Abstract
Purpose
To evaluate the clinical outcome scores of an arthroscopic margin convergence technique without the use of suture anchors to repair different types of rotator cuff tears and to determine whether the type or extent of the tear has an effect on clinical outcome scores after this procedure.
Methods
Patients receiving arthroscopic margin convergence repair without suture anchors for rotator cuff tears from 2013 to 2018 were retrospectively analyzed. Arthroscopically determined partial- or full-thickness rotator cuff tears with a minimum follow-up period of 20 months were included. Outcomes were assessed using the American Shoulder and Elbow Surgeons (ASES) shoulder score; University of California, Los Angeles (UCLA) shoulder score; and visual analog scale (VAS) score. A 2-tailed distribution paired t test was used to determine statistical significance (P < .05) between preoperative scores and scores at final follow-up. Correlation tests and linear regression analysis were used to determine the correlation between various clinical variables and outcomes. A cohort-specific minimal clinically important difference analysis was performed for each outcome score, calculated as one-half of the standard deviation of the delta score.
Results
A total of 38 patients were included for analysis: 12 with partial-thickness tears and 26 with full-thickness tears. The mean postoperative follow-up period was 33.9 months (range, 22.2-94.5 months), with a minimum follow-up period of 22 months. The mean age of the patients was 62 ± 15.1 years. The minimal clinically important difference values for the ASES, UCLA, and VAS scores were 9.68, 2.92, and 1.13, respectively. There were significant improvements in the ASES (from 29.3 ± 18.3 preoperatively to 93.7 ± 8.3 postoperatively, P = .001), UCLA (from 14.3 ± 6.2 to 32.8 ± 2.6, P = .001), and VAS (from 7.37 ± 1.8 to 0.63 ± 1.02, P = .001) clinical outcome scores. However, patients with either Patte stage 3 retraction (P = .033 for ASES score and P = .020 for UCLA score) or U-shaped tears (P = .047 for ASES score and P = .050 for UCLA score) had significantly lower clinical outcome scores than patients with less severe retraction or differently shaped tears.
Conclusions
The arthroscopic margin convergence technique without the use of suture anchors may be a suitable option in patients with partial- or full-thickness rotator cuff tears.
Level of Evidence
Level IV, therapeutic case series.
One of the most cited techniques for repair of the rotator cuff is a side-to-side suturing technique that will close large, retracted tears with fixation to the humerus at a point without additional tension when the patient’s arm is in anatomic position.1,2 In 1992, an arthroscopic technique termed “margin convergence” was described by Burkhart.3 In this technique, side-to-side suturing is performed in the anteroposterior direction.3 This technique shifts the free margin of the tendon so that this margin is closer to the greater tuberosity, thus decreasing the tension at the anchoring site.3 This technique has been especially successful in the repair of U- and L-shaped tears.
In 2005, Wolf et al.2 performed margin convergence without the use of sutures to anchor the tendon to bone. The study showed favorable long-term outcomes in patients without suture anchor fixation. Inui et al.4 used margin convergence in patients with pseudoparalysis and irreparable rotator cuff tears, showing pseudoparalysis reversal and improvement in American Shoulder and Elbow Surgeons (ASES) scores at final follow-up.
Despite the aforementioned findings, the data are sparse on patient-reported outcomes after an anchorless margin convergence repair. The purposes of this study were to evaluate the clinical outcome scores of an arthroscopic margin convergence technique without the use of suture anchors to repair different types of rotator cuff tears and to determine whether the type or extent of the tear has an effect on clinical outcome scores after this procedure.
Methods
Patient Selection
This was a retrospective analysis of all patients undergoing arthroscopic margin convergence repair without suture anchor fixation performed by a single orthopaedic surgeon (C.M.) from 2013 to 2018. The inclusion criteria were (1) full-thickness or partial-thickness tear of the rotator cuff, as determined by clinical examination, magnetic resonance imaging (MRI), and intraoperative evaluation; (2) margin convergence technique performed without the use of suture anchors; and (3) follow-up period of at least 20 months.5 Patients who underwent subacromial decompression, labral repair, or biceps tenodesis in addition to primary arthroscopic rotator cuff repair also had the potential for inclusion in the study. Patients who had less than 20-month follow-up or who died prior to acquisition of postoperative outcome measurements were excluded. Patients were also excluded if they had evidence of adhesive capsulitis or radiographic evidence of osteoarthritis, inflammatory arthritis, cervical radiculopathy, or proximal humeral fracture. Additionally, patients with irreparable rotator cuff tears, those undergoing revision surgery, and those with rotator cuff arthropathy were excluded. For patients with full-thickness tears, surgery was indicated if conservative management had failed and there was persistent, unrelieved pain and weakness. Patients with partial-thickness tears were indicated for surgical repair if greater than 50% of the rotator cuff was torn and conservative therapy failed. Anchor fixation to bone was not performed because this can lead to alterations in shoulder anatomy and mobility through medializing the rotator cuff insertion.6 This protocol was approved by the Thomas Jefferson University Institutional Review Board in compliance with all applicable federal regulations governing the protection of human subjects, and each patient provided written consent.
Outcomes were assessed using the ASES shoulder score; University of California, Los Angeles (UCLA) shoulder score; and visual analog scale (VAS) score. Other variables included in this study were sex, age, symptom duration, interval between operation and follow-up to obtain postoperative outcome measurements, and degree of shoulder abduction prior to the operation. The presence of biceps involvement, impingement, muscle atrophy, and fatty infiltration on preoperative MRI was recorded. Additionally, the level of rotator cuff retraction was assessed on frontal MRI planes and classified using the Patte classification system: stage 1, the proximal stump is near the bony insertion; stage 2, the proximal stump is at the level of the humeral head; and stage 3, the proximal stump is at the level of the glenoid.7 The presence of acromioclavicular osteoarthritis was also determined via radiographs prior to surgery. In addition, the shape of the rotator cuff tear (crescent-, U-, V-, or L-shaped) was noted on MRI and then confirmed at the time of surgery by the orthopaedic surgeon.
Surgical Technique
All surgical procedures were performed by a single senior orthopaedic surgeon (C.M.). Routine shoulder arthroscopy was performed with the patients placed in the lateral recumbent position. The glenohumeral joint was evaluated for intra-articular pathology, and devitalized tissue was debrided from the torn rotator cuff tendon. A curette was used to create a bleeding surface over the greater tuberosity, which has been shown to enhance healing of the rotator cuff to the tuberosity.2 Arthroscopic side-to-side repair without fixation to bone was then commenced. One to three sutures, depending on the size of the tear, were passed in a side-to-side fashion, from anterior to posterior, through the torn tendon to approximate the tendon edges and bring the repair over the prepared bleeding bed of bone. For full-thickness tears, a suture was passed through the anterior corner of the posterior portion of the torn tendon and then through the coracohumeral ligament. This step helped to advance the posterior leaf anteriorly, approximate the posterior leaf to the rotator interval, and brace the entire repair over the bleeding bed on the tuberosity.2 For partial-thickness articular-sided tears, the remaining intact tendon was left intact; the tear was not completed. Sutures were passed anterior to posterior in a side-to-side fashion, using 2 spinal needles, and tied over the bursal side of the rotator cuff. No suture was placed through the coracohumeral ligament for partial-thickness tears. Suture anchor fixation to the tuberosity was not performed to avoid medializing the rotator cuff insertion, shortening the muscle-tendon length, and altering shoulder anatomy and mobility.6 After the tendons were secured, the shoulder was taken through a full range of motion to ensure the approximation was maintained. If needed, acromioplasty, biceps tenotomy, and biceps tenodesis were then performed.
Rehabilitation Protocol
After surgery, the shoulder was placed in a sling for 4 weeks. Patients were enrolled in a standardized physical therapy program after surgery, which involved supervised passive range-of-motion exercises. After the initial 4 weeks, patients were transitioned into a strengthening program, also supervised by a physical therapist.
Statistical Analysis
A 2-tailed distribution paired t test was used to determine statistical significance (P < .05) between preoperative scores and scores at final follow-up. Correlation tests, including the Pearson coefficient for quantitative variables and Spearman coefficient for qualitative variables, and linear regression analysis were used to determine the correlation between various clinical variables and clinical outcomes. A cohort-specific minimal clinically important difference analysis was performed for each clinical outcome score, calculated as one-half of the standard deviation of the delta score.
Results
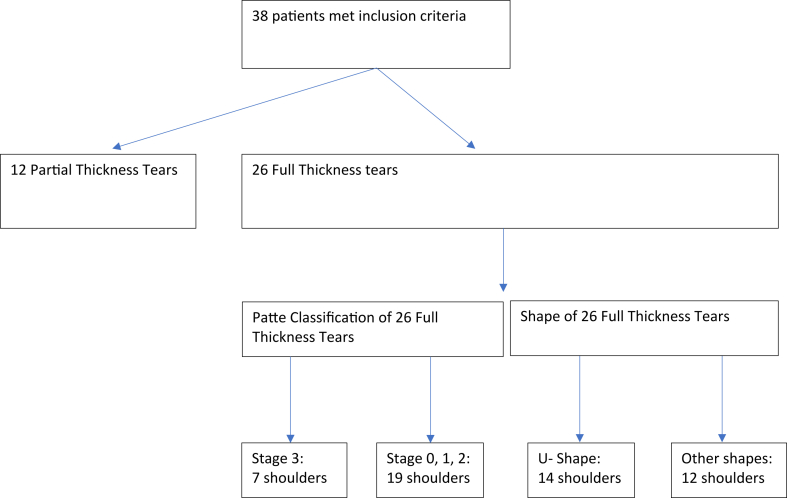
A total of 38 patients were retrospectively analyzed, of whom 24 were male and 14 were female patients. The mean age was 62 ± 15.08 years. Twenty-six patients had full-thickness rotator cuff tears, and 12 had partial-thickness tears (Fig 1). The following mechanisms of injury were noted: sport (4 patients), fall (11 patients), and other (including degenerative changes leading to tears) (23 patients). All patients were initially treated with conservative measures including physical therapy and corticosteroid injections. Preoperatively, 21 patients had full range of shoulder abduction, 8 had less than 90° of true shoulder abduction, and 9 had less than 45° of true shoulder abduction. The mean follow-up interval from the date of surgery to the date of the postoperative survey was 33.9 ± 12.4 months (range, 22-94 months) (Table 1). The minimal clinically important differences for the ASES, UCLA, and VAS scores were 9.68, 2.92, and 1.13, respectively.
Fig 1.
Flow diagram classifying patients by rotator cuff tear characteristics: full- or partial-thickness tear, extent of retraction (according to Patte classification), and tear shape.
Table 1.
Patient Demographic Characteristics
| All Patients | Patients With Full-Thickness Tears | Patients With Partial-Thickness Tears | |
|---|---|---|---|
| Average age, yr | 62 ± 15.08 | 67.92 ± 10.71 | 49.17 ± 15.53 |
| Sex | |||
| Male | 24 | 16 | 8 |
| Female | 14 | 10 | 4 |
| Mechanism of injury | |||
| Sport | 4 | 2 | 2 |
| Fall | 11 | 10 | 1 |
| Other (including degenerative tears) | 23 | 14 | 9 |
| Preoperative shoulder abduction range of motion | |||
| <45° | 9 | 7 | 2 |
| 45°-90° | 8 | 5 | 3 |
| Full | 21 | 14 | 7 |
NOTE. Data are presented as mean ± standard deviation or number.
In the study cohort, the mean ASES, UCLA, and VAS scores significantly improved from before surgery to after surgery (Table 2). There were statistically significant improvements in all clinical scores for patients with both full- and partial-thickness articular-sided rotator cuff tears (Table 3).
Table 2.
Preoperative and Postoperative ASES, UCLA, and VAS Scores Within Cohort
| All Patients (N = 38) |
P Value | ||
|---|---|---|---|
| Preoperative | Postoperative | ||
| ASES score | 29.69 ± 18.32 | 93.72 ± 8.25 | .001∗ |
| UCLA score | 14.29 ± 6.18 | 32.84 ± 2.57 | .001∗ |
| VAS score | 7.37 ± 1.83 | 0.63 ± 1.02 | .001∗ |
NOTE. Data are presented as mean ± standard deviation. All patients in the cohort showed significant improvement in ASES, UCLA, and VAS clinical outcome scores after arthroscopic margin convergence rotator cuff repair without anchors.
ASES, American Shoulder and Elbow Surgeons; UCLA, University of California, Los Angeles; VAS, visual analog scale.
Statistically significant (P < .05).
Table 3.
Preoperative and Postoperative ASES, UCLA, and VAS Scores for Full- and Partial-Thickness Rotator Cuff Tears
| Patients With Full-Thickness Tears (n = 26) | Patients With Partial-Thickness Tears (n = 12) | |
|---|---|---|
| ASES shoulder score | ||
| Preoperative | 28.52 ± 18.53 | 32.22 ± 18.41 |
| Postoperative | 92.94 ± 8.57 | 95.41 ± 7.60 |
| P value | .001∗ | .002∗ |
| UCLA shoulder score | ||
| Preoperative | 12.77 ± 6.10 | 17.58 ± 5.16 |
| Postoperative | 32.50 ± 2.80 | 33.58 ± 1.88 |
| P value | .001∗ | .002∗ |
| VAS score | ||
| Preoperative | 7.31 ± 1.93 | 7.50 ± 1.67 |
| Postoperative | 0.69 ± 1.08 | 0.50 ± 0.90 |
| P value | .001∗ | .001∗ |
NOTE. Data are presented as mean ± standard deviation. Patients with full- and partial-thickness rotator cuff tears showed significant improvements in ASES, UCLA, and VAS clinical outcome scores after arthroscopic margin convergence rotator cuff repair without anchors. There was no significant difference in postoperative clinical outcome scores between patients with full-thickness tears and those with partial-thickness tears.
ASES, American Shoulder and Elbow Surgeons; UCLA, University of California, Los Angeles; VAS, visual analog scale.
Statistically significant (P < .05).
The extent of retraction, measured by the Patte classification, and the shape of the tear were examined to assess the influence of these variables on postoperative clinical scores in patients with full-thickness tears. All patients with full-thickness tears, regardless of Patte stage or tear shape, showed significant improvements in clinical scores from preoperatively to postoperatively. However, despite overall good outcomes, Patte stage 3 retraction and U-shaped tears had a negative impact on clinical scores. Patients with Patte stage 3 retraction had significantly lower postoperative ASES and UCLA scores than patients with no retraction, Patte stage 1 retraction, and Patte stage 2 retraction. Patients with U-shaped tears had significantly lower ASES and UCLA scores than patients with other tear shapes (Table 4).
Table 4.
Outcome Scores Considering Severity and Shape of Tear
| Patients With Full-Thickness Tears (n = 26) |
||||||
|---|---|---|---|---|---|---|
| Patte Classification |
Tear Shape |
|||||
| Patte Stage 3 (n = 7) | No Retraction or Patte Stage 1 or 2 (n = 19) | P Value | U-Shaped (n = 14) | All Other Shapes (n = 12) | P Value | |
| ASES shoulder score | ||||||
| Preoperative | 21.90 ± 22.16 | 30.96 ± 17.01 | .132 | 26.07 ± 21.06 | 31.38 ± 15.47 | .226 |
| Postoperative | 87.13 ± 10.16 | 95.08 ± 7.05 | .033∗ | 90.1 ± 9.08 | 95.83 ± 7.26 | .047∗ |
| P value | .018∗ | .001∗ | — | .001∗ | .002∗ | — |
| UCLA shoulder score | ||||||
| Preoperative | 8.71 ± 6.37 | 14.26 ± 5.13 | .059 | 12.14 ± 6.60 | 13.50 ± 5.66 | .624 |
| Postoperative | 30.14 ± 3.48 | 33.37 ± 1.97 | .020∗ | 31.57 ± 2.98 | 33.58 ± 2.23 | .050∗ |
| P value | .020∗ | .001∗ | — | .001∗ | .001∗ | — |
| VAS score | ||||||
| Preoperative | 7.71 ± 2.49 | 7.16 ± 1.74 | .463 | 7.36 ± 2.30 | 7.25 ± 1.48 | .638 |
| Postoperative | 1.0 ± 1.41 | 0.58 ± 0.96 | .473 | 0.86 ± 1.23 | 0.50 ± 0.90 | .362 |
| P value | .018∗ | .001∗ | — | .001∗ | .001∗ | — |
NOTE. Data are presented as mean ± standard deviation. All patients with full-thickness tears showed significant improvements in clinical scores from preoperatively to postoperatively. Patients with either Patte stage 3 retraction or U-shaped tears had significantly lower clinical outcome scores than patients with less severe retraction or non–U-shaped tears.
ASES, American Shoulder and Elbow Surgeons; UCLA, University of California, Los Angeles; VAS, visual analog scale.
Statistically significant (P < .05).
There were no significant differences in postoperative ASES or UCLA scores when age, sex, and preoperative range of motion were evaluated in isolation. The presence of preoperative MRI findings was also examined. In patients with muscle atrophy present on MRI (n = 5), there were no significant differences in the postoperative ASES and UCLA scores when compared with patients without muscle atrophy (P = .298 and P = .964, respectively). In patients with impingement present on MRI (n = 20), there were no significant differences in the postoperative ASES and UCLA scores when compared with patients without impingement (P = .842 and P = .758, respectively). In patients with biceps involvement on MRI (n = 11), there were no significant differences in the postoperative ASES and UCLA scores when compared with patients without biceps involvement (P = .142 and P = .879, respectively).
Discussion
This study showed that patients undergoing margin convergence repair without suture anchors for full- and partial-thickness rotator cuff tears showed significant improvement in clinical outcome scores between the preoperative and postoperative periods. Patients with full-thickness rotator cuff tears and stage 3 retraction or U-shaped tears showed significantly lower postoperative ASES and UCLA scores than patients with less severe retraction and non–U-shaped tears. There was no significant difference in final functional outcomes based on age, sex, or associated pathology including biceps tear and acromioclavicular arthritis.
There is a limited amount of evidence on the use of margin convergence to repair full-thickness rotator cuff tears. In 2001, Burkhart et al.8 repaired 25 U-shaped rotator cuff tears and 34 crescent-shaped tears. The crescent-shaped tears were repaired with suture anchors alone, whereas 15 U-shaped tears were repaired with margin convergence alone and 10 U-shaped tears were repaired with margin convergence plus suture anchors. With an average follow-up period of 3.5 years, good or excellent postoperative modified UCLA scores were reported in 56 patients (94.9%) and no statistically significant difference was observed between the 3 types of repair. Despite these positive results, the possibility of an underpowered analysis should be considered given the small sample size. In 2004, Wolf et al.9 performed a study using an average of 4 margin convergence sutures and 1.2 suture anchors in 96 full-thickness rotator cuff tear repairs. Of the patients, 94% had good or excellent modified UCLA scores and 96% were satisfied and rated the operation as successful. Kim et al.10 published a study on 59 patients who underwent margin convergence repair for large U-shaped full-thickness rotator cuff tears with an average follow-up period of 38 months. A mean of 2 margin convergence sutures and 2 suture anchors were used. The authors reported significant improvements in the VAS score, range of motion, and Constant-Murley score, showing satisfactory clinical outcomes.
The improved clinical outcomes using margin convergence are thought to be due to reduced tension across the rotator cuff tendon by converging the free margin of the torn tendon in the anteroposterior direction and then placing the repaired tendon over the footprint and a prepared bone bed to promote healing.8,11 Wolf et al.2 performed margin convergence repair without the use of suture anchors on 42 full-thickness rotator cuff tears, and at an average follow-up of 73 months, 98% of patients reported good or excellent results with a modified UCLA scoring system. Tendon healing to a prepared bleeding bone bed without the use of suture anchor fixation is supported by the rotator cable suspension bridge concept of Burkhart et al.12 and evidence from second-look arthroscopy reported by Wolf et al.2 The rotator cable involves a thickened band of fibers perpendicular to the supraspinatus and infraspinatus. This cable acts biomechanically as a suspension bridge to transfer stress away from the rotator cuff and to shield the distal rotator crescent from strain or tearing, thus promoting an environment conducive to healing at the bone-tendon interface.12 Wolf et al.2 described 9 full-thickness tears repaired in a purely side-to-side fashion that showed complete healing to the tuberosity during second-look arthroscopy at 5 to 16 months postoperatively, providing evidence that the repaired rotator cuff tendon can heal to a bleeding bed on the tuberosity without the use of suture anchors. Furthermore, a repair without suture anchors reduces the risks of shortening the rotator cuff muscle-tendon length, medializing the cuff insertion, and altering the anatomy and mobility of the shoulder.6
Failure of a rotator cuff repair can be a result of tension overload. Andarawis-Puri et al.13 showed that increased strain can lead to increased rotator cuff tear propagation. Park et al.14 and Takeda et al.15 categorized the tension across the rotator cuff and showed that increased tension (>35 N) can lead to higher rates of retear after repair. Davidson and Rivenburgh16 showed that increased tension during repair has a direct correlation to decreased clinical outcomes and increased pain scores postoperatively. They recommended repairs that do not exceed 8 lb (35.6 N) of tension. It has been shown that margin convergence decreases strain across the rotator cuff by up to 58% and reduces the size of the tear gap with each suture used.17 This repair technique can lead to decreased strain and tension across the repair site to allow for anatomic healing and improved clinical outcomes.11
In massive irreparable rotator cuff tears, it makes biomechanical sense to convert the cuff into a functional tear by restoring the force couples in the coronal and transverse planes—and restoring the suspension bridge, that is, the rotator cable.12,18, 19, 20, 21, 22 Porcellini et al.22 evaluated 67 patients with irreparable supraspinatus tears and found improvement in shoulder function when compared with debridement alone by repairing the posterior aspect of the suspension bridge. Burkhart et al.18 partially repaired 11 massive rotator cuff tears and saw significant improvements in the UCLA score postoperatively. Duralde and Bair20 aimed to convert 24 massive tears to a biomechanically intact state and found good or excellent results in 16 patients, with a significant reduction in pain within the cohort. Shon et al.23 restored the posterior cuff with or without the subscapularis to restore the transverse force couple in 31 large to massive rotator cuff tears. They saw a significant improvement in postoperative scores, but patient-rated satisfaction at the final evaluation was poor, with only half of patients being satisfied. There is a biomechanical advantage in converting a rotator cuff tear to a functional tear in the setting of a massive irreparable tear.
Despite the reported mechanical advantages and strong clinical outcomes of margin convergence, the rate of retear has been reported to be high. In 2013, Kim et al.24 assessed repair integrity after margin convergence repair of U- or V-shaped rotator cuff tears at 20.2 months and reported a retear rate of 47.8%. In 2019, Kim et al.10 examined tendon repair integrity after repair of U-shaped full-thickness rotator cuff tears and found a retear rate of 54.2% with a minimum of 24-month follow-up. Patients with anchor fixation had a lower retear rate than patients with simple side-to-side repair; however, anchor fixation did not affect clinical outcomes. Other studies have shown retear rates of 28% and 34%.5,25 These inconsistent results regarding the rotator cuff retear rate raise concerns about whether rotator cuff integrity is maintained after margin convergence repair. However, other than the use of simple side-to-side repair in 1 group in the 2019 study of Kim et al., the aforementioned studies used suture anchor fixation, which could potentially shorten the muscle-tendon length of the rotator cuff. These high rates of retear with the use of suture anchors, as well as the potential benefits and reported tendon-to-bone healing with an anchorless repair stated previously, question the necessity of using anchor-to-bone fixation and provide justification for a repair without suture anchors in our cohort. Furthermore, the absence of correlation of reported retear rates with patient outcomes questions the validity of whether retear rates impact clinical function. In this study, we did not evaluate for retears postoperatively; however, no patients experienced clinical failure or required reoperation.
Twelve patients with partial-thickness tears were included in our cohort to address the goal of evaluating clinical outcomes of different types of tears, as well as assessing whether the extent of a tear affects clinical outcomes after an anchorless margin convergence repair. Surgical treatment of partial-thickness rotator cuff tears is generally indicated in patients in whom conservative measures fail, and formal repair is supported in patients with tears involving greater than 50% of the tendon thickness.26 Repair techniques generally include suturing the tendon followed by anchor fixation to bone—or completing the tear prior to repair.27 However, anchor fixation medializes the cuff insertion and can overconstrain the joint, whereas completing the tear compromises intact tissue. Margin convergence without the use of suture anchors avoids these risks of partial-thickness rotator cuff repairs, and all patients in our cohort had improved clinical outcome scores postoperatively.
The possible reasons patients with large tear retractions and U-shaped tears showed significantly lower ASES and UCLA scores are as follows: The increased retraction prior to surgical fixation could lead to increased strain on the rotator cuff tendon when approximating to the free margin. Takeda et al.15 showed that increased tear size in the medial-lateral direction showed a strong correlation with an increase in repair tension. Some tears that are classified as U-shaped may be mislabeled owing to deforming forces. As Mochizuki et al.28 described, in chronic L-shaped tears, the posteromedial leaf becomes retracted to result in a U-shaped configuration. This may lead to inappropriate tension at the repair site, leading to decreased clinical scores. During repair, the rotator cable may not have been appropriately restored to achieve biomechanical stability. Burkhart et al.12 explained that the rotator cable acts as a suspension bridge and stress shield of the rotator crescent, and failure to restore the cable can lead to biomechanical deficiency of the rotator cuff. Furthermore, increased tension may have been applied during fixation. Too much tension when approximating the anterior leaf to the posterior leaf can create a bunched and deformed appearance of the rotator cuff tendon.10 Finally, any concomitant procedures performed in patients with large tear retractions and U-shaped tears could have negatively impacted postoperative clinical outcome scores. Future studies should focus on assessing large populations to obtain prospective long-term results of patients undergoing margin convergence repair without the use of suture anchors. Categorizing patients by tear size and dimension may be compared between MRI readings and intraoperative evaluation to better show the effect of margin convergence on small, medium, and large tears. Long-term radiographic evaluation may help to determine retear rates after repair and whether they are of clinical significance. Another question that could be addressed in future studies is the cost difference between margin convergence repair and double- or single-row repair with anchors.
Limitations
There were several limitations to this study. One limitation is the small sample size. We did not perform an a priori power analysis, so the study may be underpowered and subject to β error. In addition, clinical outcome metrics were collected retrospectively and by survey assessment, leaving the possibility for recall bias. Another limitation is the lack of a control group for comparison with our surgical cohort. Future studies that include a control group will have to address selection bias when choosing which patients to undergo margin convergence repair versus the standard repair. Moreover, the variability of preoperative range of motion and concomitant procedures performed should be considered in the context of the results. MRI reports were used to classify tear size and shape by multiple radiologists, leading to the possibility of observer bias. Our study had a shorter follow-up period, so no conclusions can be made about the long-term outcomes of margin convergence repair without suture anchors. Another limitation is the lack of ultrasound or MRI follow-up to ensure the integrity of the tendon repair. Although significant improvements were found between the preoperative and postoperative assessments, a small sample size of patients from the Northeastern United States was analyzed, leading to possible selection bias.
Conclusions
The arthroscopic margin convergence technique without the use of suture anchors may be a suitable option in patients with partial- or full-thickness rotator cuff tears.
Disclosures
All authors (S.A.G., B.M., A.L., E.S., J.R., C.M., A.B.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. B.M. is a military service member. The views expressed in this manuscript reflect the results of research conducted by the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or US Government.
References
- 1.Iqbal S., Jacobs U., Akhtar A., Macfarlane R.J., Waseem M. A history of shoulder surgery. Open Orthop J. 2013;7:305–309. doi: 10.2174/1874325001307010305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolf E.M., Pennington W.T., Agrawal V. Arthroscopic side-to-side rotator cuff repair. Arthroscopy. 2005;21:881–887. doi: 10.1016/j.arthro.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 3.Baumgarten K.M. Patient-determined outcomes after arthroscopic margin convergence rotator cuff repair. Arthrosc Sports Med Rehabil. 2020;2:e517–e522. doi: 10.1016/j.asmr.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inui H., Yamada J., Nobuhara K. Does margin convergence reverse pseudoparalysis in patients with irreparable rotator cuff tears? Clin Orthop Relat Res. 2021;479:1275–1281. doi: 10.1097/CORR.0000000000001617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oh J.H., Kim S.H., Ji H.M., Jo K.H., Bin S.W., Gong H.S. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009;25:30–39. doi: 10.1016/j.arthro.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Brockmeier S.F., Dodson C.C., Gamradt S.C., Coleman S.H., Altchek D.W. Arthroscopic intratendinous repair of the delaminated partial-thickness rotator cuff tear in overhead athletes. Arthroscopy. 2008;24:961–965. doi: 10.1016/j.arthro.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 7.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;254:81–86. [PubMed] [Google Scholar]
- 8.Burkhart S.S., Danaceau S.M., Pearce C.E. Arthroscopic rotator cuff repair: Analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy. 2001;17:905–912. doi: 10.1053/jars.2001.26821. [DOI] [PubMed] [Google Scholar]
- 9.Wolf E.M., Pennington W.T., Agrawal V. Arthroscopic rotator cuff repair: 4- to 10-year results. Arthroscopy. 2004;20:5–12. doi: 10.1016/j.arthro.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Kim J.D., Rhee S.M., Kim M.S., Ro K., Rhee Y.G. Arthroscopic side-to-side repair for large U-shaped full-thickness rotator cuff tears: Is the repair integrity actually maintained? Arthroscopy. 2019;35:3211–3218. doi: 10.1016/j.arthro.2019.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Burkhart S.S., Athanasiou K.A., Wirth M.A. Margin convergence: A method of reducing strain in massive rotator cuff tears. Arthroscopy. 1996;12:335–338. doi: 10.1016/s0749-8063(96)90070-5. [DOI] [PubMed] [Google Scholar]
- 12.Burkhart S.S., Esch J.C., Jolson R.S. The rotator crescent and rotator cable: An anatomic description of the shoulder’s “suspension bridge.”. Arthroscopy. 1993;9:611–616. doi: 10.1016/s0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
- 13.Andarawis-Puri N., Ricchetti E.T., Soslowsky L.J. Rotator cuff tendon strain correlates with tear propagation. J Biomech. 2009;42:158–163. doi: 10.1016/j.jbiomech.2008.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park S.G., Shim B.J., Seok H.G. How much will high tension adversely affect rotator cuff repair integrity? Arthroscopy. 2019;35:2992–3000. doi: 10.1016/j.arthro.2019.05.049. [DOI] [PubMed] [Google Scholar]
- 15.Takeda Y., Fujii K., Suzue N., Miyatake K., Kawasaki Y., Yokoyama K. Repair tension during arthroscopic rotator cuff repair is correlated with preoperative tendon retraction and postoperative rotator cuff integrity. Arthroscopy. 2021;37:2735–2742. doi: 10.1016/j.arthro.2021.03.069. [DOI] [PubMed] [Google Scholar]
- 16.Davidson P.A., Rivenburgh D.W. Rotator cuff repair tension as a determinant of functional outcome. J Shoulder Elbow Surg. 2000;9:502–506. doi: 10.1067/mse.2000.109385. [DOI] [PubMed] [Google Scholar]
- 17.Mazzocca A.D., Bollier M., Fehsenfeld D., et al. Biomechanical evaluation of margin convergence. Arthroscopy. 2011;27:330–338. doi: 10.1016/j.arthro.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Burkhart S.S., Nottage W.M., Ogilvie-Harris D.J., Kohn H.S., Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10:363–370. doi: 10.1016/s0749-8063(05)80186-0. [DOI] [PubMed] [Google Scholar]
- 19.Denard P.J., Koo S.S., Murena L., Burkhart S.S. Pseudoparalysis: The importance of rotator cable integrity. Orthopedics. 2012;35:e1353–e1357. doi: 10.3928/01477447-20120822-21. [DOI] [PubMed] [Google Scholar]
- 20.Duralde X.A., Bair B. Massive rotator cuff tears: The result of partial rotator cuff repair. J Shoulder Elbow Surg. 2005;14:121–127. doi: 10.1016/j.jse.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 21.Pinkowsky G.J., ElAttrache N.S., Peterson A.B., Akeda M., McGarry M.H., Lee T.Q. Partial-thickness tears involving the rotator cable lead to abnormal glenohumeral kinematics. J Shoulder Elbow Surg. 2017;26:1152–1158. doi: 10.1016/j.jse.2016.12.063. [DOI] [PubMed] [Google Scholar]
- 22.Porcellini G., Castagna A., Cesari E., Merolla G., Pellegrini A., Paladini P. Partial repair of irreparable supraspinatus tendon tears: Clinical and radiographic evaluations at long-term follow-up. J Shoulder Elbow Surg. 2011;20:1170–1177. doi: 10.1016/j.jse.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Shon M.S., Koh K.H., Lim T.K., Kim W.J., Kim K.C., Yoo J.C. Arthroscopic partial repair of irreparable rotator cuff tears: Preoperative factors associated with outcome deterioration over 2 years. Am J Sports Med. 2015;43:1965–1975. doi: 10.1177/0363546515585122. [DOI] [PubMed] [Google Scholar]
- 24.Kim K.C., Shin H.D., Cha S.M., Kim J.H. Repair integrity and functional outcomes for arthroscopic margin convergence of rotator cuff tears. J Bone Joint Surg Am. 2013;95:536. doi: 10.2106/JBJS.L.00397. [DOI] [PubMed] [Google Scholar]
- 25.Moosmayer S., Lund G., Seljom U.S., et al. At a 10-year follow-up, tendon repair is superior to physiotherapy in the treatment of small and medium-sized rotator cuff tears. J Bone Joint Surg Am. 2019;101:1050–1060. doi: 10.2106/JBJS.18.01373. [DOI] [PubMed] [Google Scholar]
- 26.Matthewson G., Beach C.J., Nelson A.A., et al. Partial thickness rotator cuff tears: Current concepts. Adv Orthop. 2015;2015 doi: 10.1155/2015/458786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spencer E.E., Jr. Partial-thickness articular surface rotator cuff tears: An all-inside repair technique. Clin Orthop Relat Res. 2010;468:1514–1520. doi: 10.1007/s11999-009-1215-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mochizuki T., Sugaya H., Uomizu M., et al. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff: Surgical technique. J Bone Joint Surg Am. 2009;91(suppl 2, pt 1):1–7. doi: 10.2106/JBJS.H.01426. [DOI] [PubMed] [Google Scholar]