Abstract
The present study explores the prevalence and socio-economic demographic factors affecting childhood illnesses. Diarrhoea, fever and ARI among under-five children in the North -East states of India using NFHS-5 data Kids file. Results showed that diarrhoea, ARI, and fever among the northeastern states were highest in Meghalaya.For diarrhoea Sikkim has the highest prevalence for children within 6 months while Meghalaya has the highest prevalence in the age groups 6- 12 months and 1- 2 years old children and Arunachal Pradesh has the highest rate in the age group 2- 5 years old children. Meghalaya stands out with the highest prevalence of fever and ARI in all age groups. Compared to Sikkim, the state of Meghalaya had more diarrhoea, ARI and fever, and it was statistically highly significant. However, Tripura and Assam had significantly higher odds of having fever and ARI than Sikkim. There is an association between diarrhoea, fever, and ARI and factors such as the age of the child and caregiver, the wealth status of the household, the quality of sanitation facilities, methods of stool disposal, and the caregiver's educational level.
Keywords: North eastern Indian states, Childhood illnesses, Diarrhoea, ARI, Fever, NFHS-5
Introduction
Globally, diarrhoea ranks as the second leading cause of death among children under 5 years old, accounting for 1.5 million fatalities annually worldwide [1]. In India, it stands as the third leading cause of childhood mortality [1]. A cross-sectional study conducted across 707 districts in India, encompassing 223,785 children, reveals that 7.3 percent of children in the country suffer from diarrhoea [2]. An examination conducted among children under 3 years old in India through NFHS-5 revealed that out of 132,198 children surveyed, 8.4 percent had experienced diarrhoea in the two weeks leading up to the study. Among those lacking improved toilet facilities, the prevalence rose to 12.5%, whereas it stood at 9.7% among those utilizing improved facilities and highlight the significance of enhanced sanitation in reducing diarrhoea [3]. A study conducted in Nepal in 2019 identified that children between 7–23 months old, those experiencing Acute Respiratory Infection (ARI), and children whose mothers lacked access to prenatal care faced a heightened risk of developing diarrhoea [4]. Childhood diarrhoea presents a significant public health challenge in India, contributing to 14% of deaths among children under five. Oral Rehydration Solution and zinc are effective in managing diarrhoea [5]. According to the 2017 educational and health survey conducted in Bangladesh, approximately 5% of children reported having episodes of diarrhoea [6]. In India diarrhoea is prevalent among children from scheduled caste, rural and economically disadvantage families [7]. Environmental factors, including child stool disposal practices, and the materials used for household roofs and floors emerged as significant contributors to childhood diarrhoea [8]. The decomposition analysis conducted in Peru revealed a pro-poor inclination. Children aged 0–23 months from the lowest wealth indexes in the highland and jungle regions emerged as notable contributors [9]. In Ethiopia, the findings indicated lower odds of childhood illness when the mother's age fell within the range of 35–49 years compared to those aged 15–24 and attributed to older mothers' experience in child and health management [10]. Zinc supplements have been identified as a remedy for diarrhoea and respiratory illnesses [11].
The United Nations Sustainable Development Goals (UN SDGs) emphasizes to end preventable deaths of children under age 5 years by 2030 among all world countries including India [12]. Globally, Acute respiratory Infections (ARI), fever, and diarrhea are the prominent causes of the burden of childhood diseases along with mortality mostly in developing and low resource setting countries [13, 14].Even in India, children under age 5 years are suffering from and contributing a significant amount to the total disease burden of children under age 5 which are due to the childhood diseases of diarrhoea, ARI and fever [15–20]. Even these three childhood Illnesses depend upon some factors and needs intervention strategy to reduce the burden of preventable deaths due to these Illnesses [15, 17–24]. The prevalence of the three preventable childhood Illnesses viz Diarrhoea, fever and ARI in North-east Indian states were also high and noticed by some of the previous studies [16, 20, 25–27].Diarrheal illness represents a major worldwide public health concern and a leading cause for hospitalization among under 5 children and detoriation in quality of life on a global level [28]. Globally, sufficient medical care has been given to diarrhoea and acute respiratory infections (ARI),however they remain among the prime cause of mortality in children under five years old [1, 29]. Respiratory infections (ARI), fever and diarrhoea play a substantial role in the worldwide disease burden and mortality in developing countries [30, 31]. Numerous cases of diarrhoea remain undiagnosed, due to their mild symptoms and tend to resolve on their own, or because those affected choose not to seek medical assistance [32].
Diarrhoea stands as one of the top five causes of death for infants and children under the age of five in India [33]. Every year, millions of children under five years old worldwide lose their lives to environment-related illnesses such as Acute Respiratory Infections and acute diarrhoea [34, 35]. Extreme dehydration and the loss of fluids stand as the key factors contributing to fatalities caused by diarrhoea, impacting both adults and children [36]. Despite a decrease in the overall mortality rate for children under 5, diarrhoea continues to be a substantial factor, causing an estimated 300,000 child deaths annually in India [37] Around 400,000 children under 5 years old succumb to Acute Respiratory Infection (ARI)-related ailments annually [38–40]. A recent study based on NFHS-4 found, among the northeastern region, the state of Meghalaya performs worst in terms of diarrhoea and ARI [25].Even in NFHS-5 report, diarrhoea and ARI in Meghalaya was much higher than the national prevalence of the illnesses [7].
A study on diarrhoea in North-East India, utilizing data from DLHS-4, observed that a 61.46% of women continued normal breastfeeding, while 56.63% provided their children experiencing diarrhoea with Zinc or ORS. [41]. The Northeastern region of India, comprising of the seven sister states (Mizoram, Tripura, Assam, Manipur, Meghalaya, Arunachal Pradesh, Nagaland) as well as the Himalayan states of Sikkim, showcases diversity characterized by unique cultural, geographical, and environmental aspects [42–44]. The unique blend of climatic conditions, limited healthcare accessibility, and dense forest coverage in select areas render this region vulnerable to infectious Illnesses [42].Waterborne illnesses such as cholera, diarrhoea and typhoid prevail in this region due to inadequate sanitation facilities, low awareness levels, and limited access to safe drinking water [45]. In the DLHS-3 baseline, households show a 35 percent adoption of piped water and a 36 percent adoption of improved sanitation. There are noticeable discrepancies in coverage across various states. Piped water coverage is below 15 percent in northeastern states, especially low in Assam. Conversely, Arunachal Pradesh and Sikkim demonstrate piped water coverage rates exceeding 85 percent. Additionally, Mizoram displays improved sanitation coverage rates surpassing 80 percent [46]. Addressing infectious Illnesses in Northeast India presents a range of complex challenges. These include inadequate healthcare infrastructure, scarce trained professionals and limited accessibility to healthcare in remote areas. These obstacles hinder effective management and control of Illnesses. Socio-economic factors such as illiteracy, poverty and insufficient awareness further increase the population's susceptibility to infectious Illnesses. The government has undertaken numerous strategies in India to mitigate diarrhoea and enhance public health. These initiatives include improving access to clean water and sanitation facilities, advocating for proper hygiene practices, and promoting oral rehydration therapy for timely treatment. Additionally, the government has emphasized emphasized emphasized vaccination programs, particularly against rotavirus, a primary cause of diarrheal Illnesses in children. Ongoing endeavors involve a blend of policies, awareness campaigns, and enhancements to healthcare infrastructure to tackle these challenges persistently.
Limited research has been carried out to understand the prevalence and factors affecting the three childhood Illnesses in north east Indian states. The present study aims to estimate the prevalence, association, and socio-economic demographic and health factors affecting childhood disease illnesses, diarrhoea, fever, and ARI among under-five children in the North-East states of India.
Data source
The data used in this study was unit level data of the fifth round of National Family Health Survey data (NFHS-5) conducted in 2019–21.NFHS-5 provides the information on population, health and nutrition for India and its each state and union territories and district level estimates for many important indicators. The NFHS also provides information on crucial parameters concerning population demographics, family planning, maternal and child health, nutritional status, adult health, and instances of domestic violence, among other factors. The data is available from National Family Health Survey (NFHS-5) (rchiips.org). NFHS-5 fieldwork for India was conducted in two phases, phase one from 17 June 2019 to 30 January 2020 and phase two from 2 January 2020 to 30 April 2021 and gathered information from 636,699 households, 724,115 women, and 101,839 men. The birth file of NFHS-5 contains the information of nearly 1,274,250 children who were between 1978 to 2021.The information about each of these children along with their survival status, year of birth, sex of the child, birth order, age at death, whether a child is twin or not and other information was asked retrospectively to all the 724,115 eligible women who were ever married in the age group 15–49 years.
In this study we used the five year truncated birth history file which is popularly known as Kids file where the information for each of the children were given for past 5 years before the survey period, so here the information details about the children was asked from 2014 onwards till the year 2019–2021. Information about health and these Illnesses among the children are available for the past five years however for the vaccination and other details the information was asked for the children born in the past three years before the survey year (i.e. from 2016 onwards).
Hence in Kids file,232,920 children were nested among 176,843 ever married women.Since our study was based on the north east Indian states hence we selected the 34,222 children of all eight north east Indian states ( i.e. Sikkim, Assam,Arunachal Pradesh, Nagaland,Manipur,Mizoram,Meghalaya, Tripura).For our study for understanding the childhood Illnesses like diarrhoea,fever and Acute Respiratory Infections(ARI) we have taken only alive children which consists of 33,199 children. So the final sample for our study was 33,199 children whose information was collected in for northeast Indian states in the past five years.
The definitions for ARI, Diarrhoea used in the study were based on questions asked in NFHS from the child’s mother/respondent during the survey. The acute respiratory infection, ARI symptoms consist of cough accompanied by (1) short, rapid breathing that is chest related, and/or (2) difficult breathing that is chest related. Mothers who reported about their children under age five years who had symptoms of acute respiratory infection (ARI) in the two weeks before the survey. This question is asked only if the child had a cough in the past two weeks. Short, rapid breathing or difficulty breathing are signs of pneumonia or other acute respiratory infections, which are a principal cause of death among children (IIPS,2019).Similary Diarrhoea was defined for children under age five years with diarrhoea in the two weeks before the survey. It has considered a child with diarrhoea as those children who passed ‘three or more loose or liquid stools per day.’ while reading this question, emphasize ‘in the last 2 weeks’ [47] to reduce the response from recall bias as far as possible and also reflect the disease conditions [48–50] The question related to fever was “Has the child been ill with a fever at any time in the last 2 weeks?”.
The reponse for the three illnesses were not recorded during the same month or season for all the northeast states as the survey was conducted in phases. For example, NFHS-5 fieldwork for Arunachal Pradesh was conducted from January 2020 to March 2020 before the lockdown and from December 2020 to April 2021 post lockdown, similarly fieldwork for Assam was conducted from June, 2019 to December, 2019, for Manipur fieldwork was conducted from July, 2019 to January, 2020, for Meghalaya it was conducted between July, 2019 to November, 2019, for Mizoram from July, 2019 to November, 2019,for Nagaland it was conducted from July, 2019 to December, 2019, fieldwork for Sikkim was conducted from August, 2019 to December, 2019 and finally fieldwork for Tripura was conducted from 4 July, 2019 to 10 November, 2019 respectively.In present study, we have not considered the seasonality factor for the considered illnesses even if there is any.
In the NFHS-5, the information about diarrhoea was asked for each birth in 2014 or later. The question was asked from mothers about her under 5 years children about childhood illnesses diarrhoea as “Has had diarrhoea in the last 2 weeks” and the response was recorded in “yes” and “no”. Similarly, the questions related to fever and ARI was asked for its occurrence in the last two weeks. For our study for each of the three childhood Illnesses (like Diarrhoea, fever and ARI) we have coded “0” if the illnesses has not occurred in the past two weeks and “1” if it occurred in the past two weeks. We have estimated the prevalence and association of these three childhood Illnesses by various community characteristics (like states, place of residence) Mother or Individual characteristics like (age, education, religion, caste), Household Characteristics (wealth index, sanitation facilities, water facilities, number of children living), child characteristics (sex of the child, birth order, child’s age, caesarean delivery, stunting).
For logistic regression, each of these dichotomous childhood diseases was taken as the dependent variable, and the different community, household, individual, and child characteristics were taken as the independent variable and included in the model as dummy variables.
The kids file of NFHS-5 was used for this objective which has the information of about 33,199 alive children who were born in the year 2014 or later and the information about diarrhoea was collected from them but for vaccination since the information was collected from the year 2016 onwards, so the sample size of the children get reduced to 19,089 children. We used separate logistic regression model for examining the factors associated with diarrhoea for the two samples in the form of two models i.e. Model 1 & Model 2 respectively. Model 1 was based on 33,199 children and Model 2 based on 19,089 children when vaccination was included in model 1 as shown in Table 5.
Table 5.
Results of logistic regression of factors affecting the diarrhoea, fever and ARI among children of under 5 years in North east India,2019–21
| Variables | Diarrhoea | Fever | ARI | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 (n = 26,568) | Model2 (n = 15,118) | Model 1 (n = 26,568) | Model2 (n = 15,118) | Model 1(n = 26,568) | Model2 (n = 15,118) | |||||||
| AOR | SE | AOR | SE | AOR | SE | AOR | SE | AOR | SE | AOR | SE | |
| Community characteristics | ||||||||||||
| State/Region | ||||||||||||
| Sikkim (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Arunachal Pradesh | 1.51 | 0.342 | 1.58 | 0.481 | 0.72** | 0.106 | 0.86 | 0.17 | 2.45 | 1.05 | 0.86 | 0.17 |
| Nagaland | 1.09 | 0.269 | 1.65 | 0.533 | 0.75 | 0.12 | 0.97 | 0.207 | 1.32 | 0.616 | 0.97 | 0.207 |
| Manipur | 1.29 | 0.307 | 1.52 | 0.478 | 0.94 | 0.141 | 1.11 | 0.224 | 1.8 | 0.8 | 1.11 | 0.224 |
| Mizoram | 0.98 | 0.251 | 1.25 | 0.42 | 0.70** | 0.115 | 0.87 | 0.188 | 0.59 | 0.312 | 0.87 | 0.188 |
| Tripura | 1.34 | 0.331 | 1.55 | 0.508 | 1.34 | 0.21 | 1.70** | 0.362 | 1.39 | 0.645 | 1.70** | 0.362 |
| Meghalaya | 2.66*** | 0.613 | 3.37*** | 1.029 | 2.59*** | 0.38 | 3.67*** | 0.724 | 5.17*** | 2.23 | 3.67*** | 0.724 |
| Assam | 1.01 | 0.234 | 0.98 | 0.304 | 1.3 | 0.189 | 1.54** | 0.303 | 1.73 | 0.743 | 1.54** | 0.303 |
| Place of Residence | ||||||||||||
| Urban (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Rural | 1.09 | 0.097 | 1.16 | 0.135 | 0.86*** | 0.049 | 0.83** | 0.062 | 0.82 | 0.106 | 0.83** | 0.062 |
| Mother's characteristics | ||||||||||||
| Age | ||||||||||||
| 15–24 (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 25–34 | 0.9 | 0.063 | 0.84** | 0.072 | 0.96 | 0.046 | 1.02 | 0.061 | 1.01 | 0.115 | 1.02 | 0.061 |
| 35–49 | 0.88 | 0.086 | 0.84 | 0.106 | 0.96 | 0.064 | 0.91 | 0.081 | 1.01 | 0.153 | 0.91 | 0.081 |
| Education | ||||||||||||
| Illiterate (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Primary | 1.14 | 0.098 | 1.17 | 0.132 | 1.17** | 0.074 | 1.16 | 0.095 | 1.05 | 0.135 | 1.16 | 0.095 |
| Secondary | 0.98 | 0.078 | 0.96 | 0.101 | 1.27*** | 0.073 | 1.24*** | 0.093 | 1 | 0.119 | 1.24*** | 0.093 |
| Higher | 0.64*** | 0.094 | 0.63** | 0.119 | 1.05 | 0.099 | 0.95 | 0.115 | 0.86 | 0.184 | 0.95 | 0.115 |
| Religion | ||||||||||||
| Hindu (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Muslim | 1.65*** | 0.259 | 1.77*** | 0.345 | 1.27** | 0.13 | 1.26 | 0.166 | 1.56 | 0.398 | 1.26 | 0.166 |
| Christian | 0.91 | 0.099 | 0.77 | 0.108 | 1.11 | 0.085 | 1.03 | 0.102 | 0.76 | 0.129 | 1.03 | 0.102 |
| Others | 1.1 | 0.132 | 1.01 | 0.157 | 1.27*** | 0.11 | 1.14 | 0.131 | 1.02 | 0.192 | 1.14 | 0.131 |
| Caste | ||||||||||||
| Others (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| SC | 1.18 | 0.173 | 1.12 | 0.21 | 0.78*** | 0.071 | 0.83 | 0.098 | 2.08*** | 0.496 | 0.83 | 0.098 |
| ST | 1.38** | 0.176 | 1.32 | 0.215 | 0.76*** | 0.06 | 0.77** | 0.079 | 1.88*** | 0.413 | 0.77** | 0.079 |
| OBC | 1.40** | 0.185 | 1.31 | 0.22 | 1.14 | 0.09 | 1.11 | 0.115 | 2.37*** | 0.517 | 1.11 | 0.115 |
| Wealth Index | ||||||||||||
| Poorest (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Poorer | 0.87** | 0.056 | 0.86 | 0.07 | 0.97 | 0.043 | 0.99 | 0.056 | 0.87 | 0.085 | 0.99 | 0.056 |
| Middle | 0.86 | 0.072 | 0.85 | 0.091 | 0.83*** | 0.049 | 0.84** | 0.063 | 0.81 | 0.106 | 0.84** | 0.063 |
| Richer | 0.76 | 0.091 | 0.71** | 0.114 | 0.84** | 0.066 | 0.83 | 0.087 | 0.64** | 0.124 | 0.83 | 0.087 |
| Richest | 0.73 | 0.153 | 0.78 | 0.205 | 0.89 | 0.113 | 1.04 | 0.167 | 0.7 | 0.222 | 1.04 | 0.167 |
| Household characteristics: | ||||||||||||
| Sanitation/Toilet Facilities | ||||||||||||
| Improved (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Not improved | 1.16** | 0.073 | 1.11 | 0.09 | 1.15*** | 0.05 | 1.11 | 0.062 | 1.15 | 0.11 | 1.11 | 0.062 |
| Number of living children | ||||||||||||
| One child (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Two children | 0.7 | 0.076 | 0.82 | 0.145 | 0.63*** | 0.048 | 0.79 | 0.097 | 0.75 | 0.134 | 0.79 | 0.097 |
| 3 or more children | 0.48 | 0.076 | 0.57** | 0.146 | 0.43*** | 0.048 | 0.66 | 0.117 | 0.77 | 0.188 | 0.66** | 0.117 |
| Child characteristics | ||||||||||||
| Birth Order | ||||||||||||
| 1 BO (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 2 BO | 1.37*** | 0.151 | 1.1 | 0.196 | 1.40*** | 0.108 | 1.07 | 0.133 | 1.26 | 0.224 | 1.07 | 0.133 |
| 3 BO | 1.71*** | 0.273 | 1.44 | 0.365 | 1.87*** | 0.209 | 1.34 | 0.237 | 1.2 | 0.302 | 1.34 | 0.237 |
| 4 plus BO | 1.92*** | 0.319 | 1.72** | 0.459 | 2.53*** | 0.293 | 1.74*** | 0.322 | 1.84** | 0.464 | 1.74*** | 0.322 |
| Stunting | ||||||||||||
| No (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 1.04 | 0.057 | 0.92 | 0.067 | 0.98 | 0.037 | 0.96 | 0.047 | 1.13 | 0.096 | 0.96 | 0.047 |
| Child Age | ||||||||||||
| within 6 months (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 6–12 months | 2.18*** | 0.274 | 2.22*** | 0.299 | 1.99*** | 0.167 | 2.04*** | 0.187 | 1.89*** | 0.366 | 2.04*** | 0.187 |
| 1to less than 2 years | 1.96*** | 0.238 | 2.04*** | 0.275 | 1.91*** | 0.154 | 1.94*** | 0.176 | 1.70*** | 0.317 | 1.94*** | 0.176 |
| 2 to 5 years | 1.39*** | 0.159 | 1.37*** | 0.19 | 1.36*** | 0.102 | 1.40*** | 0.129 | 1.34 | 0.234 | 1.40*** | 0.129 |
| Caesarean delivery | ||||||||||||
| No (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Yes | 1.62*** | 0.122 | 1.64*** | 0.157 | 1.31*** | 0.069 | 1.29*** | 0.087 | 2.12*** | 0.231 | 1.29*** | 0.087 |
| Programme factors | ||||||||||||
| BCG vaccine | ||||||||||||
| No (ref.) | –- | 1 | –- | 1 | –- | 1 | ||||||
| Yes | 1.09 | 0.121 | 1.14 | 0.088 | 1.14 | 0.088 | ||||||
| DPT vaccine | ||||||||||||
| No (ref.) | –- | 1 | –- | 1 | –- | 1 | ||||||
| Yes | 0.97 | 0.097 | 0.99 | 0.069 | 0.99 | 0.069 | ||||||
| Rota virus vaccine | ||||||||||||
| No (ref.) | –- | 1 | –- | 1 | –- | 1 | 0.057 | |||||
| yes | 1.08 | 0.104 | 0.87** | 0.057 | 0.87** | |||||||
| Constant | 0.02*** | 0.007 | 0.02*** | 0.009 | 0.11*** | 0.021 | 0.08*** | 0.022 | 0.005*** | 0.003 | 0.08*** | 0.022 |
*** means p < 0.01; ** means p < 0.05
Dependent and independent variables used in the logistic regression
In the three separate logistic regressions, three different dependent variables, viz., having diarrhoea, fever, and ARI in the past two weeks before the survey, were taken as dependent variables, with “0” indicating the absence of the disease illnesses and “1” indicating their presence.
The choice governing the selection of the independent variables was based on the previous literature and the variables at least show some association with the dependent variable. The independent variables or covariates in Model 1 were kept into broad categories as community, household, individual,and child variables. The community level variables were i.e. state and place of residence, which was included as dummy variables with Sikkim as the reference category for state and place urban as reference for place of residence. In household characteristics, type of toilet facilities variable was recoded into two categories as 1 for “improved sanitation” and 0 for “unimproved sanitation” facilities. Under improved sanitation following categories of the type of toilet facility i.e. flush to piped sewer system, flush to septic tank, flush to pit latrine, ventilated improved pit latrine (vip), pit latrine with slab and composting toilet was coded as 1 and rest all of its other categories were included under unimproved category coded as “0″.Number of living children was into three categories coded as “one child”, “two children” and “3 or more children”. Similarly for the individual characteristics, Mothers age in 5 years was recategorized into three categories “15–24″,”25–34″ and “35–49″ years; Caste was categorised into “SC”,”ST”, “Obc” and “Others”; Religion into 4 categories “Hindu”,”Muslim”,”Christian” and “others”. In child characteristics birth order was categorized into four categories one birth order “1 BO”, two birth order “2 BO”,third birth order as “3 BO” and 4 or more birth order as “4 plus BO”; the z scores for height/age standard deviation variable was recategorized into two categories into stunted “yes” and not stunted “ no" as per WHO guideline; child’s age in months was computed from the subtraction of two variables ( date of survey in century month code (cmc) and date of birth of child in cmc)) and recategorized into four categories “within 6 months”, “6–12 months”,”1 to less than 2 years” and “2 to 5 years” and caesarean section included as dummy variable. In Model 2,we have included programme variables like BCG,DPT and Rota virus apart from those in Model 1. In programme factors each of the factors BCG,DPT and Rota virus vaccination was used as independent variables in its dichotomous form with vaccination date on card and vaccination marked on the card was kept under yes category and all others were kept under no category.
Methods
Logistic regression
Statistical analysis were performed using Stata version 15. Bivariate analyses involving cross-tabulations were conducted independently for each disease Illnesses(diarrhea, fever and ARI). These analyses aimed to establish connections between the occurrence of childhood illnesses and various selected variables, which would later be employed in the multivariate analysis. Significant determinants were explored using Pearson's Chi-square (χ2) test. For the multivariable analysis, logistic regressions were employed to assess the impact of explanatory variables on the probability of childhood illness. This approach was crucial in identifying significant risk factors associated with fever, ARI (acute respiratory infection), and diarrhea in children. To maintain accuracy, three distinct binary logistic regression models were employed for each illnesses separately, without considering any confounding factors.
The logistic regression model is expressed as:
where, Yi is a binary variable that takes a value of ‘1’ if the respondent has illnesses and ‘0’ otherwise, Xi is a vector of independent variables and is a vector of unknown parameters.
The estimated form of regression is define as
The odds ratio in favor of Yi = 1 was computed for X1,X2…Xk to indicate how often the group of interest is more likely to be associated with the child's illnesses than the reference group.
Table 1 shows the total sample size and information about categorical variables converted in to dummy variables used for running the logistic regression model. We see that there are missing cases in some of the dummy variable which is from the original data. But the result of this study will still give an admissible results.
Table 1.
Dummy variables descriptive statistics as used in the logistic regression model
| Variables (#) | Observations | Mean | Std. Dev | Min | Max |
|---|---|---|---|---|---|
| Overall North East Indian States | |||||
| Diarrhoea | 33,199 | 0.06 | 0.2378 | 0 | 1 |
| Fever | 33,199 | 0.151 | 0.3579 | 0 | 1 |
| Acute Respiratory Infections | 32,953 | 0.025 | 0.1554 | 0 | 1 |
| North East States | |||||
| Arunachal Pradesh | 33,199 | 0.164 | 0.3699 | 0 | 1 |
| Nagaland | 33,199 | 0.089 | 0.2843 | 0 | 1 |
| Manipur | 33,199 | 0.095 | 0.2926 | 0 | 1 |
| Mizoram | 33,199 | 0.073 | 0.2593 | 0 | 1 |
| Tripura | 33,199 | 0.06 | 0.2375 | 0 | 1 |
| Meghalaya | 33,199 | 0.193 | 0.3943 | 0 | 1 |
| Assam | 33,199 | 0.31 | 0.4624 | 0 | 1 |
| Residence | |||||
| Rural | 33,199 | 0.85 | 0.3568 | 0 | 1 |
| Mother's Age | |||||
| 25- 34 | 33,199 | 0.563 | 0.4961 | 0 | 1 |
| 35–49 | 33,199 | 0.175 | 0.3803 | 0 | 1 |
| Education | |||||
| Primary | 33,199 | 0.173 | 0.3781 | 0 | 1 |
| Secondary | 33,199 | 0.591 | 0.4917 | 0 | 1 |
| Higher | 33,199 | 0.078 | 0.2677 | 0 | 1 |
| Religion | |||||
| Muslim | 33,199 | 0.146 | 0.353 | 0 | 1 |
| Christian | 33,199 | 0.466 | 0.4989 | 0 | 1 |
| Others | 33,199 | 0.092 | 0.2891 | 0 | 1 |
| Caste | |||||
| SC | 28,341 | 0.083 | 0.2751 | 0 | 1 |
| ST | 28,341 | 0.705 | 0.4561 | 0 | 1 |
| Obc | 28,341 | 0.125 | 0.3306 | 0 | 1 |
| Wealth Index | |||||
| Poorer | 33,199 | 0.315 | 0.4645 | 0 | 1 |
| Middle | 33,199 | 0.18 | 0.3843 | 0 | 1 |
| Richer | 33,199 | 0.099 | 0.2986 | 0 | 1 |
| Richest | 33,199 | 0.032 | 0.1751 | 0 | 1 |
| Sanitation Facilities | |||||
| Sanitation Unimproved | 32,890 | 0.253 | 0.4346 | 0 | 1 |
| Birth Order | |||||
| 2 | 33,199 | 0.295 | 0.4561 | 0 | 1 |
| 3 | 33,199 | 0.152 | 0.3586 | 0 | 1 |
| 4 plus | 33,199 | 0.183 | 0.3865 | 0 | 1 |
| Stunting status | |||||
| Yes | 31,395 | 0.35 | 0.4769 | 0 | 1 |
| Child's Age | |||||
| 6–12 months | 33,199 | 0.113 | 0.3167 | 0 | 1 |
| 1–2 years | 33,199 | 0.17 | 0.3753 | 0 | 1 |
| 2- 5 years | 33,199 | 0.631 | 0.4826 | 0 | 1 |
| Living Children | |||||
| 2 | 33,199 | 0.331 | 0.4707 | 0 | 1 |
| 3_more | 33,199 | 0.37 | 0.4828 | 0 | 1 |
| Delivery | |||||
| Cesearan delivery | 33,199 | 0.137 | 0.3434 | 0 | 1 |
| Immunization Taken | |||||
| Bcg | 19,089 | 0.788 | 0.4087 | 0 | 1 |
| Dpt | 19,089 | 0.613 | 0.4871 | 0 | 1 |
| Rota virus | 19,089 | 0.269 | 0.4435 | 0 | 1 |
Results
The study sample comprised of 33,199 children age under 5 years old in the North East states of India drawn from the National Family Health Survey-5 (NFHS-5). All statistical analyses were based on the three common childhood illnesses variables such as diarrhoea, fever and ARI (Table 2 below). The children of both sexes are nearly same in the sample. The age distribution of children reveals nearly 17 percent aged 1 to 2 years, 63 percent aged 2 to 5 years while remaining 20 percent are less than 1 years of age. Cesarean deliveries accounted for nearly 18 percent of childbirths. Nearly, 35 percent of the children experienced stunting. Health-wise, 5 percent children suffered diarrhoea, 2.51 percent had Acute Respiratory Infection (ARI) and 17.36 percent had fever. Of the total children, children from Assam notably contributed 70 percent in sample, followed by Meghalaya (10.32%), Tripura (7.14%), and respectively varying contributions from Mizoram( 2.17%), Manipur(5.39%), Nagaland (2.54%), Arunachal Pradesh(2.09%), and Sikkim(0.74%). The percentage of children reported here are the weighted percentage and hence they are representative one since the sampling weights are adjustment factors applied to each case in tabulations to adjust for differences in probability of selection and interview between cases in a sample, due to either design or happenstance (IIPS & ICF,2021). Rural areas accounted for 85 percent children. The percentage of children belonging to mothers of different age groups in the sample comprises nearly one-third of children born to mothers in 25–29 age group, more than 20 percent born to 20–24 years and 30–34 years women age group respectively. Educationally, 15 percent of children born to illiterate women,17 percent children belonged to mothers who completed primary education, 61 percent children born of mothers who completed secondary education, while nearly 7 percent children belonged to mothers who attained higher education. The majority of children (45.32%) in the sample born to mothers who were Hindus, followed by Muslim children (33.34%), Christian (18.36%), and other religions (3%). Nearly 40 percent children had mothers belonged to Scheduled Castes, 27 percent children belonged to OBCs, Scheduled Tribes children comprises of nearly 16 percent, and remaining castes nearly 17 percent. Financially, 72.4 percent of children hailed from impoverished backgrounds (poorest and poorer one), 12 percent of children belonged to wealthy families (richer and richest), and 16 percent to middle class families. Children born to households with Improved water facilities were prevalent (83%), yet sanitation facilities lagged (34% only). Children born to families with one, two, and three children comprised 36 percent, 36 percent and 29 percent, respectively, of the total children in the surveyed households.
Table 2.
Study Sample description for Northeast Region of India, 2019–2021
| Variables/Characteristics | Percentage | N |
|---|---|---|
| Childhood Illness | ||
| Diarrhoea | ||
| No | 94.05 | 31,201 |
| Yes | 5.95 | 1,998 |
| ARI | ||
| No | 97.49 | 32,137 |
| Yes | 2.51 | 816 |
| Fever | ||
| No | 82.64 | 28,190 |
| Yes | 17.36 | 5009 |
| Community Characteristics | ||
| State | ||
| Sikkim | 0.74 | 609 |
| Arunachal Pradesh | 2.09 | 5,430 |
| Nagaland | 2.54 | 2,945 |
| Manipur | 5.39 | 3,140 |
| Mizoram | 2.17 | 2,406 |
| Tripura | 7.14 | 1,992 |
| Meghalaya | 10.32 | 6,392 |
| Assam | 69.62 | 10,285 |
| Place of Residence | ||
| Rural | 85.16 | 28,227 |
| Urban | 14.84 | 4972 |
| Mother's Characteristics | ||
| Age | ||
| 15–19 | 4.29 | 1087 |
| 20–24 | 27.81 | 7614 |
| 25–29 | 33.94 | 11,185 |
| 30–34 | 20.26 | 7490 |
| 35–39 | 10.47 | 4223 |
| 40–44 | 2.57 | 1222 |
| 45–49 | 0.66 | 378 |
| Education | ||
| Illiterate | 15.13 | 5264 |
| Primary | 16.51 | 5739 |
| Secondary | 61.01 | 19,617 |
| Higher | 7.35 | 2579 |
| Religion | ||
| Hindu | 45.32 | 9814 |
| Muslim | 33.34 | 4844 |
| Christian | 18.36 | 15,484 |
| Others | 3 | 3057 |
| Caste | ||
| SC | 15.71 | 2338 |
| ST | 40.35 | 19,979 |
| OBC | 27.02 | 3539 |
| Others | 16.91 | 2485 |
| Household Characteristics | ||
| Wealth Index | ||
| Poorest | 40.57 | 12,427 |
| Poorer | 31.85 | 10,456 |
| Middle | 15.61 | 5980 |
| Richer | 8.8 | 3285 |
| Richest | 3.17 | 1051 |
| Sanitation Facilities | ||
| Not improved | 65.8 | 24,578 |
| Improved | 34.2 | 8312 |
| Water facilities | ||
| Not improved | 17.05 | 5981 |
| Improved | 82.95 | 27,218 |
| Number of living children | ||
| one child | 35.61 | 9919 |
| two child | 35.84 | 11,001 |
| three or more children | 28.56 | 12,279 |
| Child Characteristics | ||
| Sex of the child | ||
| Male | 50.71 | 16,816 |
| Female | 49.29 | 16,383 |
| Birth Order | ||
| 1 BO | 41.62 | 12,304 |
| 2 BO | 31.93 | 9794 |
| 3 BO | 13.36 | 5031 |
| 4 plus BO | 13.1 | 6070 |
| Child's Age | ||
| within 6 months | 8.66 | 2875 |
| 6–12 months | 11.35 | 3753 |
| 1to less than 2 years | 17.35 | 5630 |
| 2 to 5 years | 62.64 | 20,941 |
| Caesarean delivery | ||
| No | 82.27 | 28,666 |
| Yes | 17.73 | 4533 |
| Stunting | ||
| No | 64.84 | 20,411 |
| Yes | 35.16 | 10,984 |
| Total | 100 | 33,199 |
From Table 3, it is observed that within the overall sample data, the prevalence of diarrhoea shows a high association with living in each of the North-East states of India. The place of residence whether rural or urban showed a statistically highly significant (p < 0.01) relationship with diarrhoea among under 5 children. Age of the mother was statistically significantly (p < 0.05) associated with prevalence of diarrhoea among children Similary, her educational level, religion, caste were all statistically highly significantly (p < 0.01) associated with the prevalence of diarrhoea among children. The wealth index of the family, sanitation facilities, were statistically highly significantly (p < 0.05) associated with the prevalence of diarrhoea among children while the water facilities was not associated statistically. Sex of the children and no. of living children in the family did not show any statistically significant relationship with childhood diarrhoea. In contrast, birth order of the child, stunted growth, child’s age and the type of delivery of the child were statistically significantly highly associated with diarrhoea.
Table 3.
The association of Diarrhoea, Fever and ARI with various community, household, individual and child characteristics for under-5 children in North-East Indian States, 2019–21
| Diarrhoea | Chi-square | Fever | Chi-square | ARI | Chi-square | ||||
|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | ||||
| Community characteristics | |||||||||
| State/Region | |||||||||
| Sikkim | 578 (572.3) | 31(36.7) | 𝜒2 = 238.4128, p < 0.01 | 528(517.1) | 81(91.9) | 𝜒2 = 839.0456, p < 0.01 | 596(588.1) | 7(14.9) | 𝜒2 = 201.8196, p < 0.01 |
| Arunachal Pradesh | 5119(5103.20) | 311(326.8) | 4966(4610.7) | 464(819.3) | 5266(5258.5) | 5266(133.5) | |||
| Nagaland | 2830(2767.80) | 115(177) | 2692(2500.7) | 253(444.3) | 2888(2846.7) | 31(72.3) | |||
| Manipur | 2986(2951) | 154(189) | 2762(2666.2) | 378(473.8) | 3063(3063.9) | 51(77.1) | |||
| Mizoram | 2324(2261) | 82(144.8) | 2215(2043) | 191(363) | 2377(2329.8) | 12(59.2) | |||
| Tripura | 1864(1872) | 128(119.9) | 1641(1691) | 351(300.5) | 1941(1924.1) | 32(48.9) | |||
| Meghalaya | 5761(6007.30) | 631(384.7) | 4856(5427.6) | 1536(964.4) | 6053(6187.9) | 292(147.1) | |||
| Assam | 9739(9666) | 546(619) | 8530(8733.2) | 1755(1551.8) | 9953(9965) | 265(253) | |||
| Place of Residence | |||||||||
| Rural | 26,469(26,528.2) | 1758(1698.8) | 𝜒2 = 14.6711, p < 0.01 | 23,904(23,968.2) | 4323(4258.2) | 𝜒2 = 7.6022, P < 0.01 | 27,310(27,328.1) | 712(693.9) | 𝜒2 = 3.2367, p = 0.072 |
| Urban | 4732(4672.8) | 240(299.2) | 4286(4221.8) | 686(750.2) | 4827(4808.9) | 104(122.1) | |||
| Mothers characteristics | |||||||||
| Age | |||||||||
| 15–19 | 1004(1021.6) | 83(65.4) | 𝜒2 = 16.1010, p < 0.05 | 888(923) | 199(164) | 𝜒2 = 29.5204, P < 0.01 | 1061(1059.1) | 25(26.9) | 𝜒2 = 9.0340, p = 0.172 |
| 20–24 | 7107(7155.8) | 507(458.2) | 6392(6465.2) | 1222(1148.8) | 7393(7399.1) | 194(187.9) | |||
| 25–29 | 10,533(10,511.9) | 652(673.1) | 9490(9497) | 1695(1687.6) | 10,815(10,828.1) | 288(274.9) | |||
| 30–34 | 7066(7039.2) | 424(450.8) | 6457(6359.9) | 1033(1130.1) | 7263(7233.3) | 154(183.7) | |||
| 35–39 | 3994(3968.8) | 229(254.2) | 3605(3585.8) | 618(637.2) | 4065(4078.4) | 117(103.6) | |||
| 40–44 | 1143(1148.5) | 79(73.5) | 1024(1037.6) | 198(184.4) | 1179(1175.2) | 26(29.8) | |||
| 45–49 | 354(355.3) | 24(22.7) | 334(321) | 44(57) | 361(363.8) | 12(9.2) | |||
| Education | |||||||||
| Illiterate | 4928(4947.2) | 336(316.8) | 𝜒2 = 59.0396, p < 0.01 | 4533(4469.8) | 731(794.2) | 𝜒2 = 29.5539, p < 0.01 | 5073(5095.6) | 152(129.4) | 𝜒2 = 23.9420, p < 0.01 |
| Primary | 5295(5393.6) | 444(345.4) | 4787(4873.1) | 952(865.9) | 5509(5548.1) | 180(140.9) | |||
| Secondary | 18,494(18,436.4) | 1123(1180.6) | 16,615(16,657.2) | 3002(2959.8) | 19,038(18,992.7) | 437(482.3) | |||
| Higher | 2484(2423.8) | 95(155.2) | 2255(2189.9) | 324(389.1) | 2517(2500.5) | 47(63.5) | |||
| Religion | |||||||||
| Hindu | 9305(9223.4) | 509(590.6) | 𝜒2 = 18.6605, p < 0.01 | 8340(8333.3) | 1474(1480) | 𝜒2 = 64.1915, p < 0.01 | 9537(9500.8) | 205(241.2) | 𝜒2 = 17.6036, p < 0.01 |
| Muslim | 4536(4552.5) | 308(291.5) | 3941(4113.1) | 903(730.9) | 4660(4695.8) | 155(119.2) | |||
| Christian | 14,513(14,552.1) | 971(931.9) | 13,246(13,147.8) | 2238(2336.2) | 14,993(14,985.5) | 373(380.5) | |||
| Others | 2847(2873) | 210(184) | 2663(2595.8) | 394(461.2) | 2947(2955) | 83(75) | |||
| Caste | |||||||||
| SC | 2223(2197.7) | 115(140.3) | 𝜒2 = 13.4294, p < 0.01 | 2032(1996.3) | 306(341.7) | 𝜒2 = 56.5506, p < 0.01 | 2265(2264.2) | 55(55.8) | 𝜒2 = 12.4418, p < 0.01 |
| ST | 18,717(18,779.9) | 1262(1199.1) | 17,202(17,059.1) | 2777(2919.9) | 19,322(19,342.6) | 497(476.4) | |||
| OBC | 3340(3326.6) | 199(212.4) | 2900(3021.8) | 639(517.2) | 3423(3428.6) | 90(84.4) | |||
| Others | 2360(2335.9) | 125(149.1) | 2065(2121.8) | 420(363.2) | 2438(2412.6) | 34(59.4) | |||
| Household characteristics | |||||||||
| Wealth Index | |||||||||
| Poorest | 11,560(11,679.1) | 867(747.9) | 𝜒2 = 54.3417, p < 0.01 | 10,392(10,552) | 2035(1875) | 𝜒2 = 65.6077, p < 0.01 | 11,974(12,039.3) | 371(305.7) | 𝜒2 = 31.8976,p < 0.01 |
| Poorer | 9832(9826.7) | 624(629.3) | 8801(8878.4) | 1655(1577) | 10,124(10,121) | 254(257) | |||
| Middle | 5647(5620.1) | 333(359.9) | 5188(5077.7) | 792(902.3) | 5804(5778.3) | 121(146.7) | |||
| Richer | 3146(3087.3) | 139(197.7) | 2888(2789.4) | 397(495.6) | 3209(3182.2) | 54(80.8) | |||
| Richest | 1016(987.7) | 35(63.3) | 921(892.4) | 130(158.6) | 1026(1016.2) | 16(25.8) | |||
| Sanitation Facilities | |||||||||
| Not improved | 7735(7811.4) | 577(500.6) | 𝜒2 = 16.5842, p < 0.01 | 6855(7058.5) | 1457(1253.5) | 𝜒2 = 52.0629, p < 0.01 | 7997(8043.1) | 252(205.9) | 𝜒2 = 14.1374, p < 0.01 |
| Improved | 23,174(23,097.6) | 1404(1480) | 21,075(20,871.5) | 3503(3706.5) | 23,833(23,786.9) | 563(609.1) | |||
| Water facilities | |||||||||
| Not improved | 5618(5621) | 363(360) | 𝜒2 = 0.0335, p = 0.855 | 5083(5078.6) | 898(902.4) | 𝜒2 = 0.0308, p = 0.861 | 5791(5796.8) | 153(147.2) | 𝜒2 = 0.2871, p = 0.592 |
| Improved | 25,583(25,580) | 1635(1638) | 23,107(23,111.4) | 4111(4106.6) | 26,346(26,340.2) | 663(668.8) | |||
| Child characteristics | |||||||||
| Sex of the child | |||||||||
| Male | 15,805(15,804) | 1011(1012) | 𝜒2 = 0.0023, P = 0.962 | 14,301(14,278.8) | 2515(2537.2) | 𝜒2 = 0.4621, p = 0.497 | 16,248(16,283.5) | 449(413.5) | 𝜒2 = 6.3499, p < 0.05 |
| Female | 15,396(15,397) | 987(986) | 13,889(13,911.2) | 2494(2471.8) | 15,889(15,853.5) | 367(402.5) | |||
| Birth Order | |||||||||
| 1 BO | 11,598(11,563.5) | 706(740.5) | 𝜒2 = 23.4181, P < 0.01 | 10,482(10,447.6) | 1822(1856.4) | 𝜒2 = 47.9692, p < 0.01 | 11,948(11,907.6) | 262(302.4) | 𝜒2 = 41.5336, p < 0.01 |
| 2 BO | 9229(9204.6) | 565(589.4) | 8380(8316.3) | 1414(1477.7) | 9506(9489.1) | 224(240.9) | |||
| 3 BO | 4750(4728.2) | 281(302.8) | 4342(4271.9) | 689(759.1) | 4877(4864.5) | 111(123.5) | |||
| 4 plus BO | 5624(5704.7) | 446(365.3) | 4986(5154.2) | 1084(915.8) | 5806(5875.8) | 219(149.2) | |||
| Stunting | |||||||||
| No | 19,223(19,171.8) | 1188(1239.2) | 𝜒2 = 6.4269, p < 0.05 | 17,385(17,298.8) | 3026(3112.2) | 𝜒2 = 8.0515, p < 0.01 | 19,817(19,764.2) | 455(507.8) | 𝜒2 = 16.1130, p < 0.01 |
| Yes | 10,266(10,317.2) | 718(666.8) | 9223(9309.2) | 1761(1674.8) | 10,579(10,631.8) | 326(273.2) | |||
| Child Age | |||||||||
| within 6 months | 2755(2702.0) | 120(173) | 𝜒2 = 109.5894, p < 0.01 | 2558(2441.2) | 317(433.8) | 𝜒2 = 176.9798, p < 0.01 | 2819(2803.8) | 56(71.2) | 𝜒2 = 17.1754, p < 0.01 |
| 6–12 months | 3426(3527.1) | 327(225.9) | 3011(3186.8) | 742(566.2) | 3639(3660.1) | 114(92.9) | |||
| 1to less than 2 years | 5198(5291.2) | 432(338.8) | 4587(4780.6) | 1043(849.4) | 5461(5490.6) | 169(139.4) | |||
| 2 to 5 years | 19,822(19,680.7) | 1119(1260.3) | 18,034(17,781.5) | 2907(3159.5) | 20,218(20,182.5) | 477(512.5) | |||
| C-section delivery | |||||||||
| No | 26,985(26,940.8) | 1,681(1,725.2) | 𝜒2 = 8.8218, p < 0.01 | 24,452(24,340.9) | 4214(4325.1) | 𝜒2 = 24.6019, p < 0.01 | 27,793(27,745.5) | 657(704.5) | 𝜒2 = 24.0263, p < 0.01 |
| Yes | 4,216(4,260.2) | 317(272.8) | 3,738(3849.1) | 795(683.9) | 4344(4391.5) | 159(111.5) | |||
| No. of children living | |||||||||
| one child | 9,291(9,322.0) | 628(597.0) | 𝜒2 = 5.6483, p = 0.059 | 8286(8422.4) | 1633(1496.6) | 𝜒2 = 25.3133, p < 0.01 | 9,648(9632.4) | 229(244.6) | 𝜒2 = 18.3698, p < 0.01 |
| two child | 10,386(10,338.9) | 615(662.1) | 9463(9341.2) | 1538(1659.8) | 10,679(10,637.9) | 229(270.1) | |||
| three or more | 11,524(11,540.0) | 755(739.0) | 10,441(10,426.4) | 1838(1852.6) | 11,810(11,866.7) | 358(301.3) | |||
Note the no. in the bracket() indicate the estimated frequency
From Table 3 further, it is evident that within the overall sample data, prevalence of fever showed a statistically highly significant (p < 0.01) association with the states of North-East India. The place of residence, age of the mother, education level, religion she belongs to, caste and wealth index were also statistically highly associated with fever. Water facilities was not associated while sanitation facilities and stool disposal was significantly associated with fever. Sex of the child was not associated with fever. In contrast, the birth order of the child, stunting growth, age of the child and the number of children living in the family was statistically highly associated with fever.
Furthermore, From Table 3 we notice that from the overall sample data ARI was highly associated with each of the North-East states of India. Children living in the rural and urban had not much association with ARI. The mother age had no association with the ARI illnesses but education of the mother was highly associated with ARI on their children. Religion, Caste, family wealth, sanitation facilities and stool disposal had association with ARI.While water facilities had no association with ARI. Sex of the child was associated with 0.05% level of significance. Birth order of the child, stunting growth, the age of the child and the number of children were also associated with ARI.
From Table 4, we found that among the northeastern states, prevalence of diarrhoea in Meghalaya was nearly 10 percent followed by Tripura with 6 percent. In contrast, the lowest prevalence lied in the state of Nagaland of with 3.4 percent children suffered diarrhoea. Except Mizoram where the prevalence of diarrhoea among children was 4.3 percent, rest all four states had diarrhoea nearly 5 percent. For the entire northeastern region, the prevalence was nearly 6 percent and all proportions were statistically highly significant (p < 0.01). Prevalence of diarrhoea was higher in rural area (6.2%) than urban areas (4.3%). Among the children, the prevalence of diarrhoea among both male and female under 5 years children were nearly 6 percent. Although they were statistically highly significant, there was not much difference in prevalence of diarrhoea among stunted and not stunted children (p < 0.01). Among the different age group children, the prevalence of diarrhoea was highest among the children in the age group of 6–12 months (9.2%) followed by children of 1 to less than 2-year-old (7.1%), then among the children of 2 to 5 years old (5.4%) and least among children of less than 6 months (3.7%).The prevalence of diarrhoea was higher among children who were delivered not by cesearean (6.2%) than those who were delivered by cesearean (4.5%). Mother in age group 45–49 shows that the prevalence of diarrhoea is highest among their children (7.2%) and for other age group women the prevalence of diarrhoea among their children was nearly 6 percent. It was observed that among the mother who completed their primary education, the prevalence of diarrhoea among their children was nearly 8 percent and among the children of illiterate women the prevalence of diarrhoea was 6.7 percent. The lowest prevalence of diarrhoea was observed among children of higher educated mother. Among religion the prevalence of diarrhoea among Hindu children was 4.8 percent followed by Muslim (6.5%) and among Chistian and other religion children it was nearly 7 percent.
Table 4.
The prevalence of diarrhoea, fever and ARI among under-5 years children by different socio-economic and demographic characteristics in North-East India, 2019–2021
| Variables/Characteristics | Diarrhoea | SE | Fever | SE | ARI | SE |
|---|---|---|---|---|---|---|
| Community characteristics | ||||||
| State/Region | ||||||
| Sikkim | 5.5*** | 1.386 | 18.1*** | 2.566 | 0.7** | 0.344 |
| Arunachal Pradesh | 5.1*** | 0.324 | 9.0*** | 0.468 | 2.1*** | 0.208 |
| Nagaland | 3.4*** | 0.372 | 8.8*** | 0.643 | 1.1*** | 0.22 |
| Manipur | 5.5*** | 0.539 | 13.0*** | 0.775 | 1.7*** | 0.299 |
| Mizoram | 4.3*** | 0.664 | 10.1*** | 0.973 | 0.6*** | 0.226 |
| Tripura | 6.2*** | 0.574 | 16.9*** | 0.923 | 1.3*** | 0.249 |
| Meghalaya | 10.4*** | 0.546 | 22.9*** | 0.697 | 4.8*** | 0.387 |
| Assam | 5.5*** | 0.261 | 17.7*** | 0.441 | 2.5*** | 0.172 |
| North-East India | 5.9*** | 0.198 | 17.4*** | 0.327 | 2.51*** | 0.129 |
| Place of Residence | ||||||
| Rural | 6.2*** | 0.222 | 16.4*** | 0.843 | 2.54*** | 0.141 |
| Urban | 4.3*** | 0.388 | 17.5*** | 0.355 | 2.31*** | 0.317 |
| Mother’s characteristics | ||||||
| Age | ||||||
| 15–19 | 6.3*** | 0.921 | 18.8*** | 1.717 | 2.8*** | 0.602 |
| 20–24 | 6.6*** | 0.408 | 19.1*** | 0.687 | 2.41*** | 0.263 |
| 25–29 | 5.5*** | 0.324 | 18.0*** | 0.561 | 2.75*** | 0.241 |
| 30–34 | 6.1*** | 0.447 | 14.8*** | 0.65 | 2.01*** | 0.239 |
| 35–39 | 5.3*** | 0.561 | 15.3*** | 0.868 | 2.31*** | 0.335 |
| 40–44 | 5.8*** | 1.051 | 16.8*** | 1.804 | 3.62*** | 0.451 |
| 45–49 | 7.2*** | 2.289 | 16.3*** | 3.606 | 1.21** | 2.399 |
| Education | ||||||
| Illiterate | 6.7*** | 0.55 | 16.6*** | 0.812 | 3.11*** | 0.367 |
| Primary | 7.9*** | 0.569 | 17.9*** | 0.81 | 3.26*** | 0.377 |
| Secondary | 5.6*** | 0.242 | 17.8*** | 0.426 | 2.28*** | 0.157 |
| Higher | 3.1*** | 0.509 | 13.9*** | 1.072 | 1.43*** | 0.319 |
| Religion | ||||||
| Hindu | 4.8*** | 0.274 | 16.4*** | 0.484 | 1.86*** | 0.164 |
| Muslim | 6.5*** | 0.413 | 18.9*** | 0.671 | 3.16*** | 0.289 |
| Christian | 7.5*** | 0.35 | 17.4*** | 0.473 | 2.93*** | 0.226 |
| Others | 7.4*** | 0.742 | 15.1*** | 1.024 | 8.99*** | 0.389 |
| Caste | ||||||
| SC | 4.1*** | 0.529 | 14.4*** | 0.966 | 1.91*** | 0.34 |
| ST | 6.7*** | 0.31 | 16.2*** | 0.426 | 2.79*** | 0.19 |
| OBC | 5.6*** | 0.461 | 18.9*** | 0.809 | 2.28*** | 0.296 |
| Others | 5.2*** | 0.585 | 17.2*** | 1.021 | 4.04*** | 0.284 |
| Household characteristics | ||||||
| Wealth Index | ||||||
| Poorest | 7.2*** | 0.354 | 18.1*** | 0.53 | 3.03*** | 0.231 |
| Poorer | 5.8*** | 0.345 | 18.1*** | 0.576 | 2.54*** | 0.222 |
| Middle | 5.1*** | 0.427 | 16.5*** | 0.815 | 1.9*** | 0.282 |
| Richer | 3.2*** | 0.449 | 14.3*** | 1.027 | 1.5*** | 0.311 |
| Richest | 2.1*** | 0.546 | 12.7*** | 1.589 | 1.27*** | 0.447 |
| Sanitation Facilities | ||||||
| Not improved | 6.5*** | 0.385 | 19.4*** | 0.628 | 3.01*** | 0.25355 |
| Improved | 5.6*** | 0.227 | 16.4*** | 0.379 | 2.28*** | 0.1479 |
| Water facilities | ||||||
| Not improved | 6.0*** | 0.479 | 16.4*** | 0.732 | 2.78*** | 0.328 |
| Improved | 5.9*** | 0.217 | 17.6*** | 0.364 | 2.45*** | 0.14 |
| Child characteristics | ||||||
| Sex of the child | ||||||
| Male | 6.0*** | 0.282 | 17.31*** | 0.456 | 2.82*** | 0.192 |
| Female | 5.9*** | 0.277 | 17.42*** | 0.469 | 2.18*** | 0.172 |
| Birth Order | ||||||
| 1 BO | 5.2*** | 0.283 | 17.5*** | 0.527 | 2.11*** | 0.19 |
| 2 BO | 5.8*** | 0.353 | 17*** | 0.578 | 2.49*** | 0.228 |
| 3 BO | 6.0*** | 0.558 | 16.16*** | 0.836 | 2.65*** | 0.375 |
| 4 plus BO | 8.7*** | 0.631 | 19.03*** | 0.844 | 3.67*** | 0.387 |
| Stunting | ||||||
| No | 5.8*** | 0.253 | 17.56*** | 0.424 | 2.27*** | 0.159 |
| Yes | 6.3*** | 0.347 | 17.78*** | 0.568 | 3*** | 0.242 |
| Child Age | ||||||
| within 6 months | 3.7*** | 0.486 | 11.78*** | 1.004 | 2.11*** | 0.408 |
| 6–12 months | 9.2*** | 0.705 | 22.41*** | 1.042 | 3.09*** | 0.388 |
| 1to less than 2 years | 7.1*** | 0.518 | 19.99*** | 0.822 | 3.02*** | 0.345 |
| 2 to 5 years | 5.4*** | 0.241 | 16.49*** | 0.406 | 2.31*** | 0.159 |
| Delivery by C-section | ||||||
| no | 6.2*** | 0.224 | 17.34*** | 0.357 | 2.6*** | 0.147 |
| yes | 4.5*** | 0.409 | 17.44*** | 0.809 | 1.9*** | 0.26 |
| No. of children living | ||||||
| One child | 5.6*** | 0.322 | 18.8*** | 0.59 | 2.1*** | 0.208 |
| two child | 5.4*** | 0.324 | 16.4*** | 0.538 | 2.3*** | 0.205 |
| three or more | 6.9*** | 0.39 | 16.6*** | 0.558 | 3.2*** | 0.266 |
*** means p < 0.01
** means p < 0.05
There was a greater chance of children being influence by diarrhoea among Schedule Tribe, children belonged to the poorest family and the household which have no improved sanitation and water facilities.
The data from Table 4 further indicated a statistically significantly higher prevalence of fever in Meghalaya (23%) and lowest in Arunachal Pradesh (9%). In most cases, urban areas showed a higher prevalence than rural areas. Among children, female exhibited a notably higher prevalence with fever than male and children with stunted growth. Children aged 6–12 months have high prevalence with fever, and most were born with the caesarean section birth. Mothers in the 15 to 19 years and 20–24 age group had children with higher fever prevalence than other age groups. Additionally, mothers who have completed up to primary or secondary education showed relatively higher likelihood of prevalence of fever among their children. The majority of children with higher prevalence of fever belonged to the Muslim religion and were part of the OBC. Children from the poorest families were notably more prone to fever and often lacked improved sanitation while water facilities are improved.
Data from Table 4 furthermore, highlighted the statistically significantly higher prevalence of ARI was found in Megalaya (4.8%) followed by Assam (2.5%),Arunachal Pradesh (2.1%) while in the states like Mizoram and Sikkim it was less than 1 percent.In most cases, rural areas exhibited a higher prevalence of ARI than urban areas. Among children, males showed a significantly higher prevalence with ARI than females and most children with stunted growth. Children aged 6–12 months and those children born with not cesearean delivery were linked to higher ARI. Prevalence of ARI was highest among the children of mothers with the 40–44 age group. Furthermore, mothers who completed primary education had a higher prevalence of ARI to their children.Among religion other than Hindu, Muslim and Christian the prevalence of ARI was highest i.e. 9 percent. Similarly among the children of Other caste women,the prevalence of ARI was 4 percent and higher than ST,SC and OBCs. Children from the poorest families were notably more prone to ARI and often lacked improved sanitation and water facilities.
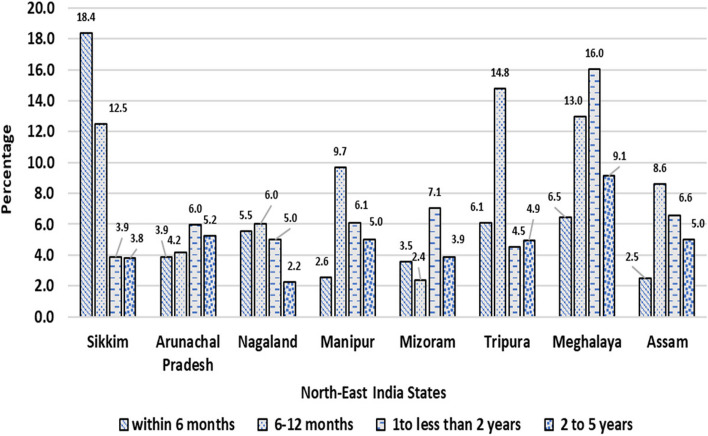
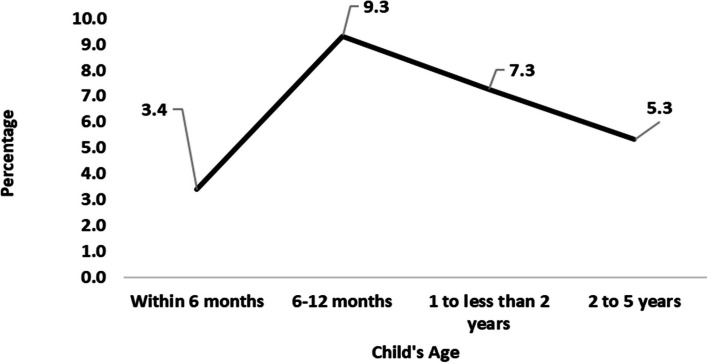
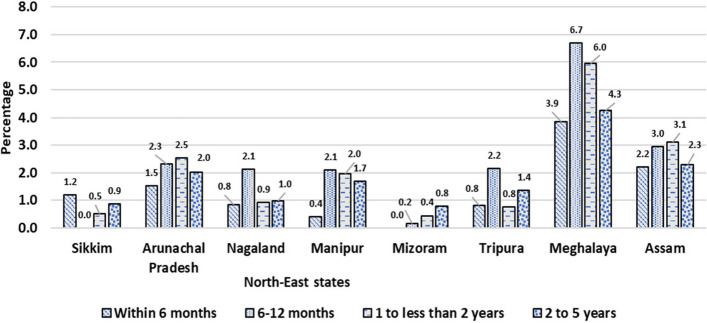
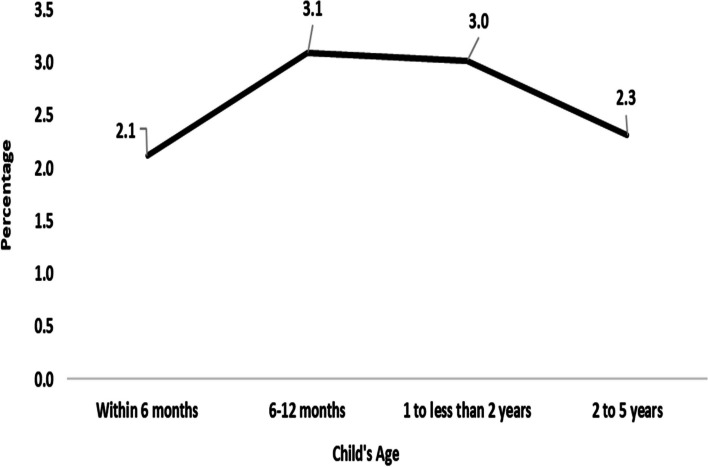
In Figs. 1 and 2 show the prevalence of diarrheoa by different age group of children in state wise and the entire north east states of India. we see that Sikkim has the highest prevalence of diarrhoea in the age group within 6 months; Meghalaya has the highest prevalence in the age group 6- 12 months and 1- 2 years old children; Arunachal Pradesh has the highest rate in the age group 2- 5 years old children. We also observed that within the entire north east states 6 -12 months old children have highly prevalence with diarrhoea.
Fig. 1.
Prevalence of diarrhoea by age groups of under-5 children in North-East Indian States,India,2019–21
Fig. 2.
Prevalence of diarrhoea by age groups of under-5 children in North-East region,India,2019–21
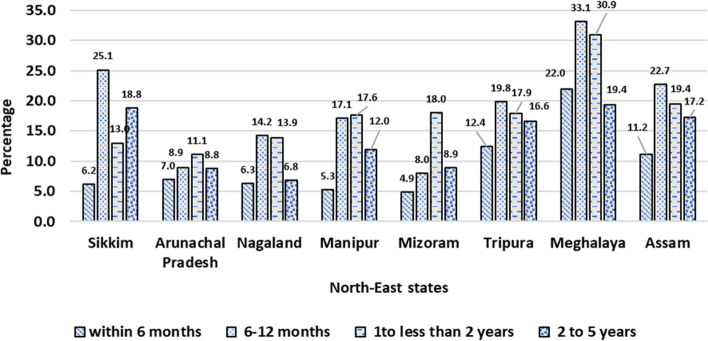
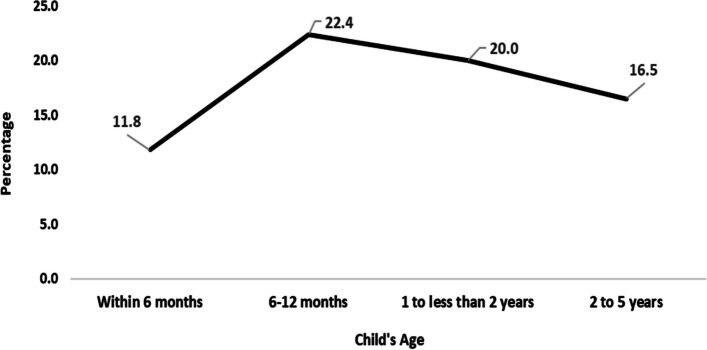
In Figs. 3 and 4 depict the prevalence of fever among children across different age groups in both individual states and the entire Northeastern region of India. Meghalaya stands out with the highest prevalence of fever within the 6-month age group. Meghalaya exhibits the highest prevalence in children aged 6–12 months and 1–2 years old, at the same time Meghalaya records the highest rates among children aged 2–5 years. A noticeable trend across all the Northeastern states is the heightened prevalence of fever among children aged 6–12 months.
Fig. 3.
Prevalence of fever by age groups of under-5 children in North-East Indian States, India,2019–21
Fig. 4.
Prevalence of fever by age groups of under-5 children in North-East region,India,2019–21
Figures 5 and 6, illustrate the prevalence of ARI among children across different age groups in both individual states and the entirety of the northeastern states of India. Notably, Meghalaya shows the highest prevalence of ARI within the 6-month age group. In Meghalaya, the highest prevalence is seen among children aged 6–12 months and those between 1–2 years old, and records the highest rates among children aged 2–5 years. An overarching observation across the entire northeastern region is the heightened prevalence of ARI among children aged 6–12 months.
Fig. 5.
Prevalence of ARI by age groups of under-5 children in North-East Indian States, India,2019–21
Fig. 6.
Prevalence of ARI by age groups of under-5 children in North-East region,India,2019–21
For diarrhoea
Table 5 indicates the result of the logistic regression of the factors affecting the diarrhoea among under-5 year children in Northeast Indian states. In Model 1, after adjusting for household, mother and child covariates, the odds of having diarrhoea was 2.6 times more in Meghalaya than in Sikkim. It was statistically highly significant (AOR = 2.66 and p < 0.01). If we examined the mother characteristics, for the children of the women who received higher education, the odds of having diarrhoea was 36 percent lesser as comparison to the children of illiterate women. In religion, the children who were born to a Muslim women had 65 percent higher chance of getting diarrhoea as comparison to the children born to a Hindu woman and it was statistically highly significant (p < 0.01). The odds of having diarrhoea among children born to a ST woman was 38 percent higher as comparison to Other caste woman (p < 0.05) and among children of OBC women the odds of having diarrhoea was 40 percent higher as comparison to Other caste women (p < 0.05). The odds of having diarrhoea among children of poorer women was 13 percent lesser as comparison to children of poorest women. Similarly among the household characteristics, the children living in the household with unimproved sanitation facilities had a 16 percent higher chance of getting diarrhoea compared to the household with improved sanitation facilities, which was statistically significant (p < 0.05). In child characteristics, as we move from children with 1st birth order to 2nd,3rd and 4 plus birth order, the odds of getting diarrhoea was more likely and statistically highly significant (p < 0.01). Similarly, the odds of having diarrhoea was 2.18 times higher among children of 6 to 12 months as comparison to children with age less than 6 months and the odds of having diarrhoea was 96 percent higher among the children aged 1 to less than 2 years as comparison to children with age less than 6 months. Again, the odds of having diarrhoea among children aged 2 to 5 years was 39 percent more as comparison to the children aged less than 6 months and it was statistically highly significant (p < 0.01). The odds of having diarrhoea among children who were born by caesarean delivery had 62 percent higher as comparison to the reference category and it was statistically highly significant (p < 0.01).In Model 2,when we adjust for programme factors like BCG,DPT and Rota virus in the Model1,the significance level of the covariate remain nearly same and the effect of the programme factors on the childhood diarrhoea was found to be insignificant. The covariates like place of residence, mother’s age, number of children living, child being stunted were insignificant.
For fever
Table 5 shows the Adjusted odds ratio (AOR) from the logistic regression to examine the factors affecting fever among under 5 year children in Northeast Indian states. Results from Model 1 showed that the in comparison to the fever among children in Sikkim, the odds of fever in Arunachal Pradesh was 28 percent less and in Mizoram it is 30 percent less respectively and it was statistically significant (p < 0.05). In Meghalaya the odds of fever is 2.59 times higher compared to the fever among children in Sikkim, which was statistically highly significant (p < 0.01). In rural areas, the odds of having fever was lower compared to urban areas (AOR = 0.86, p < 0.01). The odds of having fever among children of the women who received primary or secondary education was higher in comparison to the illiterate women. Muslim children (AOR = 1.27, p < 0.05) and the children of other religion (AOR = 1.27, p < 0.01) were more likely to get fever in comparison to Hindu children. Among the caste group, the odds of having fever was lower among the children of SC (AOR = 0.78,p < 0.01) and ST women (AOR = 0.76, p < 0.01) in comparison to children of Other caste group women. The children belonged to the middle and richer wealth Index, the odds of having fever was lower than the poorest wealth index. The chance of having fever among children living in a household with unimproved sanitation was 15 percent higher compared to the children living in a household with improved sanitation facilities. It was statistically highly significant (p < 0.01). Compared to the household with 1 child, the odds of having fever in the two children household was 37 percent lesser and for 3 or more children household it was 57 percent lesser and the result was statistically highly significant (p < 0.01). For Birth order of the children, the odds of having fever was 40 percent higher for 2nd birth order children and 87 percent higher for 3rd birth order children compared to 1st birth order children. It was statistically highly significant (p < 0.01). The odds of having fever among 4 plus birth order children was 2.53 times higher compared to 1st birth order child (p < 0.01). Among the children of different ages, the odds of having fever was respectively 99 percent higher (p < 0.01) among 6 to 12 months old children,91 percent higher(p < 0.01) for 1 to less than 2 year old children and 36 percent higher (p < 0.01) for 2 to 5 years old children in comparison to the children of less than 6 months. The children who were born out of caesarean delivery, the odds of having fever was 31 percent higher in comparison to the reference category and it was statistically highly significant (p < 0.01). When we added programme factors in Model 1,in the Model 2, the odds of having fever was higher for Tripura, Meghalaya and Assam than Sikkim. Other covariates of the model showed the similar statistically significant relationship as in Model 1. However, among the programme factors, the children who received Rota virus vaccine, the chance of having fever among children was 13 percent lesser than those who didn’t receive. In Model 1, mother’s age, and child being stunted was insignificantly affecting fever among children and In Model 2, factors like mother’s age, religion, sanitation facilities, number of living children, stunting, BCG and DPT vaccination were insignificantly affecting fever among children.
For ARI
Table 5 showed the Adjusted odds ratio (AOR) from the logistic regression to examine the factors affecting ARI among under 5-year children in Northeast Indian states. From Model 1,we found that in the state of Meghalaya the children had 5.17 times more chance of getting ARI than the children of Sikkim, which was statistically highly significant (p < 0.01). The chances of getting ARI among children belonging to the SC caste group was 2.08 times higher in comparison with children of Other caste group. Similarly, in comparison with children of Other caste group, the chances of getting ARI was 88 percent more among children of ST caste group and 2.37 higher among OBC children respectively and the results were statistically highly significant (p < 0.01). For the children who belong to richer wealth category, the odds of getting ARI was 36 percent lower compared to children from the poorest wealth category (p < 0.05). For the birth order, the children who belonged to 4 or higher birth order had a higher chance of getting ARI than 1st birth order children (AOR = 1.84, p < 0.05). If we examine the child’s age, in comparison to the children aged less than 6 months, the odds of getting ARI was 89 percent higher for children of 6 to 12 months and 70 percent more for children of the 1 to 2 year age respectively. The children who were born out of caesarean delivery, the chances of getting ARI was 2.12 times higher as comparison to those children who was not delivered by caesarean and the result was statistically highly significant (p < 0.01). If we add programme factors like BCG, DPT and Rota virus in Model 1, in Model 2, the results showed that the chances of getting ARI was higher in Tripura, Meghalaya and Assam than in Sikkim state. The rural children had lower chance of ARI than urban children. The children with secondary education had higher chance of getting ARI in comparison to illiterate women children. Other factors were similarly affecting the ARI among children as in Model 1. Among the programme factors, the chances of getting ARI was 13 percent lower among those who received Rota virus than those who did not. The BCG and DPT vaccination was insignificantly affecting ARI. In Model 1, place of residence, mother’s age, mother’s education, religion, sanitation facilities, number of living children and child being stunted was insignificantly affecting ARI among children. In Model 2, the insignificant factors were mother’s age, religion, sanitation facilities, child being stunted. Some of the highlights of the important findings emerging from previous and current research has been shown in Table 6 as ready reckoner.
Table 6.
Highlights of findings emerged from the present study on the illnesses of Diarrhoea, Fever and ARI in Northeast India,2019–21
| Known about the illnesses (Diarrhoea, Fever & ARI) in India & Northeast from previous studies |
New emerging points from our study about the illnesses (Diarrhoea, Fever & ARI) in the 8 states of Northeast India |
|---|---|
|
• A study using NFHS-4 (2015–16) data revealed that the north-east region as a reference, those from north, central and east regions were more likely to suffer from ARI. Comorbidity, sex, age and nutritional status of children were significantly associated with the prevalence of ARI [51] • It is found that among children in northeast India, the overall incidence of fever remains more or less unchanged but that of cough and diarrhoea have declined considerably during 2004–05 to 2011–12.Girls are less likely to have suffered from diarrhea than the boys; age has a significant effect on the risk of children suffering from fever and cough, toilet and having access to improved sources of drinking water lower the risk of childhood morbidities [27] • In a multicounty study including India, using NFHS4 data it was found that children who were given the measles vaccine were less likely to suffer from Diarrhoea and ARI in India [52] • Using NFHS-4 data, the study results suggests that most districts situated in India’s north and central regions had higher chances of ARI and diarrhoea and cases of diarrhoea may reduce with the improved toilet facilities, female children are less prone to ARI and Diarrhoea; stunted and wasted children are more susceptible to Diarrhoea only; young women with low education level are more likely to have children down with both the diseases, Hindu and ST have less while SC children have more chances of being sick with ARI and diarrhoea [20] • Using NFHS-4 data, the prevalence of diarrhoea and ARI was 13.8% and 3.4% among children in India. Association was observed between exclusive breastfeeding with Diarrhoea and ARI [53] • Using NFHS-4 data, prevalence of diarrhoea in India among under 5 children is higher in rural areas, not staying in Pacca house, living with unimproved sanitation facilities, belonging to under privileged community, children of younger mothers and “poor’ households [16] • Using NFHS-5 data (2019–21) a study on spatial clustering of diarrhoea in India among children under 5 years found that the Prevalence of diarrhoea in Meghalaya (10.5%), is third highest in India, with an increase in children’s age as well as mother's age the prevalence of the diarrhoea decreases. prevalence is more among male children than females, Underweight children have a greater risk of suffering from diarrhoea diseases, the odds of children living in a pucca house are less likely to suffer from diarrhoea. rich economic status reduces the risk of such morbid conditions [2] |
From NFHS-5 (2019–21) data revealed About Diarrhoea • Prevalence of diarrhoea in Meghalaya (10%), Tripura (6%), Assam, Arunachal Pradesh, Sikkim, Manipur lied (5–5.5%), Mizoram (4.3%) and least in Nagaland (3.4%) and overall northeast it is 6% • Among northeast states and age wise prevalence, Sikkim has the highest prevalence (18.4%) of diarrhoea among children of less than 6 months, Meghalaya has highest prevalence of diarrhoea for children of age-group 6–12 months and 1–2 years while Arunachal Pradesh has highest rate of diarrhoea among 2–5 years children • In comparison to the children of less than 6 months, the odds of diarrhoea among 6 to 12 months children were 2.18 times more and for 1–2 years children are 96% higher and for 2 to 5 years it is 39 percent higher • The odds of diarrhoea was higher among children born in cesarean delivery than not cesarean delivery • The vaccinations like BCG, DPT and Rota virus was found to have insignificant effect on diarrhoea in northeast states About Fever • A higher prevalence of fever was observed in Meghalaya (23%) and lowest in Arunachal Pradesh (9%) • Among all age groups of children (less than 6 months,6 to 12 months,1–2 year and 2to 5 years) in northeast Indian states, the prevalence is highest in Meghalaya • Compared to 1st birth order children, the 4 plus birth order children has more than 2 times higher odds of fever • The programme factors like BCG and DPT was insignificant, however the Rota virus vaccination lowers the odds of fever among children • The odds of fever were higher for the children born out of cesarean delivery than not born out of it About ARI • Higher prevalence of ARI was observed in Meghalaya (4.8%) followed by Assam (2.5%), Arunachal Pradesh (2.1%) while Mizoram and Sikkim it is less than 1 percent • Among all age groups of children (less than 6 months,6 to 12 months,1–2 year and 2 to 5 years) in northeast Indian states, the prevalence of ARI is highest in Meghalaya • The odds of ARI were higher for the children born out of cesarean delivery than not born out of it • In comparison to the children of less than 6 months, the odds of ARI among 6 to 12 months children and for 1–2 years children are higher • The vaccinations like BCG, DPT was insignificantly affecting the ARI, however, there is lower odds of ARI among the children who were given Rota virus than those who were not given |
Discussion and conclusion
This study delved into the socio-demographic and environmental aspects associated with diarrhoea, fever and ARI among children below five years old in India and the factors that might contribute to their occurrence. Despite a decline in the prevalence of childhood diarrhoea in recent times, the substantial burden of this preventable illness persists. We used the NFHS-5 dataset to conduct analyses using bivariate and multivariate methods. It was revealed that 5.95 percent,17.36 percent and 2.51 percent of the children had suffered diarrhoea, fever and ARI respectively, two weeks before the survey. In comparison to Sikkim, state of Meghalaya was found to have more diarrhoea, ARI and fever and it was statistically highly significant, however, Tripura and Assam had significant higher odds of having fever and ARI in comparison to Sikkim. After controlling for programme factors (mainly Rota virus) in model 2, the lower odds of having fever in Arunachal Pradesh and Mizoram were found to disappear from the previous model, which shows the impact of Rota virus on the fever among children under 5 years. Results also reveals that these Illnesses more influence the male child.There are some studies in northeast India and other parts of India and world which also found male to be more susceptible to the illnesses than female [27, 54].
The findings of this study indicated that children residing in rural regions were at a higher likelihood of encountering diarrhoea, fever, and ARI compared to those in urban areas which is same in the previous study conducted in India [8]. Clear disparities based on region and location were noticeable, showcasing increased vulnerability to the presence of diarrhoea, fever, and ARI in the northern states region and rural areas [42, 45].
In this study, caste and religion displayed notable associations with childhood diarrheal illnesses. Specifically, the research identified that children from scheduled tribes and other caste groups exhibited a reduced risk of diarrhea in comparison to those from scheduled castes. This discovery aligns with similar findings from prior studies conducted in India [55].
This study demonstrated a significant correlation between the household's wealth status and recent diarrhea among children. The research findings highlighted a decreased probability of diarrhea in children from the wealthiest wealth quintile compared to those in the poorest. A similar study in Peru has the same contribution [9]. Thus, the government's initiatives to elevate the incomes of impoverished individuals through the execution of the objectives outlined in the National Development Plan (2010- 15) serve as a crucial means toward achieving Millennium Development Goals MDG 4. The odds of having diarrhoea among children who were born by caesarean delivery had higher as comparison to the home or normal delivery. Similar findings was also found in the previous studies where the reported c-section was associated to the risk of gastroenteritis among children aged > 1 year and also less than 1 year [56–58].
Our findings shows that those who have unimproved sanitation facilities is highly associated with diarrhoea and fever. This outcome aligns with findings from a study in India [3, 46].
According to the findings of this study, there exists an association between the occurrence of diarrhoea, fever, and ARI and factors such as the age of the child and caregiver, the wealth status of the household, the quality of sanitation facilities, methods of stool disposal, and the educational level of the caregiver. It suggests directing efforts toward implementing programs that aim to decrease diarrhoea and ARI among children under five by addressing socioeconomic barriers that hinder caregivers' access to wealth and education. The window of opportunity to prevent the co-occurrence of diarrhoea, fever, and ARI in children under 5 years old is crucial during the age range of 2 to 5 years. The window of opportunity to prevent these childhood illnesses relates to the proper nutrition and follow of timely immunisation schedule, adequate water and sanitation facilities, hygiene, well ventilated houses and no indoor pollution,proper stool disposal of children [8, 59, 60]. Consequently, tailored health education and promotional initiatives targeting caregivers or mothers from disadvantaged backgrounds, having lower educational levels, and are younger should be devised to prevent these illnesses in the area. Moreover, additional interventions focusing on enhancing water sources, sanitation, and family planning strategies should also be developed.
Authors’ contributions
Mukesh- Conceptualization,Data curation,Formal Analysis,Writing the first draft and reviewed Lalrotlinga-help in writing and analysis. Ashutosh- writing,Reviwed and edited the draft. Brajesh-Reviwed and edited the draft. Vanlalhriatsaka- helped in literature review and writing the manuscript.
Funding
No funding was obtained for this research, which was done as part of an MSc dissertation.
Availability of data and materials
The link for the publicly available free dataset is mentioned below
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UNICEF (2021). Diarrhoea- UNICEF DATA. https://data.unicef.org/topic/child-health/diarrhoeal-disease/
- 2.Ghosh K, Chakraborty AS, Sen Gupta S. Identifying spatial clustering of diarrhoea among children under 5 years across 707 districts in India: a cross sectional study. BMC Pediatr. 2023;23(1):272. 10.1186/s12887-023-04073-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Merid MW, Alem AZ, Chilot D, Belay DG, Kibret AA, Asratie MH, Aragaw FM. Impact of access to improved water and sanitation on diarrhea reduction among rural under-five children in low and middle-income countries: a propensity score matched analysis. Trop Med Health. 2023;51(1):1–10. 10.1186/s41182-023-00525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thapa B, Sapkota S, Hu Y. Predictors of diarrhea among children under 24 months in Nepal: A multilevel analysis of multiple indicator cluster survey 2019. PLoS ONE. 2023;18(7): e0287974. 10.1371/journal.pone.0287974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah D, Choudhury P, Gupta P, Mathew JL, Gera T, Gogia S, Menon S. Promoting appropriate management of diarrhea: a systematic review of literature for advocacy and action: UNICEF-PHFI series on newborn and child health, India. Indian Pediatr. 2012;49:627–49. 10.1007/s13312-012-0134-1. [DOI] [PubMed] [Google Scholar]
- 6. Ferdous J. Association between maternal level of education and recent episode of diarrhea among the children under age five in Bangladesh: evidence from Bangladesh Demography and Health Survey 2017 [Master’s Thesis in Global Health, Uppsala University]. 2023. FULLTEXT01.pdf (diva-portal.org).
- 7.International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-5), 2019–21: India. Mumbai; 2021. IIPSNFHS.
- 8.Paul P. Socio-demographic and environmental factors associated with diarrhoeal disease among children under five in India. BMC Public Health. 2020;20(1):1–11. 10.1186/s12889-020-09981-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hernández-Vásquez, A., Vargas-Fernández, R., & Cayo, E. Y. T. (2023). Determinants, inequalities, and spatial patterns of diarrhea in the Peruvian under-five population: findings from nationally representative survey data. Frontiers in Public Health, 11. 10.3389/fpubh.2023.1170670 [DOI] [PMC free article] [PubMed]
- 10.Chilot D, Diress M, Yismaw Gela Y, Sinamaw D, Simegn W, Andualem AA, Belay DG. Geographical variation of common childhood illness and its associated factors among under-five children in Ethiopia: spatial and multilevel analysis. Sci Rep. 2023;13(1):868. 10.1038/s41598-023-27728-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aggarwal R, Sentz J, Miller MA. Role of zinc administration in prevention of childhood diarrhea and respiratory illnesses: a meta-analysis. Pediatrics. 2007;119(6):1120–30. 10.1542/peds.2006-3481. [DOI] [PubMed] [Google Scholar]
- 12.UNDP. (2018). What are the Sustainable Development Goals? http://www.undp.org/content/undp/en/home/sustainable-development-goals.html.
- 13.Adeoti IG, Cavallaro FL. Determinants of care-seeking behaviour for fever, acute respiratory infection and diarrhoea among children under five in Nigeria. PLoS One. 2022;17(9): e0273901. 10.1371/journal.pone.0273901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rahman A, Hossain MM. Prevalence and determinants of fever, ARI and diarrhea among children aged 6–59 months in Bangladesh. BMC Pediatr. 2022;22(1):1–12. 10.1186/s12887-022-03166-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Debsarma D, Saha J, Ghosh S. Factors associated with delay in treatment-seeking behaviour for fever cases among caregivers of under-five children in India: Evidence from the National Family Health Survey-4, 2015–16. PLoS One. 2022;17(6): e0269844. 10.1371/journal.pone.0269844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghosh K, Chakraborty AS, Mog M. Prevalence of diarrhoea among under five children in India and its contextual determinants: A geo-spatial analysis. Clinical Epidemiology and Global Health. 2021;12: 100813. 10.1016/j.cegh.2021.100813. [Google Scholar]
- 17.Hasan MM, Saha KK, Yunus RM, Alam K. Prevalence of acute respiratory infections among children in India: Regional inequalities and risk factors. Matern Child Health J. 2022;26(7):1594–602. 10.1007/s10995-022-03424-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reddy VB, Kusuma YS, Pandav CS, Goswami AK, Krishnan A. Prevalence of malnutrition, diarrhea, and acute respiratory infections among under-five children of Sugali tribe of Chittoor district, Andhra Pradesh, India. Journal of natural science, biology, and medicine. 2016;7(2):155. 10.4103/0976-9668.184702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thota S, Ladiwala N, Sharma PK, Ganguly E. Fever awareness, management practices and their correlates among parents of under five children in urban India. International journal of contemporary pediatrics. 2018;5(4):1368. 10.18203/2349-3291.ijcp20182525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vatsa, R., Ranjan, M., Bhandari, P., & Gayawan, E. (2023). Analyzing Effect of WASH Practices and District-Level Spatial Effects on Acute Respiratory Infections and Diarrhoea Among Under-Five Children in India. Applied Spatial Analysis and Policy, 1–18. 10.1007/s12061-023-09512-3
- 21.Reddaiah VP, Kapoor SK. Effectiveness of ARI control strategy on under-five mortality. The Indian Journal of Pediatrics. 1991;58:123–30. 10.1007/BF02810425. [DOI] [PubMed] [Google Scholar]
- 22.Singh, A., & Singh, M. N. (2014). Diarrhoea and acute respiratory infections among under-five children in slums: Evidence from India (No. e208v1). PeerJ PrePrints. 10.7287/peerj.preprints.208v1
- 23.Townsend J, Greenland K, Curtis V. Costs of diarrhoea and acute respiratory infection attributable to not handwashing: the cases of India and China. Tropical Med Int Health. 2017;22(1):74–81. 10.1111/tmi.12808. [DOI] [PubMed] [Google Scholar]
- 24.Winskill P, Hogan AB, Thwing J, Mwandigha L, Walker PG, Lambert B. Health inequities and clustering of fever, acute respiratory infection, diarrhoea and wasting in children under five in low-and middle-income countries: a Demographic and Health Surveys analysis. BMC Med. 2021;19(1):1–11. 10.1186/s12916-021-02018-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghosh, A., Dey, S., & Singha, R. (2023). Environmental Health Problems Among Children in North Eastern States of India. Journal of Health Management, 09720634231196961. 10.1177/097206342311969
- 26.Lalneizo, D., & Reddy, S. (2010). Health status of children in North Eastern states of India. Indian Anthropologist, 37–52. https://www.jstor.org/stable/41920125
- 27.Thangjam M, Das M, Ladusingh L. Changes in Incidence of Morbidities of Children and its Determinants in Northeast India. Demography India. 2021;50(2):44–54. [Google Scholar]
- 28.Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, Fischer F. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–210. 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.UNICEF. (2021). Pneumonia in Children Statistics-UNICEF DATA. 2021. https://data.unicef.org/topic/child-health/pneumonia/
- 30.Ullah MB, Mridha MK, Arnold CD, Matias SL, Khan MSA, Siddiqui Z, Dewey KG. Factors associated with diarrhea and acute respiratory infection in rural Bangladesh children under two years of age. BMC Pediatr. 2019;19:1–11. 10.1186/s12887-019-1738-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Troeger C, Blacker BF, Khalil IA, Rao PC, Cao S, Zimsen SR, GBD (2016) Diarrhoeal disease collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the global burden of disease study 2016. Lancet Infect Dis. 2018;18(11):1211–28. 10.1016/S1473-3099(18)30362-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.IIPS. National family health survey (NFHS-4), 2015–16. Mumbai: International Institute for Population Sciences (IIPS); 2017. p. 791–846. NFHS.
- 33.Sample Registration System (SRS). Report on cause of death: 2001–03. New Delhi: Office of the Registrar General of India, Ministry of Home Affairs; 2009. SRS - Cause of Death | Government of India (censusindia.gov.in).
- 34.World Health Organization (WHO). Strategy for a coordinated approach to the prevention and control of acute diarrhoea and respiratory infection in the South-East Asia Region (No. SEA-CD-212). WHO Regional Office for South-East Asia; 2010. Strategy for coordinated approach to prevention and control of acute diarrhoea and respiratory infection the South-East Asia Region (who.int).
- 35.Fischer W, C. L., Perin, J., Aryee, M. J., Boschi-Pinto, C., & Black, R. E. Diarrhea incidence in low-and middle-income countries in 1990 and 2010: a systematic review. BMC Public Health. 2012;12:1–7. 10.1186/1471-2458-12-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.WHO (2017).Diarrheal disease. At: https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease
- 37.Million Death Study (MDS) Collaborators. Causes of neonatal and child mortality in India: a nationally representative mortality survey. The Lancet. 2010;376(9755):1853–60. 10.1016/S0140-6736(10)61461-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jain N, Lodha R, Kabra SK. Upper respiratory tract infections. The Indian Journal of Pediatrics. 2001;68:1135–8. 10.1007/BF02722930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vashishtha VM. Current status of tuberculosis and acute respiratory infections in India: much more needs to be done! Indian Pediatr. 2010;47(1):88–9. [DOI] [PubMed] [Google Scholar]
- 40.Mathew JL, Patwari AK, Gupta P, Shah D, Gera T, Gogia S, Menon S. Acute respiratory infection and pneumonia in India: a systematic review of literature for advocacy and action: UNICEF-PHFI series on newborn and child health, India. Indian Pediatr. 2011;48:191–218. 10.1007/s13312-011-0051-8. [DOI] [PubMed] [Google Scholar]
- 41.Marbaniang SP. Women care and practices in the management of childhood diarrhea in northeast India. Child Care Pract. 2023;29(2):139–51. 10.1080/13575279.2020.1812534. [Google Scholar]
- 42.Dikshit KR, Diskshit JK. North-East India: Land, People and Economy. Springer Science and Business Media; 2014. North-East India: Land, People and Economy | SpringerLink.
- 43.Hazarika M. Prehistoric Cultural Affinities Between Southeast Asia, East Asia and Northeast India: An Exploration. In Unearthing Southeast Asia’s Past, Selected Papers from the 12th International Conference of the European Association of South East Asian Archaeologists (Vol. 1, pp. 16–25). 2013. Prehistoric cultural affinities between Southeast Asia, East Asia and Northeast India: an exploration · Southeast Asian Archaeology Bibliographic Database (pennds.org).
- 44.Tripathi RS, Roy A, Kushwaha D, Lalnunmawia F, Lalnundanga LH, Lalnunzira C, Roy PS. Perspectives of forest biodiversity conservation in Northeast India. Journal of Biodiversity, Bioprospecting and Development. 2016;3(2):1–9. 10.4172/2376-0214.100015. [Google Scholar]
- 45.CDC. Disease Threats and Global WASH Killers: Cholera, Typhoid and other Waterborne Infections. Global Water, Sanitation and Hygiene(WASH). Centers for disease control and prevention. 2020. Global Hygiene | Global Water, Sanitation, and Hygiene (WASH) | CDC.
- 46.Nandi A, Megiddo I, Ashok A, Verma A, Laxminarayan R. Reduced burden of childhood diarrheal diseases through increased access to water and sanitation in India: A modeling analysis. Soc Sci Med. 2017;180:181–92. 10.1016/j.socscimed.2016.08.049. [DOI] [PubMed] [Google Scholar]
- 47.International Institute for Population Sciences (IIPS) and ICF. (2019). Interviewer Manual, National Family Health Survey (NFHS-5), 2019–21: India. Mumbai: IIPS https://rchiips.org/NFHS/NFHS5/manuals/NFHS-5%20Interviewer%20Manual_Eng.pdf
- 48.Ngandu NK, Manda S, Besada D, Rohde S, Oliphant NP, Doherty T. Does adjusting for recall in trend analysis affect coverage estimates for maternal and child health indicators? An analysis of DHS and MICS survey data. Glob Health Action. 2016;9(1):32408. 10.3402/gha.v9.32408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Overbey KN, Schwab KJ, Exum NG. Comparison of 1-week and 2-week recall periods for caregiver-reported diarrhoeal illness in children, using nationally representative household surveys. Int J Epidemiol. 2019;48(4):1228–39. 10.1093/ije/dyz043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Manesh AO, Sheldon TA, Pickett KE, Carr-Hill R. Accuracy of child morbidity data in demographic and health surveys. Int J Epidemiol. 2008;37(1):194–200. 10.1093/ije/dym202. [DOI] [PubMed] [Google Scholar]
- 51.Hasan MM, Saha KK, Yunus RM, Alam K. Prevalence of acute respiratory infections among children in India: Regional inequalities and risk factors. Matern Child Health J. 2022;26(7):1594–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bawankule R, Singh A, Kumar K, Shetye S. Does measles vaccination reduce the risk of acute respiratory infection (ARI) and diarrhea in children: a multi-country study? PLoS One. 2017;12(1): e0169713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Srivastava S, Mishra PS, Sinha D, Kumar P. Population attributable risk for breastfeeding practices on diarrhea and acute respiratory infections among children aged 0–23 months in India-What we know and we do not know? Child Youth Serv Rev. 2020;119: 105531. [Google Scholar]
- 54.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Remuzzi G. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128. 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vijayan B, Ramanathan M. Prevalence and clustering of diarrhoea within households in India: some evidence from NFHS-4, 2015–16. J Biosoc Sci. 2021;53(1):108–20. 10.1017/S0021932020000073. [DOI] [PubMed] [Google Scholar]
- 56.Bager P, Simonsen J, Ethelberg S, Frisch M. Cesarean delivery and risk of intestinal bacterial infection. J Infect Dis. 2010;201(6):898–902. 10.1086/650998. [DOI] [PubMed] [Google Scholar]
- 57.Laubereau B, Filipiak-Pittroff B, Von Berg A, Grübl A, Reinhardt D, Wichmann HE, Koletzko S. Caesarean section and gastrointestinal symptoms, atopic dermatitis, and sensitisation during the first year of life. Arch Dis Child. 2004;89(11):993–7. 10.1136/adc.2003.043265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Merenstein DJ, Gatti ME, Mays DM. The association of mode of delivery and common childhood illnesses. Clin Pediatr. 2011;50(11):1024–30. 10.1177/0009922811410875. [DOI] [PubMed] [Google Scholar]
- 59.Sarkar R, Sivarathinaswamy P, Thangaraj B, Sindhu KNC, Ajjampur SSR, Muliyil J, Kang G. Burden of childhood diseases and malnutrition in a semi-urban slum in southern India. BMC Pub Health. 2013;13:1–14. 10.1186/1471-2458-13-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.UNICEF (2019) .The state of the world’s children 2019: children, food and nutrition: growing well in a changing world.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The link for the publicly available free dataset is mentioned below