Abstract
Background
The phenomenon of suicide risk (SR) represents a psychiatric, social and environmental emergency. The acute psychiatric ward as the Italian Service for Psychiatric Diagnosis and Care (SPDC) represents the place where SR is high due to the acute and serious conditions of people hospitalized. The objective of this study was to evaluate the characteristics of subjects admitted to a SPDC over a 6-year period for SR represented by: suicidal ideation, attempted and failed suicide.
Methods
With a retrospective single-center observational design, we collected hospitalizations from 01/01/2017 to 31/12/2022 in the SPDC of AUSL-Modena for SR, analyzed the modality of SR and compared the demographic and clinical variables of subjects with SR with those hospitalized for other clinical reasons in the same period. Data were statistically analyzed.
Results
In the 6-year of study period, we collected 2,930 hospitalizations in the SPDC of AUSL- Modena and among them, 68% (n = 528) were carried out due to SR, which represented the second leading cause of hospitalization (18%), in particular among females (Pearson Chi2 = 17.41, p < 0.001). Individuals with SR were more frequently voluntary admitted (Pearson Chi2 = 215.41, p < 0.001) for a shorter period (7.36 ± 8.16 vs 11.66 ± 15.93, t = 6.03, t-test, p < 0.001) and less frequently repeated the hospitalization during the study period for the same reason (Pearson Chi2 = 6.0, p = 0.014). The most frequent psychiatric disorders associated with SR were depressive, personality and adjustment disorders, which represented the most common factor associated with SR (68%), followed by family/relationship problems (12%) and alcohol/substance abuse (8%). We highlighted three kinds of suicidal risk: suicidal ideation (40%), often associated with personality disorders and substance use disorders, drug ingestion (30%) concomitant with conflicting family relationships and use of violent means (30%) associated with depressive disorders (Pearson Chi2 = 42.83, p = 0.002).
Conclusions
Our study provides a real-world setting evaluation of subjects hospitalized for SR and, in accordance with literature, suggests that suicidal behavior is the product of many clinical and social factors’ interaction, that occurred in a crucial moment of life in vulnerable individuals. The identification of subjects at SR represents the first step of preventive multi-professional interventions.
Keywords: Suicidal ideation, Suicide attempts by drug ingestion, Violent suicide attempts, Acute psychiatric ward, Hospitalizations for suicide risk
Background
Suicide is defined by World Health Organization (WHO) as “an act aimed at killing upon oneself, deliberately initiated and performed by the person concerned, in full awareness or expectation of its fatal outcome” [1]. According to WHO, about one million people died by suicide in 2000 [2]. Over the past 45 years, the suicide rate has increased by 65 percent worldwide [1]. For every suicide there are 20 or more suicide attempt [3]. Fifty percent of deaths occur on the first attempt [4]. Different terminologies indicate distinguish among suicidal ideation, para-suicide, self-injurious behavior, suicidal behavior, masked suicide, failed suicide and chronic suicide [5–7]. Suicidal ideation is a broad term used to describe a wide range of desires and concerns about death and suicide. Kleiman et al. (2017) [8] highlighted that suicidal ideation fluctuates over the course of hospitalization, with varying intensity, often varying even on the same day [9]. Males have been found to have a lower rate of suicide attempts than females but a very high rate of completed suicide compared to females. The male/female ratio of age-standardized suicide rates globally is 1.9 [10]. Many studies suggest that females survive suicide attempts more often than males because they use less lethal means and their outcomes are less lethal than males when they use the same method [11, 12]. According to a recent analysis in 2022 [13], women are more likely to attempt suicide than men; possible explanations include higher rates of Major Depressive Disorder (MDD), borderline personality disorder (BPD), and Post-Traumatic Stress Disorder (PTSD) among women, as well as lower rates of substance use disorder (SUD) [14, 15]. From a psychological perspective, there are three characteristics of the suicidal subject [16]:
ambivalence: until the end, the subject is conflicted in his suicidal intent, with a constant alternation between wishing for death and seeking help,
impulsivity: the suicidal act is performed by giving space to an impulse that overcomes and leads the subject to self-annihilate,
rigidity and limited thinking/tunnel vision: the pre-suicide mental state is described as altered/dissociated, particularly in the moments before the act.
During the period prior to the suicide itself, particularly limited and rigid vision in a cognitive sense was observed, with a rigidly pessimistic view of reality and little freedom of thought. Numerous are the risk factors for suicide: para-suicide, considering that more than 50 percent of suicide attempts are made by individuals who have made at least one attempt before and almost 20 percent repeat the act within the following 12 months [17, 18]; gender males commit complete suicide compared to females with a 3:1 ratio; sexual minorities [19], due to discrimination, social prejudice and lack of support; age, with a prominent peak in men after age 45 and in women after age 55; marital separations: a recent divorce increases the odds of suicide risk by 1.6 times compared to distal divorce [20]; unemployment, due to deteriorating social roles and increased stress and anxiety associated with financial problems; the COVID-19 epidemic, with increases in anxiety, insomnia, depression, alcohol and drug use, and suicidal behavior due to self-isolation and quarantine [21, 22]; health problems, particularly neurological disease (40%), cardiovascular disease (26%), and cancer (10%) [23]; trauma and abuse, with the risk of attempted suicide being two to four times higher [24]; psychiatric pathology [25] with increased risk of suicide in people with Schizophrenia, Bipolar Disorder and Major Depression [26], as well as Borderline Personality Disorder [27], Eating Behavior Disorders [28, 29]. Among the protective factors we find social support, family bonding, religion, and participation in religious activities [30], as well as having children [31]. Suicide also occurs in the hospital, where it is a relevant sentinel event, whose prevention relies on proper assessment of the patient's condition. The area most at risk are: psychiatric wards, Oncology, Gynecology and Obstetrics, the Emergency Department, and common hospital areas (terraces, stairs, etc.). Suicide prevention is considered a priority by the WHO’s “Mental Health Action Plan 2013–2020” [32]. Primary prevention interventions are aimed at reducing the incidence of suicidal behavior and are aimed at the general population. Restricting the availability and ease of access to the means used to enact suicide is listed by WHO as one of the actions needed to reduce suicide mortality [33]. Still much can be done to reduce the number of suicides committed by precipitation from high places, such as the installation of deterrent elements, such as protective nets for under bridges, overpasses, and other “risk” architectural structures, which could help reduce the number of suicides [34]. The expression Werther effect refers to the phenomenon whereby news of a suicide, published in the mass media, causes a chain of other suicides in society [35]. Secondary prevention may be applied in cases where individuals with suicide risk are identified. An important role of secondary prevention can be exerted by drug therapies and psychotherapies. Lithium is associated with reduced suicidal risk in patients with mood disorder. The anti-suicidal effect could be exerted through the reduction of mood disorder and also through the reduction of aggression and impulsivity [36], which relies on the use of pharmacological therapies (lithium, clozapine) and psychotherapy. Furthermore, according to a systematic review of the literature, individuals who drink water with a higher level of Lithium might have a reduced risk of suicide compared to the general population [37]. Another drug associated with reduced suicide risk is clozapine, probably due to a reduction in aggression and impulsivity [38]. Antidepressants may be associated with attenuated depression and suicidal behavior in adult individuals with major depression [39]. Some recent research has shown that ketamine may have an anti-suicidal effect [40], indeed, just think of the introduction of the new drug containing esketamine for the treatment of Resistant Major Depression [41]. As part of tertiary prevention, follow-up of subjects who have engaged in suicidal behaviors is critical [42], 10–12% of subjects repeat the act within 12 months. 1% go on to die by suicide in the following year and 10% to 30% in the following 10 years.
The influence of possible biomarkers of suicidal behavior has been hypothesized by some authors [43], in particular the neutrophil-to-lymphocyte ratio (NLR) which may be a trait marker for suicidal vulnerability in patients with depression [44].
Clinicians should perform a comprehensive suicide risk assessment on any individual who expresses suicidal tendencies such as ideation, thought, intention or attempt and, more specifically, when some of risk factors for suicide occur. The risk assessment is aimed at identifying the individual's suicide risk and protective factors for the implementation of personalized interventions to reduce suicide risk [45]. The assessment of suicide risk consists of four main steps: 1) assessment of suicidality (suicidal ideation and behavior, intent, plan and motivation); 2) evaluation of suicide risk factors (socio-demographic, clinical and psychological ones); 3) identification of factors underlying or precipitating the suicidal ideation and behaviour; 4) targets for intervention (psychiatric diagnosis and symptoms, distressing psychosocial situations, maladaptive traits and coping skill) [45]. Regarding suicide risk, one recent review suggests the need for a shift in focus from risk factors to machine learning-based risk algorithms [46]. In any case, suicide risk assessment should be able to discriminate those at high- and low-risk for suicidal self-directed violence [47].
Study objective
Since the identification of subjects at suicide risk (SR) represents the first step for preventive interventions, we evaluated the SR among subjects hospitalized in an acute psychiatric ward over a 6-year period, hypothesizing that some demographic and clinical characteristics could be possible indicators of suicidal risk.
Materials and methods
Study design, period and setting
The design of this study was observational, retrospective, and single center.
The study period ranged between January 1, 2017 and December 31, 2022, for a total of six years. The setting was the Service for Psychiatric Diagnosis and Care (SPDC) of AUSL-Modena, which, in accordance with Italian Laws 180/78 and 833/78 [48, 49], is in a general hospital, provides 15 beds for voluntary and involuntary hospitalizations of adults and 2 beds for adolescents. SPDC is closely connected with the Mental Health and Drug Abuse Department to which it belongs [48, 49]. The catchment area includes a population of 701,751 living in the province of Modena.
Sample eligibility criteria, selected variables and study procedure
We included all subjects hospitalized at the SPDC of AUSL-Modena during the study period with the exclusion of < 18-year individuals. We collected demographic variables of hospitalized subjects: age, sex, nationality, employment and housing conditions, educational level, presence of a support administrator (SA), who legally supports a person temporarily or permanently unable to manage his/her interests and health, according to Italian Law 6/2004 [50]. We selected the following clinical variables: clinical reason for hospitalization, diagnosis at discharge (ICD 9-CM), length of hospital stay (in days) and length of stay in involuntary hospitalizations (in days), voluntary (VHs) and involuntary hospitalizations (IHs), substance use comorbidity, medical comorbidity, previous treatment and care, previous psychiatric hospitalizations, aggressive behavior during hospitalization, psychiatric medications and mono/poly-therapy prescribed at discharge and discharge destination.
Data were collected from the discharge letters available in the information system database used at SPDC.
We analyzed the kind of suicide risk in our sample, divided in suicidal ideation, suicide attempt, and missed suicide and the pre-existing conditions to suicide risk.
We compared the demographic and clinical data of individuals admitted to the SPDC of the AUSL of Modena for SR with those of other people hospitalized in the same period for other reasons.
The data were anonymized assigning each selected patient a numerical code progressive and reported in an Excel database for statistical analysis.
Statistical analysis
We analyzed:
mean ± Standard Deviation (m ± SD) for continuous variables, t-test for the analysis of normally distributed continuous variables, which were previously assessed applying Shapiro–Wilk, Skewness-Kurtosis, and Shapiro-Francia tests;
non-parametric Kruskal–Wallis test for variables with non-normal distribution,
percentages and Pearson Chi2 test for categorical variables, Standardized Residuals (SRES ≥ 2 or ≤ -2; p < 0.05) for subcategories of variables with statistically significant differences,
multiple logistic regression, forward and backward stepwise model, between SR (= 1), as dependent variable, and the other clinical reasons (= 0).
A p-value < 0.05 was considered statistically significant. The data was analyzed using STATA-12 (Stata Corp., College Station, TX, 2011).
Ethical Considerations
The study was approved by the Ethics Committee of the North Emilia Area Vasta (Prot. 306/2022/AOU) with subsequent amendment for extension of the period examined (Prot. 10,826/2023) and authorized by the AUSL- Modena (Prot. no. 688; 27/4/2023).
Results
Demographic and clinical characteristics of our sample
In the 6 years of the study, we collected 2,930 hospitalizations in the SPDC of AUSL- Modena; 60.68% of hospitalizations were carried out by men (n = 1,778) and 39.31% by women (n = 1,152), as shown in Table 1. The mean age of the subjects was 41.48 years (± 15.03 SD); the majority of the subjects were Italians (n = 2,286, 78.02%) and only 11.46% benefited from SA; 27.09% of the sample was represented by unemployed individuals and 12.35% by pensioners for disability; most subjects had obtained a middle school diploma (34.91%) and have high school diploma (21.97%); most of them lived in parental family (27.71%) and acquired family (18.8%) (Table 1).
Table 1.
Demographic variables of subjects hospitalized for suicide risk and other clinical reasons in SPDC in the study period
| Variables | Suicide risk (n =528) |
Other clinical reasons (n =2,425) | Total (n =2,903) |
Statistical test Probability |
|---|---|---|---|---|
| SEX, n (%) | ||||
| Male | 278 (52.65%) | 1500 (62.44%) | 1778 (60.68%) |
Pearson Chi2 = 17.41 p = 0.000 SRES ≥ 2, p < 0.05 |
| Female | 250 (47.34%) | 902 (37.55%) | 1152 (39.31%) | |
| Nationality, n (%) | ||||
| Italian | 435 (82.38%) | 1851 (77.06%) | 2286 (78.02%) |
Pearson Chi2 = 7.34 p = 0.025 SRES ≥ 2, p < 0.05 |
| European non-Italian | 23 (4.35%) | 149 (6.20%) | 172 (5.87%) | |
| Extra-European | 70 (13.25%) | 402 (16.73%) | 472 (16.10%) | |
| Support administrator, n (%) | ||||
| Present | 34 (6.43%) | 302 (12.57%) | 336 (11.46%) |
Pearson Chi2 = 16.03 p = 0.000 SRES ≥ 2, p < 0.05 |
| Absent | 494 (93.56%) | 2100 (87.42%) | 2594 (88.53%) | |
| Working condition, n (%) | ||||
| Unemployed | 121 (22.91%) | 673 (28.01%) | 794 (27.09%) |
Pearson Chi2 = 26.59 p = 0.000 SRES ≥ 2, p < 0.05 |
| Employed | 117 (22.15%) | 420 (17.48%) | 537 (18.32%) | |
| Student | 49 (9.28%) | 133 (5.53%) | 182 (6.21%) | |
| Retired by age | 25 (4.73%) | 96 (3.99%) | 121 (4.12%) | |
| Disability pension | 46 (8.71%) | 316 (13.15%) | 362 (12.35%) | |
| Unknown | 170 (32.19%) | 764 (31.80%) | 934 (31.87%) | |
| Housing condition, n (%) | ||||
| Parental family | 140 (26.51%) | 672 (27.97%) | 812 (27.71%) |
Pearson Chi2 = 25.858 p = 0.000 SRES ≥ 2, p < 0.05 |
| Acquired family | 127 (24.05%) | 424 (17.65%) | 551 (18.80%) | |
| Living alone | 54 (10.22%) | 282 (11.74%) | 336 (11.46%) | |
| Community or protected facility | 67 (12.68%) | 366 (15.23%) | 433 (14.77%) | |
| Homeless | 20 (3.78%) | 99 (4.12%) | 119 (4.06%) | |
| Prison or judicial hospital | 10 (1.89%) | 11 (0.45%) | 21 (0.71%) | |
| Other or not known | 110 (20.83%) | 548 (22.81%) | 658 (22.45%) | |
| Education, n (%) | ||||
| Illiteracy | 4 (0.75%) | 28 (1.16%) | 32 (1.09%) |
Pearson Chi2 = 5.305 p = 0.380 |
| Elementary School | 24 (4.54%) | 144 (5.99%) | 168 (5.73%) | |
| Middle School | 171 (32.38%) | 852 (35.47%) | 1023 (34.91%) | |
| High School | 126 (23.86%) | 518 (21.56%) | 644 (21.97%) | |
| University Degree | 23 (4.35%) | 99 (4.12%) | 122 (4.16%) | |
| Unknown | 180 (34.09%) | 761 (31.68%) | 941 (32.11%) | |
SRES Standardized Residuals
The sample was divided based on the reason for hospitalization: patients hospitalized for SR and for other clinical reasons. Regarding the demographic variables (Table 1), we found that subjects hospitalized for SR, in comparison with people hospitalized for other clinical reasons:
were more frequently female (47.34% vs 37.55%, Pearson chi2 = 17.41, p < 0.001) and Italians (82.38% vs 77.06%, SRES = 2.67, p < 0.05; Pearson chi2 = 7.340, p = 0.025),
less frequently benefited from support administrator (6.43% vs 12.57%, Pearson chi2 = 16.03, p < 0.001),
were more frequently employed (22.15% vs 17.48%, SRES = 2.51, p < 0.05) or students (9.28% vs 5.53%, SRES = 3.23, p < 0.05) (Pearson chi2 = 26.589, p < 0.001),
lived more often in stepfamily (24.05% vs 17.65%, SRES = 3.41, p < 0.05) or in a judicial institution (1.89% vs 0.45%, SRES = 3.54, p < 0.05) (Pearson chi2 = 25.858, p < 0.001).
Regarding the clinical variables (Table 2), we found that subjects hospitalized for SR, in comparison.
Table 2.
Clinical characteristics of hospitalizations for suicide risk and other clinical reasons in SPDC in the study period
| Variables | Suicide risk (N=528) |
Other clinical reasons (N =2,425) |
Total (N=2,953) |
Statistical test Probability |
|---|---|---|---|---|
| Year, n (%) | ||||
| 2017 | 88 (16.6%) | 492 (20.48%) | 580 (19.79%) |
Pearson Chi2 = 19.394 p = 0.002 SERS ≥ 2, p < 0.05 |
| 2018 | 106 (20.07%) | 495 (20.60%) | 601 (20.51%) | |
| 2019 | 117 (22.15%) | 459 (19.10%) | 576 (19.65%) | |
| 2020 | 88 (16.66%) | 335 (13.94%) | 423 (14.43%) | |
| 2021 | 81 (15.34%) | 286 (11.90%) | 367 (12.52%) | |
| 2022 | 48 (9.09%) | 335 (13.94%) | 383 (13.07%) | |
| Repeated hospitalizations in the study period, n (%) | ||||
| Repeated hospitalizations | 52 (9.84%) | 332 (13.82%) | 384 (13.10%) |
Pearson Chi2 = 6.000 p = 0.014 SERS ≥ 2, p < 0.05 |
| Non-repeated hospitalizations | 476 (90.15%) | 2070 (86.17%) | 2552 (87.09%) | |
| Duration of hospitalizations, n (%) | ||||
| Hospitalization days, m±DS | 7.36 ± 8.16 | 11.66 ± 15.93 | 10.88 ± 14.91 | t = 6.03, t-test, p <0.001 |
| Involuntary hospitalization days, m±DS | 4.7 ± 3.85 | 7.02 ± 6.17 | 6.91 ± 6.1 | t = 2.71, t-test, p =0.003 |
| Hospitalization regime, n(%) | ||||
| Voluntary | 473 (89.58%) | 1327 (55.24%) | 1800 (61.43%) |
Pearson Chi2 = 215.410 p = 0.000 SERS ≥ 2, p < 0.05 |
| Involuntary | 55 (10.41%) | 1075 (44.75%) | 1130 (38.56) | |
| Previous treatments, n (%) | ||||
| Mental Health Service (MHS) | 252 (47.72%) | 1373 (57.16%) | 1625 (55.46%) |
Pearson Chi2 = 37.66 p = 0.000 SERS ≥ 2, p< 0.05 |
| Substance Use Service (SUS) | 30 (5.68%) | 68 (2.83%) | 98 (3.34%) | |
| Private or other specialist | 36 (6.82%) | 105 (4.36%) | 141 (4.77%) | |
| Other services | 13 (2.46%) | 38 (1.58%) | 51 (1.74%) | |
| MHS + other services | 18 (3.40%) | 130 (5.41%) | 148 (5.05%) | |
| MHS + SUS | 60 (11.36%) | 290 (12.07%) | 350 (11.94%) | |
| No previous treatment | 119 (22.53%) | 398 (16.56%) | 517 (17.64%) | |
| Substance use in comorbidity, n (%) | ||||
| Alcohol | 55 (10.41%) | 161 (6.70%) | 216 (7.37%) |
Pearson chi2 = 19.50 p= 0.002 SERS ≥ 2, p< 0.05 |
| Cannabis | 27 (5.11%) | 163 (6.78%) | 190 (6.48%) | |
| Cocaine | 19 (3.59%) | 69 (2.87%) | 88 (3.00%) | |
| Other | 9 (1.70%) | 20 (0.82%) | 29 (0.98%) | |
| Polyabuse | 61 (11.55%) | 382 (15.90%) | 443 (15.11%) | |
| No substance use | 357 (67.61%) | 1607 (66.90%) | 1964 (67.03%) | |
| Medical comorbidity, n (%) | ||||
| Present | 250 (47.34%) | 981 (40.84%) | 1231 (42.01%) |
Pearson Chi2 = 8.771 p = 0.003 SRES ≥ 2, p< 0.05 |
| Absent | 278 (52.65%) | 1421 (59.15%) | 1699 (57.98%) | |
| Aggressive behaviour during hospitalization, n (%) | ||||
| Present | 42 (7.95%) | 301 (12.41%) | 343 (11.71%) |
Pearson Chi2 = 8.771 p = 0.003 SRES ≥ 2, p< 0.05 |
| Absent | 486 (92.05%) | 2101 (86.64%) | 2,587 (88.29%) | |
SRES Standardized Residuals
with those people hospitalized for other clinical reasons:
had less frequently been previously hospitalized in an acute psychiatric ward (46.2% vs 60.44%, Pearson chi2 = 36.947, p < 0.001) and treated by a psychiatrist (77.47% vs 83.44%, SRES = -3.26, p < 0.05),
had less frequently been taken into care at a Mental Health Service (MHS) (47.72% vs 57.16%, SRES = -3.95, p < 0.05), but more frequently at a Substance Use Service (5.68% vs 2.83%, SRES = 3.3, p < 0.05) (Pearson chi2 = 38.658, p < 0.001),
presented more frequently a comorbid alcohol abuse (10.41% vs 6.7%, SRES = 2.95, p < 0.05), (Pearson chi2 = 19.573, p = 0.003).
Clinical characteristics of hospitalizations for SR
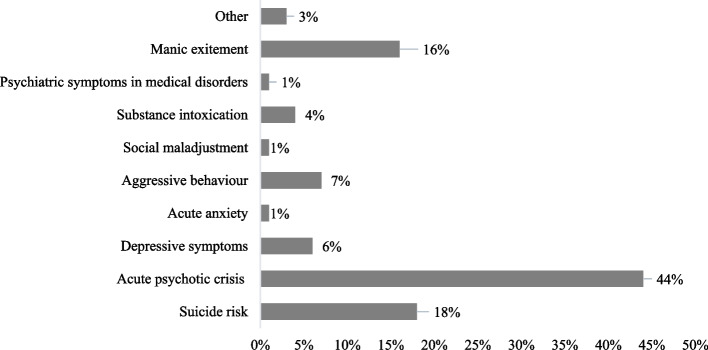
We highlighted that SR was the second reason (18%) for psychiatric hospitalizations in our sample after acute psychotic crisis (Fig. 1).
Fig. 1.
Clinical reasons for psychiatric hospitalizations in SPDC of AUSL-Modena in the study period
Hospitalizations for SR (Table 2) were more frequently voluntary (58% vs 55.24%, Pearson chi2 = 215.41, p < 0.001) and lasted significantly shorter period (t = 6.03, t-test, p < 0.001), also if subjects were involuntarily hospitalized for SR (t = 2.71, t-test, p = 0.003), compared to hospitalizations for other clinical reasons (13.82% vs 9.84%, Pearson chi2 = 6.0, p < 0.014). Hospitalizations for SR were less frequently repeated ones as in the phenomenon of revolving door. During hospitalizations, people with SR less frequently presented aggressive behaviour (12.53% vs 92.04%, Pearson chi2 = 8.771, p = 0.003) and medical comorbidities (40.84% vs 47.34%, Pearson chi2 = 7.524, p = 0.006).
As regards the psychiatric diagnoses at discharge (Table 3), statistically significant differences (Pearson chi2 = 584.68, p < 0.001) between the two groups were observed with a greater frequency of depressive disorders (22.34% vs 5.07%, SRES = 13.1, p < 0.05), personality disorders (41.09% vs 14.11%, SRES = 14.31, p < 0.05) and adjustment disorders (9.46% vs 2.41%, SRES = 7.75, p < 0.05) among subjects hospitalized for SR, whereas we appreciated a greater prevalence of schizophrenia spectrum disorders (49.95% vs 9.46%, SRES = -17.5, p < 0.05), bipolar disorders (14.15% vs 6.43%, SRES = -4.81, p < 0.05) and organic psychotic states (2.99% vs 1.13%, SRES = 2.4, p < 0.05) among patients hospitalized for other clinical reasons. Among the referrals at discharge (Table 5), people with SR were more frequently referred to a private specialist (2.07% vs 0.74%, SRES = 2.81, p < 0.05) or to judicial facility (1.89% vs 0.62%, SRES = 2.87, p < 0.05) (Pearson chi2 = 25.187 p = 0.009). Regarding the pharmacological therapy (Table 3), people hospitalized for SR less frequently were prescribed antipsychotic drugs both orally (79.92% vs 86.84%, Pearson chi2 = 16.81, p < 0.001) and long-acting injection (10.22% vs 31.51%, Pearson chi2 = 97.99, p < 0.001), whereas antidepressants were more frequently used (36.55% vs 9.57%, Pearson chi2 = 255.03, p < 0.001) compared to people hospitalized for other clinical motivations; no significant differences were highlighted between the two groups for other classes of drugs.
Table 3.
Variables related to the discharge from hospitalizations for suicide risk and other clinical reasons
| Variables | Suicide risk (N=528) | Other clinical reasons (N =2,425) | Total (N=2,953) | Statistical test probability |
|---|---|---|---|---|
| Diagnoses at discharge (ICD-9-CM), n (%) | ||||
| Organic psychosis | 6 (1.13%) | 72 (2.99%) | 78 (2.66%) |
Pearson Chi2 = 580.72 p = 0.000 SRES ≥ 2, p < 0.05 |
| Schizophrenia spectrum disorders | 50 (9.46%) | 1200 (49.95%) | 1250 (42.66%) | |
| Bipolar disorders | 34 (6.43%) | 340 (14.15%) | 374 (12.76%) | |
| Depressive disorders | 118 (22.34%) | 122 (5.07%) | 240 (8.19%) | |
| Anxiety disorders | 6 (1.13%) | 13 (0.54%) | 19 (0.64%) | |
| Personality disorders | 217 (41.09%) | 339 (14.11%) | 556 (18.97%) | |
| Substance use disorders | 27 (5.11%) | 129 (5.37%) | 156 (5.34%) | |
| Adjustment disorders | 50 (9.46%) | 58 (2.41%) | 108 (3.68%) | |
| Intellective disabilty | 6 (1.13%) | 60 (2.49%) | 66 (2.25%) | |
| Other | 14 (2.65%) | 69 (2.85%) | 83 (2.81%) | |
| Referral at discharge, n (%) | ||||
| Mental Health Service (MHS) | 148 (28.08%) | 755 (31.43%) | 903 (30.82%) |
Pearson Chi2 = 23.66 p = 0.009 SRES ≥ 2, p < 0.05 |
| Substance Use Service (SUS) | 10 (1.89%) | 27 (1.12%) | 37 (1.26%) | |
| MHS + SUS | 23 (4.36%) | 104 (5.09%) | 127 (4.33%) | |
| Private Specialist | 11 (2.07%) | 18 (0.74%) | 29 (0.99%) | |
| General Physician (GP) | 9 (1.70%) | 50 (2.08) | 59 (2.01%) | |
| Another psychiatric ward | 222 (42.12%) | 959 (39.92%) | 1181 (40.32%) | |
| Protected facility or community | 56 (10.63%) | 322 (13.41%) | 378 (12.91%) | |
| Non-psychiatric hospital ward or facility | 73 (13.83%) | 386 (15.92%) | 459 (2.74%) | |
| Non-psychiatric facility | 10 (1.89%) | 41 (1.70%) | 51 (1.74%) | |
| Judicial facility | 10 (1.89%) | 15 (0.62%) | 25 (0.85%) | |
| Other | 11 (2.08%) | 47 (1.95%) | 58 (1.98%) | |
| Prescribed drugs, N (%) | ||||
|
Oral antipsychotic drugs: present |
106 (20.07%) | 316 (13.15%) | 422 (14.40%) |
Pearson Chi2 = 16.813 p = 0.00 SRES ≥ 2, p < 0.05 |
| absent | 422 (79.92%) | 2086 (86.84%) | 2508 (85.59%) | |
|
LAI antipsychotic drugs: present |
474 (89.77%) | 1645 (68.48%) | 2119 (72.32%) |
Pearson Chi2 = 97.99 p = 0.000 SRES ≥ 2, p < 0.05 |
| absent | 54 (10.22%) | 757 (31.51%) | 811 (27.67%) | |
|
Antidepressant drugs: present |
335 (63.44%) | 2172 (90.42%) | 2507 (85.56%) |
Pearson Chi2 = 255.028 p =0.00 SRES ≥ 2, p < 0.05 |
| absent | 193 (36.55%) | 230 (9.57%) | 423 (14.43%) | |
|
Mood stabilizer drugs: present |
418 (79.16%) | 1892 (78.76%) | 2310 (78.83%) |
Pearson Chi2 = 0.041 p = 0.83 |
| absent | 110 (20.83%) | 510 (21.23%) | 620 (21.16%) | |
|
Benzodiazepines: present |
139 (26.32%) | 686 (28.55%) | 825 (28.15%) |
Pearson Chi2 = 1.067 p = 0.30 |
| absent | 389 (73.67%) | 1716 (71.44%) | 2105 (71.84%) | |
SRES Standardized Residuals
Table 5.
Correlation between SR modalities and SR pre-existing conditions, referral at discharge and sex
| Variables | Suicidal ideation | Attempted suicide by ingesting drugs | Attempted suicide by violent means | Statistical test Probability |
|---|---|---|---|---|
| SR pre-existing conditions | ||||
| Depressive disorders | 45 | 42 | 51 |
Pearson Chi2 = 42.83 p = 0.002 SRES ≥ 2 p < 0.05 |
| Personality disorders | 80 | 38 | 46 | |
| Psychosis | 10 | 11 | 11 | |
| Eating disorders | 2 | 2 | 3 | |
| Alcohol/substance use | 24 | 14 | 5 | |
| Mourning | 7 | 5 | 3 | |
| Economic and work difficulties | 9 | 10 | 4 | |
| Precarious social conditions | 14 | 5 | 4 | |
| Family relationship problems | 18 | 28 | 16 | |
| Medical illness | 5 | 1 | 5 | |
| Unknown | 0 | 3 | 0 | |
| Referral at discharge | ||||
| Other | 6 | 4 | 1 |
Pearson Chi2 = 41.32 p = 0.001 SRES ≥ 2 p < 0.05 |
| MHS | 50 | 59 | 37 | |
| SUS | 8 | 3 | 0 | |
| MHS + SUS | 12 | 7 | 4 | |
| Private specialist | 8 | 3 | 0 | |
| GP | 5 | 2 | 2 | |
| Psychiatric ward | 88 | 62 | 67 | |
| Psychiatric facility or community | 23 | 14 | 20 | |
| Non-psychiatric hospital ward or facility | 13 | 5 | 9 | |
| Judicial facility | 1 | 1 | 8 | |
| Sex | ||||
| Male | 128 | 63 | 86 |
Pearson chi2 = 16.96 p = 0.000 SRES ≥ 2 p < 0.05 |
| Female | 86 | 96 | 62 | |
At the multiple logistic regression between motivation for hospitalization (Suicide Risk = 1; Other clinical reasons = 0) and the other selected variables, the following variables were statistically significantly associated with Odds Ratio > 1 (Table 4):
the diagnoses at discharge of personality disorder (OR = 4.11; 95% Conf. Int: 1.96—8.65; p < 0.001), depressive disorder (OR = 4.70; 95% Conf. Int: 2.19 -10.07; p < 0.001) and adjustment disorder (OR = 4.40; 95% Conf. Int: 1.95—9.91; p < 0.001),
the absence of support administrator (OR = 2.64; 95% Conf. Int: 1.75—3.98; p < 0.001).
Table 4.
Multiple logistic regression (forward and backward stepwise) between suicide risk (= 1) and other clinical reasons (= 0) for hospitalizations
| Variables | OR | IC 95% | p-value |
|---|---|---|---|
| Diagnoses at discharge | |||
| Personality disorder | 4.11 | 1.96—8.65 | p = 0.000 |
| Depressive disorder | 4.70 | 2.19 -10.07 | p = 0.000 |
| Adjustment disorder | 4.40 | 1.95—9.91 | p = 0.000 |
| Schizophrenia spectrum disorder | 0.25 | 0.12—0.55 | p = 0.001 |
| Administration of support | |||
| Absence | 2.64 | 1.75—3.98 | p = 0.000 |
| Duration of hospitalization | 0.98 | 0.96—0.99 | p = 0.000 |
| Medical comorbidity | |||
| Absence | 0.74 | 0.60—0.92 | p = 0.008 |
The following variables were statistically significantly associated with Odds Ratio < 1:
the diagnosis at discharge of schizophrenia spectrum disorder (OR = 0.25; 95% Conf. Int: 0.12—0.55; p = 0.001),
duration of hospitalization (OR = 0.98; 95% Conf. Int: 0.96—0.99; p < 0.001),
the lack of medical comorbidity (OR = 0.74; 95% Conf. Int: 0.60—0.92; p = 0.008).
Characteristics of SR modality and pre-existing conditions
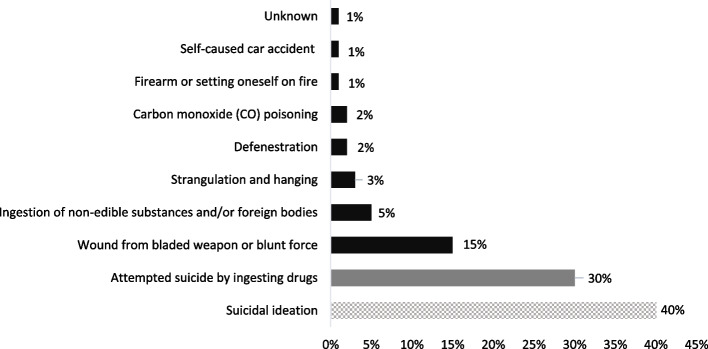
We identified the following SR within our sample (Fig. 2):
Fig. 2.
Modality of SR in our sample: suicidal ideation, attempted suicide by ingesting drugs and by violent means
40% of subjects presented suicidal ideation.
30% attempted suicide by ingesting drugs.
- 30% attempted suicide by violent means:
- bladed weapon or blunt instrument (15%)
- ingestion of non-edible substances and/or foreign bodies (5%)
- strangulation and hanging (3%)
- carbon monoxide (CO) poisoning (2%)
- defenestration (2%)
- self-caused car accident (1%)
- firearm or setting oneself on fire (1%).
Regarding the SR pre-existing conditions, we underscored the following ones:
68% psychiatric disorders, in particular Depression, Personality Disorder and Bipolar Disorder.
12% family relationship problems.
8% use of alcohol or substances.
4% precarious social conditions.
4% economic and work difficulties.
2% medical illness.
The three SR modalities (suicidal ideation, ingestion of drugs and use of violent means) we selected correlated in a statistically significant way with some pre-existing conditions (Pearson Chi = 42.83; p = 0.002) and with specific post-discharge programs (Pearson Chi = 50.07; p = 0.001) (Table 5):
suicidal ideation with personality disorders and pathological use of alcohol, referral to SUS or to a private specialist;
ingestion of drugs with relational and family problems, referral to MHS;
use of violent means with depressive disorders, referral to communities or psychiatric residential facilities.
Males in our sample presented more suicidal ideation whereas females more frequently presented drug ingestion (Pearson Chi = 16.96; p < 0.001).
Discussion
The results of our study, which analyzed the demographic and clinical characteristics of individuals hospitalized in an acute psychiatric ward over a 6-year period for suicide risk, appear generally in line with literature. SR represented the second leading cause of hospitalization (18%), in particular among females. Hospitalizations for SR were more frequently voluntary and the psychiatric disorders more frequently associated with SR were depressive, personality and adjustment disorders. SR was often complicated by family/relationship problems and alcohol/substance use. As regards the demographic characteristics of our sample, the most relevant result is the prevalence of females, which confirms the literature data concerning a higher prevalence of suicide attempts among women [51, 52]. Many studies highlight that females survive suicide attempts more often than males because they use less lethal means and, even when they use the same means, the outcome is less lethal [11, 12]. In this regard, the authors highlighted a greater prevalence of depressive disorders, borderline personality disorder and PTSD in women with suicide risk compared to men who presented prevalent substance use disorder [14, 15]. We did not underscore statistically significant differences regarding the age and nationality between the subjects with SR and others. In our study, the age of the subjects at risk of suicide was around 41 years, data confirmed by the literature [53]. The majority of subjects were employees or students. In this regard, the literature underscores that a precarious work can be considered a stress condition if compared to a more stable job [54]. Furthermore, a study indicates workplace bullying as an important cause of suicide risk among employees [55]. Other studies, however, do not confirm this data, identifying unemployment as one of the main risk factors for attempted suicide, following the resulting financial and social difficulties [56]. Among students, the risk of suicide has increased considerably in recent years, probably due to both the phenomenon of bullying and the increase in depressive symptoms among young people, as well as the difficulty of adapting to exam stress and/or social and family pressure [9, 57, 58]. We also found that the majority of subjects in our sample who presented a SR did not benefit from the support of an administrator, a fact consistent with the great social and economic support that derives from this function. As regards housing condition, the majority of subjects with SR lived with their stepfamily, where, according to some authors, there could be an increase in stressful events such as caring for children and/or financial worries or came from institutions such as prison or judicial institutions, data confirmed by the literature [59, 60].
The majority of subjects did not have a previous hospitalization in a psychiatric environment. This data is in line both with the lower frequency of treatment and care in local psychiatric services of subjects at SR in our sample and with the lower number of repeated hospitalizations for SR of the same subjects in the study period. Among our subjects with SR, treatment and care at SUS was frequent, highlighting how the use of substances of abuse, in particular alcohol, represents an important condition associated with SR. In fact, the pathological use of alcohol can represent an important risk factor for suicide through disinhibition, impulsivity and reduced judgment, but it can also be used as a means to alleviate the discomfort associated with committing a suicidal act [60]. A review showed that both alcohol and drug use disorders are strongly associated with suicide: heavy alcohol users have a five times greater risk of suicide than to social drinkers [60]. Our study highlights that subjects with SR were more often voluntarily hospitalized than involuntarily and for a shorter period than other subjects hospitalized for other reasons. When subjects at risk of suicide were involuntarily hospitalized, the duration of involuntary treatment was shorter than that of subjects hospitalized for other clinical reasons. The clinical reasons for involuntary hospitalizations such as aggressive behaviour and acute psychotic crisis were hardly present in hospitalizations for SR. Even the diagnoses at discharge were consistent with the reasons for hospitalization: in voluntary hospitalizations for SR, depressive, personality, adjustment were prevalent, whereas schizophrenia spectrum disorders and bipolar disorders prevailed among hospitalizations for other clinical reasons as well as in involuntary hospitalizations. This result is consistent with a meta-analysis [61], which highlighted that voluntary and involuntary hospitalizations respond to different clinical needs of two populations.
Regarding repeated hospitalizations, our study highlights how the risk of suicide does not represent a risk factor for subsequent hospitalizations. In our sample, subjects with SR were re-hospitalized less frequently than those who are hospitalized for other clinical reasons. Furthermore, the individuals in our sample repeatedly hospitalized were more frequently treated and cared at outpatient services, especially MHS or more than one service, were usually hospitalized for hetero-directed aggression, showed aggressive behavior during hospitalization, were prescribed Long-Acting Injectable (LAI) therapy and suffered from schizophrenia spectrum disorders. Among these subjects, we found a lower suicidal risk as reason for hospitalization, an observation consistent with literature data [62], suggesting different clinical needs.
We highlighted an increase in the number of hospitalizations for SR in the pre-pandemic period, i.e. until 01/03/2020, and a reduction in the two subsequent periods, pandemic and post-emergency. In particular, we observed the highest number of hospitalizations for SR in 2021 and the lowest number in 2022 compared to the time period considered, suggesting that the impact of Covid-19 pandemic decreased SR. According to a recent study [63], during the lockdown there was a decrease in hospitalizations for suicidal behaviors probably due to the general recommendation to seek healthcare only in urgent cases for the risk of contagion. A meta-analysis of 54 studies instead highlighted an increase in rates of suicidal behavior during the pandemic compared to rate in the pre-pandemic [64].
The literature is therefore not in agreement in highlighting the rate of suicidal behavior during the pandemic period: on the one hand it seems to have increased due to symptoms related to stress, economic difficulties, housing instability, unemployment, fragile health, organic pathologies [25], on the other hand it seems to have decreased due to greater social support, resilience, positive feelings and faith, which have been identified as protective factors for suicide risk [65].
Analysing the discharge diagnoses of our sample, we underscored that the most frequent diagnoses among subjects with SR were Personality, Depressive and Adjustment disorder. A significant number of discharged subjects suffered from borderline personality disorder, in line with what emerges from the literature, according to which people affected by this disorder have a greater risk of suicide attempts and self-harm probably due to an increase in impulsivity and self-directed aggression, compared to subjects suffering from other psychiatric pathologies [66]. The literature also confirms how depressive symptoms and loss of hope represent an important cause of attempted suicide [67].
Other studies confirmed that the risk of suicide in individuals with first- psychotic episode is high and that high rates of premature mortality, particularly from suicide, can occur in the early stages of schizophrenia [68]. Numerous studies confirm that bipolar disorder is burdened by a high risk of suicide [69]. Consistently with the discharge diagnoses, the subjects hospitalized for SR in our sample more frequently were prescribed antidepressant therapy than other types of psychoactive therapy, while antipsychotics were less frequently prescribed both orally and in long-acting formulations, due to greater frequency of depressive disorders among subjects at risk of suicide in our sample. As confirmed by the literature, antidepressants are effective in the treatment of depressed individuals, particularly in individuals who may be at risk of suicide, such as those suffering from Major Depressive Disorder [70]. However, it should be considered that the use of antidepressant therapy may determine, especially in the first weeks of treatment, an increased risk of suicide attempts due to the initial stimulation and disinhibition effect not associated with a real antidepressant effect, which is particularly worrying in child and adolescent population [71].
Upon discharge, the subjects hospitalized for suicide risk were mainly referred to another psychiatric ward for treatment continuation. This result could explain the shorter length of stay in our ward of subjects with RS compared to those hospitalized for other clinical reasons, who were more frequently refer at discharge to MHS or psychiatric residential facilities/communities. This data is confirmed in the literature, suggesting a certain caution in discharging subjects with SR at home due to greater risk of suicide within three months of discharge [72]. Furthermore, more frequently than subjects hospitalized for other clinical reasons, subjects with SR were referred for discharge to a private specialist, as requested by them, probably with the aim of promoting continuity in therapeutic relationship.
We highlighted different risk modalities, which we divided into suicidal ideation (40%), ingestion of drugs (30%) and use of violent highly lethal means (30%). The majority of subjects with RS were hospitalized for suicidal ideation, represented by thoughts relating to concrete and structured plans for death. This result is significant since suicidal ideation is usually followed by a suicide attempt; therefore, hospitalization of subjects with suicidal ideation represents a fundamental preventive measure [73]. Several meta-analyses confirm the strong correlation between suicidal ideation and subsequent completed suicide [74, 75]. In our sample, 30% of the subjects attempted suicide through the ingestion of drugs. A study highlights that suicide attempts through the ingestion of drugs represent a quarter of all deaths by suicide [76]. Among the drugs used by the subjects are mainly benzodiazepines, antidiabetic drugs and paracetamol: the increased use of these molecules probably due to due to ease access and use as well as their lethality is confirmed by literature [77, 78]. Suicide attempts with firearms are less represented in our sample, especially due to the difficulty of accessing weapons, contrary to what happens in the United States, where this method is the main one used to commit suicide [79]. The use of violent means among our subjects suggests a lethality so high as to indicate in the majority of cases a failed suicide. Among the violent means used by our sample, injuries from a sharp weapon and blunt force were the most frequent (15%), followed by the ingestion of inedible substances (5%) and attempted strangulation/hanging (3%). Among the conditions pre-existing the risk of suicide, we identified psychiatric pathology as the most frequent condition in our sample (68%), result confirmed by literature [26]. Among psychiatric pathologies, subjects who presented suicide behaviour were mainly affected by borderline personality, depressive and adjustment disorders. Numerous studies underscore the association between borderline personality disorder and suicide attempt, especially in comorbidity with major depressive disorder [27, 80, 81]. The risk of suicide in people affected by bipolar disorder is 20 to 30 times greater than in the general population [82]. We cannot underscore similar result although some subjects in our sample probably suffered from depressive episodes in bipolar disorders. However, 12% of the subjects in our sample presented suicide behaviour in concomitant with pre-existing family relationship problems: the literature confirms these results [83], highlighting how family or spouse quarrels, as well as separations, represent one of the main risk factors for suicide. Only a small percentage of our sample (2%) presented among pre-existing conditions being affected by a medical illness. This data is conditioned by the psychiatric setting where people affected by medical disorders are not hospitalized and is apparently in contrast with the literature, according to which numerous chronic pathologies represent a risk factor for suicide attempts, in particular neurological pathologies and those associated with chronic pain [84]. A report of 42 cases [85] found that people with greater burdens due to the association of psychiatric illness, physical illness and functional limitations were more likely to attempt suicide. Only 8% of the subjects in our sample present a risk of suicide in concomitance with substance use; this data is also in contrast with the literature, which instead confirms that pathological alcohol/substance use can represent both a risk factor and a lethal modality [60].
We highlighted that the three modalities of suicidal risk, i.e. self-harm ideation, ingestion of drugs and use of violent means, were associated in a statistically significant way with different pre-existing conditions and differently impacted on the referral at discharge from the ward. In particular, depressive disorders correlate with the use of violent means for committing suicide. A study confirms how the use of a cutting weapon is associated with mood disorders, in particular depressive disorders, and identifies the neck and abdomen as the areas most affected in the event of self-inflicted wounds [86]. Among the violent means, the literature highlights how hanging, due to its lethality and easy accessibility, is one of the most used methodology for suicide in depressed subjects [87]. A retrospective investigation highlights how defenestration is the most used methodology among subjects suffering from depressive and bipolar disorders, compared to schizophrenia [88]. In our sample, suicidal ideation was statistically significantly correlated with personality disorder and pathological use of alcohol, in line with literature which confirms how suicidal ideation frequently manifests in subjects suffering from personality disorder concomitantly with the occurrence of a negative event [89] and how it is frequently associated with the pathological use of alcohol [90].
The subjects in our sample who had family relationship problems attempted suicide mainly by ingesting drugs, data confirmed by literature, which highlights that paracetamol, analgesics and benzodiazepines are the most common drugs used for suicide attempt due to the ease of finding them [91, 92]. In our sample, women attempted suicide by taking drugs, whereas men presented more frequently suicidal ideation, as highlighted by the literature [93]. In particular, suicidal ideation is closely related to pathological use of alcohol according to literature [94].
Limitations and advantages of the study
This study has a number of limitations. The monocentric design of this study does not permit to generalize the results obtained to the entire Italian and international panorama. Having exclusively analyzed hospitalizations in an acute psychiatric ward, it is not possible to draw conclusions on variations regarding the totality of psychiatric hospitalizations, which include many other hospitals and residential facilities. The retrospective study design does not allow us causal inferences of the observed variables, for which prospective studies are necessary. Finally, as regards demographic variables such as work activity, education and living conditions, it was not possible to find a large percentage of data, as they were not available in the digital archives consulted. Regarding the advantages of our study, we highlight the long observation period, the large amount of data and the retrospective cohort study design, which is appropriate to identify individuals exposed to suicide risk factors, which allowed us to analyze in detail a sufficiently large sample of people with SR in a long observation period. Another advantage is the real context of the study, which provides data from daily clinical practice.
Conclusions
Our study highlights that suicide risk (SR) is more frequent among female population, in subjects treated in SUS and is frequently associated with depressive, personality and adjustment disorders. Subjects with SR were more often hospitalized in voluntary regime. In our sample, SR was the second cause of hospitalization after acute psychotic crisis and did not represent a cause for repeated hospitalizations in the study period. We found three modalities of SR which were related with psychiatric conditions: suicidal ideation (40%) often related to Personality and Substance Use Disorder, ingestion of drugs (30%) related to family relationship problems and use of violent means (30%) related to depressive disorders. Our study confirmed the literature data, suggesting that suicidal behaviour is the product of the interaction of many factors, such as psychiatric, somatic, chronic diseases, painful/traumatic life events or even social factors that occurred in a crucial moment of life in vulnerable individuals. Future prospective research may provide more comprehensive results regarding the correlations between demographic and clinical factors and suicide risk. The identification of subjects at risk represents the first step of a continuous and structured preventive multi-professional intervention, aimed at preventing and reducing suicidal behaviour. Although there is no effective algorithm to prevent suicide in clinical practice, a better recognition and understanding of clinical, psychological, sociological and biological factors can facilitate the identification of people at high risk and help the implementation of the most suitable and effective preventive and treatment programs.
Acknowledgements
The authors thank Orianna Raggioli for her precious help in language revision.
Abbreviations
- SR
Suicide Risk
- SPDC
Service for Psychiatric Diagnosis and Care
- WHO
World Health Organization
- MDD
Major Depressive Disorder
- BPD
Borderline personality disorder
- PTSD
Post-Traumatic Stress Disorder
- SUD
Substance Use Disorder
- SA
Support Administrator
- VHs
Voluntary hospitalizations
- IHs
Involuntary hospitalizations
- SD
Standard Deviation
- SRES
Standardized Residuals
- MHS
Mental health Service
- LAI
Long-Acting Injectable
- SUS
Substance Use Service
Authors’ contributions
Conceptualization, R.D., C.S. and M.R.; methodology, R.D., and C.S.; software R.D., M.R.; validation, R.D., M.R., and P.F.; formal analysis, R.D., and M.R.; investigation R.D., C.S. and M.R.; data curation, R.D., C.S. and M.R.; writing—original draft preparation, R.D. C.S. and P.F.; writing—review and editing, R.D., P.F., S.R.; supervision, S.R. All authors have read and agreed to the published version of the manuscript.
Funding
No funding.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the North Emilia Area Vasta (Prot. 306/2022/AOU) with subsequent amendment for extension of the period examined (Prot. 10826/2023) and authorized by the AUSL- Modena (Prot. no. 688; 27/4/2023). Consent for publication is not applicable. If the informed consent is waived, we would require full name of committee that waived the informed consent. As the study was conducted retrospectively, it was not possible to obtain written informed consent from the enrolled subjects, in accordance with the European GDPR 679/2016 and General Authorization n. 9/2016, extended by Provision n. 424/2018. Data access was granted to the study manager and collaborators, who were bound by confidentiality and data processing obligations under applicable regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Suicide. https://www.emro.who.int/health510topics/suicide/feed/atom.html. Accessed 21 Feb 2024.
- 2.Vanlaere L, Bouckaert F, Gastmans C. Care for suicidal older people: current clinical-ethical considerations. J Med Ethics. 2007. 10.1136/jme.2006.017897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hegerl U. Prevention of suicidal behavior. Dialogues Clin Neurosci. 2016. 10.31887/DCNS.2016.18.2/uhegerl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martinengo L, Van Galen L, Lum E, Kowalski M, Subramaniam M, Car J. Suicide prevention and depression apps’ suicide risk assessment and management: a systematic assessment of adherence to clinical guidelines. BMC Med. 2019. 10.1186/s12916-019-1461-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harmer B, Lee S, Duong TVH, Saadabadi A. Suicidal ideation. 2024. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed]
- 6.Cipriano A, Cella S, Cotrufo P. Nonsuicidal self-injury: a systematic review. Front Psychol. 2017. 10.3389/fpsyg.2017.01946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ekeberg Ø, Hem E. Chronically suicidal? Tidsskr Nor Laegeforen. 2017. 10.4045/tidsskr.17.0630. [DOI] [PubMed] [Google Scholar]
- 8.Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, Nock MK. Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. J Abnorm Psychol. 2017. 10.1037/abn0000273. [DOI] [PubMed] [Google Scholar]
- 9.Berman AL. Risk factors proximate to suicide and suicide risk assessment in the context of denied suicide ideation. Suicide Life Threat Behav. 2018. 10.1111/sltb.12351. [DOI] [PubMed] [Google Scholar]
- 10.Freeman A, Mergl R, Kohls E, Székely A, Gusmao R, Arensman E, Koburger N, Hegerl U, Rummel-Kluge C. A cross-national study on gender differences in suicide intent. BMC Psychiatry. 2017. 10.1186/s12888-017-1398-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Värnik A, Kõlves K, van der Feltz-Cornelis CM, Marusic A, Oskarsson H, Palmer A, Reisch T, Scheerder G, Arensman E, Aromaa E, Giupponi G, Gusmäo R, Maxwell M, Pull C, Szekely A, Sola VP, Hegerl U. Suicide methods in Europe: a gender-specific analysis of countries participating in the “European Alliance Against Depression.” J Epidemiol Community Health. 2008. 10.1136/jech.2007.065391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cibis A, Mergl R, Bramesfeld A, Althaus D, Niklewski G, Schmidtke A, Hegerl U. Preference of lethal methods is not the only cause for higher suicide rates in males. J Affect Disord. 2012. 10.1016/j.jad.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 13.Bommersbach TJ, Rosenheck RA, Petrakis IL, Rhee TG. Why are women more likely to attempt suicide than men? Analysis of lifetime suicide attempts among US adults in a nationally representative sample. J Affect Disord. 2022. 10.1016/j.jad.2022.05.096. [DOI] [PubMed] [Google Scholar]
- 14.Brezo J, Paris J, Tremblay R, Vitaro F, Hébert M, Turecki G. Identifying correlates of suicide attempts in suicidal ideators: a population-based study. Psychol Med. 2007. 10.1017/S0033291707000803. [DOI] [PubMed] [Google Scholar]
- 15.Monnin J, Thiemard E, Vandel P, Nicolier M, Tio G, Courtet P, Bellivier F, Sechter D, Haffen E. Sociodemographic and psychopathological risk factors in repeated suicide attempts: gender differences in a prospective study. J Affect Disord. 2012. 10.1016/j.jad.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Pompili M. Exploring the phenomenology of suicide. Suicide Life Threat Behav. 2010. 10.1521/suli.2010.40.3.234. [DOI] [PubMed] [Google Scholar]
- 17.Parra-Uribe I, Blasco-Fontecilla H, Garcia-Parés G, Martínez-Naval L, Valero-Coppin O, Cebrià-Meca A, Oquendo MA, Palao-Vidal D. Risk of re-attempts and suicide death after a suicide attempt: A survival analysis. BMC Psychiatry. 2017. 10.1186/s12888-017-1317-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Demesmaeker A, Chazard E, Hoang A, Vaiva G, Amad A. Suicide mortality after a nonfatal suicide attempt: a systematic review and meta-analysis. Aust N Z J Psychiatry. 2022. 10.1177/00048674211043455. [DOI] [PubMed] [Google Scholar]
- 19.Salway T, Ross LE, Fehr CP, Burley J, Asadi S, Hawkins B, Tarasoff LA. A systematic review and meta-analysis of disparities in the prevalence of suicide ideation and attempt among bisexual populations. Arch Sex Behav. 2019. 10.1007/s10508-018-1150-6. [DOI] [PubMed] [Google Scholar]
- 20.Stack S, Scourfield J. Recency of divorce, depression, and suicide risk. J Fam Issues. 2015. 10.1177/0192513X1349482. [Google Scholar]
- 21.Kumar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health. 2021. 10.1080/09638237.2020.1757052. [DOI] [PubMed] [Google Scholar]
- 22.Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019-a perfect storm? JAMA Psychiat. 2020. 10.1001/jamapsychiatry.2020. [DOI] [PubMed] [Google Scholar]
- 23.Kontaxakis VP, Christodoulou GN, Mavreas VG, Havaki-Kontaxaki BJ. Attempted suicide in psychiatric outpatients with concurrent physical illness. Psychother Psychosom. 1988. 10.1159/000288121. [DOI] [PubMed] [Google Scholar]
- 24.Devries KM, Mak JY, Child JC, Falder G, Bacchus LJ, Astbury J, Watts CH. Childhood sexual abuse and suicidal behavior: a meta-analysis. Pediatrics. 2014. 10.1542/peds.2013-2166. [DOI] [PubMed] [Google Scholar]
- 25.Elbogen EB, Lanier M, Blakey SM, Wagner HR, Tsai J. Suicidal ideation and thoughts of self-harm during the COVID-19 pandemic: The role of COVID-19-related stress, social isolation, and financial strain. Depress Anxiety. 2021. 10.1002/da.23162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tidemalm D, Långström N, Lichtenstein P, Runeson B, Reulbach, Bleich. Risk of suicide after suicide attempt according to coexisting psychiatric disorder: Swedish cohort study with long term follow-up. BMJ. 2008; 10.1136/bmj.a2205. [DOI] [PMC free article] [PubMed]
- 27.Soloff PH, Lynch KG, Kelly TM, Malone KM, Mann JJ. Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. Am J Psychiatry. 2000. 10.1176/appi.ajp.157.4.601. [DOI] [PubMed] [Google Scholar]
- 28.Patton GC. Mortality in eating disorders. Psychol Med. 1988. 10.1017/s0033291700009879. [DOI] [PubMed] [Google Scholar]
- 29.Tolstrup K, Brinch M, Isager T, Nielsen S, Nystrup J, Severin B, Olesen NS. Long-term outcome of 151 cases of anorexia nervosa. The Copenhagen Anorexia Nervosa Follow-Up Study. Acta Psychiatr Scand. 1985. 10.1111/j.1600-0447.1985.tb02537.x. [DOI] [PubMed] [Google Scholar]
- 30.Stack S, Lester D. The effect of religion on suicide ideation. Soc Psychiatry Psychiatr Epidemiol. 1991. 10.1007/BF00795209. [DOI] [PubMed] [Google Scholar]
- 31.Qin P, Mortensen PB. The impact of parental status on the risk of completed suicide. Arch Gen Psychiatry. 2003. 10.1001/archpsyc.60.8.797. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization. Comprehensive mental health action plan 2013–2030. 2021. https://www.who.int/publications/i/item/9789240031029. Accessed 21 Feb 2024.
- 33.Sarchiapone M, Mandelli L, Iosue M, Andrisano C, Roy A. Controlling access to suicide means. Int J Environ Res Public Health. 2011. 10.3390/ijerph8124550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Okolie C, Wood S, Hawton K, Kandalama U, Glendenning AC, Dennis M, Price SF, Lloyd K, John A. Means restriction for the prevention of suicide by jumping. Cochrane Database Syst Rev. 2020. 10.1002/14651858.CD013543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Niederkrotenthaler T, Herberth A, Sonneck G. Der, “Werther-Effekt”: Mythos oder Realität? [The “Werther-effect”: legend or reality?]. Neuropsychiatr. 2007;21(4):284–90. [PubMed] [Google Scholar]
- 36.Cipriani A, Hawton K, Stockton S, Geddes JR. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ; 10.1136/bmj.f3646. [DOI] [PubMed]
- 37.Vita A, De Peri L, Sacchetti E. Lithium in drinking water and suicide prevention: a review of the evidence. Int Clin Psychopharmacol. 2015. 10.1097/YIC.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 38.Frogley C, Taylor D, Dickens G, Picchioni M. A systematic review of the evidence of clozapine’s anti-aggressive effects. Int J Neuropsychopharmacol. 2012. 10.1017/S146114571100201X. [DOI] [PubMed] [Google Scholar]
- 39.Girardi P, Pompili M, Innamorati M, Mancini M, Serafini G, Mazzarini L, Del Casale A, Tatarelli R, Baldessarini RJ. Duloxetine in acute major depression: review of comparisons to placebo and standard antidepressants using dissimilar methods. Hum Psychopharmacol. 2009. 10.1002/hup.1005. [DOI] [PubMed] [Google Scholar]
- 40.Duman RS. Ketamine and rapid-acting antidepressants: a new era in the battle against depression and suicide. F1000Res. 2018; 10.12688/f1000research.14344.1. [DOI] [PMC free article] [PubMed]
- 41.Canuso CM, Singh JB, Fedgchin M, Alphs L, Lane R, Lim P, Pinter C, Hough D, Sanacora G, Manji H, Drevets WC. Efficacy and safety of intranasal esketamine for the rapid reduction of symptoms of depression and suicidality in patients at imminent risk for suicide: results of a double-blind, randomized placebo-controlled study. Am J Psychiatry. 2018. 10.1176/appi.ajp.2018.17060720. [DOI] [PubMed] [Google Scholar]
- 42.Angst F, Stassen HH, Clayton PJ, Angst J. Mortality of patients with mood disorders: follow-up over 34–38 years. J Affect Disord. 2002. 10.1016/s0165-0327(01)00377-9. [DOI] [PubMed] [Google Scholar]
- 43.Fusar-Poli L, Natale A, Amerio A, Cimpoesu P, Grimaldi Filioli P, Aguglia E, Amore M, Serafini G, Aguglia A. Neutrophil-to-Lymphocyte, Platelet-to-Lymphocyte and Monocyte-to-Lymphocyte Ratio in Bipolar Disorder. Brain Sci. 2021. 10.3390/brainsci11010058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ekinci O, Ekinci A. The connections among suicidal behavior, lipid profile and low-grade inflammation in patients with major depressive disorder: A specific relationship with the neutrophil-to-lymphocyte ratio. Nord J Psychiatry. 2017. 10.1080/08039488.2017.1363285. [DOI] [PubMed] [Google Scholar]
- 45.Masango S, Rataemane S, Motojesi A. Suicide and suicide risk factors: a literature review. S Afr Fam Pract. 2008. 10.1080/20786204.2008.10873774. [Google Scholar]
- 46.Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull. 2017. 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- 47.Haney EM, O’Neil ME, Carson S, Low A, Peterson K, Denneson LM, Oleksiewicz C, Kansagara D. Suicide Risk Factors and Risk Assessment Tools: A Systematic Review. Washington (DC): Department of Veterans Affairs (US); 2012. [PubMed] [Google Scholar]
- 48.LEGGE 13 maggio 1978, n. 180. Accertamenti e trattamenti sanitari volontari e obbligatori. https://www.gazzettaufficiale.it/eli/id/1978/05/16/078U0180/sg. Accessed 21 Feb 2024.
- 49.LEGGE 23 dicembre 1978, n. 833 Istituzione del servizio sanitario nazionale. https://www.gazzettaufficiale.it/eli/id/1978/12/28/078U0833/sg. Accessed 21 Feb 2024. [PubMed]
- 50.LEGGE 9 gennaio 2004, n. 6. Introduzione nel libro primo, titolo XII, del codice civile del capo I, relativo all'istituzione dell'amministrazione di sostegno e modifica degli articoli 388, 414, 417, 637 418, 424, 426, 427 e 429 del codice civile in materia di interdizione e di inabilitazione, nonchè relative norme di attuazione, di coordinamento e finali. https://www.gazzettaufficiale.it/eli/id/2004/01/19/004G0017/sg. Accessed 21 Feb 2024.
- 51.Lee GE, Kim JW, Lee KR, Hong DY, Park SO, Kim SY, Baek KJ, Jeon HJ. Vulnerable individuals and changes in suicidal behaviour during the COVID-19 pandemic in Korea. BJPsych Open. 2022. 10.1192/bjo.2022.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mościcki EK. Gender differences in completed and attempted suicides. Ann Epidemiol. 1994. 10.1016/1047-2797(94)90062-0. [DOI] [PubMed] [Google Scholar]
- 53.Henderson JP, Mellin C, Patel F. Suicide - a statistical analysis by age, sex and method. J Clin Forensic Med. 2005. 10.1016/j.jcfm.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 54.Min KB, Park SG, Hwang SH, Min JY. Precarious employment and the risk of suicidal ideation and suicide attempts. Prev Med. 2015. 10.1016/j.ypmed.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 55.Pompili M, Lester D, Innamorati M, De Pisa E, Iliceto P, Puccinno M, Fiori Nastro P, Tatarelli R, Girardi P. Suicide risk and exposure to mobbing. Work. 2008;31(2):237–43. [PubMed] [Google Scholar]
- 56.Skinner A, Osgood ND, Occhipinti JA, Song YJC, Hickie IB. Unemployment and underemployment are causes of suicide. Sci Adv. 2023. 10.1126/sciadv.adg3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim YS, Leventhal BL, Koh YJ, Boyce WT. Bullying increased suicide risk: prospective study of Korean adolescents. Arch Suicide Res. 2009. 10.1080/13811110802572098. [DOI] [PubMed] [Google Scholar]
- 58.Li W, Dorstyn DS, Jarmon E. Identifying suicide risk among college students: A systematic review. Death Stud. 2020. 10.1080/07481187.2019.1578305. [DOI] [PubMed] [Google Scholar]
- 59.Zhong S, Senior M, Yu R, Perry A, Hawton K, Shaw J, Fazel S. Risk factors for suicide in prisons: a systematic review and meta-analysis. Lancet Public Health. 2021. 10.1016/S2468-2667(20)30233-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pompili M, Serafini G, Innamorati M, Dominici G, Ferracuti S, Kotzalidis GD, Serra G, Girardi P, Janiri L, Tatarelli R, Sher L, Lester D. Suicidal behavior and alcohol abuse. Int J Environ Res Public Health. 2010. 10.3390/ijerph7041392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Walker S, Mackay E, Barnett P, Sheridan Rains L, Leverton M, Dalton-Locke C, Trevillion K, Lloyd-Evans B, Johnson S. Clinical and social factors associated with increased risk for involuntary psychiatric hospitalisation: a systematic review, meta-analysis, and narrative synthesis. Lancet Psychiatry. 2019. 10.1016/S2215-0366(19)30406-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fonseca Barbosa J, Gama MJ. The revolving door phenomenon in severe psychiatric disorders: a systematic review. Int J Soc Psychiatry. 2023. 10.1177/00207640221143282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Irigoyen-Otiñano M, Nicolau-Subires E, González-Pinto A, Adrados-Pérez M, Buil-Reiné E, Ibarra-Pertusa L, Albert-Porcar C, Arenas-Pijoan L, Sánchez-Cazalilla M, Torterolo G, Puigdevall-Ruestes M, Llorca-Bofí V. Characteristics of patients treated for suicidal behavior during the pandemic in a psychiatric emergency department in a Spanish province. Rev Psiquiatr Salud Ment. 2023. 10.1016/j.rpsm.2022.03.004. [DOI] [PubMed] [Google Scholar]
- 64.Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021. 10.1016/j.psychres.2021.113998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Papadopoulou A, Efstathiou V, Yotsidi V, Pomini V, Michopoulos I, Markopoulou E, Papadopoulou M, Tsigkaropoulou E, Kalemi G, Tournikioti K, Douzenis A, Gournellis R. Suicidal ideation during COVID-19 lockdown in Greece: prevalence in the community, risk and protective factors. Psychiatry Res. 2021. 10.1016/j.psychres.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Boot K, Wiebenga JXM, Eikelenboom M, van Oppen P, Thomaes K, van Marle HJF, Heering HD. Associations between personality traits and suicidal ideation and suicide attempts in patients with personality disorders. Compr Psychiatry. 2022. 10.1016/j.comppsych.2021.152284. [DOI] [PubMed] [Google Scholar]
- 67.Ribeiro JD, Huang X, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry. 2018. 10.1192/bjp.2018.27. [DOI] [PubMed] [Google Scholar]
- 68.Pompili M, Serafini G, Innamorati M, Lester D, Shrivastava A, Girardi P, Nordentoft M. Suicide risk in first episode psychosis: a selective review of the current literature. Schizophr Res. 2011. 10.1016/j.schres.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 69.Costa Lda S, Alencar ÁP, Nascimento Neto PJ, dos Santos MS, da Silva CG, Pinheiro Sde F, Silveira RT, Bianco BA, Pinheiro RF Jr, de Lima MA, Reis AO, Rolim Neto ML. Risk factors for suicide in bipolar disorder: a systematic review. J Affect Disord. 2015. 10.1016/j.jad.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 70.Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, Fawcett J. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010. 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Müller-Oerlinghausen B, Berghöfer A. Antidepressants and suicidal risk. J Clin Psychiatry. 1999;60(Suppl 2):94–9 discussion 111–6. [PubMed] [Google Scholar]
- 72.Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, Large MM. Suicide Rates After Discharge From Psychiatric Facilities: A Systematic Review and Meta-analysis. JAMA Psychiat. 2017. 10.1001/jamapsychiatry.2017.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry. 1985. 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- 74.Large M, Corderoy A, McHugh C. Is suicidal behaviour a stronger predictor of later suicide than suicidal ideation? A systematic review and meta-analysis. Aust N Z J Psychiatry. 2021. 10.1177/0004867420931161. [DOI] [PubMed] [Google Scholar]
- 75.Hubers AAM, Moaddine S, Peersmann SHM, Stijnen T, van Duijn E, van der Mast RC, Dekkers OM, Giltay EJ. Suicidal ideation and subsequent completed suicide in both psychiatric and non-psychiatric populations: a meta-analysis. Epidemiol Psychiatr Sci. 2018. 10.1017/S2045796016001049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gunnell D, Ho D, Murray V. Medical management of deliberate drug overdose: a neglected area for suicide prevention? Emerg Med J. 2004;21(1):35–8. 10.1136/emj.2003.000935. Erratum in: Emerg Med J. 2004;21(2):268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gunnell D, Murray V, Hawton K. Use of paracetamol (acetaminophen) for suicide and nonfatal poisoning: worldwide patterns of use and misuse. Suicide Life Threat Behav. 2000;30(4):313–26. [PubMed] [Google Scholar]
- 78.Miller TR, Swedler DI, Lawrence BA, Ali B, Rockett IRH, Carlson NN, Leonardo J. Incidence and Lethality of Suicidal Overdoses by Drug Class. JAMA Netw Open. 2020;3(3): e200607. 10.1001/jamanetworkopen.2020.0607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Conwell Y, Duberstein PR, Connor K, Eberly S, Cox C, Caine ED. Access to firearms and risk for suicide in middle-aged and older adults. Am J Geriatr Psychiatry. 2002;10(4):407–16. [PubMed] [Google Scholar]
- 80.Paris J. Suicidality in Borderline Personality Disorder. Medicina (Mex). 2019;55(6):223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yen S, Peters JR, Nishar S, Grilo CM, Sanislow CA, Shea MT, et al. Association of borderline personality disorder criteria with suicide attempts: findings from the collaborative longitudinal study of personality disorders over 10 years of follow-up. JAMA Psychiat. 2021. 10.1001/jamapsychiatry.2020.3598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tsai SY, Lee JC, Chen CC. Characteristics and psychosocial problems of patients with bipolar disorder at high risk for suicide attempt. J Affect Disord. 1999;52(1–3):145–52. [DOI] [PubMed] [Google Scholar]
- 83.da Silva RM, Mangas RM do N, Figueiredo AEB, Vieira LJE de S, de Sousa GS, Cavalcanti AMT de S, et al. The influence of family problems and conflicts on suicidal ideation and suicide attempts in elderly people. Cien Saude Colet. 2015;20(6):1703–10. [DOI] [PubMed] [Google Scholar]
- 84.Hooley JM, Franklin JC, Nock MK. Chronic pain and suicide: understanding the association. 733 Curr Pain Headache Rep. 2014;18(8):435. [DOI] [PubMed] [Google Scholar]
- 85.Conwell Y, Lyness JM, Duberstein P, Cox C, Seidlitz L, DiGiorgio A, et al. Completed suicide among older patients in primary care practices: a controlled study. J Am Geriatr Soc. 2000;48(1):23–9. [DOI] [PubMed] [Google Scholar]
- 86.Oden C, Weinschreider E, Linzie H. Self-inflicted stabbings as nonfatal suicide attempts: a systematic review and case series. J Acad Consult Liaison Psychiatry. 2023;64(3):294–304. 10.1016/j.jaclp.2023.01.002. [DOI] [PubMed] [Google Scholar]
- 87.Biddle L, Donovan J, Owen-Smith A, Potokar J, Longson D, Hawton K, Kapur N, Gunnell D. Factors influencing the decision to use hanging as a method of suicide: qualitative study. Br J Psychiatry. 2010. 10.1192/bjp.bp.109.076349. [DOI] [PubMed] [Google Scholar]
- 88.Meningaud JP, Bertrand JC, Batista D. Traumatologie maxillo-faciale liée aux défenestrations: à propos de 64 cas [Maxillofacial trauma by defenestration: 64 cases]. Rev Stomatol Chir Maxillofac. 2003;104(5):260–4. [PubMed] [Google Scholar]
- 89.Zabihi S, Jones R, Moran P, King M, Osborn D, Pitman A. The association between personality disorder traits and suicidality following sudden bereavement: a national cross-sectional survey. J Pers Disord. 2021. 10.1521/pedi_2021_35_520. [DOI] [PubMed] [Google Scholar]
- 90.Agyapong B, Shalaby R, Eboreime E, Wei Y, Agyapong VIO. Self-reported alcohol abuse and the desire to receive mental health counselling predict suicidal thoughts/thoughts of self-harm among female residents of fort McMurray. Int J Environ Res Public Health. 2022. 10.3390/ijerph192013620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zheng W, Han L, Fan Y, Yi M, Lu X, Yang J, Peng X, Yang Y. Association of mental health status between self-poisoning suicide patients and their family members: a matched-pair analysis. BMC Psychiatry. 2023. 10.1186/s12888-023-04779-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fusaroli M, Pelletti G, Giunchi V, Pugliese C, Bartolucci M, Necibi EN, Raschi E, De Ponti F, Pelotti S, Poluzzi E. Deliberate self-poisoning: real-time characterization of suicidal habits and toxidromes in the food and drug administration adverse event reporting System. Drug Saf. 2023. 10.1007/s40264-022-01269-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rajapakse T, Griffiths KM, Christensen H, Cotton S. A comparison of non-fatal self-poisoning among males and females. Sri Lanka BMC Psychiatry. 2014. 10.1186/s12888-014-0221-z. [DOI] [PMC free article] [PubMed]
- 94.Dong XS, Brooks RD, Brown S, Harris W. Psychological distress and suicidal ideation among male construction workers in the United States. Am J Ind Med. 2022. 10.1002/ajim.23340. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.