Abstract
Purpose
To assess the biomechanical performance of 2 simplified loop-and-tack biceps tenodesis techniques, all-suture anchor and all-suture anchor with a button, compared with the interference screw technique in an ovine model.
Methods
Twenty-one biceps tenodesis procedures were executed on the humeri and flexor digitorum profundus tendons of skeletally mature, female sheep. Limbs were evenly randomized into 2 experimental groups (all-suture anchor with or without button) and 1 control group (interference screw). Cyclic loading followed by a load-to-failure test was conducted. The primary outcome metric was end-cycle stiffness, or stiffness measured at the end of cyclic loading, because it modeled the resistance of the construct to the lower-force activities of postoperative physical therapy. Secondary metrics included ultimate failure load (UFL), yield load, creep, and load-to-failure stiffness. End-cycle stiffness difference-of-means testing was conducted with a minimal clinically important difference threshold of –15 N/mm (–1.5 kg/mm). Groups were compared using analysis of variance for all recorded variables.
Results
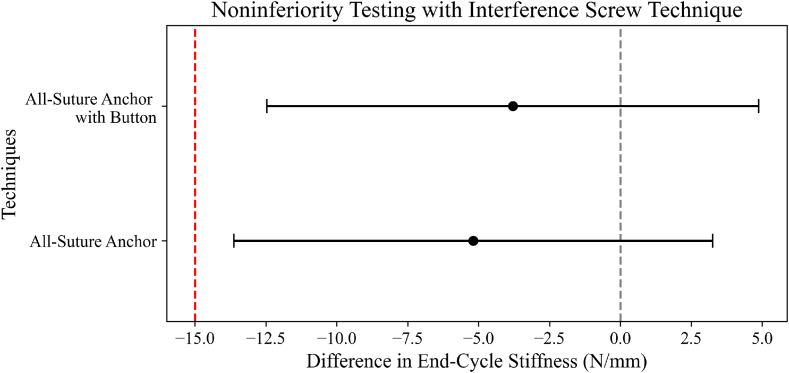
Both the all-suture anchor techniques, without a button and with a button, were found to be noninferior in end-cycle stiffness to the interference screw technique (–5.2 N/mm [95% confidence interval, –13.6 to 3.3 N/mm] and –3.8 N/mm [95% confidence interval, –12.5 to –4.9 N/mm], respectively) with a minimal clinically important difference of –15 N/mm. The all-suture techniques showed significantly lower UFL, lower yield load, greater creep, and lower load-to-failure stiffness (P < .001, P < .001, P = .002, and P < .001, respectively). Tendon dimensions did not vary significantly across groups.
Conclusions
Under subfailure loading conditions, the all-suture anchor techniques with a button and without a button showed end-cycle stiffness noninferiority to an interference screw technique; however, these techniques were inferior in all secondary outcomes, including significantly lower UFL, lower yield load, greater creep, and lower load-to-failure stiffness.
Clinical Relevance
The all-suture anchor approaches with a button and without a button may retain the natural length-tension dynamics of the long head of the biceps tendon because fixation can occur before the release of the tendon origin. Additionally, they may offer a simpler and more cost-effective alternative to prevailing arthroscopic methods.
Historically, the most clinically efficacious biceps tenodesis techniques have centered on bony fixation, which are broadly categorized into onlay and inlay modalities.1,2 Onlay methods secure the tendon to the humeral cortical surface using suture anchors or unicortical buttons. Conversely, inlay techniques integrate the tendon within the cortex via interference screws or bicortical buttons. Inlay techniques have been found to have greater fixation strength but at the cost of an increased risk of humeral fractures due to the bone tunnel, as well as an increased risk of overall revision.3, 4, 5 Contributing to the increased revision rate of inlay fixation techniques is the difficulty in maintaining the natural length-tension dynamics of the long head of the biceps tendon (LHBT). In most inlay techniques, the origin of the LHBT must be separated from the supraglenoid tubercle prior to fixation. This complicates postfixation tensioning on the biceps muscle because excessive tension can precipitate musculocutaneous nerve palsy whereas insufficient tension risks biceps cramping and the Popeye deformity.6, 7, 8, 9 However, despite the extensive amount of literature that exists regarding fixation approaches for biceps tenodesis, there has yet to be a consensus on which method is clinically superior.10,11
Our institution has developed 2 variations of an onlay technique that use both an all-suture anchor and a button. This simplified loop-and-tack method creates a minimal, 1.8-mm perforation in the humeral cortex and offers the advantage of being executed arthroscopically in under 5 minutes without the need for a cannula. Notably, it allows for the anatomic length-tension relationship to be maintained because there is fixation prior to tendon release. Although the technical benefits of the technique are clear, the biomechanical properties remain unknown.
The purpose of this study was to assess the biomechanical performance of 2 simplified loop-and-tack biceps tenodesis techniques, all-suture anchor and all-suture anchor with a button, compared with the interference screw technique in an ovine model. The study’s null hypothesis was that our all-suture anchor techniques with a button and without a button would be inferior to the interference screw standard-of-care technique in end-cycle stiffness.
Methods
Trial Design
Ovine tendons have previously been shown to be the best mimics of human tendons and, as such, were chosen for this biomechanical study.12 All animal care procedures adhered to guidelines set by our institution’s animal care and use committee, and this study was approved by the Carilion Clinic Institutional Review Board in July 2020. Twelve mature, female ovine specimens, Suffolk and Dorset crossbreeds, were humanely euthanized via barbiturate overdose as part of an unrelated research initiative. Subsequently, their tissues were preserved at –20°C until required for dissection and fixation. Both front-limb humeri and the hind limb’s superficial flexor digitorum tendon were dissected down and isolated.13, 14, 15, 16 The specimens were then randomly distributed among the 2 experimental groups (all-suture anchor with button and all-suture anchor without button) and the control group (interference screw) in a 1:1:1 ratio. After the intervention (tenodesis), the samples were stored at –20°C until the biomechanical assessment. On the testing day, the samples were thawed in a water bath at room temperature. Subsequent biomechanical outcomes were recorded and analyzed. Samples that could not complete the entire biomechanical evaluation (owing to premature failure) were omitted from the study.
Interventions
Having received identical treatment until tenodesis, the samples were split into their randomized groupings and the tenodesis procedure corresponding to each group was performed. All procedures were performed by the same orthopaedic surgeon (J.R.T.).
Interference Screw
A guide pin was placed 3 cm from the articular margin and then reamed over with a cannulated reamer 8 mm in diameter. This was tapped up to 9 mm to accommodate the large tendon size, which measured 9 mm in diameter. The end of the tendon was then introduced into the bottom of the socket, which was 30 mm in depth, and pinned in place while an 8 × 25-mm cannulated PEEK (polyether ether ketone) interference screw was secured (Fig 1, Fig 2 and Fig 1, Fig 2).
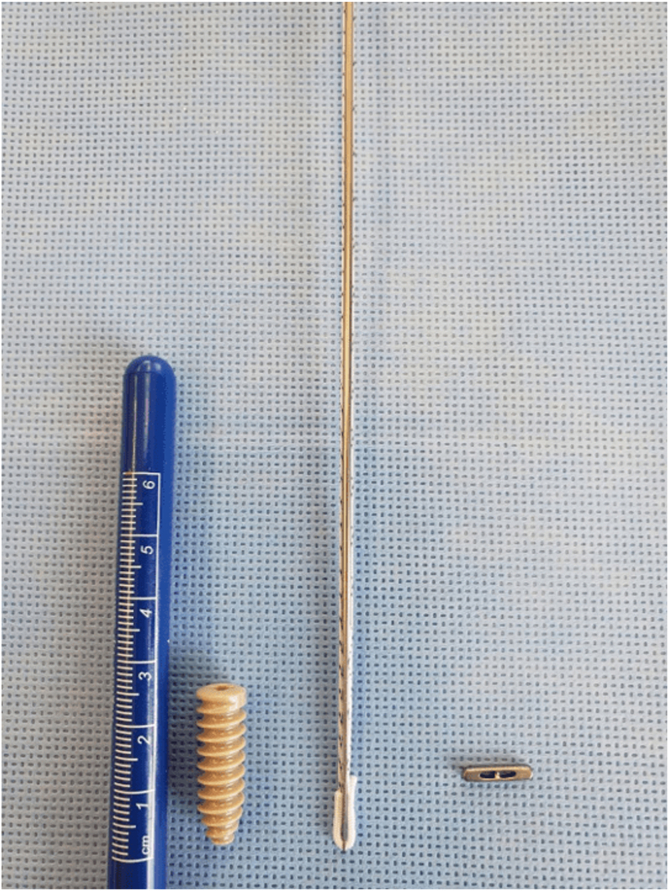
Fig 1.
Fixation materials used for each technique: interference screw (left), all-suture knotless FiberTak anchor (Arthrex, Naples, FL) (middle), and orthopaedic button (right).
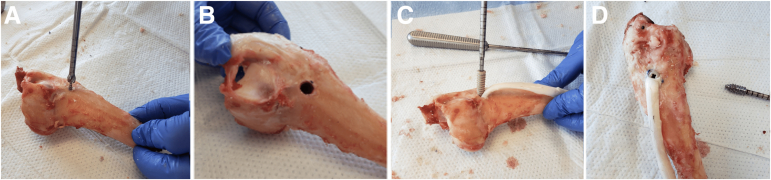
Fig 2.
Interference screw technique. (A) Guide pin with 8-mm reamer. (B) Nine-millimeter osseous tunnel. (C) Introduction of 8 × 25-mm PEEK interference screw with tendon into osseous tunnel. (D) Final interference screw construct.
All-Suture Anchor
The anchor drill guide was placed through the center of the tendon and drilled down in a subcortical manner 3 cm from the articular margin. The anchor was placed through the drill guide and tensioned to anchor under the cortex. The passing suture was then looped around the lateral half of the tendon and passed back through the anchor and tensioned to secure the tendon (Fig 1, Fig 3 and Fig 1, Fig 3).
Fig 3.
All-suture anchor technique. (A) Drill guide through tendon and bone. (B) Anchor tensioned under bone cortex. (C) Passing suture looped around tendon. (D) Final anchor fixation construct.
All-Suture Anchor With Button
The drill guide was placed through the center of the tendon and drilled down in a subcortical manner 3 cm from the articular margin. The anchor was placed through the drill guide and tensioned to anchor under the cortex. The passing suture was threaded through the button and tensioned until the button compressed the tendon to bone (Fig 1, Fig 4 and Fig 1, Fig 4).
Fig 4.
All-suture anchor technique with button. (A) Drill guide through tendon and bone. (B) Passing suture threaded through button. (C) Anchor tensioned with button in place. (D) Final anchor–with–button fixation construct.
Biomechanical Testing and Outcomes
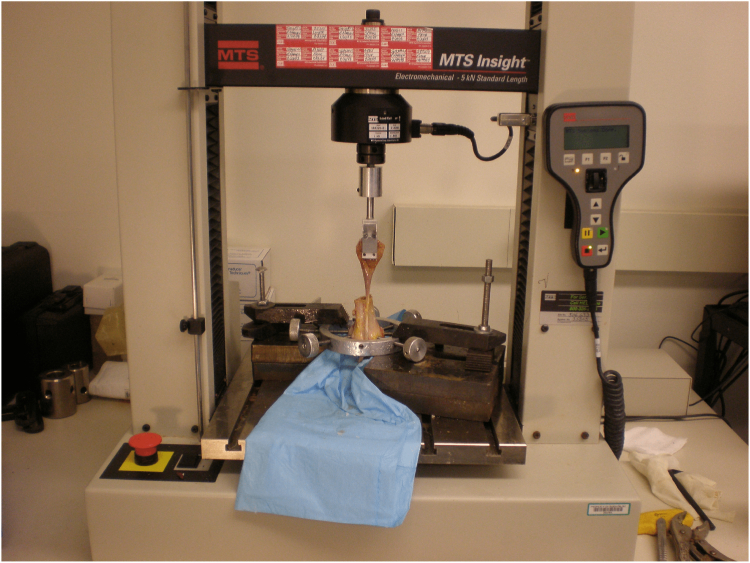
Tendon width and thickness were measured using digital calipers (Absolute AOS Digimatic; Mitutoyo, Kawasaki, Japan) with a precision of 0.01 mm. Thereafter, each tendon-humeral junction was secured in a materials testing system (MTS Insight 10; MTS Systems, Eden Prairie, MN) for biomechanical evaluation (Fig 5). A custom-made soft-tissue cryo-clamp, designed to minimize tendon slippage under tensile loads, was affixed to the test actuator and inline 1,000-N load cell. In addition, a custom threaded jig stabilized the humeral head on the materials testing system’s platform.17 This configuration ensured that tensile forces during the test aligned with the longitudinal axis of the humerus, mirroring the in vivo force vector of the LHBT.
Fig 5.
Materials testing system for tendon constructs.
Dry ice was placed within the chutes of the cryo-clamp just prior to testing. The load sequence included a preload of 5 N sustained for 1 minute, followed by cyclic loading spanning 100 cycles between 5 and 70 N at ⅓ Hz (1 cycle every 3 seconds) and culminating in a load-to-failure test at a rate of 1 mm/s.17,18 The secondary outcome ultimate failure load (UFL) was defined as the peak force observed during the load-to-failure evaluation as, at the point of failure, there is an abrupt drop in the measured load as the tendon construct deforms. To maintain the tendon graft’s condition, it was periodically moistened with saline solution. Time, force, and actuator displacement were continuously acquired at 50 Hz during testing using MTS Systems TestWorks Elite software.
From the cyclic loading phase, construct creep (defined as the tendon’s net elongation after cyclic loading) was computed as the net crosshead displacement between the average peaks of the initial and final 5 cycles. Stiffness is a measure of how much force is required for a tendon to deform. Two distinct stiffness measures were identified as primary and secondary outcomes: end-cycle stiffness and load-to-failure stiffness, respectively. The former was derived from the 95th to 100th cycles during cyclic loading, representing the average absolute difference in the peak-to-valley force normalized to the difference in the peak-to-valley crosshead displacement. The latter, load-to-failure stiffness, was the slope of the linear region of the force-displacement curve during the subsequent load-to-failure test.17,18 End-cycle stiffness was used to model the resistance of the construct to the low-force activities of postoperative physical therapy. In contrast, load-to-failure stiffness could correlate to the resistance of the construct to traumatic injury.
The yield load—the force at which the fixation began to “break” or deform—was identified from the force-displacement curve as the point at which there was a 40% decline in the slope of the linear region. This was computed using a custom-written MATLAB computer code (The MathWorks, Natick, MA). Finally, direct observation was used to determine the mode and location of failure.
Statistical Methods
The sample size was calculated a priori for a continuous-outcome, noninferiority trial with 0.8 power and an α of 5%. In addition to the assumption of a standard deviation of 7 N/mm in the primary outcome, end-cycle stiffness, the noninferiority limit—which was also the minimal clinically important difference (MCID)—was chosen to be –15 N/mm. These parameters were informed by clinical expertise and the findings of prior biomechanical studies.10,19 The resultant minimum sample size requirement was determined to be 7 specimens per group, totaling 21 samples across the study.
The difference-of-means test was used to compare the end-cycle stiffness of the experimental groups against the control group. For the experimental technique to be deemed inferior, both the average and the 95% confidence interval (CI) of the difference in means should fall below the MCID (–15 N/mm). After validation of data normality using the Kolmogorov-Smirnov test, a 1-way analysis of variance was applied to compare all variables across the 3 groups.
Results
Of the 21 samples tested, 19 completed testing and were included in the analysis. Two samples, 1 in the all-suture anchor group and 1 in the group receiving an all-suture anchor with a button, failed at cyclic loading cycles 74 and 7, respectively, and were excluded from the analysis both because the primary outcome could not be determined and because the failures were possibly confounded by outside factors. One sample was noted to have been damaged before testing, possibly during storage, and the other slipped from the testing rig and failed definitively on a second loading attempt. Both the all-suture anchor techniques, without a button and with a button, were found to be noninferior in end-cycle stiffness to the interference screw technique (–5.2 N/mm [95% CI, –13.6 to 3.3 N/mm] and –3.8 N/mm [95% CI, –12.5 to –4.9 N/mm], respectively) with an MCID of –15 N/mm.
In terms of secondary outcomes, the all-suture techniques showed significantly lower UFL, lower yield load, greater creep, and lower load-to-failure stiffness. Tendon geometry did not vary significantly across groups (Table 1). Graphical analyses of both the UFL distribution and the difference-of-means analysis of end-cycle stiffness are provided in Fig 6, Fig 7 and Fig 6, Fig 7, respectively.
Table 1.
Comparison of Recorded Biomechanical Characteristics by Technique
| Interference Screw (n = 7) | All-Suture Anchor (n = 6) | All-Suture Anchor With Button (n = 6) | P Value | |
|---|---|---|---|---|
| Stiffness, N/mm, mean (SD) | ||||
| End cycle | 33.1 (8.3) | 28.0 (6.0) | 29.4 (5.3) | .354 |
| Load to failure | 35.2 (5.9) | 10.6 (4.1) | 17.9 (6.4) | <.001 |
| Ultimate failure load, N, mean (SD) | 362.7 (105.6) | 164.3 (28.4) | 101.7 (14.9) | <.001 |
| Yield load, N, mean (SD) | 264.9 (124.4) | 93.7 (15.5) | 86.8 (9.2) | <.001 |
| Creep, mm, mean (SD) | 1.7 (1.3) | 10.1 (5.7) | 7.1 (2.4) | .002 |
| Tendon, mm, mean (SD) | ||||
| Width | 7.5 (0.5) | 7.8 (0.4) | 7.8 (0.8) | .516 |
| Thickness | 4.2 (0.5) | 4.1 (0.6) | 4.3 (0.4) | .784 |
| Method of failure, n | ||||
| Tendon tear at grip site | 4 | 0 | 0 | |
| Tendon tear at fixation site | 3 | 6 | 6 | |
| Hardware failure at fixation site | 0 | 0 | 0 |
NOTE. P values reflect analysis-of-variance testing.
SD, standard deviation.
Fig 6.
Box plot graph of ultimate failure load with scatter plot overlay. Each box represents the respective interquartile range from first to third quartile with central line at the median. Whiskers extend to the furthest data point within 1.5 times the interquartile range. Diamonds denote outliers greater than 1.5 times the interquartile range. Colored dots represent the individual data points.
Fig 7.
Noninferiority, difference-of-means testing between all-suture anchor techniques and interference screw technique.
For the all-suture anchor techniques without a button and with a button, the failure mode was universally tendon tearing at the fixation site. However, for the interference screw technique, 57.1% of tendons (n = 4) tore at the grip site (tendon–cryo-clamp interface) whereas 42.9% (n = 3) tore at the fixation site (Table 1).
Discussion
This study found that although the all-suture anchor techniques with a button and without a button were noninferior to the interference screw technique in end-cycle stiffness, the primary outcome, they were significantly inferior in all measured secondary metrics, including UFL, which calls into question their potential clinical application. A recent editorial questioned whether strain, indicated by elongation after cyclic loading, or strength, indicated by UFL, is more important when evaluating a fixation technique for biceps tenodesis.20 Because the clinically acceptable ranges of strength and strain are unknown, the trend in ex vivo models has been to choose the technique that offers the highest strength and lowest strain. As such, end-cycle stiffness, our primary outcome, is arguably among the most important biomechanical metrics when comparing tenodesis techniques. However, although noninferiority was seen in this outcome, these techniques were inferior to the standard of care in most secondary outcomes, particularly UFL. Additionally, although significantly inferior to the measured UFL of this study’s interference screw group (362.7 N), the UFL values of the all-suture groups (101.7 N and 164.3 N) are comparable to the UFL ranges of common fixation techniques found in the literature. In a biomechanical comparison study of 6 commonly used biceps tenodesis fixation techniques by Diaz et al.,21 UFL ranged from only 79 N to 136 N. A diminished time-zero UFL, although indicative of immediate postoperative construct strength, does not necessarily translate to long-term fixation outcomes. The dichotomy between the biomechanical superiority of inlay methods and their equivalent clinical outcomes to onlay techniques is a testament to this.1 Patients, barring subsequent traumatic injuries, may not exert excessive forces on the postoperative tendon during the healing phase. Thus, although the construct might succumb under high forces, it remains resilient under the low to moderate forces typically experienced postoperatively. This resilience was captured in our analysis by end-cycle stiffness that was comparable between our techniques and the gold standard. For reference, the constructs failed above 20 lb of force (>100 N of force). This threshold should exceed loads experienced within the immediate postoperative period.
An important observation in our study was that most samples failed at the soft-tissue fixation interface. In the anchor groups, failure was characterized by the tendon tearing longitudinally, whereas in the interference screw group, a transverse break at the screw site was common (Table 1). Notably, osseous fixation was consistent across the study, with all anchors and interference screws remaining embedded in bone, implying that the weak link was the tendon-implant interface. These findings provide insight into clinical failure as well. A tenodesis that fails at the tendon interface may lead to symptoms but is unlikely to require a reoperation. On the other hand, an implant that pulls out of bone, such as an interference screw, may itself cause symptoms that would require surgical removal. These data confirm that these implants will reliably remain within bone if the bone quality is optimal. Conversely, if poor bone quality is encountered, a 1.8-mm all-suture anchor may be preferable to the 8 × 25-mm PEEK screw if either were to pull out of the bone into the soft tissue of the arm.
The 2 experimental techniques explored in this study were developed to allow for fixation of the biceps tendon at native, anatomic tension, as well as to allow for a reliable, reproducible, and efficient procedure that could be performed arthroscopically. The goal of this biomechanical study is to confirm that these techniques are strong enough at time zero to justify their clinical use and further study. The degree of healing after all-suture anchor techniques will be studied in future experiments.
Limitations
This study is not without limitations. Because we used an ovine tendon model, which closely approximates human tendon but not bone, direct extrapolation of our results to human subjects may not be warranted.12 Study logistics necessitated multiple freeze-thaw cycles of the samples, which could potentially influence tendon biomechanical properties.22 Furthermore, this ex vivo analysis (based on cadaveric tissue) does not account for tissue healing or remodeling that very likely influences the clinical outcomes of these fixation techniques. Moreover, the uniform optimal bone quality observed in our samples might not represent the osteoporotic bone of the elderly patients who typically undergo tenodesis procedures. Finally, although biomechanical studies provide valuable insights into the mechanical attributes of different techniques, they are not indicative of clinical outcomes. Thus, their primary function should be to guide more comprehensive, clinically oriented research.
Conclusions
Under subfailure loading conditions, the all-suture anchor techniques with a button and without a button showed end-cycle stiffness noninferiority to an interference screw technique; however, these techniques were inferior in all secondary outcomes, including significantly lower UFL, lower yield load, greater creep, and lower load-to-failure stiffness.
Disclosures
All authors (K.C., E.R., N.J.P., V.W., J.R.T.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors thank Julianne Wood and Austin Petty for assistance with protocol development, tissue preparation, and technical assistance.
References
- 1.Jackson G.R., Meade J., Coombes K., et al. Onlay versus inlay biceps tenodesis for long head of biceps tendinopathy: A systematic review and meta-analysis. J Am Acad Orthop Surg Glob Res Rev. 2022;6:e22. doi: 10.5435/JAAOSGlobal-D-22-00255. 00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scheibel M., Schröder R.J., Chen J., Bartsch M. Arthroscopic soft tissue tenodesis versus bony fixation anchor tenodesis of the long head of the biceps tendon. Am J Sports Med. 2011;39:1046–1052. doi: 10.1177/0363546510390777. [DOI] [PubMed] [Google Scholar]
- 3.Richards D.P., Burkhart S.S. A biomechanical analysis of two biceps tenodesis fixation techniques. Arthroscopy. 2005;21:861–866. doi: 10.1016/j.arthro.2005.03.020. [DOI] [PubMed] [Google Scholar]
- 4.Beason D.P., Shah J.P., Duckett J.W., Jost P.W., Fleisig G.S., Cain E.L. Torsional fracture of the humerus after subpectoral biceps tenodesis with an interference screw: A biomechanical cadaveric study. Clin Biomech (Bristol, Avon) 2015;30:915–920. doi: 10.1016/j.clinbiomech.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Haidamous G., Noyes M.P., Denard P.J. Arthroscopic biceps tenodesis outcomes: A comparison of inlay and onlay techniques. Am J Sports Med. 2020;48:3051–3056. doi: 10.1177/0363546520952357. [DOI] [PubMed] [Google Scholar]
- 6.Virk M.S., Nicholson G.P. Complications of proximal biceps tenotomy and tenodesis. Clin Sports Med. 2016;35:181–188. doi: 10.1016/j.csm.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Werner B.C., Lyons M.L., Evans C.L., et al. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: A comparison of restoration of length-tension and mechanical strength between techniques. Arthroscopy. 2015;31:620–627. doi: 10.1016/j.arthro.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 8.Chen R.E., Voloshin I. Long head of biceps injury: Treatment options and decision making. Sports Med Arthrosc Rev. 2018;26:139–144. doi: 10.1097/JSA.0000000000000206. [DOI] [PubMed] [Google Scholar]
- 9.Lim T.K., Moon E.S., Koh K.H., Yoo J.C. Patient-related factors and complications after arthroscopic tenotomy of the long head of the biceps tendon. Am J Sports Med. 2011;39:783–789. doi: 10.1177/0363546510388158. [DOI] [PubMed] [Google Scholar]
- 10.Dekker T.J., Peebles L.A., Preuss F.R., Goldenberg B.T., Dornan G.J., Provencher M.T. A systematic review and meta-analysis of biceps tenodesis fixation strengths: Fixation type and location are biomechanically equivalent. Arthroscopy. 2020;36:3081–3091. doi: 10.1016/j.arthro.2020.05.055. [DOI] [PubMed] [Google Scholar]
- 11.Aida H.F., Shi B.Y., Huish E.G., McFarland E.G., Srikumaran U. Are implant choice and surgical approach associated with biceps tenodesis construct strength? A systematic review and meta-regression. Am J Sports Med. 2020;48:1273–1280. doi: 10.1177/0363546519876107. [DOI] [PubMed] [Google Scholar]
- 12.Hausmann J.T., Vekszler G., Bijak M., Benesch T., Vécsei V., Gäbler C. Biomechanical comparison of modified Kessler and running suture repair in 3 different animal tendons and in human flexor tendons. J Hand Surg Am. 2009;34:93–101. doi: 10.1016/j.jhsa.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Hapa O., Günay C., Kömürcü E., Çakıcı H., Bozdağ E. Biceps tenodesis with interference screw: Cyclic testing of different techniques. Knee Surg Sports Traumatol Arthrosc. 2010;18:1779–1784. doi: 10.1007/s00167-010-1180-7. [DOI] [PubMed] [Google Scholar]
- 14.Hirpara K.M., Abouazza O., O’Neill B., O’Sullivan M. A technique for porcine flexor tendon harvest. J Musculoskelet Res. 2012;10:181–186. [Google Scholar]
- 15.Jayamoorthy T., Field J.R., Costi J.J., Martin D.K., Stanley R.M., Hearn T.C. Biceps tenodesis: A biomechanical study of fixation methods. J Shoulder Elbow Surg. 2004;13:160–164. doi: 10.1016/j.jse.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Kusma M., Dienst M., Eckert J., Steimer O., Kohn D. Tenodesis of the long head of biceps brachii: Cyclic testing of five methods of fixation in a porcine model. J Shoulder Elbow Surg. 2008;17:967–973. doi: 10.1016/j.jse.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 17.Salata M.J., Bailey J.R., Bell R., et al. Effect of interference screw depth on fixation strength in biceps tenodesis. Arthroscopy. 2014;30:11–15. doi: 10.1016/j.arthro.2013.08.033. [DOI] [PubMed] [Google Scholar]
- 18.Slabaugh M.M.A., Frank R.M., Van Thiel G.S., et al. Biceps tenodesis with interference screw fixation: A biomechanical comparison of screw length and diameter. Arthroscopy. 2011;27:161–166. doi: 10.1016/j.arthro.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 19.Smuin D.M., Vannatta E., Ammerman B., Stauch C.M., Lewis G.S., Dhawan A. Increased load to failure in biceps tenodesis with all-suture suture anchor compared with interference screw: A cadaveric biomechanical study. Arthroscopy. 2021;37:3016–3021. doi: 10.1016/j.arthro.2021.03.085. [DOI] [PubMed] [Google Scholar]
- 20.Provencher M.T., Peebles A.M. Editorial commentary: What is more important: Strength or displacement? Findings of all-suture anchor versus interference screw for biceps tenodesis. Arthroscopy. 2021;37:3022–3024. doi: 10.1016/j.arthro.2021.06.009. [DOI] [PubMed] [Google Scholar]
- 21.Diaz M., Shi B.Y., Baker M.C., Binkley M.T., Belkoff S.M., Srikumaran U. Open biceps tenodesis: A biomechanical comparison of 6 fixation techniques. Orthopedics. 2020;43:E102–E108. doi: 10.3928/01477447-20200107-03. [DOI] [PubMed] [Google Scholar]
- 22.Giannini S., Buda R., Di Caprio F., et al. Effects of freezing on the biomechanical and structural properties of human posterior tibial tendons. Int Orthop. 2008;32:145–151. doi: 10.1007/s00264-006-0297-2. [DOI] [PMC free article] [PubMed] [Google Scholar]