Abstract
There is a pressing need to include older individuals in health education and uncover their specific needs. Leveraging the advantages of digitized health education, this study employed a participatory approach to engage community-dwelling older adults in co-creating a synchronous tele-education program, with dementia as the focus due to its rising prevalence and associated stigma in Singapore. Our findings demonstrate the preliminary effectiveness and feasibility of tele-education. Participants’ feedback and recommendations provided valuable insights and could guide the future development of a comprehensive tele-education program. Participants’ satisfaction with the co-design workshops also indicates the potential of involving older generations in the design process of user-centered digital health interventions in online environments. Moving forward, the study advocates collaboration among health institutes, government and social agencies, and community organizations, alongside systematic evaluation of the long-term impacts of tele-education, with the aim of improving health outcomes and reducing health inequalities among the older population.
Keywords: technology, health promotion, population aging, education, technology, older adults, telehealth, tele-education
What this paper adds
• The study highlights tele-education’s potential as an effective and feasible health education delivery to older adults.
• Older adults valued the participatory approach as a “mutual learning” opportunity, suggesting deeper involvement in co-designing and co-implementing technology-driven interventions.
• Recommendations for future tele-education programs are proposed, considering older individuals’ preferences across design, human, technological, and environmental perspectives.
Applications of study findings
• Future research could explore implementing validated knowledge assessment tools within online learning environments for more comprehensive analysis.
• Health education initiatives should prioritize tailored curricula to accommodate the diverse profiles of older learners.
• Collaboration among policymakers, health educators, social workers, caregivers, and older individuals is critical to maximize the impacts of health education.
Introduction
The global aging population is steadily increasing due to longer lifespans and declining fertility rates (World Health Organization, 2024; 2021). The proportion of individuals aged 65 years and above is projected to increase from 10% in 2022 to 16% in 2050, with the number of individuals aged over 80 years growing even faster (United Nations Department of Economic and Social Affairs, 2023). Singapore is also undergoing rapid aging, with the percentage of citizens aged 65 and above climbing from 11.1% in 2012 to 18.4% in 2022 and is expected to reach 23.8% by 2030 (National Population and Talent Division, Strategy Group et al., 2022). Additionally, the median age has risen from 39.6 years in 2012 to 42.8 years in 2022 (National Population and Talent Division, Strategy Group et al., 2022), with a noticeable increase in the proportion of citizens aged 80 and above, from 2.3% in 2012 to 3.7% in 2022 (National Population and Talent Division, Strategy Group et al., 2022). These demographic shifts have profound impacts on society, influencing various areas including the economy, living environment, and healthcare system (Prime Minister’s Office Singapore, 2023).
Aging is accompanied by gradual deterioration of physical and mental capacities and increased vulnerability to diseases (World Health Organization, 2021). Non-communicable diseases, such as cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes, are particularly prevalent among older individuals and account for 74% of all deaths globally (World Health Organization, 2022). Dementia, a range of diseases impacting cognition, memory, and daily functioning, has been acknowledged as another significant public health concern (World Health Organization, 2023). As of 2020, the global population of affected individuals surpassed 55 million, with over 10 million new diagnoses annually, translating to one case every 3.2 seconds (Alzheimer’s Disease International (ADI), n.d.). At times, the early symptoms of these health conditions may be mistaken for normal signs of aging and disregarded, as geriatrician Dr. Salzman shared, “Any changes in your physical and mental health, even small ones, can indicate the onset of these common illnesses” (Sarah Miller, 2022).
Therefore, prioritizing and improving their health has the potential to prevent and delay the onset of chronic diseases, enhance their independence and involvement in family and social activities (Chafjiri et al., 2018), and reduce the impacts on the economy and healthcare expenditures (Cylus & Al Tayara, 2021; Nozaki et al., 2017). Health promotion activities are the primary strategies that empower individuals to take control of and improve their health (World Health Organization, 1979). Health education, one of such strategies, has the potential to enhance individuals’ understanding of health and healthcare, equip them with the essential knowledge to make informed decisions about healthcare choices (Kececi & Bulduk, 2012), and control the onset and progression of diseases and disabilities (Tumosa, 2023). Despite historically overlooking the older population due to the notion of entrenched habits in this demographic (Golinowska et al., 2016), recent initiatives, notably highlighted by the World Health Organization (WHO) in the 1990s, underscore the critical role of health education in catering to the health needs of older individuals (Rana et al., 2010).
Emerging evidence has shown that limited health literacy is associated with poor health outcomes in older individuals (Chesser et al., 2016; Kim & Oh, 2020), and thus reinforces the pivotal role of health promotion and education within the healthy aging frameworks. For instance, the Healthy People 2030 framework prioritizes “promoting healthy development, healthy behaviors, and well-being across all life stages” as one of the overarching goals (Office of Disease Prevention and Health Promotion, n.d.).
Current community health education programs for older adults have raised various concerns, including outdated formats, simplistic content, and the lack of standardization and personalization (Guo & Ding, 2019). Furthermore, the challenges faced by older learners have been well-documented, such as busy schedules with medical appointments, family obligations, and social engagements (Nevada Adult Day Healthcare Centers, 2023), as well as a tendency to exhibit resistance or minimal interest in health-related information (Carter et al., 1989; Kim & Oh, 2020).
Hence, the development of effective and tailored strategies for health education program design and implementation, coupled with active engagement of the target demographic, becomes imperative. In the proposed framework for enhancing the design and implementation of health promotion and preventive interventions by Pennucci et al., co-design emerges as one of the most effective approaches for fostering active participation among laypeople, to build an alliance relationship between individuals and the healthcare system (Pennucci et al., 2022).
In literature, health education for older people has been implemented through various modes, such as lectures, seminars, and activities (Chang et al., 2017), and the integration of educational technologies like printed materials, software and video, mock-up, and telephone support (Sá et al., 2019). The use of such educational technologies is seen as a feasible and effective approach to improving care orientation (Cardoso et al., 2018) and constructing self-care knowledge and empowerment (Sá et al., 2019).
The COVID-19 pandemic has further speeded up the digitization of health education (BaylorScott & White Institute for Rehabilitation, 2019; Deldar & Froutan, 2022; He et al., 2020). Synchronous telehealth-delivered education, or tele-education, offers several strengths, for example, structured learning to ensure learners stay on track, increased real-time interaction and collaboration, and immediate feedback (ViewSonic Library, 2020). While tele-education has been adopted in medical student education (Franklin et al., 2021), health and social care professions education (Wetzlmair et al., 2022), and continuing health education programs (Bernardes et al., 2018; Ramsden et al., 2022), there is limited published evidence regarding its application in health education for older adults.
Aim and Research Questions
This study aimed to engage older adults in the co-design process of a tele-education program and investigate how this mode of health education delivery could meet their specific needs. We sought to address the following questions:
(1) What are the potential effects of tele-education on older adults’ health knowledge and awareness?
(2) What is the feasibility of tele-education for delivering health education to older adults?
(3) What are the recommendations for designing tele-education programs for older adults?
(4) How receptive are older adults to the participatory approach in an online environment?
Method
Study Design
This study employed a participatory approach in an online environment, incorporating mixed methods within the rapid prototyping. Rapid prototyping was used to facilitate the swift creation, testing, and refinement of the prototype (Kinzie et al., 2002). It also served to introduce participants to the concept of tele-education and offer them an initial experience, factoring in the fact that some older adults may not have had prior exposure to health education or telehealth. This study has been approved by the Institutional Review Board (Reference: IRB-2022-733).
Tele-Education Prototype
The prototype creation was guided by instructional design, a systematic process of creating instructional materials and learning experiences to support the learners’ acquisition of new knowledge, skills, and attitudes (Association for Talent Development & Purdue, 2024).
Topic
Singapore is facing a rising challenge of dementia due to its rapidly growing older population. As per the official statistics, approximately 10% of individuals aged 60 years or above are affected by dementia (Ministry of Health Singapore, 2022), with the majority of them residing in their communities and relying on their spouses and children as primary caregivers (Brodaty & Donkin, 2009). Some common difficulties reported by dementia caregivers included mental stress, financial burdens associated with caregiving, challenges during the COVID-19 pandemic, and feelings of longlines and rejection (National Volunteer And Philanthropy Centre, 2021). Moreover, the general public was reported to have limited knowledge and awareness of dementia, as well as discomfort when interacting with affected individuals (SMU Undergraduate Singapore, 2019). Given these challenges faced in Singapore, dementia was selected as the health topic for the prototype.
Content
The World Health Organization has identified five main themes of dementia education or health campaigns targeting the general public (World Health Organization, 2012), namely: “raising public awareness and understanding of dementia, reducing the stigma of dementia and challenging discriminatory behavior, recognizing the early signs of dementia to aid early diagnosis, living well with dementia, and the importance of a healthy lifestyle and reducing risk.” Our prototype was designed as a 45-min session in accordance with these themes and provided evidence-based information on a variety of topics related to dementia, including symptoms, complications, pathology, strategies for risk reduction, screening, and caregiving. In addition, locally relevant and available resources were shared with the participants. All materials underwent a review process by the team to ensure their credibility and suitability in the local context.
Language
Although Singapore is a multilingual society with multiple official languages and various spoken languages including dialects, the prototype was created solely in English for several reasons. First, working on a single language allowed the team to focus the resources and efforts on perfecting the prototype, as well as testing and fine-tuning the prototype more easily before extending it to other languages. Second, using a single language ensured that terminologies were standardized and consistent throughout the prototype, to avoid confusion and reduced effectiveness caused by variations in terminologies across languages.
Platform
During the COVID-19 pandemic, Zoom was widely adopted for healthcare purposes. Its various features, such as screen sharing and chat functions, allow users to interact and participate in discussions during a session. Additionally, it offers customization options like virtual backgrounds, breakout rooms, and polling, making it tailored to fit specific educational needs. Due to its accessibility, low costs, convenience, interactivity, customizability, and security, Zoom meeting was selected as the medium of the tele-education prototype. Considering the possibility that some participants may join the session on their mobile phones or lack familiarity with the platform, we used the Zoom polling feature for the knowledge assessments to minimize any inconvenience that may arise from switching to another application.
Learning Theories
Transformative learning and the “Learn, Unlearn, Relearn” were the two main adult learning theories adopted in our health education prototype creation, as older adults’ acquisition of new knowledge is affected by their accumulated knowledge and experience over time, as well as their beliefs and attitudes (Carter et al., 1989). The former theory involves critically examining one’s beliefs and assumptions as a means of personal growth (Ali Simsek, 2012); while the latter stresses the importance of continuously learning, discarding outdated or incorrect information, and regaining new knowledge (Learnlife Team, 2021). Both theories underscore the need for ongoing personal growth and development to make sense of the learners’ lives.
On account of this, a dementia knowledge assessment was planned at the outset of the session (baseline test), serving a dual purpose: to (i) evaluate participants’ baseline dementia knowledge; and (ii) enable the instructor to identify any misconceptions and thereby adjust the teaching approach accordingly. The same set of questions was posed at the end of the prototype (post-test) to determine if there had been any alteration in participants’ understanding of dementia.
Participant Recruitment
The inclusion criteria were: (1) older adults including young seniors who are aged 50 or above 1 ; (2) long-term Singapore residents dwelling in the community; (3) ability to read and converse in English; and (4) openness to using or learning to use Zoom. Participant recruitment commenced in December 2022 and employed a convenience sampling approach with multiple recruitment strategies: disseminating study information and the recruitment poster on social media platforms such as Facebook and Instagram as well as elderly chat groups, community outreach at senior centers, reaching out to previous study participants who had provided consent for future research studies, and obtaining referrals from early participants.
During participant recruitment, individuals who expressed interest in participating in the study were invited to complete an online registration form to collect their sociodemographic and socioeconomic characteristics, and their pre-existing health conditions. Those who met the eligibility criteria were then contacted via WhatsApp or text messages to receive further details of the study, schedule a co-design workshop, and provide written informed consent for study participation and video recording.
Data Collection
Data collection took place in February 2023 (Supplemental Figure 1) and all co-design workshops were conducted on Zoom and video recorded for data analysis purposes. Each session consisted of three sections: (i) a pilot test for the participants to test the feasibility and preliminary effectiveness of the pre-created tele-education prototype; (ii) Focus Group Discussion (FGD) to collect participants’ learning experience and their perceptions; and (iii) feedback to capture participants’ satisfactions and insights.
Each session accommodated a maximum of ten, with field notes documenting participants’ responses and interactions. Participants received SGD20 worth of shopping vouchers or mobile banking transfers upon successful study completion.
Outcome Measures
Multiple outcomes were collected to answer the research questions.
Effectiveness of the Prototype
The prototype’s impacts on participants’ knowledge and awareness of dementia were measured using both quantitative scores from pre-post dementia knowledge assessment and qualitative data from participants’ feedback. The knowledge assessment adopted the Dementia Knowledge Assessment Scale (DKAS), a validated tool assessing four subscales of dementia knowledge: Causes and characteristics, Communication & behavior, Care considerations, and Risks and health promotion (Annear et al., 2017). Originally a 27-item scale, DKAS was revised to a 25-item scale in 2017 (Annear et al., 2015, 2017) and has been validated and applied in various countries (Annear et al., 2017; Lee et al., 2020; Su et al., 2021). The original version is a Likert scale with five options, but the number of options was reduced to three in our study due to time constraints, cognitive load concerns for older adults, as well as possibly reduced usability of Zoom on smartphones. Participants were awarded 2 points for correct answers, 1 point for selecting “Unsure” as the only option for uncertainty, and 0 points for choosing a wrong answer, with a maximum total score of 50. The questions were reviewed before the study to ensure that they suited the local context.
Feasibility of the Prototype
The feasibility of the prototype was measured by different outcomes in this study as recommended by Bowen et al. (Bowen et al., 2009), including implementation and practicality (duration and participants’ ability to carry out the activities in the session), participants’ acceptance (satisfaction and perceived appropriateness in local setting), demand (perceived impacts), and possibility to expand, mostly through participants’ feedback. Other outcomes, such as possible areas for improvement, health information needs, and implications for practice were also gathered from participants’ feedback.
Perceptions of Tele-education
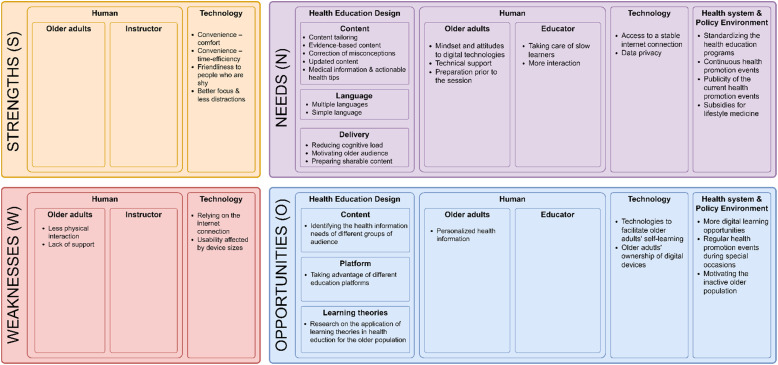
SWOT (Strengths, Weaknesses, Opportunities, Threats) analysis is a widely used strategic planning tool assessing both internal factors (strengths and weaknesses) as well as external factors (opportunities and threats) impacting organizations, plans, projects, individuals, or businesses (GÜREL, 2017). However, it often focuses on identifying problems rather than finding solutions and has a negative framing (Abdul Momin, 2023). The NOISE (Needs, Opportunities, Improvements, Strengths, and Exceptions) analysis complements the SWOT analysis by assessing current situations and future improvement strategies (Abdul Momin, 2023). In this study, we combined these tools and conducted a SNOW (Strengths, Needs, Opportunities, Weaknesses) analysis to guide the development of the moderator guide for collecting participants’ feedback using semi-structured questions (Supplemental Table 1).
Satisfaction with the Co-design Workshop
Participants’ satisfaction with the co-design workshops was assessed by a 15-item feedback form (Xu, 2019) with 11 rating items on the organization, time management, delivery, moderator, performance, and intention to participate in future research; and another four questions on participants’ experiences and their expectations.
Data Analysis
Each participant was assigned a unique identifier and all study data were deidentified before data analysis. Paired t test and Wilcoxon signed-rank test were used to evaluate the sample mean difference in the pre-post education DKAS scores. All quantitative data analyses were performed using RStudio Version 2022.12.0 + 353. Qualitative data, on the other hand, were first transcribed verbatim. We chose individual as the unit of analysis and conducted an inductive thematic analysis with line-by-line open coding while reading through all transcripts to generate the initial codes. The initial codes were then organized based on the research questions, and the generated pattern codes were used to identify themes. The team met on a regular basis to discuss the findings, aiming to enhance the validity of the analysis.
Results
Participant Characteristics and Duration of the Co-design Workshops
At thematic saturation, 32 older individuals expressed their interest in participation, among whom 25 managed to participate in one of the seven FGDs (seven individuals were unreachable). An additional session was scheduled with ten additional participants who met the same inclusion criteria and were referred by the early participants, to enrich our findings, discover new insights from an extended network, and evaluate the feasibility of delivering tele-education to larger audience groups. Ultimately, it could further validate our findings and enhance the reliability of the research. The durations of the eight co-design workshops ranged from 87.9 minutes to 195.3 minutes with a mean of 127.4 minutes.
Out of the 35 participants recruited, about two-thirds were female (24/35, 68.6%) and the majority (33/35, 94.3%) were Chinese. Their ages ranged from 53 to 82, with a mean of 66.0 (SD = 6.3). Slightly more than half (19/35, 54.3%) had an education level higher than secondary school, and half of them (18/35, 51.4%) had at least one pre-existing health condition. Table 1 summarizes the demographic characteristics of the participants, with details listed in Supplemental Table 2.
Table 1.
Demographic Characteristics of the Participants.
| Characteristics | n (%) | |
|---|---|---|
| Age (66.0 ± 6.3) | 50–54 | 1 (2.9) |
| 55–59 | 4 (11.4) | |
| 60–64 | 10 (28.5) | |
| 65–69 | 10 (28.5) | |
| 70–74 | 8 (22.9) | |
| 75–79 | 1 (2.9) | |
| 80+ | 1 (2.9) | |
| Gender | Female | 24 (68.6) |
| Male | 11 (31.4) | |
| Ethnicity | Chinese | 33 (94.3) |
| Indian | 2 (5.7) | |
| Highest education level achieved | Secondary or below | 16 (45.7) |
| Pre-university | 8 (22.9) | |
| Degree and postgraduate | 11 (31.4) | |
| Marital status | Married | 23 (65.7) |
| Single | 11 (31.4) | |
| Widowed | 1 (2.9) | |
| Living alone | No | 27 (77.1) |
| Yes | 8 (22.9) | |
| Occupation | Employed full time | 2 (5.7) |
| Employed part-time | 10 (28.5) | |
| Homemaker | 2 (5.7) | |
| Retired | 17 (48.6) | |
| Self-employed | 4 (11.5) | |
| Pre-existing health condition | None | 17 (48.6) |
| Moderate high blood pressure/hypertension | 14 (40.0) | |
| Diabetes | 7 (2.0) | |
| High cholesterol | 8 (22.9) | |
| Hyperthyroidism | 1 (2.9) | |
| Heart disease | 1 (2.9) | |
| Cancer | 1 (2.9) | |
| Fatty liver | 1 (2.9) | |
| Osteoporosis | 1 (2.9) | |
Effects of the Prototype
Dementia-related Knowledge
Misconceptions About Dementia
During the pilot test, some misconceptions of dementia were observed, for instance, “dementia cannot be avoided in older people,” “dementia is solely genetic,” “people with dementia will completely lose their ability to perform tasks,” “dementia is fatal,” and “older people with memory loss must have dementia.”
DKAS Scores
Among the 35 participants, one encountered technical failure with his smartphone and joined the session together with another participant, one was late and missed the pre-education knowledge assessment, while another one failed to submit answers for the first 2 subscales in the pre-education assessment due to Internet connection issues. Consequently, a total of 32 and 34 full responses were received for the pre-education and post-education knowledge assessments, respectively.
Table 2 summarizes the DKAS scores. At baseline, the mean total score was 34.53/50 (SD = 7.41), and the mean scores for the four subscales were 9.19/14 (SD = 2.88), 6.38/12 (SD = 2.95), 10.61/12 (SD = 1.75), and 8.33/12 (SD = 2.42). After the pilot test, significant improvements were observed in the mean scores of all four subscales [subscale 1: 10.24 (SD = 3.17), p < .05; subscale 2: 7.18 (SD = 2.93), p < .05; subscale 3: 11.65 (SD = 0.88), p < .001; and subscale 4: 9.68 (SD = 1.65), p < .001] as well as the total score [38.74 (SD = 6.14), p < .0001]. Supplemental Figures 2–4 illustrate the boxplots of the comparisons of the total score, each subscale score, and each group’s score before and after the education.
Table 2.
Summary of the DKAS Score Statistics.
| Subscale | Item | Pre-score Mean (SD) (N = 32) |
Post-score Mean (SD) (N = 34) |
Pre-education subscale Mean (SD) |
Post-education subscale Mean (SD) |
p-value |
|---|---|---|---|---|---|---|
| Causes and characteristics | 1. Most forms of dementia do not generally shorten a person’s life. | 0.66 (0.94) | 0.74 (0.96) | 9.19/14 (2.88) | 10.24/14 (3.17) | 0.049* a |
| 2. Blood vessel disease (vascular dementia) is the most common form of dementia. | 1.03 (0.90) | 1.24 (0.99) | ||||
| 3. People can recover from the most common forms of dementia. | 1.66 (0.60) | 1.79 (0.59) | ||||
| 4. Dementia is a normal part of the aging process. | 1.34 (0.90) | 1.47 (0.90) | ||||
| 5. Dementia does not result from physical changes in the brain. | 1.50 (0.80) | 1.65 (0.77) | ||||
| 6. Planning for end-of-life care is generally not necessary following a diagnosis of dementia. | 1.31 (0.97) | 1.35 (0.95) | ||||
| 7. Alzheimer’s disease is the most common form of dementia. | 1.69 (0.59) | 2.00 (0.00) | ||||
| Communication and behavior | 8. It is impossible to communicate with a person who has advanced dementia. | 0.81 (0.97) | 1.24 (0.99) | 6.38/12 (2.95) | 7.18/12 (2.93) | 0.014* b |
| 9. A person experiencing advanced dementia will not generally respond to changes in their physical environment. | 0.69 (0.93) | 0.47 (0.86) | ||||
| 10. It is important to correct a person with dementia when they are confused. | 1.38 (0.94) | 1.35 (0.95) | ||||
| 11. People experiencing advanced dementia often communicate through body language | 1.21 (0.89) | 1.24 (0.96) | ||||
| 12. Uncharacteristic behaviors in a person experiencing dementia are generally a response to unmet needs. | 1.36 (0.86) | 1.44 (0.86) | ||||
| 13. Medications are the most effective way of treating behavioral symptoms of dementia. | 0.94 (0.93) | 1.44 (0.89) | ||||
| Care considerations | 14. People experiencing dementia do not generally have problems making decisions. | 1.88 (0.48) | 2.00 (0.00) | 10.61/12 (1.75) | 11.65/12 (0.88) | 0.00076*** b |
| 15. Movement is generally affected in the later stages of dementia. | 1.76 (0.61) | 2.00 (0.00) | ||||
| 16. Difficulty eating and drinking generally occurs in the later stages of dementia. | 1.61 (0.66) | 2.00 (0.00) | ||||
| 17. People with advanced dementia may have difficulty speaking. | 1.85 (0.44) | 1.85 (0.50) | ||||
| 18. People experiencing dementia often have difficulty learning new skills. | 1.76 (0.61) | 1.94 (0.34) | ||||
| 19. Daily care for a person with advanced dementia is effective when it focuses on providing comfort. | 1.76 (0.61) | 1.85 (0.50) | ||||
| Risks and health promotion | 20. Having high blood pressure increases a person’s risk of developing dementia. | 1.24 (0.83) | 1.88 (0.48) | 8.33/12 (2.42) | 9.68/12 (1.65) | 0.00056*** b |
| 21. Maintaining a healthy lifestyle does not reduce the risk of developing the most common forms of dementia. | 1.09 (1.01) | 1.82 (0.58) | ||||
| 22. Symptoms of depression can be mistaken for symptoms of dementia. | 1.76 (0.61) | 1.97 (0.17) | ||||
| 23. The sudden onset of cognitive problems is characteristic of common forms of dementia. | 0.61 (0.83) | 0.41 (0.82) | ||||
| 24. Exercise is generally beneficial for people experiencing dementia. | 1.94 (0.35) | 1.94 (0.34) | ||||
| 25. Early diagnosis of dementia does not generally improve quality of life for people experiencing the condition. | 1.70 (0.73) | 1.65 (0.77) | ||||
| Total | 34.53 (7.41) | 38.74 (6.14) | 5.69e-05**** a |
*p ≤ .05; **p ≤ .01; ***p ≤ .001; ****p ≤ .0001.
DKAS: Dementia Knowledge Assessment Scale, SD: Standard Deviation.
aPassed Shapiro–Wilk Test (normally test), and therefore used paired t test.
bFailed Shapiro–Wilk Test (normally test), and therefore used non-parametric Wilcoxon signed-rank test.
Perceived Impacts of the Prototype
Many participants reported gaining a deeper understanding of dementia, rectifying certain misconceptions, and increasing awareness after trying this prototype. They acknowledged the prototype’s potential in fostering a more profound comprehension of individuals with dementia and caregivers’ responsibilities, enabling more effective communication with others. Moreover, all participants expressed their desire to apply acquired knowledge to motivate learning, enhance self-care practices, share information within their social network, and extend assistance to those in need. Sample quotes are summarized in Supplemental Table 3.
Feasibility of Tele-Education
Duration and Ability to Carry Out the Activities in the Session
The durations of the eight pilot-test sessions ranged from 40.3 minutes to 100.0 minutes with a mean of 70.2 minutes.
All participants joining the co-design workshops on their own smartphones or laptops (34/35) shared that they could follow the instructor and did not encounter any difficulties, except for occasional Wi-Fi instability. Sample quotes are summarized in Supplemental Table 4.
Satisfaction and Perceived Appropriateness in the Local Setting
Although the majority of the participants were new to tele-education, all of them expressed satisfaction with this mode of receiving health education and found it easy to understand and relevant to the Singapore local context. Some participants shared that their daily schedules were packed with household chores or caregiving duties, making tele-education the ideal choice for them.
In addition, participants anticipated the integration of health promotion campaigns with tele-education to enhance the impact of dementia awareness initiatives. Suggestions included organizing regular health promotion events and reaching out to less engaged older adults, incorporating free or subsidized dementia screenings into annual medical check-ups, and designing a tag for individuals with dementia to encourage public assistance and support when needed. These initiatives would serve to expand the reach of awareness efforts, target a wider group of audience, and cultivate a dementia-inclusive society. Sample quotes are summarized in Supplemental Table 5.
Demand and Possibility of Expansion
All participants recognized the significance of educating the older population about dementia, a growing health concern among Singapore’s aging population. They believed that such education could increase their awareness about dementia, facilitate early precautionary measures, and empower individuals to provide better care for their loved ones. They also expressed their desire for the prototype to evolve into a comprehensive tele-education program. Sample quotes are summarized in Supplemental Table 6.
Besides dementia, participants expressed the hope to incorporate a broader range of topics into the tele-education program. They stressed the importance of acquiring both medical knowledge and practical strategies for prevention and management. Their suggested topics are summarized in Supplemental Table 6.
Perceptions of Tele-Education—SNOW Analysis
The thematic analysis yielded 38 themes that delineated the strengths, needs, opportunities, and weaknesses (SNOW) of tele-education for the older population, encompassing various aspects such as health education design, human (older learners and instructors), technology, and environment (healthcare system and policy) (Figure 1). Sample quotes are summarized in Supplemental Table 7.
Figure 1.
SNOW (Strengths, Needs, Opportunities, Weaknesses) analysis results.
Strengths
Participants acknowledged tele-education as a convenient method for receiving health education, as it eliminated the need for travel to physical locations. Instead, they could partake in the educational sessions from the comfort of their own environment, enabling them to stay relaxed and attentive. Additionally, the tele-education platform could provide a valuable opportunity for individuals who are less socially active to interact with others without the pressure of speaking in front of a public audience.
Weaknesses
While tele-education presented several benefits, participants expressed a sense of reduced interpersonal communication and intimacy compared to in-person sessions. They also highlighted the reliance on Internet connectivity for the quality of tele-education and raised potential usability challenges posed by small device sizes. Furthermore, participants felt a lack of immediate support in the event of technical issues, particularly when they were alone.
Needs
Health Education Design
Participants stressed the importance of tailoring the health education content to the specific needs and preferences of older adults. They highlighted the need to rectify misconceptions, offer practical tips, and ensure the credibility and up-to-date nature of the information provided. Participants also acknowledged that not all health information may apply to everyone and therefore should be shared with caution. They emphasized the importance of adjusting the language to accommodate the spoken languages and literacy levels of the older audience. Strategies to minimize cognitive load and motivate older adults to embrace new information were seen as crucial. Participants also expressed the value of making educational materials sharable for future reference and with others. Additionally, some participants mentioned the benefit of involving family caregivers, including domestic workers, in the health education process.
Human
To maximize the impacts of tele-education, learners may benefit from adopting a positive mindset and attitude towards new health information and digital technologies as well as acquiring technical skills or receiving technical support. Some participants found it beneficial to prepare their questions ahead of time, enabling them to actively participate and engage in more meaningful and in-depth discussions with health educators. It was also crucial to recognize that older learners have varying levels of literacy and learning capacities, and health educators should be attentive to those who may require additional time and support. Facilitating ample opportunities for audience interaction would help ensure that all participants can effectively follow along and actively engage with the educational material.
Technology
Participants emphasized the importance of having a reliable Internet connection to maintain the quality of tele-education. They also expressed the need for better protection of their personal data in the online learning environment.
Healthy System and Policy Environment
Some participants mentioned their limited awareness of health promotion events, indicating the need for improved publicity efforts to enhance public awareness. They also emphasized the importance of organizing these events on a regular basis to achieve long-term impacts. Furthermore, participants recognized the potential confusion that may arise from distinct health information provided by different health education programs, which underscored the importance of standardizing and ensuring the consistency and credibility of health information. Moreover, some participants highlighted that financial constraints could hinder their implementation of personalized lifestyle practices, suggesting the need to lower these barriers for a smoother transition from health knowledge to practices.
Opportunities
To address these needs, participants offered several suggestions. One recommendation was to collaborate with community organizations to identify different target audience groups and delve into their specific needs before designing health education programs. Additionally, offering a hybrid format concurrently using various modes of education delivery could cater to the diverse needs of the audience. Exploring the application of adult learning theories in health education for older adults was also highlighted for further exploration.
It was also noted that blindly following general health information without consulting health professionals could pose risks. Thus, personalized health information was proposed as a promising complement to general health education programs.
Publicity of the current health promotion events could be further strengthened, for example, health promotion events on designated special occasions regularly to reinforce public awareness and engagement. Additionally, leveraging artificial intelligence algorithms like ChatGPT, could be explored to provide accessible and interactive platforms for individuals to self-access information and resources. Furthermore, strategies should be developed to address the digital divide and ensure that everyone has equal opportunities to benefit from health education initiatives.
Workshop Evaluation
Participants’ evaluation of the co-design workshops (Table 3) demonstrated their high level of acceptance. They found several aspects that interesting and valuable, including the acquisition of new knowledge, the pre- and post-assessment of dementia knowledge, active participation of the participants, engaging interactions between participants and the moderator, the moderator’s effective presentation and sharing, and the recognition of tele-education as a viable method for receiving health education. Feedback for potential improvements included the suggestion of involving more individuals in future FGDs to gather a broader range of personal experiences and ensure a manageable duration of the co-design workshops.
Table 3.
Participants' Evaluation of the Co-design Workshops.
| Items | Quartiles and Median (N = 35) | |||
|---|---|---|---|---|
| First quartile (Q1) | Third quartile (Q3) | Median | Mean | |
| 1. The workshop was very organized. | 4 | 5 | 4 | 4.4 |
| 2. Time was well managed during the workshop. | 4 | 5 | 4 | 4.3 |
| 3. The workshop was delivered clearly. | 4 | 5 | 4 | 4.3 |
| 4. The moderator was well prepared. | 4 | 5 | 5 | 4.5 |
| 5. The moderator was responsive to the questions. | 4 | 5 | 4 | 4.5 |
| 6. The moderator encouraged everyone to speak. | 4 | 5 | 4 | 4.5 |
| 7. The workshop format was appropriate for the audience. | 4 | 5 | 4 | 4.4 |
| 8. The workshop has achieved its objectives. | 4 | 5 | 4 | 4.3 |
| 9. I understand the concepts presented in the workshop. | 4 | 5 | 4 | 4.5 |
| 10. I enjoyed the workshop. | 4 | 5 | 4 | 4.4 |
| 11. I would like to participate in such workshops again in future. | 4 | 5 | 5 | 4.4 |
Discussion
Principal Findings
Since the outbreak of the COVID-19 pandemic, different local health institutes and organizations have adapted the traditional health education sessions to online platforms. Examples include virtual health workshops and exercise workshops offered by the Health Promotion Board Active Aging Programs (Health Promotion Board, 2022), CARPET skills/competencies in National Health Group (NHG Polyclinics, n.d.), and the exercises, cooking, and educational workshops by the Virtual Social Service Center of the 365 Cancer Prevention Society (365 Cancer Prevention Society, n.d.). To the best of our knowledge, there has been no published evidence regarding the design, public awareness, effectiveness, and acceptability of these programs, or the preference of older adults regarding health education topics and delivery.
To bridge this gap, our study employed a participatory approach and engaged community-dwelling older adults to pilot test the synchronous tele-education prototype and share their opinions. This approach could foster meaningful dialogue and facilitate a shared understanding of priority areas for intervention among the research team and the target population (Vallely et al., 2007). The findings of our study encouragingly demonstrated the feasibility and preliminary effectiveness of such a mode in providing dementia education and provided valuable insights into the design of future health education initiatives in both physical and virtual environments. Moreover, participants’ satisfaction with the co-design workshops further highlighted the successful implementation of the participatory approach in an online environment among older adults.
Effectiveness of Tele-Education
In this mixed-methods study, participants demonstrated significant improvement in dementia knowledge, as measured by DKAS. The insights they shared regarding the perceived impacts of the tele-education prototype on their knowledge and behavior intentions serve to triangulate and further affirm the promising effectiveness of synchronous tele-education. Consistent with our earlier interview study (Zhang et al., 2023), the findings re-emphasize the potential for technology-driven interventions in health information dissemination, behavior change promotion, and health empowerment among older adults.
It is also worth noting that “knowledge that does not change behavior is useless.” Therefore, it is crucial to supplement health education initiatives with tailored strategies or interventions to encourage active engagement and promote sustained behavior changes among the older population.
Feasibility of Tele-Education
In assessing the feasibility of the prototype, multiple outcomes were measured, and they collectively indicated that tele-education can serve as a viable method for delivering health education to older individuals. As part of the Smart Nation initiative, the Singapore government and authorities have been actively promoting positive digital habits across all age groups to build a digitally inclusive nation (Infocomm Media Development, 2024b). Efforts have been dedicated to assisting the older generation in accessing technologies at lower costs (Infocomm Media Development, 2024a) and developing technological skills (Government of Singapore, 2020; SG Digital, 2022). It is encouraging to see that more older adults are recognizing the benefits of technologies and embracing them in their health-seeking activities (Zhang et al., 2023).
Our participants acknowledged that synchronous tele-education amalgamates the advantages of various health education modes, offering learners convenient access to crucial health information, real-time interactions, and prompt feedback from peers and health educators, all without necessitating travel or additional expenses. Nonetheless, it is important to note that tele-education may not suit every individual, owing to different factors like age-related declines, limited access to technologies, poor Internet connectivity, insufficient digital literacy, privacy concerns, inadequate training or support in navigating and utilizing platforms, and potential challenges in engaging with virtual learning environments (Abuhammad, 2020). These barriers should be taken into consideration during the design process to ensure that tele-education effectively reaches the appropriate target audience and adequately addresses their specific needs and circumstances.
Involvement of Older Adults in the Co-design
In recent years, there has been a noticeable surge of interest in actively involving older adults in technology co-design processes (Taffe et al., 2018). In our study, participants expressed high acceptance and satisfaction with and a strong willingness to continue their engagement in such participatory approaches. Their feedback underscores that co-design represents a form of “mutual learning” and fosters a reciprocal knowledge exchange among designers and potential users (Fischer et al., 2021). Despite the challenges reported in the literature, including relationship and trust building, knowledge acquisition, and co-design skills (Sumner et al., 2021), our findings highlight the potential feasibility of engaging older adults in the participatory approach within an online environment, ultimately contributing to the co-development of more inclusive and equitable telehealth programs.
Recommendations for Future Health Education Design
Our findings suggest that the success of a health education program is the co-product of various factors, such as design factors (e.g., content, language, delivery, and interaction), human factors (e.g., audience’ literacy levels, health educators’ communication skills, and feedback), technological factors (e.g., access, design, and privacy), and environmental factors (e.g., social, healthy system, and policy environment). Building upon these findings, we propose a set of recommendations for refining our prototype and designing future health education programs to maximize their effectiveness and improve their inclusivity among the older population (Table 4).
Table 4.
Set of Recommendations Regarding Future Health Education Design.
| Factor | Sub-factor | Recommendations for Future Health Education Program | Application to Prototype Revisions |
|---|---|---|---|
| Health education design | Content | The educational content should be customized to address the health needs of the target audience group and suit the local context. | •Delineate different learner personas/archetypes (e.g., by literacy, health literacy, and social roles) before developing the curriculum •Develop tailored educational materials and adapt the teaching strategies accordingly |
| The content should be evidence-based and constantly updated. | N.A. | ||
| It is important to keep learners informed about the generalizability of the health information. | N.A. | ||
| Incorporating real-life examples or personal experiences can resonate empathically with older learners. | Incorporate pertinent narratives, testimonials, or encourage learners to contribute their personal experiences | ||
| Balancing medical knowledge (what and why) with actionable tips (how) is key to maximizing the practicality and effectiveness of health education. | N.A. | ||
| Introducing the interconnections between different diseases across different human body systems can provide a holistic understanding and motivate proactive involvement in disease prevention, screening, and treatment. | N.A. | ||
| Language | Making educational content available in multiple spoken languages can reach a wider audience. | •Translate the educational materials into multiple languages (e.g., Mandarin, Indian, and Malay) •Consult professional health educators on the cultural sensitivity and linguistic appropriateness of the materials |
|
| Reducing technical jargons and using simple terminologies can ease older adults’ understanding of health information. | N.A. | ||
| Delivery | Implementing strategies to reduce cognitive load, such as content chunking, eliminating unnecessary information, minimizing distractions, highlighting key information, improving content readability, and using multiple modalities, can enhance engagement. | •Replace texts on the slides with images or videos, when possible •Incorporating multi-modal teaching (videos, visuals) |
|
| Offering health education in a hybrid format (e.g., physical, synchronous tele-education, and pre-recorded videos/sharable materials) provides flexibility and reaches a broader audience group. | •Allow for hybrid health education •Make the education content sharable (e.g., record the session, and share the relevant materials after the session) |
||
| Conducting smaller group health education or health coaching sessions allows for individualized health information delivery. | Control the size of each education session, and create more learner-educator interactions | ||
| Interaction | Using two-way communication and creating more interaction opportunities could better engage and motivate older adults compared to one-way, didactic sharing by the health educator. | Create more opportunities for learner-educator interactions, and encourage learners’ active participation | |
| Human | Learner | Older learners should be motivated to accept new health information and technology use and be provided with assistance and support when necessary. | •Organize health promotion campaigns to change the mindsets of older adults toward technologies •Providing technical support for the older adults via training or preparing FAQs |
| Health educators | Health educators should closely monitor older learners’ learning progress during an education session to identify any potential confusion or difficulty, adjust pace, and provide immediate clarification or support. | N.A. | |
| Providing feedback could help learners identify any misconceptions or additional clarifications required, visualize their progress and achievements, and reinforce the important health messages. On the other hand, it can also help health educators receive constructive inputs on their performance and learners’ progress, identify potential improvements, and assess if the learning objectives have been achieved. | •Prepare formative assessments to monitor learners’ misconceptions and learning progresses •Provide timely feedback |
||
| Technology | Design | Improving the design of technologies to be more user-friendly for older adults facilitates their health education. | •Look for alternatives to Zoom platform |
| Access | Addressing the digital divide and enhancing older adults' access to technologies, from ownership to proficiency, is crucial. | N.A. | |
| Privacy | Personal information should be better protected to alleviate older people’s data privacy concerns. | N.A. | |
| Environment | Social | It would be beneficial to leverage families and social networks to promote health education initiatives and provide technical support. | •Encourage learners to participate with their family members and those in their social network |
| Health system and community | Standardizing health information across different education programs prevents confusion and the potential spread of misinformation. | N.A. | |
| Actively engaging community organizations in identifying specific needs among the target health education audience and the implementation process is of utmost importance. | N.A. | ||
| Complementing health education with other health promotion or awareness initiatives spreads the impact and creates a supportive environment for older adults. | N.A. | ||
| Continuity and regularity of health education sessions reinforce and update health information, leading to cumulative effects on older individuals' knowledge and behavior changes. | N.A. | ||
| Policy | Subsidies on lifestyle medicines can lower barriers to adopting healthy lifestyle, work in conjunction with health education efforts to facilitate the transformation of health information into sustained behavior change, and mitigate health disparities among older adults. | N.A. |
Limitations and Future Research
Our study has several limitations. Firstly, this study is exploratory, aiming to explore the feasibility of tele-education for delivering health education to older individuals. Thus, we employed multiple strategies targeting participants from diverse sociodemographic and socioeconomic backgrounds, as well as literacy and e-health literacy levels. Although the overrepresentation of participants of Chinese ethnicity and the inclusion criterion regarding owning a smart device and willingness to use or learn how to use Zoom may limit the generalizability of the findings, participants shared valuable insights beyond their personal experiences. Their sharing of observations and volunteering experiences for other older adults in the community could potentially mitigate this limitation. Future research will engage the minority groups and target the hard-to-reach, less socially active, and higher-risk subgroups within the older population to gain deeper insights into their literacy levels, health information needs, and preferences regarding health education and technology utilization, thereby designing more tailored and audience-centered education programs.
Secondly, we adjusted the DKAS scoring system for pragmatic reasons, and acknowledge that its validation fell beyond the scope of this study and was challenging given our limited sample size. Future investigations will rigorously examine how validated questionnaires can be effectively administered within the tele-education setting.
Thirdly, the use of a combination of quantitative and qualitative data allowed us to triangulate and demonstrate the preliminary effectiveness and feasibility of our education prototype; however, there was a lack of evaluation of longer-term effects. Future efforts will scale up the prototype into a comprehensive tele-education program covering different topics based on the study findings, and systematically evaluate its effectiveness, acceptability, and long-term impacts, such as participants’ knowledge retention, actual behavior changes, and improvements in health outcomes and quality of life.
Conclusion
This study embraced a participatory approach, involving community-dwelling older adults in co-designing a synchronous tele-education program. The findings demonstrate the promise of tele-education and have several implications in research and practice. Empowering older adults as “co-developers” has deepened our understanding of their preferences, needs, and challenges in health education and technology engagement. Insights and recommendations shared by participants are pivotal for refining and expanding this tele-education prototype. Future efforts will focus on crafting tailored health educational materials, minimizing cognitive load for older learners, and incorporating more personal experiences for a more accessible understanding of complex health information. Recommendations cover health education design, human, technological, and environmental aspects, aiming for more inclusive, equitable, and sustainable health education programs in both physical and online environments. Moving forward, we will prioritize collaboration with health institutes, government and social service agencies, and community organizations. Moreover, the long-term impacts of tele-education programs will be systematically evaluated to maximize effectiveness and reduce health inequalities among older individuals.
Supplemental Material
Supplemental Material for Co-Creating a Synchronous Tele-Education Program With Community-Dwelling Older Adults Using a Participatory Approach: A Mixed-Methods Study by Yichi Zhang, Wei-Peng Teo, and Yin-Leng Theng in Journal of Applied Gerontology.
Acknowledgments
We would like to thank REACH Senior Centre @ Bukit Gombak Vista for the help in disseminating the study information and participant recruitment. YZ would like to acknowledge the research scholarship from Nanyang Technological University, Singapore.
Note
We selected 50 as the age cut-off, aligning with the minimum age criteria stipulated by local health programs catering to older adults, such as the “Active Ageing Programme” (People’s, 2024) and “I am a Senior” program (Government of Singapore, n.d.).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
Ethics Statement
Ethical Approval
The study has received approval from the Institutional Review Board of Nanyang Technological University (Reference: IRB-2022-733).
ORCID iD
Yichi Zhang https://orcid.org/0000-0001-5730-9648
References
- 365 Cancer Prevention Society . (nd). Social service centres & virtual social service centre. Retrieved May 25, 2023, from https://www.365cps.org.sg/social-service-centres-and-virtual-social-service-centre/ [Google Scholar]
- Abdul Momin . (2023). 5 Alternatives to SWOT analysis tackling its limitations. PESTLE Analysis. https://pestleanalysis.com/alternatives-to-swot-analysis/ [Google Scholar]
- Abuhammad S. (2020). Barriers to distance learning during the COVID-19 outbreak: A qualitative review from parents’ perspective. Heliyon, 6(11), Article e05482. 10.1016/J.HELIYON.2020.E05482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali Simsek (2012). Transformational learning. In Encyclopedia of the sciences of learning (pp. 3341–3344): Springer. 10.1007/978-1-4419-1428-6_373 [DOI] [Google Scholar]
- Alzheimer’s Disease International (ADI) . (nd). Dementia statistics. Alzheimer’s Disease International (ADI). Retrieved March 16, 2024, from https://www.alzint.org/about/dementia-facts-figures/dementia-statistics/ [Google Scholar]
- Annear M. J., Toye C., Elliott K. E. J., McInerney F., Eccleston C., Robinson A. (2017). Dementia knowledge assessment scale (DKAS): Confirmatory factor analysis and comparative subscale scores among an international cohort. BMC Geriatrics, 17(1), 168. 10.1186/s12877-017-0552-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annear M. J., Toye C. M., Eccleston C. E., McInerney F. J., Elliott K. E. J., Tranter B. K., Hartley T., Robinson A. L. (2015). Dementia knowledge assessment scale: Development and preliminary psychometric properties. Journal of the American Geriatrics Society, 63(11), 2375–2381. 10.1111/jgs.13707 [DOI] [PubMed] [Google Scholar]
- Association for Talent Development, Purdue Online. (2024). What is instructional design? Purdue Online. Retrieved March 19, 2023, from. https://online.purdue.edu/blog/education/what-is-instructional-design
- BaylorScott & White Institute for Rehabilitation . (2019). Patient education during COVID-19. BaylorScott&White Institute for Rehabilitation. https://www.bswrehab.com/about-us/blog/patient-education-during-covid-19/ [Google Scholar]
- Bernardes A. C. F., Coimbra L. C., Serra H. O. (2018). Use of Maranhão Telehealth Program as a tool to support continuing health education. Revista Panamericana de Salud Publica/Pan American Journal of Public Health, 42, Article e134. 10.26633/RPSP.2018.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen D. J., Kreuter M., Spring B., Cofta-Woerpel L., Linnan L., Weiner D., Bakken S., Kaplan C. P., Squiers L., Fabrizio C., Fernandez M. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. 10.1016/J.AMEPRE.2009.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodaty H., Donkin M. (2009). Family caregivers of people with dementia. Dialogues in Clinical Neuroscience, 11(2), 217–228. 10.31887/DCNS.2009.11.2/HBRODATY [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardoso R. d. S. S., Sá S. P. C., Domingos A. M., Sabóia V. M., Maia T. N., Padilha J. M. F. d. O., Nogueira G. d. A. (2018). Educational technology: A facilitating instrument for the elderly care. Revista Brasileira de Enfermagem, 71(Suppl 2), 786–792. 10.1590/0034-7167-2017-0129 [DOI] [PubMed] [Google Scholar]
- Carter W. B., McKenna M., Martin M. L., Andresen E. M. (1989). Health education: Special issues for older adults. Patient Education and Counseling, 13(2), 117–131. 10.1016/0738-3991(89)90055-4 [DOI] [PubMed] [Google Scholar]
- Chafjiri R. T., Shirinkam F., Karimi H. (2018). Investigating the effect of education on health-promoting lifestyle among the elderly of Ramsar in 2017. Journal of Family Medicine and Primary Care, 7(3), 612–617. 10.4103/JFMPC.JFMPC_306_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang K. S., Tsai W. H., Tsai C. H., Yeh H. I., Chiu P. H., Chang Y. W., Chen H. Y., Tsai J. M., Lee S. C. (2017). Effects of health education programs for the elders in community care centers – evaluated by health promotion behaviors. International Journal of Gerontology, 11(2), 109–113. 10.1016/J.IJGE.2017.03.009 [DOI] [Google Scholar]
- Chesser A. K., Keene Woods N., Smothers K., Rogers N. (2016). Health literacy and older adults: A systematic review. Gerontology and Geriatric Medicine, 2, Article 233372141663049. 10.1177/2333721416630492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cylus J., Al Tayara L. (2021). Health, an ageing labour force, and the economy: Does health moderate the relationship between population age-structure and economic growth? Social Science & Medicine, 287, Article 114353. 10.1016/J.SOCSCIMED.2021.114353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deldar K., Froutan R. (2022). The process of digitalization of patient education: Speeding up during covid-19 pandemic. International Journal of Community Based Nursing and Midwifery, 10(2), 156–157. 10.30476/IJCBNM.2021.93265.1912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer B., Östlund B., Dalmer N. K., Rosales A., Peine A., Loos E., Neven L., Marshall B. (2021). Co-design as learning: The differences of learning when involving older people in digitalization in four countries. Societies, 11(2), 66. 10.3390/SOC11020066 [DOI] [Google Scholar]
- Franklin G., Martin C., Ruszaj M., Matin M., Kataria A., Hu J., Brickman A., Elkin P. L. (2021). How the COVID-19 pandemic impacted medical education during the last year of medical school: A class survey. Life, 11(4), 294. 10.3390/LIFE11040294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golinowska S., Groot W., Baji P., Pavlova M. (2016). Health promotion targeting older people. BMC Health Services Research, 16(Suppl 5), 345. 10.1186/S12913-016-1514-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Singapore . (2020). Digital training for seniors. Government of Singapore. https://www.gov.sg/article/digital-training-for-seniors [Google Scholar]
- Government of Singapore . (nd). I am a senior. Government of Singapore. Retrieved June 23, 2023, from https://www.gov.sg/article/i-am-a-senior [Google Scholar]
- Guo Y., Ding W. (2019). Study on the persuasive design method of health education for the elderly adults. Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics), 11592 LNCS, 22–33. 10.1007/978-3-030-22012-9_2 [DOI] [Google Scholar]
- Gürel E. (2017). SWOT analysis: A theoretical review. The Journal of International Social Research, 10(51), 994–1006. 10.17719/JISR.2017.1832 [DOI] [Google Scholar]
- He X., Shelden D., Kraftson A., Else T., Auchus R. J. (2020). A virtual teaching clinic for virtual care during the COVID-19 pandemic. Clinical Diabetes and Endocrinology, 6(1), 25. 10.1186/S40842-020-00108-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Promotion Board . (2022). Pulling together pushing ahead - health promotion board annual report 2021/2022. In Health promotion board. https://hpb.gov.sg/docs/default-source/annual-reports/hpb_annual_report_2021-2022.pdf?sfvrsn=9ebc8734_2 [Google Scholar]
- Infocomm Media Development Authority. (2024. a). Digital for life movement. Infocomm Media Development Authority . Retrieved May 27, 2023, from https://www.imda.gov.sg/digitalforlife/About-Us
- Infocomm Media Development Authority. (2024. b). Mobile plans for seniors. SG: Digital. Retrieved May 28, 2023, from https://www.imda.gov.sg/en/seniorsgodigital/Go-Digital-Mobile-Plans [Google Scholar]
- Kececi A., Bulduk S. (2012). Health education for the elderly. Geriatrics, 85(11), 16–18. IntechOpen. 10.5772/33472 [DOI] [Google Scholar]
- Kim M. Y., Oh S. (2020). Nurses’ perspectives on health education and health literacy of older patients. International Journal of Environmental Research and Public Health, 17(18), 6455. 10.3390/IJERPH17186455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinzie M. B., Cohn W. F., Julian M. F., Knaus W. A. (2002). A user-centered model for web site design: Needs assessment, user interface design, and rapid prototyping. Journal of the American Medical Informatics Association: JAMIA, 9(4), 320–330. 10.1197/JAMIA.M0822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Learnlife Team . (2021). Learn, Unlearn, Relearn. Retrieved March 26, 2023, from https://blog.learnlife.com/learn-unlearn-relearn
- Lee J. M. G., Chan C. Q. H., Low W. C., Lee K. H., Low L. L. (2020). Health-seeking behaviour of the elderly living alone in an urbanised low-income community in Singapore. Singapore Medical Journal, 61(5), 260–265. 10.11622/smedj.2019104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health Singapore . (2022). Speech by associate professor Kenneth Mak, Director of medical services, Ministry of health and member, Lee Kong chian school of medicine governing board, at the launch of the dementia research centre Singapore, 25 April 2022, 10.30am. Ministry of Health. https://www.moh.gov.sg/news-highlights/details/speech-by-associate-professor-kenneth-mak-director-of-medical-services-ministry-of-health-and-member-lee-kong-chian-school-of-medicine-governing-board-at-the-launch-of-the-dementia-research-centre-singapore-25-april-2022-10.30am [Google Scholar]
- National Population and Talent Division, Strategy Group, P. M. O., Singapore Department of Statistics, Ministry of Home Affairs, Immigration & Checkpoints Authority, & Ministry of Manpower . (2022). Population in brief 2022. https://www.strategygroup.gov.sg/files/media-centre/publications/Population-in-Brief-2022.pdf
- National Volunteer And Philanthropy Centre . (2021). Towards a dementia-inclusive Singapore. [Google Scholar]
- Nevada Adult Day Healthcare Centers . (2023, September 17). The importance of health education for seniors. Nevada Adult Day Healthcare Centers. https://www.nevadaadultdaycare.com/the-importance-of-health-education-for-seniors/#:∼:text=Seniors_educated_about_risk_factors,as_diabetes_and_heart_disease [Google Scholar]
- NHG Polyclinics . (nd). Health literacy rolling out the CARPET to engage patients(Zoom). Retrieved May 25, 2023, from https://www.nhgp.com.sg/patients-resources/pca/Pages/Courses/Health-Literacy---Rolling-Out-the-CARPET-to-Engage-Patients(Zoom).aspx
- Nozaki M., Kashiwase K., Saito I. (2017). Health spending in Japan: Macro-fiscal implications and reform options. The Journal of the Economics of Ageing, 9, 156–171. 10.1016/J.JEOA.2016.11.002 [DOI] [Google Scholar]
- Office of Disease Prevention and Health Promotion . (nd). Healthy people 2030 framework. U.S. Department of Health and Human Services. Retrieved October 31, 2023, from https://health.gov/healthypeople/about/healthy-people-2030-framework [Google Scholar]
- Pennucci F., De Rosis S., Murante A. M., Nuti S. (2022). Behavioural and social sciences to enhance the efficacy of health promotion interventions: Redesigning the role of professionals and people. Behavioural Public Policy, 6(1), 13–33. 10.1017/BPP.2019.19 [DOI] [Google Scholar]
- People’s Association. (2024). Active ageing. People’s Association. Retrieved June 23, 2023, from https://www.pa.gov.sg/our-programmes/active-ageing/
- Prime Minister’s Office Singapore . (2023). PM lee Hsien Loong at the ‘Singapore ageing: Issues and challenges ahead’ Book launch. Prime Minister’s Office Singapore. https://www.pmo.gov.sg/Newsroom/PM-Lee-Hsien-Loong-at-the-Singapore-Ageing-Issues-and-Challenges-Ahead-Book-Launch. [Google Scholar]
- Ramsden R., Colbran R., Christopher E., Edwards M. (2022). The role of digital technology in providing education, training, continuing professional development and support to the rural health workforce. Health Education, 122(2), 126–149. 10.1108/he-11-2020-0109 [DOI] [Google Scholar]
- Rana A. K. M. M., Kabir Z. N., Lundborg C. S., Wahlin Å. (2010). Health education improves both arthritis-related illness and self-rated health: An intervention study among older people in rural Bangladesh. Public Health, 124(12), 705–712. 10.1016/j.puhe.2010.07.005 [DOI] [PubMed] [Google Scholar]
- Sá G. G. d. M., Silva F. L., Santos A. M. R. D., Nolêto J. D. S., Gouveia M. T. d. O., Nogueira L. T. (2019). Technologies that promote health education for the community elderly: Integrative review. Revista Latino-Americana de Enfermagem, 27, Article e3186. 10.1590/1518-8345.3171.3186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarah Miller (2022). Signs of aging you shouldn’t ignore. Jefferson Health. https://www.jeffersonhealth.org/your-health/living-well/signs-of-aging-you-shouldnt-ignore [Google Scholar]
- SG Digital . (2022). Infocomm media development authority. https://www.imda.gov.sg/SeniorsGoDigital
- SMU Undergraduate Singapore . (2019). 3 in 4 persons with dementia feel ashamed and rejected, Singapore’s first national survey on dementia finds. SMU Office of Admission & Financial Assistance. https://admissions.smu.edu.sg/our-community/news/3-4-persons-dementia-feel-ashamed-and-rejected-singapores-first-national-survey [Google Scholar]
- Su H. F., Koo M., Lee W. L., Sung H. C., Lee R. P., Liu W. I. (2021). A dementia care training using mobile e-learning with mentoring support for home care workers: A controlled study. BMC Geriatrics, 21(1), 126. 10.1186/S12877-021-02075-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumner J., Chong L. S., Bundele A., Wei Lim Y. (2021). Co-designing technology for aging in place: A systematic review. The Gerontologist, 61(7), e395–e409. 10.1093/GERONT/GNAA064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taffe S., Pedell S., Wilkinson A. (2018). Reimagining ageing: Insights from teaching co-design methods with designers, seniors and industry partners. Design for Health, 2(1), 107–116. 10.1080/24735132.2018.1450945 [DOI] [Google Scholar]
- Tumosa N. (2023). Using the age-friendly health systems framework to track wellness and health promotion priorities of older adults in the global community. International Journal of Environmental Research and Public Health, 20(5), 4617. 10.3390/IJERPH20054617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Department of Economic and Social Affairs . (2023). UNDESA World social report 2023: Leaving No one behind in an ageing World. https://desapublications.un.org/file/1087/download [Google Scholar]
- Vallely A., Shagi C., Kasindi S., Desmond N., Lees S., Chiduo B., Hayes R., Allen C., Ross D. (2007). The benefits of participatory methodologies to develop effective community dialogue in the context of a microbicide trial feasibility study in Mwanza, Tanzania. BMC Public Health, 7(1), 133. 10.1186/1471-2458-7-133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ViewSonic Library . (2020). The pros and cons of synchronous distance learning. ViewSonic Library. https://www.viewsonic.com/library/education/the-pros-and-cons-of-synchronous-distance-learning/ [Google Scholar]
- Wetzlmair L. C., O’Carroll V., O’Malley A. S., Murray S. (2022). Teleconsultation in health and social care professions education: A systematic review. The Clinical Teacher, 19(5), Article e13519. 10.1111/TCT.13519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (1979). Health promotion. https://www.who.int/teams/health-promotion/enhanced-wellbeing/seventh-global-conference/community-empowerment [Google Scholar]
- World Health Organization . (2012). Dementia: A public health priority. https://iris.who.int/handle/10665/75263 [Google Scholar]
- World Health Organization . (2021). Ageing and health. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health [Google Scholar]
- World Health Organization . (2022). Noncommunicable diseases. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases [Google Scholar]
- World Health Organization . (2023). Dementia. https://www.who.int/news-room/fact-sheets/detail/dementia [Google Scholar]
- World Health Organization . (2024). Ageing. Retrieved February 4, 2023, from https://www.who.int/health-topics/ageing#tab=tab_1
- Xu X. (2019). Smartphone apps for caregivers of children with atopic dermatitis : User profile, app scope and co-design. Nanyang Technological University. 10.32657/10356/137738 [DOI] [Google Scholar]
- Zhang Y., Lee E. W. J., Teo W. P. (2023). Health-seeking behavior and its associated technology use: Interview study among community-dwelling older adults. JMIR Aging, 6, Article e43709. 10.2196/43709 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Co-Creating a Synchronous Tele-Education Program With Community-Dwelling Older Adults Using a Participatory Approach: A Mixed-Methods Study by Yichi Zhang, Wei-Peng Teo, and Yin-Leng Theng in Journal of Applied Gerontology.