Video
Introduction
According to Wei et al,1 160,000 to 200,000 PEG-tube placements occur each year in the United States. Of these, 1% to 2% have peristomal leakage, but the incidence may be even greater. In a prospective study by Koulentaki et al,2 the authors found that 7% of initial PEG-tube replacements were indicated because of peristomal leakage.
Multiple risk factors are involved, including immunosuppression and some device-related components, such as the skin disc being placed too tightly against the abdominal wall or being set too loosely and thus not creating a seal with the inner bumper. Leakage creates irritation of the surrounding peristomal skin and therefore causes further leakage, often leading to a vicious cycle of continued leakage.
Initial management of peristomal leakage usually involves counseling of patients regarding tampering with the external device, which causes leakage. Also included in the initial management are treatment with barrier creams, instituting antisecretory therapy, and consulting dermatology for wound care. Wound swabs are taken and, if the result is positive, topical antibacterials with topical steroids are prescribed. Upsizing the gastrostomy tube often causes the tract to enlarge and exacerbates the leak, and the last resort is to remove the PEG tube and replace it at a different site.3 We describe a novel approach using a simple, small-caliber suction tube placed in the space around the gastrostomy site and under the skin disc connected to a negative-pressure source to address the persistent peristomal leak. The principle behind the technique is to create a system that constantly aerates the surrounding skin and suctions the extravasated contents through a continuous negative-pressure source attached to the suction tube.
Case presentation
A 75-year-old man with a history of esophageal adenocarcinoma status post-chemotherapy, radiation, and Ivor Lewis esophagectomy presented with persistent leakage around the immature tract of the percutaneous endoscopic jejunostomy tube (20F balloon) site (placed 2 weeks previously) as the result of oropharyngeal dysphagia that was unresponsive to conservative management with proton pump inhibitor therapy and barrier creams in consultation with dermatology (Fig. 1). Skin erythema, drainage, and ulceration were found surrounding the stomal opening. We used a locking multipurpose pigtail catheter (8.5F; Cook Medical, Bloomington, Ind, USA) and sutured this to the part of the external disc in contact with the skin with the holes in the loop facing centrally (as shown in Video 1, available online at www.videogie.org). Alternatively, a 10F nasojejunal tube threaded into the holes of the skin disc/external bolster can be used with perforations made such that they are in close contact with the skin (as shown in Video 1).
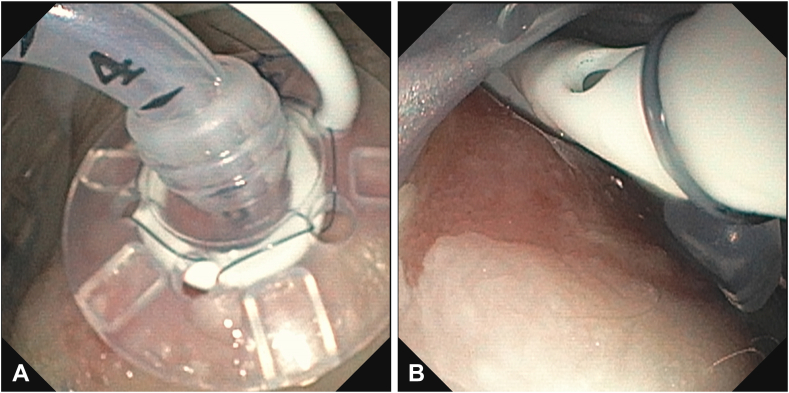
Figure 1.
A, Shows a percutaneous endoscopic jejunostomy tube with a multipurpose drainage catheter drain sutured to the skin disc/external bolster. B, Shows the holes in the multipurpose drainage catheter facing centrally towards the leak site.
The disc aerator apparatus was placed back on to the jejunostomy tube, and then the tube was attached to a continuous negative-pressure suction source of 100 mm Hg (Figs. 2 and 3). On postprocedure day 4, the leakage had significantly improved, leading to substantial reduction of the inflammation around the percutaneous endoscopic jejunostomy tube site (Fig. 4). We have successfully managed 5 cases of persistent peristomal leak using an aerator device, and the mean time for healing in these cases was 5 days.
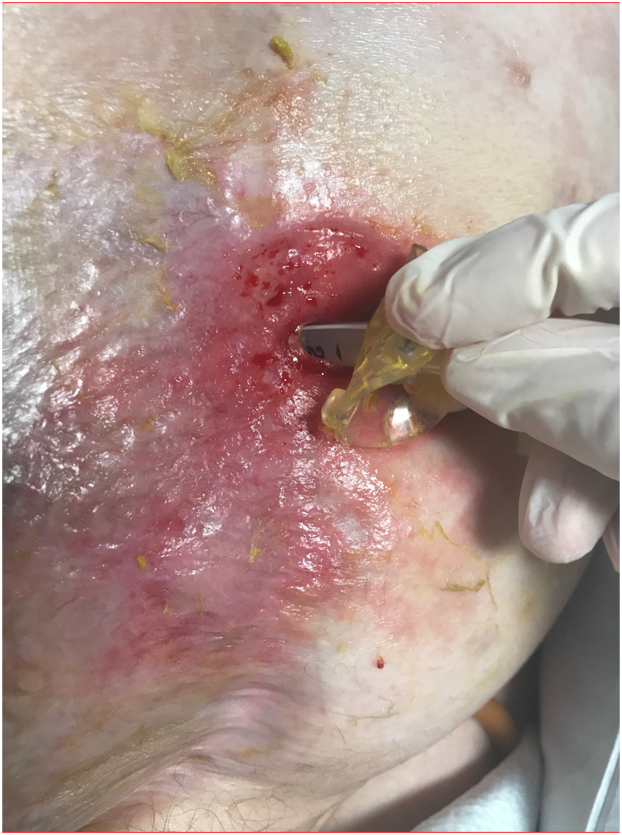
Figure 2.
Persistent peristomal leakage and inflammation around the percutaneous endoscopic jejunostomy tube site is shown.
Figure 3.
PEG tube is shown with a perforated nasojejunal tube threaded through the holes of the skin disc/external bolster.
Figure 4.
Postprocedure image showing decreased leakage after placement of the aerator device.
Conclusions
We describe the modification of a gastrostomy/jejunostomy tube at the initial site to prevent and treat persistent peristomal leakage. The materials required are readily accessible in endoscopy suites, and the device assembly is straightforward. The combination of using a gastrostomy tube with a small-caliber suction tube for the drainage of extravasated contents and providing aeration to the wound promotes wound healing and thereby halts the continuous cycle of leakage and inflammation. This approach is suitable for patients in whom conservative management of peristomal leakage has failed, and its use could avoid unnecessary PEG-tube replacement.
Disclosure
All authors disclosed no financial relationships.
Supplementary data
1Preparation of an aerator tube with a locking loop multipurpose drainage catheter drain and preparation of an aerator tube with a perforated nasojejunal tube.
References
- 1.Wei M., Ho E., Hegde P. An overview of percutaneous endoscopic gastrostomy tube placement in the intensive care unit. J Thorac Dis. 2020;13:5277–5296. doi: 10.21037/jtd-19-3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koulentaki M., Reynolds N., Steinke D., et al. Eight years' experience of gastrostomy tube management. Endoscopy. 2002;34:941–945. doi: 10.1055/s-2002-35843. [DOI] [PubMed] [Google Scholar]
- 3.Schrag S.P., Sharma R., Jaik N.P., et al. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis. 2007;16:407–418. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1Preparation of an aerator tube with a locking loop multipurpose drainage catheter drain and preparation of an aerator tube with a perforated nasojejunal tube.