Abstract
Rheumatic heart disease leads to significant cardiovascular morbidity and mortality globally. This case presentation emphasizes the importance of considering patients’ unique socioeconomic factors, such as crowded living conditions and multigenerational housing, to implement culturally sensitive approaches to prevention, diagnosis, secondary antibiotic prophylaxis, and management.
Key Words: rheumatic heart disease, secondary antibiotic prophylaxis
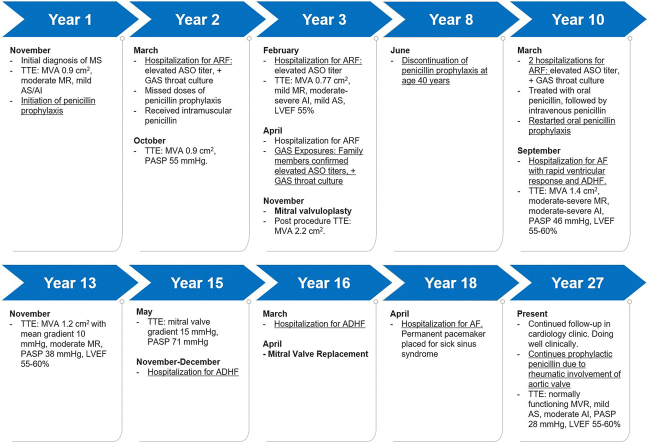
Graphical Abstract
History of Presentation
This presentation follows the clinical course of a woman with rheumatic heart disease (RHD) over 27 years (Figure 1). The patient was 35 years old when a murmur was auscultated during pregnancy. A postpartum transthoracic echocardiogram (TTE) revealed rheumatic valvular disease involving the mitral and aortic valves, with severe mitral stenosis (MS), a mitral valve area (MVA) of 0.9 cm2, moderate mitral regurgitation (MR), mild aortic stenosis, and mild aortic regurgitation.
Learning Objectives
-
•
To discuss the progressive course of rheumatic heart disease and significant cardiovascular morbidity.
-
•
To identify social factors to consider in determining secondary antibiotic prophylaxis duration.
Figure 1.
Timeline Displaying Clinical Progression of RHD as Related to Our Case Presentation
ADHF = acute decompensated heart failure; ARF = acute rheumatic fever; ASO = anti-streptolysin O; AF = atrial fibrillation; AI = aortic insufficiency; AS = aortic stenosis; LVEF = left ventricular ejection fraction; MR = mitral regurgitation; MS = mitral stenosis; MVA = mitral valve area; MVR = mitral valve replacement; PASP = pulmonary artery systolic pressure; GAS = group A streptococcus; TTE = transthoracic echocardiogram.
Secondary antibiotic prophylaxis with intramuscular penicillin was initiated. One year later, she was hospitalized with recurrent acute rheumatic fever (ARF), and the workup revealed elevated antistreptolysin antibodies and a positive β-hemolytic streptococcus group A throat culture. She was noted to have variable compliance with oral antibiotic prophylaxis and her MS had progressed with an MVA of 0.77 cm2. The Wilkins score was 5/16, and the patient underwent successful percutaneous mitral balloon valvuloplasty at age 37 years. Postprocedure, her MVA was 2.2 cm2, and she remained in sinus rhythm for 3 years post-valvuloplasty, after which she had documented atrial fibrillation (AF), and warfarin was initiated. She subsequently had multiple additional admissions for acute decompensated heart failure and AF with rapid ventricular response, requiring multiple rate and rhythm control medications. She was continued on guideline-based antibiotic prophylaxis until she reached 40 years of age.
Seven years after valvuloplasty, at age 43 years, she presented with fever, chills, night sweats, and diffuse joint pain. She denied exposure to sick contacts or recent travel outside of the country. Vital signs were within normal limits. Physical examination was notable for prominent S1, normal S2, and grade II/IV diastolic and grade II/VI systolic murmur. She was admitted for parenteral antibiotics.
Medical History
The patient’s medical history was pertinent for hypertension and hypothyroidism. Social history was notable for emigrating from South America. She lived in a multigenerational home with her husband, children, and grandchildren. At the time of the initial MS diagnosis, her household included an adult child, 2 elementary school-aged children, and a newborn in addition to her and her husband. Within 1 year of her diagnosis, her child’s partner and a grandchild were also living in the home. In total, there were up to 8 people, including 4 young children, living in a 1-bedroom apartment during this period.
Differential Diagnosis
Recurrent ARF, acute decompensated heart failure, acute renal failure, and infectious etiologies were all considered in the differential diagnosis.
Investigations
Laboratory evaluation revealed elevated antistreptolysin antibodies of 1,408 IU/mL and positive β-hemolytic streptococcus group A throat culture. The patient’s family members were noted to be positive carriers for streptococcus infection on throat culture. TTE revealed a left ventricular ejection fraction of 60% to 65%, MVA of 2.2 cm2, mild to moderate MR, moderate to severe aortic regurgitation, and pulmonary artery systolic pressure (PASP) of 42 mm Hg.
Management
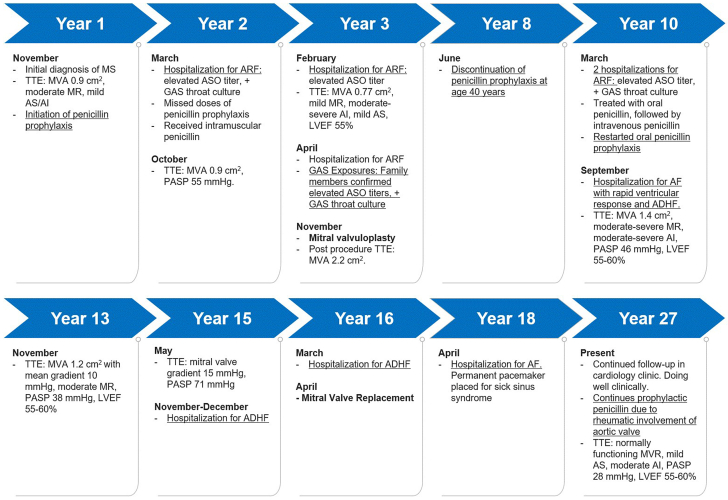
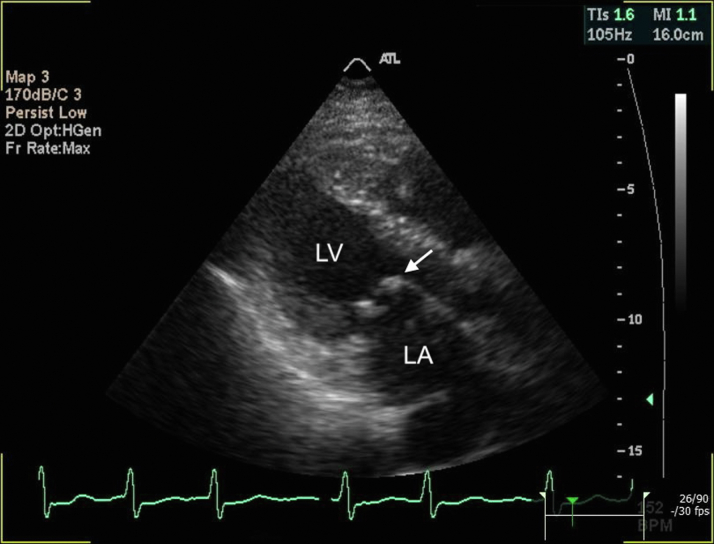
Given recurrent presentations for ARF, high-transmission living environment, and variable compliance with oral therapy, the patient was transitioned to a monthly intramuscular penicillin injection. Five years later, a surveillance TTE revealed an elevated mitral valve gradient to 15 mm Hg and PASP of 71 mm Hg (Figure 2, Figure 3, Figure 4, Video 1).
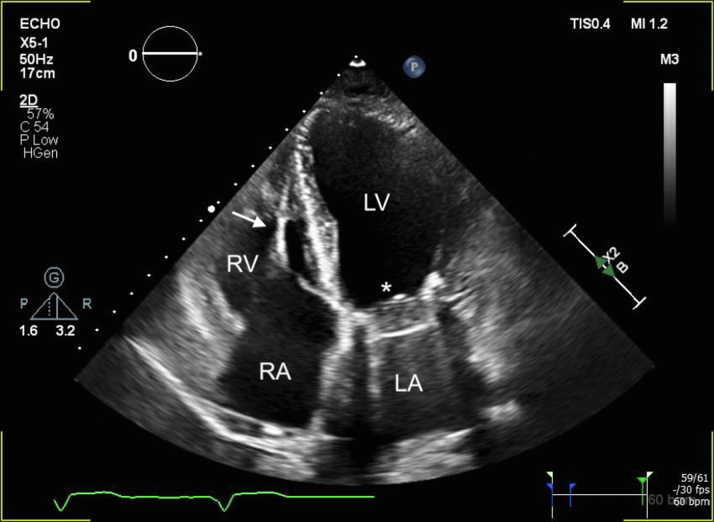
Figure 2.
Presurgical Transthoracic Echocardiogram
Parasternal long-axis view showing the thickened mitral valve leaflets with doming of the anterior mitral leaflet (arrow). LA = left atrium; LV = left ventricle.
Figure 3.
Presurgical M-Mode Echocardiogram Directed Through the Mitral Valve
Thickening and a reduced anterior mitral leaflet E-F slope is demonstrated.
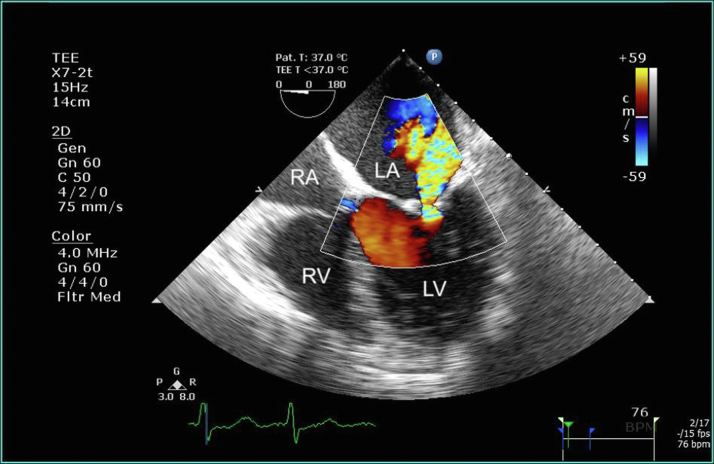
Figure 4.
Presurgical Transesophageal Echocardiogram
Display of 4-chamber view with color Doppler demonstrating moderate mitral regurgitation. LA = left atrium; LV = left ventricle; RA = right atrium; RV = right ventricle.
She had multiple repeat hospitalizations for decompensated heart failure and ultimately underwent mitral valve replacement 13 years after her valvuloplasty at age 50 years. Two years later, she developed worsening paroxysmal AF and sick sinus syndrome, necessitating permanent pacemaker placement.
Discussion
ARF and RHD affect an estimated 40 million people globally and are leading causes of cardiovascular death during the first 5 decades of life, prominent among marginalized populations.1, 2, 3 In nonendemic regions such as the United States, mortality from RHD disproportionally affects populations of immigrants and those from low socioeconomic backgrounds.4
RHD more commonly affects the left-sided valves, particularly the mitral valve, causing acute valvulitis and valvular regurgitation. Isolated aortic disease can also occur but is rare.4 Chronic inflammation, progressive fibrosis, and recurrent bouts lead to commissural fusion and valvular stenosis. Patients with RHD can develop additional complications such as heart failure, endocarditis, arrhythmias, and cardiovascular death.4
Patients with a history of ARF are at very high risk of developing recurrences after subsequent group A streptococcal pharyngitis, which can lead to RHD or worsen existing RHD. Secondary prophylaxis with penicillin reduces streptococcal infections, recurrent attacks of ARF, and frequency and duration of hospitalization in patients with ARF or RHD.5,6 A recent randomized controlled trial of secondary antibiotic prophylaxis in Ugandan children and adolescents with latent RHD found that secondary antibiotic prophylaxis reduced the risk of disease progression at 2 years.7
Current guidelines are based primarily on expert opinion and lack a concise strategy for optimal duration of antibiotic prophylaxis.2 These recommendations focus on patient age, presence and severity of cardiac sequela, and time since the last episode of ARF. However, basing the duration of secondary antibiotic prophylaxis on the last episode of ARF can be problematic, as up to one-third of patients with ARF report no history of pharyngitis and most individuals with RHD have no known history of ARF.4 Current expert consensus recommends considering the risk of group A streptococcus exposure, including high-risk occupations and living environments, before stopping prophylaxis. Moreover, in some individuals, lifetime prophylaxis may be necessary. Social risk factors such as residing within crowded areas, including multigenerational households, is common within some immigrant populations.2 The number of multigenerational Latino households has been found to be about one-third or 31.7%.8 Additionally, high-risk status such as parents and grandparents with young children, healthcare workers, military recruits, and teachers should be considered.2
Follow-Up
The patient has continued routine follow-up in the cardiology clinic and is overall doing well. Her most recent TTE was notable for normal left ventricle ejection fraction, normally functioning mechanical mitral valve, and a PASP of 28 mm Hg (Figure 5). She continues on metoprolol tartrate, amiodarone, digoxin, warfarin for AF, maintenance diuretic with furosemide, and prophylactic penicillin because of the rheumatic involvement of the aortic valve.
Figure 5.
Transthoracic Echocardiogram
Display of 4-chamber view at 10 years after mitral valve replacement. Arrow demonstrates permanent pacemaker lead. Abbreviations as in Figure 4.
Conclusions
There is a strong need to highlight factors beyond patient age and time since the last ARF episode in considering the duration of secondary prophylaxis. Our case highlights the importance of consideration of socioeconomic, environmental, and cultural factors in the management of ARF and RHD within immigrant communities. Although the prevailing wisdom is that ARF is rare in patients over age 30 years, this does not appropriately weigh exposure through living and working conditions. By recognizing the unique circumstances of immigrant and underserved communities, physicians can implement culturally sensitive approaches to management, helping to mitigate the burden of RHD and improve health outcomes for vulnerable patient populations.
Funding Support and Author Disclosures
Dr Jonathan Soverow has received institutional research support from Eli Lilly and Novartis. All other authors have reported that they have no relationships relevant to the contents of this article to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For a supplemental video, please see the online version of this article.
Appendix
Presurgical transthoracic echocardiogram. Parasternal long-axis view showing the thickened mitral valve leaflets with doming of the anterior mitral leaflet.
References
- 1.Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors. 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gerber M.A., Baltimore R.S., Eaton C.B., et al. Prevention of rheumatic fever and diagnosis and treatment of acute streptococcal pharyngitis. Circulation. 2009;119:1541–1551. doi: 10.1161/CIRCULATIONAHA.109.191959. [DOI] [PubMed] [Google Scholar]
- 3.Carapetis J.R., Beaton A., Cunningham M.W., et al. Acute rheumatic fever and rheumatic heart disease. Nat Rev Dis Primers. 2016;2 doi: 10.1038/nrdp.2015.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar R.K., Antunes M.J., Beaton A., et al. Contemporary diagnosis and management of rheumatic heart disease: implications for closing the gap. Circulation. 2020;142:337–357. doi: 10.1161/CIR.0000000000000921. [DOI] [PubMed] [Google Scholar]
- 5.Manyemba J., Mayosi B.M. Penicillin for secondary prevention of rheumatic fever. Cochrane Database Syst Rev. 2002;3 doi: 10.1002/14651858.CD002227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawrence J.G., Carapetis J.R., Griffiths K., Edwards K., Condon J.R. Acute rheumatic fever and rheumatic heart disease: incidence and progression in the Northern Territory of Australia, 1997 to 2010. Circulation. 2013;128(5):492–501. doi: 10.1161/CIRCULATIONAHA.113.001477. [DOI] [PubMed] [Google Scholar]
- 7.Beaton A., Okello E., Rwebembera J., et al. Secondary antibiotic prophylaxis for latent rheumatic heart disease. N Engl J Med. 2022;386:230–240. doi: 10.1056/NEJMoa2102074. [DOI] [PubMed] [Google Scholar]
- 8.National Association of Hispanic Real Estate Professionals Insights from the SHHR: multigeneration living among Latinos. March 2023. https://nahrep.org
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Presurgical transthoracic echocardiogram. Parasternal long-axis view showing the thickened mitral valve leaflets with doming of the anterior mitral leaflet.