote, mendeley, RefWorks, or zotero. J Med Library Association: JMLA. (2018) 106(3):399. doi: 10.5195/jmla.2018.468 [DOI] [Google Scholar]
- 111. Irwin MR, Olmstead R, Carrillo C, Sadeghi N, Nicassio P, Ganz PA, et al. Tai chi chih compared with cognitive behavioral therapy for the treatment of insomnia in survivors of breast cancer: a randomized, partially blinded, noninferiority trial. J Clin Oncol. (2017) 35(23):2656. doi: 10.1200/JCO.2016.71.0285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Cheng D, Wang X, Hu J, Lv Y, Feng H, Zhang Y, et al. Effect of tai chi and resistance training on cancer-related fatigue and quality of life in middle-aged and elderly cancer patients. Chin J Integr Med. (2021) 27:265–72. doi: 10.1007/s11655-021-3278-9 [DOI] [PubMed] [Google Scholar]
- 113. Casuso-Holgado MJ, Heredia-Rizo AM, Gonzalez-Garcia P, Muñoz-Fernández MJ, Martinez-Calderon J. Mind–body practices for cancer-related symptoms management: an overview of systematic reviews including one hundred twenty-nine meta-analyses. Supportive Care Cancer. (2022) 30(12):10335–57. doi: 10.1007/s00520-022-07426-3 [DOI] [PubMed] [Google Scholar]
- 114. Inoue K, Onishi K, Arao H. The effectiveness of complementary therapy as mind–body practice on quality of life among cancer survivors: a quasi-experimental study. Asia-Pacific J Oncol Nurs. (2021) 8(6):687–95. doi: 10.4103/apjon.apjon-2124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Osypiuk K, Kilgore K, Ligibel J, Vergara-Diaz G, Bonato P, Wayne PM. “Making peace with our bodies”: a qualitative analysis of breast cancer survivors' experiences with qigong mind–body exercise. J Altern Complementary Med. (2020) 26(9):827–34. doi: 10.1089/acm.2019.0406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Osypiuk K, Ligibel J, Giobbie-Hurder A, Vergara-Diaz G, Bonato P, Quinn R, et al. Qigong mind-body exercise as a biopsychosocial therapy for persistent post-surgical pain in breast cancer: a pilot study. Integr Cancer Therapies. (2020) 19:1534735419893766. doi: 10.1177/1534735419893766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. He S, Xia C, Li H, Cao M, Yang F, Yan X, et al. Cancer profiles in china and comparisons with the USA: a comprehensive analysis in the incidence, mortality, survival, staging, and attribution to risk factors. Sci China Life Sci. (2024) 67(1):122–31. doi: 10.1007/s11427-023-2423-1 [DOI] [PubMed] [Google Scholar]
- 118. Chen S, Cao Z, Prettner K, Kuhn M, Yang J, Jiao L, et al. Estimates and projections of the global economic cost of 29 cancers in 204 countries and territories from 2020 to 2050. JAMA Oncol. (2023) 9(4):465–72. doi: 10.1001/jamaoncol.2022.7826 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.