Abstract
Periodontitis is the inflammation of the supporting structures around the dentition. Several microbial agents, mostly bacteria, have been identified as causative factors for periodontal disease. On the other hand, oral cavity is a rich reservoir for viruses since it contains a wide variety of cell types that can be targeted by viruses. Traditionally, the focus of research about the oral flora has been on bacteria because the most widespread oral diseases, like periodontitis and dental caries, are outcomes of bacterial infection. However, recently and especially after the emergence of coronavirus disease 2019, there is a growing tendency toward including viruses also into the scope of oral microbiome investigations. The global high prevalence of periodontitis and viral infections may point out to a concomitant or synergistic effect between the two. Although the exact nature of the mechanism still is not clearly understood, this could be speculated through the manipulation of the immune system by viruses; hence facilitating the furthermore colonization of the oral tissues by bacteria. This review provides an extensive and detailed update on the role of the most common viruses including herpes family (herpes simplex, varicella-zoster, Epstein-Barr, cytomegalovirus), Human papillomaviruses, Human immunodeficiency virus and severe acute respiratory syndrome coronavirus 2 in the initiation, progression and prognosis of periodontitis.
Keywords: Virus, Periodontitis, Bacteria, Herpesvirus, Herpes simplex virus, Varicella-zoster virus, Epstein-Barr virus, Cytomegalovirus, Human papillomaviruses, SARS-CoV-2, Human immunodeficiency virus
Core Tip: Periodontitis affects millions of people worldwide. It has been connected to several systemic inflammations and infections. Periodontitis is a complex and multifactorial disease. The main microorganisms involved in periodontitis are bacteria. However, viruses may have a contribution in the etio-pathogenesis of periodontitis also. In this article we extensively reviewed the role of some of the most common viruses in the initiation and progression of periodontitis.
INTRODUCTION
Periodontitis which is an immune-inflammatory disease is characterized by the host's response to the presence of subgingival polymicrobial biofilms, eventually leading to clinical attachment loss of periodontium and alveolar bone degeneration. Gingivitis, or gum inflammation, usually does not cause any serious problems at first. If it spreads further the soft tissue and bone that firmly anchors the teeth, called the periodontium, could be harmed also. Inflammation of this periodontium is known as periodontitis in medicine[1]. Twenty percent of adults globally are thought to suffer from severe periodontal diseases, with over 1 billion incidences believed to exist[2].
Periodontitis has multiple contributing factors. One of the key components is a person's genetic susceptibility to the disease. Numerous bacteria have been identified in the field of microbiology. Porphyromonas gingivalis (P. gingivalis), Aggregatibacter actinomycetemcomitans (A. actinomycetemcomitans), and Treponema denticola (T. denticola) are among the most crucial bacteria that have been linked to the disease's onset and progression[3]. Subgingival calculus was revealed to be a local component connected with the beginning of the condition, and dental plaque was linked to its advancement. Therefore, the etio-pathogenesis of periodontitis involves a variety of bacteria, both beneficial and detrimental host immune responses, environmental variables that are modifiable and those that are not, as well as genetic and epigenetic factors[4,5].
Oral cavity, on the other hand, is a significant source of viruses since it has a diverse range of cell types that viruses can target. Because bacterial infections are the cause of the most common oral diseases, such as dental caries and periodontitis, research on the oral flora has traditionally focused on bacteria[6]. However, conditions have changed with the development of molecular biology technologies.
Detecting viruses in periodontitis is crucial for understanding their role in the disease. Two advanced molecular techniques, polymerase chain reaction (PCR) and next-generation sequencing (NGS), have significantly improved the sensitivity and specificity of viral detection in periodontal tissues. PCR is a widely used method for detecting viral DNA or RNA in subgingival plaque samples. PCR and its quantitative variant, qPCR, are highly sensitive and specific techniques that can amplify and quantify viral genetic material. For example, Chalabi et al[6] used PCR to detect periodontopathic bacteria and herpesviruses in chronic periodontitis, demonstrating the presence of these pathogens in periodontal pockets[6]. Similarly, Thomasini and Pereira utilized PCR-based assays to identify herpesviral infections in the oral cavity, highlighting the relevance of viral detection in periodontal disease[7]. NGS is another powerful technique that allows comprehensive analysis of the viral genome in periodontal samples. NGS can identify and quantify a broad range of viral species, providing a detailed profile of the viral community present in periodontal tissues. This method offers several advantages over traditional techniques, including high throughput, deep sequencing depth, and the ability to detect low-abundance viruses. Carrozzo and Scally employed NGS to study the oral microbiome and its association with hepatitis C virus (HCV) infection, providing insights into the complex interactions between viruses and periodontal disease[8]. Both PCR and NGS have significantly advanced our ability to detect and analyze viruses in periodontitis. PCR is particularly useful for targeted detection and quantification of specific viral pathogens, while NGS provides a comprehensive overview of the viral community and its diversity. The integration of these techniques in periodontal research has led to a better understanding of the viral contributions to periodontal inflammation and disease progression.
There has been an increasing trend recently, particularly with the rise of coronavirus disease 2019 (COVID-19), to include viruses in the scope of studies on the oral microbiota. While some viruses are systemic and involve secondarily the oral cavity, others have a relative predilection for the oral tissues. Only a small percentage of the viruses that live in the oral cavity are pathogenic and have the potential to cause symptoms. The majority of viruses are commensals. The significant frequency of viral infections and oral diseases worldwide may indicate a concurrent or synergistic influence between the two[8]. Even though the precise mechanism is yet unknown, it may be related to viruses' ability to influence the immune system, which in turn allows bacteria to colonize oral and dental tissue. This has led to viral-bacterial plaque hypothesis. Moreover, a similar correlation between several viral infections and oral cancer can be proposed[9]. This review provides an extensive and detailed update on the role of the most common viruses including herpes family (herpes simplex, varicella-zoster, Epstein-Barr, cytomegalovirus), human papillomaviruses (HPV), human immunodeficiency virus (HIV) and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the initiation, progression and prognosis of periodontitis.
HUMAN HERPESVIRUS
Human herpesvirus (HHV) refers to a broad family of DNA viruses that includes the varicella-zoster virus (VZV), cytomegalovirus (CMV), Epstein-Barr virus (EBV), and, more recently, the herpes simplex virus (HSV), which comes in two kinds, HSV-1 and HSV-2. The only known natural reservoir for these endemic viruses is humans[10]. These viruses are prone to latency, repeated infections, and dissemination. All eight varieties result in a primary infection and remain dormant within particular cell types for the duration of the host's life. These viruses can reactivate and induce asymptomatic or symptomatic reactivation. Saliva and vaginal fluids carry the viruses, which can spread to new hosts[7].
In 2016, 491 million persons worldwide or 13% of the population between the ages of 15 and 49- were projected to have HSV-2 infection. In the same year, an estimated 3.7 billion persons worldwide, or 66% of those between the ages of 0 and 49, contracted HSV-1[11]. Table 1 provides some key information on the main target cells of the HHV types, their oral and systemic pathologies.
Table 1.
Key information on the human herpes virus types, the main target cells, their oral and systemic pathologies
|
Human herpes virus
|
Main target cells
|
Oral pathology
|
Systemic pathology
|
| HHV-1 and 2 (HSV 1 and 2) | Mucoepithelial cells (orofacial and genital tract) | Primary herpetic gingivostomatitis. Recurrent herpetic gingivostomatitis. Chronic herpetic gingivostomatitis. Herpes labialis. Increased risk of periodontitis | Genital ulcers |
| HHV-3 (VZV) | Mucoepithelial cells and T cells (orofacial and any skin or mucosa of the body) | Possible oral vesicles and ulcers, increased risk of periodontitis | Primary infection: Varicella (chicken pocks). Recurrent infection: Herpes zoster (shingles) |
| HHV-4 (EBV) | Mucoepithelial cells and B cells | Hairy leukoplakia, leukoplakia, nasopharyngeal carcinoma, ulcerations and palatal petechiae, oral lymphoma, increased risk of periodontitis | Infectious mononucleosis, lymphoma |
| HHV-5 (CMV) | Monocytes, fibroblasts, lymphocytes and epithelial cells | Oral vesicles and ulcers, increased risk of periodontitis | Infectious mononucleosis |
| HHV-6 | T cells, epithelial cells, monocytes, fibroblasts and more | Unknown | |
| HHV-7 | T cells, epithelial cells, monocytes, fibroblasts and more | Unknown | |
| HHV-8 | Not identified | Ulcers and tumors | Kaposi’s sarcoma |
EBV: Epstein-Barr virus; CMV: Cytomegalovirus; HHV: human herpes virus, HSV: Herpes simplex virus; VZV: Varicella-zoster virus.
Numerous causes served as inspiration for periodontal HHV research. The 1960s periodontal model was centered on dental biofilm and plaque. However, the low frequency of periodontitis in some patients with large biofilm buildup and the quick progression of juvenile (aggressive) periodontitis lesions with modest biofilms, cannot be explained by the presence of biofilm production alone[7]. Results of periodontal biofilm eradication techniques have been inconsistent. In the late 1970s, due to these clinical circumstances, the etiology of severe periodontitis shifted from a broad microbiologic disease to a specific infection involving different anaerobic bacteria. However, bacterial infections alone cannot explain periodontitis' site-specificity, especially its bilateral symmetrical distribution around the mouth's midline. The site-specificity of periodontitis pointed to herpesviruses, which are the prototype agents for tissue tropism infectious (e.g., herpes labialis)[12]. The pattern of HHV infection may account for a number of characteristic features of periodontal diseases, including: (1) The localized pattern of tissue destruction, which may be caused by viral tissue tropism; (2) The disease's episodic, progressive nature, which may be caused by temporary local immunosuppression resulting from either an active or latent viral infection; and (3) The fact that some people have periodontopathogenic bacteria but still have healthy gums maybe due to lack of viral infection[13].
Many studies have found a significant incidence of HHVs in periodontal disease beginning in the mid-1990s. The presence of HHVs in gingival tissue, gingival cervicular fluid (GCF), and subgingival plaque in periodontal disease suggests that HHVs might be involved in the periodontal disease etiology. First of all, it has been demonstrated that human gingiva from clinically healthy individuals can get infected with HSV, indicating that these cells may serve as a reservoir for the latent virus[14]. Eventually, it was shown that the gingival tissue of periodontitis sites had a higher frequency of viral detection than did healthy locations[15]. Furthermore, also in the in GCF, it was observed that the frequency of HHV detection from periodontally diseased sites was higher than that from gingivitis/healthy sites[16]. Again, it was shown that subgingival plaque from periodontally diseased locations had a higher frequency of viral detection than plaque from healthy sites[17]. Moreover, it was found that the GCF of periodontal lesions contained active HHVs[18]. Additionally, the relationship between HHVs and periodontal bacterial infections was examined in a number of investigations[19]. Lastly, extensive populations were the subject of epidemiological investigations. For instance, a recent study that examined periodontitis and HSV co-infection used extensive cross-sectional data from the National Health and Nutrition Examination Survey (NHANES), which included 4733 adults aged 30-50. Both HSV-1 [odds ratio (OR) = 1.09, P < 0.001] and HSV-2 (OR = 1.06, P = 0.030) infections were substantially linked to periodontitis after controlling for variables. Those with HSV-1 (+) and HSV-2 (+) and HSV-1 (+) and HSV-2 (-) infection demonstrated greater incidence of periodontitis in all subgroups (OR = 1.15, OR = 1.09, P < 0.001) in subgroup analyses compared to those without HSV infection[20].
These preliminary studies accumulated through time to form a considerable amount of literature body on the same association studied globally. Starting from the last decade, this series of investigations led to several systematic reviews and meta-analyses on the available data. Table 2 collects a list of selected systematic reviews and meta-analyses on the association between HHV and periodontitis. Findings from these reviews show a pattern and a potential consistency. For the EBV, which is the most studied HHV, a strong correlation with chronic, aggressive and advanced periodontitis was seen. This may reflect the high prevalence of EBV in most of the oral cavity tissues, its virulence and aggressive pathogenicity. However, when it comes to the apical periodontitis and peri-implantitis, negative association was reported[21-23]. The same pattern is true for human CMV (HCMV) since most of the data shows a strong association between its detected prevalence and chronic, advanced and aggressive periodontitis but not with apical periodontitis[24]. Regarding the HSV, statistically significant relation with chronic, advanced and aggressive periodontitis were reported[25]; although in one meta-analysis including twelve studies no significant association was seen[26]. Finally, the same result was repeated in a recent umbrella review including six meta-analyses. The association between HHVs and marginal periodontitis was significant in contrast to the apical periodontitis of endodontic origin[27].
Table 2.
A list of systematic reviews and meta-analyses on the association between human herpesviruses and periodontitis
|
Ref.
|
Study design
|
Findings
|
Conclusion
|
Reported statistical significance
|
| Jakovljevic et al[27], 2022 | Umbrella review including six meta-analyses on HHVs detection in MP and apical periodontitis of endodontic origin (APEO) | MP risk increased with subgingival HHVs. The connection was robust (OR > 3.0), although confidence intervals were broad, heterogeneity was high, and studies were small. However, systematic reviews of APEO and HHVs found no significant relationships | There was a substantial correlation between HHVs and MP, but not APEO, according to low-quality, highly unclear research | MP: Yes; APEO: No |
| Arduino et al[26], 2023 | Meta-analysis of eight observational studies on HSV-1 in endodontic peri-apical lesions including 194 adult patients | Pooled HSV-1 prevalence was 4.8% (95%CI: 2.0%–11.4%; adjusted for small-study effect); 8.1% (95%CI: 4.4%–14.5%, quality-adjusted); and 6.8% (95%CI: 3.6%–11.0%, random-effects) | 3%–11% of periapical disease patients had HSV-1 colonization. Such data do not suggest HSV-1 causes the onset and progression of periodontitis | No |
| Arduino et al[25], 2022 | Meta-analysis of twelve case–control and cross- sectional studies (738 cases, 551 controls), investigating HSV-1 in subgingival plaque/crevicular fluid and periodontitis | For any type of periodontitis, the pooled ORs were 44 (95%CI: 1.9–10.2); for chronic periodontitis, they were 28 (95%CI: 1.0–8.3); and for aggressive periodontitis, they were 118 (95%CI: 5.4–25.8) | HSV-1 was associated with periodontitis | Yes |
| Maulani et al[21], 2021 | Meta-analysis of studies on EBV, involving 1354 periodontitis patients and 819 healthy controls | When subgingival EBV was found, there was an increased incidence of periodontitis: OR = 7.069 (95%CI: 4.197–11.905, P < 0.001) | An elevated risk of periodontitis is linked to a high frequency of EBV detection | Yes |
| Roca-Millan et al[22], 2021 | Meta-analysis of five researches on EBV and peri-implantitis. The study included 274 patients (125 men and 149 women) and 388 implants (197 healthy, 166 peri-implantitis, and 25 mucositis) | In the peri-implant sulcus, there was no significant difference in EBV presence between peri-implantitis and healthy implant groups (OR = 4.14; 95%CI: 0.93-18.37; P = 0.06) | EBV prevalence in the sulcus was not statistically different between peri-implantitis and normal implant groups | No |
| Li et al[28], 2017 | Meta-analysis of twelve case-control studies on the presence of HHVs in AgP involving 322 patients and 342 controls | EBV showed substantial connection with AgP, however publication bias was present (10 studies: OR = 6.11, 95%CI: 2.13–17.51, P = 0.0008). HCMV and HSV-1 also showed significant associations (12 studies: OR = 3.63, 95%CI: 2.15–6.13 P = 0.009; 4 studies: OR = 19.19, 95%CI: 4.16–79.06, P < 0.001). Relation between HSV-2 and AgP was inconclusive (2 studies: OR = 3.46, 95%CI: 0.51–23.51, P = 0.20) | AgP showed strong associations with EBV, HCMV, and HSV-1. But there was a lot of heterogeneity among the studies | Yes |
| Zhu et al[29], 2015 | Meta-analysis of 12 studies (including 552 cases and 371 controls) investigated the association between HHVs and chronic periodontitis | EBV: 12 studies (OR = 5.74, 95%CI: 2.53–13.00, P < 0.001). HCMV: 10 studies (OR = 3.59, 95%CI: 1.41–9.16, P = 0.007). HSV: 2 studies (OR = 2.81 95%CI: 0.95–8.27, P = 0.06). HHV-7: 1 study (OR = 1.00, 95%CI: 0.21–4.86) | Chronic periodontitis was highly correlated with both HCMV and EBV. Inadequate evidence was found for HHV-7 and HSV | EBV: Yes; HCMV: Yes; HSV: No; HHV-7: No |
| Botero et al[24], 2020 | Meta-analysis of 32 studies on HCMV in periodontitis (26 studies involving periodontitis and 6 involving apical periodontitis) | Significantly elevated periodontitis risks with subgingival HCMV (OR = 5.31; 95%CI: 3.15-8.97). HCMV was not linked to apical periodontitis (OR 3.65; 95%CI: 0.49-27.10) | HCMV was significantly associated with periodontitis but not with apical periodontitis | Periodontitis: Yes; Apical periodontitis: No |
| Gao et al[23], 2017 | Meta-analysis of 21 case–control studies (including 995 patients and 564 healthy people) on the association between EBV and periodontitis | Significant differences were found in the odds of periodontitis and EBV detection (OR = 6.199, 95%CI: 3.119–12.319, P < 0.001) | An elevated risk of periodontal diseases was connected with a high prevalence of EBV | Yes |
| Alzahrani[19], 2016 | Systematic review of 12 studies on the association between HHVs and risk of AgP and AP | In contrast to healthy individuals, HHVs (HSV, CMV, and EBV) levels were elevated and linked to AgP and AP | Yes | |
| Jakovljevic et al[30], 2014 | Meta-analysis of 17 cross-sectional studies on the association of HCMV and EBV with apical periodontitis | No statistically significant relationship between the presence of HCMV and EBV messenger RNA transcripts (P = 0.083 and P = 0.306, respectively) and the clinical features of apical periodontitis | HCMV and EBV were common in symptomatic and large-size periapical lesions, but not statistically significant | No |
HSV: Herpes simplex virus; AgP: Aggressive periodontitis; MP: Marginal periodontitis; APEO: Apical periodontitis of endodontic origin; EBV: Epstein-Barr virus; HCMV: Human cytomegalovirus; AP: Advance periodontitis; HHV: Human herpesvirus; OR: Odds ratio.
The exact mechanism by which HHVs affect the initiation and progression of periodontitis is still to be uncovered. However a HHV-bacterial model for periodontitis have been proposed briefly as follows: Important components of periodontal pathosis in the herpesviral-bacterial model of periodontitis include immunopathogenicity of the virus, its escaping capability from immune system, latency, reactivation after latency, and tissue/site tropism[28-31]. First, bacteria in the dental biofilm cause gingivitis, which opens the door for latent HHV to reach the periodontium through macrophages, T-lymphocytes, and B-lymphocytes. Latent HHV can reactivate on its own or during times when the host's defenses are weakened, as in the case of concurrent infections, drug-induced immunosuppression, unusually high levels of emotional stress, hormonal fluctuations, physical trauma, etc. Interestingly enough, the majority of conditions that activate herpesviruses are also thought to be risk factors or markers of periodontitis. As previously mentioned, the herpesvirus infection can release pro-inflammatory cytokines that may activate osteoclasts and matrix metalloproteinases, so compromising the immune system's ability to combat periodontopathic bacteria[32].
In conclusion, based on the mentioned data, an association between HHVs (especially EBV, HCMV and HSV) and marginal periodontitis is highly plausible; however all the data shows no such relation with apical periodontitis. This conclusion may support the hypothesis that HHVs have an affinity toward reaching and infecting the gingiva and periodontium but not the pulpal and apical periodontal tissues.
HIV
HIV is a single stranded RNA virus that belongs to the family of Retroviridae. Two main species have been identified: HIV-1 and HIV-2. The former is exhibited globally and responsible for most of the cases, while the latter predominates in West Africa and is related with a relatively decreased risk of transmission and slower progression of the disease. By the end of 2022, there were an anticipated 39 million HIV-positive individuals worldwide, with the World Health Organization (WHO) African Region housing two thirds of them. In 2022, 1.3 million new cases of HIV infection and 630000 deaths from HIV-related causes were reported[33].
It's critical to distinguish between two things when discussing HIV/acquired immunodeficiency syndrome (AIDS): First, the infection pattern both prior to and following contemporary antiretroviral therapy (ART). Due to the introduction and widespread use of ART since 1996, AIDS-which was defined by a fast advancing immunodeficiency course that ultimately results in death- has recently been reduced to a chronic condition that could be managed[33]. Therefore, those living with HIV experience longer life expectancies, lower rates of death and morbidity, and roughly the same rates of development of chronic non-HIV-related illnesses as the general population[34]. These patients also saw improvements in their quality of life. The second point is that industrialized and developing countries have different illness distribution and types. Unfortunately, socioeconomic factors like poverty, prejudice, stigma, and inadequate healthcare systems continue to be major obstacles to treatment and prevention initiatives in underdeveloped nations[35].
A series of oral manifestations of HIV infection have been identified including oral hairy leukoplakia, oral candidiasis, oral warts, salivary gland diseases, Kaposi sarcoma, linear gingival erythema, necrotizing ulcerative gingivitis, necrotizing ulcerative periodontitis and chronic periodontitis[36]. In a recent meta-analysis, the overall prevalence of the manifestations were reported as follows: Oral candidiasis (35%), pseudomembranous candidiasis (19%), oral hairy leukoplakia (12%), Kaposi sarcoma (5%) and erythematous candidiasis (18%)[37]. Atypical lesions affecting the periodontal tissues, such as necrotizing ulcerative gingivitis, necrotizing ulcerative periodontitis, and linear gingival erythema, were seen prior to the development of ART[38]. However, there has been a noticeable decrease in the incidence of oral candidiasis, hairy leukoplakia, and destructive and atypical periodontal disease in HIV patients since the introduction of combined ART[39]. HIV-positive patients on ART had a statistically significant reduction in the prevalence of angular cheilitis, erythematous candidiasis, oral herpes, pseudomembranous candidiasis, Kaposi sarcoma, and oral hairy leukoplakia when compared to those who were not on ART[40].
The most prevalent kind of periodontal disease, chronic periodontitis, has been the subject of epidemiological research. A variety of potential correlations between HIV and the frequency and severity of periodontal illnesses were documented. Prior to the development of ART, certain research found that HIV patients who also had chronic periodontal disease experienced higher levels of attachment loss than non-infected patients, and this was associated with decreasing CD4 counts[41] and a greater extent of gingival recession, with or without greater alveolar bone loss[42]. However, in the combined ART era, studies have reported reductions in the prevalence of periodontal diseases in adults with HIV[40,43]. Moreover, studies carried out during the era of combined ART have not discovered any discernible variations in the frequency or severity of periodontal disease between HIV-positive patients receiving these therapies and non-infected individuals[43]. Furthermore, a large longitudinal study conducted on a cohort of women from 1995 to 2002 found no significant differences between HIV-positive and HIV-negative women in terms of baseline mean probing depths, clinical attachment levels, the advancement of attachment loss, or pocket depths[44]. When comparing HIV patients receiving ART vs those not, it seemed that patients on ART had a significantly lower prevalence of necrotizing gingivitis, and there was no statistically significant difference in the prevalence of either chronic or necrotizing periodontitis between the two groups[45]. Periodontal inflammation was common in HIV patients regardless of ART status, and in participants with virological suppression, the periodontal treatment reduced periodontitis along with a concurrent decrease in IL-6 and an increase in CD4. These findings highlight the impact of periodontal treatment on local inflammation and periodontitis in HIV patients[46]. A recent systematic review showed that HIV infection does not seriously threaten implant survival in the short term, but the data was of high quality[47].
In the combined ART era, as in the pre-combined ART era, there have been conflicting results regarding the relationship between periodontal attachment loss or pocket depth and CD4 counts and/or HIV viral load. Even though HIV can be found and measured in the subgingival biofilm of HIV-positive people[48], some research found no significant differences in periodontal parameters[49,50] or in tooth loss patterns[51], or the stages of HIV infection particularly for patients with a CD4 count higher than 500 cells/mm3[52]. However, patients on combined ARTs who showed resistance to the therapy or a lack of compliance did show a slight increase in tooth loss along with a 10-fold increase in viral load[44]. Meanwhile, a different study found that patients on combined ART who had a CD4 count of less than 200 cells/mm3 were more likely to develop periodontal disease[53]. Lastly, in HIV-positive individuals, the severity of periodontitis was linked to greater frequencies of circulating CD8+ senescent cells, raised CRP levels, and an increased prevalence of P. gingivalis[54].
In children, early research conducted in the pre-ART era indicated high incidence of gingivitis and early periodontitis in many different nations worldwide. Clinical markers such as bleeding on probing, increasing depths of probing, and/or loss of clinical attachment were used in these studies[55-57]. More recently, in the age of ART, extensive cross-sectional and prospective epidemiological studies have been conducted to examine the impact of these medications on the prevalence and severity of periodontal problems in children and adolescents. A large multicenter prospective cohort research included 2767 HIV-positive children from United States and Puerto Rico indicated that children on combined ART had significantly decreased occurrences of oral candidiasis and herpes zoster when compared to children on pre-combined ART[58]. In addition, a recent meta-analysis reported that HIV-positive children taking ART had a significantly higher prevalence of periodontal diseases (three-fold), oral ulcer (6-fold), oral candidiasis (17-fold) and mucosal hyperpigmentation (20-fold) than the healthy controls[59].
The periodontal microbiota of HIV-positive patients has been the subject of numerous studies. According to the findings of certain studies, the subgingival microbiota of people with HIV infection and those without it is similar in composition[60,61]. Other research found that HIV-positive individuals had higher prevalence of periodontal pathogens, including Prevotella intermedia, A. actinomycetemcomitans, P. gingivalis, T. forsythia, Fusobacterium nucleatum and T. denticola, as well as a mixture of these species[62-64].
HIV targets the immune system, namely CD4+ T cells, which causes widespread viremia and leading to a status known as AIDS. Most bodily fluids, including blood, saliva, urine, tears, breast milk, ear secretions, semen, and vaginal secretions can contain the HIV virus in people who are positive for the infection[65]. HIV is typically found in saliva at much lower concentrations in patients than in blood. Saliva has been found to contain RNA and DNA of HIV[66,67]. Serum and HIV-positive macrophages and lymphocytes from gingival crevicular fluid, which the latter is elevated during periodontal disease, are potential sources of infectious HIV DNA in saliva[68]. It's unclear how exactly the HIV enters the periodontium. However, it is well known that the presence of inflammation causes the surface of the oral epithelium to express higher number of receptors, including HIV receptors, which may increase the epithelium's permeability[69].
In conclusion, ART has decreased aggressive forms of atypical periodontitis, while the results on chronic periodontitis are inconclusive. A higher prevalence of traditional periodontal pathogens, which are typically also found in non-infected persons, is present in the subgingival microbiota of HIV-positive patients with chronic periodontitis. Moreover, the extreme immunosuppression appears to encourage the colonization of these species and other species that are uncommon in the subgingival microbiota. This mandates a closer and personalized monitoring and follow-up of HIV patients concerning their periodontal health status.
SARS-COV-2
The coronavirus is a common single-stranded RNA virus that is extremely infectious among humans and animals and can cause respiratory infections ranging from mild to severe. Late in 2019, a novel strain of the β-coronavirus family, known as SARS-CoV-2, surfaced in Wuhan, China. It quickly spread throughout the globe, forcing the WHO to designate the disease a global pandemic on March, 2020[70].
The virus enters the body and generates viremia, which initiates the early stage of the sickness, which typically lasts three to seven days. The illness may then progress into a second stage where the virus enters the bloodstream and targets a variety of tissues and organs[71]. Critical organ damage, including damage to the heart, lungs, nervous system, gastrointestinal tract, and kidneys, causes the patient's condition to worsen. Furthermore, a pathological inflammatory reaction labeled the "cytokine storm" raises the COVID-19 mortality rate. This cytokine storm is indicative of an overreaction of the immune system, as indicated by increased levels of inflammatory mediators in the blood[72]. One of the main ways that SARS-CoV-2 is contagious is because of a spike of protein on its surface that can bind to the angiotensin-converting enzyme 2 (ACE 2), which is found on the membrane of several human body cells[73]. Actually, the fact that ACE 2 is highly expressed in the lower respiratory tract, namely on alveolar pneumocytes, is one of the main mechanisms that SARS-CoV-2 infection can harm the lungs and cause acute respiratory distress syndrome[74].
Severe COVID-19 disease has been linked to a number of risk factors. These include comorbidities like obesity and the existence of underlying disorders, as well as factors like advanced age and sex (male), as well as diabetes, hypertension, cerebrovascular disease, cardiovascular disease and chronic renal disease[73].
It appears that the oral cavity contributes significantly to the pathogenicity of COVID-19. The oral cavity exhibits high expression levels of membrane proteins such as transmembrane protease serine 2 and ACE 2, which are utilized by SARS-CoV-2 to infect cells[75]. Similar to those in the lungs and tonsils, these membrane proteins have been detected at similar concentrations on the epithelial cells of the oral mucosa, tongue, gingiva, salivary glands, and periodontal pockets[76]. Furthermore, oral fluids and saliva may contain SARS-CoV-2; the oral viral load has been linked to the severity of the disease[77].
There have been some nonspecific oral lesions linked to COVID-19 infection. Lip necrosis, dry mouth, fissured or depapillated tongue, oral vesiculobullous or pustulous lesions, and hemorrhagic or erythematous mucosal lesions are a few of these[75]. Patients with systemic diseases that include some degree of immunosuppression are more likely to have these lesions[78]. The oral lesions can affect both keratinized and nonkeratinized mucosa, and they resemble a number of viral diseases[79]. The degree of oral lesions is mostly influenced by an older age and the severity of COVID-19 infection. The beginning of oral lesions typically corresponds with taste and smell chemosensory dysfunctions[80].
Several epidemiological studies have been performed to investigate the association between periodontitis and COVID-19 infection, severity, complications and mortality. A comprehensive investigation involving 1299010 people examined the genotyping of single nucleotide variants linked to periodontitis. Higher susceptibility to COVID-19 infection (OR = 1.029; 95%CI: 1.003–1.055, P = 0.024) and severity of COVID-19 (OR = 1.030; 95%CI: 1.003–1.058, P = 0.027) was significantly linked to periodontitis. The authors came to the conclusion that there may be a causal relationship between periodontitis and COVID-19 severity and susceptibility to infection[81]. Larvin et al[82] investigated self-reported oral health indicators (bleeding gums, loose teeth and painful gums) in 13253 individuals (1616 positive COVID-19 patients and 11637 negative participants) during the course of a 6-month study. Those with loose teeth did not show an increased risk of death or hospital admission (OR = 1.85; 95%CI: 0.92–2.72), in comparison to the control group. On the other hand, persons who tested positive for COVID-19 and experienced bleeding or sore gums were more likely to die (OR = 1.71; 95%CI: 1.05–2.72). Insufficient evidence was available to determine a link between periodontitis and an increased risk of COVID-19 infection. However, among those who tested positive for COVID-19, those with periodontal disease had a significantly higher death rate[82]. The same researchers looked at the self-reported oral health indicators (loose teeth, bleeding and painful gums) in 58897 participants who were followed up for nearly a year, this time with a focus on body weight. Hospital admission rates for patients with periodontal disease were 57% higher [hazard ratio (HR) = 1.57; 95%CI: 1.25-1.97] than for the obese group without the illness. Obesity-related death rates were substantially higher in people with periodontal disease (HR = 3.11; 95%CI: 1.91-5.06) than in people without the illness. The authors speculated that the relationship between obesity and higher hospitalization and death rates could be exacerbated by the effects of periodontal disease[83]. A study conducted in Qatar with 568 participants examined the connection between COVID-19 issues and periodontitis. In the study, dental panoramic radiographs were utilized to assess the condition of the periodontal tissue. After adjusting for potential confounders like age, gender, smoking, body mass index, and other chronic diseases, the study's findings showed a significant correlation between moderate to severe periodontitis and a higher risk of COVID-19 complications, including death (OR = 8.81, 95%CI: 1.00-77.7), admissions to an intensive care unit (OR = 3.54, 95%CI: 1.39-9.05), and the need for assisted ventilation (OR = 4.57, 95%CI: 1.19-17.4)[84]. A similar study with 137 COVID-19 patients found that patients with signs of oral disease (radiographic alveolar bone loss, dental caries, and apical periodontitis) had a significantly higher risk of developing COVID-19 complications compared to those without oral diseases. These complications included positive symptomatology, hospitalizations, and mortality. The study used oral examination records and panoramic X-rays. However, a positive specific correlation with periodontitis could not be observed[85]. Regarding systematic reviews, a study found a reciprocal relationship between COVID-19 and periodontitis; but for peri-implantitis, the authors came to the conclusion that there was still a lack of information[86]. According to a mendelian randomization research there was no correlation between periodontitis and hospitalization for COVID-19 (OR = 0.97, 95%CI: 0.78–1.20; P = 0.76), vulnerability to COVID-19 (OR = 1.04, 95%CI: 0.88–1.21; P = 0.65), or severity of COVID-19 disease (OR = 1.01, 95%CI: 0.92–1.11; P = 0.81)[87]. A meta-analysis, on the other hand, clearly suggested that COVID-19 patients with periodontal disease have a 4-fold increased risk of hospitalization, a 6-fold increased risk of assisted ventilation, and a 7-fold increased risk of death[88]. However, a systematic review stated that there is no evidence to support or contradict a strong relationship between periodontitis and the likelihood of COVID-19 complications and death[89].
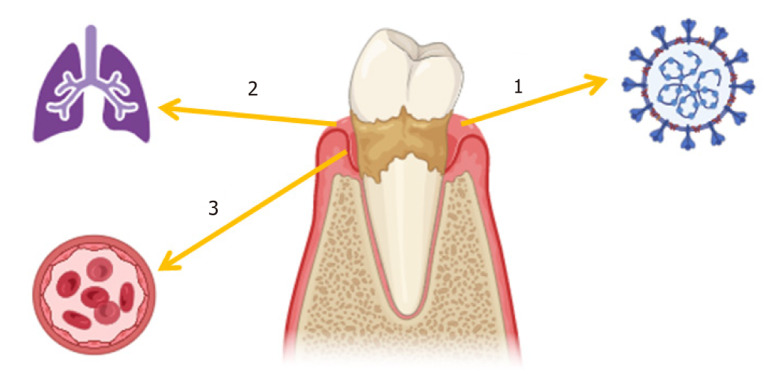
Investigations are ongoing to determine the biological mechanism directing a possible association between COVID-19 and periodontitis. It is commonly known that the linkages between systemic disorders including diabetes, cardiovascular disease, and rheumatoid arthritis and periodontitis are caused by the translocation of periodontal bacteria to blood and consequent systemic inflammation[90,91]. Furthermore, a number of risk factors, such as smoking, old age, obesity, diabetes, hypertension, and cardiovascular disease, are shared by both the severity of COVID-19 disease and periodontitis[1,73,83,92]. A probable correlation between periodontitis and greater severity of COVID-19 infection has been indicated by several investigations due to the increased systemic risk of periodontitis. Certain researchers have questioned if COVID-19 risk factors for periodontal illnesses should be given the same weight as cardiovascular, diabetes, and other conditions[93]. It is unclear, nonetheless, if there are particular processes and pathological pathways connecting periodontitis and greater COVID-19 severity, or if these factors could simply operate as comorbidities. Researchers have suggested a number of mechanisms to explain this association and provide evidence for the connection between COVID-19 infection and periodontitis: (1) SARS-CoV-2 can be detected in periodontal pockets. In COVID-positive cadaver biopsies, SARS-CoV-2 was found in periodontal tissues[94]. This pathogenic environment may allow SARS-CoV-2 to enter through damaged epithelia or by upregulating ACE 2 receptor expression by periodontal bacterial pathogens[95]. These suggest that periodontal pockets may harbor SARS-CoV-2 and allow it to enter the bloodstream; (2) COVID-19 patients can aspirate pathogens from periodontitis. The well-established association between oral microbiome and respiratory illnesses may also relate periodontitis to COVID-19 severity. Poor dental hygiene and periodontitis may collect respiratory microorganisms in the mouth. These pathogens may be eventually aspirated into the lung. For instance, hospital-acquired pneumonia and pneumonia deaths are more common in older adults with periodontal pockets[96]. In a systematic review, respiratory disease and periodontitis were linked to higher prevalence of chronic obstructive pulmonary disease, obstructive sleep apnea, and COVID-19 infection[97]. Respiratory diseases related to periodontitis may worsen COVID-19 and result in a higher mortality[98]. Some periodontopathic bacteria increase ACE 2 and respiratory tract inflammatory cytokines. Bronchoalveolar fluid from COVID-19 patients contained oral opportunistic infections[99]. Lung hypoxia in COVID-19 patients may further encourage the growth of oral microbiota anaerobes; and (3) Periodontitis causes systemic inflammation. High C-reactive protein and proinflammatory cytokines in periodontitis promote systemic inflammation that might aggravate conditions like diabetes and cardiovascular disease[90,91]. Periodontitis synergistically stimulates peripheral leukocytes to local and remote inflammatory stimuli, preparing the immune system for a stronger innate response[100]. COVID-19 infection can trigger a "cytokine storm" an uncontrollable hyperinflammatory reaction. The condition is marked by increased serum levels of interleukin family, C-reactive protein, and tumor necrosis factor-α, and decreased T-lymphocyte numbers[101]. In COVID-19 hospital records, patients with periodontitis had far higher blood levels of inflammatory markers such C-reactive protein than those without periodontitis[84]. Based on this premise, inflammatory upregulation may link periodontitis to COVID-19 severity. Figure 1 shows how periodontitis and COVID-19 may interact (Figure 1). (1) Periodontal pocket act like a reservoir for SARS-CoV-2 and an entrance into the blood stream; (2) Periodontitis as a source for increased direct inoculation of periodontopathic bacteria into the respiratory system in COVID-19 patients; and (3) Periodontitis as a source for increased systemic inflammation and priming the immune system in COVID-19 patients.
Figure 1.
Possible mechanisms of interaction between periodontitis and coronavirus disease 2019 infection. (1) Periodontal pocket act like a reservoir for severe acute respiratory syndrome coronavirus 2 and an entrance into the blood stream; (2) Periodontitis as a source for increased direct inoculation of periodontopathic bacteria into the respiratory system in coronavirus disease 2019 (COVID-19) patients; and (3) Periodontitis as a source for increased systemic inflammation and priming the immune system in COVID-19 patients. (Created at BioRender.com)
Given these connections between periodontitis and COVID-19 severity, periodontal treatment may help prevent and manage COVID-19 problems[102,103]. Impaired immune response, medicines, and reduced diet intake make COVID-19 patients more susceptible to oral dysbiosis. Due to illness and hospitalization, critically ill individuals have poor oral hygiene, which worsens dysbiosis[104]. Periodontitis can be prevented by everyday oral hygiene and professional biofilm removal. Periodontal therapy have decreased the severity of pneumonia and other systemic infections, improves the gingival epithelial barrier, preventing oral harmful viruses and bacteria from entering the bloodstream. Thus, periodontal care may lessen COVID-19's systemic effects and, regular oral hygiene may reduce aspiration pneumonia and COVID-19 complications[98].
To sum up, there are a number of similarities between COVID-19 and periodontitis, such as their effects on systemic inflammation and shared comorbidities. In fact, a few preliminary investigations have suggested a potential link between periodontitis and the likelihood of contracting COVID-19 and its consequences. These correlations may be caused by a priming effect on systemic inflammation, but periodontal bacteria in the lungs may also play a role. In this case, reducing COVID-19 infections and consequences may be aided by preventative dental hygiene practices and periodontal treatment. Nevertheless, more investigation would be required to validate these theories.
HPV
HPV is a double-stranded DNA virus. HPV is one of the three most prevalent sexually transmitted infections (STIs) in both genders and the most prevalent viral STI, which is primarily sexually transmitted. Currently, HPV is the most prevalent infection linked to cancer in women; it has been found in over 90% of cases of cervical cancer, the fourth most deadly type of cancer in women[105,106].
Multiple symptoms, including benign warty or potentially malignant lesions, intraepithelial neoplasia, and invasive carcinomas, can result from HPV infections[107]. There are currently over 200 known HPV genotypes, about 40 of which are mucosal HPV types, meaning they affect the mucosa. The alpha genus of HPV is primarily clinically significant because it harbors the majority of mucosal HPVs, both high-risk and low-risk varieties[108]. High-risk mucosal HPVs, such HPV-16 and HPV-18, produce squamous intraepithelial lesions that can proceed to squamous cell carcinoma in the head and neck area and/or anogenital tract, while low-risk mucosal HPVs, like HPV-6 and HPV-11, cause benign papilloma/condyloma[109]. The global pooled prevalence for genital HPV in men, derived from 35 countries, was 21% for high-risk-HPV and 31% for any HPV[110]. The estimated global prevalence of genital HPV in women was 11.7%[111]. The global incidence of oral HPV in healthy individuals is believed to be between 4 to 7.5%[112,113].
HPV has been detected in the oral cavity especially in the gingival crevicular fluid, gingival tissue, oral swab and oral rinse samples[114-116]. It's possible that HPV enters the human body through the oral cavity first. The main oral manifestations of HPV include oral papillomas/condylomas, focal epithelial hyperplasia and squamous cell carcinoma of the oropharyngeal region[117].
The oral mucosa can harbor HPV infection asymptomatically. The mouth's border, oropharynx, tonsil cryptal epithelium, salivary gland ductal epithelium, and inflammatory gingival pocket are among the potential reservoirs. Another possible reservoir is a latent HPV infection in epithelial basal cells, where a local irritation might trigger a transition from stable to vegetative viral DNA replication[117].
The majority of research on oral HPV has been on its association with oropharyngeal cancer. Nonetheless, a number of research also investigated the connection between periodontitis and HPV found in the gingival/periodontal tissue. For instance, data from the United States NHANES from 2009 to 2012 allowed for the analysis of almost 6000 people (30–69 years old) with clinically determined HPV and periodontal status. After controlling for confounding variables, the adjusted OR for the presence of HPV in oral rinse specimens of participants with periodontal disease was 1.04 (95%CI: 0.63–1.73)[115]. In another study, 223 patients with known periodontal disease status, oral hygiene practices, and HPV-positive oral rinse samples were included. Ten (4.5%) of these individuals tested positive for HPV-16 DNA. Among the participants who tested positive for HPV-16 DNA, periodontal disease was linked to three (30%) and poor oral hygiene to seven (70%) of them[118]. Moreover, in a multivariable analysis, adults with severe periodontitis had higher odds of oral HPV infection than adults with none or mild periodontal disease (OR = 2.9, 95%CI: 1.0-8.4, P < 0.05). Adults with pocket depth > 6 mm and clinical attachment loss ≥ 7 mm exhibited 2- to 3-fold increased risks of HPV infection[119]. Furthermore, PCR analysis of gingival biopsies obtained from patients with periodontal disease who had a clinical diagnosis of periodontitis revealed the presence of high-risk HPV strains in 26% (8/31) of the samples[116]. Again, when eight participants with widespread chronic periodontitis had their periodontal pockets scraped, HPV E6/E7 mRNA was found in four of the eight samples[120]. In a study with 822 patients, McDaniel et al[121] found that those without a vaccination against HPV and periodontitis had a higher incidence of oral HPV[121].
Furthermore, a higher number of oral bacteria was linked to higher HPV16 E6 viral copy numbers in hospital patients, indicating a possible link between oral HPV infection and viral replication and inadequate oral hygiene[122]. As a result, there was evidence for a tendency toward a positive connection between oral HPV-16 infection and clinical oral health. Furthermore, there was a strong correlation found between the prevalence of Fusobacterium nucleatum and T. denticola and the HPV16 DNA positive in gingival crevicular fluid[123]. Therefore, it is thought that the prevalence of oral HPV and periodontal microorganisms are connected. It is hypothesized that whereas periodontal disease provide an environment in which oral HPV infections can thrive, oral HPV infections may also make periodontal diseases worse.
However, some negative findings also reported in the literature about the correlation between periodontitis and identified HPV in periodontium. For instance, HPV-16 was not found in any of the 104 gingival samples examined in a case-control study that included gingivitis, periodontitis, and healthy periodontium[114]. PCR was used to screen 74 oral biopsies from kidney transplant recipients and non-recipients with gingivitis and/or periodontitis for the presence of HPV and EBV viruses. In transplant recipients, EBV was substantially linked to periodontitis and/or gingivitis (P = 0.011) but not HPV (P = 0.766)[124]. There was no correlation found between the periodontal state and the presence of HPV in the oral cavity in an investigation from Argentine involving women with gynecological infections[125]. Finally, a very recent meta-analysis found that among people with confirmed periodontitis, there was no significant increase in the likelihood of high-risk oral HPV infection (OR = 4.71, 95%CI: 0.57–38.97). However, compared to people without periodontitis, individuals with the disease had a 3.65-fold increased risk of developing an oral HPV infection of any kind (95%CI: 1.67–8.01)[126].
The precise nature and degree of the link between HPV and the onset and progression of periodontal disease remains unclear. In addition, the mechanism is also under investigation. Nonetheless, it is well known that HPV has a tropism for squamous epithelium. Viral particles cause micro-abrasions or epithelial injury, which expose the basal cells of the epithelium. There is still some mystery about HPV receptors and the way the virus enters cells. Briefly, HPV-16 attaches to laminin in the extracellular matrix or basement membrane, which causes epithelial cells to die.
In conclusion, people with periodontal disease may have HPV in their periodontal epithelium, and these individuals often have a higher risk of developing periodontitis. It is believed that basal keratinocytes in the ulcerated gingival sulcus epithelium are infected by HPV in the inflammatory periodontal tissue. A distinct oral microbiome may be linked to oral HPV infection, even if the precise connections between periodontopathic bacteria and HPV are still unknown. Using clinical definitions of oral HPV infection and periodontitis and concentrating on high-risk populations for oral HPV infection, future longitudinal research should assess this association in more detail. Examining this correlation is crucial since periodontitis may indicate who is more susceptible to oral HPV infection and maybe oropharyngeal malignancies linked to HPV. As a result, treating patients with chronic periodontitis is essential to maintaining dental health and hygiene and preventing potentially fatal conditions like oral cancer.
HEPATITIS B AND C VIRUSES
HCV is an RNA virus that is a member of the flaviviridae family of viruses. Hepatitis B virus (HBV), on the other hand, is a DNA virus that only infects humans. These viruses are not immediately cytopathic; rather, they multiply in the cytoplasm of hepatocytes[127]. Fast viral replication, ongoing cell-to-cell transmission, and a weak T-cell immune response to viral antigens appear to be necessary for persistent infection[128].
An estimated 50 million people worldwide suffer from a chronic HCV infection, and one million new cases are reported each year. According to WHO estimates, hepatitis C killed about 242 thousand individuals in 2022[129]. According to WHO predictions, 1.2 million new cases of chronic hepatitis B infection occur annually, impacting 254 million people worldwide in 2022. Hepatitis B is expected to have killed 1.1 million people in 2022. Millions of people are afflicted with viral hepatitis and its aftereffects despite the availability of an efficient treatment and vaccine[130].
Acute and chronic hepatitis, non-alcoholic fatty liver disease (NAFLD), liver fibrosis and cirrhosis, hepatocellular cancer, and extra-hepatic symptoms are among the sequelae and effects of HCV and HBV. Regarding the extra-hepatic symptoms, glomerulonephritis and polyarteritis nodosa have been reported in cases of persistent HBV infection[131]. Mixed cryoglobulinemia, along with the accompanying systemic vasculitis, is a common extra-hepatic symptom of chronic HCV infection[132]. Possible clinical manifestations include weakness, arthralgias, purpura, and renal dysfunction. Primary oral manifestations of HBV and HBV include lichen planus, Sjögren-like sialadenitis, and oral squamous cell carcinoma[133,134].
Periodontitis have been studied in relation to various aspects of liver disease, such as NAFLD, liver cirrhosis (LC), hepatocellular carcinoma and liver transplantation. For instance, in a Finnish cohort study comprised of 6165 individuals without baseline liver diseases were followed up for 12 years. During the follow-up, 79 patients had a serious liver incident. In the general population, periodontitis was linked to incidence of liver disease, regardless of other factors[135]. Periodontal disease is a risk factor for NAFLD, according to numerous cross-sectional and epidemiological studies. According to certain in vivo animal models, periodontopathic bacterial infection quickens the course of NAFLD and is associated with increased steatosis[136]. Furthermore, the presence of periodontopathic bacteria in the liver may indicate a direct correlation between these bacteria and NAFLD. Additionally, the lipopolysaccharide produced by P. gingivalis and A. actinomycetemcomitans induces inflammation and intracellular lipid buildup in hepatocytes[136,137]. Out of four epidemiological systematic review and meta-analyses on the association between NAFLD and periodontitis, three of them found significant correlation[138-141]. Grønkjaer[142] conducted a systematic review of the literature from 1981 to 2014 and found that, according to multiple different periodontal indicators, patients with LC had a higher incidence of periodontal disease. But the type and degree of the relationship were still unknown, particularly in terms of whether periodontal disease and the severity and etiology of cirrhosis are associated[142]. In a recent meta-analysis, cirrhotic patients presented a greater and significant mean of clinical attachment loss, probing depth and alveolar bone loss than those without LC. Authors concluded that LC patients have poor periodontal conditions and a higher prevalence of periodontitis[143]. Concerning the risk of hepatocellular, Al-Maweri et al[144] systematically reviewed the published literature on the link between tooth loss/periodontitis and the risk of liver cancer. Researchers stated that available evidence suggests a possibility; however, the evidence was not conclusive enough[144]. In most of these researches, the clinical liver condition is investigated, rather than the exact presence and effect of HBV/HCV. Therefore, it is important to bear in mind that the studied liver conditions may have been caused by other non-viral causes.
Some other research examined periodontitis in individuals with confirmed HCV and HBV infections. Hepatitis virus infection and periodontitis were positively correlated in a large cross-sectional study from the NHANES spanning the years 2003–2018, with 5755 individuals (OR = 2.60; 95%CI: 1.51-4.49). Additionally, there was a high correlation (OR = 2.13; 95%CI: 1.19-3.82) found between moderate periodontitis and hepatitis virus infection. This correlation was even more pronounced for severe periodontitis (OR = 3.58; 95%CI: 1.77-7.21). Significantly, there was a constant positive correlation between periodontitis and hepatitis virus infection in several subgroups[145]. In patients with chronic hepatitis C who had periodontitis, positive associations were seen between the levels of IL-1β and IL-1α in gingival fluid and specific clinical periodontal criteria; and this was also related with the age of the viral hepatitis C diagnosis[146]. Salivary occult blood test was used in a retrospective research to screen for periodontal disease in 351 individuals with liver disorders due to HBV, HCV, or both. Multivariate research revealed that five factors—being 65 years of age or older, tooth brushing just once a day, having a platelet count below 80000, and being obese—were linked to periodontal disease. The authors mentioned that the development of viral liver disease may be linked to periodontitis[147]. Using the CPITN index (Community Periodontal Index of Treatment Needs), Coates et al[148] examined the periodontal condition in patients with hepatitis C. Despite no discernible variation in CPITN categories across the persons examined, there was a clear indication of poor periodontal health in the hepatitis patients[148]. Aspartate amino-transferase levels in the gingival tissue of patients with periodontal disease have been demonstrated to be elevated and to be correlated with the activity of the disease[149]. Additionally, non-surgical periodontal therapy has been shown to improve periodontal inflammation in patients with chronic viral hepatitis[150]. Finally, in animal model study, authors concluded that periodontitis may be an independent risk factor for liver fibrosis in rats when periodontitis was induced by ligatures[151].
Based on these and the similar findings, the concept of oral-intestine-liver axis has been proposed. This is explained through certain premises: The etiology of periodontitis is largely influenced by bacteria of the red complex, which are abundant in deep periodontal pockets and active periodontal lesions[152]. These particular periodontal infectious agents are easily swallowed and go from the oral cavity to the stomach, where they may significantly alter the gut microbiota. It has recently proposed that the cause of some systemic disease, particularly liver disease, might be the disruption of the composition of the intestinal microbiota by orally derived periodontal pathogenic bacteria[153]. Due to the possibility of liver-related consequences and the translocation of oral bacteria and their toxins into the intestine, periodontitis may be especially concerning in patients with liver disease. Systemic endotoxemia, usually intestinal in origin, is linked to liver damage, liver disease development, and decompensation of cirrhosis[154,155]. Hence, the mechanisms linking periodontitis to viral hepatitis include periodontopathogenic bacteria, pro-inflammatory mediators and oxidative stress.
To sum up, there seems to be a bi-directional relation between periodontitis and certain liver diseases of viral origin. Additional research is necessary to determine whether there is a connection between the viral infection and other inflammatory markers found in the gingival fluid. This will allow us to better understand if patients with viral hepatitis who are already at risk of developing periodontal disease or those who are already at risk of developing periodontitis may express other biomarkers specific to the liver more frequently.
CONCLUSION
Although periodontitis is mainly a bacterial inflammation, several other modifiable and non-modifiable risk factors may play role in its initiation and progression. Viruses may take part directly through attacking the periodontal tissue and indirectly through increasing the vulnerability of the immune system and providing a higher chance for the colonization of the periodontopathic bacteria in the oral cavity. Further clinical, translational, experimental, epigenetic and epidemiological research is needed to clarify the exact nature and extent of the role of viruses in periodontitis. This will positively affect the life of millions among healthy population and virally infected people with periodontitis.
Footnotes
Conflict-of-interest statement: Authors declare that they have no conflict of interests.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Virology
Country of origin: France
Peer-review report’s classification
Scientific Quality: Grade A
Novelty: Grade A
Creativity or Innovation: Grade A
Scientific Significance: Grade A
P-Reviewer: Zhang H S-Editor: Liu H L-Editor: A P-Editor: Zhang YL
Contributor Information
Mohammed Khalid Mahmood, Aix-Marseille University, CNRS, EFS, ADES, Marseille 13000, France.
Mohammed Taib Fatih, College of Dentistry, Komar University of Science and technology, Sulaimani 46001, Iraq.
Handren Ameer Kurda, College of Dentistry, Sulaimani University, Sulaimani 46001, Iraq.
Nwsiba Khalid Mahmood, Department of Biology, College of Science, Sulaimani University, Sulaimani 46001, Iraq. mo.barzinji88@gmail.com.
Farman Uthman Shareef, Department of Medical Laboratory Science, College of Science, Charmo University, Chamchamal/Sulaimani 46001, Iraq.
Hemin Faraidun, Department of Biology, University of Freiburg, Mina Biotech, Freiburg 79098, Germany.
Herve Tassery, Department of Odontology, Timone Hospital, Aix Marseille University, APHM, Marseille 13000, France, LBN Laboratory, Montpellier 34000, France.
Delphine Tardivo, Department of Odontology, Timone Hospital, Aix Marseille University, APHM, CNRS, EFS, ADES, Marseille 13000, France.
Romain Lan, Department of Odontology, Timone Hospital, Aix Marseille University, APHM, CNRS, EFS, ADES, Marseille 13000, France.
Zana Fuad Noori, Department of Dentistry, American University of Sulaimani Iraq AUIS, Sulaimani 46001, Iraq.
Balen Hamid Qadir, College of Dentistry, Komar University of Science and technology, Sulaimani 46001, Iraq.
Arman Dlshad Hassan, Department of Biomedical Science, University of Denver, Denver, CO 80014, United States.
References
- 1.Ioannou AL, Kotsakis GA, Hinrichs JE. Prognostic factors in periodontal therapy and their association with treatment outcomes. World J Clin Cases. 2014;2:822–827. doi: 10.12998/wjcc.v2.i12.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhansali RS. Non-surgical periodontal therapy: An update on current evidence. World J Stomatol. 2014;3:38. [Google Scholar]
- 3.Albandar JM. Epidemiology and risk factors of periodontal diseases. Dent Clin North Am. 2005;49:517–532, v-vi. doi: 10.1016/j.cden.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Xu HM, Shen XJ, Liu J. Establishment of models to predict factors influencing periodontitis in patients with type 2 diabetes mellitus. World J Diabetes. 2023;14:1793–1802. doi: 10.4239/wjd.v14.i12.1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahmood MK, Kurda HA, Qadir BH, Tassery H, Lan R, Tardivo D, Abdulghafor MA. Implication of serum and salivary albumin tests in the recent oral health related epidemiological studies: A narrative review. Saudi Dent J. 2024;36:698–707. doi: 10.1016/j.sdentj.2024.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chalabi M, Rezaie F, Moghim S, Mogharehabed A, Rezaei M, Mehraban B. Periodontopathic bacteria and herpesviruses in chronic periodontitis. Mol Oral Microbiol. 2010;25:236–240. doi: 10.1111/j.2041-1014.2010.00571.x. [DOI] [PubMed] [Google Scholar]
- 7.Thomasini RL, Pereira FSM. Impact of different types of herpesviral infections in the oral cavity. World J Stomatol. 2016;5:22. [Google Scholar]
- 8.Carrozzo M, Scally K. Oral manifestations of hepatitis C virus infection. World J Gastroenterol. 2014;20:7534–7543. doi: 10.3748/wjg.v20.i24.7534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Markopoulos AK. Role of human papillomavirus in the pathogenesis of oral squamous cell carcinoma. World J Exp Med. 2012;2:65–69. doi: 10.5493/wjem.v2.i4.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abdel Massih RC, Razonable RR. Human herpesvirus 6 infections after liver transplantation. World J Gastroenterol. 2009;15:2561–2569. doi: 10.3748/wjg.15.2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Looker KJ, Welton NJ, Sabin KM, Dalal S, Vickerman P, Turner KME, Boily MC, Gottlieb SL. Global and regional estimates of the contribution of herpes simplex virus type 2 infection to HIV incidence: a population attributable fraction analysis using published epidemiological data. Lancet Infect Dis. 2020;20:240–249. doi: 10.1016/S1473-3099(19)30470-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Slots J, Rams TE. Herpesvirus-Bacteria pathogenic interaction in juvenile (aggressive) periodontitis. A novel etiologic concept of the disease. Periodontol 2000. 2024;94:532–538. doi: 10.1111/prd.12501. [DOI] [PubMed] [Google Scholar]
- 13.Slots J. Periodontal herpesviruses: prevalence, pathogenicity, systemic risk. Periodontol 2000. 2015;69:28–45. doi: 10.1111/prd.12085. [DOI] [PubMed] [Google Scholar]
- 14.Zakay-Rones Z, Hochman N, Rones Y. Immunological response to herpes simplex virus in human gingival fluid. J Periodontol. 1982;53:42–45. doi: 10.1902/jop.1982.53.1.42. [DOI] [PubMed] [Google Scholar]
- 15.Contreras A, Nowzari H, Slots J. Herpesviruses in periodontal pocket and gingival tissue specimens. Oral Microbiol Immunol. 2000;15:15–18. doi: 10.1034/j.1399-302x.2000.150103.x. [DOI] [PubMed] [Google Scholar]
- 16.Kamma JJ, Contreras A, Slots J. Herpes viruses and periodontopathic bacteria in early-onset periodontitis. J Clin Periodontol. 2001;28:879–885. doi: 10.1034/j.1600-051x.2001.028009879.x. [DOI] [PubMed] [Google Scholar]
- 17.Yapar M, Saygun I, Ozdemir A, Kubar A, Sahin S. Prevalence of human herpesviruses in patients with aggressive periodontitis. J Periodontol. 2003;74:1634–1640. doi: 10.1902/jop.2003.74.11.1634. [DOI] [PubMed] [Google Scholar]
- 18.Contreras A, Slots J. Active cytomegalovirus infection in human periodontitis. Oral Microbiol Immunol. 1998;13:225–230. doi: 10.1111/j.1399-302x.1998.tb00700.x. [DOI] [PubMed] [Google Scholar]
- 19.Alzahrani AA. Association between human herpes virus and aggressive periodontitis: A systematic review. Saudi J Dent Res. 2017;8:97–104. [Google Scholar]
- 20.Song Y, Liu N, Gao L, Yang D, Liu J, Xie L, Dan H, Chen Q. Association between human herpes simplex virus and periodontitis: results from the continuous National Health and Nutrition Examination Survey 2009-2014. BMC Oral Health. 2023;23:675. doi: 10.1186/s12903-023-03416-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maulani C, Auerkari EI, C Masulili SL, Soeroso Y, Djoko Santoso W, S Kusdhany L. Association between Epstein-Barr virus and periodontitis: A meta-analysis. PLoS One. 2021;16:e0258109. doi: 10.1371/journal.pone.0258109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roca-Millan E, Domínguez-Mínger J, Schemel-Suárez M, Estrugo-Devesa A, Marí-Roig A, López-López J. Epstein-Barr Virus and Peri-Implantitis: A Systematic Review and Meta-Analysis. Viruses. 2021;13 doi: 10.3390/v13020250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao Z, Lv J, Wang M. Epstein-Barr virus is associated with periodontal diseases: A meta-analysis based on 21 case-control studies. Medicine (Baltimore) 2017;96:e5980. doi: 10.1097/MD.0000000000005980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Botero JE, Rodríguez-Medina C, Jaramillo-Echeverry A, Contreras A. Association between human cytomegalovirus and periodontitis: A systematic review and meta-analysis. J Periodontal Res. 2020;55:551–558. doi: 10.1111/jre.12742. [DOI] [PubMed] [Google Scholar]
- 25.Arduino PG, Cabras M, Lodi G, Petti S. Herpes simplex virus type 1 in subgingival plaque and periodontal diseases. Meta-analysis of observational studies. J Periodontal Res. 2022;57:256–268. doi: 10.1111/jre.12968. [DOI] [PubMed] [Google Scholar]
- 26.Arduino PG, Alovisi M, Petti S. Herpes simplex virus type 1 in periapical pathoses: Systematic review and meta-analysis. Oral Dis. 2024;30:865–876. doi: 10.1111/odi.14645. [DOI] [PubMed] [Google Scholar]
- 27.Jakovljevic A, Andric M, Jacimovic J, Milasin J, Botero JE. Herpesviruses in Periodontitis: An Umbrella Review. Adv Exp Med Biol. 2022;1373:139–155. doi: 10.1007/978-3-030-96881-6_7. [DOI] [PubMed] [Google Scholar]
- 28.Li F, Zhu C, Deng FY, Wong MCM, Lu HX, Feng XP. Herpesviruses in etiopathogenesis of aggressive periodontitis: A meta-analysis based on case-control studies. PLoS One. 2017;12:e0186373. doi: 10.1371/journal.pone.0186373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhu C, Li F, Wong MC, Feng XP, Lu HX, Xu W. Association between Herpesviruses and Chronic Periodontitis: A Meta-Analysis Based on Case-Control Studies. PLoS One. 2015;10:e0144319. doi: 10.1371/journal.pone.0144319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jakovljevic A, Andric M. Human cytomegalovirus and Epstein-Barr virus in etiopathogenesis of apical periodontitis: a systematic review. J Endod. 2014;40:6–15. doi: 10.1016/j.joen.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 31.Contreras A, Mardirossian A, Slots J. Herpesviruses in HIV-periodontitis. J Clin Periodontol. 2001;28:96–102. doi: 10.1034/j.1600-051x.2001.280115.x. [DOI] [PubMed] [Google Scholar]
- 32.Slots J. Herpesvirus periodontitis: infection beyond biofilm. J Calif Dent Assoc. 2011;39:393–399. [PubMed] [Google Scholar]
- 33.Carpenter CC, Fischl MA, Hammer SM, Hirsch MS, Jacobsen DM, Katzenstein DA, Montaner JS, Richman DD, Saag MS, Schooley RT, Thompson MA, Vella S, Yeni PG, Volberding PA. Antiretroviral therapy for HIV infection in 1998: updated recommendations of the International AIDS Society-USA Panel. JAMA. 1998;280:78–86. doi: 10.1001/jama.280.1.78. [DOI] [PubMed] [Google Scholar]
- 34.Ball SC. Increased longevity in HIV: caring for older HIV-infected adults. Care Manag J. 2014;15:76–82. doi: 10.1891/1521-0987.15.2.76. [DOI] [PubMed] [Google Scholar]
- 35.Tran BX, Phan HT, Latkin CA, Nguyen HLT, Hoang CL, Ho CSH, Ho RCM. Understanding Global HIV Stigma and Discrimination: Are Contextual Factors Sufficiently Studied? (GAP(RESEARCH)) Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16111899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tappuni AR. The global changing pattern of the oral manifestations of HIV. Oral Dis. 2020;26 Suppl 1:22–27. doi: 10.1111/odi.13469. [DOI] [PubMed] [Google Scholar]
- 37.Moosazadeh M, Shafaroudi AM, Gorji NE, Barzegari S, Nasiri P. Prevalence of oral lesions in patients with AIDS: a systematic review and meta-analysis. Evid Based Dent. 2021 doi: 10.1038/s41432-021-0209-8. [DOI] [PubMed] [Google Scholar]
- 38.Itin PH, Lautenschlager S. Viral lesions of the mouth in HIV-infected patients. Dermatology. 1997;194:1–7. doi: 10.1159/000246047. [DOI] [PubMed] [Google Scholar]
- 39.Ryder MI, Shiboski C, Yao TJ, Moscicki AB. Current trends and new developments in HIV research and periodontal diseases. Periodontol 2000. 2020;82:65–77. doi: 10.1111/prd.12321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Almeida VL, Lima IFP, Ziegelmann PK, Paranhos LR, de Matos FR. Impact of highly active antiretroviral therapy on the prevalence of oral lesions in HIV-positive patients: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2017;46:1497–1504. doi: 10.1016/j.ijom.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 41.Ndiaye CF, Critchlow CW, Leggott PJ, Kiviat NB, Ndoye I, Robertson PB, Georgas KN. Periodontal status of HIV-1 and HIV-2 seropositive and HIV seronegative female commercial sex workers in Senegal. J Periodontol. 1997;68:827–831. doi: 10.1902/jop.1997.68.9.827. [DOI] [PubMed] [Google Scholar]
- 42.McKaig RG, Thomas JC, Patton LL, Strauss RP, Slade GD, Beck JD. Prevalence of HIV-associated periodontitis and chronic periodontitis in a southeastern US study group. J Public Health Dent. 1998;58:294–300. doi: 10.1111/j.1752-7325.1998.tb03012.x. [DOI] [PubMed] [Google Scholar]
- 43.Kroidl A, Schaeben A, Oette M, Wettstein M, Herfordt A, Häussinger D. Prevalence of oral lesions and periodontal diseases in HIV-infected patients on antiretroviral therapy. Eur J Med Res. 2005;10:448–453. [PubMed] [Google Scholar]
- 44.Alves M, Mulligan R, Passaro D, Gawell S, Navazesh M, Phelan J, Greenspan D, Greenspan JS. Longitudinal evaluation of loss of attachment in HIV-infected women compared to HIV-uninfected women. J Periodontol. 2006;77:773–779. doi: 10.1902/jop.2006.P04039. [DOI] [PubMed] [Google Scholar]
- 45.Ntolou P, Pani P, Panis V, Madianos P, Vassilopoulos S. The effect of antiretroviral therapyon the periodontal conditions of patients with HIV infection: A systematic review and meta-analysis. J Clin Periodontol. 2023;50:170–182. doi: 10.1111/jcpe.13735. [DOI] [PubMed] [Google Scholar]
- 46.Valentine J, Saladyanant T, Ramsey K, Blake J, Morelli T, Southerland J, Quinlivan EB, Phillips C, Nelson J, DeParis K, Webster-Cyriaque J. Impact of periodontal intervention on local inflammation, periodontitis, and HIV outcomes. Oral Dis. 2016;22 Suppl 1:87–97. doi: 10.1111/odi.12419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sivakumar I, Arunachalam S, Choudhary S, Buzayan MM. Does HIV infection affect the survival of dental implants? A systematic review and meta-analysis. J Prosthet Dent. 2021;125:862–869. doi: 10.1016/j.prosdent.2020.04.001. [DOI] [PubMed] [Google Scholar]
- 48.Pavan P, Pereira VT, Souza RC, Souza CO, Torres SR, Colombo AP, da Costa LJ, Sansone C, de Uzeda M, Gonçalves LS. Levels of HIV-1 in subgingival biofilm of HIV-infected patients. J Clin Periodontol. 2014;41:1061–1068. doi: 10.1111/jcpe.12306. [DOI] [PubMed] [Google Scholar]
- 49.Gonçalves LS, Ferreira SM, Silva A Jr, Villoria GE, Costinha LH, Colombo AP. Association of T CD4 lymphocyte levels and chronic periodontitis in HIV-infected brazilian patients undergoing highly active anti-retroviral therapy: clinical results. J Periodontol. 2005;76:915–922. doi: 10.1902/jop.2005.76.6.915. [DOI] [PubMed] [Google Scholar]
- 50.Brito A, Escalona LA, Correnti M, Perrone M, Bravo IM, Tovar V. Periodontal conditions and distribution of Prevotella intermedia, Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans in HIV-infected patients undergoing anti-retroviral therapy and in an HIV-seronegative group of the Venezuelan population. Acta Odontol Latinoam. 2008;21:89–96. [PubMed] [Google Scholar]
- 51.Engeland CG, Jang P, Alves M, Marucha PT, Califano J. HIV infection and tooth loss. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:321–326. doi: 10.1016/j.tripleo.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 52.Vastardis SA, Yukna RA, Fidel PL Jr, Leigh JE, Mercante DE. Periodontal disease in HIV-positive individuals: association of periodontal indices with stages of HIV disease. J Periodontol. 2003;74:1336–1341. doi: 10.1902/jop.2003.74.9.1336. [DOI] [PubMed] [Google Scholar]
- 53.Vernon LT, Demko CA, Whalen CC, Lederman MM, Toossi Z, Wu M, Han YW, Weinberg A. Characterizing traditionally defined periodontal disease in HIV+ adults. Community Dent Oral Epidemiol. 2009;37:427–437. doi: 10.1111/j.1600-0528.2009.00485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Groenewegen H, Delli K, Vissink A, Spijkervet FKL, Bierman WFW. Immune markers and microbial factors are related with periodontitis severity in people with HIV. Clin Oral Investig. 2023;27:1255–1263. doi: 10.1007/s00784-022-04758-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Howell RB, Jandinski JJ, Palumbo P, Shey Z, Houpt MI. Oral soft tissue manifestations and CD4 lymphocyte counts in HIV-infected children. Pediatr Dent. 1996;18:117–120. [PubMed] [Google Scholar]
- 56.Santos LC, Castro GF, de Souza IP, Oliveira RH. Oral manifestations related to immunosuppression degree in HIV-positive children. Braz Dent J. 2001;12:135–138. [PubMed] [Google Scholar]
- 57.Ranganathan K, Geethalakshmi E, Krishna Mohan Rao U, Vidya KM, Kumarasamy N, Solomon S. Orofacial and systemic manifestations in 212 paediatric HIV patients from Chennai, South India. Int J Paediatr Dent. 2010;20:276–282. doi: 10.1111/j.1365-263X.2010.01050.x. [DOI] [PubMed] [Google Scholar]
- 58.Gona P, Van Dyke RB, Williams PL, Dankner WM, Chernoff MC, Nachman SA, Seage GR 3rd. Incidence of opportunistic and other infections in HIV-infected children in the HAART era. JAMA. 2006;296:292–300. doi: 10.1001/jama.296.3.292. [DOI] [PubMed] [Google Scholar]
- 59.Lam PPY, Zhou N, Yiu CKY, Wong HM. Impact of Antiretroviral Therapy on Oral Health among Children Living with HIV: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2022;19 doi: 10.3390/ijerph191911943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brady LJ, Walker C, Oxford GE, Stewart C, Magnusson I, McArthur W. Oral diseases, mycology and periodontal microbiology of HIV-1-infected women. Oral Microbiol Immunol. 1996;11:371–380. doi: 10.1111/j.1399-302x.1996.tb00198.x. [DOI] [PubMed] [Google Scholar]
- 61.Tsang CS, Samaranayake LP. Predominant cultivable subgingival microbiota of healthy and HIV-infected ethnic Chinese. APMIS. 2001;109:117–126. doi: 10.1034/j.1600-0463.2001.d01-113.x. [DOI] [PubMed] [Google Scholar]
- 62.Valian NK, houshmand B, Ardakani MT, Mahmoudi S. Microbiological study of periodontal disease in populations with HIV: a systematic review and meta-analysis. 2021 preprint. [DOI] [PubMed] [Google Scholar]
- 63.Patel M, Coogan M, Galpin JS. Periodontal pathogens in subgingival plaque of HIV-positive subjects with chronic periodontitis. Oral Microbiol Immunol. 2003;18:199–201. doi: 10.1034/j.1399-302x.2003.00064.x. [DOI] [PubMed] [Google Scholar]
- 64.Ramos MP, Ferreira SM, Silva-Boghossian CM, Souto R, Colombo AP, Noce CW, Gonçalves LS. Necrotizing periodontal diseases in HIV-infected Brazilian patients: a clinical and microbiologic descriptive study. Quintessence Int. 2012;43:71–82. [PubMed] [Google Scholar]
- 65.Lackner AA, Lederman MM, Rodriguez B. HIV pathogenesis: the host. Cold Spring Harb Perspect Med. 2012;2:a007005. doi: 10.1101/cshperspect.a007005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Spear GT, Alves ME, Cohen MH, Bremer J, Landay AL. Relationship of HIV RNA and cytokines in saliva from HIV-infected individuals. FEMS Immunol Med Microbiol. 2005;45:129–136. doi: 10.1016/j.femsim.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 67.Yeung SC, Kazazi F, Randle CG, Howard RC, Rizvi N, Downie JC, Donovan BJ, Cooper DA, Sekine H, Dwyer DE. Patients infected with human immunodeficiency virus type 1 have low levels of virus in saliva even in the presence of periodontal disease. J Infect Dis. 1993;167:803–809. doi: 10.1093/infdis/167.4.803. [DOI] [PubMed] [Google Scholar]
- 68.Mataftsi M, Skoura L, Sakellari D. HIV infection and periodontal diseases: an overview of the post-HAART era. Oral Dis. 2011;17:13–25. doi: 10.1111/j.1601-0825.2010.01727.x. [DOI] [PubMed] [Google Scholar]
- 69.Challacombe SJ, Naglik JR. The effects of HIV infection on oral mucosal immunity. Adv Dent Res. 2006;19:29–35. doi: 10.1177/154407370601900107. [DOI] [PubMed] [Google Scholar]
- 70.SeyedAlinaghi S, Oliaei S, Kianzad S, Afsahi AM, MohsseniPour M, Barzegary A, Mirzapour P, Behnezhad F, Noori T, Mehraeen E, Dadras O, Voltarelli F, Sabatier JM. Reinfection risk of novel coronavirus (COVID-19): A systematic review of current evidence. World J Virol. 2020;9:79–90. doi: 10.5501/wjv.v9.i5.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Taherkhani R, Taherkhani S, Farshadpour F. Dynamics of host immune responses to SARS-CoV-2. World J Clin Cases. 2021;9:4480–4490. doi: 10.12998/wjcc.v9.i18.4480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bahmani M, Chegini R, Ghanbari E, Sheykhsaran E, Shiri Aghbash P, Leylabadlo HE, Moradian E, Kazemzadeh Houjaghan AM, Bannazadeh Baghi H. Severe acute respiratory syndrome coronavirus 2 infection: Role of interleukin-6 and the inflammatory cascade. World J Virol. 2022;11:113–128. doi: 10.5501/wjv.v11.i3.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nassar M, Nso N, Alfishawy M, Novikov A, Yaghi S, Medina L, Toz B, Lakhdar S, Idrees Z, Kim Y, Gurung DO, Siddiqui RS, Zheng D, Agladze M, Sumbly V, Sandhu J, Castillo FC, Chowdhury N, Kondaveeti R, Bhuiyan S, Perez LG, Ranat R, Gonzalez C, Bhangoo H, Williams J, Osman AE, Kong J, Ariyaratnam J, Mohamed M, Omran I, Lopez M, Nyabera A, Landry I, Iqbal S, Gondal AZ, Hassan S, Daoud A, Baraka B, Trandafirescu T, Rizzo V. Current systematic reviews and meta-analyses of COVID-19. World J Virol. 2021;10:182–208. doi: 10.5501/wjv.v10.i4.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rezaei M, Ziai SA, Fakhri S, Pouriran R. ACE2: Its potential role and regulation in severe acute respiratory syndrome and COVID-19. J Cell Physiol. 2021;236:2430–2442. doi: 10.1002/jcp.30041. [DOI] [PubMed] [Google Scholar]
- 75.Iranmanesh B, Khalili M, Amiri R, Zartab H, Aflatoonian M. Oral manifestations of COVID-19 disease: A review article. Dermatol Ther. 2021;34:e14578. doi: 10.1111/dth.14578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Şehirli AÖ, Aksoy U, Koca-Ünsal RB, Sayıner S. Role of NLRP3 inflammasome in COVID-19 and periodontitis: Possible protective effect of melatonin. Med Hypotheses. 2021;151:110588. doi: 10.1016/j.mehy.2021.110588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Herrera D, Serrano J, Roldán S, Sanz M. Is the oral cavity relevant in SARS-CoV-2 pandemic? Clin Oral Investig. 2020;24:2925–2930. doi: 10.1007/s00784-020-03413-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dziedzic A, Wojtyczka R. The impact of coronavirus infectious disease 19 (COVID-19) on oral health. Oral Dis. 2021;27 Suppl 3:703–706. doi: 10.1111/odi.13359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Katz J, Yue S, Xue W. Dental diseases are associated with increased odds ratio for coronavirus disease 19. Oral Dis. 2022;28 Suppl 1:991–993. doi: 10.1111/odi.13653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Farid H, Khan M, Jamal S, Ghafoor R. Oral manifestations of Covid-19-A literature review. Rev Med Virol. 2022;32:e2248. doi: 10.1002/rmv.2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang Y, Deng H, Pan Y, Jin L, Hu R, Lu Y, Deng W, Sun W, Chen C, Shen X, Huang XF. Periodontal disease increases the host susceptibility to COVID-19 and its severity: a Mendelian randomization study. J Transl Med. 2021;19:528. doi: 10.1186/s12967-021-03198-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Larvin H, Wilmott S, Wu J, Kang J. The Impact of Periodontal Disease on Hospital Admission and Mortality During COVID-19 Pandemic. Front Med (Lausanne) 2020;7:604980. doi: 10.3389/fmed.2020.604980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Larvin H, Wilmott S, Kang J, Aggarwal VR, Pavitt S, Wu J. Additive Effect of Periodontal Disease and Obesity on COVID-19 Outcomes. J Dent Res. 2021;100:1228–1235. doi: 10.1177/00220345211029638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Marouf N, Cai W, Said KN, Daas H, Diab H, Chinta VR, Hssain AA, Nicolau B, Sanz M, Tamimi F. Association between periodontitis and severity of COVID-19 infection: A case-control study. J Clin Periodontol. 2021;48:483–491. doi: 10.1111/jcpe.13435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sirin DA, Ozcelik F. The relationship between COVID-19 and the dental damage stage determined by radiological examination. Oral Radiol. 2021;37:600–609. doi: 10.1007/s11282-020-00497-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mancini L, Americo LM, Pizzolante T, Donati R, Marchetti E. Impact of COVID-19 on Periodontitis and Peri-Implantitis: A Narrative Review. Front Oral Health. 2022;3:822824. doi: 10.3389/froh.2022.822824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Song J, Wu Y, Yin X, Zhang J. Relationship between periodontitis and COVID-19: A bidirectional two-sample Mendelian randomization study. Health Sci Rep. 2023;6:e1413. doi: 10.1002/hsr2.1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Baima G, Marruganti C, Sanz M, Aimetti M, Romandini M. Periodontitis and COVID-19: Biological Mechanisms and Meta-analyses of Epidemiological Evidence. J Dent Res. 2022;101:1430–1440. doi: 10.1177/00220345221104725. [DOI] [PubMed] [Google Scholar]
- 89.Espinoza-Espinoza DAK, Dulanto-Vargas JA, Cáceres-LaTorre OA, Lamas-Castillo FE, Flores-Mir C, Cervantes-Ganoza LA, López-Gurreonero C, Ladera-Castañeda MI, Cayo-Rojas CF. Association Between Periodontal Disease and the Risk of COVID-19 Complications and Mortality: A Systematic Review. J Int Soc Prev Community Dent. 2021;11:626–638. doi: 10.4103/jispcd.JISPCD_189_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zardawi F, Gul S, Abdulkareem A, Sha A, Yates J. Association Between Periodontal Disease and Atherosclerotic Cardiovascular Diseases: Revisited. Front Cardiovasc Med. 2020;7:625579. doi: 10.3389/fcvm.2020.625579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Llambés F, Arias-Herrera S, Caffesse R. Relationship between diabetes and periodontal infection. World J Diabetes. 2015;6:927–935. doi: 10.4239/wjd.v6.i7.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Liu H, Chen S, Liu M, Nie H, Lu H. Comorbid Chronic Diseases are Strongly Correlated with Disease Severity among COVID-19 Patients: A Systematic Review and Meta-Analysis. Aging Dis. 2020;11:668–678. doi: 10.14336/AD.2020.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Basso L, Chacun D, Sy K, Grosgogeat B, Gritsch K. Periodontal Diseases and COVID-19: A Scoping Review. Eur J Dent. 2021;15:768–775. doi: 10.1055/s-0041-1729139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fernandes Matuck B, Dolhnikoff M, Maia GVA, Isaac Sendyk D, Zarpellon A, Costa Gomes S, Duarte-Neto AN, Rebello Pinho JR, Gomes-Gouvêa MS, Sousa SCOM, Mauad T, Saldiva PHDN, Braz-Silva PH, da Silva LFF. Periodontal tissues are targets for Sars-Cov-2: a post-mortem study. J Oral Microbiol. 2020;13:1848135. doi: 10.1080/20002297.2020.1848135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mancini L, Quinzi V, Mummolo S, Marzo G, Marchetti E. Angiotensin-Converting Enzyme 2 as a Possible Correlation between COVID-19 and Periodontal Disease. Appl Sci. 2020;10:6224. [Google Scholar]
- 96.Awano S, Ansai T, Takata Y, Soh I, Akifusa S, Hamasaki T, Yoshida A, Sonoki K, Fujisawa K, Takehara T. Oral health and mortality risk from pneumonia in the elderly. J Dent Res. 2008;87:334–339. doi: 10.1177/154405910808700418. [DOI] [PubMed] [Google Scholar]
- 97.Molina A, Huck O, Herrera D, Montero E. The association between respiratory diseases and periodontitis: A systematic review and meta-analysis. J Clin Periodontol. 2023;50:842–887. doi: 10.1111/jcpe.13767. [DOI] [PubMed] [Google Scholar]
- 98.Brock M, Bahammam S, Sima C. The Relationships Among Periodontitis, Pneumonia and COVID-19. Front Oral Health. 2021;2:801815. doi: 10.3389/froh.2021.801815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Alfaifi AA, Holm JB, Wang TW, Lim J, Meiller TF, Rock P, Sultan AS, Jabra-Rizk MA. Oral Microbiota Alterations in Subjects with SARS-CoV-2 Displaying Prevalence of the Opportunistic Fungal Pathogen Candida albicans. Microorganisms. 2024;12 doi: 10.3390/microorganisms12071356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fine N, Chadwick JW, Sun C, Parbhakar KK, Khoury N, Barbour A, Goldberg M, Tenenbaum HC, Glogauer M. Periodontal Inflammation Primes the Systemic Innate Immune Response. J Dent Res. 2021;100:318–325. doi: 10.1177/0022034520963710. [DOI] [PubMed] [Google Scholar]
- 101.Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R. The COVID-19 Cytokine Storm; What We Know So Far. Front Immunol. 2020;11:1446. doi: 10.3389/fimmu.2020.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Said KN, Al-Momani AM, Almaseeh JA, Marouf N, Shatta A, Al-Abdulla J, Alaji S, Daas H, Tharupeedikayil SS, Chinta VR, Hssain AA, Abusamak M, Salih S, Barhom N, Cai W, Sanz M, Tamimi F. Association of periodontal therapy, with inflammatory biomarkers and complications in COVID-19 patients: a case control study. Clin Oral Investig. 2022;26:6721–6732. doi: 10.1007/s00784-022-04631-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hosoglu S, Mahmood MK. COVID-19 infection among dentists in Iraqi Kurdistan Region. J Infect Dev Ctries. 2022;16:1439–1444. doi: 10.3855/jidc.15962. [DOI] [PubMed] [Google Scholar]
- 104.Darestani MN, Akbari A, Yaghobee S, Taheri M, Akbari S. COVID-19 Pandemic and Periodontal Practice: The Immunological, Clinical, and Economic Points of View. Biomed Res Int. 2022;2022:3918980. doi: 10.1155/2022/3918980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bae JM. Human papillomavirus infection and gastric cancer risk: A meta-epidemiological review. World J Virol. 2021;10:209–216. doi: 10.5501/wjv.v10.i5.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sigaroodi A, Nadji SA, Naghshvar F, Nategh R, Emami H, Velayati AA. Human papillomavirus is associated with breast cancer in the north part of Iran. ScientificWorldJournal. 2012;2012:837191. doi: 10.1100/2012/837191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Shigeishi H, Sugiyama M, Ohta K. Relationship between the prevalence of oral human papillomavirus DNA and periodontal disease (Review) Biomed Rep. 2021;14:40. doi: 10.3892/br.2021.1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Soheili M, Keyvani H, Soheili M, Nasseri S. Human papilloma virus: A review study of epidemiology, carcinogenesis, diagnostic methods, and treatment of all HPV-related cancers. Med J Islam Repub Iran. 2021;35:65. doi: 10.47176/mjiri.35.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.World Health Organization. Human papillomavirus vaccines: WHO position paper, May 2017-Recommendations. Vaccine. 2017;35:5753–5755. doi: 10.1016/j.vaccine.2017.05.069. [DOI] [PubMed] [Google Scholar]
- 110.Bruni L, Albero G, Rowley J, Alemany L, Arbyn M, Giuliano AR, Markowitz LE, Broutet N, Taylor M. Global and regional estimates of genital human papillomavirus prevalence among men: a systematic review and meta-analysis. Lancet Glob Health. 2023;11:e1345–e1362. doi: 10.1016/S2214-109X(23)00305-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bruni L, Diaz M, Castellsagué X, Ferrer E, Bosch FX, de Sanjosé S. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis. 2010;202:1789–1799. doi: 10.1086/657321. [DOI] [PubMed] [Google Scholar]
- 112.Kreimer AR, Bhatia RK, Messeguer AL, González P, Herrero R, Giuliano AR. Oral human papillomavirus in healthy individuals: a systematic review of the literature. Sex Transm Dis. 2010;37:386–391. doi: 10.1097/OLQ.0b013e3181c94a3b. [DOI] [PubMed] [Google Scholar]
- 113.Tam S, Fu S, Xu L, Krause KJ, Lairson DR, Miao H, Sturgis EM, Dahlstrom KR. The epidemiology of oral human papillomavirus infection in healthy populations: A systematic review and meta-analysis. Oral Oncol. 2018;82:91–99. doi: 10.1016/j.oraloncology.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 114.Horewicz VV, Feres M, Rapp GE, Yasuda V, Cury PR. Human papillomavirus-16 prevalence in gingival tissue and its association with periodontal destruction: a case-control study. J Periodontol. 2010;81:562–568. doi: 10.1902/jop.2009.090571. [DOI] [PubMed] [Google Scholar]
- 115.Wiener RC, Sambamoorthi U, Jurevic RJ. Association of periodontitis and human papillomavirus in oral rinse specimens: Results from the National Health and Nutrition Survey 2009-2012. J Am Dent Assoc. 2015;146:382–389. doi: 10.1016/j.adaj.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hormia M, Willberg J, Ruokonen H, Syrjänen S. Marginal periodontium as a potential reservoir of human papillomavirus in oral mucosa. J Periodontol. 2005;76:358–363. doi: 10.1902/jop.2005.76.3.358. [DOI] [PubMed] [Google Scholar]
- 117.Syrjänen S. Oral manifestations of human papillomavirus infections. Eur J Oral Sci. 2018;126 Suppl 1:49–66. doi: 10.1111/eos.12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sun CX, Bennett N, Tran P, Tang KD, Lim Y, Frazer I, Samaranayake L, Punyadeera C. A Pilot Study into the Association between Oral Health Status and Human Papillomavirus-16 Infection. Diagnostics (Basel) 2017;7 doi: 10.3390/diagnostics7010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ortiz AP, González D, Vivaldi-Oliver J, Castañeda M, Rivera V, Díaz E, Centeno H, Muñoz C, Palefsky J, Joshipura K, Pérez CM. Periodontitis and oral human papillomavirus infection among Hispanic adults. Papillomavirus Res. 2018;5:128–133. doi: 10.1016/j.pvr.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Dayakar MM, Shipilova A, Gupta D. Periodontal pocket as a potential reservoir of high risk human papilloma virus: A pilot study. J Indian Soc Periodontol. 2016;20:136–140. doi: 10.4103/0972-124X.170815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.McDaniel JT, Davis JM, McDermott RJ, Maxfield I, Kapatamoyo K. Predicted prevalence of oral human papillomavirus (HPV) by periodontitis status and HPV vaccination status. J Public Health Dent. 2020;80:132–139. doi: 10.1111/jphd.12357. [DOI] [PubMed] [Google Scholar]
- 122.Shigeishi H, Sugiyama M, Ohta K, Yokoyama S, Sakuma M, Murozumi H, Kato H, Takechi M. High HPV16 E6 viral load in the oral cavity is associated with an increased number of bacteria: A preliminary study. Biomed Rep. 2018;8:59–64. doi: 10.3892/br.2017.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shigeishi H, Murodumi H, Ohta K, Sugiyama M. Detection of HPV16 E6 DNA in periodontal pockets of middle‐aged and older people. Oral Sci Int. 2021;18:50–55. [Google Scholar]
- 124.Baez CF, Savassi-Ribas F, Rocha WM, Almeida SG, Gonçalves MT, Guimarães MA, Cavalcanti SM, Varella RB. Association of Epstein-Barr virus (EBV) but not human papillomavirus (HPV) with gingivitis and/or periodontitis in transplant patients. Rev Inst Med Trop Sao Paulo. 2016;58:58. doi: 10.1590/S1678-9946201658058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Fuster-Rossello L, Ribotta E, Cuffini C, Fuster-Juan M. Human papilloma virus in oral mucosa and its association with periodontal status of gynecologically infected women. Acta Odontol Latinoam. 2014;27:82–88. doi: 10.1590/S1852-48342014000200007. [DOI] [PubMed] [Google Scholar]
- 126.Ali A, Lassi ZS, Kapellas K, Jamieson L, Rumbold AR. A systematic review and meta-analysis of the association between periodontitis and oral high-risk human papillomavirus infection. J Public Health (Oxf) 2021;43:e610–e619. doi: 10.1093/pubmed/fdaa156. [DOI] [PubMed] [Google Scholar]
- 127.Schaefer S. Hepatitis B virus taxonomy and hepatitis B virus genotypes. World J Gastroenterol. 2007;13:14–21. doi: 10.3748/wjg.v13.i1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Caccamo G, Saffioti F, Raimondo G. Hepatitis B virus and hepatitis C virus dual infection. World J Gastroenterol. 2014;20:14559–14567. doi: 10.3748/wjg.v20.i40.14559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Updated Recommendations on Treatment of Adolescents and Children with Chronic HCV Infection, and HCV Simplified Service Delivery and Diagnostics [Internet]. Geneva: World Health Organization; 2022– . [PubMed] [Google Scholar]
- 130.Vittal A, Ghany MG. WHO Guidelines for Prevention, Care and Treatment of Individuals Infected with HBV: A US Perspective. Clin Liver Dis. 2019;23:417–432. doi: 10.1016/j.cld.2019.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Irshad M, Mankotia DS, Irshad K. An insight into the diagnosis and pathogenesis of hepatitis C virus infection. World J Gastroenterol. 2013;19:7896–7909. doi: 10.3748/wjg.v19.i44.7896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Aslan AT, Balaban HY. Hepatitis E virus: Epidemiology, diagnosis, clinical manifestations, and treatment. World J Gastroenterol. 2020;26:5543–5560. doi: 10.3748/wjg.v26.i37.5543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Utsumi T, Lusida MI. Viral hepatitis and human immunodeficiency virus co-infections in Asia. World J Virol. 2015;4:96–104. doi: 10.5501/wjv.v4.i2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Salama II, Raslan HM, Abdel-Latif GA, Salama SI, Sami SM, Shaaban FA, Abdelmohsen AM, Fouad WA. Impact of direct-acting antiviral regimens on hepatic and extrahepatic manifestations of hepatitis C virus infection. World J Hepatol. 2022;14:1053–1073. doi: 10.4254/wjh.v14.i6.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Helenius-Hietala J, Suominen AL, Ruokonen H, Knuuttila M, Puukka P, Jula A, Meurman JH, Åberg F. Periodontitis is associated with incident chronic liver disease-A population-based cohort study. Liver Int. 2019;39:583–591. doi: 10.1111/liv.13985. [DOI] [PubMed] [Google Scholar]
- 136.Mei EH, Yao C, Chen YN, Nan SX, Qi SC. Multifunctional role of oral bacteria in the progression of non-alcoholic fatty liver disease. World J Hepatol. 2024;16:688–702. doi: 10.4254/wjh.v16.i5.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Komazaki R, Katagiri S, Takahashi H, Maekawa S, Shiba T, Takeuchi Y, Kitajima Y, Ohtsu A, Udagawa S, Sasaki N, Watanabe K, Sato N, Miyasaka N, Eguchi Y, Anzai K, Izumi Y. Periodontal pathogenic bacteria, Aggregatibacter actinomycetemcomitans affect non-alcoholic fatty liver disease by altering gut microbiota and glucose metabolism. Sci Rep. 2017;7:13950. doi: 10.1038/s41598-017-14260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Alakhali MS, Al-Maweri SA, Al-Shamiri HM, Al-Haddad K, Halboub E. The potential association between periodontitis and non-alcoholic fatty liver disease: a systematic review. Clin Oral Investig. 2018;22:2965–2974. doi: 10.1007/s00784-018-2726-1. [DOI] [PubMed] [Google Scholar]
- 139.Chen Y, Yang YC, Zhu BL, Wu CC, Lin RF, Zhang X. Association between periodontal disease, tooth loss and liver diseases risk. J Clin Periodontol. 2020;47:1053–1063. doi: 10.1111/jcpe.13341. [DOI] [PubMed] [Google Scholar]
- 140.Wijarnpreecha K, Panjawatanan P, Cheungpasitporn W, Lukens FJ, Harnois DM, Pungpapong S, Ungprasert P. The Association between Periodontitis and Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-analysis. J Gastrointestin Liver Dis. 2020;29:211–217. doi: 10.15403/jgld-841. [DOI] [PubMed] [Google Scholar]
- 141.Alazawi W, Bernabe E, Tai D, Janicki T, Kemos P, Samsuddin S, Syn WK, Gillam D, Turner W. Periodontitis is associated with significant hepatic fibrosis in patients with non-alcoholic fatty liver disease. PLoS One. 2017;12:e0185902. doi: 10.1371/journal.pone.0185902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Grønkjær LL. Periodontal disease and liver cirrhosis: A systematic review. SAGE Open Med. 2015;3:2050312115601122. doi: 10.1177/2050312115601122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bie M, Wu P, Zhou J, Li Y, Zhao L. Periodontal health status in cirrhotic patients: a systematic review and meta-analysis. BMC Oral Health. 2023;23:362. doi: 10.1186/s12903-023-03052-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Al-maweri SA, Ibraheem WI, Al-akhali MS, Shamala A, Halboub E, Alhajj M. Periodontal disease, tooth loss, and the risk of liver cancer: A systematic review. 2021 preprint. [DOI] [PubMed] [Google Scholar]
- 145.Chen X, Zeng Z, Xiao L. The association between periodontitis and hepatitis virus infection: a cross-sectional study utilizing data from the NHANES database (2003-2018) Public Health. 2024;226:114–121. doi: 10.1016/j.puhe.2023.11.005. [DOI] [PubMed] [Google Scholar]
- 146.Surlin P, Gheorghe DN, Popescu DM, Martu AM, Solomon S, Roman A, Lazar L, Stratul SI, Rusu D, Foia L, Boldeanu MV, Boldeanu L, Danilescu M, Rogoveanu I. Interleukin-1α and -1β assessment in the gingival crevicular fluid of periodontal patients with chronic hepatitis C. Exp Ther Med. 2020;20:2381–2386. doi: 10.3892/etm.2020.8906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Nagao Y, Kawahigashi Y, Sata M. Association of Periodontal Diseases and Liver Fibrosis in Patients With HCV and/or HBV infection. Hepat Mon. 2014;14:e23264. doi: 10.5812/hepatmon.23264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Coates EA, Brennan D, Logan RM, Goss AN, Scopacasa B, Spencer AJ, Gorkic E. Hepatitis C infection and associated oral health problems. Aust Dent J. 2000;45:108–114. doi: 10.1111/j.1834-7819.2000.tb00249.x. [DOI] [PubMed] [Google Scholar]
- 149.Yucekal-Tuncer B, Uygur C, Firatli E. Gingival crevicular fluid levels of aspartate amino transferase, sulfide ions and N-benzoyl-DL-arginine-2-naphthylamide in diabetic patients with chronic periodontitis. J Clin Periodontol. 2003;30:1053–1060. doi: 10.1046/j.0303-6979.2003.00426.x. [DOI] [PubMed] [Google Scholar]
- 150.Gheorghe DN, Popescu DM, Salan A, Boldeanu MV, Ionele CM, Pitru A, Turcu-Stiolica A, Camen A, Florescu C, Rogoveanu I, Surlin P. Non-Surgical Periodontal Therapy Could Improve the Periodontal Inflammatory Status in Patients with Periodontitis and Chronic Hepatitis C. J Clin Med. 2021;10 doi: 10.3390/jcm10225275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Mester A, Ciobanu L, Taulescu M, Apostu D, Lucaciu O, Filip GA, Feldrihan V, Licarete E, Ilea A, Piciu A, Oltean-Dan D, Scurtu I, Berce C, Campian RS. Periodontal disease may induce liver fibrosis in an experimental study on Wistar rats. J Periodontol. 2019;90:911–919. doi: 10.1002/JPER.18-0585. [DOI] [PubMed] [Google Scholar]
- 152.Nagao Y, Tanigawa T. Red complex periodontal pathogens are risk factors for liver cirrhosis. Biomed Rep. 2019;11:199–206. doi: 10.3892/br.2019.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Arimatsu K, Yamada H, Miyazawa H, Minagawa T, Nakajima M, Ryder MI, Gotoh K, Motooka D, Nakamura S, Iida T, Yamazaki K. Oral pathobiont induces systemic inflammation and metabolic changes associated with alteration of gut microbiota. Sci Rep. 2014;4:4828. doi: 10.1038/srep04828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Åberg F, Helenius-Hietala J. Oro-hepatic link, endotoxemia, and systemic inflammation: The role of chronic periodontitis. Hepatology. 2016;63:1736. doi: 10.1002/hep.27953. [DOI] [PubMed] [Google Scholar]
- 155.Bajaj JS, Betrapally NS, Hylemon PB, Heuman DM, Daita K, White MB, Unser A, Thacker LR, Sanyal AJ, Kang DJ, Sikaroodi M, Gillevet PM. Salivary microbiota reflects changes in gut microbiota in cirrhosis with hepatic encephalopathy. Hepatology. 2015;62:1260–1271. doi: 10.1002/hep.27819. [DOI] [PMC free article] [PubMed] [Google Scholar]