Abstract
Rationale & Objective
Given the organ shortage in the United States, increasing living donation is vital to improving access to kidney transplantation, but many donor candidates do not complete the donor evaluation. Our objective was to understand potential living donors’ perceived health and its association with the likelihood of completing the donor evaluation process.
Study Design
Potential donors’ self-reported health was ascertained using the Patient Reported Outcomes Measurement Information System (PROMIS) global physical and mental health and the Davies and Ware Health Perceptions surveys.
Setting & Participants
Potential living donors who expressed interest in donation at a single medical center were recruited prospectively between 2017 and 2022.
Exposure
Donors' self-reported health and health perceptions.
Outcomes
Completion of the donor evaluation.
Analytical Approach
Adjusted linear and logistic regression models were used to examine the association between self-reported health and health perceptions with outcomes.
Results
A total of 1,347 individuals were included for study; 46% (N = 613) were < 40 years of age, 71% (n = 951) were female, 22% (n = 294) were of Hispanic ethnicity, and 16% (n = 215) completed the donor evaluation. The mean PROMIS global physical health (17.0 ± 1.9) and mental health (15.5 ± 2.7) raw scores were higher among donor candidates proceeding to completion of the donor evaluation when compared with those who withdrew early in the process (16.3 ± 2.2 for physical health and 14.9 ± 3.1 for mental health). Every z-score change in the PROMIS physical health score was associated with 1.48-fold higher odds of completing the donor evaluation (95% CI, 1.19-1.85). Fully adjusted models incorporating the PROMIS scores for predicting the completion of donor evaluations had a c-statistic of 0.70. Potential donors’ Davies and Wares health perceptions did not predict the likelihood of completing the donor evaluation in fully adjusted models.
Limitations
Data are derived from a single center and may not generalize to the donor evaluation process at other transplant centers.
Conclusions
Donor candidates’ self-reported physical health may serve as a predictor of the likelihood of completing the donor evaluation process and a potential avenue for future interventions.
Index Words: Living donor, transplantation, mental health, physical health, donor evaluation
Plain Language Summary
This study was designed to understand the health perceptions of living donor candidates. We found that donor candidates’ self-reported physical health strongly predicted their likelihood of completing the donor evaluation process. Further studies are needed to understand whether addressing donors’ self-perceptions of health may increase rates of completion of the donor evaluation.
In 2019, the Advancing American Kidney Health Initiative was launched by the federal government to encourage the pursuit of kidney transplantation as the preferred modality for kidney replacement therapy.1,2 Given the current organ shortage in the United States, meeting this goal would require expansion of access to donors—both deceased and living. However, rates of living donor transplantation have declined since 2005 despite the implementation of multiple policies and programs to address potential barriers to donation—including coverage of donor income loss, travel costs, and dependent care.3,4 Furthermore, many potential living donors ultimately do not complete the evaluation process or decline to donate, even if deemed to be acceptable candidates.5,6
The rates of living donation among candidates who begin the evaluation process have varied in the literature, but have been reported to be as low as 10%.6 Although previous studies identified reasons individuals who had completed the donor evaluation ultimately did not donate,7, 8, 9, 10, 11, 12 potential donors who abort the donor evaluation early (eg, after first contact with the transplant center for screening for absolute contraindications) are likely to be excluded from such studies. It is possible those who do not move forward in the donor evaluation are less healthy and therefore at higher risk for complications after donation. It is also possible that an individual’s perceptions of their own health (eg, reflecting guilt surrounding unhealthy behaviors) may influence their willingness to complete the donor evaluation process or engage with transplant centers in the evaluation process.13, 14, 15 However, one study found that those with healthier lifestyles tended to be more pessimistic about their health.16
The objectives of this study were to examine potential donors’ self-rated physical and mental health and health perceptions (with a particular focus on capturing potential donors early in the evaluation process) and to examine the association between potential donors’ perceived health and the odds of completing the donor evaluation. We hypothesized that less favorable perceived health would predict lower odds of completion of the donor evaluation process.
Methods
Study Population
We performed a prospective study at the University of California San Francisco between 2017 and 2022. At our center, the evaluation process starts with potential donors completing an online screening questionnaire to determine if there are clear medical contraindications to donation (eg, elevated body mass index and presence of insulin-dependent diabetes). Potential donors are also asked to view a video introducing the living donor process online at this stage of the evaluation process. If they complete this online screening questionnaire without having clear contraindications identified, they were able to participate in our research survey by clicking on a link.
After the completion of the online questionnaire, potential donors receive a telephone call from our donor coordinator and are interviewed to identify any other potential contraindications to donation (eg, history of recurrent kidney stones, cancer, and strong family history of early or unexplained cardiac death). If there are none, potential donors are asked to perform initial local laboratory testing and provide 2 self-reported blood pressure measurements. Additional consultations with experts (eg, a hematologist for a clotting propensity and rheumatologist for concern over connective tissue disease) would also be pursued as needed at the discretion of the evaluating clinician at this stage. If no contraindications are identified and the kidney function appears acceptable, potential donors are invited to present for an in-person evaluation and a computed tomography scan is completed. This is also the phase of the evaluation process when potential donors meet the social worker and all members of the transplant team, including a surgeon and nephrologist. After this in-person evaluation, the donor evaluation is considered complete, and the donor is presented to a selection committee. Shortly thereafter, potential donors are notified of the transplant center’s decision surrounding their eligibility to proceed with donation.
Potential donors who clicked on our survey link after passing the initial online questionnaire screen were invited to answer questions about their self-rated physical and mental health and health perceptions (health outlook, resistance to illness, health worry, and sickness orientation). All survey participants were provided with a small gift card in appreciation for their time. Potential donors were informed that their responses on this survey would not be shared with the transplant center and would have no bearing on the clinical evaluation of eligibility for donation.
Potential participants were recruited for study participation before the transplant center made any final decisions about their eligibility for kidney donation. Thus, some potential donors included for study were ultimately deemed ineligible for donation by the clinical teams. We also invited individuals who had previously completed our survey but who ultimately decided to abort the clinical workup as a living kidney donor to complete laboratory testing (serum creatinine and urine albumin to creatinine ratio ascertainment) as part of our research program (not for donation purposes).
The study protocol was approved by the University of California, San Francisco institutional review board. Informed consent was obtained from all participants.
Survey Content
Our survey included questions from the validated Patient Reported Outcomes Measurement Information System (PROMIS) global health survey, which includes questions about the respondent’s physical and mental health (Item S1). This survey has been validated in healthy populations and summative scores derived.17 In addition, we also included questions about individuals’ health perceptions leveraging a validated survey instrument developed by Davies and Ware known as the general health perceptions measures.18 This instrument includes questions about an individual’s health outlook, resistance to illness, health worry or concern, and sickness orientation. All responses were on a Likert scale from 1-5, with higher scores reflecting a more positive outlook. An overall score for each domain was calculated by summing the individual scores for each question within that domain, and average scores were derived.
Outcomes
The primary outcome was whether the potential donor completed the evaluation process. We did not designate donor nephrectomy as our primary outcome because that is influenced by factors outside of the potential donor’s control (eg, whether the intended recipient is ready for a transplant or the selection of an alternative donor candidate to proceed).
A secondary outcome was the predonation 15-year estimate of the risk for kidney failure for donors, which we used as an objective metric of a donor candidate’s health using a validated tool.19 This risk calculator uses the donor candidate’s age, sex, race, eGFR, systolic blood pressure, use of hypertension medication, body mass index, noninsulin dependent diabetes, urine albumin to creatinine ratio, and smoking history (current, former, or never smoker) to compute their risk (as a linear outcome on a percentage scale).
Statistical Analysis
Initially, t tests and χ2 tests were used to compare the responses to our survey based on whether potential donors completed the donor evaluation process.
We used logistic regression to examine the association between perceived health and completion of the donor evaluation, adjusted for age, biological sex, race or ethnicity (by self-report), and relationship to the intended recipient. We included separate models using initially only the PROMIS global and mental health scores as predictors that were adjusted for age, sex, race or ethnicity, and donor relationship to the intended recipient, then repeated analyses including only the 4 Davies and Ware health perception domains, and finally performed a fully adjusted model that included both sets of self-reported health and health perceptions. For comparability across the survey domains and results, all scores were converted to z-scores using the sample mean within models, and outcomes were reported based on a per standard deviation change in the z-score. We explored the c-statistics of these models to assess the discrimination of the health perception responses for the likelihood of completing the donor evaluation process.
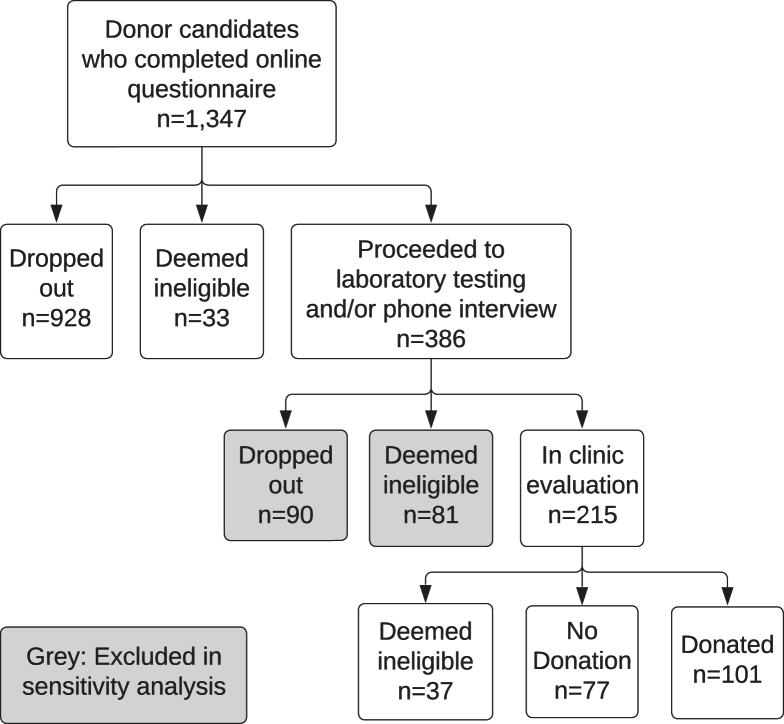
In sensitivity analysis, we excluded donor candidates who aborted the evaluation process early on (n = 171 who dropped out or were deemed ineligible after the telephone interview or laboratory testing, Fig 1) and repeated our logistic regression models.
Figure 1.
Cohort derivation.
To evaluate our secondary outcome, we used linear regression models to examine the association between self-reported physical health, mental health, and each of the domains of the health perceptions survey with the predicted risk of kidney failure for potential donors with such data available in multivariable analysis, adjusted for age, sex, race or ethnicity (by self-report), and relationship to the intended recipient to calculate the predicted risk of end-stage kidney disease (as a % risk over a 15-year period). This risk was only computed among those who had laboratory data (n = 277, which included the 215 donors who presented for in-clinic evaluation and 62 donors who did not move forward to the in-clinic evaluation). Data required for calculating the predicted risk of kidney failure were missing for 40 individuals (n = 35 with missing urine albumin or creatinine ratio, n = 7 with missing body mass index, n = 7 missing serum creatinine, and n = 6 with missing systolic blood pressure) who otherwise had the required elements for an estimate of risk, and hence these missing datapoints were imputed with chained single imputation using data from other donor candidates.
All analyses were conducted using Stata 17 (StataCorp LLC, College Station, TX).
Results
Participants
A total of 1,347 individuals were included for analysis. ∼46% of participants (n = 613) were < 40 years of age, 71% (n = 951) were female, 294 (22%) were Hispanic, and 16% (n = 211) of Asian or Pacific Islander race or ethnicity. About 30% of participants (n = 404) were friends or coworkers, and ∼23% were parents, children, or siblings of the intended recipient (Table 1).
Table 1.
Donor Characteristics by Stage of Completion of the Donor Evaluation Process
| N (Column %), Median (25th and 75th Percentile), or Mean ± SD | Total |
Initial Online Screen |
Proceeded to Laboratory Testing or Telephone Interview |
Presented for In-person Donor Evaluation |
P |
|---|---|---|---|---|---|
| 1,347 (100.0%) | 961 (71.3%) | 171 (12.7%) | 215 (16.0%) | ||
| Dropped out of the evaluation | 1,018 (76) | 928 (97) | 90 (53) | 0 (0) | <0.001 |
| Deemed ineligible for donation | 158 (12) | 33 (3) | 81 (47) | 44 (20) | <0.001 |
| Age (y) | 0.044 | ||||
| <40 | 613 (46) | 437 (45) | 70 (41) | 106 (49) | |
| 40-64 | 607 (45) | 430 (45) | 78 (46) | 99 (46) | |
| 65+ | 127 (9) | 94 (10) | 23 (13) | 10 (5) | |
| Female | 951 (71) | 672 (70) | 130 (76) | 149 (69) | 0.25 |
| Race | 0.17 | ||||
| Asian/Pacific Islander | 211 (16) | 142 (15) | 25 (15) | 44 (20) | |
| Hispanic | 294 (22) | 200 (21) | 46 (27) | 48 (22) | |
| Non-Hispanic Black | 98 (7) | 73 (8) | 9 (5) | 16 (7) | |
| Non-Hispanic White | 744 (55) | 546 (57) | 91 (53) | 107 (50) | |
| Donor relationship to intended recipient | <0.001 | ||||
| Parent | 61 (5) | 37 (4) | 12 (7) | 12 (6) | |
| Child | 110 (8) | 72 (7) | 10 (6) | 28 (13) | |
| Sibling | 135 (10) | 91 (9) | 17 (10) | 27 (13) | |
| Spouse | 104 (8) | 68 (7) | 5 (3) | 31 (14) | |
| Extended family | 192 (14) | 147 (15) | 13 (8) | 32 (15) | |
| Friend/Coworker | 404 (30) | 304 (32) | 50 (29) | 50 (23) | |
| Altruistic | 67 (5) | 34 (4) | 15 (9) | 18 (8) | |
| Other/Unknown | 274 (20) | 208 (22) | 49 (29) | 17 (8) | |
| 15-year predicted ESKD riska (%) | N/A | N/A | 0.08 (0.04-0.13)b | 0.08 (0.05-0.15) | 0.74 |
| How do you rate your overall health? | 3.8 ± 0.8 | 3.8 ± 0.8 | 3.4 ± 0.9 | 4.1 ± 0.8 | <0.001 |
| How well do you carry out your social activities & roles? | 4.0 ± 0.9 | 4.0 ± 0.9 | 3.8 ± 1.0 | 4.1 ± 0.7 | 0.019 |
| PROMIS physical and mental health | |||||
| Global physical health | 16.3 ± 2.3 | 16.3 ± 2.2 | 15.3 ± 2.7 | 17.0 ± 1.9 | <0.001 |
| To what extent are you able to carry out your everyday physical activities? | 4.7 ± 0.6 | 4.7 ± 0.6 | 4.5 ± 0.8 | 4.8 ± 0.5 | <0.001 |
| How would you rate your physical health? | 3.6 ± 0.9 | 3.7 ± 0.9 | 3.1 ± 1.0 | 3.9 ± 0.8 | <0.001 |
| How would you rate your fatigue on average? | 3.9 ± 0.8 | 3.9 ± 0.8 | 3.7 ± 0.9 | 4.1 ± 0.7 | <0.001 |
| How would you rate your pain, with 0 being none and 10 being the worst pain imaginable? | 2.0 ± 2.1 | 2.1 ± 2.1 | 2.3 ± 2.3 | 1.5 ± 1.9 | <0.001 |
| Global mental health | 14.9 ± 3.0 | 14.9 ± 3.1 | 14.3 ± 3.1 | 15.5 ± 2.7 | <0.001 |
| In general, how would you rate your quality of life? | 4.0 ± 0.9 | 4.0 ± 0.8 | 3.7 ± 0.9 | 4.2 ± 0.8 | <0.001 |
| In general, how would you rate your mental health, including your mood and ability to think? | 3.7 ± 1.0 | 3.7 ± 1.0 | 3.6 ± 1.0 | 3.9 ± 0.9 | 0.005 |
| How often are you bothered by emotional problems such as feeling anxious, depressed, or irritable? | 3.4 ± 0.9 | 3.4 ± 0.9 | 3.4 ± 0.9 | 3.4 ± 0.8 | 0.84 |
| In general, how would you rate your satisfaction with your social activities and relationships? | 3.8 ± 1.0 | 3.8 ± 1.0 | 3.7 ± 1.0 | 4.0 ± 0.9 | 0.002 |
| Davies and Ware Health Perceptions | |||||
| Summary score: health outlook | 15.3 ± 2.5 | 15.3 ± 2.5 | 14.6 ± 2.6 | 15.8 ± 2.1 | <0.001 |
| You probably will get sick a lot in the future. | 4.3 ± 0.8 | 4.3 ± 0.8 | 4.1 ± 1.0 | 4.5 ± 0.7 | <0.001 |
| You expect to have better health than others. | 3.6 ± 0.9 | 3.6 ± 0.9 | 3.4 ± 0.9 | 3.7 ± 0.9 | 0.005 |
| Your health will be worse in the future compared to now. | 3.4 ± 1.1 | 3.4 ± 1.1 | 3.3 ± 1.1 | 3.4 ± 1.1 | 0.31 |
| You expect a healthy life. | 4.1 ± 0.8 | 4.1 ± 0.8 | 3.9 ± 0.8 | 4.2 ± 0.7 | <0.001 |
| Summary score: resistance to illness | 15.4 ± 2.7 | 15.4 ± 2.7 | 15.2 ± 2.7 | 15.7 ± 2.4 | 0.21 |
| You get sick easier than others. | 4.4 ± 0.9 | 4.3 ± 0.9 | 4.2 ± 0.9 | 4.5 ± 0.8 | 0.011 |
| People get sick easier than you do. | 3.7 ± 0.9 | 3.6 ± 0.9 | 3.7 ± 0.9 | 3.7 ± 0.9 | 0.70 |
| Your body resists illness. | 3.4 ± 0.9 | 3.4 ± 1.0 | 3.5 ± 0.9 | 3.4 ± 0.9 | 0.99 |
| Whenever something is going around, you catch it. | 3.9 ± 0.8 | 3.9 ± 0.8 | 3.8 ± 0.9 | 4.0 ± 0.7 | 0.054 |
| Summary score: health worry∗ | 13.1 ± 2.4 | 13.2 ± 2.4 | 12.8 ± 2.4 | 13.2 ± 2.3 | 0.19 |
| You never worry about your health.∗ | 3.3 ± 1.1 | 3.3 ± 1.1 | 3.5 ± 1.0 | 3.1 ± 1.1 | <0.001 |
| You worry about your health more than others.∗ | 2.5 ± 1.1 | 2.5 ± 1.1 | 2.6 ± 1.0 | 2.3 ± 1.0 | 0.089 |
| Others are more concerned about their health than you are yours.∗ | 3.6 ± 1.0 | 3.6 ± 1.0 | 3.4 ± 1.0 | 3.9 ± 0.9 | <0.001 |
| Your health is a concern (a priority).∗ | 3.7 ± 1.0 | 3.8 ± 1.0 | 3.3 ± 1.0 | 3.8 ± 1.0 | <0.001 |
| Summary score: sickness orientation | 7.4 ± 1.5 | 7.4 ± 1.5 | 7.4 ± 1.5 | 7.5 ± 1.5 | 0.69 |
| Getting sick is part of life. | 3.5 ± 1.0 | 3.5 ± 1.0 | 3.6 ± 1.0 | 3.6 ± 1.0 | 0.35 |
| You accept that sometimes you are sick. | 3.9 ± 0.8 | 3.9 ± 0.7 | 3.8 ± 0.7 | 3.9 ± 0.8 | 0.95 |
Note: Higher scores represent more positive health status or positive health perception with the exception of the health worry summary score and its components, denoted by an asterisk (∗), where greater values indicate greater concern for one’s health.
ESKD, end-stage kidney disease.
The PROMIS global physical and mental health scores range from a minimum of 4 and maximum of 20, with greater scores indicating better health. The individual questions on the PROMIS survey have responses on a Likert scale of 1 to 5, with the exception of the pain score which ranges from 0-10 (but is rescaled to a scale of 1-5 during computation of the summative PROMIS scores).
For the Davies and Ware Health Perceptions, individual question responses were scored on a Likert scale between 1 and 5, with higher scores represent more positive health status or positive health perception with the exception of the health worry summary score and its components, where greater values indicate greater concern for one’s health. Davies and Ware Summary Scores were a simple summation of their constituent scores, with a maximum score of 20 for health outlook, resistance to illness, and health worry summary scores, and maximum of 10 for the sickness orientation summary score.
This is the predicted % risk of the donor developing kidney failure over a 15-year horizon if they undergo donation.
N = 62 who completed laboratory testing and had sufficient data elements for a 15-year ESRD risk to be computed.
Approximately 71% (n = 961) of individuals completed the survey at the time of their initial contact with the transplant center (during the online screening process) but did not move forward in the donor evaluation process, of whom 33 individuals were deemed ineligible for donation at this early stage after their questionnaire was reviewed by the donor team (Fig 1). Among donors who proceeded to a telephone interview and laboratory screening (n = 386), 21% (n = 81) were deemed ineligible, and 23% (n = 90) withdrew from the donor evaluation process. Only 16% of the initial cohort (n = 215) completed the donor evaluation process (Fig 1). Of those who completed the latter steps of the donor evaluation, which included an in-person visit and computed tomography scan, 47% donated (n = 101).
Table 1 shows mean raw scores for each question on the Global Physical and Mental Health Surveys and a breakdown of the health outlook scores derived from the Davies and Wares survey by question. The mean PROMIS global physical health (17.0 ± 1.9) and mental health (15.5 ± 2.7) raw scores were higher among donor candidates proceeding to completion of the donor evaluation compared with those who withdrew early in the process after initial online questionnaire (16.3 ± 2.2 for physical health and 14.9 ± 3.1 for mental health). A similar pattern was noted for the health domains of the Davies and Ware survey.
Potential Donors’ Health Perceptions and the Odds of Completing Donor Evaluation
The PROMIS physical health score predicted the odds of presenting for an in-person clinic evaluation (OR 1.50; 95% CI, 1.22-1.84 per SD z-score change in physical health score, Model 1; Table 2). This association between the physical health score and completion of the donor evaluation persisted even when models included the Davies and Wares health perceptions, with every standard deviation in z-score change being associated with 1.48 times higher odds (95% CI, 1.19-1.85; Model 3; Table 2) of completing the donor evaluation. Potential donors’ self-reported mental health score did not predict the odds of completing the donor evaluation (OR 1.02 per SD in z-score change; 95% CI, 0.84-1.24) in fully adjusted analysis. Models incorporating the PROMIS mental and physical health scores had a c-statistic of 0.70.
Table 2.
Association Between Potential Donors’ Characteristics and Perceived Health With the Odds of Completing the Donor Evaluation Process
| Model 1 (PROMIS Health) |
Model 2 (Davies and Ware Health Perceptions) |
Model 3 (PROMIS Health + Davies and Ware Health Perceptions) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| PROMIS physical and mental health (per SD change in z-score) | |||||||||
| Global physical health | 1.50 | (1.22-1.84) | < 0.001 | 1.48 | (1.19-1.85) | 0.001 | |||
| Global mental health | 1.04 | (0.85-1.26) | 0.72 | 1.02 | (0.84-1.24) | 0.84 | |||
| Davies and Ware Health Perceptions (per SD change in z-score) | |||||||||
| Health outlook | 1.32 | (1.09-1.59) | 0.004 | 1.15 | (0.94-1.40) | 0.19 | |||
| Resistance to illness | 1.04 | (0.86-1.26) | 0.66 | 0.95 | (0.78-1.16) | 0.62 | |||
| Health worry | 0.97 | (0.84-1.13) | 0.74 | 0.98 | (0.84-1.14) | 0.79 | |||
| Sickness orientation | 1.15 | (0.98-1.35) | 0.08 | 1.16 | (0.99-1.36) | 0.06 | |||
| C-statistic | 0.70 | (0.66-0.73) | 0.69 | (0.65-0.72) | 0.70 | (0.67-0.74) | |||
Note: All models adjusted for age, sex, race/ethnicity, and donor relationship to the intended recipient.
The Davies and Ware health outlook of potential donors was associated with the odds of completing the donor evaluation (OR 1.32 per SD change in health outlook z- score; 95% CI, 1.09-1.59; Model 2 in Table 2), but this association was attenuated in models including both the PROMIS and Davies and Ware Health Perceptions and was no longer statistically significant. The addition of the Davies and Wares health perception domains to models did not improve the c-statistic (0.70, Table 2).
In sensitivity analysis, when we excluded potential donors who were deemed ineligible or dropped out of the evaluation process after telephone screening or laboratory testing (n = 171), results were similar (Table S1).
Exploration of the Association of Potential Donors’ Health Perceptions With the Predicted Risk of Kidney Failure After Donation
The mean 15-year predicted risk of post-donation kidney failure among potential donors who completed laboratory testing was 0.08% (25th and 75th percentiles; 0.04%, 0.13%). In adjusted analysis, there was no statistically significant association between potential donors’ self-reported global or physical mental health and the predicted risk of end-stage kidney disease following donation in the subset of donor candidates with such data available (Table S2).
Discussion
In this study, we found consistent and statistically significant differences in donors’ self-reported physical and mental health and health perceptions among those who completed the donor evaluation when compared with those who did not. Donor candidates’ self-reported physical health predicted the likelihood of progression to completion of the donor evaluation with moderate risk discrimination. At our transplant center, ∼76% of individuals who initially expressed an interest in considering living kidney donation and participated in our study dropped out of the donor evaluation process, despite only a small percentage (2.4%) being deemed ineligible early on after passing an initial online questionnaire-based screening tool. Ultimately, only 16% completed the donor evaluation, and 8% underwent donation.
It is well recognized that there are medical and nonmedical barriers to living kidney donation and that better strategies are needed to increase living kidney donation rates in the United States.5,9,12,20, 21, 22, 23, 24 Previous studies of barriers to living donation have identified medical factors such as obesity,25, 26, 27 travel costs,10,28 financial costs of donation, and income loss as some important facotrs.29,30 However, few studies have focused on potential donors’ perceived health as a predictor of the likelihood of completing the donor evaluation process. Although there have been multiple advances in the last decade to protect living donors from income loss and to support travel and time off from work, our data suggest that a larger source of dropout in the living donor process could be related to the candidates’ self-perceived health, and particularly, physical health. When raising awareness of the benefits of donation to the public,31,32 addressing perceptions about whether one is physically healthy enough to serve as a living donor could be an intervention that deserves further investigation to increase rates of living donation.
Although several qualitative studies have been performed to identify barriers to living donation, it may be difficult to capture donor attitudes and beliefs regarding living donation if only those who have completed the entire donor evaluation are included, and only small numbers of individuals can be recruited for in-depth interviews or focus groups.7,8,24 In addition, recall bias and knowledge of the intended recipient’s outcome (in non-altruistic donors) may influence potential donors’ rationale for declining or agreeing to donate.33 Our study’s strength lies in the systematic capture of donors’ perceived health early in the donor evaluation process and before the potential donors’ knowledge of the subsequent clinical course of their intended recipient. We believe that this is one of the largest studies that has included potential donors who did not progress in the donor evaluation process after their initial contact with the transplant center where they passed an online questionnaire that screened for donation eligibility. This is supported by a lower rate of completion of donor evaluation and donor nephrectomy when compared with previous studies.5,34,35
It is known that systemic barriers contribute to attrition during the donor evaluation process, such as poor communication among providers and also limited provider knowledge surrounding living donor eligibility.23,36 The lengthy donor evaluation process has also been identified as one reason for high dropout rates during donor evaluation.34,37 Our data suggest that screening candidates’ perceived physical health at the time of first donor contact with the transplant center could potentially help identify a subgroup of potential donors who are more likely to complete the donor evaluation process and expedite the time to identification of a kidney donor.
However, there are a few limitations to note in our study. First, we do not know whether all of those who initially contacted the transplant center to express interest in donation would ultimately have been deemed eligible for donation because they declined to proceed with the donor evaluation, though the rates of ineligibility were generally low after donors passed an initial screen online. Second, we do not know the reasons for the failure to proceed with the donor evaluation, including whether potential donors’ social networks or intended recipients may have influenced the decision to move forward with completion of the donation evaluation or donor nephrectomy.21,27,31 Third, transplant centers are known to have large variations in their donor evaluation processes, and hence our findings may not generalize to all centers.38 Although we examined the association between self-reported health and health perceptions and the likelihood of completing the donation evaluation in aggregate, we acknowledge that reasons that led donor candidates to abort the evaluation process may have differed at different stages. Finally, potential donors who consented to participate in our study may have differed from those who declined to participate.
In conclusion, potential donors’ self-reported physical health was strongly predictive of completion of the donor evaluation process. Future interventions may be needed to address potential donors’ self-reported physical health in addition to other medical or nonmedical barriers to donation to increase the number of living kidney donors in the era of organ shortage.
Article Information
Authors’ Full Names and Academic Degrees
Elaine Ku, MD, MAS, Sabrina Legaspi, MA, Timothy P. Copeland, PhD, Deborah B. Adey, MD, Adrian M. Whelan, MB, MAS, Garrett R. Roll, MD, Charles E. McCulloch, PhD, Brian K. Lee, MD, and Kirsten L. Johansen, MD
Authors’ Contributions
Research idea and study design: EK and KLJ; data acquisition: SL, DBA, BKL, and AMW; data analysis/interpretation: TPC, EK, and CEM; statistical analysis: TC and CEM; supervision or mentorship: DBA, AMW, GRR, CEM, and BKL. Each author contributed important intellectual content during article drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
R01 DK 115269 to KLJ and EK.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received March 13, 2024, as a submission to the expedited consideration track with 4 external peer reviews. Direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form May 28, 2024.
Footnotes
Complete author and article information provided before references.
Item S1: Survey instruments.
Table S1: Association Between Reported Health Measures and Donor Candidates’ Odds of an In-Person Evaluation Excluding 171 Donors Deemed Ineligible at the Phone Interview/Laboratory Testing Phase Before In-person Clinic Evaluation.
Table S2: Association Between Reported Health Measures and Donor Candidates’ Estimated 15-Year Risk of Kidney Failure (as a %) After Donation Among 277 Patients With Sufficient and Clinical Laboratory Data Available in Adjusted Linear Regression.∗
Supplementary Materials
Item S1; Table S1, S2.
References
- 1.Lentine K.L., Mannon R.B. The advancing American kidney health (AAKH) executive order: promise and caveats for expanding access to kidney transplantation. Kidney360. 2020;1(6):557–560. doi: 10.34067/KID.0001172020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quinn R.R., Lam N.N., Ravani P., Oliver M.J., Blake P.G., Tonelli M. The advancing American kidney health initiative: the challenge of measuring success. J Am Soc Nephrol. 2022;33(6):1060–1062. doi: 10.1681/ASN.2021121619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lentine K.L., Smith J.M., Hart A., et al. OPTN/SRTR 2020 annual data report: kidney. Am J Transplant. 2022;22(Suppl 2):21–136. doi: 10.1111/ajt.16982. [DOI] [PubMed] [Google Scholar]
- 4.Purnell T.S., Luo X., Cooper L.A., et al. Association of race and ethnicity with live donor kidney transplantation in the United States from 1995 to 2014. JAMA. 2018;319(1):49–61. doi: 10.1001/jama.2017.19152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kasiske B.L., Ahn Y.S., Conboy M., et al. Outcomes of living kidney donor candidate evaluations in the living donor collective pilot registry. Transplant Direct. 2021;7(5):e689. doi: 10.1097/TXD.0000000000001143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar K., Tonascia J.M., Muzaale A.D., et al. Racial differences in completion of the living kidney donor evaluation process. Clin Transpl. 2018;32(7) doi: 10.1111/ctr.13291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanson C.S., Ralph A.F., Manera K.E., et al. The lived experience of “being evaluated” for organ donation: focus groups with living kidney donors. Clin J Am Soc Nephrol. 2017;12(11) doi: 10.2215/CJN.03550417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alvaro E.M., Siegel J.T., Turcotte D., Lisha N., Crano W.D., Dominick A. Living kidney donation among Hispanics: a qualitative examination of barriers and opportunities. Prog Transplant. 2008;18(4):243–250. doi: 10.1177/152692480801800406. [DOI] [PubMed] [Google Scholar]
- 9.Barnieh L., McLaughlin K., Manns B.J., Klarenbach S., Yilmaz S., Hemmelgarn B.R. Barriers to living kidney donation identified by eligible candidates with end-stage renal disease. Nephrol Dial Transplant. 2011;26(2):732–738. doi: 10.1093/ndt/gfq388. [DOI] [PubMed] [Google Scholar]
- 10.Weng F.L., Lee D.C., Dhillon N., et al. Characteristics and evaluation of geographically distant vs geographically nearby living kidney donors. Transplant Proc. 2016;48(6):1934–1939. doi: 10.1016/j.transproceed.2016.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zazoulina J., Khehra K., Gill J. Motivators and barriers to living donor kidney transplant as perceived by past and potential donors. Can J Kidney Health Dis. 2022;9 doi: 10.1177/20543581221137179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nimmo A., Taylor D., Bailey P. In: Living Kidney Donation: A Practical Guide. Sharif A., Lipkin G., editors. Springer International Publishing; Cham: 2022. Barriers to Living Kidney Donation Barriers to living kidney donation; pp. 87–103. [Google Scholar]
- 13.Taber J.M., Leyva B., Persoskie A. Why do people avoid medical care? A qualitative study using national data. J Gen Intern Med. 2015;30(3):290–297. doi: 10.1007/s11606-014-3089-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ware D., Landy D.C., Rabil A., Hennekens C.H., Hecht E.M. Interrelationships between self reported physical health and health behaviors among healthy US adults: from the NHANES 2009–2016. Public Health Pract. 2022;4 doi: 10.1016/j.puhip.2022.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zarini G.G., Vaccaro J.A., Canossa Terris M.A., et al. Lifestyle Behaviors and self-rated health: The Living for Health Program. J EnvironPublic Health. 2014;2014 doi: 10.1155/2014/315042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Layes A., Asada Y., Kepart G. Whiners and deniers – what does self-rated health measure? Soc Sci Med. 2012;75(1):1–9. doi: 10.1016/j.socscimed.2011.10.030. [DOI] [PubMed] [Google Scholar]
- 17.Barile J.P., Reeve B.B., Smith A.W., et al. Monitoring population health for Healthy People 2020: evaluation of the NIH PROMIS® Global Health, CDC Healthy Days, and satisfaction with life instruments. Qual Life Res. 2013;22(6):1201–1211. doi: 10.1007/s11136-012-0246-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.RAND corporation Davies and Ware Health Perceptions Survey. https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwi_zezU4LCDAxUMIkQIHS4fBccQFnoECBcQAQ&url=https%3A%2F%2Fwww.rand.org%2Fcontent%2Fdam%2Frand%2Fpubs%2Freports%2F2007%2FR2711.pdf&usg=AOvVaw2_vpJz1DMap5hoddPSFsL2&opi=89978449
- 19.Grams M.E., Sang Y., Levey A.S., et al. Kidney-failure risk projection for the living kidney-donor candidate. N Engl J Med. 2016;374(5):411–421. doi: 10.1056/NEJMoa1510491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Segev D.L. Innovative strategies in living donor kidney transplantation. Nat Rev Nephrol. 2012;8(6):332–338. doi: 10.1038/nrneph.2012.82. [DOI] [PubMed] [Google Scholar]
- 21.Garg A.X. Helping more patients receive a living donor kidney transplant. Clin J Am Soc Nephrol. 2018;13(12):1918–1923. doi: 10.2215/CJN.00760118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salter M.L., Gupta N., King E., et al. Health-related and psychosocial concerns about transplantation among patients initiating dialysis. Clin J Am Soc Nephrol. 2014;9(11):1940–1948. doi: 10.2215/CJN.03310414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sandal S., Charlebois K., Fiore J.F., Jr., et al. Health professional-identified barriers to living donor kidney transplantation: A Qualitative Study. Can J Kidney Health Dis. 2019;6 doi: 10.1177/2054358119828389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siegel J.T., O’Brien E.K., Alvaro E.M., Poulsen J.A. Barriers to living donation among low-resource Hispanics. Qual Health Res. 2014;24(10):1360–1367. doi: 10.1177/1049732314546869. [DOI] [PubMed] [Google Scholar]
- 25.Locke J.E., Reed R.D., Massie A., et al. Obesity increases the risk of end-stage renal disease among living kidney donors. Kidney Int. 2017;91(3):699–703. doi: 10.1016/j.kint.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sachdeva M., Sunday S., Israel E., et al. Obesity as a barrier to living kidney donation: a center-based analysis. Clin Transplant. 2013;27(6):882–887. doi: 10.1111/ctr.12246. [DOI] [PubMed] [Google Scholar]
- 27.Bailey P.K., Tomson C.R.V., MacNeill S., et al. A multicenter cohort study of potential living kidney donors provides predictors of living kidney donation and non-donation. Kidney Int. 2017;92(5):1249–1260. doi: 10.1016/j.kint.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 28.Hays R.E., Thomas A.E., Mathias E., Mezrich J., Mandelbrot D.A. Barriers to the use of a federal travel grant by living kidney donors. Clin Transpl. 2017;31(2) doi: 10.1111/ctr.12876. [DOI] [PubMed] [Google Scholar]
- 29.Rodrigue J.R., Schold J.D., Morrissey P., et al. Predonation direct and indirect costs incurred by adults who donated a kidney: findings from the KDOC study. Am J Transplant. 2015;15(9):2387–2393. doi: 10.1111/ajt.13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fu R., Sekercioglu N., Hishida M., Coyte P.C. Economic consequences of adult living kidney donation: a systematic review. Value Health. 2021;24(4):592–601. doi: 10.1016/j.jval.2020.10.005. [DOI] [PubMed] [Google Scholar]
- 31.Getchell L.E., McKenzie S.Q., Sontrop J.M., Hayward J.S., McCallum M.K., Garg A.X. Increasing the rate of living donor kidney transplantation in Ontario: donor- and recipient-identified barriers and solutions. Can J Kidney Health Dis. 2017;4 doi: 10.1177/2054358117698666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waterman A.D., Robbins M.L., Peipert J.D. Educating prospective kidney transplant recipients and living donors about living donation: practical and theoretical recommendations for increasing living donation rates. Curr Transplant Rep. 2016;3(1):1–9. doi: 10.1007/s40472-016-0090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thiessen C., Kulkarni S., Reese P.P., Gordon E.J. A call for research on individuals who opt out of living kidney donation: challenges and opportunities. Transplantation. 2016;100(12):2527–2532. doi: 10.1097/TP.0000000000001408. [DOI] [PubMed] [Google Scholar]
- 34.Habbous S., Arnold J., Begen M.A., et al. Duration of living kidney transplant donor evaluations: findings from 2 multicenter cohort studies. Am J Kidney Dis. 2018;72(4):483–498. doi: 10.1053/j.ajkd.2018.01.036. [DOI] [PubMed] [Google Scholar]
- 35.Waterman A.D., Peipert J.D., Hyland S.S., McCabe M.S., Schenk E.A., Liu J. Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clin J Am Soc Nephrol. 2013;8(6):995–1002. doi: 10.2215/CJN.08880812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sandal S., Schiller I., Dendukuri N., et al. Identifying modifiable system-level barriers to living donor kidney transplantation. Kidney Int Rep. 2022;7(11):2410–2420. doi: 10.1016/j.ekir.2022.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weng F.L., Morgievich M.M., Kandula P. The evaluation of living kidney donors: how long is too long? Am J Kidney Dis. 2018;72(4):472–474. doi: 10.1053/j.ajkd.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garg N., Lentine K.L., Inker L.A., et al. The kidney evaluation of living kidney donor candidates: US practices in 2017. Am J Transplant. 2020;20(12):3379–3389. doi: 10.1111/ajt.15951. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Item S1; Table S1, S2.