Abstract
BACKGROUND
Hyperplastic polyps, which represent 30%-93% of all gastric epithelial polyps, are the second most common type of gastric polyps after fundic gland polyps. They were previously considered to have no risk of neoplastic transformation. Recently, an increasing number of cases of gastric hyperplastic polyps (GHPs) combined with neoplastic changes have been reported; however, the specific mechanism underlying their transformation has not been thoroughly explored.
AIM
To investigate the clinical, endoscopic, and pathological characteristics of the neoplastic transformation of GHPs and explore the risk factors.
METHODS
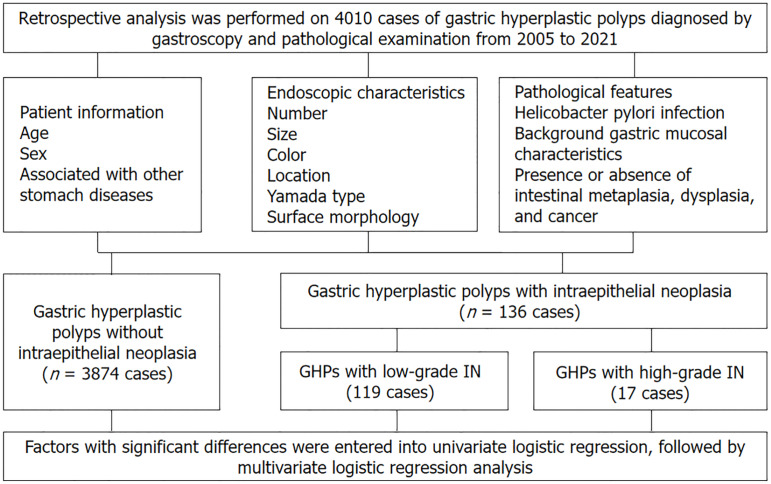
A retrospective analysis was performed on 4010 cases of GHPs diagnosed by gastroscopy and pathological examination at the hospital from 2005 to 2021. In total, 3874, 119, and 17 cases were in the group without intraepithelial neoplasia (IN), with low-grade IN, and with high-grade IN, respectively. The data analysis examined the association of endoscopic and pathological features with risk factors for neoplastic transformation. Factors with significant differences were entered into univariate logistic regression, followed by multivariate logistic regression analysis.
RESULTS
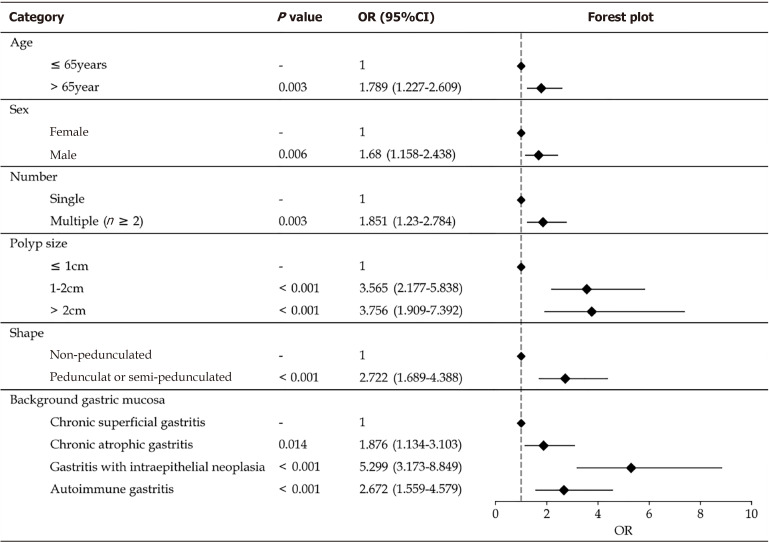
Univariate analysis revealed diameter, multiple polyp presence, redness, rough surface, lobulation, erosion, Yamada classification, location, and gastric mucosa were risk factors for neoplastic transformation. Multivariate analysis showed that age > 65 years [odds ratio (OR) = 1.789; 95% confidence interval (CI): 1.227-2.609; P = 0.003], male sex (OR = 1.680; 95%CI: 1.158-2.438; P = 0.006), multiple polyps (OR = 1.851; 95%CI: 1.230-2.784; P = 0.003), pedunculated or semi-pedunculated shape (OR = 2.722; 95%CI: 1.689-4.388; P < 0.001), and polyp diameter were significantly associated with GHPs that demonstrated neoplastic transformation. Compared with chronic superficial gastritis, autoimmune gastritis, atrophic gastritis, and gastritis with IN were independent risk factors for neoplastic transformation [(OR = 2.672; 95%CI: 1.559-4.579; P < 0.001), (OR = 1.876; 95%CI: 1.134-3.103; P = 0.014), and (OR = 5.299; 95%CI: 3.173–8.849; P < 0.001), respectively].
CONCLUSION
Male sex, age > 65 years, multiple polyps, pedunculated or semi-pedunculated shape, polyp size > 1 cm, and specific background gastric mucosa are key indicators for predicting neoplastic transformation of GHPs.
Keywords: Endoscopy, Gastric hyperplastic polyps, Neoplastic transformation, Pathology, Risk factors, Tumour
Core Tip: Our results show that larger diameter, the presence of multiple polyps, pedunculated or semi-pedunculated shape, and specific background gastric mucosa were risk factors for neoplastic transformation. Furthermore, age > 65 years and male sex were important indicators for predicting the risk of malignant transformation of gastric hyperplastic polyps. Our findings suggest that for polyps with the abovementioned endoscopic and pathological features, clinicians should be alert to the possibility of neoplastic transformation to improve the diagnosis rate of the neoplastic transformation of gastric hyperplastic polyps. Additionally, our study showed that Helicobacter pylori infection was not associated with the risk.
INTRODUCTION
Gastric hyperplastic polyps (GHPs) are the second most common type of gastric polyps after fundic gland polyps[1]. They typically do not cause obvious clinical symptoms and were previously considered to have no risk of neoplastic transformation. Recently, an increasing number of reports have emerged on GHPs combined with neoplastic change; however, the specific mechanism has not been thoroughly explored[2,3]. While our understanding of the neoplastic transformation mechanism of GHPs remains limited, knowledge regarding this condition is continuously advancing. Further research will contribute to a better understanding of the development of GHPs and provide more accurate diagnostic and treatment strategies for patients. Therefore, this study aimed to identify the endoscopic and pathological features of GHPs and discuss the risk of neoplastic transformation associated with these features to assist in clinical diagnosis and treatment.
MATERIALS AND METHODS
Study design and patients
This was a retrospective, single-centre study conducted at Peking University Third Hospital from 1 January 2005 to 31 December 2021. All patients were treated by endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), or endoscopic forceps removal and were pathologically diagnosed as hyperplastic polyps. The inclusion criteria for patients were age ≥ 18 years, polyp diagnosis based on gastroscopy morphology, and hyperplastic polyp diagnosis based pathology. In contrast, the exclusion criteria were familial adenomatous polyposis, juvenile polyposis, Peutz-Jeghers syndrome, and Cronkhite–Canada syndrome. Ultimately, 4010 cases were enrolled in this study.
The Ethics Committee (No. M2023153) of the Peking University Third Hospital approved this clinical study and its protocol was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was not required from the patients due to the retrospective nature of the study.
Data collection
Patient information, such as age and sex, was retrospectively collected from medical records. Detailed characteristics, including the location, presence of single or multiple polyps, size, endoscopic appearance of polyp (Yamada’s classification of polyps, mucosal erosion, lobulation, and surface roughness), and pathological features (presence or absence of dysplasia and adenocarcinoma) of polyps were examined. Background gastric mucosal characteristics (chronic superficial gastritis, chronic atrophic gastritis with or without intraepithelial neoplasia, and autoimmune gastritis) were also considered. A skilled pathologist assessed the gastric mucosal background. The location of GHPs in the stomach was classified as the lower third comprising the gastric antrum and angle; the middle third consisting of the lower and mid-body regions of the stomach; and the upper third comprising the fundus, cardia, and high-body of the stomach. Additionally, the presence or absence of Helicobacter pylori (H. pylori) was assessed using histological examination of biopsy specimens, H. pylori Warthin-Starry silver staining, or 13C-urea breath tests. H. pylori status was considered positive if any of these test results were positive. GHPs with neoplasia were defined as those with histopathological confirmation of dysplasia or cancerous lesions in the endoscopically resected specimens. At least two pathologists confirmed each case with neoplasia. Further details are presented in Figure 1.
Figure 1.
Flow diagram of date collection. GHPs: Gastric hyperplastic polyps; IN: Intraepithelial neoplasia.
Research methods
Patients’ basic information, in addition to gastroscopic and histopathological data, was retrospectively analyzed. According to histopathological results, hyperplastic polyps were categorised into hyperplastic polyps without intraepithelial neoplasia, with low-grade intraepithelial neoplasia, and with high-grade intraepithelial neoplasia, in which low-grade intraepithelial neoplasia included mild and moderate dysplasia whereas high-grade intraepithelial neoplasia comprised a high-grade dysplasia and carcinogenesis. Factors that influence neoplastic transformations were also analyzed. Neoplastic transformations were defined histologically by the presence of dysplasia or adenocarcinoma within GHPs. Further details are presented in Figure 1.
Statistical analysis
All statistical analyses were performed using Statistical Product and service solutions statistics for windows, version 26.0 (international business machines corporation, Armonk, NY, United States). Normally distributed measurement data are expressed as mean ± SD, and comparisons between groups were made using ordinary analysis of variance and independent sample t-test. Non-normally distributed measurement data are presented as median (range). Count data are expressed as percentages, and χ2 or Fisher’s exact test was used for comparisons between groups. Factors with significant differences were entered into univariate logistic regression, followed by multivariate logistic regression analysis. The results were determined using odds ratio (OR) and 95% confidence interval (CI). Statistical significance was set at P < 0.05.
RESULTS
General patient information
Between 2005 and 2021, 4010 cases of GHPs were confirmed based on gastroscopy and pathological examination at our hospital. Among these, 3874, 119, and 17 cases were in the groups without intraepithelial neoplasia, with low-grade intraepithelial neoplasia, and with high-grade intraepithelial neoplasia (5 cases with high-grade dysplasia and 12 with carcinogenesis), respectively. The mean ages of patients in the hyperplastic polyp, low-grade intraepithelial neoplasia, and high-grade intraepithelial neoplasia groups were 57.86 ± 0.22, 64.49 ± 1.13, and 67.93 ± 2.55 years, respectively. Continuous variables were transformed into grade variables, namely age (≤ 45, 45-65, and > 65 years), revealing significant differences. The age of patients in the neoplastic transformation group increased significantly. In terms of sex, GHPs without intraepithelial neoplasia were found more frequently in females (63%). In total, 49% of patients were male in the intraepithelial neoplasia group. The number of male patients significantly differed among the groups (P < 0.05). H. pylori infection was observed in 20%, 17%, and 12% of patients in the GHPs without intraepithelial neoplasia, with low-grade intraepithelial neoplasia, and with high-grade intraepithelial neoplasia groups, respectively, with no significant difference. Further details are presented in Table 1 and Table 2.
Table 1.
Features of gastric hyperplastic polyps in different groups and univariate logistic regression analysis of risk factors for neoplastic transformation
|
|
GHPs without IN (n = 3874)
|
GHPs with IN (n = 136) |
χ
2 test
|
Univariate analysis
|
||
|
χ
2 value
|
P value
|
P value
|
OR (95%CI)
|
|||
| Age (mean ± SD), years | 57.86 ± 0.22 | 64.76 ± 1.04 | 37.178 | < 0.001 | < 0.001 | 1.761 (1.459-2.126) |
| ≤ 45 years, n (%) | 699 (18) | 9 (6) | ||||
| 45-65 years, n (%) | 1988 (51) | 54 (40) | ||||
| > 65 years, n (%) | 1187 (31) | 73 (54) | ||||
| Sex, n (%) | 9.057 | 0.011 | 0.003 | 1.672 (1.188-2.356) | ||
| Male | 1423 (37) | 67 (49) | ||||
| Female | 2451 (63) | 69 (51) | ||||
| H. pylori infection, n (%) | 782 (20) | 22 (16) | 1.865 | 0.172 | 0.174 | 0.721 (0.450-1.155) |
| Multiple polyps, n (%) | 1122 (29.4) | 62 (46) | 23.162 | < 0.001 | < 0.001 | 2.275 (1.614-3.207) |
| Polyp size (mean ± SD), cm | 0.66 ± 0.01 | 203.055 | < 0.001 | < 0.001 | 3.634 (2.948-4.478) | |
| ≤ 1 cm | 3406 (88) | 66 (48) | ||||
| 1 cm-2 cm | 374 (10) | 53 (39) | ||||
| > 2 cm | 94 (2) | 17 (13) | ||||
| Endoscopic color, n (%) | 18.626 | < 0.001 | 0.03 | 0.671 (0.472-0.972) | ||
| Normal | 2113 (55) | 53 (40) | ||||
| Red | 1488 (40) | 82 (60) | ||||
| White | 275 (5) | 1 (0) | ||||
| Mucosal erosion, n (%) | 289 (8) | 30 (22) | 38.701 | < 0.001 | < 0.001 | 3.538 (2.318-5.402) |
| Polyp lobulation, n (%) | 185 (5) | 25 (18) | 49.109 | < 0.001 | < 0.001 | 4.491 (2.840-7.102) |
| Mucosal roughness, n (%) | 864 (22) | 69 (51) | 59.494 | < 0.001 | < 0.001 | 3.588 (2.542-5.064) |
| Endoscopic classification, n (%) | 169.676 | < 0.001 | < 0.001 | 2.604 (2.210-3.067) | ||
| I | 2480 (64) | 35 (26) | ||||
| II | 1007 (26) | 42 (31) | ||||
| III | 233 (6) | 27 (20) | ||||
| IV | 155 (4) | 32 (23) | ||||
| Location, n (%) | 23.926 | < 0.001 | < 0.001 | 1.750 (1.384-2.212) | ||
| Upper third | 1457 (38) | 31 (23) | ||||
| Middle third | 1715 (44) | 60 (44) | ||||
| Lower third | 702 (18) | 45 (33) | ||||
| Background gastric mucosa, n (%) | 81.877 | < 0.001 | < 0.001 | 1.699 (1.472-1.960) | ||
| Autoimmune gastritis | 364 (9.4) | 29 (21) | ||||
| Chronic superficial gastritis | 2466 (64) | 42 (31) | ||||
| Chronic atrophic gastritis | 712 (18) | 31 (23) | ||||
| Gastritis with IN | 332 (9) | 34 (25) | ||||
OR: Odds ratio; CI: Confidence interval; GHPs: Gastric hyperplastic polyps; IN: Intraepithelial neoplasia; H. pylori: Helicobacter pylori.
Table 2.
Multivariate logistic regression analysis of risk factors for neoplastic transformation of gastric hyperplastic polyps
|
Risk factors
|
P value
|
OR
|
95%CI
|
| Age | |||
| ≤ 65 years | 1 | ||
| > 65 year | 0.003 | 1.789 | 1.227-2.609 |
| Sex | |||
| Female | 1 | ||
| Male | 0.006 | 1.680 | 1.158-2.438 |
| Number | |||
| Single | 1 | ||
| Multiple (n ≥ 2) | 0.003 | 1.851 | 1.230-2.784 |
| Polyp size | |||
| ≤ 1 cm | 1 | ||
| 1 cm-2 cm | < 0.001 | 3.565 | 2.177-5.838 |
| > 2 cm | < 0.001 | 3.756 | 1.909-7.392 |
| Endoscopic color-red | 0.701 | 0.916 | 0.619-1.356 |
| Mucosal erosion | 0.271 | 0.75 | 0.454-1.255 |
| Polyp lobulation | 0.264 | 0.73 | 0.432-1.263 |
| Mucosal roughness | 0.128 | 1.38 | 0.912-2.093 |
| Shape | |||
| Non-pedunculated | 1 | ||
| Pedunculated or semi-pedunculated | < 0.001 | 2.722 | 1.689-4.388 |
| Location, n (%) | |||
| Upper third | 1 | ||
| Middle third | 0.066 | 0.609 | 0.368-1.011 |
| Lower third | 0.055 | 1.624 | 0.968-2.724 |
| Background gastric mucosa | |||
| Chronic superficial gastritis | 1 | ||
| Chronic atrophic gastritis | 0.014 | 1.876 | 1.134-3.103 |
| Gastritis with intraepithelial neoplasia | < 0.001 | 5.299 | 3.173-8.849 |
| Autoimmune gastritis | < 0.001 | 2.672 | 1.559-4.579 |
OR: Odds ratio; CI: Confidence interval.
Endoscopic features
In terms of polyp size, the mean diameters of GHPs without intraepithelial neoplasia, with low-grade intraepithelial neoplasia, and with high-grade intraepithelial neoplasia were 0.66 ± 0.01, 1.25 ± 0.07, and 2.2 ± 0.32 cm, respectively, with significant difference (P < 0.001). Continuous variables were transformed into grade variables, namely polyp size (≤ 1 cm, 1 cm-2 cm, and > 2 cm), revealing significant differences. The diameter of GHPs with intraepithelial neoplasia was significantly larger than in the GHPs group (χ2 = 203.055, P < 0.001), with 82% of GHPs with high-grade intraepithelial neoplasia having a diameter of > 1 cm, which was significantly more frequent than in the low-grade intraepithelial neoplasia group (P < 0.05). Among GHPs without intraepithelial neoplasia, 70.6% were mainly single, while the proportion of multiple polyps increased with lesion progression. Multiple polyps were common (65%) in the high-grade intraepithelial neoplasia group.
According to Yamada’s classification of polyps, simple GHPs were most commonly classified as Yamada type I (64%), while the proportion of polyps that exhibited intraepithelial neoplasia was significantly reduced, only 26% (χ2 = 169.676, P < 0.001). High-grade intraepithelial neoplasia polyps showed a difference with pedunculated or semi-pedunculated shapes, as Yamada types III and IV classifications accounted for 47% and 41% of these polyps, respectively.
GHPs without intraepithelial neoplasia were observed in the upper and middle third of the stomach (38% and 44%, respectively). Polyps with intraepithelial neoplasia were more likely to occur in the middle and lower third of the stomach (44% and 33%, respectively), with significant differences between the groups (χ2 = 23.926, P < 0.001). Additionally, Polyps with high-grade intraepithelial neoplasia were more likely to occur in the middle third of the stomach (65%).
Regarding polyp colour, GHPs without intraepithelial neoplasia were mainly the colour of the surrounding mucosa. The proportion of polyps with redness increased with lesion progression (58% and 76% of polyps in the low-grade and high-grade intraepithelial neoplasia groups, respectively), with significant differences (χ2 = 18.626, P < 0.001). Regarding endoscopic morphology, lesion progression was accompanied by mucosal erosion, increased lobulation, and greater surface roughness, with significant differences between the groups (P < 0.001). Further details are presented in Table 1.
Pathological features
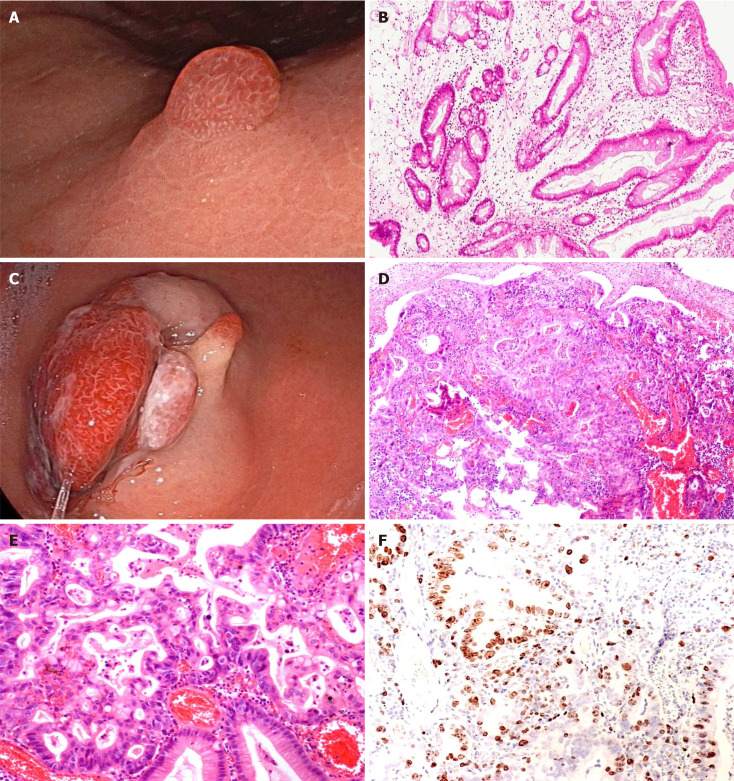
We analyzed the pathological results of all polyps. The incidence of polyps with high-grade dysplasia and carcinogenesis was 3.1% (124/4010) and 0.3% (12/4010), respectively. In the analysis of the background gastric mucosa, significant differences were observed between the groups. The background gastric mucosa of GHPs mainly demonstrated chronic superficial gastritis, accounting for 64%. However, in the group with intraepithelial neoplasia, autoimmune gastritis, atrophic gastritis, and gastritis with intraepithelial neoplasia of the surrounding gastric mucosa were present in 21%, 23%, and 25%, respectively, with significant differences (χ2 = 81.877, P < 0.001) (Table 1). Further details are presented in Figure 2.
Figure 2.
Endoscopic and pathological features of gastric hyperplastic polyps. A: Gastric hyperplastic polyp, smooth surface, same color as surrounding mucosa; B: Pathological manifestation of gastric hyperplastic polyps (Hematoxylin-eosin staining); C: Gastric hyperplastic polyp with carcinomatous transformation, with multiple pedunculated/sub-pedunculated shape, measuring > 3 cm in diameter, rough and red surface; D and E: The pathology of gastric hyperplastic polyp with carcinomatous transformation (Hematoxylin-eosin staining); F: Ki-67 positive of the lesion (immunohistochemical staining).
Univariate and multivariate analyses of the potential risk factors for neoplastic transformation
Univariate and multivariate logistic regression analyses were performed to explore potential associations between risk factors and the presence of neoplastic transformation in GHPs. Low-grade and high-grade intraepithelial neoplasia polyps were combined into one group (GHPs with intraepithelial neoplasia group) and compared with the GHPs without intraepithelial neoplasia group. In the univariate analysis, significant differences were observed in the age and sex of patients, and diameter, endoscopic classification, location, surface morphology (mucosal erosion, lobulation, and surface roughness), and background gastric mucosa of polyps. The differences in these factors between groups were significant (P < 0.05). More specifically, male sex, larger diameter, the presence of multiple polyps, red polyps, rough surface, erosion, and lobulation in the middle third of the stomach, in addition to Yamada type III and IV classifications, with special background gastric mucosa were risk factors for neoplastic transformation. However, no significant difference was observed in terms of H. pylori infection (P > 0.05) (Table 1).
Statistically significant risk factors were included in multivariate logistic regression analysis. They were categorised into two groups according to age (< 65 and ≥ 65 years), while polyps with pedunculated or semi-pedunculated shape (corresponding to Yamada type III and IV classifications) were classified into one group and others polyps were categorised into another group (corresponding to Yamada types I and II). The results showed that age > 65 years (OR = 1.789; 95%CI: 1.227-2.609; P = 0.003], male sex (OR = 1.680; 95%CI: 1.158-2.438; P = 0.006), multiple polyps (OR = 1.851; 95%CI: 1.230-2.784; P = 0.003), and pedunculated or semi-pedunculated shape (OR = 2.722; 95%CI: 1.689-4.388; P < 0.001) were significantly associated with GHPs that demonstrated neoplastic transformation. Additionally, polyp diameter was an independent risk factor for harbouring a neoplasm in GHP. Compared with a size of ≤ 1 cm, diameters of 1 cm-2 cm and > 2 cm significantly differed [(OR = 3.565; 95%CI: 2.177-5.838; P < 0.001), (OR = 3.756; 95%CI: 1.909-7.392; P < 0.001), respectively]. Multivariate analysis also showed that specific background gastric mucosa was an independent risk factor for harbouring a neoplasm in GHPs. Compared with chronic superficial gastritis, autoimmune gastritis, atrophic gastritis, and gastritis with intraepithelial neoplasia were significantly different (OR = 2.672; 95%CI: 1.559-4.579; P < 0.001), (OR = 1.876; 95%CI: 1.134-3.103; P = 0.014), and (OR = 5.299; 95%CI: 3.173-8.849; P < 0.001), respectively] (Table 2). Further details are presented in Table 2. We generated a forest map based on independent risk factors, as shown in Figure 3.
Figure 3.
Forest plot of risks for neoplastic transformation of gastric hyperplastic polyps. OR: Odds ratio; CI: Confidence interval.
GHPs with low-grade and high-grade intraepithelial neoplasia were selected for comparison and univariate regression analysis. The result showed that compared with a size of ≤ 1 cm, a diameter of 1 cm-2 cm significantly differed (OR = 6.956; 95%CI: 1.159-41.729; P < 0.05), and pedunculated or semi-pedunculated shape (OR = 7.375; 95%CI: 1.615-33.671; P < 0.05) were significantly associated with GHPs that demonstrated high-grade intraepithelial neoplasia. No significant difference was found in other univariate regression analyses between GHPs with low-grade and high-grade intraepithelial neoplasia, as shown in Table 3.
Table 3.
Analysis of gastric hyperplastic polyps with low-grade and high-grade intraepithelial neoplasia
|
|
GHPs with low-grade IN (n = 119)
|
GHPs with high-grade IN (n = 17)
|
χ
2 test
|
Univariate analysis
|
||
|
χ
2 value
|
P value
|
P value
|
OR (95%CI)
|
|||
| Age (mean ± SD), years | 64.49 ± 1.13 | 67.93 ± 2.55 | 0.6621 | 0.404 | 1.461 (0.600-3.555) | |
| ≤ 45 years, n (%) | 8 (7) | 1 (6) | ||||
| 45-65 years, n (%) | 49 (41) | 5 (30) | ||||
| > 65 years, n (%) | 62 (52) | 11 (65) | ||||
| Sex (male), n (%) | 57 (48) | 10 (59) | 0.710 | 0.399 | 0.402 | 1.544 (0.554-4.355) |
| H. pylori infection, n (%) | 20 (17) | 2 (12) | 0.6541 | 0.655 | 0.702 (0.148-3.322) | |
| Multiple polyps, n (%) | 51 (43) | 11 (65) | 2.035 | 0.154 | 0.542 | 2.133 (0.741-6.145) |
| Polyp size (mean ± SD), cm | 1.25 ± 0.07 | 2.2 ± 0.32 | 16.624 | 0.024 | 0.017 | |
| ≤ 1 cm | 63 (52) | 3 (18) | - | 1 | ||
| 1 cm-2 cm | 46 (39) | 7 (41) | 0.034 | 6.956 (1.159-41.729) | ||
| > 2 cm | 10 (8) | 7 (41) | 0.490 | 1.766 (0.352-8.865) | ||
| Endoscopic color, n (%) | 3.382 | 0.184 | 0.232 | 2.455 (0.826-7.294) | ||
| Normal | 50 (42) | 4 (24) | ||||
| Red | 69 (58) | 13 (76) | ||||
| Mucosal erosion, n (%) | 23 (20) | 7 (41) | 4.403 | 0.051 | 0.224 | 2.891 (0.994-8.411) |
| Polyp lobulation, n (%) | 19 (16) | 6 (35) | 3.704 | 0.054 | 0.086 | 2.781 (0.947-8.703) |
| Mucosal roughness, n (%) | 58 (49) | 11 (65) | 1.517 | 0.218 | 0.237 | 1.928 (0.670-5.552) |
| Endoscopic classification, n (%) | 0.0201 | 0.331 | ||||
| I | 35 (29) | 0 (0) | ||||
| II | 40 (34) | 2 (12) | ||||
| III | 19 (16) | 8 (47) | ||||
| IV | 25 (21) | 7 (41) | ||||
| Shape, n (%) | 8.600 | 0.003 | ||||
| Non-pedunculated | 75 (63) | 2 (12) | - | 1 | ||
| Pedunculated or semi-pedunculated | 44 (37) | 15 (82) | 0.010 | 7.375 (1.615-33.671) | ||
| Location, n (%) | 4.451 | 0.103 | 0.302 | 0.632 (0.316-1.263) | ||
| Upper third | 27 (23) | 4 (24) | ||||
| Middle third | 49 (41) | 11 (65) | ||||
| Lower third | 43 (36) | 2 (12) | ||||
| Background gastric mucosa, n (%) | 0.5531 | 0.644 | 1.788 (0.362-8.388) | |||
| Autoimmune gastritis | 24 (20) | 5 (29) | ||||
| Chronic superficial gastritis | 39 (33) | 3 (18) | ||||
| Chronic atrophic gastritis | 26 (22) | 5 (29) | ||||
| Gastritis with IN | 30 (25) | 4 (24) | ||||
P value means using Fisher’s exact test.
OR: Odds ratio; CI: Confidence interval; GHPs: Gastric hyperplastic polyps; IN: Intraepithelial neoplasia; H. pylori: Helicobacter pylori.
Treatment
Regarding treatment, the total and curative resection rates of 17 patients with high-grade intraepithelial neoplasia were 100% each. These rates are considered to be due to the fact that the cancer focus was mostly located in the polyp, the boundary was clear, and the operation was easy. The postoperative complication rate of ESD and EMR was 0, suggesting that endoscopic treatment was effective.
DISCUSSION
Gastric polyps are a simple type of stomach polyp that usually cause mucosal damage, most commonly in cases of chronic and autoimmune gastritis caused by H. pylori infection. They are generally considered benign; however, in a few cases, they may progress to dysplasia (0.2%-10%) and adenocarcinoma (0.6%-3%)[2]. The neoplastic transformation of gastric polyps is diagnosed based on the current Nakamura criteria as follows: (1) Benign and neoplastic lesions coexist in the same polyp; (2) Sufficient evidence indicates that the benign part has the characteristics of benign polyps, and (3) The neoplastic part has obvious cellular and structural atypia[3]. In this study, the tissue carcinogenesis rate of GHPs was 0.3%, and the probability of concurrent dysplasia and intestinal metaplasia occurrence was 3.1% and 5%, respectively, which is broadly consistent with previous findings[4].
Regarding clinical features, the incidence of GHPs increased with age. The mean age of the patients in this study was 58 years, of which 45-65 years were the age groups with the highest incidence (51%). Furthermore, the incidence of GHPs was higher in females (63%). We observed significant differences in the age and sex of patients among the groups. The probability of neoplastic transformation of polyps increased with older age, whereas the proportion of neoplastic transformation was significantly higher in males with polyps.
Regarding the endoscopic features, an increasing number of reports have recently emerged on GHPs combined with neoplastic changes. A polyp size of > 1 cm is considered a risk factor for neoplastic transformation[3]. The erosive morphology differs significantly between hyperplastic polyps with neoplastic transformation and simple hyperplastic polyps (P < 0.005)[5]. In our study, large polyps, the presence of multiple polyps, rough surface, lobulation, mucosal erosion, and Yamada type III and IV classifications were considered risk factors for neoplastic transformation, suggesting that polyp morphology should be considered. In several international studies, multivariate analysis revealed a diameter of > 25 mm (OR = 84; 95%CI: 7.4-954), peripheral mucosal findings, accompanied by intestinal metaplasia (OR = 7.6; 95%CI: 1.0-55) and dysplasia (OR = 86; 95%CI: 10-741) to be significantly correlated with the neoplastic transformation of polyps[6].
Furthermore, the relationship between H. pylori infection and GHPs remains unclear. A large database study in the United States showed that the rate of H. pylori infection in the hyperplastic polyp group was lower than that in the control group[7]. However, considering the factors influencing the background gastric mucosa and the possibility of previous eradication of H. pylori infection is essential in the treatment of hyperplastic polyps[8]. The British gastroenterological of society strongly recommends the eradication of H. pylori in patients with hyperplastic polyps and endoscopic follow-up after 3-6 months of treatment[9]. H. pylori is considered a carcinogen of gastric cancer; however, in our study on the neoplastic transformation of GHPs, H. pylori infection was not found to be a significant risk factor (P > 0.05) after comparison between the groups. Even when compared with the group without intraepithelial neoplasia, it showed a gradually decreasing trend. Therefore, the carcinogenic mechanism may differ from that of H. pylori causing gastric cancer, which is an interesting finding.
GHPs are usually associated with inflammatory lesions of the local gastric mucosal tissue, particularly long-standing H. pylori infection-associated gastritis and autoimmune metaplastic atrophic gastritis[4], which are used as markers of an abnormal background gastric mucosa rather than an isolated pre-neoplastic lesion. According to Orlowska et al[10], the risk of developing neoplastic tumours in the gastric mucosa outside the polyps is slightly higher than that in the polyps. Markowski et al[4] reported a 7.1% chance of neoplastic transformation of the mucosa around the gastric polyp, whereas the polyp was neoplastic with a conversion rate of 2.1%.
In our study, multivariate analysis showed that specific background gastric mucosa was an independent risk factor for harbouring a neoplasm in GHPs. Compared with chronic superficial gastritis, autoimmune gastritis, atrophic gastritis, and gastritis with intraepithelial neoplasia were significantly different [(OR = 2.672; 95%CI: 1.559-4.579; P < 0.001), (OR = 1.876; 95%CI: 1.134-3.103; P = 0.014), and (OR = 5.299; 95%CI: 3.173-8.849; P < 0.001), respectively] (Table 2). In the high-grade intraepithelial neoplasia group, chronic atrophic gastritis with intraepithelial neoplasia accounted for 24% of cases (4/17), of which two were cases of gastric cancer. Autoimmune gastritis in the background gastric mucosa accounted for 29% of cases (5/17) in the high-grade intraepithelial neoplasia group, which is consistent with previous studies showing that patients with autoimmune gastritis are prone to polyp. Although the mechanism remains unclear, some studies suggest that it is related to mucosal atrophy or hypergastrinemia blood syndrome[11]. In Japan, a case of hyperplastic polyp carcinogenesis with submucosal and lymphatic invasion occurring on the basis of gastritis has been reported[12]. Therefore, the association between the background gastric mucosa and hyperplastic polyps should be emphasised in the clinical diagnosis of gastric polyps, and an adequate biopsy of the surrounding mucosa is recommended to evaluate any underlying gastric disease[13].
Studies have shown that cancers associated with GHPs are highly differentiated. Among the 17 patients in our study, except for 5 cases of high-grade intraepithelial neoplasia, the rest were differentiated cancers. Four cases were tubular adenocarcinoma, and one was papillary adenocarcinoma, all of which were differentiated adenocarcinomas. However, the remaining seven cases could not be conclusively diagnosed with a specific pathological type, and no poorly differentiated or undifferentiated cancers were found. These findings align with the results of previous literature and are also comparable to those reported in other studies. Of these cases, immune combination analysis revealed that two cases were caudal type homeobox (CDX)-2 (-) and one was CDX-2 (+). Currently, the exact mechanism underlying the carcinogenesis of hyperplastic polyps remains unclear. Previous studies have suggested that the most simple tissue type of hyperplastic polyps is differentiated adenocarcinoma[14]. A small number of poorly differentiated adenocarcinomas have been reported. Imura et al[15] studied six cases of cancerous polyps. Mucin (MUC) 5AC was detected in the normal, dysplastic, and cancerous parts of the polyp, and MUC2 was negative, supporting the diagnosis of adenocarcinoma as the gastric phenotype[15]. Terada[16] found that all cancerous lesions in GHPs were p53 positive with high expression of the Ki-67 marker and that 82% of 51 patients with GHP dysplasia were also p53 positive with dysplastic lesions, exhibiting a higher Ki-67 Labelling index. However, the intestinal metaplasia within GHPs that were p53-negative showed low Ki-67 staining. Their study suggests that intestinal metaplasia is unrelated to the neoplastic transformation of GHPs, contradicting the theory of the GHP enteric-dysplasia-carcinogenic sequence and strongly suggesting the presence of hyperplasia-dysplasia-adenocarcinoma sequences.
This study has some limitations. First, the overall number of carcinogenesis cases in this study was small. Therefore, further expanding the sample size is necessary for more in-depth research to explore the risk factors for neoplastic transformation. Other limitations of the study include its single-center and retrospective design. Additionally, basic experiments such as specific immunohistochemical experiments or analyses of gene expression are needed to further explore the specific mechanisms underlying the carcinogenesis of hyperplastic polyps. However, the overall sample size of this study was large, and we believe that the results will contribute to the clinical treatment of GHPs.
CONCLUSION
GHPs pose a risk of neoplastic transformation; however, the mechanism remains unclear and needs to be further explored. Polyps with large endoscopic diameter (> 1 cm), multiple polyps, pedunculated or semi-pedunculated shape, diameter of > 1 cm, specific background gastric mucosa, age > 65 years, and male sex were independent risk factors. Clinicians should be alert to the possibility of neoplastic transformation to improve the diagnosis rate of the neoplastic transformation of GHPs. The association between the background gastric mucosa and the neoplastic transformation of GHPs should be emphasised in the clinical diagnosis. During endoscopy, the background mucosa should also be carefully observed if necessary. Furthermore, H. pylori infection was not found to be a significant risk factor (P > 0.05) after comparison between the groups. Even when compared with the group without intraepithelial neoplasia, it showed a gradually decreasing trend, which is an interesting finding.
Footnotes
Institutional review board statement: This study was approved by the Peking University Third Hospital Medical Science Research Ethics Committee (No. M2023153).
Informed consent statement: Since this is a retrospective study, informed consent was not required from the patients.
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade C, Grade C
Novelty: Grade C, Grade C
Creativity or Innovation: Grade B, Grade C
Scientific Significance: Grade C, Grade C
P-Reviewer: Juneja D S-Editor: Fan M L-Editor: A P-Editor: Zhao YQ
Contributor Information
Dong-Xue Zhang, Department of Gastroenterology, Peking University Third Hospital, Beijing 100191, China.
Zhan-Yue Niu, Department of Gastroenterology, Peking University Third Hospital, Beijing 100191, China.
Ye Wang, Department of Gastroenterology, Peking University Third Hospital, Beijing 100191, China.
Ming Zu, Department of Gastroenterology, Peking University Third Hospital, Beijing 100191, China.
Ya-Han Wu, Department of Gastroenterology, Peking University Third Hospital, Beijing 100191, China.
Yan-Yan Shi, Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing 100191, China.
He-Jun Zhang, Department of Gastroenterology, Peking University Third Hospital, Beijing 100191, China.
Jing Zhang, Department of Gastroenterology, Peking University Third Hospital, Beijing 100191, China.
Shi-Gang Ding, Department of Gastroenterology, Peking University Third Hospital, Beijing 100191, China. dingshigang222@163.com.
Data sharing statement
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
References
- 1.Kővári B, Kim BH, Lauwers GY. The pathology of gastric and duodenal polyps: current concepts. Histopathology. 2021;78:106–124. doi: 10.1111/his.14275. [DOI] [PubMed] [Google Scholar]
- 2.Salomao M, Luna AM, Sepulveda JL, Sepulveda AR. Mutational analysis by next generation sequencing of gastric type dysplasia occurring in hyperplastic polyps of the stomach: Mutations in gastric hyperplastic polyps. Exp Mol Pathol. 2015;99:468–473. doi: 10.1016/j.yexmp.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Han AR, Sung CO, Kim KM, Park CK, Min BH, Lee JH, Kim JY, Chang DK, Kim YH, Rhee PL, Rhee JC, Kim JJ. The clinicopathological features of gastric hyperplastic polyps with neoplastic transformations: a suggestion of indication for endoscopic polypectomy. Gut Liver. 2009;3:271–275. doi: 10.5009/gnl.2009.3.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Markowski AR, Markowska A, Guzinska-Ustymowicz K. Pathophysiological and clinical aspects of gastric hyperplastic polyps. World J Gastroenterol. 2016;22:8883–8891. doi: 10.3748/wjg.v22.i40.8883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu H, Zhang Q, Chen G, Pritchard DM, Zhang S. Risk factors and clinical correlates of neoplastic transformation in gastric hyperplastic polyps in Chinese patients. Sci Rep. 2020;10:2582. doi: 10.1038/s41598-020-58900-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.João M, Areia M, Alves S, Elvas L, Taveira F, Brito D, Saraiva S, Teresa Cadime A. Gastric Hyperplastic Polyps: A Benign Entity? Analysis of Recurrence and Neoplastic Transformation in a Cohort Study. GE Port J Gastroenterol. 2021;28:328–335. doi: 10.1159/000514714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sonnenberg A, Genta RM. Prevalence of benign gastric polyps in a large pathology database. Dig Liver Dis. 2015;47:164–169. doi: 10.1016/j.dld.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Nam SY, Park BJ, Ryu KH, Nam JH. Effect of Helicobacter pylori eradication on the regression of gastric polyps in National Cancer Screening Program. Korean J Intern Med. 2018;33:506–511. doi: 10.3904/kjim.2016.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goddard AF, Badreldin R, Pritchard DM, Walker MM, Warren B British Society of Gastroenterology. The management of gastric polyps. Gut. 2010;59:1270–1276. doi: 10.1136/gut.2009.182089. [DOI] [PubMed] [Google Scholar]
- 10.Orlowska J, Jarosz D, Pachlewski J, Butruk E. Malignant transformation of benign epithelial gastric polyps. Am J Gastroenterol. 1995;90:2152–2159. [PubMed] [Google Scholar]
- 11.Hu HY, Ji M, Chen GY, Zhang ST. [The association of gastric hyperplastic polyps and autoimmune metaplastic atrophic gastritis] Zhonghua Xiaohuaneijing Zazhi. 2020;37:573–577. [Google Scholar]
- 12.Yamanaka K, Miyatani H, Yoshida Y, Ishii T, Asabe S, Takada O, Nokubi M, Mashima H. Malignant transformation of a gastric hyperplastic polyp in a context of Helicobacter pylori-negative autoimmune gastritis: a case report. BMC Gastroenterol. 2016;16:130. doi: 10.1186/s12876-016-0537-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pimentel-Nunes P, Libânio D, Marcos-Pinto R, Areia M, Leja M, Esposito G, Garrido M, Kikuste I, Megraud F, Matysiak-Budnik T, Annibale B, Dumonceau JM, Barros R, Fléjou JF, Carneiro F, van Hooft JE, Kuipers EJ, Dinis-Ribeiro M. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019;51:365–388. doi: 10.1055/a-0859-1883. [DOI] [PubMed] [Google Scholar]
- 14.Forté E, Petit B, Walter T, Lépilliez V, Vanbiervliet G, Rostain F, Barsic N, Albeniz E, Gete GG, Gabriel JCM, Cuadrado-Tiemblo C, Ratone JP, Jacques J, Wallenhorst T, Subtil F, Albouys J, Giovannini M, Chaussade S, Landel V, Ponchon T, Saurin JC, Barret M, Pioche M. Risk of neoplastic change in large gastric hyperplastic polyps and recurrence after endoscopic resection. Endoscopy. 2020;52:444–453. doi: 10.1055/a-1117-3166. [DOI] [PubMed] [Google Scholar]
- 15.Imura J, Hayashi S, Ichikawa K, Miwa S, Nakajima T, Nomoto K, Tsuneyama K, Nogami T, Saitoh H, Fujimori T. Malignant transformation of hyperplastic gastric polyps: An immunohistochemical and pathological study of the changes of neoplastic phenotype. Oncol Lett. 2014;7:1459–1463. doi: 10.3892/ol.2014.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Terada T. Malignant transformation of foveolar hyperplastic polyp of the stomach: a histopathological study. Med Oncol. 2011;28:941–944. doi: 10.1007/s12032-010-9556-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.