Dear Editor,
In this letter, we describe a rare presentation of pseudotumoural eosinophilic cystitis (EC) that mimicked a bladder tumor infiltrating into the left seminal vesicle. The objective was to raise awareness of the rare presentation of EC where it can extend beyond the confines of bladder wall. The report also highlights the importance of considering EC in the differential diagnosis of bladder tumors, especially in patients with a history of allergies, autoimmune disorders, or infections, even if the preoperative imaging is strongly suggestive of malignancy. The patient understood and agreed to each treatment plan. The consent was also obtained for the publication.
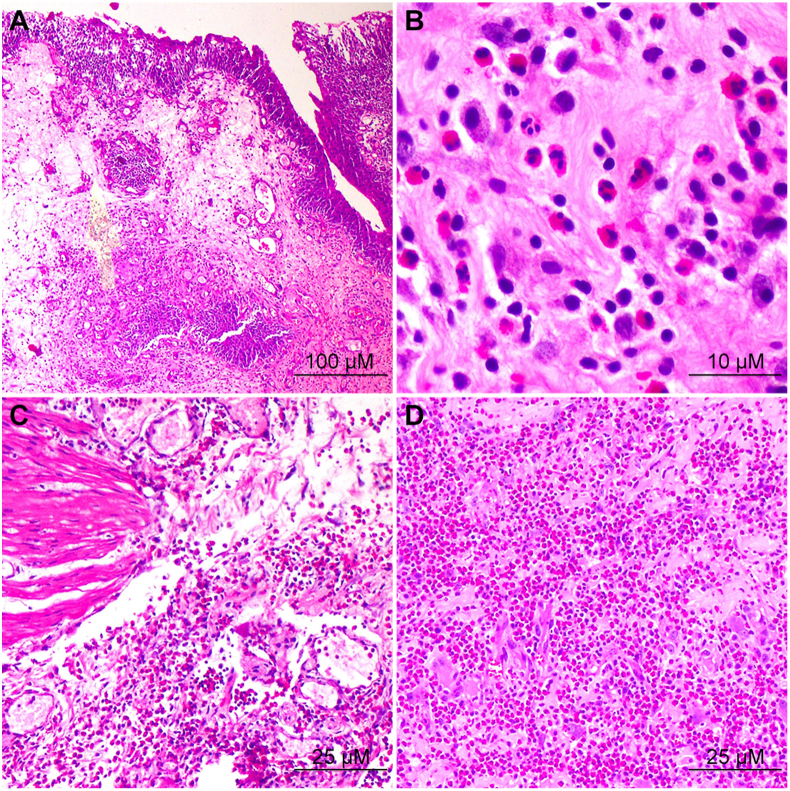
A 40-year-old male patient, who had a history of bronchial asthma and recurrent urinary tract infections, presented with dysuria and intermittent visible hematuria associated with clots for the past 3 months. The patient denied any prior history of urological malignancies, was a non-smoker, and had no significant family history of urological or autoimmune diseases. Physical examination showed no palpable bladder mass or tenderness. Digital rectal examination revealed a normal prostate gland with no palpable nodules or induration. The rest of the physical examination was unremarkable. Imaging was done using transabdominal ultrasound and computed tomography scan of the abdomen and pelvis, which revealed a mass arising from the left posterolateral and lateral wall of the bladder, measuring approximately 5 cm×3 cm, with an irregular surface and infiltration into the left seminal vesicle (Supplementary Fig. 1). No evidence of lymphadenopathy or distant metastases was noted. A transurethral resection of the bladder tumor was performed under regional anesthesia with an obturator block. Histopathological examination revealed infiltration of eosinophils into the bladder wall, consistent with EC (Fig. 1). No evidence of malignancy could be noted. The patient was followed up at 3 months and 6 months with repeat ultrasonography. Follow-up imaging studies showed no evidence of recurrence, and the patient's urinary symptoms were resolved without the need for any additional treatment.
Figure 1.
Hematoxylin-eosin staining results of the resected specimen. (A) The bladder lining exhibiting inflammation and swelling of the underlying connective tissue, indicative of cystitis (100×); (B) A subsection of Fig. 1A under higher magnification revealing a substantial presence of eosinophilic infiltrates, identified by their brick-red cytoplasm, as well as few mast cells and apoptotic stromal cells (1000×); (C) The sheets of eosinophils infiltrating the connective tissue (400×); (D) The sheets of eosinophilic infiltrates in the stroma (400×).
EC is a rare entity with a pooled analysis done in 200 cases showing only 135 cases reported in international literature [1]. The cause of EC remains unclear, although the disease has been related to a variety of potential etiologic factors, such as allergies, bladder cancer, trauma, parasitic infections, and a variety of different drugs [1,2]. Recently, BRAF mutation in hematopoietic cells indicating a relation to other myeloproliferative syndromes has been suggested as a novel driver of EC [3]. The condition usually follows a benign course in most cases [2]. In rare cases, such as the one presented, it can manifest as a pseudotumor that resembles the imaging characteristics of a bladder tumor, with extension beyond the confines of the bladder wall. A high index of suspicion is required for diagnosis because of non-specific clinical and imaging characteristics [4]. Although EC has been reported to follow a self-limiting course and resolving spontaneously, it can lead to substantial morbidity if left untreated or managed inappropriately [5]. In cases where treatment is necessary due to persistent symptoms, transurethral resection of the lesion followed by systemic antihistamines, corticosteroids, and non-steroidal anti-inflammatory drugs, either individually or in combination, is a frequently employed strategy for symptom management and inflammation reduction in EC patients [5]. Intravesical administration of steroids or dimethyl sulfoxide has also been reported as a viable treatment option [6]. In addition to steroids, immunosuppressive agents such as cyclosporine have also been used successfully in combination with steroids in the treatment of EC [7]. In recent times, the application of biologic agents in managing EC has gained significant attention. Benralizumab, a monoclonal antibody that selectively targets the interleukin-5 receptor alpha subunit on eosinophils, has been among the prominent agents of interest [8].
In conclusion, due to the limited number of reported cases and absence of consensus on preoperative diagnosis and treatment, further research is required to establish optimal management strategies for EC. It is essential for clinicians to consider EC as a possible differential diagnosis in patients exhibiting clinical symptoms suggestive of bladder malignancy, given the infiltrative nature of EC, as demonstrated in the presented case. Maintaining a high-degree of clinical suspicion is critical to avoid misdiagnosis and inappropriate management of pseudotumoral EC, which can mimic bladder cancer. Once the diagnosis is confirmed, treatment options vary and may include corticosteroids, non-steroidal anti-inflammatory drugs, intravesical instillation of steroids or dimethyl sulfoxide, and immunosuppressive agents. Recent reports indicated that benralizumab, a monoclonal antibody targeting eosinophils, may be a promising treatment option for refractory EC. However, further research is required to establish its efficacy.
Author contributions
Study concept and design: Padmaraj Hegde, Anshuman Singh.
Data acquisition: Anshuman Singh, Kasi Viswanath Gali.
Data analysis: Vivek Pai.
Drafting of manuscript: Anshuman Singh, Kasi Viswanath Gali.
Critical revision of the manuscript: Padmaraj Hegde, Anshuman Singh.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajur.2023.07.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
Supplementary Figure 1.
Coronal section of computed tomographic scan showing heterogenously enhancing lesion over left lateral and posterolateral bladder wall infiltrating into the left seminal vesicle.
References
- 1.van den Ouden D. Diagnosis and management of eosinophilic cystitis: a pooled analysis of 135 cases. Eur Urol. 2000;37:386–394. doi: 10.1159/000020183. [DOI] [PubMed] [Google Scholar]
- 2.Itano N.M.B., Malek R.S. Eosinophilic cystitis in adults. J Urol. 2001;165:805–807. [PubMed] [Google Scholar]
- 3.Choi M.Y., Tsigelny I.F., Boichard A., Skjevik Å.A., Shabaik A., Kurzrock R. BRAF mutation as a novel driver of eosinophilic cystitis. Cancer Biol Ther. 2017;18:655–659. doi: 10.1080/15384047.2017.1360449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasan A., Abdel-Al I., Nafie K., Rashad M.F., Abozied H., Elhussiny M.E.A., et al. Clinicopathological characteristics and outcomes of eosinophilic cystitis: a retrospective study. Ann Med Surg (Lond) 2021;68 doi: 10.1016/j.amsu.2021.102626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Popescu O., Landas S., Haas G. The spectrum of eosinophilic cystitis in males: case series and literature review. Arch Pathol Lab Med. 2009;133:289–294. doi: 10.5858/133.2.289. [DOI] [PubMed] [Google Scholar]
- 6.Chia D. Eosinophilic cystitis and haematuria: case report of a rare disease and common presentation. Int J Surg Case Rep. 2016;24:43–45. doi: 10.1016/j.ijscr.2016.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adeleye O., Trickett J.S., Wright B.L., Khan A. Refractory eosinophilic cystitis controlled with low-dose cyclosporine therapy: a case report. Urol Case Rep. 2021;39 doi: 10.1016/j.eucr.2021.101829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Konstantinou G.N., Voukelatou V. Eosinophilic cystitis refractory to steroids successfully treated with benralizumab: a case report. Front Allergy. 2023;3 doi: 10.3389/falgy.2022.1055129. [DOI] [PMC free article] [PubMed] [Google Scholar]