Abstract
Background
Assessing maternal health care utilisation is imperative for the health of both mother and her child. Maternal education is an important determinant in subsequent maternal health care usage, according to research. There is a dearth of research on the causal relationship between maternal education and maternal health services as well as examining the performance of different propensity score methods for estimating absolute effects. Therefore, this study aims to estimate the effect of maternal education on usage of maternal health services minimising the confounding effect and to compare different propensity score approaches to estimate absolute effects of maternal education on usage of maternal health services.
Methods
We used data from a cross-sectional study conducted by icddr,b in Bangladesh. A total of 1300 recently delivered mothers were included in this study. We used different propensity score (PS) methods to estimate the causal effect of maternal education on receiving maternal health services, including PS matching, PS weighting, covariate adjustment using PS, as well as used modified log-Poisson regression with and without multiple covariates.
Results
The study revealed highly imbalanced possible confounding factors for mother's educational level, which might lead to erroneous estimates. All methods indicated a significant effect of higher maternal education, whether measured as a continuous scale or a binary variable (secondary or higher vs. below secondary) on maternal health services, significantly increased the likelihood of receiving four or more ANC, delivered at facility, PNC within 42 days and receiving all maternal health services compared to the mothers with lower level of education. The PS weighting provided precise estimates with a low range of confidence interval.
Conclusions
The results provided important insights on how well these techniques worked to reduce effect of confounding variables and achieve precise estimates. Propensity score weighting method performed better in terms of providing more precise estimates with a narrower range of confidence intervals, indicating that this method may be a reliable approach for estimating the causal effect of maternal education on maternal health service utilisation. However, careful consideration should be given to selecting the most appropriate method.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13690-024-01423-0.
Keywords: Maternal education, Health services, Observational study, Causality, Confounding, Comparison, Bangladesh
| Text box 1. Contributions to the literature |
|---|
| • This study uses advanced propensity score methods to rigorously estimate the causal effect of maternal education on maternal health service utilisation in Bangladesh, addressing a gap in existing literature. |
| • By comparing multiple propensity score methods and covariate adjustment methods, the research provides insights into the most effective techniques for minimising confounding in observational studies. |
| • The findings emphasise the critical role of maternal education in improving health outcomes, informing policymakers to target educational initiatives for women, especially in hard-to-reach areas of Bangladesh, to enhance maternal health service utilisation. |
Introduction
Globally, approximately 810 women died every day from avoidable causes associated with pregnancy and delivery in 2017 [1]. Bangladesh maternal mortality and Health Care Survey (BMMS) 2016 reported that maternal mortality ratio (MMR) is 196 per 100,000 live births [2]. Maternal deaths are caused by a variety of factors that vary by location. Maternal mortality is high as a result of low levels of maternal health care seeking behavior, particularly in developing countries [3]. Maternal health has become a global priority since maternal health care services can save the lives of millions of women of reproductive age [3]. It refers to the mother’s health throughout her pregnancy, childbirth, and postpartum period. Maternal health care services are antenatal care (ANC), delivery care and postnatal care (PNC) services. However, maternal health care utilisation among women is low [4]. For maternal survival to improve, women’s use of health services during pregnancy, childbirth, and early childhood must increase [5].
Bangladesh Demographic and Health Survey (BDHS) 2017-18 which includes estimates for the three years prior to the survey, documented that about 47%, 49%, and 52% of women who had a live birth had four or more ANC visits throughout their pregnancy, delivered at a health facility, and had postnatal care from a medically qualified provider within two days of delivery, respectively [4]. On the other hand, the most recent Sustainable Development Goals (SDGs) aimed to reduce MMR to 70 per 100,000 live births worldwide by 2030 [6].
Evidence from the previous study indicates that maternal education is a significant predictor of health care utilisation, even when controlled for the household’s socioeconomic status [7, 8]. However, these findings are based on different observational studies. These studies include those conducted in Latin America [9, 10], Africa [11–14], and Asia [15–18]. A randomised controlled trial (RCT) would ensure whether these associations are causal [19]. However, due to the complexity of such a design, observational studies are common in practice, where the researcher has no control over the background characteristics or the random allocation of treatments [20]. Therefore, using observational studies to assess the causal treatment effect is not feasible unless confounding factors are controlled, at least to a certain extent. Pan et al. [21] highlighted that propensity score methods are widely recognised and effective statistical tools for reducing selection bias in observational data, thereby enhancing the validity of causal inferences drawn from such studies. A study applied propensity score method in a cross-sectional study conducted by Sekine et al. [22] to evaluate causal effect of child marriage on unmet needs for modern contraception, and unintended pregnancy.
Propensity score (PS) is a very practical and widely used tool, was first proposed by Rosenbaum and Rubin [23–25] has been used for strengthening causal effect estimates using observational data by minimising the confounding that occurs frequently in observational studies. There are several approaches that utilise the PS for minimising confounding: matching on the PS, inverse probability of treatment weighting using the PS, covariate adjustment using the PS and stratification [23]. When the outcome is binary, the treatment’s effect can be expressed using relative measures of effect (the odds ratio and the relative risk). Moreover, maternal mortality varies considerably throughout Bangladesh, with hard-to-reach places having high rates [26]. There is a dearth of research on the causal association between maternal education and maternal health services in these areas as well as examining the performance of different propensity score methods for estimating causal effect. There is a lack of clear guidance on how to make a sensible choice between the various PS methods and conventional covariate adjustment for this type of database. A study documented that while PS methods have theoretical advantages over conventional covariate adjustment, their relative performance in real-world scenarios is poorly characterised [27]. The authors compared different PS methods and traditional covariate adjustment based on precision (standard error) using four large-scale cardiovascular observational studies [27]. Therefore, this study describes and applies the PS methods to estimate the effect of maternal education on maternal health services using observational data with mothers from hard-to-reach areas in Bangladesh and compares the results from different approaches for estimating the causal effect. It is beneficial to conduct this study as there is no study that estimates the causal relationship between maternal education and maternal health services using appropriate methods i.e., propensity score methods in case of observational study.
Methods
Study design and setting
We used data from a cross-sectional study conducted by icddr,b from October – November 2019 in Bangladesh. The study was conducted in 13 sub-districts located adjacent to 12 different hard-to-reach coastal areas of Bangladesh (Additional file 1: Appendix 1).
Study population, sampling technique and sample size
The study included mothers who delivered six months prior to the survey. The survey’s inclusion criteria were recently delivered mothers with a child aged 0 to 6 months. A simple cluster sampling procedure was implemented to select the mothers. A total of 1300 recently delivered mothers were finally interviewed.
Data collection
The data was collected through a face-to-face interview with the help of structured questionnaires. The questionnaire consisted of socio-demographic characteristics, ANC history, PNC history, delivery history. It specifically asked the information on the number of ANC visits, PNC visits, and the place of delivery. A team of field research managers and six female data collectors were trained in research ethics and questionnaire administration. Face to face interviews were conducted to collect the data.
Outcome variables
This study employed four outcome variables: receiving four or more ANC, facility-based delivery, PNC within 42 days, and receiving all these three above-mentioned maternal health services. These four variables were considered being binary variables in conducting the analysis. The first outcome variable, four or more ANC visits was recorded as a 1 for mothers who had four or more ANC visits, whereas those who had less than 4 visits were coded as 0. The place of the delivery is indicated by the second outcome variable, facility-based delivery. Respondents were asked about whether the delivery was at home or health facilities, including medical college hospital, district hospital, upazilla health complex, family welfare center, NGO clinic, private medical college hospital/clinic. The place of delivery had been grouped into two categories, home and facility-based delivery and coded as 0 for home delivery and 1 for facility-based delivery. A response to the third outcome variable, PNC within 42 days, was recorded as 1 if the respondents received PNC within 42 days, otherwise, it was coded as 0. The fourth outcome variable receiving all maternal health services (four or more ANC, facility-based delivery and PNC within 42 days) coded as 1 if the respondents received all above-mentioned maternal health services otherwise coded as 0.
Exposure
In this study, we considered maternal educational level as the exposure, analysing it both as a continuous variable and as a binary categorised scale. The education system in Bangladesh has three levels: primary, secondary and higher education [28]. Aside from that, as indicated by the National Education Policy (2010), the primary education level has been extended to the eighth grade [29]. This study categorised the mother’s education level into two groups. An education level with > 8 was used to classify the individual as exposed to secondary or higher education level, coded as 1, otherwise introduced as having below the secondary level of education, coded as 0.
Covariates
Several socioeconomic and demographic characteristics were considered as potential covariates in this study based on the literature review and the design of the study. These included religion (Islam and Others), husband education (> 8 and < = 8), distance to health centre in km (0–1, 2–3, and 4 or more), age at marriage in years (less than 18, 18 or more), pregnancy number (1, 2, 3, and 4 or more) and wealth quintile (poorest, poorer, middle, richer and richest). Wealth quintile was calculated based on ownership of household goods (such as housing materials, type of latrines, availability of electricity, and ownership of radio and/or television, etc.) using the principal component analysis (PCA) method.
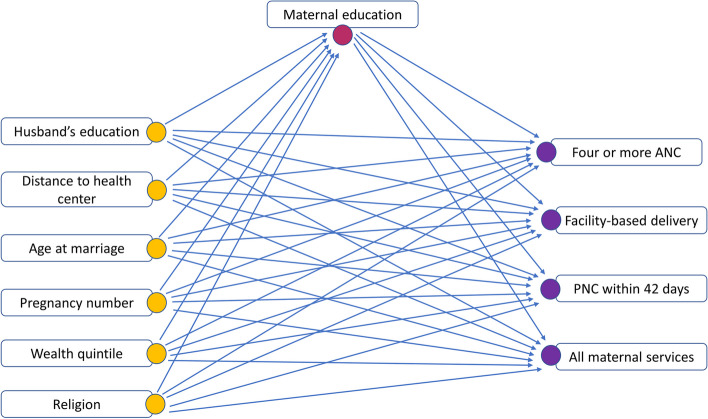
Figure 1 presents the relationships between the variables to illustrate the hypothesised causal relationships between maternal education and the utilisation of maternal health services. We identified maternal education as exposure and utilisation of maternal health services as outcome variables, and rest of the variables as covariates as we aimed to isolate the total effect of maternal education on receiving maternal health services without any decomposition, by adjusting for all measured covariates.
Fig. 1.
Causal diagram indicating relationship among covariates, maternal education and the utilisation of maternal health services
Statistical analysis
We used the statistical software package Stata 14 [30] and R 4.3.3 [31] to perform the analysis. Descriptive statistics, including frequency and percentage were used to illustrate the distribution of the mothers receiving maternal health services across a set of socioeconomic and demographic characteristics. To show the distribution of maternal education within the same set of characteristics, we reported frequency and percentage for categorised maternal education, and mean and standard deviation (SD) for continuous scale of maternal education. The p-value from the chi-square test in case of categorical variables and two sample t-test (covariates with two categories) or ANOVA (covariates with more than two categories) for continuous variables were reported to show the association or difference, respectively. We used the propensity score (PS) methods to reduce the confounding effect and assess the causal effect of exposure considering both binary and continuous exposure to investigate whether the effects of maternal education on receiving maternal health services (ANC, facility-based delivery and PNC) exists. We fitted modified log-Poisson regression models employing generalised estimating equations (GEE) framework to account for clustered data obtained from 13 sub-districts for our four binary outcome variables. The modified log-Poisson approach is generally preferred to estimate risk ratio (RR) in case of binary outcome variables [32]. In the context of GEE to analyse clustered outcome data, we have used an exchangeable working correlation matrix. It is natural to use such a working correlation matrix when the outcome data are measured at a single point in time and the clustering arises through some natural grouping of individuals (e.g., in different areas) [32]. We reported crude RR, adjusted RR, RR after incorporating PS and their corresponding 95% confidence interval (CI) from the modified log-Poisson regression models under GEE approach. A study conducted by Elze et al. (2017) using four observational cardiovascular studies, reported standard error (SE) on the effect (i.e., log hazrd ratio) scale, and compared which method provides precise estimates based on SE. We compared the commonly used PS methods (matching, weighting, covariate adjustment), along with unadjusted and multivariate adjusted method in terms of CI range. We considered the usual sandwich variance estimator when employing weighting approach. Absolute standardised mean differences (SMDs) before and after incorporating PS were used to assess the balance in covariates. For binary variable, SMDs are calculated as difference between two sample percentage derived from exposed and unexposed groups divided by the pooled standard deviation, , where and are the weighted prevalence of covariate j in exposed and unexposed group. Absolute SMDs values of less than 0.1 are considered negligible [33].
Propensity score methods for binary exposure
Propensity score
The probability of receiving a treatment conditional on a set of observed covariates is known as the propensity score [23]. It can be defined as, ; , where is the treatment indicator (exposure: maternal education, taking 1 if mothers exposed to secondary or higher level of education), (religion, husband education, distance to health centre, age at marriage, pregnancy number and wealth quintile) are the given covariates and is the propensity scores (PS) [23]. The propensity scores () were estimated using modified log-Poisson under GEE approach, where maternal education status as the dependent variable and all other given covariates serving as covariates in the model.
PS matching
PS matching is the process of producing matched sets of exposed and unexposed subjects who have a propensity score that is similar in value to one another [34]. Pair matching (one-to-one matching) is the most common application of PS matching [33]. Only one untreated subject (below the secondary level of education) is matched to one treated subject (exposed to secondary or higher education level) who have similar estimated PS value to produce matching pairs in pair matching. As a result, this method may not utilise data from all participants. This matching can be improved by persisting that pairs cannot differ by more than a fixed value which is called caliper. We considered a caliper of width equal to 0.2 of the standard deviation of the logit of the propensity score as this caliper width has been found to perform well in a wide variety of settings [35]. We also considered two-to-one matching in our analysis to have a larger sample in PS matching analysis, where two untreated subjects are matched to one treated subject. PS matching provides an estimation of the average treatment effect among the treated (ATT) parameter [21], focusing on the mothers who received secondary or higher education.
PS weighting
This method utilise data from all participants. There are various types of weighting methods, including inverse probability of treatment weighting (IPTW), standardised mortality ratio weighted (SMRW) and stabilised weighting (SW) method. This present study samples are weighted using commonly used inverse probability of treatment (exposed to secondary or higher education level or not) weighting [33, 36] to ensure that they are representative of specific populations [37]. The IPTW that documents estimation of the average treatment effect (ATE) parameter can be defined as, . An alternate weight that documents estimation of the ATT can be defined as, (Z is the indicator of maternal education status and is the estimated propensity score) [34]. These weights are then incorporated into the outcome model. Marginal computations was conducted to determine the treatment effect (maternal education) on the outcome (usage of maternal health services) [38].
PS covariate adjustment
This method utilise data from all participants. In the covariate adjustment approach, an indicator variable denoting exposure condition (exposed to secondary or higher education level or not) and the estimated PS is used to model the outcome variable (usage of maternal health services) [33]. This approach provides us with the estimation of ATE parameter [21].
Generalised propensity score methods for continuous exposure
Austin et al. (2019) [39] considers to designate the conditional density of the continuous exposure given the observed baseline covariates, using the terms [40]. In our case, considered T as the continuous exposure, where is the generalised propensity score. It is suggested that one may set out that, the continuous exposure T given covariate X, is normally distributed with mean and variance [41]. Thus, we estimated by the normal density . This is a two-step process where a regression model is first fitted to the data, and in the second step, the value of the conditional density function is determined at the value of quantitative exposure. To estimate the GPS, we fitted linear model under GEE approach where continuous maternal education is the dependent variable and baseline covariates worked as covariate in the model. However, in the context of a binary exposure, matching is a well-established approach in causal inference. Though, in the context of a continuous treatment or exposure, matching is not [42].
GPS weighting
A stabilising factor is considered in practice in GPS to discard the large weights [43]. We derived weights from the GPS and that is defined as [39, 44, 45], where the numerator is included to make stable the weights, final estimated stabilised IPW. A reasonable choice for W has been suggested as an estimate of the marginal density function of T [45]. This density function was determined by computing the mean and the variance of the continuous exposure in the overall sample [39], . These weights then were applied in a weighted outcome regression in order to estimate a causal effect. This approach provides the ATE estimation parameter [41].
GPS covariate adjustment
To perform the covariate adjustment using the GPS, the outcome is regressed on the quantitative exposure and the estimated GPS [40]. This approach yields the estimated parameter for the average treatment effect (ATE) [41].
Simple and multiple regressions
For both cases (binary exposure and continuous exposure), simple and multiple modified log-Poisson regressions within GEE framework were used to estimate the effect of maternal education on maternal health services. Simple model that is unadjusted method estimates the crude association between maternal education and the utilisation of maternal health services without controlling for confounders. Multiple adjusted method performs regression model adjusting for potential confounders, shared adjusted estimate of association.
Results
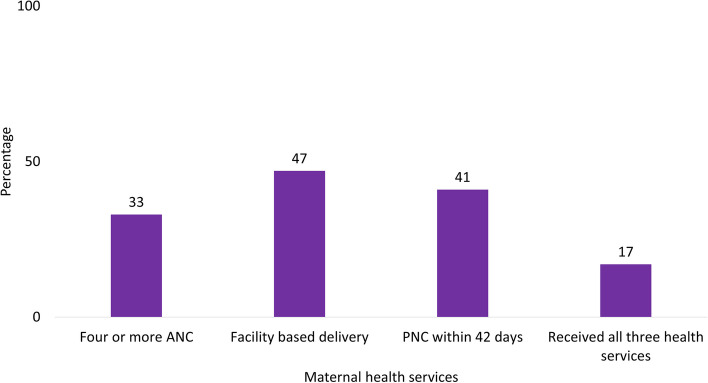
Around 33%, 47%, 41%, and 17% of mothers received four or more ANC, facility-based delivery, PNC within 42 days, and all three maternal health services, respectively (Fig. 2).
Fig. 2.
Percentage of mothers receiving maternal health services
Maternal education, wealth index, religion, husband education, and pregnancy number were associated with attending maternal health services (four or more ANC, facility-based delivery, PNC within 42 days, and receiving all health services) (Table 1). Around 49%, 64%, 58%, and 31% of the mothers with secondary or higher levels of education attended four or more ANC, facility-based delivery, PNC within 42 days, and received all health services, respectively. About 28% of the mothers from the richest group received all health services as compared to about 12% of the mothers from the poorest group. A small proportion of mothers (11%) received all maternal health services whose husband’s education was below secondary level. Considering the distance to the health care centres, 38% of the mothers attended four or more ANC and about half of the mothers had facility-based delivery as well as PNC within 42 days when the distance was between 0 and 1 km. Around 22% of the mothers whose age was 18 or more at marriage received all health services as compared to around 14% of the mothers whose age was below 18 at marriage. About 20% of the mothers with their first pregnancy received all health services as compared to about 12% of the mothers with four or more pregnancies.
Table 1.
Association between the use of maternal health services and each level of maternal education, as well as each level of covariates
| Background characteristics | N | Maternal health services | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Four or more ANC | Facility based delivery | PNC within 42 days | Received all health services | ||||||
| n (%) | P-value | n (%) | P-value | n (%) | P-value | n (%) | P-value | ||
| Maternal education | |||||||||
| <=8 | 924 | 244 (26.4) | < 0.001 | 378 (40.9) | < 0.001 | 320 (34.6) | < 0.001 | 101 (10.9) | < 0.001 |
| > 8 | 376 | 185 (49.2) | 239 (63.6) | 216 (57.5) | 116 (30.8) | ||||
| Wealth Index | |||||||||
| Poorest | 260 | 80 (30.8) | 0.001 | 88 (33.9) | < 0.001 | 96 (36.9) | < 0.001 | 32 (12.3) | < 0.001 |
| Poorer | 261 | 80 (30.7) | 111 (42.5) | 99 (37.9) | 38 (14.6) | ||||
| Middle | 259 | 71 (27.4) | 117 (45.2) | 99 (38.2) | 33 (12.7) | ||||
| Richer | 260 | 84 (32.3) | 132 (50.8) | 95 (36.5) | 40 (15.4) | ||||
| Richest | 259 | 113 (43.6) | 168 (64.9) | 146 (56.4) | 73 (28.2) | ||||
| Religion | |||||||||
| Islam | 1206 | 388 (32.2) | 0.023 | 557 (46.2) | 0.001 | 476 (39.5) | < 0.001 | 189 (15.7) | < 0.001 |
| Others | 94 | 41 (43.6) | 60 (63.8) | 60 (63.8) | 28 (29.8) | ||||
| Husband education | |||||||||
| <=8 | 963 | 249 (25.9) | < 0.001 | 397 (41.2) | < 0.001 | 339 (35.2) | < 0.001 | 103 (10.7) | < 0.001 |
| > 8 | 337 | 180 (53.4) | 220 (65.3) | 197 (58.5) | 114 (33.8) | ||||
| Distance to health centre | |||||||||
| 0–1 km | 373 | 140 (37.5) | 0.086 | 186 (49.9) | 0.242 | 167 (44.8) | 0.177 | 72 (19.3) | 0.276 |
| 2–3 km | 476 | 150 (31.5) | 231 (48.5) | 196 (41.2) | 75 (15.8) | ||||
| 4 or more | 451 | 139 (30.8) | 200 (44.4) | 173 (38.4) | 70 (15.5) | ||||
| Age at marriage | |||||||||
| Less than 18 | 842 | 258 (30.6) | 0.014 | 386 (45.8) | 0.113 | 331 (39.3) | 0.057 | 117 (13.9) | < 0.001 |
| 18 or more | 458 | 171 (37.3) | 231 (50.4) | 205 (44.8) | 100 (21.8) | ||||
| Pregnancy no. | |||||||||
| 1 | 433 | 162 (37.4) | 0.002 | 236 (54.5) | < 0.001 | 202 (46.7) | 0.003 | 88 (20.3) | 0.043 |
| 2 | 363 | 132 (36.4) | 177 (48.8) | 157 (43.3) | 60 (16.5) | ||||
| 3 | 258 | 74 (28.7) | 108 (41.9) | 92 (35.7) | 39 (15.1) | ||||
| 4 or more | 246 | 61 (24.8) | 96 (39.0) | 85 (34.6) | 30 (12.2) | ||||
Covariates: (wealth index, religion, husband education, distance to health centre, age at marriage and pregnancy number)
Maternal education was significantly associated with various socioeconomic and demographic characteristics including wealth index, religion, husband education, age at marriage and pregnancy number (Table 2). We considered both binary and continuous scale of maternal education. In the poorest group, 24% of mothers had secondary or higher education, while in the richest group, this figure was 41%. Among mothers practicing Islam, 27% had attained secondary education or higher, while among mothers of other religions, this percentage was 51%. For mothers whose husbands had an education level of 8 years or less, 16% had secondary or higher education, compared to 66% when husbands had more than 8 years of education. Among mothers married at less than 18 years of age, average grade level is close to 6, in contrast to, for those married at 18 years or older, it is close to 8th grade. For mothers with their first pregnancy, 43% had secondary or higher education, compared to 9% for those with four or more pregnancies.
Table 2.
Association between maternal education (considering as both categorical and continuous scale) and baseline covariates
| Characteristics/covariates | Maternal education | ||||
|---|---|---|---|---|---|
| Categorical exposure | Continuous exposure | ||||
| Below secondary ( < = 8) | Secondary or above (> 8) | Education level | |||
| n (%) | n (%) | P-value | Mean (SD) | P-value | |
| Wealth Index | |||||
| Poorest | 198 (76.2) | 62 (23.9) | < 0.001 | 6.2 (3.2) | < 0.001 |
| Poorer | 185 (70.9) | 76 (29.1) | 6.1 (3.4) | ||
| Middle | 202 (78.0) | 57 (22.0) | 6.0 (3.2) | ||
| Richer | 185 (71.2) | 75 (28.9) | 6.3 (3.5) | ||
| Richest | 154 (59.5) | 105 (40.5) | 7.5 (3.8) | ||
| Religion | |||||
| Islam | 878 (72.8) | 328 (27.2) | < 0.001 | 6.3 (3.4) | < 0.001 |
| Others | 46 (48.9) | 48 (51.1) | 8.1 (3.5) | ||
| Husband education | |||||
| <=8 | 808 (83.9) | 155 (16.1) | < 0.001 | 5.4 (3.0) | < 0.001 |
| > 8 | 116 (34.4) | 221 (65.6) | 9.3 (3.1) | ||
| Distance to health centre | |||||
| 0–1 km | 268 (71.9) | 105 (28.2) | 0.384 | 6.4 (3.4) | 0.848 |
| 2–3 km | 346 (72.7) | 130 (27.3) | 6.4 (3.4) | ||
| 4 or more | 310 (68.7) | 141 (31.3) | 6.5 (3.6) | ||
| Age at marriage | |||||
| Less than 18 | 665 (79.0) | 177 (21.0) | < 0.001 | 5.8 (3.1) | < 0.001 |
| 18 or more | 259 (56.6) | 199 (43.5) | 7.5 (3.9) | ||
| Pregnancy no. | |||||
| 1 | 245 (56.6) | 188 (43.4) | < 0.001 | 7.6 (3.2) | < 0.001 |
| 2 | 254 (70.0) | 109 (30.0) | 6.9 (3.3) | ||
| 3 | 202 (78.3) | 56 (21.7) | 5.8 (3.3) | ||
| 4 or more | 223 (90.7) | 23 (9.4) | 4.2 (3.1) | ||
Covariates: (wealth index, religion, husband education, distance to health centre, age at marriage and pregnancy number)
All methods including multivariable adjusted, PS-covariate adjustment, PS-weighting, and PS-matching indicate a significant effect of maternal education (employing both binary and continuous exposure) on maternal health services where mothers exposed to secondary or higher levels of education were more likely to have four or more ANC, delivered at the facility, PNC within 42 days as well as receiving all maternal health services compared to the mothers who have below secondary level of education., Alternatively, a one-unit increase in educational grade leads to significant improvements in receiving maternal health services (Table 3). The effect estimates resulting from different methods to control for confounding were different. In case of binary exposure, considering the maternal health service named four or more ANC, all methods resulted in an estimated risk ratio less than the unadjusted risk ratio of 1.74 (95% CI: 1.48–2.05). The PS weighting (ATE and ATT) yielded the smallest estimated range of CI (ATE CI: 1.12–1.56 and ATT CI: 1.06–1.49). In the case of facility-based delivery, PNC within 42 days and receiving all maternal health services, the PS weighting (ATE and ATT) provided the smallest estimated range of CI. Regarding continuous exposure, estimates and the range of its corresponding CI were lower than those observed with binary exposure. In this case, PS-weighting also provided the smallest estimated range of CI.
Table 3.
Causal effect estimates by different methods of propensity score and effect estimates by multivariable-adjusted method
| Methods | Maternal Health Services | |||||||
|---|---|---|---|---|---|---|---|---|
| Four or more ANC | Facility based delivery | PNC within 42 days | Received all health services | |||||
| RR (95% CI) | Range of CI | RR (95% CI) | Range of CI | RR (95% CI) | Range of CI | RR (95% CI) | Range of CI | |
| Binary exposure | ||||||||
| Unadjusted | 1.74 (1.48–2.05) | 0.57 | 1.48 (1.32–1.66) | 0.34 | 1.51 (1.33–1.71) | 0.38 | 2.51 (1.99–3.18) | 1.19 |
| Multivariable adjusted | 1.32 (1.11–1.56) | 0.45 | 1.21 (1.06–1.38) | 0.32 | 1.28 (1.12–1.48) | 0.36 | 1.61 (1.21–2.14) | 0.93 |
| PS-Covariate Adjustment | 1.31 (1.10–1.56) | 0.46 | 1.20 (1.06–1.37) | 0.31 | 1.27 (1.11–1.46) | 0.35 | 1.58 (1.13–2.05) | 0.92 |
| PS-Weighting ATE | 1.36 (1.12–1.56) | 0.44 | 1.26 (1.12–1.42) | 0.30 | 1.31 (1.16–1.48) | 0.32 | 1.58 (1.14–2.04) | 0.90 |
| PS-Weighting ATT | 1.26 (1.06–1.49) | 0.43 | 1.24 (1.10–1.41) | 0.31 | 1.20 (1.09–1.36) | 0.27 | 1.34 (1.00-1.81) | 0.81 |
| PS-Matching (1:1) | 1.64 (1.38–1.89) | 0.51 | 1.40 (1.22–1.61) | 0.39 | 1.49 (1.28–1.76) | 0.48 | 2.39 (1.83–2.98) | 1.15 |
| PS-Matching (1:2) | 1.71 (1.49–1.97) | 0.48 | 1.43 (1.21–1.63) | 0.42 | 1.46 (1.23–1.68) | 0.45 | 2.42 (1.89–3.02) | 1.13 |
| Continuous exposure | ||||||||
| Unadjusted | 1.10 (1.04–1.17) | 0.13 | 1.09 (1.03–1.15) | 0.12 | 1.10 (1.05–1.17) | 0.12 | 1.21 (1.12–1.30) | 0.18 |
| Multivariable adjusted | 1.08 (1.02–1.13) | 0.11 | 1.07 (1.03–1.13) | 0.10 | 1.07 (1.02–1.10) | 0.08 | 1.19 (1.10–1.26) | 0.16 |
| PS-Covariate Adjustment | 1.11 (1.06–1.17) | 0.11 | 1.09 (1.05–1.14) | 0.09 | 1.07 (1.01–1.12) | 0.11 | 1.18 (1.09–1.27) | 0.16 |
| PS-Weighting | 1.10 (1.05–1.14) | 0.09 | 1.10 (1.06–1.13) | 0.07 | 1.06 (1.02–1.11) | 0.09 | 1.17 (1.11–1.23) | 0.12 |
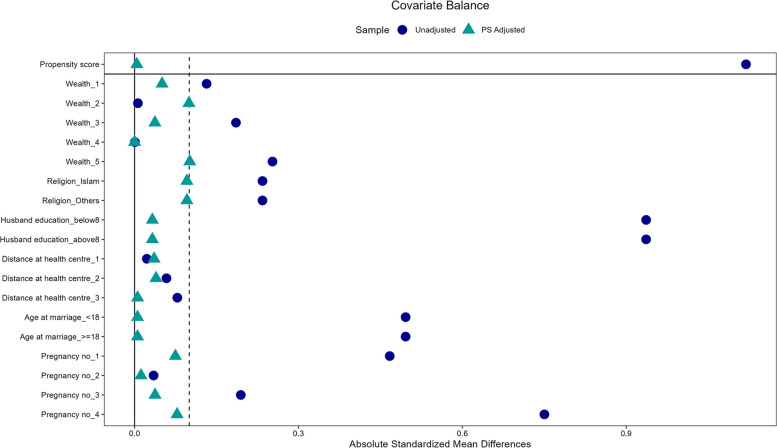
The Love plot [46] was used to visualise the absolute standardised mean difference (SMDs) in education level before and after PS weighting for assessing covariate balance (Fig. 3). A lower absolute value denotes a more balanced state. As can be observed, for unadjusted observational data, educational level exposure varies by covariates (wealth index, religion, husband education, distance to health centre, age at marriage and pregnancy number). After PS weighting adjustment, the majority of adjusted SMDs fall inside the 0.1 thresholds (dash-line), indicating substantial improvement in covariate balance across the exposure status (mothers’ educational level), resulting the satisfactory balance (Additional file 1: Appendix 2).
Fig. 3.
Absolute standardised mean differences for educational level before and after PS weighting
Discussion
The findings of this study revealed that maternal education is related to maternal health services in Bangladesh. By analysing maternal education as both a binary (secondary or higher vs. below secondary) and a continuous variable, we consistently found that higher educational levels were associated with increased use of maternal health services. After adjusting the PS, all methods including PS-covariate adjustment, PS-weighting, and PS-matching showed that mothers with a secondary or higher level of education had a higher likelihood of receiving health services (four or more ANC, delivered at the facility, PNC within 42 days as well as receiving all maternal health services) compared to the mothers with below secondary level of education. Similarly, when education was treated as a continuous variable, a higher educational level was consistently associated with an increased likelihood of receiving these maternal health services.
Under the causal inference concept, this study provides a rigorous estimation of the causal contribution of maternal education on the utilisation of maternal health services. The study’s findings showed that educational attainment is an important determinant for the proper use of maternal health services, women with secondary or higher education having a higher number of ANC visits, facility-based delivery, and PNC within 42 days. A low percentage (17%) of mothers received all three maternal health services. Around 30% of mothers with secondary or higher levels of education received all three maternal health services, whereas only around 10% of mothers below the secondary level of education received all three maternal health services. According to a study conducted in Bangladesh, the educational level of women has a significant impact on the optimal adoption of ANC services [47]. Studies in Bangladesh and elsewhere have revealed a strong association between the education of women and their utilisation of health facility delivery and other maternal health care [48–50]. Another study conducted in Bangladesh by Mosiur et al. [51] reported that mothers with a higher level of education have a higher likelihood of receiving PNC.
Education may have an impact on female reproductive health by causing late marriage, deferred childbearing, a lower fertility rate, increased independence in reproductive health decisions, the freedom to choose when and where to seek medical assistance without approval from anybody, and economic empowerment [52]. Regardless of the fact that education is linked to personal and family income levels, it is also related to the use of prenatal and natal services when income and wealth family index are controlled, as they were in this study. Similar findings have been found in Nigeria [53, 54], Kenya [55, 56], Netherlands [57] as well as several more countries [58, 59]. In addition, several studies, have found that illiterates had the highest risk of maternal and newborn illness, mortality, and disability, as well as the lowest utilisation of maternity services [56, 57, 59, 60].
In this study, we conducted an in-depth assessment of many of the available PS and covariate-adjustment approaches. Different techniques of estimation were shown to have varying estimates of the associated risk ratios in the study. In case of binary exposure, of the different propensity score methods examined, matching method matched sets of treated (exposed to secondary or higher level of education) and untreated (below secondary level of education) subjects who have a propensity score that is similar in value to one another. The number of untreated subjects in this study is many times greater than the number of treated subjects, PS matching usually resulted in all or nearly all treated patients being successfully matched, while many untreated patients remained unmatched and be excluded from the analysis (which may lead to slightly reduced efficiency). PS-covariate adjustment showed similar results like multivariable adjusted in estimating effect of maternal education on receiving maternal health services. Moreover, the standard deviation of the estimates was higher than that obtained by PS-weighting approaches. We examined two different IPTW approaches for assessing absolute effects of maternal education on usage of maternal health services. PS weighting (ATE and ATT) provides narrower range of CI among all the methods to estimate effect of maternal education on maternal health services. The weighted analysis provides the theoretical advantage of utilising data from all samples of the study and is not affected by additional uncontrolled confounding due to the inability to locate an exact match for each treatment subject [61]. A study conducted by Jiaqi et al. (2016) [62] performed simulation studies and reported that when PS is accurately modeled, indicate that weighting produces unbiased estimates.
Binary categorisation of education can lead to information loss, resulting in less precise estimates with larger standard errors. Conversely, treating education as a continuous variable preserves information, leading to more precise estimates with smaller standard errors. While binary models are simpler and easier to interpret, they may oversimplify the exposure-outcome relationship. Nevertheless, PS-weighting performed better in terms of precision in both approaches. In summary, much of the difference between the adjustment procedures arose. It may vary depending on the different settings of different types of study. However, in the evaluation and interpretation of the influence of maternal education on receiving maternal health care services in case of using observational study, the weighted estimates are preferred.
What insights can we have from these experiences to make recommendations for the future applications of propensity score methods and covariate adjustment? As with any study, the main analysis strategy should be defined in advance. A useful approach is to review the baseline covariates before accessing outcome data to identify the most suitable PS method or covariate adjustment, considering factors like the overlap in PS between treatment and control groups. Relying on a single method (which may have its flaws) might be too limiting, so it is wise to predefine several analyses using alternative approaches. This helps assess whether findings on the estimated treatment effect are consistent, thereby enhancing confidence in the primary results.
Strengths and limitations
We believe this is the first study conducted in Bangladesh, providing a rigorous estimation of the causal contribution of maternal education on maternal health services. The use of propensity score approaches is one way of reducing bias in observational studies. PS approaches may be more suited in situations when the event is infrequent (compared to the number of observed baseline variables) and the sample size is insufficient to take into account the multiple covariates [63]. However, in this study, the analysis was carried with a relatively large sample size, which was considered to be a strength. Another key strength of this study is its comprehensive evaluation of several propensity score methods (PS matching, PS weighting, and covariate adjustment) and covariate-adjustment approach. Additionally, we considered maternal education as both a binary and continuous exposure, which allowed us to capture more nuanced effects of educational attainment. The consistent findings across these methods and exposure measures enhance the robustness of our conclusions regarding the impact of maternal education on maternal health services. From the density plot of PS, we observed that there is a common support region where the propensity scores of both groups overlapped as well as small SMDs values after PS adjustment indicating balancing of the covariates (Additional file 1: Appendices 2–3). We assumed that all relevant confounders were measured and included in the propensity score model. We observed that mothers with higher education levels were more likely to receive four or more ANC visits, opt for facility delivery, and obtain PNC services within 42 days. These observed outcomes reflect the potential outcomes if those mothers indeed had those education levels. This assumption was supported by the alignment of our findings with previous studies [47–51], suggesting that the observed relationships between maternal education and health service utilisation are valid and consistent with the causal effect of education.
Despite our efforts to adjust for measured confounders, unmeasured confounding remains a possibility. PS approaches do not account for unknown variables that might influence whether or not subjects receive treatment i.e., being exposed to secondary or higher level of education (this is why a randomised controlled trial is desirable) [63]. As a result, there may still be unmeasured confounding, which should be considered as a limitation. In addition, to ensure that our findings can be applied to other communities, research in other parts of Bangladesh are required because the study participants were from riverine regions. Therefore, our findings need to be evaluated with caution, and more studies need to be conducted to validate findings.
Conclusion and recommendations
Educational status was found to be significantly associated with ANC, delivery and PNC services. The findings provided important insights into the efficiency of various PS approaches for reducing the influence of confounding variables and achieving accurate estimates. All methods indicated a significant causal effect of maternal education on the usage of maternal health services. However, the propensity score weighting method demonstrated better results in terms of providing more precise estimates with a narrower range of confidence intervals. This indicates that this method may be a robust approach for estimating the causal effect that maternal education has on the utilisation of maternal health services. PS weighting can be employed to evaluate the causal influence in a scenario discussed in this study. These findings may be utilised by policymakers and healthcare practitioners for the purpose of establishing targeted initiatives that are aimed at increasing maternal education, particularly in places that are difficult to reach. An education campaign for women is required; regular knowledge-enhancing seminars for pregnant mothers may play an important role in raising awareness of the need for having access to maternal health care facilities. For future positive health outcomes, government efforts should be targeted to improve women’s education at least to the secondary level.
Supplementary Information
Acknowledgements
This research study was funded by the Department of Foreign Affairs, Trade and Development (DFATD), through Advancing Sexual and Reproduction Health and Rights (AdSEARCH), Grant number: SGDE-EDRMS-#9926532, Purchase Order 7428855, Project P007358. icddr,b acknowledges with gratitude the commitment of Grand Challenges Canada to its research efforts. icddr,b is also grateful to the Governments of Bangladesh, Canada, Sweden and the UK for providing core/unrestricted support. We want to humbly pay our gratitude to the mothers from hard-to-reach areas, that we have included in our paper. The authors would like to express their sincere gratitude to StatReader training sessions organized by MCHD, icddr,b, as the insights and skills acquired during these sessions were instrumental in the design and execution of this research.
Authors' contributions
EA as first author and AA as senior author conceptualised, developed, incorporated feedback from all authors, and finalised the manuscript. MSR, ATH, ABS and PBC assisted EA in data analysis and interpretation. MSR, AS, SEA, and AER reviewed the first draft and provided their input. All authors read and approved the final manuscript.
Funding
This research study was funded by the Department of Foreign Affairs, Trade and Development (DFATD).
Data availability
Summary statistic of the data analysed in this work are all provided in the main manuscript document and its supplements.
Declarations
Ethics approval and consent to participate
Ethical approval for this study was obtained from the institutional review board (IRB) of International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b). Participants were informed about the study’s goal, benefits, and risks. Everyone who took part in the study did so of their own free will and received a data protection declaration in line with the Helsinki Declaration. Prior to conducting the interview, written informed consent was obtained from participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ema Akter, Email: eakter@isrt.ac.bd, Email: ema.akter@icddrb.org.
Anisuddin Ahmed, Email: anisuddin@icddrb.org, Email: anisuddin.ahmed@uu.se.
References
- 1.World Health Organization (WHO). Maternal mortality:fact-sheets. 2019. Available from: https://wwww.hoint/news-room/fact-sheets/detail/maternal-mortality.
- 2.National Institute of Population Research and Training (NIPORT), International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), and MEASURE Evaluation. Bangladesh Maternal Mortality and Health Care Survey 2016: Final Report. Dhaka, Bangladesh, and Chapel Hill, NC, USA: NIPORT, icddr,b, and MEASURE Evaluation. 2019. https://niport.portal.gov.bd/sites/default/files/files/niport.portal.gov.bd/miscellaneous_info/4c534fbe_dc9c_491e_89d7_1f85ab298e93/2020-08-23-18-28-35970449b61ba2439986d9e68dfd83b4.pdf.
- 3.Kifle D, Azale T, Gelaw YA, et al. Maternal health care service seeking behaviors and associated factors among women in rural Haramaya District, Eastern Ethiopia: a triangulated community-based cross-sectional study. Reprod Health. 2017;14:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institute of Population Research and Training (NIPORT), and ICF. 2020. Bangladesh Demographic and Health Survey 2017-18. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT and ICF. https://dhsprogram.com/pubs/pdf/FR344/FR344.pdf.
- 5.Greenaway ES, Leon J, Baker DP. Understanding the association between maternal education and use of health services in Ghana: exploring the role of health knowledge. J Biosoc Sci. 2012;44:733–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations. Sustainable Development Goals. https://unstats.un.org/sdgs/metadata/?Text=&Goal=3&Target.
- 7.Cleland JG, Van Ginneken JK. Maternal education and child survival in developing countries: the search for pathways of influence. Soc Sci Med. 1988;27:1357–68. [DOI] [PubMed] [Google Scholar]
- 8.Raghupathy S. Education and the use of maternal health care in Thailand. Soc Sci Med. 1996;43:459–71. [DOI] [PubMed] [Google Scholar]
- 9.Bicego GT and Boerma J. Maternal education, use of health services, and child survival: An analysis of data from the Bolivia DHS Survey. Columbia: Institute for Resource Development/Macro Systems, Inc.; 1990. https://dhsprogram.com/pubs/pdf/wp1/wp1.pdf.
- 10.Elo IT. Utilization of maternal health-care services in Peru: the role of women’s education. Health Transition Rev. 1992;2:49–69. [PubMed]
- 11.Fosu GB. Access to health care in urban areas of developing societies. J Health Soc Behav 1989;30:398–411. [PubMed]
- 12.Caldwell JC. Education as a factor in mortality decline an examination of Nigerian data. Popul Stud 1979;33:395–413.
- 13.Farah A-A, Preston SH. Child mortality differentials in Sudan. Popul Dev Rev 1982;8:365–83.
- 14.Fosu GB. Maternal influences on preventive health behavior in children. Int Q Community Health Educ. 1991;12:1–19. [DOI] [PubMed] [Google Scholar]
- 15.Caldwell JC. Routes to low mortality in poor countries. Popul Dev Rev. 1986;36:171–220. [DOI] [PubMed]
- 16.Caldwell JC. Cultural and social factors influencing mortality levels in developing countries. Annals Am Acad Political Soc Sci. 1990;510:44–59. [Google Scholar]
- 17.Caldwell JC, Reddy PH, Caldwell P. The social component of mortality decline: an investigation in South India employing alternative methodologies. Popul Stud. 1983;37:185–205. [PubMed] [Google Scholar]
- 18.Sushama P. N. Social context of health behaviour in Kerala. In What We Know About Health Transition; The Cultural, Social and Behavioural Determinants of Health (Edited by Caldwell J. et al.). Canberra: The Australian National University Press; 1989. p. 77.
- 19.Coffman DL, Balantekin KN, Savage JS. Using propensity score methods to assess causal effects of mothers’ dieting behavior on daughters’ early dieting behavior. Child Obes. 2016;12:334–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Talukder A, Akter N, Sazzad Mallick T. Exploring association between individuals’ stature and type 2 diabetes status: propensity score analysis. Environ Health Insights. 2019;13:1178630219836975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pan W, Bai H. Propensity score methods for causal inference: an overview. Behaviormetrika. 2018;45:317–34. [Google Scholar]
- 22.Sekine K, Carandang RR, Ong KIC, et al. Identifying the causal effect of child marriage on unmet needs for modern contraception and unintended pregnancy in Nepal: a cross-sectional study using propensity score matching. BMJ open. 2021;11: e043532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 24.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79:516–24. [Google Scholar]
- 25.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33–8. [Google Scholar]
- 26.Biswas A, Halim A, Rahman F, et al. Factors associated with maternal deaths in a hard-to-reach marginalized rural community of Bangladesh: a cross-sectional study. Int J Environ Res Public Health. 2020;17: 1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elze MC, Gregson J, Baber U, et al. Comparison of propensity score methods and covariate adjustment: evaluation in 4 cardiovascular studies. J Am Coll Cardiol. 2017;69:345–57. [DOI] [PubMed] [Google Scholar]
- 28.Rahman AE, Ameen S, Hossain AT, et al. Success and time implications of SpO2 measurement through pulse oximetry among hospitalised children in rural Bangladesh: variability by various device-, provider-and patient-related factors. J Global Health. 2022;12:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Education Policy. 2010. Available from: https://www.reliefwebint/report/bangladesh/national-education-policy-2010-enbn.
- 30.StataCorp. Stata statistical software: release 14. College Station: StataCorp LP; 2015. [Google Scholar]
- 31.R Core Team. (2024). R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/.
- 32.Gallis JA, Turner EL. Relative measures of association for binary outcomes: challenges and recommendations for the global health researcher. Ann Global Health. 2019;85:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46:399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Austin PC, Schuster T. The performance of different propensity score methods for estimating absolute effects of treatments on survival outcomes: a simulation study. Stat Methods Med Res. 2016;25:2214–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brookhart MA, Wyss R, Layton JB, et al. Propensity score methods for confounding control in nonexperimental research. Circulation: Cardiovasc Qual Outcomes. 2013;6:604–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morgan SL, Todd JJ. 6. A diagnostic routine for the detection of consequential heterogeneity of Causal effects. Sociol Methodol. 2008;38:231–82. [Google Scholar]
- 38.Austin PC, Stuart EA. Estimating the effect of treatment on binary outcomes using full matching on the propensity score. Stat Methods Med Res. 2017;26:2505–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Austin PC. Assessing the performance of the generalized propensity score for estimating the effect of quantitative or continuous exposures on binary outcomes. Stat Med. 2018;37:1874–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hirano K, Imbens G. The propensity score with continuous treatments. Applied bayesian modeling and causal inference from incomplete-data perspectives. John Wiley & Sons, Ltd; 2004.
- 41.Austin PC. Assessing covariate balance when using the generalized propensity score with quantitative or continuous exposures. Stat Methods Med Res. 2019;28:1365–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wu X, Mealli F, Kioumourtzoglou M-A, et al. Matching on generalized propensity scores with continuous exposures. J Am Stat Assoc. 2024;119:757–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brown DW, Greene TJ, Swartz MD, et al. Propensity score stratification methods for continuous treatments. Stat Med. 2021;40:1189–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Imbens GW. The role of the propensity score in estimating dose-response functions. Biometrika. 2000;87:706–10. [Google Scholar]
- 45.Zhang Z, Zhou J, Cao W, et al. Causal inference with a quantitative exposure. Stat Methods Med Res. 2016;25:315–35. [DOI] [PubMed] [Google Scholar]
- 46.Ahmed A, Husain A, Love TE, et al. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006;27:1431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: assessing the extent of compliance with the WHO recommendations. PLoS ONE. 2018;13: e0204752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Colombara DV, Hernández B, Schaefer A, et al. Institutional delivery and satisfaction among indigenous and poor women in Guatemala, Mexico, and Panama. PLoS ONE. 2016;11: e0154388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kamal SM, Hassan CH, Alam GM. Determinants of institutional delivery among women in Bangladesh. Asia Pac J Public Health. 2015;27:NP1372-1388. [DOI] [PubMed] [Google Scholar]
- 50.Tekelab T, Yadecha B, Melka AS. Antenatal care and women’s decision making power as determinants of institutional delivery in rural area of Western Ethiopia. BMC Res Notes. 2015;8:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mosiur Rahman M, Haque SE, Sarwar Zahan M. Factors affecting the utilisation of postpartum care among young mothers in Bangladesh. Health Soc Care Commun. 2011;19:138–47. [DOI] [PubMed] [Google Scholar]
- 52.Umar AS. Does female education explain the disparity in the use of antenatal and natal services in Nigeria? Evidence from demographic and health survey data. Afr Health Sci. 2017;17:391–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fawole A, Shah A, Fabanwo A, et al. Predictors of maternal mortality in institutional deliveries in Nigeria. Afr Health Sci. 2012;12:32–40. [PMC free article] [PubMed] [Google Scholar]
- 54.Ononokpono DN, Odimegwu CO. Determinants of maternal health care utilization in Nigeria: a multilevel approach. Pan Afr Med J. 2014;17:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Desai M, Phillips-Howard PA, Odhiambo FO, et al. An analysis of pregnancy-related mortality in the KEMRI/CDC health and demographic surveillance system in western Kenya. PLoS ONE. 2013;8: e68733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yego F, D’este C, Byles J, et al. Risk factors for maternal mortality in a Tertiary Hospital in Kenya: a case control study. BMC Pregnancy Childbirth. 2014;14:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ory BE, Van Poppel FW. Trends and risk factors of maternal mortality in late-nineteenth-century Netherlands. History Family. 2013;18:481–509. [Google Scholar]
- 58.Ahmed S, Creanga AA, Gillespie DG, et al. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS ONE. 2010;5:e11190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang, Wenjuan, Soumya Alva, Shanxiao Wang, and Alfredo Fort. Levels and Trends in the Use of Maternal Health Services in Developing Countries. DHS Comparative Reports No. 26. Calverton: ICF Macro; 2011. https://dhsprogram.com/pubs/pdf/CR26/CR26.pdf.
- 60.Folaranmi OO. Women empowerment as a determinant of investments in children in selected rural communities in Nigeria. Afr Res Rev. 2013;7:138–61. [Google Scholar]
- 61.Rosenbaum PR, Rubin DB. The bias due to incomplete matching. Biometrics. 1985;41:103–16. [PubMed] [Google Scholar]
- 62.Li J, Handorf E, Bekelman J, et al. Propensity score and doubly robust methods for estimating the effect of treatment on censored cost. Stat Med. 2016;35:1985–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Barnieh L, James MT, Zhang J, et al. Propensity score methods and their application in nephrology research. J Nephrol. 2011;24:256–62. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Summary statistic of the data analysed in this work are all provided in the main manuscript document and its supplements.